Running head: IMPLEMENTING A RISK INDEX TOOL 1 · Figure 4 2016 Patient Population by Age and Sex...
Transcript of Running head: IMPLEMENTING A RISK INDEX TOOL 1 · Figure 4 2016 Patient Population by Age and Sex...
Running head: IMPLEMENTING A RISK INDEX TOOL 1
A Quality Improvement Project: Implementing a Risk Index Tool to Guide
Naloxone Prescribing in Patients on Chronic Opioid Therapy
Peggie L. Powell
VCU School of Nursing – DNP Program
DNP Project Advisor: Holly Buchanan, DNP, ANP-BC
DNP Project Content Expert: Manhal Saleeby, MD
DNP Project Team Member: Juli J. Moseley, PharmD
IMPLEMENTING A RISK INDEX TOOL 2
Table of Contents
List of Tables ................................................................................................................................. 4
List of Figures ................................................................................................................................ 5
Abstract .......................................................................................................................................... 6
Introduction .................................................................................................................................... 7
Problem Statement ......................................................................................................................... 8
Purpose ............................................................................................................................. 10
Clinical Question ...…………………............…….......................................................... 10
Review of the Literature .............................................................................................................. 11
Background and Significance ...................................................................................................... 22
Conceptual Framework .................................................................................................... 24
Needs Assessment ............................................................................................................ 25
Key Stakeholders ............................................................................................................. 31
Barriers and Facilitators ................................................................................................... 33
Benchmarks ...................................................................................................................... 34
Budget .............................................................................................................................. 35
Project Description........................................................................................................................ 37
Project Mission ................................................................................................................ 38
Goals and Objectives ....................................................................................................... 38
Outcome Measures ........................................................................................................... 39
Project Design .............................................................................................................................. 42
Methods ............................................................................................................................ 42
Potential Risks and Threats .............................................................................................. 49
IMPLEMENTING A RISK INDEX TOOL 3
Project Evaluation Plan ................................................................................................................ 50
Data Analysis Plan ........................................................................................................... 53
Discussion and Implications ........................................................................................................ 55
Clinical Implications ........................................................................................................ 56
DNP Essentials ................................................................................................................. 57
Quality and Safety ............................................................................................................ 57
Plan for Sustainability ...................................................................................................... 58
References .................................................................................................................................... 64
Appendix A Flow Diagram of the Search Process ................................................................... 71
Appendix B RIOSORD Tool used in the Veterans’ Health Administration ........................... 72
Appendix C RIOSORD Tool used in the Commercial Insurance Population ......................... 73
Appendix D Proposed DNP Project Budget ............................................................................. 74
Appendix E The Stetler Model of Research Utilization .......................................................... 75
Appendix F Example of a Naloxotel Comprehensive Progress Note ..................................... 76
Appendix G Example of a Naloxotel Prior Authorization Letter ............................................. 77
Appendix H Opioid Overdose Symptoms and Resuscitation Instructions ............................... 78
Appendix I Nurse Checklist for Naloxone Training ............................................................... 79
Appendix J Overdose Prevention Tips and Naloxone Resources ........................................... 80
Appendix K Proposed DNP Project Timeline .......................................................................... 81
Appendix L RIOSORD Provider Satisfaction Survey ............................................................. 82
Appendix M Relationship of the DNP Essentials to the DNP Project ...................................... 83
IMPLEMENTING A RISK INDEX TOOL 4
List of Tables
Table 1 Conversion of Opioid Dose to Morphine Milligram Equivalents ....................... 15
Table 2 Project Application of the Stetler Model of Research Utilization ...................... 25
Table 3 Benefits of DNP Project to Patients and Institution ............................................. 36
Table 4 DNP Project Goals and Objectives ...................................................................... 39
Table 5 Covariates Analyzed in the IMS RIOSORD Tool ............................................... 40
Table 6 Aligning Goals and Objectives with Outcome Measures .................................... 41
Table 7 Conversion of RIOSORD Score to Risk Class and Probability of Overdose or
Serious OIRD ....................................................................................................... 45
Table 8 Steps to Achieve Sustainability Objectives ......................................................... 61
IMPLEMENTING A RISK INDEX TOOL 5
List of Figures
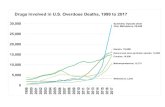
Figure 1 Comparison of prescription opioid sales and death rates ....................................... 9
Figure 2 Prescription opioid overdose deaths from 2001 to 2014 ..................................... 26
Figure 3 Distribution of the economic burden of prescription opioid overdose, abuse,
and dependence .................................................................................................... 28
Figure 4 2016 Patient Population by Age and Sex ............................................................. 29
Figure 5 2016 Patient Population by Insurance .................................................................. 30
Figure 6 The different formulations of naloxone available to prescribe ............................ 48
Figure 7 The predicted probability (risk classes, by percentiles) versus observed incidence
of overdose or serious opioid-induced respiratory depression ............................ 52
IMPLEMENTING A RISK INDEX TOOL 6
Abstract
Background: Chronic pain and the treatment of chronic pain are challenges faced by healthcare
providers across the nation. Patients who take opioids for chronic pain significantly increase
their risk for serious opioid-induced respiratory depression (OIRD) and overdose if they do not
take the medication as prescribed. Due to the rise in opioid overdose deaths, much attention is
focused on improving prescribing practices for opioid pain medication in the treatment of
chronic noncancer pain. A recommended risk mitigation strategy is to co-prescribe naloxone
when prescribing opioids for patients at high risk for overdose. Purpose: The purpose of this
project is to implement a validated risk assessment strategy that may reduce and/or prevent
overdose deaths from prescription opioids. Design: The project will utilize a prospective cohort
study design in which the Risk Index for Overdose or Serious Opioid-Induced Respiratory
Depression (RIOSORD) tool will be used to evaluate appropriate patients risk of overdose or
serious OIRD and examine how the tools use influences the prescribing practice of naloxone as a
rescue medication for patients on chronic opioid therapy. Outcome measures: Primary outcome
measures include the calculated RIOSORD score for each patient assessed, the number of high-
risk patients, and the number of naloxone prescriptions provided. Secondary outcome measures
include an analysis of the individual covariates from the RIOSORD tool. Implications:
Utilizing a validated, risk assessment tool to increase access to naloxone aligns well with the
national call for action to reduce opioid overdoses and promote safe opioid prescribing.
Keywords: chronic opioid therapy, overdose, naloxone, risk assessment
IMPLEMENTING A RISK INDEX TOOL 7
A Quality Improvement Project: Implementing a Risk Index Tool to Guide
Naloxone Prescribing in Patients on Chronic Opioid Therapy
Chronic pain and the treatment of chronic pain are public health challenges faced by
healthcare providers across the nation. Chronic pain is defined as pain that lasts longer than
three months or past the time expected for normal tissue healing; chronic pain may be the result
of an underlying medical condition or disease, injury, inflammation, medical treatment, or an
unknown cause (Dowell, Haegerich, & Chou, 2016). For the purpose of this project, chronic
pain is used to reference chronic noncancer pain (CNCP).
It is estimated that over 100 million people in the United States suffer from chronic pain
and that chronic opioid therapy (COT) may be an appropriate treatment for some of these
chronic pain sufferers (Volkow, 2014). According to Dowell et al. (2016), evidence indicates
that short-term use of opioid pain medication is effective in reducing pain and improving
functional status in persons with noncancer nociceptive and neuropathic pain in randomized
clinical trials lasting ≤12 weeks. However, only a few studies have been conducted to rigorously
assess the long-term benefits of opioids (i.e., at least one year later) in patients with CNCP
(Dowell et al., 2016).
Despite the lack of evidence to support use of long-term opioid therapy in the
management of CNCP, its use has increased substantially in recent years and has been
accompanied by an increase in drug related deaths (Cheung et al., 2014; Volkow, 2014). From
1999 to 2014, more than 165,000 persons died from opioid overdoses in the United States
(Dowell et al., 2016). Manchikanti et al. (2014) estimate that Americans consume 99% of the
world’s supply of hydrocodone and 83% of the world’s supply of oxycodone. Prescription
opioid-related deaths have quadrupled in the United States since 1999 and approximately 80% of
IMPLEMENTING A RISK INDEX TOOL 8
these deaths are due to unintentional overdose (Rudd, Aleshire, Zibbell, & Gladden, 2016;
Zedler, Xie, et al., 2015).
Opioids are highly addictive in certain populations due to the release within the brain of a
naturally occurring neurotransmitter called dopamine. Dopamine creates pleasurable sensations
that are reinforcing for continued behavior (National Institute on Drug Abuse [NIDA], 2014).
This addictive nature of opioids makes them vulnerable to misuse and abuse (Cheung et al.,
2014). Patients who take opioids for chronic pain significantly increase their risk for negative
adverse events if they do not take the medication as prescribed (e.g., taking more than
prescribed, taking them by an alternate route, or taking them in combination with certain other
medications and/or alcohol). Opioids depress the central nervous system, which can result in
serious, life-threatening consequences such as sedation, respiratory depression, and potentially
death. The combined effects from alcohol and other medications significantly increase the risk
for overdose and death (World Health Organization [WHO], 2014).
Problem Statement
Overdose deaths have increased in parallel to prescriptions written for opioid pain
medication (Rudd et al., 2016; Dowell et al., 2016). Figure 1 demonstrates a comparison of
prescription opioid sales and death rates from 1999 to 2013. Dowell et al. (2016) note that
prescriptions written by primary care providers account for nearly half of all opioid sales. It was
also noted that opioid prescribing rates among healthcare providers increased 7.3% per capita
from 2007 to 2012 with rates increased more for family practice, general practice, and internal
medicine (Dowell et al., 2016). Overall, healthcare providers in the United States wrote 259
million prescriptions for opioids in 2012; this equates to one prescription for every adult in
IMPLEMENTING A RISK INDEX TOOL 9
America (Dowell et al., 2016). In 2014, overdose deaths from prescription opioids increased to
approximately 19,000 deaths in the United States; this is more than three times the number
reported in 2001 (Substance Abuse and Mental Health Services Administration [SAMHSA],
2016b). Considering the potentially fatal outcome of overdose, much attention is focused on
improving prescribing practices for opioid pain medication in the treatment of CNCP. Such
statistics are staggering and indicate the need for a call to action to reduce the opioid overdose
epidemic. These findings also demonstrate the importance of utilizing strategies to reduce or
prevent overdose deaths from prescription opioids in addition to recommendations for safe
opioid prescribing for those with chronic pain.
Figure 1. Comparison of prescription opioid sales and death rates. This chart
demonstrates a comparison of prescription opioid sales in relation to death
rates from opioid use during years 1999 through 2013.
Source: *Automation of Reports and Consolidated Orders System of the
Druge Enforcement Administration (2012 data not available); **CDC,
National Vital Statistics System mortality data, 2015.
IMPLEMENTING A RISK INDEX TOOL 10
Both the Centers for Disease Control and Prevention (CDC) and SAMHSA recommend
that clinicians consider a co-prescription for naloxone when prescribing opioids for patients at
high risk of overdose as a risk mitigation strategy. Naloxone is an opioid antagonist that can
reverse respiratory depression and prevent death if administered in a timely fashion to a person
suspected of an opioid overdose. The CDC indicates that naloxone distribution programs are
associated with reduced risk for overdose death at the community level (Dowell et al., 2016).
Additionally, it is noted that friends and family are capable of administering naloxone once they
are properly educated and trained (Dowell et al., 2016; WHO, 2014).
Purpose of the Project
The purpose of this project is to implement a risk assessment strategy that may reduce
and/or prevent overdose deaths from prescription opioids. Specifically, this project will utilize a
validated risk assessment tool that quantifies a patient’s risk of overdose or serious opioid-
induced respiratory depression (OIRD) and examine how its utilization influences the
prescribing practice of naloxone as a rescue medication for patients on COT. The project will
also examine current naloxone prescribing patterns and potential factors influencing a provider’s
decision to co-prescribe naloxone prior to implementing a risk assessment tool. Additionally, the
project will assess provider satisfaction and ease of use. Implementing measures to improve
opioid prescribing practices supports the CDC’s goal for access to safe, effective pain treatment
while reducing risk for overdose (Dowell et al., 2016).
Clinical Question
The recommendation to prescribe naloxone for patients at increased risk of opioid
overdose raises the clinical questions of how to determine which patients are at increased risk
and how to measure risk of unintentional overdose in patients on COT. Neither SAMHSA nor
IMPLEMENTING A RISK INDEX TOOL 11
the CDC makes a recommendation for use of a specific tool. Available risk mitigation strategies
such as provider education, written opioid agreements, urine drug screens, prescription drug
monitoring programs, and screening for aberrant behavior may be beneficial in assessing for
misuse or abuse but they do not assess for or measure risk of overdose or OIRD. The only
published tool that provides an actual quantitative measure of overdose risk from opioid pain
medication is the Risk Index for Overdose or Serious Opioid-Induced Respiratory Depression
(RIOSORD; Zedler, Xie, et al., 2015). Considering the increased use of COT to treat CNCP and
the subsequent rise in opioid-related deaths, the PICOT question addressed in this Doctor of
Nursing Practice (DNP) project is: Among providers who prescribe COT, does use of the
RIOSORD assessment tool, compared to not using a risk-screening tool, increase the prescribing
practice of naloxone over a six-month period?
Review of the Literature
Methods
Relevant literature was reviewed for evidence addressing the use of opioids to treat
chronic pain and available risk mitigation strategies to reduce misuse, abuse, and overdose. The
electronic databases utilized in the search process were PubMed, the Cumulative Index to
Nursing and Allied Health Literature (CINAHL), the Cochrane Library, PsychInfo, and National
Guideline Clearinghouse. Key terms used in the search process were chronic opioid therapy,
overdose, naloxone, and risk assessment; these terms were combined utilizing the Boolean
operator “AND”. The search was limited to English language, peer reviewed journal articles,
and a publication date of 2011-2016. Studies were included if abstracts were available as well as
access to full text, were conducted within the United States, and limited to adults only. One
additional study was included based on the review of an article from the literature search. A total
IMPLEMENTING A RISK INDEX TOOL 12
of 613 records were identified, which was narrowed to 520 records after removing duplicates.
The titles and abstracts of the 520 articles were screened for inclusion. Articles were excluded (n
= 391) if they focused on specific opioid pain medications or illicit drugs; applied directly to
cancer-related pain, palliative care, or end of life; involved in-patient, hospital, or operative
settings; pertained directly to drug screening or testing; pertained to substance use disorder or
addiction; or involved pregnant women or children. A total of 129 full-text articles were further
reviewed for eligibility and 17 articles were included in this DNP project. Appendix A contains
a flow diagram of the search process. Common themes noted in the review of literature include
the use of opioid guidelines, the risk of overdose in relation to morphine-equivalent dose (MED)
and opioid formulation, and the use of risk instruments and other mitigation strategies such as the
SAMHSA toolkit and the RIOSORD tool to assess for aberrant behavior and risk of overdose.
Opioid guidelines. Opioid prescribing guidelines provide recommendations for
clinicians who prescribe opioids for persons with pain. However, multiple guidelines are
available and there is no consensus on which guideline clinicians should follow. In a systematic
review of available guidelines, Nuckols et al. (2014) note that recommendations provided by the
professional organizations American Pain Society and American Academy of Pain Medicine are
of high quality and are applicable to a broad range of adults with pain. Dowell et al. (2016) also
note that state and federal agencies such as the Washington Agency Medical Directors Group
(2015) and the U.S. Department of Veterans Affairs/Department of Defense (2010) provide their
own recommendations for opioid prescribing which are of good quality. Common elements
noted across most of these guidelines are recommendations for dosing thresholds and dosing
titration in addition to risk mitigation strategies such as the use of risk assessment tools,
IMPLEMENTING A RISK INDEX TOOL 13
treatment agreements, urine drug screenings, and the use of state prescription drug monitoring
programs (Dowell et al., 2016).
There is, however, considerable variability in specific recommendations such as the range
of dosing thresholds (MED of 90 to 200mg/day), the intended audience such as primary care
versus pain specialists, and the strength of the evidence upon which recommendations are based
(Cheung et al., 2014; Dowell et al., 2016). There is no clear consensus on a reasonable MED in
the treatment of CNCP but 100 to 120 mg morphine equivalents seems to be a reference level for
heightened caution due to evidence of increased morbidity and mortality at these doses (Cheung
et al., 2014). Recommendations from the CDC opioid guideline are directed at primary care
clinicians treating chronic pain and are based on a systematic review of the best available
evidence along with expert, public, and stakeholder input (Dowell et al., 2016). The literature
review performed by the CDC expanded upon a previously published systematic review
sponsored by the Agency for Healthcare Research and Quality (AHRQ) in 2014 on the efficacy
and risks of long-term opioid therapy for chronic pain. Additional literature searches were
conducted to identify new studies and to update the existing review; there were 39 studies from
the AHRQ review and seven more studies from the updated review. Review of the evidence
sought to address five clinical concerns regarding the use of long-term opioid therapy to treat
chronic pain:
1. effectiveness and comparative effectiveness;
2. harms and adverse events;
3. dosing strategies;
4. risk assessment and risk mitigation strategies; and
5. effect of opioid therapy for acute pain on long-term use (Dowell et al., 2016).
The first four concerns were addressed in the previous 2014 AHRQ-sponsored systematic
review. However, the fifth concern was added for the purpose of developing the 2016 CDC
IMPLEMENTING A RISK INDEX TOOL 14
guideline and the updated systematic review was performed to address it. Thus,
recommendations from the CDC guideline provides guidance on determining when to initiate or
continue opioids for chronic pain; opioid selection, dosage, duration, follow-up, and
discontinuation; and assessing risk and addressing harms of opioid use. Common factors
associated with an increased risk of opioid overdose identified by Dowell et al. (2016) include
the following:
use of extended-release or long-acting (ER/LA) opioid formulations;
MED >100mg/day;
a co-concurring prescription for benzodiazepines;
increased duration of opioid use;
the presence of sleep apnea or other sleep-disordered breathing;
renal and/or hepatic insufficiency;
older age (i.e., >65 years old);
pregnancy;
depression or other mental health conditions; and
alcohol or other substance use disorder(s).
Opioid prescribing guidelines are intended to promote safe opioid prescribing and to
improve patient outcomes. When making clinical decisions, prescribers are encouraged to
consider the patient-provider relationship in addition to the patient’s individual circumstances
including pain relief and benefit from COT; functional status and quality of life; medication side
effects; warning signs for addiction, abuse, or misuse; and any mood changes. These factors are
often referred to as the “five A’s” of analgesia therapy: activity, analgesia, adverse effects, and
aberrant behaviors, and affect (Agency for Clinical Innovation, n.d.).
Morphine-equivalent dose. Calculating the total daily dose of opioids helps to identify
patients who may benefit from closer monitoring, reduction of dose, prescribing of naloxone, or
other measures to reduce risk of overdose (CDC, 2016d). In order to calculate the total daily
dose, the clinician determines the dose of each opioid that the patient takes, converts dose(s) into
morphine milligram equivalents (MME) according to the CDC’s MME conversion factor in
IMPLEMENTING A RISK INDEX TOOL 15
Table 1, and then adds them all together. This conversion is referred to as the morphine
equivalent dose (MED) and is expressed as mg/day.
Higher doses of opioids are associated with an increased risk of overdose and death,
although some risk is associated even with relatively low doses (MED 20-50mg/day; CDC,
2016d). A randomized controlled trial conducted by Chou et al. (2015) found a significant
increase in risk of overdose when comparing MED 20-49mg/day to 200mg/day. The adjusted
odds ratio was 1.32 for MED 20-49mg/day, 95% CI [0.94, 1.84] compared to 2.88 for MED at
least 200mg/day, 95% CI [1.79, 4.63]. Another randomized controlled trial by Dowell et al.
(2015) found an adjusted odds ratio of 2.08 for MED 1-140mg/day, 95% CI [1.55, 2.78]
compared to 6.14 for MED ≥450mg/day, 95% CI [4.92, 7.66]. Nuckols et al. (2014) note that
Table 1
Conversion of Opioid Dose to Morphine Milligram Equivalents
Opioid Conversion Factor
Codeine 0.15
Fentanyl transdermal (in mcg/hr) 2.4
Hydrocodone 1
Hydromorphone 4
Methadone
1-20 mg/day 4
21-40 mg/day 8
41-60 mg/day 10
> 61-80 mg/day 12
Morphine 1
Oxycodone 1.5
Oxymorphone 3
Note. Doses are in mg/day except where noted.
Source: Centers for Disease Control and Prevention. (2016c,
August 25). Injury prevention & control: Opioid overdose,
guideline resources. Retrieved September 5, 2016, from
http://www.cdc.gov/drugoverdose/prescribing/resources.html
IMPLEMENTING A RISK INDEX TOOL 16
risk for serious or fatal overdose increased 1.9 to 3.1 fold with MED 50-100 mg/day and
increased even more dramatically with MED >100 to 200 mg/day. Two studies conducted by
Zedler indicated similar findings: odds ratio 4.96 for MED >100mg/day, 95% CI [3.24, 7.61]
(Zedler, Xie, et al., 2015) and odds ratio 4.1 for MED ≥100 mg/day, 95% CI [2.6, 6.5] (Zedler et
al., 2014). The CDC recommends prescribing the lowest effective dose, to “start low and go
slow”, and to avoid increasing to MED >90mg/day if possible. Morphine equivalent doses of
>50mg/day increase risk of overdose by at least two times the risk associated with <20mg/day
(CDC, 2016d).
Opioid formulations. The use of extended-release or long-acting opioid formulations is
associated with greater risk for overdose (Dowell et al., 2016; Zedler, Xie, et al., 2015). In a
2014 study conducted by Zedler et al., ER/LA opioid formulations were significantly associated
with increased risk of toxicity and overdose. Additionally, Nuckols et al. (2014) suggest that
only experienced clinicians prescribe methadone and that clinicians in general need to be aware
of risks associated with fentanyl patches. The CDC (2016d) notes that the MED conversion
factor for methadone increases at higher doses and absorption of fentanyl is affected by heat and
other factors such as patient weight. Sensitivity analysis by Wakeland, Schmidt, Gilson,
Haddox, and Webster (2011) suggests that the increase in opioid-related deaths may be related to
prescriber perception of reduced risk with use of long-acting opioids. Wakeland et al. (2011)
also suggest that prescriber education on the use of ER/LA opioids may be effective in reducing
opioid deaths, but little empirical evidence exists to support this finding.
Risk assessment tools. Various risk assessment tools are available to assess for aberrant
behavior in patients for whom opioids are prescribed or considered. These include the Opioid
Risk Tool (ORT), Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R),
IMPLEMENTING A RISK INDEX TOOL 17
Brief Pain Inventory (BPI), and the Chronic Opioid Misuse Measure (COMM). A systematic
review by Nuckols et al. (2014) noted that the self-administered SOAPP-R and COMM
performed well in higher-quality observational studies for detecting aberrant behavior.
However, the CDC opioid prescribing guideline notes that there is insufficient evidence that the
use of such tools is beneficial in identifying risks associated with opioid overdose, abuse, or
addiction (Dowell et al., 2016). This recommendation is based on the variability of sensitivity
and specificity scores for each tool: ORT sensitivity 0.58-0.75 and specificity 0.54-0.86 in five
studies; SOAPP-R sensitivity 0.25 and 0.53 and specificity 0.62 and 0.73 in two studies, and BPI
sensitivity 0.73 and 0.83, specificity 0.43 and 0.88 in two studies (Dowell et al., 2016). It is also
important to note that results gained from the use of self-report questionnaire tools are subject to
the validity of the patient’s answers.
The aforementioned risk assessment tools identify patients at risk for aberrant behavior in
relation to opioid therapy but the tools do not measure the patient’s risk for overdose or
respiratory depression. Thus, tools that screen for overdose or serious OIRD are needed. The
retrospective study conducted by Zedler, Xie, et al. in 2015 indicates that patients at increased
risk of overdose or serious OIRD are likely to benefit from a co-prescription for naloxone as do
recommendations provided by SAMHSA (2016b) and the CDC (Dowell et al., 2016). The
RIOSORD tool is the only published tool that actually measures a patient’s risk for possible
overdose or OIRD. This tool is explored in more depth below.
Dowell et al. (2016) note that there is insufficient evidence that patient education, pill
counts, written treatment agreements, urine drug screens, or use of state prescription drug
monitoring programs are beneficial at mitigating risks but that most experts agree that co-
prescribing naloxone should be considered for patients at increased risk for overdose. Although
IMPLEMENTING A RISK INDEX TOOL 18
the effectiveness of treatment agreements, urine drug screenings, and use of state prescription
drug monitoring programs is not demonstrated in research studies to date, their use is
recommended by most opioid prescribing guidelines. Additionally, Nuckols et al. (2014)
indicate that such risk assessment tools are helpful in monitoring patients on COT and may be
beneficial in curbing abuse and misuse of opioids, which in turn reduces the risk of overdose.
The SAMHSA Opioid Overdose Prevention Toolkit and the RIOSORD tool are discussed below.
SAMHSA toolkit. In August 2015, the Virginia Department of Health issued a letter to
all clinicians encouraging adoption of the SAMHSA Opioid Overdose Prevention Toolkit. This
toolkit provides information for prescribers to use as recommendations to mitigate risks when
prescribing opioid pain medications in addition to expanding access to naloxone in Virginia
(Levine, Brown, & Ferguson, 2015). SAMHSA (2016b) stresses that healthcare providers can
reduce the toll of opioid overdose through the care they take in prescribing opioids and
monitoring the patient’s response, as well as by identifying and addressing overdose. SAMHSA
(2016b) identified five strategies for opioid overdose prevention:
encourage providers, persons at high risk, family members, and others to learn how to
prevent and manage opioid overdose;
ensure access to treatment for individuals who are misusing or addicted to opioids or who
have other substance use disorders;
ensure ready access to naloxone;
encourage the public to call 911; and
encourage prescribers to use state Prescription Drug Monitoring Programs.
As previously mentioned, SAMHSA recommend that clinicians consider a co-prescription of
naloxone for patients at high risk of overdose but no specific screening tool with which to
measure overdose risk is provided or recommended.
RIOSORD tool. Zedler, Xie, et al. developed the RIOSORD (i.e., Risk Index for
Overdose or Serious Opioid-Induced Respiratory Depression) tool in 2015 using a retrospective,
IMPLEMENTING A RISK INDEX TOOL 19
case-control analysis of health care data from the Veteran’s Heath Administration (VHA)
inpatient and outpatient databases. Items included in the RIOSORD tool were selected from
variables found to have a statistically significant association with overdose or serious OIRD (see
Appendix B). Zedler, Xie, et al. (2015) found that the following factors are associated with an
increased odds ratio for overdose or OIRD: ER/LA opioid formulations, route of administration,
MED >100mg/day, and receipt of opioid prescriptions from multiple providers. These findings
are consistent with those identified in the CDC guideline as risk factors for overdose. Zedler,
Xie, et al. (2015) also notes that persons possessing the above-mentioned risk factors also
demonstrated greater health care utilization than controls. Variables with the most significant
positive associations were used to develop the RIOSORD tool: MED >100mg/day, history of
opioid dependence, hospitalization during the 6 months before the overdose or serious OIRD
event, liver disease, and the use of ER/LA opioids (Zedler, Xie, et al., 2015).
The RIOSORD tool provides a quantitative risk assessment for opioid overdose that is
evidence-based and is intended to provide clinical decision support. The tool demonstrated good
calibration and discrimination (i.e., predicted probability) between patients with and without
serious OIRD in the VHA population; the average predicted probability was 3% in the lowest
risk class and 94% in the highest (Zedler, Xie, et al., 2015). The personalized risk assessment
provided by the RIOSORD tool is useful in determining if an alternate medication, dose, or
formulation may reduce risk for OIRD; if clinical or behavioral recommendations are indicated;
or if a co-prescription for naloxone is recommended. The VHA sample included only men with
the majority being >55 years old. Hence, the validity of the results is unclear in other
populations such as younger patients, women, or those with commercial insurance. It is also
IMPLEMENTING A RISK INDEX TOOL 20
important to note that studies of the RIOSORD tool focused on the use of prescription opioids
and did not include use of heroin or opioids used for non-medical purposes.
Later in 2015, the original RIOSORD tool (VHA RIOSORD) was modified and further
validated in a retrospective, nested, case-control study of over 18 million patients from the
United States with a pharmacy claim for an opioid between January 1, 2009 and December 31,
2013 (Zedler, Saunders, Joyce, Vick, & Murrelle, 2015). This sample consisted of a much larger
population from the IMS PharMetrics Plus™ database of integrated commercial health plan
claims that is comprised of both medical and pharmacy claims. The objective of this study was
to validate and extend the RIOSORD tool in a larger population that is more representative of
medical users of prescription opioids in the United States (Zedler, Saunders, et al., 2015). The
IMS sample was deemed more representative because it included patients younger than 55 years
of age, females, and patients with commercial insurance in comparison to the VHA sample.
Zedler, Saunders, et al. (2015) found that the predictive performance of the revised RIOSORD
(IMS RIOSORD) in this large commercial insurance database was excellent and similar to the
VHA RIOSORD performance. The strongest predictors of overdose or serious OIRD in the IMS
population consisted of eight coexisting clinical conditions (e.g., neuropsychiatric disorders and
impaired drug metabolism or excretion) and eight characteristics of the prescribed opioid (e.g.,
specific medication characteristics and concomitant benzodiazepines or anti-depressants; Zedler,
Saunders, et al., 2015). Multivariable modeling of these covariates in the IMS population
demonstrated a C-statistic of 0.90, which indicates excellent discrimination between cases and
controls (Zedler, Saunders, et al., 2015).
The RIOSORD tool used in the commercial insurance population consisted of 16
questions with a total score of 146 points versus 17 questions with a total score of 115 points in
IMPLEMENTING A RISK INDEX TOOL 21
the VHA RIOSORD (see Appendix C). Covariates in the previously developed VHA RIOSORD
were modified as necessary to accommodate differences in the available commercial insurance
data population (Zedler, Saunders, et al., 2015). The total score in points corresponds with a risk
class that ranges from 1 to 7 with 1 being the lowest risk and 7 being the highest risk. The
average predictive probability of an event across the seven risk classes ranged from 2% in the
lowest risk class (0-4 points) to 83% in the highest risk class (>42 points; Zedler, Saunders, et
al., 2015). Patients identified as having increased risk for overdose or serious OIRD would
benefit from interventions to mitigate the risk of opioid overdose such as a co-prescription for
naloxone. Zedler, Saunders, et al. (2015) however, did not make a recommendation as to which
risk class she would start to consider a co-prescription for naloxone; instead, this decision is left
to the clinician that is prescribing the opioid. Nonetheless, use of the RIOSORD tool provides an
excellent opportunity to provide patient education regarding their individual risk of serious
OIRD.
Discussion
Misuse and abuse of opioids can lead to serious adverse outcomes such as overdose and
possibly death, which present an increasingly severe public health problem in the United States
(Wakeland et al., 2011). A great deal of the evidence demonstrates the need for increased
provider awareness in addition to increased vigilance with prescribing opioid pain medication to
address this epidemic. Provider education should focus on risk mitigation strategies including
the safe use of ER/LA opioid formulations, use of <100mg/day MED if possible, utilization of
risk assessment tools, adequate monitoring of patients’ opioid usage, recognition of high quality
opioid prescribing guidelines, and a co-prescription for naloxone to prevent opioid overdose
deaths. Several screening tools exist to assess for aberrant prescription drug-related behaviors
IMPLEMENTING A RISK INDEX TOOL 22
but only one tool assesses for the risk of overdose or the likelihood of OIRD. Nonetheless, use
of all available screening tools is encouraged because they can provide opportunity to expand the
patient-provider relationship and encourage open communication.
The aim of this project is to utilize the RIOSORD tool to identify individuals on COT
that are at increased risk of unintentional opioid overdose or serious OIRD and provide them
with a co-prescription of naloxone as a means to encourage safe opioid use and prevent overdose
deaths. The RIOSORD is the first tool intended to provide clinicians with the clinical decision
support to assess the risk of serious OIRD and determine the possible need for naloxone. This
tool provides a current, quantitative, evidence-based risk assessment that is able to determine
baseline risk status and provide on-going risk monitoring at future appointments. Review of the
literature clearly indicates that more rigorous, high quality studies are needed to provide
evidence-based practice recommendations in the care of patients on long-term opioid therapy.
Background and Significance
Historically, clinicians have used opioid pain medications to treat acute conditions such
as post-operative pain and pain related to trauma in addition to pain associated with cancer
and/or life-limiting illness (i.e., palliative care; Juurlink & Dhalla, 2012). However, in recent
decades, the United States has seen a dramatic increase in opioid prescribing for many chronic
pain conditions (Alford, 2016). Chronic pain is a significant problem for millions of Americans
and many may have disabling symptoms that interfere with day-to-day functions at home or in
the workplace (Juurlink & Dhalla, 2012). Recommended treatment for chronic pain incorporates
a multimodal approach with pain medication being only one part of the treatment plan.
However, access to recommended multidisciplinary services is sometimes limited by factors
such as cost, lack of insurance, non-coverage of services, lack of transportation, lack of services
IMPLEMENTING A RISK INDEX TOOL 23
in rural areas, and co-morbid health conditions that may limit treatment options such as surgery
(Juurlink & Dhalla, 2012). Due to such limitations, clinicians may initiate opioid pain
medication early in the management of chronic pain.
The use of long-term opioids to treat CNCP became common in the 1990s. The rise in
opioid use during this time coincided with the introduction of several new opioid formulations
such as OxyContin®, an extended-release oxycodone (without abuse deterrent properties) that
was introduced in 1995 within the United States (Juurlink & Dhalla, 2012). The American
Academy of Pain Management (AAPM) and the American Pain Society (APS) also endorsed
chronic opioid therapy during this time. Both the AAPM and the APS encouraged liberal use of
opioids to treat chronic pain based on research that indicated the development of addiction was
low when opioids were used for the relief of pain (Juurlink & Dhalla, 2012). In 2000, the Joint
Commission introduced new pain management standards, which emphasized that patients have
the right to pain relief (Manchikanti et al., 2012). The Joint Commission recommended regular
evaluation of pain in hospitalized patients as the “fifth vital sign” although pain is subjective and
not an objective measurement such as heart rate or temperature (Juurlink & Dhalla, 2012).
Support from national organizations along with the use of opioids in high doses and aggressive
pharmaceutical marketing has contributed to the prevalence of the opioid overdose epidemic.
Unfortunately, growth in the use of opioid pain medication to treat chronic pain has been
associated with increased misuse of prescription opioids and an increase in deaths due to
unintentional overdose (Alford, 2016).
Evidence indicates that patients on COT who are at risk of overdose are likely to benefit
from co-prescribing of naloxone. A study funded by the National Institutes of Health
demonstrated that naloxone can be successfully prescribed to a substantial proportion of patients
IMPLEMENTING A RISK INDEX TOOL 24
receiving COT and that naloxone co-prescribing was associated with reduced opioid-related
emergency room visits (Coffin et al., 2016). The RIOSORD provides clinicians with a validated
risk assessment tool with the ability to identify which patients may benefit from receiving a co-
prescription for naloxone. Fudin (2015) indicates that clinicians and even pharmacists can utilize
the RIOSORD tool to screen patients for risk of unintentional overdose or OIRD. Discussion of
the patient’s RIOSORD score provides an opportunity for a conversation about the possibility of
unintentional overdose and the benefits of risk-reduction strategies such as the co-prescribing
and use of naloxone. It is felt that use of the RIOSORD tool is a practical approach to screen for
risk of overdose in clinical practice and provide guidance on naloxone prescribing (Zedler, Xie,
et al., 2015; Fudin, 2015).
Conceptual Framework
The Stetler model of research utilization is the selected conceptual framework for this
project as it provides the structure and guidance needed to evaluate the literature, synthesize the
evidence, and initiate translation of information into practice. The Stetler model is an evidence-
based practice model that helps practitioners to incorporate evidence into daily practice and to
create formal change within an organization (National Collaborating Centre for Methods and
Tools, 2011). The model consists of five phases that serve as steps in identifying and utilizing
tasks to facilitate safe and effective evidence-based practice (Dang et al., 2015). Table 2 outlines
the phases involved in the Stetler model of research utilization and the specific tasks involved in
the application of each phase to this project.
The primary goal of this project is to utilize the RIOSORD score to guide naloxone
prescribing, which may reduce or prevent opioid-related deaths. The Stetler model of research
utilization is appropriate for this project because it is a practitioner-oriented model that utilizes
IMPLEMENTING A RISK INDEX TOOL 25
the critical thinking process to develop evidence-based practice changes. Implementation of the
RIOSORD tool to quantify a patient’s risk of overdose and increase access to naloxone
demonstrates effective use of evidence-based practice change by the clinician.
Needs Assessment
Drug overdose deaths in the United States hit record numbers in 2014 and at least half of
all opioid overdose deaths involved a prescription opioid (CDC, 2016c). Figure 2 demonstrates
the total number of U.S. overdose deaths involving opioid pain relievers from 2001 to 2014. The
total number of deaths increased by 3.4 times during that period (NIDA, 2015). Based on the
NIDA statistics, 78 Americans die every day from an opioid overdose and nearly half of a
million people died from opioid overdose from 2000 to 2014 (CDC, 2016c). The CDC (2016c)
acknowledges that overdoses from prescription opioid pain relievers are a driving factor in the
15-year increase in opioid overdose deaths. The most common opioids involved in overdose
Table 2
Project Application of the Stetler Model of Research Utilization
Phase Task
1. Preparation Identify problem, background and significance,
needs assessment, and outcome measures
2. Validation Review literature, synthesize evidence, and
assess tool validity
3. Comparative
Evaluation/Decision Making
Discuss findings, applicability and feasibility,
and additional information needed
4. Translation/Application Utilize evidence and implement change
5. Evaluation Measure outcomes, evaluate change
effectiveness, and disseminate findings
IMPLEMENTING A RISK INDEX TOOL 26
deaths are methadone, oxycodone, and hydrocodone (CDC, 2016b). Deaths from opioid
overdoses between 1999 and 2014 were highest among people aged 25 to 54 years of age; non-
Hispanic whites and American Indian or Alaskan Natives, compared to non-Hispanic blacks and
Hispanics; and men, but the mortality gap between men and women is closing (CDC, 2016b).
There were approximately 1.5 times more drug overdose deaths in the United States than deaths
from motor vehicle crashes in 2014 (CDC, 2016b).
The CDC analyzed data from the National Vital Statistics System multiple cause-of-death
mortality files for years 2013 and 2014 in order to track trends and shifting characteristics of
drug overdose deaths (Rudd et al., 2016). Results from this analysis noted significant increases
in drug overdose death rates in the Northeast, Midwest, and South census regions; the five states
with the highest rates of death were West Virginia, New Mexico, New Hampshire, Kentucky and
Ohio in 2014 (Rudd et al., 2016). Statistically significant increases in overdose death rate due to
Figure 2. Prescription opioid overdose deaths from 2001 to 2014. This chart illustrates
the number of overdose deaths from prescription opioids; the chart is overlayed with a
line graph to show number of deaths by females and males.
Source: CDC Wonder; National Institute on Drug Abuse; National Institutes of Health;
U.S. Department of Health and Human Services.
02,0004,0006,0008,000
10,00012,00014,00016,00018,00020,000
Total Female Male
IMPLEMENTING A RISK INDEX TOOL 27
drug overdose were also noted in Alabama, Georgia, Illinois, Indiana, Maine, Maryland,
Massachusetts, Michigan, New Hampshire, New Mexico, North Dakota, Ohio, Pennsylvania,
and Virginia (Rudd et al., 2016). Specifically, there was a 14.7% increase in overdose death rate
within the state of Virginia (Rudd et al., 2016). In Virginia, there was a total of 980 deaths with
an age adjusted rate of 11.7% in 2014 compared to 854 deaths with an age adjusted rate of 10.2%
in 2013 (Rudd et al., 2016). In 2013, Virginia’s Medicaid program spent $28 million on
members admitted to emergency departments and hospitals for treatment of substance use
disorder with $10 million of this spending occurring in Southwest Virginia (VCU School of
Medicine, 2016). Opioid prescriptions alone cost Medicaid $26 million annually (VCU School
of Medicine, 2016).
The total economic burden for opioid-related overdose, abuse, and dependence in the
United States is estimated to be $78.5 billion (Florence, Zhou, Luo, & Xu, 2016). Figure 3
provides an overview of the distribution of the economic burden of prescription opioid overdose,
abuse, and dependence. Over one-third of this amount ($28.9 billion) is due to increased health
care and substance abuse treatment costs and approximately one-quarter of the cost is borne by
the public sector in health care, substance abuse treatment, and criminal justice costs (Florence et
al., 2016). Fatal cases account for just over one quarter of the costs ($21.5 billion; Florence et
al., 2016).
Although many people benefit from prescription opioid pain medication to manage pain,
prescription opioids are often diverted for improper use (SAMHSA, 2016a). According to the
2013 and 2014 National Survey on Drug Use and Health, 50.5% of people who misused
prescription painkillers got them for free from a friend or relative compared to 22.1% who got
them from a prescriber (SAMHSA, 2016a). The CDC notes that individuals at highest risk of
IMPLEMENTING A RISK INDEX TOOL 28
overdose are about four times more likely than the average user to buy the drugs from a dealer or
other stranger (CDC, 2016a). Implementing safer opioid prescribing practices and utilizing the
CDC guideline may help to reduce the amount of prescription opioids available for nonmedical
use.
The clinical setting for the DNP project is Virginia Commonwealth University
Community Memorial Hospital (VCU-CMH) Pain Management Services, which is a pain
management office in a rural setting with one physician and one nurse practitioner. The practice
is a hospital-owned entity with affiliation to a larger health system that is located over 60 miles
away and it is the only pain management practice within the immediate area. Between the two
Figure 3. Distribution of the opioid economic burden. This pie chart depicts the distribution
of the economic burden from prescription opioid overdose, abuse, and dependence.
Source: Florence, C. S.; Zhou, C.; Luo, F.; Xu, L. (2013). The economic burden of
prescription opioid overdose, abuse, and dependence in the United States. Medical Care,
54(10), pp. 901-906, doi: 10.1097/MLR.0000000000000625
Copyright © 2016 Medical Care. Published by Lippincott Williams & Wilkins.
IMPLEMENTING A RISK INDEX TOOL 29
providers, a mean of 264 established patients and 31 new patients are seen per month. The
physician sees all new patients for the first visit encounter. The patient population at VCU-CMH
Pain Management Services is 68% white, 38% African American, and 1% other race; 60% of the
patients are between 40 and 64 years of age and 60% are female. Forty-eight percent of the
population has Medicare insurance. This information is depicted in Figures 4 and 5.
Patients are seen at least every three months for routine follow-up, assessment, and
medication refills. The majority of patients are prescribed an opioid pain medication. According
to the CDC (2016a), an estimated 1 out of 5 patients with noncancer pain are prescribed opioids
in an office-based setting. Virginia is cited as prescribing opioid pain medications to 72-82.1 out
Figure 4. VCU-CMH Pain Management Services patient population. This chart
demonstrates the patient population by age and sex per month for 2016.
Jan Feb Mar Apr May Jun Jul Aug Sept
18-39 yr 42 41 47 40 43 41 32 45 38
40-64 yr 194 210 205 223 223 251 197 220 208
>64 yr 94 107 92 103 117 112 94 117 102
Female 105 213 238 241 255 294 110 236 239
Male 226 146 109 124 128 110 213 142 109
0
50
100
150
200
250
300
350
Nu
mb
er
of
Pat
ien
ts
Patients per Month
2016 Patient Population by Age and Sex
18-39 yr 40-64 yr >64 yr Female Male
IMPLEMENTING A RISK INDEX TOOL 30
of 100 persons (CDC, 2016a). Nationally, the lowest concentration is 52-71 per 100 persons and
the highest 96-143 per 100 persons (CDC, 2016a). All of Virginia’s surrounding states are
among those with the highest prescribing rates including North Carolina, which is less than 20
miles away from VCU-CMH Pain Management Services.
National statistics indicate that most opioid overdose deaths occur in persons aged 25-54
years of age, non-Hispanic whites, and men. The majority of patients seen at VCU-CMH Pain
Management Services fit into at least two of these categories, although VCU-CMH sees fewer
patients 18-39 years of age than any other age group. Even though men are most likely to die of
an opioid overdose, women are more likely to use prescription opioids, which is demonstrated in
the clinic’s demographics noted above (CDC, 2016a). Data from the CDC (2016a) also indicates
that the economic burden of prescription opioid overdose (in addition to abuse and dependence)
Figure 5. VCU-CMH Pain Management Services patient population. This
pie chart demonstrates patient population by insurance for 2016.
48%
27%
17%
4%2% 2%
2016 Patient Population by Insurance
Medicare
Private
Medicaid
Worker's Compensation
Uninsured
CHAMPUS/VA
IMPLEMENTING A RISK INDEX TOOL 31
falls mostly onto the private sector (18%) and Medicaid populations (7%). Forty-four percent of
the patients at VCU-CMH Pain Management Services are insured by private (27%) and
Medicaid (17%) insurances.
Demographic similarities between VCU-CMH Pain Management Services patient
population and national/state statistics of persons affected by opioid-related overdoses and
clinician prescribing practices clearly indicate the need for risk mitigation strategies to reduce
opioid-related morbidity and mortality. Safer opioid prescribing includes taking measures to
protect patients with chronic pain who are medically dependent on opioid pain medication to
improve their functional status and quality of life. Such efforts include use of recommendations
from the CDC guideline for prescribing opioids for chronic pain, patient and provider education
on the correct use of opioid pain medication for chronic pain, and expanding access to and the
use of naloxone. Evaluating patients for risk of overdose will help to determine which patients
would most benefit from the availability of in-home naloxone.
Key Stakeholders
The increasing prevalence of opioid overdose, misuse, and abuse signifies the need for
change among medical societies and policymakers to help improve this public health burden.
Initiatives to reduce the opioid overdose epidemic can strengthen relationships among
stakeholders such as policymakers, clinicians, pharmacists, pharmaceutical companies, law
enforcement, first responders, health insurers, healthcare systems, communities, and families.
The Virginia General Assembly passed legislation in 2015 to expand access to naloxone so that
family members and other individuals can possess and use naloxone to reverse an opioid
overdose at home or in the community if needed (Levine et al., 2015). Additionally, the Virginia
Board of Pharmacy approved a protocol for the prescribing and dispensing of naloxone and the
IMPLEMENTING A RISK INDEX TOOL 32
Virginia Department of Behavioral Health & Developmental Services (DBHDS) Office of
Substance Abuse Services established REVIVE! as the Opioid Overdose and Naloxone
Education (ONE) program for the Commonwealth of Virginia. The REVIVE! ONE program
provides education on how to recognize and respond to an opioid overdose including
administration of naloxone. This training program is available to professionals, stakeholders,
and others with an interest in the opioid overdose epidemic.
In August 2016, Dr. Vivek H. Murthy, the U.S. Surgeon General, initiated the
TurnTheTide campaign to raise awareness of the opioid overdose epidemic. Clinicians were
asked “to pledge their commitment to turn the tide on the opioid crisis” (Murthy, 2016, para. 5).
This pledge recommended that clinicians become educated in the treatment of pain, screen
patients for opioid use disorder and provide referral to evidence-based treatment if needed, and
to treat addiction as a chronic illness and not a moral failing (Murthy, 2016). Lastly, the CDC
developed a funded program called Prevention for States that provides specific state health
departments with resources to advance interventions for preventing prescription drug overdoses
(CDC, 2016e). Such resources include maximizing prescription drug monitoring programs,
community or insurer/health system interventions, state policy evaluations, and rapid response
projects. Clinicians and other healthcare professionals are encouraged to engage with local
agencies, law enforcement, community advocates, community service boards, and other
community partners to create local solutions to address opioid overdose and treatment at the
local and regional levels (Levine et al., 2015).
In accordance with national calls to improve opioid prescribing practices and reduce the
risk of opioid-related deaths, the intended audiences for this project are patients on COT and
prescribers of opioids. The key stakeholders involved are the patients in addition to their
IMPLEMENTING A RISK INDEX TOOL 33
families and communities, the prescribers and clinical staff, and management of the clinical
setting, which includes the office manager, the vice-president of physician services, and the chief
executive officers from both the local hospital (CMH) and its affiliate partnership (VCU Health
System). Decisions within the office are made through collaboration between the two providers,
office manager, and the vice-president of physician services with approval from the local
hospital’s chief executive officer as needed.
Barriers and Facilitators
A major potential barrier to the project includes limited time during appointments to
screen for risk of overdose or OIRD. This barrier may affect whether the screening is performed,
as well as the ability to provide adequate patient education on risk of overdose and use of
naloxone to prevent overdose deaths. Lack of prescription drug coverage and the high cost of
certain naloxone delivery systems may limit patient access to naloxone. Some insurances require
a prior authorization for certain naloxone delivery systems, which is time consuming for both the
office staff and clinicians. A majority of insurances provides coverage for generic naloxone
administered intranasally via a syringe and atomizer, but this delivery method is cumbersome
and more difficult to administer than commercially available pre-prepared, ready-to-use delivery
systems (e.g., the Evzio® Auto-Injector and Narcan® Nasal Spray). Possible strategies to
overcome these barriers include utilizing patient assistance programs from the pharmaceutical
company or developing a pre-authorization letter template that is tailored to the patient’s needs.
These strategies may hasten the prior authorization process and thus reduce patient wait time for
this life-saving medication.
The office staff and clinicians at VCU-CMH Pain Management are dedicated to quality
care and patient safety in the treatment of chronic pain conditions. The staff demonstrates
IMPLEMENTING A RISK INDEX TOOL 34
effective teamwork and is knowledgeable of the patient population and their needs, which are
important attributes when incorporating change within an established system. Other strengths
that will facilitate project implementation include use of written opioid agreements with all
patients on COT, use of an electronic medical record (EMR) with the ability to track prescribing
practices, and use of referral guidelines to ensure the appropriateness of patients referred to the
office for chronic pain treatment.
Benchmarks
In March of 2015, Health and Human Services Secretary Burwell introduced the Opioid
Initiative to address opioid-related morbidity and mortality in the United States (U.S. Department
of Health and Human Services [HHS], n.d.). The initiative targets the following three focus
areas: 1) reforming prescribing practices to reduce excess opioid prescribing; 2) improving
naloxone development, distribution, and access; and 3) expanding access to medication-assisted
treatment (HHS, n.d.). Selected metrics to measure progress toward the agency priority goal of
reducing opioid-related morbidity and mortality include:
a decrease in the total morphine milligram equivalents dispensed in the U.S. outpatient
retail pharmacy setting by 10%;
an increase in the number of prescriptions dispensed for naloxone in the U.S. outpatient
retail pharmacy setting by 15%; and
an increase in the number of unique patients receiving prescriptions for buprenorphine
and naltrexone in the U.S. outpatient retail pharmacy setting by 10% (HHS, n.d.).
No other quality measures or benchmarks exist on opioid overdose deaths in patients on
COT or the practice of co-prescribing naloxone among clinicians. The Drug Policy Alliance
(2016) notes that the nation needs new metrics in which to measure the success of our nation's
drug policies and that the primary measure of effectiveness should be a reduction in opioid-
related harm such as overdose deaths versus measuring for slight fluctuations in drug use. A
scientific analysis performed by NIDA found a 1,170% increase in prescriptions of naloxone
IMPLEMENTING A RISK INDEX TOOL 35
dispensed from retail pharmacies in the U.S. between the fourth quarter of 2013 and the second
quarter of 2015 (NIDA, 2016). Many organizations such as SAMHSA, CDC, NIDA, World
Health Organization, and U.S. Department of Health and Human Services recommend expanding
of the use of naloxone as an effective strategy to reduce opioid-related deaths. An appropriate
goal to gauge the success of this DNP project would be a 15% increase in the number of
prescriptions written for naloxone by clinicians at VCU-CMH Pain Management as noted in the
aforementioned agency priority goal. Although another important measure would be a reduction
in the total morphine milligram equivalents prescribed, that metric is not within the scope of this
project.
Budget
In terms of economic analysis, the cost-consequence analysis method pertains to this
project because it allows for comparison between costs and health-related outcomes so that
stakeholders can form their own opinions regarding the best treatment option. The outcome is to
prevent opioid-related deaths by utilizing the RIOSORD score to guide naloxone prescribing;
ultimately, the pertinent health outcomes of consideration are that of life or death for patients’
receiving COT. Use of naloxone in an opioid-related emergency is a life-saving measure that is
effective in preventing death or other possible detrimental effects. However, lack of naloxone
availability contributes to negative outcomes that lead to consequential expenses such as
hospitalization or funeral expenses. These consequential expenses result in increased costs to
third party payers such as insurance companies or the family. Except for the cost of a medication
that goes unused, there are no negative consequences associated with prescribing naloxone to a
high-risk patient who never has an opioid-related emergency. However, one must consider cost
to the patient or insurance company for obtaining the medication in comparison to costs of a
IMPLEMENTING A RISK INDEX TOOL 36
negative outcome. Table 3 provides a summary of benefits of this DNP project to both the
patient and the institution.
A cost analysis was performed to evaluate the potential cost and sustainment of outcomes
of this DNP project. The major expense associated with the project is for materials and supplies,
which will be used to make copies of the RIOSORD questionnaire and patient education
handouts on signs of overdose and naloxone administration. An electronic version of the
RIOSORD tool, referred to as Naloxotel, will be utilized to screen patients for risk of overdose.
Use of Naloxotel will be provided free of charge by Dr. Jeffrey Fudin from Remitigate, LLC.
However, copies of the completed questionnaires will be required to facilitate data collection and
entry, and a copy will be provided to the patient if desired. Educational videos on naloxone
administration are available at no cost via the PrescribetoPrevent.org and www.narcan.com
websites. Total direct costs of the project are $155.97. The indirect costs are expenses that are
already associated with the established practice setting and thus will not add to costs of project
Table 3
Benefits of DNP Project to Patients and Institution
Benefits to Patient Benefits to Institution
Provision of a life-saving medication if
needed
Adherence to opioid prescribing
recommendations
Opportunity to receive education on
contributing factors for increased risk of
overdose or serious OIRD
Implementation of a decision support tool to
quantify risk for overdose or serious OIRD
Increased access to naloxone Utilization of forward thinking risk
mitigation strategies
Quality care with improved outcomes and
increased safety for those on COT
Patient safety, improved outcomes, and
quality care for patients requiring COT
Notes. COT = chronic opioid therapy; OIRD = opioid-induced respiratory depression.
IMPLEMENTING A RISK INDEX TOOL 37
implementation. These costs include that for the two providers that will screen patients for
overdose as well as additional office staff (i.e., two nurses and one clerical worker), facilities,
and the EMR with electronic prescribing capability. Total indirect costs are $61,938.00 for a six-
month period. Provider and nurse salary is based on a total of 120 hours per staff member for the
six months; this allows for ten minutes per patient (five minutes for the clerical worker) with a
projected total of 1,440 patients screened (i.e., 720 patients per provider/nurse). A detailed
budget for the DNP project is presented in Appendix D. The minimal direct costs associated
with this DNP project should not hinder future sustainment of its efforts. Once patients receive
their initial overdose or serious OIRD screening, it can be repeated annually or as needed to
update the individual’s risk index and reinforce overdose education and prevention efforts.
Annual use will also provide an opportunity to renew the naloxone prescription if out of date.
Project Description
This DNP quality improvement project examines the associations between COT, the
opioid overdose epidemic, and the possibility of serious OIRD in patients receiving COT.
Inappropriate opioid pain medication use in addition to prescribing high doses of opioids (i.e.,
>100mg MED) are contributory to the increased morbidity and mortality in patients on COT
secondary to the possibility of serious OIRD. This project strives to promote quality care to
those suffering with CNCP while encouraging safe opioid prescribing and safe opioid use. The
DNP project team consists of the DNP student who will lead as the project investigator; a clinical
advisor assigned by the school of nursing, and two content experts who were selected by the
DNP student. The first content expert is an anesthesiologist who is board certified in pain
management and the second content expert is a doctor of pharmacy at a local retail pharmacy.
The Stetler model of research utilization is the selected conceptual framework to provide
IMPLEMENTING A RISK INDEX TOOL 38
structure and guidance for the translation of evidence-based research into practice change for this
DNP project. Appendix E provides a schematic of the Stetler model. In addition to aligning
well with national calls for safer opioid prescribing, this DNP project enhances the current state
of practice at VCU-CMH Pain Management Services through increased awareness for overdose
risk screening and the existence of a validated risk assessment tool.
Mission Statement
The mission of this project is to provide effective pain management treatment to those
with various chronic pain conditions in compliance with current pain management guidelines
while concentrating on patient safety and quality outcomes through the provision of naloxone to
those determined to be at an increased risk of serious OIRD. The project mission is reflective of
the organizational mission, which is to provide excellence in the delivery of healthcare (VCU
Health CMH, 2016). Organizational quality improvement strategic plans that correlate to the
DNP project include a focus on quality and excellence, creating patient-focused systems, and
meeting growth demands of the outpatient population. Such strategic plans help to unify future
directions and purposes of VCU-CMH with its medical staff while considering the community’s
needs and prioritization of areas for improvement. The organization’s vision is to be a national
leader in healthcare through continuous improvement while recognizing the following values:
integrity at all levels; compassion and service towards others; teamwork that revolves around
respectful and collegial relationships among physicians, employees, patients, and volunteers;
ethical behavior; excellence in our processes and outcomes; and professionalism (VCU Health
CMH, 2016).
Goals and Objectives
IMPLEMENTING A RISK INDEX TOOL 39
The DNP student, as the project investigator, defines the scope of this project in two
primary goals directed at the project intervention/clinicians (goal #1) and the patient population
(goal #2). Table 4 summarizes the primary goals and corresponding objectives.
Outcome Measures
Primary outcome measures include the calculated RIOSORD score for each patient
assessed, the number of high-risk patients, and the number of naloxone prescriptions provided.
Secondary outcome measures include an analysis of the individual covariates from the IMS
Table 4
DNP Project Goals and Objectives
Goal #1 Goal #2
Reduce or prevent opioid-related overdoses
over the six-month project period.
Demonstrate safe opioid use as evidenced
by lack of a serious OIRD event or proper
treatment of a serious OIRD event over
the six-month project period.
Objectives: Objectives:
1. Familiarize clinicians with factors
associated with increased risk of overdose
and/or serious OIRD in patients on COT.
2. Provide information on development of
the RIOSORD tool including differences
in the VHA and IMS populations.
3. Implement use of the IMS RIOSORD tool
in clinical practice to assess risk of
overdose or serious OIRD.
4. Utilize the RIOSORD risk index score to
guide naloxone co-prescribing in patients
on COT found to be at increased risk of
overdose or serious OIRD.
1. Educate patients on factors associated
with increased risk of overdose or
serious OIRD.
2. Provide patient’s with individualized
risk of overdose or serious OIRD
based on RIOSORD score.
3. Provide a co-prescription of naloxone
to use in an opioid-related emergency
if needed.
4. Educate patient and family/friends on
the signs and treatment of opioid
overdose including the proper use of
naloxone.
Note. COT = chronic opioid therapy; IMS = commercial insurance; OIRD = opioid-induced
respiratory depression; RIOSORD = Risk Index for Overdose or Serious Opioid-Induced
Respiratory Depression; VHA = Veteran’s Health Administration.
IMPLEMENTING A RISK INDEX TOOL 40
RIOSORD tool itself (e.g., certain co-morbid health conditions over the past six months and
current medication consumption). Table 5 provides an outline of these covariates.
Table 6 provides a description of how the project goals and objectives link to the primary
and secondary outcome measures. Other secondary long-term outcomes of interest include
whether an overdose or serious OIRD event occurred; if so, did the patient have naloxone
available to use, was naloxone used, and results of the serious OIRD event. However, data for
such long-term outcomes will not be collected as a longitudinal study for longer than six months
would be necessary to obtain this data.
Table 5
Covariates Analyzed in the IMS RIOSORD Tool
Co-morbid Health Conditions Current Medication Consumption
Substance use disorder
Bipolar disorder or schizophrenia
Stroke or other cerebrovascular disease
Chronic kidney disease (with clinically
significant renal impairment)
Heart failure
Non-malignant pancreatic disease
Chronic pulmonary disease
Chronic headache
Fentanyl (transdermal or transmucosal)
Morphine
Methadone
Hydromorphone
ER/LA opioid formulation (including
any of the above named opioids)
Concomitant benzodiazepine use
Concomitant anti-depressant use
Current opioid dose >100mg MED
(includes all prescription opioids
consumed on a daily basis)
Note. ER/LA = extended-release/long-acting; IMS = commercial insurance; MED =
morphine equivalent dose.
Adapted from: Zedler, B., Saunders, W., Joyce, A., Vick, C., & Murrelle, L. (2015).
Validation of a screening risk index for overdose or serious prescription opioid-induced
respiratory depression. Poster session presented at the 2015 American Academy of Pain
Medicine Annual Meeting, National Harbor, MD.
IMPLEMENTING A RISK INDEX TOOL 41
Table 6
Aligning Goals and Objectives with Outcome Measures
Goals/Objectives Outcome Measures
Goal #1: Reduce or prevent opioid-related
overdoses over the six-month project period.
Objectives: Primary Outcomes:
1. Familiarize clinicians with factors associated
with increased risk of overdose and/or serious
OIRD in patients on COT.
2. Provide information on development of the
RIOSORD tool including differences in the
VHA and IMS populations.
(Review of the DNP project proposal
will meet objectives 1-2.)
3. Implement use of the IMS RIOSORD tool in
clinical practice to assess risk of overdose or
serious OIRD.
1. Calculated RIOSORD score for
each patient assessed.
2. Number of patients determined to
be “increased risk” for overdose or
serious OIRD.
4. Utilize the RIOSORD risk index score to guide
naloxone co-prescribing in patients on COT
found to be at increased risk of overdose or
serious OIRD.
3. Number of prescriptions written
for naloxone.
Goal #2: Demonstrate safe opioid use as
evidenced by lack of a serious OIRD event or
proper treatment of a serious OIRD event over the
six-month project period.
Objectives: Secondary Outcomes:
1. Educate patients on factors associated with
increased risk of overdose or serious OIRD.
2. Provide patient’s with individualized risk of
overdose or serious OIRD based on RIOSORD
score.
3. Provide a co-prescription of naloxone to use in
an opioid-related emergency if needed.
4. Educate patient and family/friends on the signs
and treatment of opioid overdose including the
proper use of naloxone.
1. Assess for presence of covariates
included in the RIOSORD tool.
(Administering and reviewing
RIOSORD results with the patient
will also satisfy objectives 1-4.)
Note. COT = chronic opioid therapy; DNP = Doctor of Nursing Practice; IMS = commercial
insurance; OIRD = opioid-induced respiratory depression; RIOSORD =Risk Index for
Overdose or serious opioid-induced respiratory depression; VHA = Veteran’s Health
Administration.
IMPLEMENTING A RISK INDEX TOOL 42
Project Design
The DNP project will utilize a prospective cohort study design in which the RIOSORD
tool will be used to evaluate risk of overdose or serious OIRD and examine how the tools use
influences the prescribing practice of naloxone as a rescue medication for patients on COT.
Additionally, a retrospective chart review will be performed to determine naloxone prescribing
patterns and factors influencing a provider’s decision to co-prescribe naloxone prior to
implementing a risk assessment tool such as the RIOSORD.
Methods
Subjects. Inclusion criteria for the study include clinicians who prescribe opioid pain
medication for 90 days or longer in patients with chronic pain (i.e., pain lasting three months or
beyond the expected duration of healing; Dowell et al., 2016). Data will be collected on both the
prescribers and the patients. Only established patients with a chronic pain condition who are
prescribed continuous opioid pain medication(s) for 90 days or longer will be screened for
overdose or serious OIRD risk screening process. New patients will not be screened at their
initial visit due to time constraints of the office visit and other information that must be reviewed
at the initial visit; however, these patients may be screened at subsequent visits. Exclusion
criteria includes patients who have not been prescribed continuous opioid pain medication(s) for
at least 90 days or who have not had a chronic pain condition for at least three months, anyone
less than 18 years of age, and patients scheduled for an initial encounter (e.g., new patient
appointment).
Setting. The site chosen for the DNP project is a chronic pain management office
located in rural Southside Virginia that serves a wide range of patients over the age of 18 years
with various chronic pain conditions. Although the office is located in Mecklenburg County,
IMPLEMENTING A RISK INDEX TOOL 43
most patients travel from the surrounding seven counties (i.e., Halifax, Charlotte, Lunenburg,
Brunswick, Greensville, Nottoway, and Prince Edward) for pain management treatment. The
next closest pain management office is located 42 miles away in Roanoke Rapids, North
Carolina.
Southside Virginia shares a long border with North Carolina that equals 9,082 square
miles (University of Virginia [UVA], 2011). Southside Virginia occupies more than one-fifth of
the state’s land mass, but contains only 6% of its total population (UVA, 2011). According to
the 2010 census, the total population for Southside Virginia was 504,660 persons with a 1.4%
growth rate and a population density of 56 persons per square mile (UVA, 2011). In regards to
race and ethnicity, 64% of the population is white, 32% is black, 2% Hispanic, and 2% other
including Asian (UVA, 2011). Labor force statistics show that 31% of adults 25-64 years old
were either not working or looking for work in 2011 which is higher than state (20%) and
national (22%) levels of out-of-labor force adults (UVA, 2011). Unemployment was 10.8% in
2009, higher than Virginia’s unemployment rate (7.5%) and the national rate (9.7%; UVA,
2011). Regarding household income, more than 36% earn less than $25,000 per year, 17% fall
below the poverty line (compared to 10% statewide), and 13% receive food stamps (UVA,
2011). Overall, 32% of Southside households do not have adequate income to meet their regular
expenditures (e.g., housing, food, and transportation) without help from government programs,
family and friends, or local organizations (UVA, 2011).
The pain management office has one physician and one nurse practitioner who serve
patients within a 150-mile radius. The physician is an anesthesiologist with board certification in
pain management for 11 years and a total of 28 years in practice; the nurse practitioner is board
certified in Family Practice with three years of pain management experience and approximately
IMPLEMENTING A RISK INDEX TOOL 44
10 years of primary care experience. Other office resources include two licensed practical nurses
with a combined total of 40 years of nursing experience, one clerical worker with twenty years of
medical office experience, and an office manager with 29 years of medical office management
experience.
Tools. The RIOSORD tool designed for use in the commercial insurance or general
population (IMS RIOSORD) will be the tool implemented in the project to screen for risk of
serious OIRD in patients that meet the above-stated inclusion criteria. The IMS RIOSORD tool
is a 16-item questionnaire that is designed to be completed by the clinician. The first eight
questions inquire if the patient being screened has had either an inpatient, outpatient, or
emergency department visit over the last six months for certain medical conditions including
substance use disorder, bipolar/schizophrenia, chronic kidney disease with clinically significant
renal impairment, heart failure, non-malignant pancreatic disease, chronic pulmonary disease, or
chronic headache. The last eight questions are in relation to medications consumed by the
patient including fentanyl, morphine, methadone, hydromorphone, an ER/LA formulation of any
opioid, a benzodiazepine, an anti-depressant, and if the patient’s maximum prescribed opioid
dose is >100mg MED.
Once the questionnaire is completed, the first step is to determine the RIOSORD score;
the maximum score for the 16-item questionnaire is 146 points. The second step involves
identification of the risk class for overdose or serious OIRD, which corresponds to an average
probability of overdose or serious OIRD. Table 7 provides a conversion of the IMS RIOSORD
score in points to risk class and average probability of overdose or serious OIRD. A copy of the
IMS RIOSORD tool is provided in Appendix C.
IMPLEMENTING A RISK INDEX TOOL 45
Remitigate, LLC will provide access to an electronic version of the RIOSORD tool called
Naloxotel. Remitigate, LLC was founded in 2015 by pain therapeutics pharmacist Dr. Jeffrey
Fudin in collaboration with Dr. Nadia Shahzad and Dr. Nicholas W. D. Jarrett; the company
provides software solutions for medical professionals who care for patients taking long-term
opioids (Remitigate, LLC, n.d.). Naloxotel is a software application that assigns a percent risk of
OIRD based on a validated multivariate linear regression model coupled with drug interactions
based on the research by Zedler, Xie, et al. (Remitigate, LLC, n.d.). The software application
will enable clinicians and even pharmacists to generate a comprehensive progress note of the
OIRD assessment that can be printed and scanned or transferred into the patient’s EMR. The
Table 7
Conversion of RIOSORD Score to Risk Class and Probability of Overdose
or Serious OIRD
RIOSORD Score
(Points)
Risk Class Average Probability of
Overdose or Serious OIRD
0-4 1 2%
5-7 2 5%
8-9 3 7%
10-17 4 15%
18-25 5 30%
26-41 6 55%
>42 7 83%
Note. OIRD = opioid-induced respiratory depression; RIOSORD = Risk
Index for Overdose or Serious Opioid-Induced Respiratory Depression.
Adapted from Zedler, B., Saunders, W., Joyce, A., Vick, C., & Murrelle, L.
(2015). Validation of a screening risk index for overdose or serious
prescription opioid-induced respiratory depression. Poster session
presented at the 2015 American Academy of Pain Medicine Annual
Meeting, National Harbor, MD.
IMPLEMENTING A RISK INDEX TOOL 46
software also has the capability to create a prior authorization request letter for in-home naloxone
access (Remitigate, LLC, n.d.). Permission to use the Naloxotel application along with free
software access through December 31, 2017 has been granted to the project team members that
are directly involved in data collection (i.e., the DNP student and content expert). Naloxotel
training will be completed prior to the start of the project, which merely involves using the
software a few times to become familiar with its applications and features. The providers
involved in the use of the application (i.e., the DNP student and content expert) will discuss use
of the application and clarify any concerns or questions of its use with Dr. Fudin prior to start of
the project. Examples of the comprehensive progress note and prior authorization letter
generated by Naloxotel are provided in Appendices F and G.
Intervention and Data Collection. The intervention is to co-prescribe naloxone to
patients on COT found to have an increased risk of serious OIRD as a rescue medication to use
in the event of an opioid-related emergency. Neither study conducted by Zedler, Xie, et al.
(2015) nor Zedler, Saunders, et al. (2015) indicates a recommended score in which to qualify
patients for a co-prescription of naloxone. However, in a study conducted by Cleary, Raouf,
Nguyen, Carpenter, and Fudin (2016) utilizing the VHA RIOSORD tool, a RIOSORD score of
>25 points was chosen to qualify patients for naloxone for in-home use due to the associated
>14% probability for OIRD. Using the VHA RIOSORD cut-off score as a guide, an IMS
RIOSORD score of >10 will be used in this project to determine which patients are viewed as
“increased risk” for opioid overdose or serious OIRD. An IMS RIOSORD score of 10-17
corresponds to risk class 4, which carries a 15% probability of serious OIRD (Zedler, Saunders,
et al., 2015). The patients that are determined to be “increased risk” will receive the
intervention, which is a co-prescription for naloxone. The Naloxotel prior authorization letter
IMPLEMENTING A RISK INDEX TOOL 47
states the patient has received education on opioid risk factors, how to minimize such risks, and
was offered naloxone for in-home use and that the patient has agreed to fill the prescription for
naloxone. Thus, patient education on the purpose and proper administration of naloxone is
warranted.
Naloxone hydrochloride is a short-acting, non-addictive, opioid antagonist that is used for
respiratory or central nervous system depression from opioid overdose with over 30 years of
proven effectiveness if administered correctly and in a timely fashion (Merlin, Ariyaprakai, &
Fh, 2015; Zedler et al., 2014). In 1971, naloxone received US Food and Drug Administration
approval and subsequently became the standard first-line agent in the emergency setting for rapid
reversal of accidental or intentional opioid overdose (Merlin et al., 2015). Naloxone is available
in many different forms including generic and brand name versions. Generic naloxone is
available as an intramuscular injection or an intranasal mucosal atomizer may be used for
intranasal delivery. Brand name versions of naloxone include the Evzio Auto-Injector or the
Narcan Nasal Spray. See Figure 6 for a pictorial of the different formulations of naloxone that
are available to prescribe.
In addition to co-prescribing naloxone, education will be provided on the symptoms of
opioid overdose, rescue breathing, and proper administration of naloxone (education must be
specific to the prescribed method of delivery). An example of a patient education handout on
opioid overdose symptoms and resuscitation instructions is provided in Appendix H. Free
instructional video downloads are available from PrescribetoPrevent.org on how to administer
generic intramuscular and intranasal naloxone as well as the brand name Evzio Auto-Injector. A
video demonstration on the use of the brand name Narcan Nasal Spray is available at
www.narcan.com. The videos can be used in the office for patient education and training on
IMPLEMENTING A RISK INDEX TOOL 48
naloxone administration but patients may also access the videos at home to educate family and
friends on naloxone administration. The office nurses will be beneficial in providing assistance
with patient education on naloxone training. Appendix I contains a nurse checklist to ensure that
naloxone training is consistent and that patients receive the appropriate education depending on
type of naloxone delivery system prescribed. One important aspect of naloxone training is to
advise patients to inform family and/or friends where the naloxone is stored in addition to proper
Narcan Nasal Spray Generic naloxone with intranasal
(brand name) mucosal atomizer
Evzio Auto-Injector Generic naloxone for
(brand name) intramuscular injection
Figure 6. Naloxone delivery systems. This pictorial demonstrates the various
formulations of naloxone delivery systems that are available to prescribe.
IMPLEMENTING A RISK INDEX TOOL 49
use of the prescribed formulation of naloxone. Education on the use of the prescribed naloxone
device is crucial to ensure correct administration and delivery of the life-saving medication. For
example, if prescribing the generic naloxone intranasal spray, it is important that the patient and
family/friend knows how to assemble the intranasal mucosal atomizer device and that half of the
dose is administered in one nostril followed by the other half in the opposite nostril. However, if
the brand named Narcan Nasal Spray is prescribed, the full dose is administered in only one
nostril. It is also important to remind patients to be aware of expiration dates on the naloxone
and to request refills as needed based on use and expiration of the product. Appendix J contains
a patient education handout that provides naloxone resources and overdose prevention tips.
Timeline. DNP project implementation is expected to begin in February 2017 pending
approval or exemption from the Internal Review Board of VCU Health System. A student
affiliation agreement for students at VCU Health System entities will be secured prior to the start
date. This agreement confers access to patient information, use of medical records, and the
confidentiality of patient data and/or health information. The DNP student as well as
representatives from VCU Health System and CMH sign this agreement.
The project will be conducted for a total of six months with an expected end date of
August 2017. Prior to implementation of the actual project, at least two Plan-Do-Study-Act
(PDSA) cycles will be conducted in January 2017 to test the planned practice change and
determine if any modifications are needed with implementation. Communication within the
project practice setting will be conducted during the daily morning huddles and as needed
throughout the day to address any deficiencies or clarify any concerns among the project team
members and other available staff resources. Project evaluation will begin in September 2017
and end in December 2017. Appendix K provides a detailed timeline of the DNP project.
IMPLEMENTING A RISK INDEX TOOL 50
Potential Risks and Threats
A foreseeable risk to the success of this project is that a patient does experience an
overdose or serious OIRD event and does not have naloxone available for in-home use. It would
be important to determine if the patient had been assessed for risk of serious OIRD, if naloxone
was prescribed, and if the patient filled the naloxone prescription. The lack of naloxone
availability is a contributory cause of opioid overdose deaths in patients on COT and a primary
reason for this DNP project. This could be a result of the patient not filling the prescription, lack
of coverage by insurance, high out-of-pocket cost for the prescription, or family/friends not
knowing where the naloxone is stored. Another potential risk or threat is the inability to use the
naloxone appropriately by family members or friends. Due to the timeliness of this topic in the
midst of the opioid overdose epidemic, prescribing practices of naloxone are starting to increase
despite the use of a validated tool to assess risk of overdose or serious OIRD. This could be
viewed as a threat to the project and affect comparison to designated benchmark goals.
Project Evaluation
Implementation of a risk mitigation strategy such as the RIOSORD tool and utilizing
recommendations for safe opioid prescribing practices in patients on COT aligns well with
national goals to improve access to safe, effective pain treatment and reducing the risk for
overdose with prescription opioids (i.e., CDC and National Pain Strategy; Dowell et al., 2016).
As previously mentioned, the metric in which to gauge the success of this DNP project is a 15%
increase in the number of prescriptions written for naloxone by clinicians at VCU-CMH Pain
Management. This benchmark aligns well with the HHS Opioid Initiative agency priority goal
of reducing opioid-related morbidity and mortality, which includes a 15% increase in the number
IMPLEMENTING A RISK INDEX TOOL 51
of prescriptions dispensed for naloxone in the U.S. outpatient retail pharmacy setting as one of
the outcome measures.
The IMS RIOSORD tool will be used to assess patients’ risk for serious OIRD if the
patient meets pre-determined inclusion criteria described under Subjects in the Methods section.
An IMS RIOSORD score of >10 will be used as the cut-off score to determine which patients are
at “increased risk” for overdose or serious OIRD; this score corresponds to a 15% probability of
overdose or serious OIRD. Multivariable logistic regression modeling of the strongest OIRD-
associated variables within the commercial insurance population demonstrated a C-statistic of
0.90, which indicates excellent discrimination between cases and controls (Zedler, Saunders, et
al., 2015). Such models are considered strong and reliable if the C-statistic is greater than 0.8,
which indicates that the probability of predicting the outcome is better than by chance alone
(University of Manitoba, 2011). Covariates from the original VHA RIOSORD tool were
modified to accommodate for differences in the commercial insurance population and point
values were assigned to the most statistically significant RIOSORD predictors based on the
corresponding β-coefficients (Zedler, Saunders, et al., 2015). Thus, the 16 covariates included in
the IMS RIOSORD were found to be statistically significantly associated with serious OIRD in
the commercial insurance population. These particular covariates were selected with an effort to
balance both the scientific and statistical robustness of each variable’s association with OIRD
against the need for a practical yet brief instrument that possesses optimum simplicity and
accuracy when completed by a clinician within a typically busy care setting (Zedler, Saunders, et
al., 2015). The predictive validity of the IMS RIOSORD tool was assessed by comparing the
distribution of predicted probabilities, by percentiles, with the observed incidence of overdose or
serious OIRD within the study sample (Zedler, Saunders, et al., 2015). Among the seven risk
IMPLEMENTING A RISK INDEX TOOL 52
classes, the average predictive probability of a serious OIRD event ranged from 2% in the lowest
risk class (class 1, 0-4 points) to 83% in the highest risk class (class 7, >42 points), and the
observed occurrence of overdose or serious OIRD increased commensurately (Zedler, Saunders,
et al., 2015). Figure 7 demonstrates the increase in predictive probability compared to the
observed occurrence of overdose or serious OIRD.
At the end of the six-month project period, both providers will complete the RIOSORD
Provider Satisfaction Survey as a summative assessment of this project. The survey assesses for
ease of use and provider satisfaction with the RIOSORD tool. Such information is helpful to
Figure 7. The predicted probability versus observed incidence of overdose or serious
OIRD. This chart demonstrates the predicted probability (risk classes, by percentiles)
versus observed incidence of overdose or serious OIRD.
Note. OIRD = opioid-induced respiratory depression.
Source: Zedler, B., Saunders, W., Joyce, A., Vick, C., & Murrelle, L. (2015). Validation
of a screening risk index for overdose or serious prescription opioid-induced respiratory
depression. Poster session presented at the 2015 American Academy of Pain Medicine
Annual Meeting, National Harbor, MD.
IMPLEMENTING A RISK INDEX TOOL 53
gain insight into the clinical applicability and feasibility of continued use of the RIOSORD tool,
which will be summarized in the project evaluation. The DNP student developed this survey due
to lack of a pre-existing questionnaire that addressed provider satisfaction and ease of use. The
RIOSORD Provider Satisfaction Survey is provided in Appendix L.
Data Analysis Plan
A copy of each RIOSORD questionnaire will be imported or scanned into each patient’s
EMR and a copy will be kept by the project investigator (DNP student) for data collection. Data
from the questionnaire will be transferred into a Microsoft Excel spreadsheet for future data
analysis (i.e., total RIOSORD score, risk class, probability of overdose or serious OIRD, and
presence of individual covariates from the RIOSORD tool). Project data will be de-identified as
to be compliant with the Health Insurance Portability and Accountability Act, which ensures the
protection of individually identifiable health information. Patient name, chart number, and date
of birth will not be recorded as to protect patient identification; instead, a random identification
number will be assigned to each patient included in the project. This information will be stored
in a single password protected document that only the project investigator can access. Data will
be saved on a password protected encrypted flash drive that will remain in the sole possession of
the project investigator (i.e., DNP student). The project investigator will also be the only person
collecting and maintaining data as to maintain consistency in the data collection process.
However, it is possible that input from the visit provider will be necessary for clarification
purposes on occasion. Other information to collect includes patient demographics (e.g., age,
race, and gender), date of visit/RIOSORD assessment, visit provider, date of onset of chronic
pain, length of time on COT, prescribed opioid(s), total MED of all prescribed opioid(s), whether
IMPLEMENTING A RISK INDEX TOOL 54
naloxone was prescribed (or previously prescribed), and formulation of naloxone prescribed.
This information will be obtained by review of each patients’ EMR.
During the six months of project implementation, the project investigator will also
conduct a retrospective chart reviews to obtain information on factors that may have influenced a
provider to co-prescribe naloxone prior to project implementation. Data will be extracted from
patient visits of the six months prior to the project start date to serve as comparison data. Data to
collect during the retrospective chart reviews includes date of data extraction, number of eligible
patients, number of times naloxone was prescribed, and contributing factors that influenced
naloxone prescribing. This information will be obtained from a combination of sources
including the daily schedule for each provider, the medication list to determine if patient was
“eligible” (e.g., prescribed opioids for 90 days or longer) and if naloxone was prescribed, and
review of previous office notes to infer contributing factors for prescribing naloxone.
Summary statistics will be used to provide a description of primary outcome #1
(calculated RIOSORD score for each patient assessed). Such descriptive/summary statistics of
the RIOSORD score include measures of central tendency (mean, median, and mode) and
measures of dispersion (standard deviation, range, and quartiles). Primary outcomes #2 (the
number of patients determined to be “increased risk” for overdose or serious OIRD) and #3 (the
number of prescriptions written for naloxone) will be reported as an overall count and percentage
of those screened. In order to determine if the benchmark goal of a 15% increase in naloxone
prescribing is met, both the count and percentages of naloxone prescribing for six months before
and six months after implementation of the RIOSORD tool will be collected and compared. A
control chart (i.e., P-chart) can be utilized to demonstrate the average number of naloxone
prescriptions written per week both before and after implementation of the RIOSORD tool and
IMPLEMENTING A RISK INDEX TOOL 55
thus evaluate the effectiveness of the RIOSORD tool in increasing naloxone prescribing. A P-
chart (“P” stands for “percent” or “proportion”) is used to demonstrate count data of
nonconforming units (e.g., yes/no, pass/fail, either/or; Carey, 2003). The nonconforming unit in
this study is whether naloxone was co-prescribed (i.e., yes/no). It may be beneficial to post the
P-chart in a common staff area in order to monitor progress of the DNP project and to promote
use of the RIOSORD tool. A possible limitation of the project’s findings include that the DNP
student is both the project investigator and a subject in the project, which introduces the potential
for bias.
Inferential statistics will be used to analyze secondary outcome measures, which include
covariates from the RIOSORD tool itself. A statistical analysis such as multiple logistic
regression that seeks a relationship between the dependent and independent variable(s) is
appropriate for this outcome measure because this test inquires if one measure predicts the other,
if one measure depends on the other, or if there is a trend between two sets of measures.
Multiple logistic regression models estimate the odds probability of the dependent variable (i.e.,
whether or not naloxone is co-prescribed) occurring as the values of the independent variables
(i.e., covariates of the RIOSORD tool) change (Keller & Kelvin, 2013). An odds ratio measures
how much more likely an outcome is to occur given certain conditions or exposures; statistical
significance of the odds ratio is determined by the p-value (Keller & Kelvin, 2013). The
dependent variable in logistic regression models is dichotomous (i.e., having two categories) and
the independent variable(s) can be of any measurement (Keller & Kelvin, 2013). The advantage
of multiple logistic regression is that it allows for computation of odds ratios that are adjusted to
account for the effect of other variables on both the risk factor and the outcome (Keller &
Kelvin, 2013). JMP Pro 12 data analysis software will be used to conduct statistical analyses.
IMPLEMENTING A RISK INDEX TOOL 56
Discussion and Implications
Review of the literature regarding management of CNCP with COT strongly indicates the
need for rigorous, high quality studies that evaluate and promote patient safety and quality
improvement outcomes. Treating chronic pain patients can be challenging and requires a
multimodal plan of care. The potential for misuse, abuse, addiction, or overdose should be
recognized as part of this plan in addition to increasing access to naloxone. Utilizing the
RIOSORD tool in clinical practice will identify patients at risk for accidental overdose, which
can lead to OIRD and possibly death. The RIOSORD score can guide naloxone prescribing to
identify which patients are most likely to benefit from the availability of in-home naloxone.
Rather than providing a naloxone prescription to all individuals prescribed an opioid, the
RIOSORD score will provide a quantitative risk measurement to guide this decision.
Clinical Implications
Utilizing a validated, risk assessment tool to increase access to naloxone aligns well with
the national call for action to reduce opioid overdoses and promote safe opioid prescribing. The
implications for this project specifically include the ability to educate patients on their risk for
OIRD (or overdose), increase provider knowledge on factors that contribute to increased risk for
OIRD, increase access to naloxone for the clinic’s patient population, and thus reduce or prevent
opioid-related overdose. Implications for future practice are to raise awareness to the availability
of the RIOSORD tool and promote its use. The project also anticipates the ability to provide
information on feasibility of RIOSORD use in clinical practice as well as generalizability based
on data obtained from provider satisfaction surveys. Other implications inferred from the
literature review include the need to increase provider education within the pain management
arena including utilization of the CDC guideline for prescribing opioids for chronic pain in
IMPLEMENTING A RISK INDEX TOOL 57
addition to increasing access to naloxone, recognition of substance use disorder, and referral for
medication-assisted therapy when needed. Zedler, Xie, et al. (2015) note that patients that are
prescribed ER/LA opioid formulations, MED >100mg/day, and/or opioids from multiple
providers are prone to greater healthcare utilization. Clinical implications of this DNP project
(i.e., patient education on OIRD, provider knowledge on risk factors for OIRD, and increasing
access to naloxone) include a possible reduction in unnecessary utilization of healthcare services
for opioid-related emergencies. Recommendations for future research include the need to
monitor patients for use of in-home naloxone. Studies should include the identification of
variables that contribute to the need for naloxone and their relation to those included in the
RIOSORD assessment. Continuous process improvement and monitoring the reliability of the
tools performance is crucial to its success and recommendations for use.
DNP Essentials. Using the Stetler model of research utilization as its guide, this DNP
project seeks to demonstrate synthesis of information from the available literature and utilization
of its findings to implement a practice change. The project will support learnings from the
Virginia Commonwealth University School of Nursing DNP program curriculum and
demonstrate an understanding of the foundations expected of a DNP prepared nurse. Once
completed, the project will fully meet The Essentials of Doctoral Education for Advanced
Nursing Practice developed by the American Association of Colleges of Nursing in October
2006. The DNP Essentials consist of required foundational competencies and curricular
elements of the DNP program that are core to all advanced practice nursing roles (American
Association of Colleges of Nursing, 2006). There are eight foundational DNP Essentials.
Appendix M provides a table outlining the relationship the DNP Essentials to this DNP project.
IMPLEMENTING A RISK INDEX TOOL 58
Quality and Safety. This DNP project is a quality improvement initiative for practice
change. The aforementioned purpose is to implement a risk assessment strategy that may reduce
and/or prevent overdose deaths from prescription opioids. At this time, there is no local or
national protocol in place to guide the recommendation to increase access to naloxone.
However, the RIOSORD provides the capability to fulfill this need. Implementation of the
RIOSORD tool will seek to identify individuals on COT that are at increased risk of serious
OIRD or unintentional overdose and serve as a guide to provide a co-prescription for in-home
naloxone if needed in the event of an opioid related emergency. The aims demonstrate an
evidence-based approach to improve patient outcomes, increase quality of care, and promote safe
opioid use and safe opioid prescribing practices.
In order to ensure quality of the project itself, the Stetler model of research utilization
served as a framework for project planning. The Stetler model aligns well with the revised
Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) guidelines, which
supports the reporting of findings from systems level projects to improve the quality, safety, and
value of healthcare (SQUIRE, 2015). In order to fulfill SQUIRE guidelines, baseline
measurement of variables should be obtained. Measurement of current naloxone prescribing
practices will serve as a comparison to evaluate the effectiveness of the proposed practice
change. A 15% increase in naloxone prescribing is the set goal to measure success of the
practice change. Detailed information about the intervention in addition to validity and
reliability on utilization of any clinical tools should be addressed. The RIOSORD is a validated
tool that has demonstrated reliability in both the VHA and IMS populations. Utilization of the
SQUIRE 2.0 guidelines not only helps to ensure the quality of a project but also improves the
ability to generalize findings to similar situations or replicate findings in similar populations.
IMPLEMENTING A RISK INDEX TOOL 59
Plan for Sustainability
The preliminary plan for sustainability includes strategic planning to promote the
ongoing use of the RIOSORD tool to assess risk for overdose and OIRD, the need to reassess
risk status regularly, and the need to follow-up with patients in relation to prescribing naloxone.
Establishing a strategic plan that includes transparency and sustainability objectives is beneficial
to the success of the practice change and its continued use. Transparency allows for the free
flow of ideas and the ability to discuss what is and is not working among all participants in the
DNP project. Sustainability objectives for this project are to continue use of the RIOSORD tool,
maintain an up-to-date RIOSORD score yearly or as needed, and provide adequate patient
education on overdose and OIRD in relation to COT so that patients will follow through with
recommendations for in-home naloxone. Table 8 provides an outline of recommended steps to
achieve the above objectives. The project investigator will be responsible for steps during
initiation of the project; however, as the project progresses and benefits of the RIOSORD tool
become evident, clinical staff will become empowered to continue its use. Transparency, early
involvement, and buy-in from the clinical staff will promote sustainment of the project.
The project investigator will serve as the project champion and will provide regular
project updates to stakeholders and the health system’s local decision makers. Stakeholders and
decision makers will need to be educated on the importance of the DNP project and its
contribution to local and national calls for help in reducing the opioid overdose epidemic. Such
informational updates will be beneficial to identify potential decision makers to win over as well
as who might be the best contact(s). Informational training sessions will be provided for clinical
providers and staff to ensure that patients are educated properly and consistently. A patient
education checklist will aid in ensuring this expectation. Stakeholders, decision makers, and
IMPLEMENTING A RISK INDEX TOOL 60
clinical providers/staff will be encouraged to contact the project investigator as needed with any
questions or concerns. The project investigator will utilize available resources in providing
appropriate information to stakeholders and decision makers. A faculty advisor from VCU
School of Nursing DNP program and two content experts (i.e., a pain management specialist and
a doctor of pharmacy) are included in the DNP project team; they will serve as consultants to the
project investigator (i.e., DNP student) as needed. Dr. Jeffrey Fudin from Remitigate, LLC will
serve as a contact for the Naloxotel software application. Heather Thomson, MS, Associate
Director of Medical Science, Director of Health Economics and Outcomes Research of kaléo
Pharma has been a beneficial resource to provide information and feedback during the project
proposal and implementation phases in addition to helping establish contact with Dr. Barbara
Zedler who developed the RIOSORD tool.
On-going operational costs specific to this project include printing supplies and cost for
use of the Naloxotel software. Dr. Jeffrey Fudin has granted free access until December 31,
2017 for now. However, the yearly rate to continue use is $25.00/year per user to utilize the
PC/Mac versions of the Naloxotel software; a mobile application is not available at this time. An
alternative would be to utilize a paper version of the RIOSORD tool but that would increase the
cost of printing supplies. Benefits to the continued use of the electronic software includes the
ability to choose whether the patient is from the general population or is a U.S. military veteran,
built-in calculations for the RIOSORD score and MED of prescribed opioids, and generation of a
prior authorization letter regarding the patient’s individualized RIOSORD score including need
for in-home naloxone. The current EMR is slated to convert to Cerner in the fall of 2017, which
should not pose a problem with use of the Naloxotel software application itself. The planned
process of uploading or scanning RIOSORD results into the EMR should be feasible with
IMPLEMENTING A RISK INDEX TOOL 61
continued use. No other capital equipment depreciation or replacement is anticipated at this
time.
Table 8
Steps to Achieve Sustainability Objectives
Steps to achieve
objective:
Who does
the work? What does success look like?
What resources
are needed?
• Due date:
1. Identify staff
concerns regarding
RIOSORD use.
• PI Staff questions answered and
solutions provided in regards to
use of RIOSORD.
Staff time
• Daily
2. Monitor for proper
use of RIOSORD
tool.
• PI Naloxotel software is properly
utilized to obtain RIOSORD
score.
PI Time
• Weekly
3. Utilize an EMR
clinical alert to
repeat RIOSORD
screening yearly.
• PI
• Clinical
Providers
Clinical providers repeat
RIOSORD screening yearly;
EMR clinical alert resets.
Clinical alert
development;
clinical provider
time
• Yearly
4. Encourage clinical
providers to repeat
RIOSORD
screening as needed.
• PI
• Clinical
Providers
RIOSORD screening updated
when there are changes in
patient’s medical or
psychological status,
medications, and/or MED status;
naloxone prescription renewed if
indicated.
Clinical provider
time
• As needed
5. Educate patients on
the risk of overdose
and OIRD with
COT, purpose of in-
home naloxone, and
delivery method of
prescribed naloxone.
• Clinical
Providers
• Nursing
staff
Patients on COT are
knowledgeable of the risk for
overdose and OIRD and proper
use of prescribed naloxone
device.
Staff training
sessions; clinical
provider/nursing
staff time
• January 2017
(training)
• On-going
6. Monitor patient
compliance on
filling naloxone
prescription.
• Clinical
Providers
• Nursing
staff
Patients fill prescription for
naloxone as recommended and
inform family/friends of its
location and use.
Staff training
sessions; clinical
provider/nursing
staff time
IMPLEMENTING A RISK INDEX TOOL 62
• January 2017
(training)
• On-going
7. Identify patient’s
questions and
concerns regarding
RIOSORD score
and/or naloxone use.
• Clinical
Provider
• Nursing
staff
Patient questions and concerns
on RIOSORD score and/or
naloxone use are
answered/solved.
Clinical
provider/nursing
staff time
• On-going
8. Monitor for use of
in-home naloxone.
• Clinical
Provider
• Nursing
staff
Patients report on use of
naloxone at follow-up
appointments and ask for refill
as needed.
Clinical
provider/nursing
staff time
• On-going
9. Perform monthly
random chart
reviews to monitor
for RIOSORD use
and associated
patient outcomes.
• PI RIOSORD use continued on all
patients prescribed opioid pain
medication and updated yearly.
Data collected on an ongoing
process utilizing an Excel
document to store data.
Clinical
provider/nursing
staff time
• Monthly for
random chart
reviews
• Weekly for
data collection
10. Monitor provider
satisfaction.
• PI Provider satisfaction surveys
administered yearly.
Clinical
provider/nursing
staff time
• Yearly
Note. COT = chronic opioid therapy; EMR = electronic medical record; MED = morphine
equivalent dose; OIRD = Overdose or Serious Opioid-Induced Depression; PI = Project
Investigator; RIOSORD = Risk Index for Overdose or Serious Opioid-Induced Depression.
Plans for dissemination include poster presentations, sharing knowledge of the
RIOSORD tool and Naloxotel software with affiliate clinics (i.e., VCU-CMH practices), and
other local primary care offices. An application will be submitted for a poster presentation of the
literature review findings at the Virginia Council for Nurse Practitioner’s (VCNP) annual
conference in March 2017. Once the project is completed, a poster presentation at the 2018
VCNP annual conference would be appropriate in addition to a pain management conference
such as the International Conference on Opioids held in Boston, Massachusetts annually.
IMPLEMENTING A RISK INDEX TOOL 63
Publication will be considered; relevant peer-reviewed publications include the Practical Pain
Management, which is a comprehensive journal for information on chronic pain and/or The
Journal of Pain, which publishes original articles related to all aspects of pain. Dr. Jeffrey Fudin
is a member of the editorial board of Practical Pain Management and will be instrumental in
providing assistance from a publication perspective.
IMPLEMENTING A RISK INDEX TOOL 64
References
Agency for Clinical Innovation. (n.d.). 5As – Opioid therapy monitoring tool. Retrieved from
http://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0019/212761/5_As_of_Analgesia.p
df
Alford, D. (2016). Opioid prescribing for chronic pain: achieving the right balance through
education. The New England Journal of Medicine, 374(4), 301-303.
American Association of Colleges of Nursing. (2006, October). The essentials of doctoral
education for advanced nursing practice. Retrieved from
http://www.aacn.nche.edu/publications/position/DNPEssentials.pdf
Carey, R. G. (2003). Improving healthcare with control charts: Basic and advanced SPC
methods and case studies. Milwaukee, WI: ASQ Quality Press.
Centers for Disease Control and Prevention. (2016a, March 16). Injury prevention & control:
Opioid overdose, prescribing data. Retrieved November 11, 2016, from
http://www.cdc.gov/drugoverdose/data/overdose.html
Centers for Disease Control and Prevention. (2016b, June 21). Injury prevention & control:
Opioid overdose, prescription opioid overdose data. Retrieved September 29, 2016, from
http://www.cdc.gov/drugoverdose/data/overdose.html
Centers for Disease Control and Prevention. (2016c, June 21). Injury prevention & control:
Opioid overdose, understanding the epidemic. Retrieved September 5, 2016, from
http://www.cdc.gov/drugoverdose/epidemic/index.html
Centers for Disease Control and Prevention. (2016d, August 25). Injury prevention & control:
Opioid overdose, guideline resources. Retrieved September 5, 2016, from
http://www.cdc.gov/drugoverdose/prescribing/resources.html
IMPLEMENTING A RISK INDEX TOOL 65
Centers for Disease Control and Prevention. (2016e, August 30). Injury prevention & control:
Opioid overdose, prevention for states. Retrieved September 28, 2016, from
http://www.cdc.gov/drugoverdose/states/state_prevention.html
Cheung, C. W., Qiu, Q., Choi, S., Moore, B., Goucke, R., & Irwin, M. (2014). Chronic opioid
therapy for chronic non- cancer pain: A review and comparison of treatment guidelines.
Pain Physician, 17(5), 401-414.
Chou, R., Turner, J. A., Devine, E. B., Hansen, R. N., Sullivan, S. D., Blazina, I., . . . Deyo, R.
A. (2015). The effectiveness and risks of long-term opioid therapy for chronic pain: A
systematic review for a National Institutes of Health pathways to prevention workshop.
Annals of Internal Medicine, 162(4), 276-286 11p. doi:10.7326/M14-2559
Cleary, J. H., Raouf, M., Nguyen, U., Carpenter, M. R., & Fudin, J. (2016). Automated software
platform to assess pre-validated risk for opioid-induced respiratory depression to qualify
patients for in-home naloxone. Poster session presented at the 2016 International
Conference on Opioids, Boston, MA.
Coffin, P., Behar, E., Rowe, C., Santos, G., Coffa, D., Bald, M., & Vittinghoff, E. (2016).
Nonrandomized intervention study of naloxone coprescription for primary care patients
receiving long-term opioid therapy for pain. Annals of Internal Medicine, 165(4), 245-52.
Dang, D., Melnyk, B. M., Fineout-Overholt, E., Ciliska, D., DiCenso, A., Cullen, L., . . .
Stevens, K. R. (2015). Models to guide implementation and sustainability of evidence-
based practice. In Evidence-based practice in nursing & healthcare: A guide to best
practice (3rd ed.), (pp. 274-315). Philadelphia, PA: Wolters Kluwer.
IMPLEMENTING A RISK INDEX TOOL 66
Dowell, D., Haegerich, T. M., & Chou, R. (2016, March 18). CDC guideline for prescribing
opioids for chronic pain – United States, 2016. MMWR Recommendations and Reports;
65(1): 1-49. doi: http://dx.doi.org/10.15585/mmwr.rr6501e1
Drug Policy Alliance. (2016). A sensible plan. Retrieved October 5, 2016, from
http://www.drugpolicy.org/new-solutions-drug-policy/sensible-plan
Florence, C. S., Zhou, C., Luo, F., & Xu, L. (2016). The economic burden of prescription opioid
overdose, abuse, and dependence in the United States, 2013. Medical Care, 54(10), 901-
906.
Fudin, J. (2015, December 18). Risk tool helps pharmacists qualify patients for take-home
naloxone. Pharmacy Times, 12. Retrieved from
http://www.pharmacytimes.com/contributor/jeffrey-fudin/2015/12/risk-tool-helps-
pharmacists-qualify-patients-for-take-home-naloxone
Juurlink, D., & Dhalla, I. (2012). Dependence and addiction during chronic opioid therapy.
Journal of Medical Toxicology, 8(4), 393-399. Doi:10.1007/s13181-012-0269-4
Kellar, S. P. & Kelvin, E. A. (2013). Monro’s statistical methods for health care research (6th
ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Levine, M. J., Brown, D., & Ferguson, D. (2015, August 31). Opioid overdose risk mitigation
(Clinicians’ Letters, 2015). Retrieved from Virginia Department of Health:
http://www.vdh.virginia.gov/clinicians/
Manchikanti, L., Helm, S., Fellows, B., Janata, J. W., Pampati, V., Grider, J. S., & Boswell, M.
V. (2012). Opioid epidemic in the United States. Pain Physician, 15(Suppl. 3), ES9-38.
IMPLEMENTING A RISK INDEX TOOL 67
Merlin, M. A., Ariyaprakai, N., & Fh, A. (2015). Assessment of the safety and ease of use of the
naloxone auto-injector for the reversal of opioid overdose. Open Access Emergency
Medicine, 2015, 21-24.
Murthy, V. H. (2016, August). The Surgeon General’s call to end the opioid crisis (Clinician
Letter). Retrieved September 28, 2016, from http://turnthetiderx.org/
National Collaborating Centre for Methods and Tools. (2011). Stetler model of evidence-based
practice. Hamilton, ON: McMaster University. Retrieved June 25, 2016, from
http://www.nccmt.ca/resources/search/83
National Institute on Drug Abuse. (2014, July). Drugs, brains, and behavior: The science of
addiction (NIH Publication No. 14-5605). Retrieved September 4, 2016, from
https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/preface
National Institute on Drug Abuse. (2015, December). Overdose death rates. Retrieved
September 29, 2016, from https://www.drugabuse.gov/related-topics/trends-
statistics/overdose-death-rates
National Institute on Drug Abuse. (2016, February 18). Naloxone prescriptions from
pharmacies increased ten-fold. Retrieved October 5, 2016, from
https://www.drugabuse.gov/news-events/news-releases/2016/02/naloxone-prescriptions-
pharmacies-increased-ten-fold
Nuckols, T. K., Anderson, L., Popescu, I., Diamant, A. L., Doyle, B., Di Capua, P., & Chou, R.
(2014). Opioid prescribing: A systematic review and critical appraisal of guidelines for
chronic pain. Annals of Internal Medicine, 160(1), 38-47. Doi:10.7326/0003-4819-160-1-
201401070-00732
Remitigate, LLC. (n.d.). Remitigate. Retrieved from http://www.remitigate.com/
IMPLEMENTING A RISK INDEX TOOL 68
Rudd, R. A., Aleshire, N., Zibbell, J.E., & Gladden, R.M. (2016, January 1). Increases in drug
and opioid overdose deaths: United States, 2000-2014. Morbidity and Mortality Weekly
Report, 64(50); 1378-82. Retrieved from
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm
SQUIRE. (2015). Revised standards for quality improvement reporting excellence: SQUIRE
2.0. Retrieved from http://www.squire-
statement.org/index.cfm?fuseaction=Page.ViewPage&PageID=471
Substance Abuse and Mental Health Services Administration. (2016a, February 23). Opioids.
Retrieved September 29, 2016, from http://www.samhsa.gov/atod/opioids
Substance Abuse and Mental Health Services Administration. (2016b). SAMHSA opioid
overdose prevention toolkit (HHS Publication No. SMA 16-4742). Retrieved from
http://store.samhsa.gov/product/Opioid-Overdose-Prevention-Toolkit-Updated-
2016/SMA16-4742
U.S. Department of Health and Human Services. (n.d.). FY 16-17: Agency priority goal.
Reduce opioid-related morbidity and mortality. Retrieved October 5, 2016, from
https://www.performance.gov/node/47231?view=public
University of Manitoba. Manitoba Centre for Health Policy, Community Health Sciences.
(2011, October 24). Term: C-statistic. Retrieved October 16, 2016, from http://mchp-
appserv.cpe.umanitoba.ca/viewDefinition.php?definitionID=104234
University of Virginia. Weldon Cooper Center for Public Service. (2011, April). Regional
profile: Southside Virginia stat chat. Retrieved from
http://www.coopercenter.org/sites/default/files/node/13/Southside_Region_CooperCenter.pd
f
IMPLEMENTING A RISK INDEX TOOL 69
Volkow, N. D. (2014, May 14). America’s addiction to opioids: Heroin and prescription drug
abuse. Retrieved from https://www.drugabuse.gov/about-nida/legislative-
activities/testimony-to-congress/2016/ mericas-addiction-to-opioids-heroin-prescription-
drug-abuse
VCU Health Community Memorial Hospital. (2016.) Mission, vision and values. Retrieved
from http://www.vcu-cmh.org/content/MissionVisionAndValues.htm
VCU School of Medicine. (2016, January). The opioid crisis among Virginia Medicaid
beneficiaries. Retrieved from
http://hbp.vcu.edu/media/hbp/policybriefs/pdfs/Senate_OpioidCrisisPolicyBrief_Final.pdf
Wakeland, W., Schmidt, T., Gilson, A. M., Haddox, J. D., & Webster, L. R. (2011). System
dynamics modeling as a potentially useful tool in analyzing mitigation strategies to reduce
overdose deaths associated with pharmaceutical opioid treatment of chronic pain. Pain
Medicine, 12, S49-58 1p. doi:10.1111/j.1526-4637.2011.01127.x
World Health Organization. (2014, November). Management of substance abuse: Information
sheet on opioid overdose. Retrieved September 4, 2016, from
http://www.who.int/substance_abuse/information-sheet/en/
Zedler, B., Saunders, W., Joyce, A., Vick, C., & Murrelle, L. (2015). Validation of a screening
risk index for overdose or serious prescription opioid-induced respiratory depression.
Poster session presented at the 2015 American Academy of Pain Medicine Annual Meeting,
National Harbor, MD.
Zedler, B., Xie, L., Wang, L., Joyce, A., Vick, C., Brigham, J., … Murrelle, L. (2015).
Development of a risk index for serious prescription opioid-induced respiratory
IMPLEMENTING A RISK INDEX TOOL 70
depression or overdose in veterans’ health administration patients. Pain Medicine 16(8),
1566-1579. Doi:10.1111/pme.12777
Zedler, B., Xie, L., Wang, L., Joyce, A., Vick, C., Kariburyo, F., . . . Murrelle, L. (2014). Risk
factors for serious prescription opioid-related toxicity or overdose among veterans health
administration patients. Pain Medicine, 15(11), 1911-1929. Retrieved from
http://proxy.library.vcu.edu/login?url=http://search.ebscohost.com.proxy.library.vcu.edu/
login.aspx?direct=true&AuthType=ip,url,cookie,uid&db=s3h&AN=99620845&site=eho
st-live&scope=site
IMPLEMENTING A RISK INDEX TOOL 71
Appendix A
Flow Diagram of the Search Process
Iden
tifi
cati
on
Scr
eenin
gE
ligib
ilit
yIn
cluded
Articles identified through
database searching
(n = 613)
Additional articles identified
through other sources
(n = 0)
Articles after duplicates removed
(n = 520)
Abstracts screened
(n = 520)
Abstracts excluded
(n = 391)
Full-text articles assessed for
eligibility
(n = 129)
Full-text articles excluded,
with reasons
(n = 112)
Studies included
(n = 17)
IMPLEMENTING A RISK INDEX TOOL 72
Appendix B
RIOSORD Tool used in the Veterans’ Health Administration
Source: Fudin, J. (2015, December 18). Risk tool helps pharmacists qualify patients for
take-home naloxone. Pharmacy Times, 12. Retrieved from
http://www.pharmacytimes.com/contributor/jeffrey-fudin/2015/12/risk-tool-helps-
pharmacists-qualify-patients-for-take-home-naloxone
IMPLEMENTING A RISK INDEX TOOL 73
Appendix C
RIOSORD Tool used in the Commercial Insurance Population
Source: Zedler, B., Saunders, W., Joyce, A., Vick, C., & Murrelle, L. (2015). Validation of a screening risk index
for overdose or serious prescription opioid-induced respiratory depression. Poster session presented at the 2015
American Academy of Pain Medicine Annual Meeting, National Harbor, MD.
IMPLEMENTING A RISK INDEX TOOL 74
Appendix D
Proposed DNP Project Budget
Budget period: February 2017 – August 2017
Direct Costs
Category Calculations Final Costs
I. Materials/Supplies/
Educational Handouts
a. Paper 30 pt/d x 3d/wk = 90 pt/wk
90 pt/wk x 16 wks = 1440 pts
(1 case, 5000 sheets) x 2
cases
111.98
c. Toner Black, yields 11,000 pages 43.99
II. Naloxotel (electronic
RIOSORD tool)
0
III. Other
a. Educational videos 0
Total Direct Costs = $ 155.97
Indirect Costs
Category Calculations Final Costs
I. Staffing salary/wages
a. MD (1) $ 216/hr x 120 hr 25,920.00
b. NP (1) $ 49/hr x 120 hr 5,880.00
a. Nurses (2 LPNs) $ 18/hr x 120 hr (x 2) 4,320.00
b. Clerical (1) $ 12/hr x 60 hr 720.00
II. Equipment
a. Computers, copiers,
printer, scanner
0
III. Information Technology
a. EMR system $ 1300/mo x 6 mo 7,800.00
b. E-prescribing (included in EMR cost)
IV. Facilities
a. Office rental $ 2,500/mo x 6 mo 15,000.00
b. Office utilities $ 366/mo x 6 mo 2,196.00
c. Office maintenance $ 17/mo x 6 mo 102.00
Total Indirect Costs = $ 61,938.00
Notes. Indirect costs are already part of the established practice setting. COT = chronic
opioid therapy; d = days; DNP = Doctor of Nursing Practice; EMR = electronic medical
record; hr = hours; LPN = licensed practical nurse; MD = medical doctor; mo = months; NP =
nurse practitioner; pt = patients; RIOSORD = Risk Index for Overdose or Serious Opioid-
Induced Respiratory Depression; wk = weeks.
IMPLEMENTING A RISK INDEX TOOL 75
Appendix E
The Stetler Model of Research Utilization
Source: Stetler, C. (2001). Updating the Stetler Model of research utilization to facilitate evidence-based practice. Nursing
Outlook, 49(6), 272-279.
IMPLEMENTING A RISK INDEX TOOL 76
Appendix F
Example of a Naloxotel Comprehensive Progress Note
Documented: 09/11/16
Provider: Dr. Joe Payne, Physician
Patient: Jane Doe, 00/00/0000, ID 123456 Prescribed drugs:
hydrocodone 20 mg/day
methadone 30 mg/day
Total Morphine Dose:
288mg/day
The following parameters were evaluated and identified to elevate risk for opioid-induced
respiratory depression in this patient:
Within the past 6 months the patient had a healthcare visit (outpatient, inpatient, or ED) involving any
the following health conditions:
- Chronic kidney disease with clinically significant renal impairment
- Chronic pulmonary disease (e.g., emphysema, chronic bronchitis, asthma, pneumoconiosis,
asbestosis)
- Chronic headache (e.g., migraine)
Prescribed Drugs or Drug Classes Identified by RIOSORD:
Methadone
An extended-release or long-acting (ER/LA) formulation of any prescription opioid, including the
above A prescription antidepressant (e.g., fluoxetine, citalopram, venlafaxine, amitriptyline)
The following parameters were evaluated and identified to elevate risk for opioid-induced respiratory
depression to this patient above that which is calculated for the validated RIOSORD: carisopridol,
hydoxazine
Predicted Opioid Risk Assessment - 83%
This patient was evaluated for percent risk of opioid-induced respiratory depression using the
validated RIOSORD [1, 2] analysis tool. This patient was determined to have a(n) 83% risk based on
the unique criteria outlined herein.
357 Delaware Avenue, #214, Delmar, NY 12054 E [email protected] P 781-472-4637 www.naloxotel.com
IMPLEMENTING A RISK INDEX TOOL 77
Appendix G
Example of a Naloxotel Prior Authorization Letter
Documented: 09/11/16
Provider: Dr. Joe Payne, Physician
Patient: Jane Doe, 00/00/0000, ID 123456 Prescribed drugs:
hydrocodone 20 mg/day
methadone 30 mg/day
Total Morphine Dose:
288mg/day
This patient was evaluated for percent risk of opioid-induced respiratory depression using the
validated RIOSORD [1, 2] analysis tool. This patient was determined to have a(n) 83% risk based on
the unique criteria outlined herein.
For this reason, naloxone for in-home use is recommended for this patient. This recommendation is
consistent with AMA, ASAM, FDA, CDC, SAMHSA and other professional organization
recommendations or guidelines to provide in-home naloxone for patients receiving opioids that are at
risk for opioid induced respiratory depression.
This patient is on hydrocodone 20mg/day which is metabolized by CPY 2D6 to a more active
metabolite and by 3A4 to an inactive metabolite. For this reason, a medication inducer or inhibitor
may increase or decrease these levels and place the patient at higher risk
Patient and caregiver was/were counseled on opioid risk factors, how to minimize such risks, and
offered naloxone for in-home use. Based on the overall assessment and understanding of patient
and/or caregiver, it is determined that the best option for this patient is: Evzio Auto-Injector. This is
due to the following reason(s): Patient's caregiver lacks the manual dexterity or strength to manipulate
intranasal dosage form, Patient has medically documented physical or pathological issue to one or
both naris.
Patient agrees to fill prescription for naloxone as outlined above. Education about overdose
prevention and instructions for use of Evzio Auto-Injector for OPIOID OVERDOSE reversal were
provided to this patient and/or caregiver. Method of contact was In-person. Length of the session was
40 minutes.
1. Zedler, Barbara, et al. "Development of a Risk Index for Serious Prescription Opioid-Induced Respiratory Depression or
Overdose in Veterans' Health Administration Patients." Pain Medicine 16.8 (2015): 1566-1579.
2. Zedler BK, Saunders W, Joyce A, Vick C, Murrelle L. Validation of a screening risk index for serious prescription opioid-
induced respiratory depression or overdose in a national commercial insurance claims database. Pain Medicine, 2015.
357 Delaware Avenue, #214, Delmar, NY 12054 E [email protected] P 781-472-4637 www.naloxotel.com
IMPLEMENTING A RISK INDEX TOOL 78
Appendix H
Opioid Overdose Symptoms and Resuscitation Instructions
IMPLEMENTING A RISK INDEX TOOL 79
Appendix I
Nurse Checklist for Naloxone Training
_____
1. Determine need for naloxone training based on type of naloxone delivery system
prescribed.
_____ 2. Play appropriate video to provide an overview and demonstration of the prescribed
method of naloxone delivery.
_____ 3. Demonstrate use of the Evzio Auto-Injector using the trainer device (if this is the
prescribed naloxone delivery system).
_____ 4. Provide patient with a copy of the Naloxotel Comprehensive Progress Note, which
explains the patient’s opioid risk assessment and probability of opioid-induced
respiratory depression.
_____ 5. Provide patient education handouts on opioid overdose resuscitation, naloxone
resources, and overdose prevention tips.
_____ 6. Provide written instructions for the prescribed naloxone delivery device.
_____ 7. Ask patient if there are any questions and provide answers if able. If not able, have
the visit provider talk to patient regarding concerns prior to discharge from clinic.
_____ 8. Submit Naloxotel prior authorization letter if needed for insurance coverage
determination for the prescribed naloxone delivery system.
_____ 9. Follow-up with patient via phone call one week after appointment date to inquire if
the prescription for naloxone was filled and if there are any further questions.
IMPLEMENTING A RISK INDEX TOOL 80
Appendix J
Overdose Prevention Tips and Naloxone Resources
How to Avoid Overdose:
Only take medication that is prescribed for you
Do not take more than prescribed
Call if your pain worsens
Never mix pain medication with alcoholic beverages
Avoid taking pain medication at the same time as sleep medications
Store pain medication in a secure location
Bring any unused medication to the office for disposal
Learn how to use naloxone
Teach family/friends how to respond to an overdose
Learn how to use naloxone:
Naloxone is a medication that can be given as an injection into the thigh muscle or
sprayed up the nose to reverse the effects of an opioid pain medication and save lives.
Call 911 for help; even after giving naloxone. More than one dose of naloxone may
be required to fully reverse an overdose.
Follow Opioid Overdose Resuscitation instructions to provide rescue breathing until
help arrives.
Be sure that family/friends know where naloxone is stored and how to use it.
There are various ways to give naloxone to someone. It is important to become
familiar with the delivery method that is prescribed.
Visit PrescribeToPrevent.com to view educational videos on how to respond to an
overdose and how to use naloxone. Use the Patient Education tab to gain access to
the educational videos that are available for viewing.
Other sources:
Evzio.com to learn how to use the Evzio AutoInjector.
Narcan.com to learn how to use the Narcan nasal spray.
IMPLEMENTING A RISK INDEX TOOL 81
Appendix K
Proposed DNP Project Timeline
Project Implementation
Project starts
Start data collection
Start retrospective chart reviews
Project Implementation
Project ends
Complete data collection
Complete retrospective chart reviews
Project
Planning Begins
October 2016 December 2016 January 2017 February 2017 August 2017 September 2017 December 2017
Project
Proposal
Project Evaluation
Finalize all data collection
Begin data analysis
PDSA Cycles Project Evaluation
Finalize data analysis
IMPLEMENTING A RISK INDEX TOOL 82
Appendix L
RIOSORD Provider Satisfaction Survey
Please respond to the following questions using a scale of 1 to 10.
(1 = the lowest rating and 10 = the highest rating)
1. How would you rate ease of use of the RIOSORD during patient visits?
1 2 3 4 5 6 7 8 9 10
2. How would you rate the perceived benefit of using the RIOSORD tool in clinical practice?
1 2 3 4 5 6 7 8 9 10
3. How would you rate the overall usefulness of the RIOSORD tool?
1 2 3 4 5 6 7 8 9 10
4. How would you rate your overall satisfaction with use of the RIOSORD?
1 2 3 4 5 6 7 8 9 10
5. Would you recommend other clinicians to use the RIOSORD tool in clinical practice?
(1 = would not recommend…10 = highly recommend)
1 2 3 4 5 6 7 8 9 10
6. How would you rate the amount of time required to administer the RIOSORD?
(1 = it did not take a long time/did not significantly add to the patient visit time…10
= took too long/added significantly to the patient visit time)
1 2 3 4 5 6 7 8 9 10
7. How would you rate your likelihood of continuing to use the RIOSORD questionnaire?
(1 = would not continue to use…10 = will continue to use)
1 2 3 4 5 6 7 8 9 10
IMPLEMENTING A RISK INDEX TOOL 83
Appendix M
Relationship of the DNP Essentials to the DNP Project
DNP Essential DNP Project
I. Scientific Underpinnings
for Practice
The project demonstrates integration of nursing science with
knowledge gained from ethical, biophysical, psychosocial,
analytical, and organizational sciences. This knowledge
translates into the highest level of nursing practice as
evidenced by evaluation and synthesis of evidence obtained
from review of the literature in regards to COT and opioid-
related overdose, use of a theoretical model to guide the
DNP project, and implementation of a new practice
approach to increase access to naloxone.
II. Organizational and
Systems Leadership for
Quality Improvement and
Systems Thinking
The project implements and evaluates a care delivery
approach to meet the current and future needs of patients on
COT. Use of the Stetler model of research utilization will
guide the decision-making processes for the delivery of
quality healthcare and provision of patient safety for those
on COT. The project investigator acts as the project
champion or leader through this process.
III. Clinical Scholarship and
Analytical Methods for
Evidence-Based Practice
The project designs and implements a quality improvement
plan and processes to evaluation outcomes to promote safe,
timely, effective, and patient-centered care. The RIOSORD
tool is a validated risk assessment tool used to obtain an
individualized score for the probability of overdose that the
clinician can use to determine need for in-home naloxone.
Data collection will help to identify naloxone-prescribing
patterns to improve practice and the practice environment.
Dissemination of findings via poster presentations at various
nurse practitioner and/or pain management conferences will
help to improve patient outcomes beyond the local level.
IV. Information
Systems/Technology and
Patient Care Technology
for the Improvement and
Transformation of Health
Care
The project demonstrates the selection of a software
application (i.e., Naloxotel) that evaluates and monitors
patient outcomes in relation to healthcare delivery and
quality improvement in patient outcomes. The project
investigator analyzes and communicates critical elements in
the selection, use, and evaluation of patient care technology
with the project team and clinical project setting.
V. Health Care Policy for
Advocacy in Health Care
The project investigator critically analyzes health policies
for recommendations to reduce opioid-related overdose
IMPLEMENTING A RISK INDEX TOOL 84
deaths and increasing access to naloxone. The project
investigator also demonstrates the ability to educate others
such as stakeholders and staff on the importance of
improving healthcare outcomes and promoting safe opioid
use through use of evidence-based practice guidelines such
as the CDC opioid prescribing guidelines.
VI. Interprofessional
Collaboration for
Improving Patient and
Population Health
Outcomes
The DNP project involves use of effective communication
skills to build interprofessional collaborative relationships
in the development of a quality improvement, patient safety
scholarly project. The project investigator employs
consultative skills at workshops and conferences to establish
collaborative relationships and contacts. The project
investigator also provides leadership to the project team
from conception to completion of the project in addition to
planning for sustainability.
VII. Clinical Prevention and
Population Health for
Improving the Nation’s
Health
The DNP project analyzes epidemiological, biostatistical,
and other appropriate scientific data related to the
population health of persons suffering from CNCP as well
as the prevalence of opioid-related overdose. The project
investigator synthesizes information related to clinical
prevention of opioid-related overdose deaths and promotes
improvement of patient outcomes/patient safety through
implementation of interventions to address access to
naloxone in addition to safer opioid prescribing practices.
The project investigator will also evaluate the effectiveness
of strategies to reduce opioid-related morbidity and
mortality.
VIII. Advanced Nursing
Practice
The DNP project conducts a systematic assessment of
physical and mental health and illness parameters in patients
on COT that contribute to risk for overdose. Utilization of
the RIOSORD tool provides a comprehensive risk
evaluation in which to guide clinical judgement and systems
thinking in regards to naloxone prescribing. The project
investigator and/or clinician(s) use this information to
educate and guide patients on appropriate risk reduction
strategies. The sharing of knowledge gleaned from the
review of the literature, synthesis of information, and
conception of this project contributes to the development
and sustainment of therapeutic relationships with patients,
staff, colleagues, and other professionals in relation to the
delivery of optimal healthcare, improvement of patient
outcomes, and promotion of safe opioid use. The project
investigator also acts as a mentor and provides guidance and
IMPLEMENTING A RISK INDEX TOOL 85
Notes. CDC = Centers for Disease Control and Prevention; CNCP = chronic noncancer pain;
COT = chronic opioid therapy; DNP = Doctor of Nursing Practice; RIOSORD = risk index for
overdose or opioid-induced respiratory depression.
Source: American Association of Colleges of Nursing. (2006, October). The essentials of
doctoral education for advanced nursing practice. Retrieved from
http://www.aacn.nche.edu/publications/position/DNPEssentials.pdf
support for other nurses to achieve excellence in nursing
practice.