Robotic Intracerebral Hemorrhage Evacuation: An In-Scanner...
Transcript of Robotic Intracerebral Hemorrhage Evacuation: An In-Scanner...

Robotic Intracerebral Hemorrhage Evacuation:
An In-Scanner Approach with Concentric Tube Robots
Isuru S. Godage, Member, IEEE, Andria A. Remirez, Student Member, IEEE, Raul Wirz, Member, IEEE,
Kyle D. Weaver, Jessica Burgner-Kahrs, Member, IEEE, and Robert J. Webster III, Senior Member, IEEE
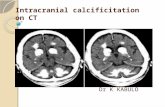
Abstract— Several robotic systems have been proposed forremoving blood from the brain in patients who have undergonea hemorrhagic stroke. In this paper we explore the use of image-based feedback to address tissue deformation when aspiratinga hemorrhage in a phantom model. This is the first timeintraoperative image feedback has been used with a concentrictube robot in this application. We describe a layer by layerapproach to motion planning. Computed tomography (CT)images are collected periodically during hemorrhage removal.After each CT scan, the robot’s tip path is re-planned toaccount for the tissue deformation that has occurred since theprevious scan. We compare open loop hemorrhage removal toour sequential imaging-replanning approach, illustrating thatthe latter has the potential to enhance the safety and efficacyof the procedure.
I. INTRODUCTION
Intracerebral hemorrhage (ICH), or bleeding in the brain,
is a life-threatening condition which occurs with a fre-
quency of 24.6 per 100,000 person-years [1]. This means
that approximately 1 in 50 people are likely to have an
ICH in their lifetime, given current life expectancy1. The
high incidence, 40% mortality rate, and high frequency
of debilitating complications even in patients who survive,
makes ICH a compelling public health challenge [2]. An ICH
occurs when a cerebral blood vessel ruptures, causing blood
to escape into the brain and pool, forming a hematoma (a
collection of semi-clotted blood outside the blood vessels)
which compresses surrounding brain tissue.
ICH is typically treated with medication and observation.
In some cases, open surgery is attempted to remove the
hematoma. This is because it is commonly believed by
neurosurgeons that there is an at-risk volume of brain tissue
that can be saved, provided it can be decompressed [3]–
[6]. This provides strong motivation for surgical intervention,
yet traditional surgical approaches have not been effective in
This research was supported in part by the National Science Foundationunder CAREER award IIS-1054331 and in part by the National Institutes ofHeath under award R21 NS087796. The content is solely the responsibilityof the authors and does not necessarily represent the official views of theNational Science Foundation or the National Institutes of Health.
I. S. Godage, A. A. Remirez, R. Wirz, and R. J. Webster III are with theDepartment of Mechanical Engineering, Vanderbilt University, Nashville,TN USA [email protected]
K. D. Weaver is with the Department of Neurological Surgery, VanderbiltUniversity Medical Center, Nashville, TN USA.
J. Burgner-Kahrs is with the Center of Mechatronics (MZH), LeibnizUniversitaet Hannover, Germany.
1This is based on the assumption that risk is consistent at all ages, andneglects the possibility of some people having more than one in their lives.Thus, it is a rough approximation, but useful for tangibly understanding themagnitude of the public health challenge posed by ICH.
reducing overall mortality rates to date, and there remains
no treatment of proven clinical benefit for the majority of
ICH patients [7]. One potential reason for this is the invasive
nature of surgical interventions, which disrupt a substantial
volume of healthy tissue to enable access to the site of the
hemorrhage. Indeed, less invasive, endoscopic methods of
ICH evacuation have shown benefit for some specific groups
of patients [8]. Goradia et al. first explored robotic assistance
in endoscopic ICH evacuation using a straight morcellator
to debulk the hemorrhage, concluding that robotic assistance
may help prevent damage to healthy brain tissue during the
procedure [9]. We have previously proposed that a steerable
needle-based approach may benefit patients [10], and other
steerable robots are under development for neurotargeting
applications [11] such as ICH.
Needle-based neurosurgery itself has long been of interest
in surgical robotics [12]–[14]. Most prior systems use straight
needle paths to hit specific targets in the brain. ICH debulking
poses a different challenge, since it requires dexterous motion
of the needle tip within the hematoma. This challenge was an
early motivation for the development of bevel-steered needles
[15], [16], but ICH removal has yet to be achieved with
them, likely due to challenges achieving tight curvatures and
integrating lumens or other interventional tools. Concentric
tube robots have been previously explored in benchtop,
animal, or cadaver experiments for a variety of neursurgical
applications [17]–[19] requiring steering of a needle-sized
curved device.
One way to debulk a hematoma less invasively – through
a needle-sized entry path – was introduced by the authors
previously [10]. The system uses an image-guided concentric
tube robot to debulk an ICH from within, in a minimally
invasive manner. We use the same robot (described in Section
II) in this work. See [20], [21] for a description of the
general mechanics-based model that describes these robots.
In this paper we use a special case of concentric tube robot
that does not require the solution to a beam mechanics
problem to compute forward kinematics, the same special
case considered in [10].
Our contribution in this paper is the integration of intra-
operative computed tomography (CT) imaging, as well as a
description of one way to plan the tip path of the robot within
the hematoma. We use a layer-by-layer motion planning
approach that decomposes the 3D planning problem into a
series of 2D planning problems. Some prior research has
focused on motion planning for concentric tube robots (see
e.g. [22]–[24].) However, prior motion planning research has
2015 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS)Congress Center HamburgSept 28 - Oct 2, 2015. Hamburg, Germany
978-1-4799-9994-1/15/$31.00 ©2015 IEEE 1447

typically focused on obstacle avoidance rather than coverage
of a volume in space. Additionally, prior results generally
assume a single robot (i.e. a fixed set of several tubes)
which is unchanged throughout the task. This is in contrast
to our approach for ICH, in which only two tubes are used
at any given time, but one of them can be removed and
replaced with a new tube of a different curvature whenever
desired. The experiments in Section IV demonstrate that
the use of imaging feedback and periodic replanning can
prevent damage to surrounding healthy brain tissue due to
deformation of the tissue during hemorrhage evacuation.
II. SYSTEM OVERVIEW AND WORKFLOW
Figure 1 shows the robotic intracerebral hemorrhage evac-
uation system. The actuation unit for the concentric tube
robot (which was previously described in [10]) is mounted
on a lockable articulated arm, which holds it in place above
the patient’s head. The actuation unit delivers a concentric
tube robot into the patient’s brain. We use a special case
concentric tube robot that has only two tubes, with the
outer tube being straight and stiff, relative to the superelastic
curved inner cannula (see Fig. 2). The kinematics of this
robot are given in [10]. The robot is able to insert-retract
both its outer and inner tubes, and also axially rotate its inner
cannula. By doing this, the robot can articulate its tip inside
the hemorrhage (the interested reader can find information
on the workspace of concentric tube robots like this in [25]).
Suction is attached to the back of the inner tube, enabling
the robot to aspirate material.
In [10] we described a potential interventional workflow
based on preoperative CT images with intraoperative optical
tracking. Here, we propose use of intraoperative CT imaging,
which can enable a more aggressive removal of hemorrhage
material. We will discuss the pros and cons of both ap-
proaches in Section V. Both may be clinically feasible, and
each has advantages and disadvantages.
The workflow we propose in this paper is as follows.
First the patient and the robot will be placed in the scanner
as shown in Fig. 1. A preoperative scan will be collected,
and the robot will contain fiducial markers that enable its
six degree-of-freedom pose to be determined in relation
to patient anatomy (see e.g. [26] for one way to perform
registration of a robot to image space in a CT scanner). The
robot will then be repositioned to aim its insertion direction
according to the physician’s desired insertion trajectory. A
second scan may now be collected to verify alignment.
Next, planning software similar to that used for tube
optimization in [10] will be used to select curved tubes to be
used sequentially to aspirate the hematoma from an existing
set available in the operating room (in [10] we showed that
a small number of options is sufficient to capture anatomical
variability across a patient dataset). The path for each tube
will then be planned as described in Section III. After the
surgeon approves the plan, the robot will insert its outer tube
into the patient to the hematoma, the first curved tube will
be installed, and aspiration initiated, likely starting at the
centroid of the hematoma. At any time during aspiration,
lockable
articulated arm
CT scanner
needle
robot
actuation unit
Fig. 1: Illustration of robotic ICH evacuation system concept.
Fig. 2: (a) An illustration of a two-tube concentric tube robot inserted intoa simulated hemorrhage. (b) An overlay of several configurations that canbe achieved by inserting and retracting both tubes and axially rotating theprecurved, superelastic inner cannula.
the physician may stop the robot, and obtain a new CT
scan. Then software will replan the sequence of tubes and
the paths of each, the surgeon will approve the plan, and
the robot will again commence aspiration. We imagine this
being done iteratively until the physician determines that a
sufficient volume of hemorrhage material has been removed.
III. MOTION PLANNING
In [10], motion planning was left to future work. Exper-
iments were conducted by manually entering a sequence of
coordinates for the needle tip, as the experimenter visually
observed the procedure through semi-transparent gelatin. In a
clinical scenario, automated motion planning is desirable. We
employ a layer-by-layer motion planning approach, which
decomposes the tip motion planning problem into a series of
2D problems.
We begin by segmenting the hematoma volume from
the images, an then slice it into two-dimensional layers
perpendicular to the axis of the needle. For each layer, a
spiral tip path is then generated as shown in Fig. 3, which
begins at the centroid of the layer and spirals outward, taking
on the shape of the boundary of the hematoma within that
layer as it approaches the edges. We note that a safety margin
can be intentionally left around the periphery of the lesion,
1448

Fig. 3: Illustration of the spiral trajectory generated by the motion planningalgorithm for an example layer of the targeted hemorrhage volume.
and this is likely to be desirable in a clinical implementation.
The entire trajectory of the tip is completed by sequentially
moving from the ending point of the path in one layer to
the starting point of the path in the next layer, until all the
layers have been traversed.
As blood is removed by the robot and pressure is relieved
from the surrounding brain tissue, the size and shape of
the hematoma and surrounding brain tissue will change due
to brain deformation. Hence, we expect multiple iterations
of imaging and motion planning to typically be useful in
maximizing the volume of hemorrhage that can be removed
safely without damaging the surrounding brain tissue.
IV. IN-SCANNER EXPERIMENTS
We conducted a series of experiments in a CT scanner
to explore the benefits of iterative scanning and re-planning
during hemorrhage aspiration. These experiments used the
phantom shown in Fig. 4, and the experimental setup shown
in Fig. 5.
A. Phantom Brain and Hematoma Preparation
The complete brain phantom is shown in Fig. 4. The brain
phantom (see Fig. 4). was made of 5% by weight Knox™
gelatin, formed in a brain mold. This concentration has been
shown to provide some mechanical properties similar to
mouse brain tissue, particularly in terms of shear modulus
[27]. The hemorrhage was also composed of Knox™ gelatin
but with a 2% by weight concentration to represent the semi-
coagulated blood in a hematoma. The hematoma was molded
first, and embedded in the brain gel before it was fully
solidified. The hematoma was shaped in a 45 mm diameter
spherical mold with Barium Sulfate added for CT contrast
enhancement (0.5% by weight).
After casting, the complete brain phantom was placed
inside a life size plastic human skull model (see Fig. 4). A
layer of foam was placed under the gelatin brain in the skull
to support the brain at the proper level (i.e., with its surface
touching the inside surface of the skull cap).
B. Experimental Procedure
The brain phantom, robot, and CT scanner were arranged
as shown in Fig. 5. The head phantom was held securely in
place on a wooden platform with elastic VELCRO™ bands.
C
D B
A
Fig. 4: The anatomical model used in the experiments consists of (A) agelatin brain phantom, (B) an embedded hematoma model (Note that thehematoma model is spherical, although refraction from the brain surfacemay make it appear otherwise in the image), (C) a rigid plastic skull, and(D) a foam cushion to support the brain and hold it against the skull cap.
A
B
F
D
E
C
Fig. 5: Our experimental setup: (A) the robot inserted through a burr holeon top of the skull, (B) the lockable positioning arm holding the robot,(C) the brain phantom from Fig. 4), (D) the Xoran XCAT CT scanner, (E)Simulink™ Realtime system, and (F) the vacuum pump.
The tip of the outer tube was aimed toward the hematoma
and inserted a short distance into the brain through a small
opening created in the skull to simulate a burr hole. A CT
scan was collected and the location of the hemorrhage with
respect to the needle tip was identified via segmenting in 3D
Slicer [28]. The resulting stereo lithography (STL) file was
imported into Matlab for motion planning. The joint-space
coordinates corresponding to the desired spiral path were
generated using the inverse kinematic model [10]. During
robot motion, the robot was controlled using the Matlab™
Simulink™ environment under the Simulink Real-Time sys-
tem setup. The software transitions between the joint-space
reference trajectory points via linear interpolation.
In the experiments in this paper, the path planner described
in Section III was employed, with a 2.5 mm layer spacing
and 2.5 mm maximum spiral pitch at a speed of 2 mms−1
at the tip. A 5 mm safety margin was left at the periphery of
the hematoma in the planning process. Suction was applied
using a Gomco model 300 medical grade suction pump.
1449

Clot
Brain
A
B
Fig. 6: CT scan images from the open loop debulking experiment. Theleft image shows the pre-operative scan and the right image shows thepostoperative scan, where (A) illustrates damage to brain tissue and (B)shows the remainder of the hematoma.
(a)
~5mm
(b)
Fig. 7: An illustration of the hematoma before and after the open loopexperiment. The left image shows the preoperative CT scan with residualhematoma overlaid in green. The right image shows a closeup of thehematoma.
C. Open Loop Experiment
This experiment was designed to evaluate whether the
hematoma could be safely aspirated without iterative imaging
and re-planning. The initial hematoma volume was measured
at 40.8 mL. Upon completion of the procedure, a CT
scan was taken and is shown in Fig. 6. Segmenting the
postoperative scan data, we find that 7.16 mL of hematoma
was left behind accounting for 82% removal (see Fig. 7a).
Upon close inspection of the CT images, it is evident that
the aspiration process damaged healthy brain tissue due to
tissue deformation, despite the planned 5 mm safety margin
(Fig. 7b).
This damage is visible in Fig. 8 which compares the
extent of tissue damage within the brain tissue region of the
phantom model with respect to the final estimated hematoma
volume. The concentric tube tip trajectories in different
aspiration layers and tearing of the brain model are visible in
the image. This indicates that brain deformation during the
aspiration process results in significant hematoma geometry
changes, and motivates a desire for intraprocedural imaging
feedback.
D. Intraoperative Imaging and Replanning Experiment
In this experiment we used iterative CT imaging with re-
planning with the goal of improving safety and accuracy. The
preoperative CT is shown in Fig. 9a. The initial hematoma
volume was 42.49 mL. The procedure was divided into 3
iterations, with a CT image volume collected at the start
Fig. 8: Visualization of damage to the brain tissue (red volume) with respectto the final hematoma volume (blue sphere).
A
B
(a) (b)
(c) (d)
Fig. 9: CT image feedback from the closed loop debulking experiment(a) pre-operative, (b) first intra-operative image, (c) second intra-operativeimage, and (d) final CT image of the completed aspiration procedure.
of each. The first iteration lasted approximately 1/4 of the
duration that would have been required for a full open-loop
experiment (as was done in Section IV-C). The CT image
taken at the start of the second iteration is shown in Fig. 9b
which shows partial removal of the hematoma.
The remaining hematoma volume at the start of the second
iteration was 35.0 mL, and a new motion plan was generated
for the second iteration based on the new image volume.
The motion plan was then implemented until approximately
1/2 of the aspiration of the remaining hematoma material
had been completed. The image shown in Fig. 9c was then
collected which showed 18.7 mL of hematoma remaining.
While the 5 mm margin was impinged upon, the tip of the
cannula did not damage brain tissue.
The third and final iteration then commenced, resulting
in the postoperative CT image shown in Fig. 9d, illustrating
that the expected hematoma volume has been removed with
no appreciable damage to surrounding brain tissue. Figure
1450

(a)
~2mm
(b)
Fig. 10: An illustration of the hematoma before and after the iterativeimaging-replanning experiment. The left image shows the preoperative ctscan with residual hematoma overlaid in brown. The right image shows acloseup of the hematoma. One can observe that while the planned 5 mmmargin was not maintained, it served its purpose in preventing brain tissuefrom being damaged.
10 compares the initial and final volumes of the hematoma
illustrating the 85% aspiration achieved (final volume 6.54
mL). Comparing Fig. 10 to Fig. 7, one can see that the use
of intraoperative imaging made the procedure safer.
V. DISCUSSION AND CONCLUSIONS
The experimental results presented in this paper demon-
strate the potential usefulness of intra-operative imaging
during hemorrhage aspiration. If one were to use preoperative
images alone, one would have to be much more conservative
in removing only the center of the hematoma, and leaving a
large safety margin to account for tissue deformation. While
this may still lead to clinical benefit (physicians do not
know how much hematoma material must be removed for
clinical benefit to begin, but estimate that even as little as
25% removal may be clinically useful), it may sometimes
be desirable to be more aggressive in removing hematoma
material. Intraoperative CT imaging enables one to observe
tissue deformation and compensate for it in the motion plan.
Of course, the price to be paid for this is additional radiation
to the patient from additional scans. This may be deemed a
price worth paying, since an ICH is a life or death situation
with 40% mortality.
There is substantial opportunity for optimization within
the framework described in this paper. While we began our
aspiration at the edge of the hematoma, it would probably be
preferable to begin at the center (or in another statistically
optimal location, based on a brain deformation model) in a
clinical implementation. The trajectory planning/replanning
algorithm could also be optimized to work directly in 3D
rather than using the layer-by-layer approach we employed
here which would be particularly useful for hematoma shapes
with more complex geometry [29].
We have not reported procedure durations in this paper,
because we have not yet optimized the system to minimize
procedure time. Our complete aspirations (all iterations, not
including imaging time) in this paper took approximately 50
minutes each, which is not much different than the 20-40
minutes it typically takes a surgeon to resect a hematoma
once he/she has opened the brain and reached the hematoma
surface. In future work, we plan to optimize both path
planning and the speed with which the robot’s tip moves
within the hematoma to minimize procedure time. Suction
pressure can also be optimized to control the volume locally
aspirated at the cannula tip, at a given position. While it
is desirable to remove the hematoma as fast as is safely
possible, we believe that procedure durations of roughly an
hour will be easily tolerated clinically. Another open question
we plan to study in the future is how coagulated the blood can
be and still be aspirated through tubes of various diameters.
Our hypothesis is that there will be a period of time in
which the hematoma is sufficiently soft that it can be locally
aspirated.
Intraoperative image feedback appears useful for account-
ing for brain shift and increasing the portion of hematoma
targeted. However radiation dose is a concern, and so it will
be useful in future work to optimize the percentage of the
plan targeted at each iteration to minimize the number of
scans required. Toward the same objective, it would also be
useful in future work to introduce brain deformation models,
to predict the deformation of the brain as hematoma material
is aspirated [30]. Burr hole ultrasound imaging is another
possibility for image feedback that eliminates the radiation
issue. A benefit of ultrasound would be real-time feedback
[31], [32]. A drawback would be the lower quality images
provided, and the probable need to create a second opening
in the skull to place the ultrasound transducer on the brain
surface.
VI. CONCLUSIONS
This paper compared the initial experimental results for
minimally invasive robotic intracerebral hemorrhage evac-
uation with and without intraoperative CT feedback. The
experiments were carried out on phantom brain-hematoma
models. A simple, 2D-layer-based aspiration path planner
was employed. Both experiments produced comparable re-
sults in hematoma removal and aspiration efficiency but
the procedure with feedback significantly reduced the brain
tissue damage. Analysis of CT image data of the experiments
showed that the hematoma-brain boundary changes during
aspiration, necessitating image feedback. This is as expected
based on prior literature describing substantial brain shift
during neurosurgical interventions. Future research will in-
vestigate optimizing imaging frequency, optimizing motion
planning algorithms, and potentially employing ultrasound
for real-time feedback. We believe that the basic approach
described in this paper holds great promise for testing
the hypothesis that surgical outcomes today are not better
because of the drawback of disrupting a substantial volume
of healthy brain tissue. If this hypothesis proves correct, a
future robotic system of the type we describe in this paper
may save many lives, by providing a minimally invasive
intervention for ICH.
REFERENCES
[1] C. J. van Asch, M. J. Luitse, G. J. Rinkel, I. van der Tweel, A. Algra,and C. J. Klijn, “Incidence, case fatality, and functional outcome ofintracerebral haemorrhage over time, according to age, sex, and ethnic
1451

origin: a systematic review and meta-analysis,” The Lancet Neurology,vol. 9, no. 2, pp. 167–176, 2010.
[2] M. Dey, A. Stadnik, and I. A. Awad, “Thrombolytic evacuation ofintracerebral and intraventricular hemorrhage,” Current Cardiology
Reports, vol. 14, no. 6, pp. 754–760, 2012.
[3] A. I. Qureshi, A. D. Mendelow, and D. F. Hanley, “Intracerebralhaemorrhage,” Lancet, vol. 373, no. 9675, pp. 1632–1644, 2009.
[4] J. Broderick, S. Connolly, E. Feldmann, D. Hanley, C. Kase,D. Krieger, M. Mayberg, L. Morgenstern, C. S. Ogilvy, P. Vespaet al., “Guidelines for the management of spontaneous intracerebralhemorrhage in adults,” Stroke, vol. 38, no. 6, pp. 2001–2023, 2007.
[5] W.-Z. Wang, B. Jiang, H.-M. Liu, D. Li, C.-Z. Lu, Y.-D. Zhao, andJ. W. Sander, “Minimally invasive craniopuncture therapy vs. con-servative treatment for spontaneous intracerebral hemorrhage: resultsfrom a randomized clinical trial in China,” Int. Journal of Stroke,vol. 4, no. 1, pp. 11–16, 2009.
[6] N. Etminan, K. Beseoglu, B. Turowski, H.-J. Steiger, and D. Hanggi,“Perfusion CT in patients with spontaneous lobar intracerebral hemor-rhage: Effect of surgery on perihemorrhagic perfusion,” Stroke, vol. 43,pp. 759–763, 2012.
[7] L. Elijovich, P. V. Patel, and J. C. Hemphill III, “Intracerebralhemorrhage.” in Seminars in neurology, vol. 28, no. 5, 2008, pp. 657–667.
[8] L. M. Auer, W. Deinsberger, K. Niederkorn, G. Gell, R. Kleinert,G. Schneider, P. Holzer, G. Bone, M. Mokry, E. Korner, G. Kleinert,and S. Hanusch, “Endoscopic surgery versus medical treatment forspontaneous intracerebral hematoma: a randomized study,” Journal of
Neurosurgery, vol. 70, no. 4, pp. 530–535, 1989.
[9] T. M. Goradia, R. H. Taylor, and L. M. Auer, “Robot-assistedminimally invasive neurosurgical procedures: First experimental ex-perience,” in Lecture Notes in Computer Science, 1997, pp. 319–322.
[10] J. Burgner, P. J. Swaney, R. A. Lathrop, K. D. Weaver, and R. J.Webster III, “Debulking from within: A robotic steerable cannulafor intracerebral hemorrhage evacuation,” IEEE Trans. on Biomedical
Engineering, vol. 60, pp. 2567–2575, 2013.
[11] E. Ayvali, C.-P. Liang, M. Ho, Y. Chen, and J. P. Desai, “Towardsa discretely actuated steerable cannula for diagnostic and therapeuticprocedures,” The Int. Journal of Robotics Research, vol. 31, no. 5, pp.588–603, 2012.
[12] D. F. Louw, T. Fielding, P. B. McBeth, D. Gregoris, P. Newhook,and G. R. Sutherland, “Surgical robotics: a review and neurosurgicalprototype development.” Neurosurgery, vol. 54, no. 3, pp. 525–36;discussion 536–7, 2004.
[13] R. Taylor, “A Perspective on Medical Robotics,” Proceedings of the
IEEE, vol. 94, no. 9, pp. 1652–1664, 2006.
[14] G. Dogangil, B. L. Davies, and F. Rodriguez y Baena, “A review ofmedical robotics for minimally invasive soft tissue surgery,” Procs. of
the Institution of Mechanical Engineers, Part H: Journal of Engineer-
ing in Medicine, vol. 224, no. 5, pp. 653–679, 2010.
[15] J. A. Engh, G. Podnar, D. Kondziolka, and C. N. Riviere, “Towardeffective needle steering in brain tissue.” Annual Int. Conf. of the
IEEE Engineering in Medicine and Biology Society, vol. 1, pp. 559–62, 2006.
[16] R. J. Webster III, J. S. Kim, N. J. Cowan, G. S. Chirikjian, and A. M.Okamura, “Nonholonomic Modeling of Needle Steering,” Int. Journal
of Robotics Research, vol. 25, no. 5/6, pp. 509–526, 2006.
[17] D. B. Comber, E. J. Barth, and R. J. Webster III, “Design and Controlof an Magnetic Resonance Compatible Precision Pneumatic Active
Cannula Robot,” ASME Journal of Medical Devices, vol. 8, no. 1, p.011003, 2014.
[18] J. Burgner, D. C. Rucker, H. B. Gilbert, P. J. Swaney, P. T. RussellIII, K. D. Weaver, and R. J. Webster III, “A Telerobotic System forTransnasal Surgery,” IEEE/ASME Trans. on Mechatronics, vol. 19,no. 3, pp. 996–1006, 2014.
[19] E. Butler, R. Hammond-Oakley, S. Chawarski, A. Gosline, P. Codd,T. Anor, J. Madsen, P. Dupont, and J. Lock, “Robotic neuro-endoscopewith concentric tube augmentation,” in IEEE/RSJ Int. Conf. on Intel-
ligent Robots and Systems, 2012, pp. 2941–2946.[20] P. E. Dupont, J. Lock, B. Itkowitz, and E. Butler, “Design and Control
of Concentric-Tube Robots,” IEEE Trans. on Robotics, vol. 26, no. 2,pp. 209–225, 2010.
[21] D. C. Rucker, B. A. Jones, and R. J. Webster III, “A Geometrically Ex-act Model for Externally Loaded Concentric-Tube Continuum Robots,”IEEE Tran. on Robotics, vol. 26, no. 5, pp. 769–780, 2010.
[22] L. A. Lyons, R. J. Webster III, and R. Alterovitz, “Motion Planningfor Active Cannulas,” in IEEE/RSJ Int. Conf. on Intelligent Robots
and Systems, 2009, pp. 801–806.[23] L. Torres and R. Alterovitz, “Motion planning for concentric tube
robots using mechanics-based models,” in IEEE/RSJ Int. Conf. on
Intelligent Robots and Systems, 2011, pp. 5153–5159.[24] C. Bergeles and P. Dupont, “Planning stable paths for concentric tube
robots,” in IEEE/RSJ Int. Conf. on Intelligent Robots and Systems,2013, pp. 3077–3082.
[25] J. Burgner-Kahrs, H. B. Gilbert, J. Granna, P. J. Swaney, andR. J. W. III, “Workspace characterization for concentric tube contin-uum robots,” in IEEE/RSJ Int. Conf. on Intelligent Robots and Systems,2014, pp. 1269–1275.
[26] S. Xu, G. Fichtinger, R. H. Taylor, and K. R. Cleary, “3d motion track-ing of pulmonary lesions using ct fluoroscopy images for roboticallyassisted lung biopsy,” in Medical Imaging. Int. Society for Opticsand Photonics, 2004, pp. 394–402.
[27] S. M. Atay, C. D. Kroenke, A. Sabet, and P. V. Bayly, “Measurement ofthe dynamic shear modulus of mouse brain tissue in vivo by magneticresonance elastography,” Journal of Biomechanical Engineering, vol.130, no. 2, p. 021013, 2008.
[28] S. Pieper, M. Halle, and R. Kikinis, “3D Slicer,” in IEEE Int. Symp.
on Biomedical Imaging: Nano to Macro, 2004, pp. 632–635.[29] Y. Guo, J. Granna, K. Weaver, R. W. III, and J. Burgner-Kahrs,
“Comparison of optimization algorithms for a tubular aspiration robotfor maximum coverage in intracerebral hemorrhage evacuation,” inThe Hamyln Symposium on Medical Robotics, 2015, pp. 11–12.
[30] M. Miga, K. D. Paulsen, P. J. Hoopes, F. E. Kennedy Jr, A. Hartov,D. W. Roberts et al., “In vivo quantification of a homogeneous braindeformation model for updating preoperative images during surgery,”IEEE Trans. on Biomedical Engineering, vol. 47, no. 2, pp. 266–273,2000.
[31] S. A. Ahmadi, A. Plate, M. Schuberth, F. Milletari, N. Navab,and K. Botzel, “P116. DBS electrode imaging using 3d transcranialultrasound–a feasibility study with first quantitative results,” Clinical
Neurophysiology, vol. 126, no. 8, pp. e106–e107, 2015.[32] G. Unsgaard, A. Gronningsaeter, S. Ommedal, and T. A. N. Hernes,
“Brain operations guided by real-time two-dimensional ultrasound:new possibilities as a result of improved image quality,” Neurosurgery,vol. 51, no. 2, pp. 402–412, 2002.
1452