riskreporter - Church Mutual Insurance Company · kitchen manager and chef at Franklin Apartments...
Transcript of riskreporter - Church Mutual Insurance Company · kitchen manager and chef at Franklin Apartments...
Vol . 7issue 4
Winter2007
senior livingA quarter ly publicat ion by Church Mutual Insurance Co m p a n y
risk reporterin
side
Dealing with food in resident rooms
Identifying foodborne illnesses
The right glove for the job
Recognize, eliminatefoodborne illnesses In recent months, food safety calamities have made the headlines with frightening regularity.• Thousands of people have been struck with the norovirus
everywhere from group living environments to cruise ships• E. coli outbreaks from September to December caused
hundreds of illnesses and three deaths• A tomato-linked salmonella outbreak in fall 2006 felled
400 people.
The Centers for Disease Control and Prevention (CDC) estimatesthat approximately 76 million people get sick each year fromfoodborne illnesses, causing 300,000 hospitalizations and 5,000 deaths. These estimates are much higher than reportedoutbreak numbers would suggest because the gastroenterologicalproblems caused by foodborne illnesses are often mistaken forthose of other conditions, for example, flu-like symptoms.Nausea and vomiting may be signs of everything from stress tomedication allergies to a head injury, brain damage or congestiveheart failure; diarrhea can be the result of allergies, chronicbowel disorders or medications.
The primary causes of foodborne illnesses are bacteria, virusesand parasites. Of these, 55 percent of reported illnesses whoseetiology could be determined were caused by bacterialpathogens, an especially troubling fact for the elderly.
“The effects of aging and medications can compromise a person’simmune system and their ability to fight pathogens,” saidCarleen Russell, a nutritionist with the Iowa Department ofElder Affairs. “This is especially true with bacterial pathogensbecause many elderly are taking antacids or using proton pumpinhibitors, which lower stomach acids—the body’s naturaldefense against bacteria.”
The best strategy for an assisted living facility to minimize theincidence of foodborne illnesses is to stress the importance ofcreating a culture of food safety.
“Food safety requires a committed, long-term approach,” saidCatherine Strohbehn, adjunct associate professor with the Hotel,Restaurant and Institution Management Department at Iowa
(See foodborne illness, page 2)
PAGE 2 Recognize, eliminate foodborne illnesses winter 2007
ResourcesIowa State has created a wealth oftraining materials and food safetybackground information. Visit theirsite at www.iowahaccp.iastate.edu.
Other good resources include:www.cdc.govwww.fda.gov
The National RestaurantAssociation’s ServSafe program:www.nraef.org/servsafe
(foodborne illness)State University. “Administratorsmust hire employees who have theright attitude about food safety, becommitted to monitoring andprovide the financial resourcesto support their commitment.You can’t tell your employeesthat it’s important to wash theirhands and then gripe if theyuse too much soap.”
Written procedures“Written policies provide theframework for your food serv-ice program and help to showthat your organization hastaken reasonable care to pro-tect the safety of your food,your residents and your staff,”Strohbehn said.
Policies should cover safe food handling, cleaning standards andhealth situations that would preclude employees from workingwith food.
Food safety documentation shouldalso be included in your policies.
“Record every step of your foodproduction process from where itcame from and how it’s stored to thetemperature that food was servedat,” Strohbehn said.
Mom was right“Properly washing one’s hands isthe single most important step thatpeople can take for disease control,and the practice must be stressed,”Strohbehn said.
Hang posters that remind employ-ees to wash their hands and list thesteps required to do it correctly.Strohbehn also likes to see sinksthat are free from clutter andinclude all needed supplies close athand: hot and cold water, soap andpaper towels.
“Our staff understands that eventhe cleanest person is exposed to—and can transmit—a variety ofmicroorganisms,” said Mike Brown,administrator at the Crystal Creekfacility in Canton, Mich.
Gel sanitizers are increasingly pop-ular, but don’t expect them to takethe place of thorough hand washing.
“It’s great to see them in a hallwaywhere people can use them to kill
germs on elevator buttons and door-knobs, but they’re not typically agood choice during food prep,”Russell said. “If you have foodresidue on your hands, the gel can’tsanitize through that.”
Follow the “4 Cs”The Food and Drug Administration(FDA) recommends a four-stepapproach to food safety.
• Clean (and sanitize)“Cleaning means it looks good; sanitizing means you’ve removedgerms and pathogens,” Strohbehn said. Employees must have the right tools and cleaning agents for the job. All utensils and dishes should be sanitized
either with a high-temperature wash (typically 165-180 F) or a chemical, usually chlorine or a cleaning compound. Food prep surfaces can be sanitized with a solution of one teaspoon chlorine
bleach per quart of water.
• SeparateKeep raw meats, poultry and seafood away from otherfoods, especially foods that will be served without cool-ing, and use different cutting boards when preparing these items. Cutting boards are available in a wide variety of colors and can be color-coded to use.
These foods also need to be separated during storage.
“Meat should be stored on the bottom shelf of the refrigerator with a tray under it to catch any drips,” said Clarissa Toy, kitchen manager and chef with Franklin Apartments in Southfield, Mich.
• CookUse a thermometer to determine that food is cooked to the appropriate temperature and held there during serving. Don’t forget to check the accuracy of thermometers on a regular basis. There are numerous Web sites that provide instructions for calibrating thermometers. Just
For more informationHazard Analysis and Critical ControlPoint (HACCP) is a food safety programcreated by the FDA. It’s currentlyrequired in many food processingestablishments, and a recent studysponsored by the U.S. Department ofAgriculture examined the possibility ofapplying it to the assisted living envi-ronment. To learn more about the study,go to www.fsis.usda.gov/PDF/Slides_092906_Jsneed.pdf.
Labeling food storage containers is a good way to ensurethat food does not remain in the refrigerator too long.
(See foodborne illness, page 4)
PAGE 3
Being able to choose what to eat andwhen are two of life’s simple pleas-ures. But when food is improperlystored in resident rooms, it can lead toproblems with illness and pest infestations.
IllnessAn assessment of your facility’s residents should drive policy regarding food in rooms, and thesepolicies should be shared at the timeof admission. Limited physical acuityand cognitive abilities can impair aresident’s capacity to handle, store,clean or even determine if a food issafe to eat.
“Many of our residents suffer fromAlzheimer’s, so there are no cookingfacilities in their rooms—just a smallrefrigerator,” said Mike Brown, admin-istrator at the Crystal Creek facility inCanton, Mich. “We discourage themfrom taking food back to their rooms.”
To avoid health-related problems,
have staff do periodic checks of refrigerators and cabinets and alsoinvolve family members and residentsin this process.
“If a resident requests a meal in theirroom, it’s dated, and housekeepingchecks later that day to see if the foodhas been eaten,” said Clarissa Toy,kitchen manager and chef at FranklinApartments in Southfield, Mich. “If ithasn’t, we remove it and throw it away,and our staff will also remove anyother questionable food items.”
Pest infestationsAccording to Zia Sidiqqi, director ofquality assurance for commercial services at Orkin, pests need fourthings to thrive: access, water, shelterand food. Eliminate these and pestsare less likely to be a problem.
AccessExclusion is critical. Have mainte-nance look at points of entry. Repairscreens and seal around pipes coming
into the building and at any cracks atwall/floor junctures. It’s also importantto limit doorway access. “If I’m insidea closed building, I shouldn’t be ableto see any daylight around the edgesof the doors,” Sidiqqi said.
During move-in, examine residents’items—including plants—for anysigns of bug infestations.
ShelterEliminate rodent hiding places. Thisincludes bushes and yard debris outside and empty boxes, bottles,bags, newspapers and cans inside.
FoodProper storage is critical. All fooditems should be kept in tightly closedcontainers, spills and crumbs shouldbe cleaned up immediately—toastersand toaster ovens can be in-room cul-prits—and all surfaces should be keptclean of food debris.
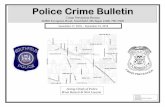
Dealing with food in resident rooms
the knitting technology allows for abigger range of glove sizes.”Gloves are typically made with a mixof fibers—for example, Kevlar and apoly/cotton blend; Dyneema is oftenmixed with Lycra for flexibility.
“The higher the level of non-Kevlar/Dyneema fibers, the morecomfortable and flexible the glove—but the less protection it offers,”Muehlenkamp said.
for meat handling,” said BrianMuehlenkamp, product manager forConney Safety, a safety products distributor in Madison, Wis.“Kevlar is cut-resistant if you’re using a straight-edged knife, but itwon’t help with a serrated knife or if aknife point is poked directly into theglove fabric.”
Dyneema is more cut-resistant thanKevlar and also stands up to chemicals better—though it is moreexpensive. Kevlar gloves typically run $4-$15 per pair, and Dyneema glovescost about $5-$20 per pair.
“You can bleach Dyneema, which isimportant for sanitizing, and it wearsbetter than Kevlar—you’ll be able toget four to five washings out of aDyneema glove,” said Kim Hosey, thehand protection products specialist atNorth Safety Products. “You can oftenget a better fit with Dyneema because
When properly selected and used,kitchen gloves can help protect stafffrom injury and residents from illness.There’s no one glove that will effec-tively meet all needs, so be prepared to provide your staff with avariety of options and consider enlisting the help of a glove expertfrom a local safety supply resource.The breadth of choices and pricepoints is nothing short of astonishing.
For food handling, employees shouldwear gloves at all times. Latex, vinyl,nitrile and chloroprene are commonchoices and offer varying degrees ofprotection, durability and punctureresistance.
To reduce cutting risks, gloves madeof Kevlar and Dyneema are goodoptions.
“The most cut-resistant gloves aremade of metal mesh, but these limitdexterity and are typically only used
Selecting the right glove for the job
The use of a puncture-resistant glove helps reduce the risk of cuts to kitchen staff.
Win
ter
07 CChhuurrcchh MMuuttuuaall IInnssuurraannccee CCoommppaannyy wwwwww..cchhuurrcchhmmuuttuuaall..ccoomm
3000 Schuster Lane P.O. Box 357 Merrill, WI 54452-0357
EEddiittoorr:: Rick Schaber (800) 554-2642 Ext. 4587 [email protected]
Is it a foodborne illness?It isn’t always easy to identify a foodborne illness, especially if the affected personhas chronic gastroenterological problems such as nausea or diarrhea, anddiagnosis is made more difficult by the fact that the incubation period can beanywhere from hours to weeks. If multiple people suffer similar symptoms afterconsuming the same food, this may indicate a foodborne illness, though the onlyway to tell definitively is by analyzing stool samples.
As per CDC recommendations, the resident’s physician should be contacted if the resident exhibits any of the following signs/symptoms:• High fever (temperature over 101.5 F, measured orally)• Blood in stools• Prolonged vomiting that prevents keeping liquids down• Signs of dehydration—decrease in urination, dry mouth and throat, dizzy
feeling when standing up• Diarrheal illness that lasts more than three days
Stool cultures are recommended if a resident is:• Immunocompromised• Febrile• Has bloody diarrhea, severe abdominal pain or clinically severe/persistent
illness
Recommended treatment will often include the following:• Rehydration • Use of products to limit the duration and severity of simple
diarrhea (these medications should be avoided if there is high fever or blood in the stool because they may make the illness worse)
staff should not report to work. Goodhand washing remains critical—forresidents and staff—and staff who areworking with ill residents should alsowear protective clothing—gloves, facemasks and eye protection and a labcoat that is removed and launderedafter dealing with the ill resident.
Train, train, trainAnyone who will be in contact withfood should receive thorough, ongoingtraining about food safety, and it’s alsoa good idea to share general food safetyinformation with all facility staff.
“We benefit from having as manyknowledgeable people on staff as
use your favorite search engine and type in “calibrating
thermometers.”
• ChillIt’s critical to store/serve foods at temperatures below 41 F or above 140 F. If food has been between these two temperatures for two hours or one hour at 90 F, do not serve it.
When bringing foods from a hot temperature to cool, do so as quickly as possible. Never put a large container of hot food in the refrigerator—it won’t cool quickly enough.
Don’t fill the refrigerator too full: cold air must be able to circulate tochill effectively. Defrost foods in the refrigerator—never on a kitchencounter—and ensure temperature accuracy with both external and internal thermometers that are checked regularly. Label foods so that they don’t remain in the refrig-erator too long: cooling slows down but doesn’t completely stop the growth of bacteria.
Limit kitchen access “Only kitchen staff is allowed in ourkitchen; everyone else needs to standat the doorway, and we’ll bring themwhatever they need,” Toy said. “Andwe have strict policies about whereyou put on protective items. Hairnetsgo on outside the kitchen; aprons assoon as you walk in.”
In the age of universal workers, havinga designated kitchen staff isn’t alwayspossible. In these instances, makesure that any staff members who comeinto the kitchen wear hairnets, washtheir hands and understand properfood handling techniques.
If an illness does occur, ill residentsshould remain in their rooms, and ill
possible—they can help us to seefood-related problems that we’re notexposed to,” Toy said. “During ourweekly manager meetings, I have thechance to share food safety updates,and the managers take this informationback to their staff.”
Strohbehn said it’s important that yourstaff understands why things need tobe done a certain way.
“If people understand the sciencebehind a policy/procedure, they’remore likely to follow it,” she said.“Create a culture where people takeresponsibility.”
(foodborne illness)