Safety and immunogenicity of heptavalent pneumococcal CRM ...
Transcript of Safety and immunogenicity of heptavalent pneumococcal CRM ...
nd mice ' basis. vodem! J<hes 1n .myc"
excreted
l Safety """oot
"""""' '"""'"" flocu1y :e from
of
W1{1f'I :essary
n cl.nal he Sode or
' slS\I.
grea1er
enol on
iencyot ·•11%1.
e of wolh a m(7%1.
lufts.
n!2%l
ol,
""" (2%1.
n adu t
toon
. and
rong e.
of
JIOI )'r.gas eed
ayfor
Perualr Infect Dis J , 1999;18:757~3 Copyright Q 1999 by Lippincott Williams & Wilkins, Inc.
~- ..
Vol. 18, No. 9 Printed in U.S.A.
Safety and immunogenicity of heptavalent pneumococcal CRM197 conjugate vaccine in infants and toddlers HENRY R. SHINEFIELD, MD, STEVEN BLACK, MD, PAULA RAY, MPH, IH CHANG, PHD, NED LEWIS, MPH, BRUCE FIREMAN, MA, JILL HACKELL, MD, PETER R. PARADISO, PHD, GEORGE SIBER, MD, ROBERT KOHBERGER, PHD, DACE V. MADORE, PHD, FRANK J. MALINOWSKI, MD,* ALAN KIMURA, MD, PHD,t CHINH LE, MD, IRENE LANDAW, MD, JANET AGUILAR, MD AND JOHN HANSEN, BA
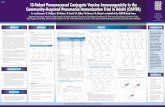
Objectives. The objectives of this study were (1) to determine the safety and immunogenicity of heptavalent pneumococcal CRM197 conjugate (PNCRM7) vaccine in infants and (2) to determine the effect of concurrent hepatitis B immunization during the primary series and the effect of concurrent diphtheria and tetanus toxoid and acellular pertussis [DTaP (ACEL-IMUNE)] and conjugate CRM197 Haemophilus influenzae type b [HbOC (HibTITER) immunization at time of the booster dose on the safety and immunogenicity of PNCRM7and these other concurrently administered vaccines.
Methods. This was a randomized doubleblinded study in 302 healthy infants in the Northern California Kaiser Permanente (NCKP) Health Plan. Infants received either PNCRM7 vaccine or meningococcal group C conjugate vaccine as a control at 2, 4 and 6 months of age and a booster at 12 to 15 months of age. Study design permitted the evaluation of immunology and safety of concurrent administration of routine vaccines. Antibody titers were determined on blood samples drawn before and 1 month after the primary series and the booster dose.
Results. After the third dose of PNCRM7 geometric mean concentrations (GMCs) ranged from 1.01 for serotype 9V to 3.72 µg/ml for serotype 14. More than 90% of all subjects had a post-third dose titer of 2::0.15 µg/ml for all serotypes, and the
Accepted for publication May 4, 1999. From the Kaiser Permanente Pediatric Vaccine Study Center
of Northern California, Oakland, CA (HRS, SB, PR, NL, BF, CL, IL, JA), and Wyeth Lederle Vaccines, Raonor, PA (IC, DM, JH, PP, GS, RK).
*Current address: Axis Genetics, Gaithersburg, MD. tCurrent address: Bio Chem Pharma, Northborough, MA. Key words: Conjugate heptavalent pneumococcal vaccine, con-
current administration. Address for reprints: Henry R. Shinefield, M.D., Ka iser
Permanente, Vaccine Study Center, 4131 Geary Blvd., San Francisco, CA 94118. E-mail [email protected].
757
percentage of infants with a post-third dose titer of ~1.0 µg/ml ranged from 51 % for type 9V to 89% for type 14. After the PNCRM7 booster dose, the GMCs of all seven serotypes increased significantly over both post-Dose 3 and pre-Dose 4 antibody levels. In the primary series there were no significant differences in GMCs of pneumococcal antibodies between the subjects given PNCRM7 alone or concurrently with hepatitis B vaccine. At the toddler dose concurrent administration of PNCRM7 and DTaP and HbOC resulted in a near conventional threshold for statistical significance of a post-Dose 4 GMC for serotype 23F [alone 6. 75 µg/ml vs. concurrent 4.11 µg/ml (P = 0.057)] as well as significantly lower antibody GMCs for H. influenzre polyribosylribitol phosphate, diphtheria toxoid, pertussis toxin and filamentous hemagglutinin. For all antigens there were no differences between study groups in defined antibody titers that are considered protective.
Conclusion. We conclude that PNCRM7 vaccine was safe and immunogenic. When this vaccine was administered concurrently at the booster dose with DTaP and HbOC vaccines, lower antibody titers were noted for some of the antigens when compared with the antibody response when PNCRM7 was given separately. Because the GMCs of the booster responses were all generally high and all subjects achieved similar percentages above predefined antibody titers, these differences are probably not clinically significant.
INTRODUCTION Despite the availability of multiple antimicrobial
agents and the development of capsular polysaccharide vaccines, S. pneumoniae remains one of the most important pathogens responsible for diseases in infants and children. As a result of the development of a successful conjugate vaccine against H. infiuenzae type
PTAB PAGE 1/7 MERCK EXHIBIT 1041
758 THE PEDIATRIC INFECTIOUS DISEASE JOURNAL Vol. 18, No. 9, Sept., 1999
b (Rib), the pneumococcus is now a primary cause of meningitis in infants and children.1 In addition up to 40% of cases of acute otitis media are caused by this organism.
2 Worldwide the pneumococcus is believed to
be responsible for a considerable proportion of the more than 4 to 5 million annual childhood deaths associated with respiratory disease. 3 This extensive disease burden as well as the increasing incidence of antimicrobial resistant pneumococci have resulted in efforts to dev~lop a successful anti-pneumococcal conjugate vaccme. . This repo~t.describes the evaluation of the safety and 1mmunogemc1ty of a heptavalent conjugate pneumococcal CPNCRM7) vaccine in infants and toddlers in the Northern California Kaiser Permanente (NCKP) Health Plan before its evaluation of efficacy.
PARTICIPANTS AND STUDY DESIGN After approval by the NCKP Institutional Review
Board in May, 1996, 2-month-old infants in six centers in NCKP were randomized 2:1 to receive either the PNCRM7 or meningococcal Group C conjugate vaccine as a control at -2, 4 and 6 months of age after ob:aining ?arental informed consent. All subjects received conjugate CRM197 H. infiuenzae type b, diphtheria, tetanus toxoid and whole cell pertussis [DTwPHbOC (TETRAMUNE)] and oral polio [OPV (ORIMUNE)) concurrently at each visit. In addition within each vaccine group one-half of the subjects wer~ given a concurrent injection of hepatitis B vaccine at each visit in the same right thigh as the DTwP-HbOC. The other half received the hepatitis B vaccine at least 2 w~eks before or after the investigational conjugate vaccmes. ~t 12 to 15 months of age subjects in each study vaccme group were further randomized in a 3:3:2 to re~eive either (1) a fourth dose of the conjugate study vaccme concurrently with diphtheria toxoid tetanus toxoid and acellular pertussis (DTaP (ACEL-ThfuNE)] and conjugate CRM197 H. infiuenzae type b [HbOC (HibTITER)] vaccines or (2) conjugate study vaccine a~o~e or (3) DTaP and HbOC alone. On the follow-up ~sit 1 month later, the subjects were given the vaccmes that they had not received at the first visit (no vaccination, DTaP and HbOC alone or the fourth dose of conjugate vaccine, respectively).
Vaccines. PNCRM7 contains polysaccharides of pneumococcal serotype 4, 6B, 9V, 14, 19F and 23F and oligosaccharide of serotype 18C which are conjugated to the protein carrier CRM (a nontoxic variant of d . h h . . ) 197 ip t ena toxin by reductive amination. Each sero-
type is co~jugated as a monovalent preparation before compoundmg as a multivalent vaccine. Each 0.5 ml contains 2 µ,g of saccharide of serotypes 4, 9V, 14, 18C, 19F and 23F an? 4 µ,g of serotype 6B along with - 20 µ,g of CRM197 earner protein and - 0.5 mg of aluminum phosphate as an adjuvant.
The meningococcal Group C conjugate vaccine was a Neisseria meningitidis Group C oligosaccharide coupled to CRM197 by reductive amination. Each 0.5-ml dose contains 4 µ,g/ml of saccharide with 1.0 mg/ml aluminum phosphate as an adjuvant.
The OPV and DTwP-HbOC administered were Food and Drug Administration-approved commercial vaccines both manufactured by Wyeth-Lederle.
Assessment of safety. The parents/guardians of each subject were given a diary report card and a digital thermometer and asked to monitor untoward effects for 14 days after each vaccination. This included recording temperature for 2 days and at any other time that the subject appeared febrile. Evidence and extent of inflammation, induration or swelling at the injection site were also recorded. Telephone interviews of parents/guardians were conducted at 48 to 72 h and 10 to 14 days after receipt of each dose of vaccine to collect information regarding local and systemic side effects. To further assess vaccine safety emergency room utilization rates 30 days after vaccination as well as hospitalization rates 60 days after vaccination for specific diagnosis were compared within the NCKP through the use of comprehensive databases.
Evaluation of immunogenicity. To evaluate the immunogenicity of the study vaccine and any potential for interference with routine childhood immunizations, serum specimens were obtained just before the first dose of study vaccine, 1 month after the third dose of study vaccine, before the toddler booster dose and 1 month after the toddler dose. Specimens were labeled and sent to Wyeth Lederle laboratories for blinded analysis for antibodies to the seven pneumococcal serotypes as well as serologic responses to Rib polyribosylribitol phosphate (PRP), diphtheria, tetanus, pertussis, hepatitis B and polio antigens. Standard enzyme-linked immunosorbent assay4 (ELISA) was used to quantitate serum IgG to each of the seven pneumococcal vaccine serotypes. ELISA units were expressed as micrograms/ml with the use of standard reference serum 89SF. The lower quantitation limit of the assay is 0.01 µg/ml for all seven serotypes. Any concentration below that limit was reported as 0.005 µ,glml.
Standard ELISA methods were used for determining antibodies to diphtheria, tetanus, Hib PRP, pertussis toxin, pertussis fimbriae, pertussis filamentous hemagglutinin and pertussis pertactin. Antibodies to poliovirus (Sabin strains 1, 2, 3) were determined by neutralization assay. Poliovirus antibody titers ~1:10
represent immunity. The anti-hepatitis B surface antigen enzyme immunoassay (AUSAB; Abbott Laboratories, North Chicago, IL) kit was used to determine anti-hepatitis B surface antigen antibody concentrations. Antibody concentration was expressed as
PTAB PAGE 2/7 MERCK EXHIBIT 1041
'1999
was a e cou-0.5-ml mg/ml
a Food .I vac-
ms of and a oward ~luded
rtime axtent ection ,f parl 10 to ::ollect :ffects. 1 utilihospi?ecific rough
te the en ti al .tions, ) first ose of and 1 ibeled inded al seyribo, per-1dard 1 was seven were
1dard nit of . Any 0.005
ining ;us sis hempolio-neu~1:10
e anboramine ntrad as
Vol. 18, No. 9, Sept., 1999 THE PEDIATRIC INFECTIOUS DISEASE JOURNAL 759
TABLE 1. Geometric mean concentrations of pneumococcal antibody in recipients of pneumococcal (PNCRM7) and control vaccines
Geometric Menn Concentration (µg/ml)
Sero- Prevnccinntion Post-Dose 3 Mean fold type rise in
PNCRM7 Control PNCRM7 Control PNCRM7
N 156 82 156 82 4 0.10 0.08 1.30 0.02 13.7
(0.08-0.11)* (0.06-0.10) (1.13-1.50) (0.02-0.03) (10.6-17.6) 6B 0.31 0.32 1.22 0.07 3.9
(0.25-0.38) (0.23-0.45) (0.98-1.53) (0.05-0.09) (2.9-5.5) 9V 0.19 0.18 1.01 0.04 5.2
(0.17-0.23) (0.14-0.22) (0.88-1.16) (0.03-0.05) (4.2-6.5) 14 0.39 0.30 3.72 0.o7 9.6
(0.29-0.52) (0.19-0.48) (3.16-4.38) (0.05-0.09) (6.6-14.0) 18C 0.18 0.16 1.44 0.03 7.9
(0.15-0.22) (0.13-0.21) (1.25-1.65) (0.02-0.03) (6.2-10.0) 19F 0.40 0.30 1.95 0.05 4.9
(0.32- 0.49) (0.22-0.42) ( 1.62-2.34) (0.04-0.06) (3.6-6.6) 23F 0.18 0.16 2.54 0.03 13.8
(0.15-0.23) (0.11-0.20) (2.13-3.02) (0.02-0.03) (10.1-18.8)
• Numbers in parentheses, 95% confidence interval.
mIU/ml with the use of WHO hepatitis B immunoglobulin Reference Preparation No. 26-1-1977. An antibody concentration of ~10 mIU/ml was considered seropositive.
Statistical methods. Subjects were included in the immunogenicity analysis if they were vaccinated according to protocol schedule and the post-Dose 3 (or 4) blood draw was within 21 to 63 days after dosing. All subjects with available data were included in the safety analysis. The geometric means of antibody concentrations (GMC) to pneumococcal serotypes were determined for each vaccine group at each time point as well
12
..-. e ]>10
!.. d 0 ·c {; d ... v d 0
8
u 6 d .. ... ~ v
'.S 4 ... B
~ 2
0
Pre booster Postbooster Mean fold rise in
PNCRM7 Control PNCRM7 Control PNCRM7
87 49 87 49 0.23 0.02 1.76 0.03 7.5
(0.20-0.28) (0.02-0.03) (1.41-2.20) (0.03-0.04) (6.1-9.2) 0.71 0.14 9.05 0.16 12.7
(0.54-0.94) (0.11-0.19) (6.64-12.36) (0.12-0.22) (9.4-17.1 ) 0.39 0.06 3.16 0.07 8.0
(0.33-0.47) (0.04-0.07) (2.56-3.88) (0.06-0.10) (6.5-9.8) 1.94 0.04 10.46 0.03 6.4
(1.59-2.38) (0.03-0.05) (8.46-12.93) (0.03-0.04) (4.5-6.5) 0.33 0.06 2.84 0.07 8.6
(0.28-0.39) (0.04-0.09) (2.26-3.57) (0.05-0.11) (6.8-11.0) 0.56 0.09 3.04 0.13 5.5
(0.44-0.71) (0.07-0.13) (2.35-3.95) (0.09-0.18) (4.2-7.2) 0.61 0.04 5.25 0.06 10.3
(0.39- 0.66) (0.03-0.06) (4.07-6.79) (0.04-0.07) (8.2-13.0)
as the proportion of children achieving at least 0.15 and 1 µ.g/ml of concentrations. A two-sample t test (on logarithmic scale) was used to compare the post-third dose GMC to pneumococcal serotypes in the group receiving PNCRM7 and concurrent hepatititis B with that in the goup receiving no concurrent hepatitis B. Similarly the post-booster dose GMC of the group receiving DTaP and HbOC concurrently with PNCRM7 was compared with that of the group receiving booster doses of PNCM7 alone by two-sample t test or Wilcoxon rank sum test, depending on the concentration distribution of each serotype. A comparison of the GMC to
4 68 9V 14
Serotype IRC 19F 23F
= pre dose I = post dose 3 - pre boost = post boost
FIG. 1. GMC responses and confidence interval to each serotype in subjects receiving primary and booster doses of PNCRM7.
PTAB PAGE 3/7 MERCK EXHIBIT 1041
760 THE PEDIATRIC INFECTIOUS DISEASE JOURNAL Vol. 18, No. 9, Sept., 1999
100 ,....--~~~~~~~~~-=:;-~~~~~~~-, Immunogenicity. A substantial immunologic response was elicited to all 7 pneumococcal serotypes by PNCRM7. However there was a marked difference in response to individual serotypes both in the primary and toddler responses as well as to the degree of antibody decay that followed the third dose of vaccine. GMCs after the third vaccine dose ranged from a low of 1.01 µg/ml for serotype 9V to a high of 3.72 µg/ml for type 14 (Table 1; Fig. 1). After the primary series in the subjects who received PNCRM7, there was a marked drop in antibody concentration for all serotypes before the booster dose. The preboost toddler titer fell to a low of 0.23 for type 4 to a high of 1.94 µg/ml for type 14. Approximately 1 month postboost all GMCs were well above 1 µg/ml. The lowest GMC was with type 4 (1.8 µg/ml) and the highest again with type 14 (10.46 µg/ml ) (Table 1; Fig. 1). More than 90% of all subjects had a post-third dose titer of ~0.15 µg/ml for all serotypes and the percentage of infants with a postthird dose titer ~1.0 µg/ml ranged from 51% for type 9V to 89% for type 14 (Fig. 2).
90-l--~~~--.:=-~--t?.5-~4
80+-----t
70 +-----.....---;
60
50
40
30
20
10
o.i..u.:- =-,....,.,. 4 SB 9V 14 18C
~ost dose 3 • pre dose 4 fl! post d~e 4] 23F
FIG. 2. Proportion of children with antibody concentration 2: 1 µg/ml.
each antigen in the concurrent DTaP and HbOC vaccines was also made by two-sample t test between the group receiving a booster dose ofDTaP and HbOC with concurrent PNCRM7 and the group receiving DTaP and HbOC alone. Comparisons of proportion of children achieving at least a given level of concentrations between groups were made by Fisher's exact test in all cases. A within subject comparison oflocal reactions at injection site of PNCRM7 and the site of the concurrent DTP/HbOC (TETRAMUNE) was made using sign test for the first three doses.
RESULTS Enrolled in the study 302 healthy infants 2 months
of age with 272 completing the 3-dose primary series, and 211 of the original subjects were rerecruited for the booster dose. Characteristics of the subjects were generally evenly distributed between the groups. A total of 38 subjects were discontinued from the study. The reasons for withdrawal were adverse events (3), parental request (10), lost to follow-up (including left health plan) (17), protocol deviation (7) and OPV contraindication because a family member was receiving chemotherapy (1).
In the group of infants who received meningococcal Group C conjugate vaccine the post-Dose 3 pneumococcal GMCs ranged from 0.02 for serotype 4 to 0.07 µg/ml for serotypes 6B and 14. After the booster dose in the controls the pneumococcal GMCs ranged from 0.03 to 0.16 µg/ml. The percentage of control subjects with a post-third dose anti-pneumococcal titer of ~0.15 µ.g/ml ranged from 1 % (type 4) to 22% (type 14).
Within the PNCRM7 treatment group, 81 subjects (51.9%) received hepatitis B (Hep B) concurrently with PNCRM7 at 2, 4 and 6 months of age and 75 subjects (48.1%) received hepatitis B vaccine at least 2 weeks apart from study vaccine. The post-Dose 3 GMCs for all pneumococcal serotypes in both study groups were significantly greater than the predose antibody titers. For all serotypes there was no significant difference in the GMCs between groups (Table 2). More than 95% of subjects in each subgroup responded with an antibody titer of ::::0.15 µg/ml except for type 6B; 90.1 and 89.3% achieved this level in the concurrent hepatitis and
TABLE 2. Comparison of GMCs and percent of subjects with defined pneumococcal antibody levels after a primary series of PNCRM7 with and without hepatitis B vaccine
PNCRM7/Hep B (N = 81) PNCRM7 (N = 75)* p
Type A. B. c. D. E. F.
GMT 2:0.15 µg/ml 2:1.0 µg/ml GMT 2:0.15 µglml 2:1.0 µg/ml A vs. Dt B vs. E:j: C vs. F:j:
4 1.4 98.8 67.9 1.2 97.3 61.3 0.320 0.608 0.407 6B 1.3 90.l 56.8 1.1 89.3 53.3 0.385 > 0.99 0.748 9V 1.1 98.8 54.3 1.0 97.3 46.7 0.396 0.608 0.423 14 3.2 100 80.3 4.4 100 98.7 0.067 < 0.001 18C 1.5 98.8 74.1 1.4 100 66.7 0.655 > 0.99 0.380 19F 2.1 97.5 81.5 1.8 97.3 82.7 0.390 > 0.99 > 0.99 23F 2.9 100 85.2 2.2 96.0 77.3 0.070 0.109 0.224
• N 14 for serotype 14. t P values comparing the GMCs between PNCRM7 and PNCRM7/hepatitis B groups were based on analysis of covariate and concurrent hepatitis B as a clnssificntion vanable. * P values assess t.he difference between PNCRM7 and PNCRM7/hepalitis B groups by Fisher's exact test (two-sided).
Vol. U
PNCR! cant dJ was n~ 98.7% with e 85.2% hepati vaccin1 percen ters fo polio t: 100 ar
For CRM7 this VI
(Table old fo1 rate u' vs. 4.1 resp or were E
the pr tion of these
Si gt noted the pe comp;; as ab in bot body of:::: 0 97.9~ re spec titer f
Saf theD' after 1 site vi
series
TABJ
Type
4 6B 9V 14 18C 19F 23F
•Pva instead t
+ P val
PTAB PAGE 4/7 MERCK EXHIBIT 1041
., 1999
gic rerpes by mce in rimary ~ree of accine. t low of /ml for ; in the riarked before o a low rpe 14. re well 4 (1.8 (10.46 ibjects for all i. post>r type
lCOCCal
mococµg/ml in the ).03 to with a µg/ml
ibjects ywith ibjects weeks for all were
titers. nee in ::J5%of tibody 89.3% s and
'ies of
Ft
W7 748 123 )01 180 l9 l24
•ariable.
Vol. 18, No. 9, Sept., 1999 THE PEDIATRIC INFECTIOUS DISEASE JOURNAL 761
PNCRM7 alone groups, respectively. The only significant difference between groups for GMC 2": 1.0 µg/ml was noted for serotype 14 [concurrent 80.3% vs. alone 98.7% (P < 0.001). For other serotypes the percentage with antibody levels ?:1.0% was between 46.7 and 85.2% (Table 2). When the response to concurrent hepatitis vaccine (based on 81 subjects) and oral polio vaccine (based on 146 subjects) was evaluated, the percentage of subjects achieving defined antibody titers for hepatitis (?: 10 mill/ml), polio type 1 (?: 1: 10), polio type 2 (?:1:10) and type 3 (?:1:10) was 92.6, 95.2, 100 and 97.9%.
For all serotypes GMCs were higher when the PNCRM7 vaccine was given alone as opposed to giving this vaccine with DTaP and HbOC as a booster dose (Table 3). However, the only near conventional threshold for statistical difference seen in response to separate vs. concurrent PNCRM7 was to serotype 23F (6.67 vs. 4.13 µ,g/ml (P = 0.057)) . The proportion of children responding with antibody concentrations > 0.15 µg/ml were similar for both groups. For all seven serotypes the proportion of subjects with an antibody concentration of > 1.0 µg/ml in no case differed by > 10% between the separate and concurrent regimens.
Significant differences in antibody GMCs were also noted for Hib PRP, for diphtheria toxoid and for some of the pertussis antigens when PNCRM7 was given alone compared with giving it together with DTaP and HbOC as a booster dose (Table 4). However, 100% of subjects in both groups achieved diphtheria and tetanus antibody titers of ?:0.01 IU/ml. Hib PRP antibody titers of ?: 0.15 µg/ml were 100% for both groups and 100 and 97.9% at ?:1.0 µg/ml for PNCRM7 alone vs. combined, respectively. There was a 4-fold rise from the predose titer for all four pertussis antigens in both groups.
Safety. Injection site reactogenicity was greater for the DTwP-HbOC/Hep B than for the PNCRM7 vaccine after each primary series dose. Rates at the PNCRM7 site vs. DTwP-HbOC/Hep B site ranged across primary series doses as follows: erythema, 16 to 18% vs. 18 to
TABLE 4. Geometric mean concentrations of antibodies to DTaP and HbOC after the booster dose with or without
concurrent 7VPnC administration
Treatment Group
Antigen Units 7VPnC
P* DTaP/HbOC concurrent (N = 26) DTaP/HbOC
(N= 47)
Haemphilus µg/ml 47.9 22.7 0.020 infiuenzae PRP
Diphtheria toxoid IU/ml 3.2 2.0 0.027 Tetanus toxoid IU/ml 18.8 14.4 0.146 Pertussis toxoid EU/ml 121.2 68.6 0.015 Filamentous EU/ml 48.2 29.0 0.040
hemagglutinin Fimbriae 2 EU/ml 3.8 5.2 0.477 Pertactin EU/ml 83.0 84.4 0.950
* P value assesses the difference between treatment groups with n t test (two sided). EU, enzyme immunoassay unit.
29%; induration, 9 to 11 % vs. 19 to 21 %; tenderness, 21 to 24% vs. 26 to 28% and were statistically less severe at the PNCRM7 site than at the DTwP-HbOC sites (Table 5). After the booster dose of PNCRM7 or PNCRM7 along with DTaP and HbOC, the rates of local reactogenicity between sites were similar: erythema, 9.1 vs. 6.1 (P = 0.35); induration, 6.4 vs. 3.7% (P = 0.30); and tenderness, 15.5 vs. 9.8% (P = 0.16)].
For assessment of systemic reactions after the primary series, because all subjects received DTwP-HbOC and study vaccine at the same time it was not possible to determine the events specifically contributed by PNCRM7 over that which would occur after DTwPHbOC only. The rate offever ?:38.0°C within 48 h after each primary series dose was 21.5, 33.5 and 29.6%, respectively. Irritability in the primary series ranged from 58.1 to 68.9%. For the toddlers' dose there were no significant differences in these events among those subjects who received PNCRM7 concoinitantly with DTaP and HbOC or DTaP and HbOC alone; fever ?:38°C within 48 h after the booster dose was 11.0 and 16.2% (P = 0.31), and irritability was 47.6 and 38.1% (P = 0.87), respectively.
TABLE 3. Comparison of GMCs and proportion of children with defined pneumococcal antibody concentrations after booster dose of PNCRM7, DTaP and HbOC with those receiving PNCRM7 alone
PNCRM7, DTaP, HbOC (N = 47) PNCRM7 Alone (N = 40) P (Post-Dose 4)
Type 2:0.15 µ.g/ml 2: 1.0 µ,g/ml 2:0.15 µg/ml 2:1.0 µ.g/ml
A. B. c. D. E. F. G. H. I. J. A us. F* C us. Ht E us. J t GMT Pre-Dose 4 Post-Dose 4 Pre-Dose 4 Post-Dose 4 GMT Pre-Dose 4 Post-Dose 4 Pre-Dose 4 Post-Dose 4
4 1.6 68.1 100 2.1 70.2 2.0 68.3 100 9.8 67.5 0.395 1.00 0.819 6B 7.2 89.4 97.9 31.9 85.l 11.8 90.2 100 41.5 94.9 0.081 1.00 0.174 9V 2.8 93.6 100 8.5 87.2 3.6 85.4 100 19.5 94.9 0.263 1.00 0.283 l4 8.8 97.9 100 74.5 97.9 12.8 100 100 75.6 100 0.088 1.00 LOO 18C 2.9 87.2 100 0 89.4 3.0 85 100 10.0 82.1 0.917 1.00 0.365 19F 2.8 89.4 97.9 19.2 83.0 3.3 85 100 27.5 85.0 0.567 1.00 1.00 23F 4.1 80.9 100 25.5 87.2 6.8 92.5 100 25 95 0.057 1.00 0.279
• P values were based on t test on concentrations on log scale for all serotypes except 68. Serotype 6B data showed nonnormal distribution and the \Vilcoxon rank sum test was used instead of the t test.
t P values were based on fisher's exact test.
PTAB PAGE 5/7 MERCK EXHIBIT 1041
762 THE PEDIATRIC INFECTIOUS DISEASE JOURNAL Vol. 18, No. 9, Sept., 1999
TABLE 5. Local reactions within 48 h of injection* among infants receiving DTwP-HbOC, OPV, hepatitis Bt and PNCRM7 and toddlers receiving DTaP and HbOC and
PNCRM7
Reaction N PNCRM7 D'l\vP-HbOC DTaP + HbOC
Redness Dose 1 183 Dose 2 159 Dose 3 160 Dose 4 110
Swelling Dose 1 183 Dose 2 159 Dose 3 160 Dose 4 110
Tenderness Dose 1 183 Dose 2 159 Dose 3 160 Dose 4 110
• Telephone interviews.
(%) (%) (%)
17.0 18.0 18.0 29.0 16.0 22.0 9.1
10.0 19.0 11.0 20.0
9.0 21.0 6.4
24.0 27.3 21.0 26.0 23.0 28.0 15.5
>0.999 0.002 0.122
6.1 0.350
0.008 0.007
<0.001 3.7 0.302
0.383 0.144 0.057
9.8 0.155
t One-half of infants m each treatment group were randomized to receive hepatitis B vaccine simultaneously with PNCRM7, DTwP-HbOC and OPV. * P value with sign test ; assesses difference between PNCRM7 and DTwP-HbOC/
hepatit.is B iajection sites for Doses 1, 2, 3; and difference between PNCRM7 and DTaP + HbOC for Dose 4.
There were 12 emergency room visits that occurred within 30 days of any dose in study participants. They included croup, otitis, febrile illness and urinary tract infection. All were considered not vaccine-related. One hypotensive hyporesponsive episode that occurred 15 min after receiving PNCRM7, DTwP-HbOC/Hep and OPV with complete recovery within 1 h was considered as possibly vaccine-related. There were 8 hospitalizations after primary series doses of vaccines. None was considered to be vaccine-related. Two occurred <30 days after vaccination (perianal infection, rule out sepsis). After the booster dose there were 4 emergency room visits (viral illness, 2 otitis media and burn) and 5 hospitalizations (pneumonia, otitis media, elective surgery, asthma and cough). None were thought to be vaccine-related.
DISCUSSION PNCRM7 is an immunogenic vaccine in infants.
However, each serotype contained in the vaccine acted as an immunologically independent agent. There was a quantitative difference among serotypes in both the primary antibody responses as well as in the antibody decay after the primary three-dose series. After the booster dose there was an amnestic response but with a marked serotype variation. These data are similar to those reported by Rennels et al.5 who studied the same heptavalent conjugate vaccine.
A fundamental question is the amount of antibody necessary to protect against invasive pneumococcal disease. At present there is no defined protective pneumococcal antibody concentration. Animal and other human data suggest a range between 0.06 and 2.9 µ,g/ml. 6
-8 Protection against pneumococcal disease rep-
resents a greater challenge than that encountered by Hib disease. With Rib conjugate vaccine the production of antibody against a single antigen was protective. To be protected from pneumococcal disease antibody is required for >80 serotypes. For acute pneumococcal otitis media local antibody production may be protective, although previous studies suggest that serum antibody also plays a role. Precise protective titers can not be determined from these earlier data. 6•
9•
10
Our study design permitted us to evaluate the effect on antibody titers when PNCRM7 was given concomitantly or separately with some of the other routine infant vaccines. During the primary series concurrent administration of PNCRM7 alone or with hepatitis B resulted in similar pneumococcal GMCs of antibodies in both groups. Antibody responses to hepatitis B and polio vaccine were also within expected ranges.
After the booster dose a near conventional threshold for statistical significance for type 23F was noted when the PNCRM7 vaccine was given at the same time as DTaP and HbOC compared with PNCRM7 given alone. However, the pneumococcal antibody titers in these subjects (4.1 µg/ml) were considerably higher than any titer proposed as necessary for protection. Despite statistically significant lower GMCs for Rib PRP, diphtheria toxoid and pertussis antibodies when these vaccines were given concurrently with PNCRM7, the concentrations of antibodies that were produced were above those considered to be protective.11
-15 At defined
endpoints there was no difference in response to any antigen after the administration of the primary series of vaccines or after the toddler booster dose.
Although the lower antibody titers observed after concomitant administration of vaccines did not seem to be clinically significant in our study, this was not the case in some of the studies involving other vaccines. For example combining DTaP and Hib vaccines decreased Rib antibody titers 10-fold to a concentration considered clinically unacceptable.16 Interference resulting in reduced antibody concentrations have been noted with viral vaccines as well. 17
· 18 In the case of
bacterial vaccines recent data suggest that the phenomenon of interference is the result of simultaneous administration of vaccines sharing common protein epitopes. 19 Therefore the possibility of depressed antibody concentrations must be considered and appropriate studies done before proposing the simultaneous administration of vaccines for clinical practice.
PNCRM7 appears to be a safe vaccine. The local reaction rate and systemic reaction rate are similar to those seen with other licensed infant vaccines.20 No unusual untoward reactions were seen in our study cohort.
CONCLUSION We conclude that PNCRM7 vaccine was safe and
Vol. 18
immune concurr vaccine the ant sponse Becaus1 general centage probab]
ACKNC This I
Vaccines
REFEF 1. Sch1.1
gitis 970-
2. Klei1 Coul ferer 1979
3. Shat op in
4. Qua1 weig stan 199f
5. Rem imm gate 101:
6. Shl.ll sacc med
7. Rub Jar expE ceed Age1 to 21 olog
8. Sala Flei (BP.
PTAB PAGE 6/7 MERCK EXHIBIT 1041
'1999
red by .uction ive. To ody is )COCcal Jrotecserum !TS can
! effect ncomioutine urrent titis B bodies Band
eshold lwhen Liile as alone. these
many >espite 'diph-these
(7, the :l were .efined to any series
I after eem to wt the ::cines. es de:ration 1ce ree been :ase of e pbemeous irotein :l anti)roprimeous
~ local ilar to _20 No study
fe and
Vol. 18, No. 9, Sept., 1999 THE PEDIATRIC INFECTIOUS DISEASE JOURNAL 763
immunogenic. When this vaccine was administered concurrently at the booster dose with DTaP and HbOC vaccines, lower antibody titers were noted for some of the antigens when compared with the antibody response when PNCRM7 was not given concurrently. Because the GMCs of the booster responses were all generally high and all subjects achieved similar percentages above predefined levels, these differences are probably not clinically significant.
ACKNOWLEDGMENT This study was supported by a grant from Wyeth-Lederle
Vaccines.
REFERENCES 1. Schuchat A, Robinson K, Wenger JD, et al. Bacterial menin
gitis in the United States in 1995. N Engl J Med 1997;337: 970-6.
2. Klein JO. The microbiology of otitis media. In: Wiet RJ, Coulthard SW,eds. Proceedings of the Second National Conference on Otitis Media. Columbus, OH: Ross Laboratories, 1979;43-6.
3. Shann F. Etiology of severe pneumonia in children in developing countries. Pediatr Infect Dis 1986;5:247-52.
4. Quataert SA, Kirch CS, Wied! W, et al. Assignment of weight-based antibody units to a human antipneumococcal standard reference serum lot 89-S. Clin Diagn Lab Immunol 1995;2:590- 7.
5. Rennels MB, Edwards KM, Keyserling HL, et al. Safety and immunogenicity of heptavalent pneumococcal vaccine conjugated to CRM197 in United States infants. Pediatrics 1998; 101:604-11.
6. Shurin PA, Rehmus JM, Johnson CE, et al. Bacterial polysaccharide immune globulin for prophylaxis of acute otitis media in high risk children. J Pediatr 1993;123:801-10.
7. Rubin LG, Mardy GV, Pais L, Carlone G. Human anticapsular antibody concentration required for protection against experimental pneumococcal bacteremia [Abstract G47). Proceedings of the 35th Interscience Conference of Antimicrobial Agents and Chemotherapy, San Francisco, CA, September 17 to 20, 1995. Washington, DC: American Society for Microbiology, 1995.
8. Saladino RA, Stack AM, Malley R, Thompson CM, Siber CR, Fleiser GO. Bacterial polysaccharide immune globulin CBPIG) protects infant rats with S. pneumoniae (SP) pneu-
monia from bacteremia, meningitis and death. Pediatr Res 1996;36:184A.
9. Giebink GC, Koskela M, Vella PP, et al. Pneumococcal capsular polysaccharide-meningococcal outer membrane protein complex conjugate vaccines: immunogenicity and efficacy in experimental pneumococcal otitis media. J Infect Dis 1993;167:347-55.
10. Teele DW, Klein JO, Bratton Let al. Use of pneumococcal vaccine for prevention of recurrent acute otitis media in infants in Boston. Rev Infect Dis 1981;3:S113-8.
11. Robbins JB, Parke JC Jr, Schneerson R, Whisnant JK. Quantitative measurement of "natural" and immunizationinduced H. influenzae type b capsular polysaccharide antibodies. Pediatr Res 1973;7:103-10.
12. Kayhty H, Peltola H, Karanko V, Makela PH. The protective level of serum antibodies to the capsular polysaccharide of Haemophilus influenzae type b. J Infect Dis 1983;147:1100.
13. Anderson P. The protective level of serum antibodies to the capsular polysaccharide of Haemophilus influenzae type b. J Infect Dis 1984;149:1034-5.
14. Volk VK, Gottshall RY, Anderson HD, et al. Antigenic responses to booster dose of diphtheria and tetanus toxoids: seven to thirteen years after primary inoculation of noninstitutionalized children. Public Health Rep 1962;77:185-94.
15. McComb JA. The prophylactic dose of homologous tetanus antitoxin. N Engl J Med 1964;270:175-8.
16. Eskola J, Olander RM, Hovi T, et al. Randomised trial of the effect of co-administration with acellular pertussis DTP vaccine on immunogenicity of Haemophilus influenzae type b conjugate vaccine. Lancet 1996;348:1688-92.
17. Watson BM, Laufer DS, Kuter BJ, et al. Safety and immunogenicity of a combined live attenuated measles, mumps, rubella, and varicella vaccine (MMRR11V) in healthy children. J Infect Dis 1996;173:731-4.
18. Shinefield HR, Black SB, Staehle BO, et al. Safety, tolerability and immunogenicity of concomitant injections in separate locations of M-M-R®11, VARIVAx® and TETRAMUNE® in healthy children us. concomitant injections of M-M-R®-1! and TETRAMUN~ followed six weeks later by VARIVAX"". Pediatr Infect Dis J 1998;17:980-5.
19. Dagan R, Eskola J , Leclerc C, Leroy 0. Reduced response to multiple vaccines sharing common protein epitopes that are administered simultaneously to infants. Infect Immun 1998; 66:2093-8.
20. Black SB, Shinefield HR, Ray P, et al. Safety of combined oligosaccharide conjugate Haemophilus infiuenzae type b (HbOC) and whole cell diphtheria-tetanus toxoids-pertussis vaccine in infancy. Pediatr Infect Dis J 1993;12:981.
Announcement Second World Congress of Pediatric Infectious Diseases. November 2 to 6, 1999, Manila, Philippines.
Full information with regular updates can be found on the Web page at www.wspid.com. To contact the Organizing Secretariat for printed announcements, please contact Ian Shepherd. Tel.: ( +52 5)661 7505; Fax: ( +52 5)662 9964; E-mail: [email protected].
PTAB PAGE 7/7 MERCK EXHIBIT 1041