Rheumatic Fever Guideline 1(2)
-
Upload
ahmad-badrul-amin -
Category
Documents
-
view
21 -
download
2
description
Transcript of Rheumatic Fever Guideline 1(2)
-
Evi
den
ce-b
ased
, b
est
pra
ctic
e N
ew Z
eala
nd G
uid
elin
es f
or
Rh
eum
atic
Fev
er for[ Guidelines ]
Rheumatic Fever
New Zealand
Evidence-based, best practice Guidelines on:
1. Diagnosis, Management and Secondary Prevention
2. Sore Throat Management
3. Proposed Rheumatic Fever
Primary Prevention Programme
1. Diagnosis, Management and Secondary Prevention
NHF0239 80pp Cover 4C.indd 2 21/6/06 12:12:39
-
Endorsed by:
NHF0239 80pp Cover 4C.indd 3-4NHF0239 80pp Cover 4C.indd 3-4 21/6/06 12:34:5821/6/06 12:34:58
-
Table of Contents
1. Scope and Purpose of Guideline 5
2. About the Guideline 5
Disclaimer 5
Outlineofgradingmethodologyused 6
Endorsingorganisations 6
Organisationsconsulted 6
NewZealandguidelines:Writinggroup 7
Otherreviewersandcontributors 8
Secreteriatsupport 8
3. Introduction 9
Keypoints 9
Pathogenesis 9
Epidemiology 9
CosttoNewZealand 11
Populationprojections 11
PreventionofARFandRHD 11
DIAGNOSIS AND MANAGEMENT 13
4. Diagnosis of Acute Rheumatic Fever 14
Importanceofaccuratediagnosis 14
Currentapproachestodiagnosis 14
Clinicalfeaturesofacuterheumaticfever-majormanifestations 16
Clinicalfeaturesofacuterheumaticfever-minormanifestations 18
EvidenceofaprecedinggroupAstreptococcalinfection 19
Otherlesscommonclinicalfeatures 19
Echocardiography 19
Differentialdiagnosis 22
Investigations 23
5. Management of ARF 24
Observationandgeneralhospitalcare 28
Discharge 29
SECONDARY PREVENTION 31
6. Prophylaxis Regimes 32
Penicillin 32
Dose 32
Frequency 32
Secondaryprophylaxiswhilebreastfeeding,inpregnancyandwhileonoralcontraceptives 33
Secondaryprophylaxisinanti-coagulatedcases 34
7. Duration of Secondary Prophylaxis 34
8. Protocol for Secondary Prophylaxis Delivery 36
9. Anaphylaxis 37
10.Improving Adherence to Secondary Prophylaxis 37
ReducingthepainofBPGinjections 37
Education 38
ARFRegisters 38
KeydataelementsofARF/RHDregisters 40
Outreachandout-of-town 42
Non-compliance 42
11. Routine Review and Structured Care Planning 43
NHF0239 80pp Inside.indd 2 21/6/06 12:11:52
-
1Evidence-based, best practice New Zealand Guidelines for Rheumatic Fever
1. DIAGNOSIS, MANAGEMENT AND SECONDARY PREVENTION
He korokoro ora he manawa ora,Mo tatou katoa
( A healthy throat, a healthy heart for us all)
JUNE 2006
NHF0239 80pp Inside.indd 1NHF0239 80pp Inside.indd 1 3/7/06 11:13:263/7/06 11:13:26Process CyanProcess CyanProcess MagentaProcess MagentaProcess YellowProcess YellowProcess BlackProcess BlackPANTONE 186 CVCPANTONE 186 CVC
-
312. Prevention of Infective Endocarditis 44
13. Case Finding: Surveillance and Screening 44
Surveillance 44
Screeningforrheumaticheartdisease 45
Suggestedindicatorsforevaluation 46
14. Implementation 47
15. Algorithms 50
Algorithm1.GuideforthediagnosisofARF 50
Algorithm2.GuidefortheuseofechocardiographyinARF 52
Algorithm3.Guideforthedurationofsecondaryprophylaxis 53
16. References 54
17. Appendices 63
AppendixA:Guidelinedevelopmentprocess 63
AppendixB:JonescriteriaforthediagnosisofARF 64
AppendixC:UseofechocardiographyinARF 66
AppendixD:MedicationsusedinARF 68
AppendixE:Comparisonofintramuscularpenicillinandoralpenicillinforsecondaryprevention 70
AppendixF:Anaphylaxisrecognitionandmanagement 71
AppendixG:Protocolforfollow-upofnon-compliantcases 72
AppendixH:Walletcardforinfectiveendocarditisprevention 73
18. Glossary 74
19. Notes 75
NHF0239 80pp Inside.indd 3 21/6/06 12:11:53
-
List of Tables
Table1. Levelsofevidenceforclinicalinterventionsandgradesofrecommendation 6
Table2. NewZealandguidelinesforthediagnosisofARF 15
Table3. MajormanifestationsofARF 16
Table4. MinormanifestationsofARF 18
Table5. UpperlimitsofnormalforserumstreptococcalantibodytitresusedinNewZealandforARFdiagnosis 19
Table6. Minimalechocardiographiccriteriatoallowadiagnosisofpathologicalvalvularregurgitation 20
Table7. SeverityofARFcarditis 21
Table8. DifferentialdiagnosesofcommonmajormanifestationsofARF 22
Table9. InvestigationsinsuspectedARF 23
Table10. Prioritiesinmanagingacuterheumaticfever 24
Table11. Guidelinesforgeneralin-hospitalcare 28
Table12. Recommendedantibioticregimensforsecondarypreventionofacuterheumaticfever/rheumaticheartdisease 33
Table13. NewZealandrecommendationsforthedurationofsecondaryprophylaxis 34
Table14. Suggestedprotocolforthedeliveryofsecondaryprophylaxisbycommunitynurses 36
Table15. MeasuresthatmayreducethepainofbenzathinepenicillinGinjections 37
Table16. PrimaryaimsofARFregistersystems 39
Table17. Recommendedelementsofregister-basedcontrolprogramme 39
Table18. Datasetforacuterheumaticfeverregister 40
Table19. RecommendedroutinereviewandmanagementplanforARFandRHD 43
Table20. RecommendedelementsofascreeningprogrammeinNewZealand 45
Table21. ProposedindicatorsforevaluatingARF/RHDcontrolprogrammes 46
Table22. UsesofechocardiographyinARF 66
Table23. DiagnosticandclinicalutilityofsubclinicalrheumaticvalvedamageinARF 67
Table24. MedicationsusedinARF 68
Table25. Recommendeddoseofadrenalineinanaphylaxis 71
NHF0239 80pp Inside.indd 4 21/6/06 12:11:53
-
5[1. Scope and Purpose of Guideline]
[2. About the Guideline]
ThisguidelinehasbeendevelopedbyTheNationalHeartFoundationofNewZealandand theCardiacSocietyofAustraliaandNew Zealand. This guideline will be complemented by further guidelines on appropriate sore throat management and primarypreventionofacuterheumaticfever(ARF).
Theobjectivesofthisguidelineare:
toidentifyandpresenttheevidenceforbestpracticeinARFdiagnosis
toidentifythestandardofcarethatshouldbeavailabletoallpeopleinNewZealand
toidentifyareaswherecurrentmanagementstrategiesmaynotbeinlinewithavailableevidence
toensurethathigh-riskpopulationsreceivethesamestandardofcareasthatavailabletoother NewZealanders.
Thisguidelinewasdevelopedbyawritinggroupcomprisedofexpertsinrheumaticfever.SelectedindividualswithexperienceinARFandrelevantstakeholderswerealsoinvolved.Theseincludedarangeofgeneralandspecialistclinicians,alliedhealthprofessionals,Ma-oriandPacificprofessionals,andlayrepresentativegroups.
ThisguidelinehasbeenproducedforNewZealandandisendorsedbyNewZealandorganisations.
ThechairsoftheguidelinewritingcommitteewereinvolvedinthedevelopmentofasimilardocumentfortheAustralianpopulation,withtheunderstandingthattheAustralianguidelineswouldbeadaptedfortheNewZealandsetting.WearegratefulforthecontributionofourAustraliancolleagues.
ThedevelopmentprocessisdescribedinAppendixA.
Disclaimer ThisdocumenthasbeenproducedbyTheNationalHeartFoundationofNewZealandand theCardiacSocietyofAustraliaandNewZealand forhealthprofessionals.Thestatementsandrecommendations itcontainsare,unless labelledasexpertopinion,basedonindependentreviewoftheavailableevidence.Interpretationofthisdocumentbythosewithoutappropriatehealthtrainingisnotrecommended,otherthanattherequestof,orinconsultationwith,arelevanthealthprofessional.
Inaddition,therecommendationsinthisguidelinearenotintendedtoreplaceclinicaljudgmentofeachindividualcase.Treatmentshould take into account comorbidities, drug tolerance, lifestyle, living circumstances, cultural sensibilities and wishes. Whenprescribingmedication, clinicians shouldobserveusual contra-indications,bemindful ofpotential adversedrug interactionsandallergies,monitorresponsesandensureregularreview.
NHF0239 80pp Inside.indd 5 21/6/06 12:11:53
-
Endorsing organisations TheCardiacSocietyofAustraliaandNewZealand
TheNationalHeartFoundationofNewZealand,alongwith:
TeHotuManawaMa-ori
PacificIslandsHeartbeat
PaediatricSocietyofNewZealand
TheRheumaticFeverTrust.
Organisations consulted AustralasianSocietyforInfectiousDiseases
AustralasianFacultyofPublicHealthMedicine
NationalHeartFoundationofAustralia
NewZealandNursesOrganisation
NewZealandMinistryofHealth
PasifikaMedicalAssociationofNewZealand
RoyalAustralasianCollegeofPhysicians
TeOhuRataoAotearoa-Ma-oriMedicalPractitionersAssociation.
Richbodyofhigh-qualityRCTdata
LimitedbodyofRCTdataorhigh-qualitynon-RCTdata
Noevidenceavailablepanelconsensusjudgment
LEVEL OFEVIDENCE STuDY DESIGN GRADE OF RECOMMENDATION
I A
II B
III-I B
III-2 B
III-3 C
IV C
D/I
Table 1. Levels of Evidence for Clinical Interventions and Grades of Recommendation
Outline of grading methodology usedThereviewincludeslevelsofevidenceandaccompanyinggradesofrecommendation(Table1).
Evidenceobtainedfromasystematicreviewofallrelevantrandomisedcontrolledtrials(RCT)
Evidenceobtainedfromatleastoneproperlydesignedrandomisedcontrolledtrial
Evidenceobtainedfromwell-designedpseudo-randomisedcontrolledtrials(alternateallocation orsomeothermethod)
Evidenceobtainedfromcomparativestudieswith concurrentcontrolsandallocationnotrandomised(cohortstudies),case-controlstudies,orinterruptedtimeserieswithacontrolgroup
Evidenceobtainedfromcomparativestudieswithhistoricalcontrol,2ormoresingle-armstudies,orinterruptedtimeserieswithaparallelcontrolgroup
Evidenceobtainedfromcaseseries,eitherpost-testorpre-testandpost-test
Insufficientevidenceavailableexpertopinionor panelconsensusjudgment
Note: The levels of evidence and grades of recommendations are adapted from the National Heart Foundation of Australia Rheumatic Fever guidelines. (Details can be found at www.nhf.com.au)
NHF0239 80pp Inside.indd 6 21/6/06 12:11:53
-
7New Zealand guidelines: Writing group
Professor Diana Lennon (Co-chair)ProfessorofPopulationChild&YouthHealth,UniversityofAuckland
Dr Nigel Wilson (Co-chair)PaediatricCardiologist,StarshipChildrensHospital
Dr Polly Atatoa-CarrPublicHealthMedicineRegistrar
Dr Bruce ArrollAssociateProfessorofGeneralPractice,UniversityofAuckland
Ms Elizabeth FarrellPublicHealthNurse,CountiesManukauDistrictHealthBoard
Dr Jonathan JarmanMedicalOfficerofHealth,NorthlandDistrictHealthBoard
Dr Melissa KerdemelidisRheumaticFeverTrustResearchFellow
Mr Henare MasonProjectManager,CountiesManukauDistrictHealthBoard
Dr Johan MorreauPaediatrician,RotoruaHospital
Dr Ross NicholsonPaediatrician,KidzFirstHospital,MiddlemoreHospital
Dr Briar PeatSeniorLecturerinGeneralMedicine,UniversityofAuckland
Ms Heather SpinettoSpecialistCardiacNurse,StarshipChildrensHospital
Dr Lesley VossPaediatricianinInfectiousDiseases,StarshipChildrensHospital.
NHF0239 80pp Inside.indd 7 21/6/06 12:11:54
-
Other Reviewers and ContributorsDrRohanAmeratunga MsEricaAmon DrJeremyArmishaw MsCatherineAtkinson
DrAnitaBell DrCatherineBremner MsJosephineCottrell ProfessorBartCurrie
DrAlanFarrell DrTomGentles DrDavidGraham MsMichelleHooker
DrDavidJamison ProfessorEdwardKaplan DrAndrewKerr MsTraceyKunac
DrGraemeLear MsLindsayLowe MsMaoiteleLowen MrJohnKristiansen
DrChrisMansell DrFraserMaxwell DrMalcolmMcDonald DrMargotMcLean
MsAndreaMockford DrPhilipMoore DrChrisMoyes MsMarthaNgawaka
MsMaureenOHalloran DrTeuilaPercival DrNeilPoskitt MsKathyRennie
DrJanSinclair DrWarrenSmith MsReneeStreatfield DrRichardTalbot
DrCraigThornley MsLupeToilolo DrWendyWalker MsJoannaWilliams
DrElizabethWilson MsIsabelleTeokotaiWhite
AucklandDistrictNursingGroup.
Secretariat SupportMrsShaelynnSchaumkel.
Australian Guidelines Writing GroupDrAlexBrown;AssociateProfessorJonathanCarapetis(Chair);DrKeithEdwards;DrCliveHadfield;ProfessorDianaLennon;MsLynettePurton;DrAndrewTonkin;DrWarrenWalsh;DrGavinWheatonandDrNigelWilson.
Australian Guidelines reviewers and contributorsDrLeslieEBolitho;DrAndrewBoyden;DrChristianBrizard;DrRichardChard;MsEleanorClune;DrArthurCoverdale;DrSophieCouzos;ProfessorBartCurrie;DrJamesEdward;DrTomGentles;ProfessorMarciaGeorge;DrJefferyHanna;DrNoelHayman;DrAnaHerceg;DrMarcusIlton;DrJenniferJohns;DrJohnKnight;DrJohnMcBride;DrMalcolmMcDonald;DrJohanMorreau;DrMichaelNicholson;DrRossNicholson;MsSaraNoonan;DrBriarPeat;DrPeterPohlner;Dr JimRamsey;Dr JennyReath;MsEmmaRooney;DrWarrenSmith;DrLesleyVoss;DrMarkWenitong;MrChrisWilson;DrElizabethWilsonandDrKeithWollard.
DeclarationNoconflictsofinterestwereinvolvedinthedevelopmentofthisguideline.DrPollyAtatoa-CarrwhocoordinatedthewritingofthisguidelinewasfundedbyTheNationalHeartFoundationofNewZealandandtheAustralasianFacultyofPublicHealthMedicine.
NHF0239 80pp Inside.indd 8 21/6/06 12:11:54
-
9Key points
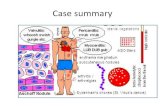
Acute rheumatic fever, an auto-immune response to group A streptococcus infection of the upper respiratory tract, may result in damage to the mitral and/or aortic valves and therefore rheumatic heart disease. Recurrences are likely in the absence of preventative measures and may cause further cardiac valve damage
Although acute rheumatic fever is rare in industrialised countries, it is a signi cant cause of disease among Ma-ori and Paci c children in New Zealand. The incidence of rheumatic heart disease is also high among these populations, with signi cant rates of procedures and death among young adults
Appropriate treatment of sore throats in high risk populations will eliminate group A streptococcus in most cases, and prevent individual cases of acute rheumatic fever
Prevention of recurrences, and therefore rheumatic heart disease prevention, with intramuscular penicillin is both effective and highly cost-effective.
Acuterheumaticfever(ARF)isanauto-immuneconsequenceofinfectionwiththebacteriumgroupAstreptococcus(GAS).Itcausesanacutegeneralisedinflammatoryresponseandanillnessthataffectsonlycertainpartsofthebody,mainlytheheart,joints,brainandskin.IndividualswithARFareoftenseverelyunwell,ingreatpainandrequirehospitalisation.Despitethedramaticnatureoftheacuteepisode,ARFleavesnolastingdamagetothebrain,jointsorskin.1
However, thedamage to theheart,ormorespecifically themitraland/oraorticvalves,may remainonce theacuteepisodehasresolved.Thisisknownasrheumaticheartdisease(RHD).PeoplewhohavehadARFpreviouslyaremuchmorelikelythanthewidercommunitytohavesubsequentepisodes.2TheserecurrencesofARFmaycausefurthercardiacvalvedamage.HenceRHDsteadilyworsensinpeoplewhohavemultipleepisodesofARF.
Becauseofitshighprevalenceindevelopingcountries,RHDisthemostcommonformofpaediatricheartdiseaseintheworld.Inmanycountriesitisthemostcommoncauseofcardiacmortalityinchildrenandadultsagedlessthan40years.3
PathogenesisARFhasbeenshown todevelop inapproximatelyone to threepercentof those inanepidemicsituationofuntreatedexudativepharyngitisand/oraculturepositiveforGAS.Despitethehighincidenceinsomeethnicgroups(suchasMa-oriandPacificpeopleinNewZealand),ageneticpredispositiontoARFremainsunproven.1SomestrainsofGAShavebeenrepeatedlyidentifiedascausativeinARF (and therefore labelledrheumatogenic)andother rheumatogenicstrainscontinue toappear. The roleofskin infectionsremainsuncertain.4,5
FollowingGASinfection,thereisalatentperiodaveragingthreeweeksbeforethesymptomsofARFbegin.Bythetimethesymptomsdevelop,theinfectingstrainofGAShasusuallybeeneradicatedbythehostimmuneresponse.
EpidemiologyTheburdenofARFin industrialisedcountriesdeclineddramaticallyduringthe20thCentury,duemainlyto improvements in livingstandards(andhencereducedtransmissionofGAS)andbetteravailabilityofmedicalcare.6,7InmostaffluentpopulationsARFisnowrare.RHDisalsorareinyoungerpeopleinindustrialisedcountries,althoughitisstillseeninsomeelderlypatients,alegacyofARFhalfacenturyearlier.
Bycontrast,ARFandRHDremaincommoninmanydevelopingcountries. ArecentreviewoftheglobalburdenofGAS-relateddiseaseestimatedthatthereisaminimumof15.6millionpeoplewithRHD,another1.9millionwithahistoryofARFbutnocarditiswhostillrequirepreventivetreatment,470,000newcasesofARFeachyearandover230,000deathsduetoRHDannually.8Almostallcasesanddeathsoccurindevelopingcountries.Thesefiguresarealllikelytobeunderestimatesofthetrueburdenofthedisease.
[3. Introduction]Key points
Acute rheumatic fever, an auto-immune response to group A streptococcus infection of the upper respiratory tract, may result in damage to the mitral and/or aortic valves and therefore rheumatic heart disease. Recurrences are likely in the absence of preventative measures and may cause further cardiac valve damage
Although acute rheumatic fever is rare in industrialised countries, it is a signi cant cause of disease among Ma-ori and Paci c children in New Zealand. The incidence of rheumatic heart disease is also high among these populations, with signi cant rates of procedures and death among young adults
Appropriate treatment of sore throats in high risk populations will eliminate group A streptococcus in most cases, and prevent individual cases of acute rheumatic fever
Prevention of recurrences, and therefore rheumatic heart disease prevention, with intramuscular penicillin is both effective and highly cost-effective.
NHF0239 80pp Inside.indd 9 21/6/06 12:11:54
-
10
ThereissubstantialregionalvariationintheburdenofARFandRHD.ThehighestdocumentedratesintheworldhavebeenfoundinMa-oriandPacificpeopleinNewZealand,AboriginalAustraliansandthoseinPacificIslandnations.9,10,11TheprevalenceofRHDisalsohighinSub-SaharanAfrica,LatinAmerica,theIndiansubcontinent,theMiddleEastandNorthernAfrica.8
NewZealandhashadsustainedhighratesofARFandRHDformanydecadeswithRHDbeingasignificantcauseofprematuredeathinthiscountry.12,13,14AnumberofsurveysofARFandRHDincidencehavebeenconductedsincetheearly1900sinNewZealand.Inthe1920s,surveysofschoolrecordsinNewZealanddeterminedanapproximateannualtotalpopulationincidenceofARFof65per100,000.9From1956to1973,theWairoaCollegeStudydeterminedthatthedeclineinincidenceofARFseeninotherdevelopedcountries was not evident in New Zealand and those pockets of the country which experienced isolation and socio-economicdeprivationhadsignificantlyhigherratesofbothARFandRHD.15
From 1995 to 2000, around 100 cases of ARFwere notified annually inNewZealand,with an incidence of 13.8 per 100,000populationin5to14yearolds.14From1993to1999,theAucklandRegisterrecordedanincidenceof21.9per100,000populationin5to14yearolds.Aucklandaccountsfor60%oftheactivecasesonNewZealandregisters.16,17
ARFispredominantlyadiseaseofchildrenagedbetween5to14years,withapeakataroundeightyears.ItisraretodiagnoseARFundertheageofthree(beforefullmaturationoftheimmunesystem).18,19AsRHDrepresentsthecumulativeheartdamageofpreviousARFepisodes,theprevalenceofRHDpeaksinthethirdandfourthdecadesoflife.20,21Therefore,althoughARFisadiseasewithitsrootsinchildhood,itseffectsarefeltthroughoutadulthood,especiallyintheyoungadultyearswhenpeoplemightotherwisebeattheirmostproductive.
The disparity of ethnicity in rheumatic fever populations has been described in many world centers where population groupsexperiencinglowsocio-economicstatusandlivinginovercrowdedsituationspresentwithahighincidenceofARF.19InNewZealand,Ma-oriandPacificpeopleshavethehighestburdenofbothARFandRHD.Despitethesignificantissuesregardingtheaccuracyofethnicitydatainpastmorbidityandmortalitystatistics,theratesofARFinMa-orihavealwaysbeenreportedassignificantlygreaterthanthoseseeninnon-Ma-ori.Forexample,from1949to1953thereportedincidenceofARFinMa-orichildren(ratesofgreaterthan1000per100,000)was11timesthatofthenon-Ma-oripopulation.9Theage-specificannualnotificationratesforARFbetween1990to1995forchildrenaged10to14yearswas77.7per100,000forPacificchildren,30.4per100,000forMa-orichildrenand1per100,000forEuropeanchildren.14Aucklandalsodisplaysthispattern:theannualincidenceofARFin5to14yearoldMa-orichildrenfrom1993to1999was41.2per100,000population,Pacificchildren83.7per100,000population/yearandtherestofthepopulation1.4per100,000population/year.21Dependingontheyearanalysed,thePacifichospitalisationratesareatleastninetimesthatofEuropeans/others.TheMa-orihospitalisationrateisjustoverfivetimesthatofEuropeans/others.23
Aswell ashigher ratesof initialARF incidence,Ma-ori andPacificpeoplealsohave thehighest ratesofARF recurrence. From1973to1982(priortotheintroductionofsystematicprophylaxisdelivery)recurrenceratesinMa-oriwere40%comparedto22%innon-Ma-ori.24AreviewofcasesintheAucklandrheumaticfeverregisterfrom1993to1999foundthatalthoughthetotalrecurrencerateshaddroppedsignificantlyfromthe1980s(22%to5.5%),alloftherecurrencesfoundwereinMa-oriandPacificpeople.16,17ItisthereforenotsurprisingthatMa-oriandPacificpeoplehavemuchhigherratesofcarditis,RHDandconsequentheartfailure,astheriskofthesecomplicationsincreaseswitheachattackofARF.
IthasnotbeenproventhatMa-oriandPacificpeoplehaveincreasedgeneticsusceptibilitytorheumaticfever.Itismorelikelythattheover-representationofthesesectorsofthepopulationreflectsacombinationofovercrowdedconditions,socio-economicdeprivation,anincreasedincidenceofupperrespiratoryinfectionswithGAS,anddifferenttreatmentoptionsoropportunitiesforappropriateandeffectivehealthcare.11,19,22
NHF0239 80pp Inside.indd 10 21/6/06 12:11:55
-
11
Cost to New ZealandThere are significant personal, community and national costs associatedwith ARF andRHD. These result from repeated andprolonged hospitalisation, the resources required formedical prophylaxis and treatment, surgical intervention, negative physicaland psychological experience, disruption of the lives of cases and their families and often premature death.25 In 1991, it wasestimatedthatthetotalcostofARFandRHDtotheAucklandhealthservicealonewas$3.6million,withchronicRHDaccountingfor71%ofthecosts.CostsinvolvedwerethedirectcostsofGPandoutpatientvisits,prescriptioncharges,travel,radiologyandthecostsofinformalcaregivenbyhouseholdmembers.20Inadditiontothesedirectcosts,thereareanumberofindirectcostsofARFandRHD,whichareoftendifficulttomeasure.Theseincludenotonlythelossofquantityoflife(ithasbeenestimatedthatfivetotenyoungpeopledieeachyearasadirectresultofARForRHD),butalsothelossofqualityoflife.Thisoccursthroughtimeawayfromeducationandoccupation,impactsonphysicaldevelopmentandfamilyrelationships,psychologicaleffectsandthelossofabilityforchildrenandyoungadultstorealisetheirfullpotential.12,20
Population projectionsCurrentlyMa-oriandPacificpeopleinNewZealandmakeupasizeablepercentageofthechildhoodpopulation.In2001,approximately37%ofMa-oriand40%ofPacificpeopleinNewZealandwereundertheageof15(comparedto23%European).ThemedianageofEuropeanswas36.8years,whilefortheMa-oriandPacificethnicgroupsthecomparablefigureswere21.9and21.0yearsrespectively.26It is reasonable topredict that theNewZealandpopulation in the futurewill representhighgrowthandasustainedyouthfulagestructureintheMa-oriandPacificpopulationswithmany(particularlychildren)livinginpoorsocio-economiccircumstance.26AllthesefeatureshavesignificantimplicationsforARFincidence,prevalenceandprevention.
Prevention of ARF and RHDPrimary prevention
In the future, a cost-effective vaccine for group A streptococcimay be the ideal solution for the primary prevention of ARF.27,28Scientificproblemshavesofarpreventedthedevelopmentofsuchavaccine,28andcurrentlypreventionofaninitialattackofARFrequiresthepromptandaccuratediagnosisandadequateantibiotictreatmentofGASthroatinfections.28,29,30ARFcanbepreventediftheprecedingthroatinfectionistreatedinatimelyandeffectiveway.3,31,32Recommendedtreatmentofstreptococcalthroatinfectionisintramuscular(IM)benzathinepenicillinoraten-daycourseoforalphenoxymethylpenicillin,bothofwhicheradicatethestreptococcifromthepharynx.Theoraltreatmentisoftenusedbecauseitissafe,inexpensiveandlesspainful.
Secondary prevention
Overthelast30yearsoneofthemajorsuccessesinARFmanagementhasbeenthemarkeddeclineinrecurrent(andoftendisabling)attacksofrheumaticfever,duetotheavailabilityofeffectiveantibioticsforsecondaryprophylaxis.32SecondarypreventionofARFisdefinedasthecontinuousadministrationofantibiotics(usuallyparenteralbenzathinepenicillinevery28days)tocaseswithpreviousARForwell-documentedRHD.28TheaimofsecondarypreventionistostoprecolonisationorreinfectionofthethroatwithgroupAstreptococciandtherebypreventingrecurrenceofARF.3TheriskofARFafterthefirstattackofgroupAstreptoccociisapproximately0.3-3%,butwithsubsequentinfectionthisriskrisesto25-75%.2Inaddition,thosewhosuffercarditisduringtheirinitialattackaresignificantlymorelikelytodevelopfurthercarditiswithsubsequentstreptococcalthroatinfections.33ThesystematicuseofregularantibioticprophylaxisinknownARFcaseshasbeenshowntoreducetheincidenceofrecurrentrheumaticfever,reducetheneedforhospitalisationandsurgery,decreasetherapidityandseverityofRHDandimprovequalityoflife.28,34Furthermore,nationalpreventionprogrammesbasedonsecondarypreventionhavethepotentialforconsiderablecostsavings,andhavebeenfoundtobeacost-effectivemethodofreducingmortalityandmorbidityfromARFinternationallyandinNewZealand.20,22,28,35
NHF0239 80pp Inside.indd 11 21/6/06 12:11:55
-
1
NHF0239 80pp Inside.indd 12 21/6/06 12:11:55
-
13
Diagnosis andManagement][
NHF0239 80pp Inside.indd 13 21/6/06 12:11:57
-
1
[4. Diagnosis of Acute Rheumatic Fever (ARF)]Importance of accurate diagnosisItisimportantthatanaccuratediagnosisofARFismadeas:
over-diagnosiswillresultintheindividualreceivingbenzathinepenicillinG(BPG)injectionsunnecessarily everyfourweeksforaminimumoftenyears
under-diagnosisofARFmayleadtotheindividualsufferingafurtherattackofARF,cardiacdamageand prematuredeath.
ThediagnosisofARFreliesonhealthprofessionalsbeingawareofthediagnosticfeatures,particularlywhenpresentationisdelayedoratypical.InAucklandforexample,between1993and1999,fourpatientsdiagnosedwithsepticarthritisbygeneralmedicineandorthopaedicphysicians,subsequentlydevelopedacuterheumaticfever.16,17
Currently,thereisnolaboratorytestdiagnosticforARF,sodiagnosisremainsaclinicaldecision.Thepre-testprobabilityfordiagnosisofARFvariesaccordingtolocationandethnicity.Forexample,inaregionwithhighincidenceofARF(suchastheNorthernhalfoftheNorthIsland),apersonwithfeverandarthritisismorelikelytohaveARFthanoneinalowincidenceregion(suchastheSouthIsland).Ma-oriandPacificpeoplearealsomorelikelythannon-Ma-oriandPacificpeopletohaveARF.
Current approaches to diagnosisTheJonescriteriaforthediagnosisofARFwereintroducedin1944.36ThecriteriadividetheclinicalfeaturesofARFintomajorandminormanifestations,basedontheirprevalenceandspecificity.Majormanifestationsarethosethatmakethediagnosismorelikely,whereasminormanifestationsareconsideredtobesuggestive,butinsufficientontheirown,foradiagnosisofARF.TheexceptiontothisisinthediagnosisofrecurrentARF.
TheJonescriteriahavebeenperiodicallymodifiedandupdated.The1992updateiscurrentlythemostwidelyusedandquotedversion.37
ThereareimportantcircumstanceswhereARFcanbediagnosedwithoutstrictlyadheringtotheJonescriteriaandtheseinclude:
choreaastheonlymanifestationofARF
indolentcarditis(carditisofinsidiousonsetandslowprogression)astheonlymanifestationofARF.37
Boththesetypesofpatientsmayhaveinsufficientsupportinghistorical,clinicalorlaboratoryfindingstofulfiltheJonescriteria.
The1992Jonescriteriaare intendedonly for the initial attackofARF. Furtherdiscussionof theJonescriteriacanbe found inAppendixB.
EachchangetotheJonescriteriawasmadetoimprovespecificityattheexpenseofsensitivity,largelyinresponsetothefallingincidenceofARFinAmerica.Asaresult,thecriteriamaynotbesensitiveenoughtopickupdiseaseinhighincidencepopulations,suchasMa-oriandPacificpeople.Insuchpopulations,theconsequencesofunder-diagnosisarelikelytobegreaterthanthoseofover-diagnosis.
AllcasesofsuspectedARFshouldbejudgedagainstthemostrecentversionoftheJonescriteria,butthecriterianeednotberigidlyadheredtowhenARFisthemostlikelydiagnosis.
AnexpertgroupconvenedbytheWorldHealthOrganisation(WHO)hasrecentlyprovidedadditionalguidelinesastohowtheJonescriteriashouldbeappliedinprimaryandrecurrentepisodes.38
The main modification made to the Jones 1992 criteria for these New Zealand guidelines is the acceptance of echocardiographic evidence of carditis as a major manifestation. In addition there is greater emphasis that monoarthritis may be a presenting feature if there is a history of non-steroidal anti-inflammatory drug (NSAID) use that is likely to have aborted classical ARF migratory polyarthritis.
NHF0239 80pp Inside.indd 14 21/6/06 12:11:58
-
15
DIAGNOSTIC REQuIREMENTS
InitialepisodeofARF
InitialepisodeofARF
InitialepisodeofARF
RecurrentattackofARF inacasewithknownpastARForRHD
2majoror1majorand2minormanifestationsplusevidenceofaprecedingGASinfection*
StrongclinicalsuspicionofARF,butinsufficientsignsandsymptomstofulfildiagnosisofdefiniteorprobableARF
Minormanifestations(seeTable4forkeypointsinidentifyingminormanifestations)
FeverRaisedESRorCRPPolyarthralgia
ProlongedP-RintervalonECG.
CATEGORY
DefiniteARF
ProbableARF
PossibleARF
Categoriesofdefinite,probableandpossibleARFcanbedeterminedbytheapplicationoftheNewZealandcriteriatoeachcase(Table2).
Table 2. New Zealand Guidelines for the Diagnosis of ARF
All categories assume that other more likely diagnoses have been excluded. Please see additional tables for details about specifi c manifestations.CRP = C-reactive protein; ECG = electrocardiogram; ESR = erythrocyte sedimentation rate; GAS = group A streptococcus; RHD = rheumatic heart disease
*
**
***
#
Elevated or rising antistreptolysin O or other streptococcal antibody (Table 5), is suffi cient for a diagnosis of defi nite ARF. A positive throat culture or rapid antigen test for GAS alone is less secure as 50% of those with a positive throat culture will be carriers only. Therefore, a positive culture alone demotes a case to probable or possible ARF
Most cases of recurrence fulfi l the Jones criteria. However in some cases (such as new carditis on previous RHD) it may not be clear. Therefore in order to avoid under-diagnosis, a presumptive diagnosis of rheumatic recurrence may be made where there are several minor manifestations and evidence of a preceding GAS infection in a person with a reliable history of previous ARF or established RHD. In addition, WHO (2004) recommendations state that where there is established RHD, a recurrent attack can be diagnosed by the presence of two minor manifestations plus evidence of a preceding group A streptococcal infection28
Acceptance of echocardiographic evidence of carditis as a major criterion is a modifi cation to the Jones (1992) update
When carditis is present as a major manifestation (clinical and/or echocardiographic), a prolonged P-R interval cannot be considered an additional minor manifestation in the same person
Other causes of arthritis/arthralgia should be carefully excluded, particularly in the case of monoarthritis e.g. septic arthritis (including disseminated gonococcal infection), infective or reactive arthritis and auto-immune arthropathy (e.g. juvenile chronic arthritis, infl ammatory bowel disease, systemic lupus erythematosus, systemic vasculitis and sarcoidosis. Note that if polyarthritis is present as a major manifestation, polyarthralgia cannot be considered an additional minor manifestation in the same person.
1majorand2minorwiththeinclusionofevidenceofaprecedingGASinfection*asaminormanifestation(Jones,1956)39
2majoror1majorand2minororseveral**minorplusevidenceofaprecedingGASinfection*(Jones,1992)37
Carditis(includingevidenceofsubclinicalrheumaticvalvediseaseonechocardiogram)#
Polyarthritis(orasepticmonoarthritiswithhistoryofNSAIDuse)Chorea(canbestand-aloneforARFdiagnosis)ErythemamarginatumSubcutaneousnodules
Majormanifestationsmodified*** fromJones1992(seeTable3forkeypointsinidentifyingmajormanifestations)
Special consideration should be given to high-risk population groups such as Ma-ori and Pacifi c people, and those residing in poor socio-economic circumstances. In these cases, it may be important to err on the side of diagnosis and prophylaxis.
NHF0239 80pp Inside.indd 15 21/6/06 12:11:58
-
1
Clinical features of acute rheumatic fever - major manifestationsThemajormanifestationsofARFandfeaturesfortheirdiagnosisarepresentedinTable3.
Table 3. Major Manifestations of ARF
Arthritis* MostcommonpresentingsymptomofARF(occurringinupto75%offirstattacks)
Classifiedasswellingofthejointinthepresenceoftwoormoreofthefollowing: limitationofmovement,hotnessofthejointandpaininthejointand/ortenderness.42Typically,thearthritisof ARFisextremelypainful
Largejointsareusuallyaffected,especiallykneesandankles
Polyarthritisisusuallyasymmetricalandmigratory(onejointbecominginflamedasanothersubsides)butcanbeadditive(multiplejointsprogressivelybecominginflamedwithoutwarning)
HighlyresponsivetosalicylateandNSAIDtherapy-usuallyrespondswithin3days
MonoarthritismaybeapresentingfeatureifthereisahistoryofNSAIDuseearlyinthecourseoftheillness(prematurelyabortingthemanifestationofpolyarthritis).**ThisdiagnosisisbestmadebyaphysicianexperiencedinARF
Thediagnosisofarthritisofthehipisacceptedbyhistoryofpainprecludingweightbearingand/orlimitationofmovementonexamination
Inordertosatisfypolyarthritisasamanifestation,atleastonejointshouldhavebeenobservedinaclinicalsettingaccompaniedbyadefinitehistoryofarthritisinotherjoints(GradeD)
Carditis Valvulitisusuallypresentsclinicallyasanapicalholosystolicmurmurwithorwithoutamid-diastolicflowmurmur(Carey-Coombsmurmur)oranearlydiastolicmurmuratthebaseoftheheart(aorticregurgitation)
Althoughpericarditisandmyocarditismayoccur,cardiacinflammationinARFalmostalwaysaffectsthevalves,especiallythemitralandaorticvalves43,44
Earlydisease leadstovalvularregurgitation,whereasprolongedorrecurrentdiseasemay leadto increasedvalvularregurgitationorstenoticlesions43
Therheumaticaetiologycanusuallybeconfirmedbyatypicalappearanceonechocardiography(seeTables6and7)
InNewZealand,echocardiographicevidenceofsubclinicalcarditiscanalsobeacceptedasamajormanifestation
CongestiveheartfailureinARFresultsfromvalvulardysfunctionsecondarytovalvulitisandisnotduetoprimarymyocarditis45
Thenaturalhistoryofvalveregurgitationisa25-50%improvementbyoneyear46
Ifpericarditisispresent,thefrictionrubmayobscurevalvularmurmurs.
POINTS FOR DIAGNOSISMAJOR MANIFESTATION
Patientswhodonot fulfil thesecriteria,but inwhomtheclinician remainssuspicious that thediagnosismaybeARF,shouldbemaintainedonoralpenicillinand reviewed in two to fourweekswitha repeatechocardiogramtodetect theappearanceofnewlesions.40,41Ifthereisevidenceofrheumaticvalvediseaseclinicallyoronechocardiogram,thediagnosisisconfirmedandlong-termsecondaryprophylaxiscanbecommenced.IfthereisnoevidenceofcarditisandnoalternativediagnosishasbeenfoundthenARFmaybethediagnosisbyexclusion.Thosewithepidemiologicalriskfactors(Ma-ori,Pacificandlowsocio-economicstatus)shouldbecommencedonsecondaryprophylaxiswithdueconsiderationofanalternativediagnosis(suchasrheumatological)andtheneedforongoingreview.
NHF0239 80pp Inside.indd 16 21/6/06 12:11:58
-
17
Sydenhamschorea Consists of jerky, uncoordinated movements, especially affecting the hands, feet, tongue and face. Themovementsdisappearduringsleep.Theymayaffectonesideonly(hemichorea)
Usefulsignsinclude:47
themilkmaidsgrip(rhythmicsqueezingwhenthepatientgraspstheexaminersfingers) spooning(flexionofthewristsandextensionofthefingerswhenthehandsareextended) thepronatorsign(turningoutwardsofthearmsandpalmswhenheldabovethehead) inabilitytomaintainprotrusionofthetongue
Thismanifestationaffectsfemalespredominantly,particularlyinadolescence48,49
Chorea may occur after a prolonged latent period following GAS infection50,51,52 therefore no additionalmanifestations(includingraisedantibodytitres)arerequiredinordertomakeadiagnosisofARF
Choreahasastrongassociationwithcarditis,***henceechocardiographyisessential forassessmentofallpatientswithchorea,regardlessofthepresenceofcardiacmurmurs(LevelIV,GradeC).Afindingofsubclinicalcarditisbyechowill furthersupport thediagnosisofchoreaasamanifestationofARF (GradeD). Even intheabsenceofechocardiographicevidenceofcarditis,patientswithchoreashouldbeconsideredatriskofsubsequent cardiac damage.53 Therefore, they should all receive secondary prophylaxis, and be carefullyfollowedupforsubsequentdevelopmentofRHD
ChoreaistheARFmanifestationmostlikelytorecurandisoftenassociatedwithpregnancyororalcontraceptiveuse.Thevastmajorityofcasesresolvewithin6months(usuallywithin6weeks)althoughrarecaseslastingaslongas3yearshavebeendocumented47
Subcutaneousnodules
Rare(lessthan2%ofcases)buthighlyspecificmanifestationofARF54
Theyare0.5-2.0cmindiameter,round,firm,freelymobileandpainlessnodulesthatoccurincropsofupto12overtheelbows,wrists,knees,ankles,Achillestendon,occiputandposteriorspinalprocessesofvertebrae
Tendtoappear1-2weeksaftertheonsetofothersymptoms,lastonly1-2weeks(rarelymorethan1month)
Stronglyassociatedwithcarditis
Subcutaneousnodulesare rarely seenas the solemajor criterion inARFandshouldbeaccompaniedbyadditionalmajorcriteriainordertomakethediagnosis
Erythemamarginatum
Rareaswellasdifficulttodetect(especiallyindark-skinnedpeople)
Occursascircularpatternsofbrightpinkmaculesorpapulesthatblanchunderpressureandspreadoutwardsinacircularorserpiginouspatternonthetrunkandproximalextremities(almostneveronface).Therashmaybemoreapparentaftershowering
Notitchyorpainfulandnotaffectedbyanti-inflammatorymedication
Mayrecurforweeksormonths,despiteresolutionoftheotherfeaturesofARF
ErythemamarginatumisrarelyseenasthesolemajorcriterioninARFandshouldbeaccompaniedbyadditionalmajorcriteriainordertomakethediagnosis.
ARF should always be considered in the differential diagnosis of patients presenting with arthritis in high-risk populations. In the hospital setting, physicians and surgeons should collaborate when the diagnosis of arthritis is unclear. Patients with sterile joint aspirates in the absence of previous antibiotic exposure should never be treated speculatively for septic arthritis without further investigation, particularly in areas with high ARF/RHD prevalence
Note that in New Zealand, NSAIDs are now readily available over the counter and have therefore often been used prior to presentation
During recent outbreaks of ARF in the USA, up to 71% of patients with chorea had carditis.55 Even though clinically evident carditis increases the risk of later development of RHD, prior to cardiac echocardiography approximately 25% of patients with pure chorea also eventually developed RHD.53,56 This is explained by the fi nding that over 50% of patients with chorea, but without cardiac murmurs, have echocardiographic evidence of mitral regurgitation.5
*
POINTS FOR DIAGNOSISMAJORMANIFESTATION
***
**
NHF0239 80pp Inside.indd 17 21/6/06 12:11:59
-
1
Clinical features of acute rheumatic fever - minor manifestations
TheminormanifestationsofARFandfeaturesfortheirdiagnosisarepresentedinTable4.
POINTS FOR DIAGNOSISMINOR MANIFESTATION
Arthralgia MaysuggestARFifthearthralgiaoccursinthesamepatternasrheumaticpolyarthritis(migratory,asymmetricalandaffectinglargejoints)
If polyarthritis ispresentasamajormanifestation,polyarthralgiacannotbeconsideredanadditionalminormanifestationinthesameperson
Alternativediagnoses(assuggested inTable8)shouldbeconsidered inapatientwitharthralgiathat isnottypicalofARF
Fever MostmanifestationsofARFareaccompaniedbyfever(withtheexceptionofchorea)
InNew Zealand, an oral, tympanic or rectal temperature greater than or equal to 38C on admission, ordocumentedduringthecurrentillness,shouldbeconsideredasfever(LevelIV,GradeC)
Fever,likearthritisandarthralgia,isusuallyquicklyresponsivetosalicylate/NSAIDtherapy
Elevatedacutephasereactants
InNewZealand,aserumCRPlevelof30mg/LorESRof50mm/hmeetsthisdiagnosticcriterion(GradeD)
TheESRinARFistypically>80mm/hr,usuallyremainselevatedfor>4weeks,andmayremainelevatedfor3-6monthsdespiteamuchshorterdurationofsymptoms
TheserumCRPconcentrationrisesmorerapidlythantheESRandalsofallsmorerapidlywithresolutionoftheattack
ProlongedP-Rinterval Anelectrocardiogram(ECG)shouldbeperformedinallcasesofsuspectedARF(LevelIV,GradeC)
TheP-Rintervalincreasesnormallywithagethereforeneedstobeage-adjusted.ThefollowingupperlimitsofnormalareusedinNewZealand:*
Age3-12years:0.16seconds Age12-16years:0.18seconds Age17+years:0.20seconds
AprolongedP-Rintervalisoccasionallyanormalvariant,butonethatresolvesovertheensuingdaystoweeksmaybeausefuldiagnosticfeatureofARFincaseswheretheclinicalfeaturesarenotdefinitive.**Inthesecases,arepeatECGafter1-2monthsmaybeuseful
Extremefirstdegreeblocksometimesleadstoajunctionalrhythm,usuallywithaheartratesimilartothesinusrate
Seconddegree,andevencompleteheartblock,canoccurand,ifassociatedwithaslowventricularrate,maygivethefalseimpressionthatcarditisisnotsignificant
Intheabsenceofclinicalorechocardiographiccarditis,asecondorthirddegreeblockaccompaniedbyothermanifestationsofARFishighlysupportiveofthediagnosis(GradeD)
Whencarditisispresentasamajormanifestation(clinicaland/orechocardiographic),prolongedP-Rintervalcannotbeconsideredanadditionalminormanifestationinthesameperson.
Table 4. Minor Manifestations of ARF
*
**
Adapted from Park M K. 58 p42.
In a recent resurgence of ARF in the USA, 32% of patients had abnormal AV conduction, usually a prolonged P-R interval. A small proportion had more severe conduction abnormalities, which were sometimes found by auscultation or echocardiography in the absence of evidence of valvulitis.57
NHF0239 80pp Inside.indd 18 21/6/06 12:11:59
-
19
Evidence of a preceding group A streptococcal infectionGASareisolatedfromthroatswabsinlessthantenpercentofARFcasesinNewZealand5andlessthanfivepercentofcasesinAboriginalAustralians.54ThislatterfiguremaybearesultoflaterpresentationofARF,as28%ofAboriginalAustralianshavebeenfoundtopresentaschorea59comparedtosixpercentofARFcasesinAuckland(1993-1999).22,23Apositiveculturewithoutsupportiveantibodyelevationmaybecarriageinupto50%ofcases.37Streptococcalantibodytitresarethereforecrucialinconfirmingthediagnosis.ThemostcommonlyusedtestsaretheplasmaantistreptolysinO(ASO)andtheantideoxyribonucleaseB(anti-DNaseB)titres.TheserumASOtitrereachesamaximumataboutthreetosixweeksafterinfectionandtheserumanti-DNaseBtitrecantakeuptosixtoeightweekstoreachamaximum.60Therateofdeclineoftheseantibodiesvariesenormously,withtheASOtitrestartingtofallsixtoeightweeksandtheanti-DNaseBtitrethreemonthsafterinfection.61Intheabsenceofreinfection,theASOtitreusuallyapproachespre-infectionlevelsaftersixto12months,whereastheanti-DNaseBtitretendstoremainelevatedforlonger.62Thereferencerangefortheseantibodytitresvarieswithageandgeographicallocation.Inapopulationwithahighrateofstreptococcalinfections,manychildrenwillhavehighbackgroundstreptococcaltitres.Theupperlimitofnormalapproachattemptstodeterminearaisedtitreoverandabovethisbackground,andthereforeselectoutthosechildrenwhohavehadarecentstreptococcalinfection.63InNewZealand,anASOtitreofgreaterthanorequalto480and/oranantiDNaseBtitreofgreaterthanorequalto680isacceptedassignificant(GradeD)Table5.
Established from residual sera from children (under 15 years) hospitalised in Auckland in 1982. Lower levels may be acceptable in the very young or those over the age of 15 years. A two-tube (two-fold) rise or fall in antibody titres after 10 -14 days would also be diagnostic.Note that evidence of a preceding GAS infection is not necessary for the diagnosis of chorea as ARF.
TITRE (Iu/ML)
480
ANTIBODY TEST
ASO(anti-streptolysinO)
Anti-DNaseB 680
AllcasesofsuspectedARF(choreaisanexception)shouldhaveelevatedserumstreptococcalserologydemonstrated.Iftheinitialtitreisbelowtheupperlimitofnormal,testingshouldberepeated10to14dayslater(GradeD).
Other less common clinical featuresTheseincludeepistaxis,abdominalpain,rheumaticpneumonia(pulmonaryinfiltratesinpatientswithacutecarditis),mildelevationsofplasmatransaminaselevelsandmicroscopichaematuria,pyuriaorproteinuria.NoneisspecificforARFbutepistaxisandabdominalpainoccurcommonly.
EchocardiographyPrior to the introduction of echocardiography, the diagnosis of rheumatic carditis relied on clinical evidence of valvulitis orpericarditis,supportedbyradiographicevidenceofcardiomegaly.Today,allpatientswithsuspectedordefiniteARFshouldundergoechocardiography,ifpossible,toidentifyevidenceofcarditis(GradeC).
InNewZealand,echocardiologyfacilitiesarereadilyavailableinthelargercentersforpopulationsathigh-riskofARF.Theuseofechocardiographyasamajorcriterion forARFdiagnosis requiresexpert interpretationadhering toechocardiographicdiagnosticstandards.ThesestandardsconcurwithrecentWHOechocardiographiccriteriaforARFandaresummarisedinTable6(LevelIV).ThesecriteriacanreadilydistinguishasmallcolourjetofphysiologicalregurgitationinanormalchildfrompathologicalregurgitationinachildwithRHD.
Table 5. Upper Limits of Normal for Serum Streptococcal Antibody Titres Used in New Zealand for ARF Diagnosis
NHF0239 80pp Inside.indd 19 21/6/06 12:12:0
-
0
Table 6. Minimal Echocardiographic Criteria to Allow a Diagnosis of Pathological Valvular Regurgitation
Echocardiography allows the operator to comment on the appearance of valves that are affected by rheumatic inflammation. The degree of thickening gives some insight into the duration of valvulitis, no significant thickening occurs in the first weeks of acute rheumatic carditis (Level IV)
Only after several months is immobility of the subchordal apparatus and posterior leaflet observed. Several other findings have also been reported, including acute nodules, seen as a beaded appearance of the mitral valve leaflets.64 Although none of these morphological features is unique to ARF, the experienced echocardiographic operator can use their presence as supportive evidence of a rheumatic aetiology of valvulitis.
InNewZealand,ARFcarditisisclassifiedmild,moderateorsevere(Table7)andthesecategoriesareusedtoguidethedurationofsecondaryprophylaxis(seeSection7andTable13).
MITRAL REGuRGITATION
Colour:
Substantialcolourjetseenin2planesextendinggreaterthanorequalto2cmbeyondthevalveleaflets
ContinuouswaveorpulsedDoppler:
Holosystolicwithwell-definedhighvelocityspectralenvelope
Bothmitralandaorticvalveshavepathologicalregurgitation
Themitralregurgitantjetisdirectedposteriorly,asanteriormitralvalveprolapseismorecommonthanposteriorvalveprolapse
Multiplejetsofmitralregurgitation
ThepresenceofmorphologicaloranatomicalchangesconsistentwithRHD(seetext),butexcludingslightthickeningofvalveleaflets:
Definitethickeningofmitralvalveleaflets,indicativeofchronicRHD*
Elbowordoglegdeformity**ofanteriormitralvalveleaflet.
If theaetiologyof aorticormitral regurgitationonDopplerechocardiography isnotclear, the following featuressupportadiagnosisofrheumaticvalvedamage:
AORTIC REGuRGITATION
*
**
Colour:
Substantialcolourjetseenin2planesextendinggreaterthanorequalto1cmbeyondthevalveleaflets
ContinuouswaveorpulsedDoppler:
Holodiastolicwithwell-definedhighvelocityspectralenvelope
Source: Adapted with permission from Wilson N J. & Neutze J M.65 These criteria further evolved as part of the development of the Australian guidelines on rheumatic fever diagnosis and the WHO working groups on echocardiography.66
NHF0239 80pp Inside.indd 20 21/6/06 12:12:0
-
1
MODERATE CARDITIS
Anyvalvelesionofmoderateseverityclinically(e.g.mildormoderatecardiomegaly),or
Anyechocardiographicevidenceofcardiacchamberenlargementor
Anymoderateseverityvalvelesiononecho**
Mitralregurgitationisconsideredmoderateifthereisabroadhigh-intensityproximaljetfillinghalftheleftatriumora lesservolumehigh-intensityjetproducingprominentbluntingofpulmonaryvenousinflow41
Aorticregurgitationisconsideredmoderateifthediameteroftheregurgitantjetis15%to30%ofthediameterofthe leftventricularoutflowtractwithflowreversalinupperdescendingaorta41
SEVERE CARDITIS
AnyimpendingorpreviouscardiacsurgeryforRHD,or
Anyseverevalvelesionclinically(significantcardiomegalyexpected,and/orheartfailure),or
Anyseverevalvelesiononecho:
AbnormalregurgitantcolourandDopplerflowpatternsinpulmonaryveinsareaprerequisiteforseveremitral regurgitation41
Dopplerreversalinlowerdescendingaortaisrequiredforsevereaorticregurgitation.41
Valvular regurgitation is usually relatively mild in the absence of pre-existing disease; in fi rst episodes of ARF, severe mitral and aortic regurgitation occurred in less than 10% of patients in New Zealand41
When there is both mitral and aortic regurgitation, one must be moderate by echo criteria in order for the carditis to be classifi ed of moderate severity.
Ifvalvulitisisnotfoundatpresentation,itmayappearwithintwoweeks,40oroccasionallywithinonemonth41butnolonger.ThusanequivocalinitialechocardiographshouldbefollowedupintwotofourweeksifthefindingswouldalterthediagnosisofARF.
Usuallyitisnotpossibletoconfidentlydistinguishbetweenacutecarditisandpre-existingrheumaticvalvediseasebyechocardiography.InapatientwithknownpreviousRHD,thediagnosisofacutecarditisduringarecurrenceofARFreliesonaccuratedocumentationofthecardiacfindingsbeforetherecurrence,sothatnewclinicalorechocardiographicfeaturescanbeconfirmed.But,inapatientwithnopriorhistoryofARForRHD,itmakeslittledifferencewhetherechocardiographicchangesareneworold.
FurtherdetailsontheuseofechoinARFcanbefoundinAppendixC.
MILD CARDITIS*
Mildmitraloraorticregurgitationclinicallyand/oronecho(fulfillingtheminimalechostandardsinTable6)withnoclinicalevidence ofheartfailureandnoevidenceofcardiacchamberenlargementonCXR,ECGorechocardiography
Table 7. Severity of ARF Carditis
*
**
Tricuspid and pulmonary regurgitation graded mild or greater may be seen in people with normal hearts who have fever, volume overload or pulmonary hypertension. For this reason a diagnosis of carditis should not be based on right-side regurgitation alone. Although pulmonary and tricuspid regurgitation are often seen in association with left-sided lesions in ARF, pressure and volume overload must be excluded before attributing even moderate tricuspid regurgitation to valvulitis. If both left and right-sided lesions coexist in ARF carditis, then the predominant infl uence for diagnosis is the severity of the left-sided lesion.
NHF0239 80pp Inside.indd 21 21/6/06 12:12:1
-
Table 8. Differential Diagnoses of Common Major Manifestations of ARF
Source: Adapted from Lennon D. 2004,32 and Carapetis J et al. 2005.67
POLYARTHRITIS AND FEVER
Otherinfections*(includinggonococcal)
Connectivetissueandotherauto-immunedisease**
Reactivearthropathy
Sicklecellanaemia
Infectiveendocarditis
Leukaemiaorlymphoma
Goutandpseudogout
Henoch-Schonleinpurpura
Post-streptococcalreactivearthritis***
Other,e.g.HIV/AIDS,leukaemia
CARDITIS CHOREA
DIF
FER
EN
TIA
L D
IAG
NO
SE
S
Innocentmurmur
Mitralvalveprolapse
Congenitalheartdisease
Infectiveendocarditis
Hypertrophiccardiomyopathy
Myocarditisviraloridiopathic
Pericarditisviraloridiopathic
Systemiclupuserythematosus
Drugingestion(extrapyramidalsyndrome)#
Wilsonsdisease(usuallyadultonset)
Ticdisorder
Congenital,e.g.hyperbilirubinaemia
Choreoathetoidcerebralpalsy
Encephalitis
Familialchorea(includingHuntingtons)
Intracranialtumour
Hormonal
Metabolic,e.g.Lesch-Nyhan, hyperalanaemia,ataxia,telangiectasia
Antiphospholipidantibody
Differential diagnosisManyoftheclinicalfeaturesofARFarenon-specific,soawiderangeofdifferentialdiagnosesshouldbeconsideredasshowninTable8.32,67
Includes bacterial arthritis (e.g. Staphylococcus aureus, Neisseria gonorrhea), influenza b, cytomegalovirus, Epstein-Barr Virus, mycoplasma, rubella (also post-vaccination), hepatitis B, parvovirus, Yersinia spp and other gastrointestinal pathogens
Includes rheumatoid arthritis, juvenile chronic arthritis, inflammatory bowel disease, systemic lupus erythematosus, systemic vasculitis, sarcoidosis and others
Some patients present with arthritis not typical of ARF, but with evidence of recent streptococcal infection and are said to have post-streptococcal reactive arthritis. In these cases the arthritis may affect joints that are not commonly affected in ARF (such as the small joints of the hand), and is less responsive to anti-inflammatory treatment. These patients are said not to be at risk of carditis, and therefore do not require secondary prophylaxis. However, some patients diagnosed with post-streptococcal reactive arthritis have developed later episodes of ARF, indicating that the initial diagnosis should have been atypical ARF (Level IV)68,69
It is recommended that the diagnosis of post-streptococcal reactive arthritis should rarely, if ever, be made in high-risk populations, and with caution in low-risk populations (Grade C). Patients so diagnosed should receive secondary prophylaxis for at least 5 years (Grade D). Echocardiography (see algorithm 2) should be used to confirm the absence of valvular damage in all of these cases before discontinuing secondary prophylaxis (Grade D)
Drugs and toxins include anticonvulsants, antidepressants, lithium, scopolamine, calcium channel blockers, methylphenidate, theophylline and antihistamines
Some cases of chorea are mild or atypical and may be confused with motor tics or the involuntary jerks of Tourettes syndrome. There may therefore be confusion between Sydenhams chorea and these conditions. The term PANDAS (Pediatric Auto-immune Neuropsychiatric Disorder Associated with Streptococcal infection) refers to a subgroup of children with tic or obsessive-compulsive disorders (OCD), whose symptoms may develop or worsen following GAS infection.
Five criteria have been used to define the PANDAS subgroup:70,71
The presence of a Tic disorder and/or OCD Pre-pubertal age of onset (usually between 3 and 12 years of age) Abrupt symptom onset and/or episodic course of symptom severity Temporal association between symptom exacerbations and streptococcal infection (approx 7-14 days) Presence of neurologic abnormalities during periods of symptom exacerbation (typically adventitious movements or motoric hyperactivity)
*
**
***
#
NHF0239 80pp Inside.indd 22 21/6/06 12:12:1
-
3
Investigations Therecommendedinvestigations inARFare listed inTable9.Other investigationsmaybeappropriatedependingontheclinicalpictureandpotentialdifferentialdiagnoses.
Whitebloodcellcount
Erythrocytesedimentationrate(repeatweeklyoncediagnosisconfirmed)
C-reactiveprotein
Bloodculturesiffebrile
Electrocardiogram(repeatasnecessaryifconductionabnormalitymorethanfirstdegree)
Chestx-rayifclinicalorechocardiographicevidenceofcarditis
Echocardiogram(repeatasnecessaryin2-4weeksifequivocalorifseriouscarditis)
Throatswab(preferablybeforegivingantibiotics)cultureforgroupAstreptococcus
Anti-streptococcalserology:bothanti-streptolysinOandanti-DNaseBtitres,ifavailable(repeat10-14dayslaterif1sttestnot confirmatory)
Serologyandauto-immunemarkersforauto-immuneorreactivearthritis(includingANA-AntiNuclearAntibody)
Repeatedbloodculturesifpossibleendocarditisorsepticarthritis
Jointaspirate(microscopyandculture)forpossiblesepticarthritis*
JointX-ray
Copper,caeruloplasmin,anti-nuclearantibody,drugscreen,andconsiderCT/MRIheadforchoreiformmovements.**
RECOMMENDED FOR ALL CASES
TESTS FOR ALTERNATIVE DIAGNOSES, DEPENDING ON CLINICAL FEATuRES
Typically, the synovial fl uid in joints affected by ARF contains 10,000 to 100,000 white blood cells/mm3 (predominantly neutrophils). The protein concentration is approximately 4g/dL, glucose levels are normal, gram stain negative and a good mucin clot is present72
The chorea of ARF can be readily diagnosed on the basis of history, physical examination and laboratory evaluation. Neuroimaging is seldom necessary and should be reserved for cases who have an atypical presentation such as hemichorea.73
Table 9. Investigations in Suspected ARF
However, the evidence supporting PANDAS as a distinct disease entity has been questioned.71 Hence, in New Zealand populations with a high prevalence of ARF, clinicians should rarely (if ever) make a diagnosis of PANDAS, and should rather err on the side of over-diagnosis of ARF and secondary prophylaxis (Grade D). If ARF is excluded, secondary prophylaxis is not needed, but such cases should be carefully followed up to ensure that they do not develop carditis in the long term
Includes oral contraceptives, pregnancy (chorea gravidarum), hyperthyroidism and hypoparathyroidism.
*
**
NHF0239 80pp Inside.indd 23 21/6/06 12:12:2
-
Ideally,allthosewithsuspectedARF(firstepisodeorrecurrence)shouldbehospitalisedassoonaspossibleafteronsetofsymptoms(GradeD).Thisensuresthatallinvestigationsareperformedand,ifnecessary,observationscompletedforaperiodpriortocommencingtreatmenttoconfirmthediagnosis.Hospitalisationalsoprovidesanidealopportunityforeducation
Observationpriortoanti-inflammatorytreatment(paracetamol[1stline]forfeverorjointpain)
Investigations(asperTable9)
TREATMENT
All cases
CONFIRMATION OF THE DIAGNOSIS
ADMISSION TO HOSPITAL*
[5. Management of ARF]
Antibiotics**
OralpenicillinV(250mgtwicedaily)shouldbecommencedinallcaseswhilethediagnosisisbeingestablished.Toreliablyeradicate GAS,oralpenicillinshouldbegivenforthefull10days
Oralerythromycinusedincaseswithreliablydocumentedpenicillinallergy***(10daysoferythromycinethylsuccinate(EES)40mg/kg perdayin2-4divideddoses,maximum1g/dayinchildrenor400mgtwicedailyinadolescentsandadults).76EESiscurrentlythe onlyfullysubsidisedoralerythromycininNewZealand
Intravenousantibioticsarenotindicated.Roxithromycinisnotrecommendedbecauseofthelimitedavailableevidencethatitisnot aseffectiveaserythromycinineradicatingGASfromtheupperrespiratorytract77
ThefirstdoseofintramuscularbenzathinepenicillinG(BPG1,200,000Uor600,000Uiflessthan20kg)shouldalsobegiveninhospitalinassociationwitheducationabouttheimportanceofsecondaryprophylaxis.OncethefirstdoseofBPGisgiven,theoralpenicillinisstopped
Arthritis/arthralgia
Salicylates/NSAIDS
ThearthritisofARFhasbeenshownincontrolledtrialstoresponddramaticallytosalicylatesandhasalsobeennotedtorespondto otherNSAIDtherapy,78,79,80oftenwithinhoursandalmostalwayswithin3days (LevelII)
SalicylatesarerecommendedasfirstlinetreatmentbecauseoftheextensiveexperiencewiththeiruseinARF.38,81,82Theyshould becommencedincaseswitharthritisorseverearthralgiaassoonasthediagnosisofARFhasbeenconfirmed(GradeB),butthey shouldbewithheldifthediagnosisisnotcertain.Insuchcases,paracetamolorcodeineshouldbeusedinsteadforpainrelief
Aspirinshouldbestartedatadoseof60-100mg/kg/day(4-8g/dayinadults)in4-5divideddoses.Ifthereisanincompleteresponse within2weeks, thedosemaybe increased to125mg/kg/day,butwith thesehigherdosescareful observation for featuresof salicylatetoxicityisadvised.Iffacilitiesareavailable,bloodlevelsmaybemonitoredeveryfewdays,andthedoseincreaseduntil serumlevelsof20-30mg/100dLarereached.Toxiceffects(tinnitus,headache,hyperpnoea)arelikelyabove20mg/100dLbutoften resolveafterafewdays
Mostcasesrequire10daysorlessofaspirintherapyandthereforebloodlevelmonitoringisseldomnecessary.Manyneedaspirin foronly1-2weeks,althoughsomeneeditforupto6weeks.Insuchcases,thedosecanoftenbereducedto60-70mg/kg/day
ThemajorpriorityinthefirstfewdaysafterpresentationinARFisconfirmationofthediagnosis.Exceptinthecaseofheartfailuremanagement,noneofthetreatmentsofferedtocaseswithARFhavebeenproventoaltertheoutcomeoftheacuteepisodeortheamountofdamagetoheartvalves.74,75Thus,thereisnourgencytobegindefinitivetreatment.TheprioritiesinmanagingARFareoutlinedinTable10.
Table 10. Priorities in Managing Acute Rheumatic Fever
NHF0239 80pp Inside.indd 24 21/6/06 12:12:2
-
5
TREATMENT CONTINuED
Activity Arthritisalone
Mild carditis Moderate carditis Severe carditis
In hospital 1-2weeks 2-3weeks 4-6weeks 2-4months
Mobilisefreelyastolerated
House arrest (activity and school work at home)
1-2weeksafterdischarge
2-3weeks 4-6weeks 2-4months
School 2weeks 2-4weeks 1-3months 2-3months
Gradualreturntofullactivity Avoidsportandphysicaleducation
Full activity(sport)
After6weeks
After3months After3-6months Variable
Urgentechocardiogram
Anurgentechocardiogramandcardiologyassessmentarerecommendedforallcaseswithheartfailure
aftertheinitial1-2weeks.32Asthedoseisreduced,orwithin3weeksofdiscontinuingaspirin,jointsymptomsmayrecur.Thisdoes notindicaterecurrence,andcanbetreatedwithanotherbriefcourseofhigh-doseaspirin.MostARFepisodessubsidewithin6 weeks,and90%resolvewithin12weeks.Approximately5%ofcasesrequire6monthsormoreofsalicylatetherapy83
ThereisalsotheriskofReyessyndromeinchildrenreceivingsalicylateswhodevelopcertainviralinfections,particularlyinfluenza.Itisrecommendedthatchildrenreceivingaspirinduringtheinfluenzaseason(autumn/winter)alsoreceiveaninfluenzavaccine(GradeD)
Naproxenhasbeenused (10-20mg/kg/day)successfully in thosewithARF, includingonesmall randomised trial,andhasbeen advocatedasasaferalternativetoaspirin(LevelIII-I).84,85Ithastheadvantageofonlytwice-dailydosing,lesshepatotoxicity,anditis alsoavailableinanelixirforyoungchildren.Theexperiencewiththismedicationislimited,sotherecommendationcurrentlyisto restrictittothoseintoleranttoaspirin,ortouseitasastep-downtreatmentoncecasesaredischargedfromhospital(GradeD)
Paracetamol
Mildarthralgiaandfevermayrespondtoparacetamolalone
Fever
Low-gradefeverdoesnotrequirespecifictreatment.Feverwillusuallyresponddramaticallytosalicylatetherapy.Feveralone,orfeverwithmildarthralgiaorarthritis,maynotrequiresalicylates,butcaninsteadbetreatedwithparacetamol
Carditis/heart failure
Bedrest
In thepre-penicillinera,prolongedbedrest in thosewithrheumaticcarditiswasassociatedwithshorterdurationofcarditis, fewerrelapsesandlesscardiomegaly.86Ambulationshouldbegradualandastoleratedincaseswithheartfailure,orsevereacutevalvedisease,especiallyduringthefirst4weeks,oruntiltheserumCRPlevelhasnormalisedandtheESRhasnormalisedordramaticallyreduced.Thosewithmilderornocarditisshouldremaininbedonlyaslongasnecessarytomanageothersymptoms,suchasjointpain(GradeD).
Aguideforactivitylevelsisshownbelow(AdaptedfromLennonD.200432)(GradeD).
NHF0239 80pp Inside.indd 25 21/6/06 12:12:2
-
Anti-failuremedication
Diuretics/fluidrestrictionformild-moderatefailure
ACEinhibitorsformoreseverefailure,particularlyifaorticregurgitationpresent
Glucocorticoidsoptionalforseverecarditis74
Digoxinifatrialfibrillationpresent
Thereislittleexperiencewithbeta-blockersinheartfailureduetoacutecarditis,andtheiruseisnotrecommended (GradeD)
Detailed recommendations for themanagement of heart failure can be found in a separate Heart Foundation clinical guideline(availableathttp://www.nzgg.org.nz)
Valvesurgery
Surgeryisusuallydeferreduntilactiveinflammationhassubsided.Rarely,valveleafletorchordaetendinaeruptureleadstosevereregurgitationwhichrequiresemergencysurgery.Thiscanbesafelyperformedbyexperiencedsurgeons,althoughtheriskappearstobeslightlyhigherthanwhensurgeryisperformedafteractiveinflammationhasresolved.87Valvereplacement,ratherthanrepair,isusuallyperformedduringtheacuteepisode,becauseofthetechnicaldifficultiesofrepairingfriable,inflamedtissue.Nevertheless,veryexperiencedsurgeonsmayachievegoodresultswithrepairinthissituation
Chorea
Sydenhamschoreaisself-limited.Mostcaseswillresolvewithinweeksandalmostallcaseswithin6months,88althoughrarecasesmaylastaslongas2-3years.59,89,90Mildormoderatechoreadoesnotrequireanyspecifictreatment,asidefromrestandacalmenvironment.Over-stimulationorstresscanexacerbatethesymptoms.Sometimeshospitalisationisusefultoreducethestressthatfamiliesfaceindealingwithabnormalmovementsandemotionallability
Becausechoreaisbenignandself-limiting,andanti-choreamedicationsarepotentiallytoxic,treatmentshouldonlybeconsideredifthemovementsinterferesubstantiallywithnormalactivities,placethepersonatriskofinjuryorareextremelydistressingtothepatient,familyandfriends.Aspirinandglucocorticoidtherapydonothaveasignificanteffectonrheumaticchorea47
Smallstudiesof intravenousimmunoglobulin(IVIG)havesuggestedmorerapidrecoveryfromchorea,buthavenotdemonstratedreduced incidenceof long-termvalvedisease innon-choreaARF.41,91 Untilmoreevidence isavailable, IVIG isnotrecommended,exceptforseverechorearefractorytoothertreatments(LevelII/IV,GradeC)
Carbamazepineandvalproicacid+arenowpreferredtohaloperidol,whichwaspreviouslyconsideredthefirst-linemedicaltreatmentforchorea.92,93Asmall,prospectivecomparisonofthese3agentsrecentlyconcludedthatvalproicacidwasthemosteffective94
Otheranti-choreamedicationsshouldbeavoidedbecauseofpotentialtoxicity.Becauseofthesmallpotentialforlivertoxicitywithvalproicacid,itisrecommendedthatcarbamazepinebeusedinitiallyforseverechorearequiringtreatment,andthatvalproicacidbeconsideredforrefractorycases(LevelIII2,GradeB).Aresponsemaynotbeseenfor1-2weeks,andsuccessfulmedicationmayonlyreduce,butnoteliminate,thesymptoms.Medicationshouldbecontinuedfor2-4weeksafterchoreahassubsidedandthenwithdrawn.Recurrencesofchoreaareusuallymildandcanbemanagedconservativelybut,insevererecurrences,themedicationcanbere-startedifnecessary
CLINICAL FOLLOW-uP
Allcasesshouldreceiveregularreviewandoutpatientfollow-upshouldbeinitiatedpriortodischarge
Thefrequencyanddurationofreviewisdependentontheindividualclinicalneedsandlocalcapacityandshouldbecomemorefrequentintheeventofsymptomonset,symptomaticdeteriorationorachangeinclinicalfindings
Particularcareshouldbetakenwhencasesaretransferredfrompaediatrictoadultservices.Acasecanbemadeformaintaininglessseverecasesinthepaediatricservicesuntildischargeatage21inordertoensurecontinuityoffollow-up
Jointcardiologyandgeneralpaediatric/physicianmanagementforcaseswithseverecarditisarerecommended
FurtherinformationregardingfrequencyandnatureofroutinereviewcanbefoundinSection11
NHF0239 80pp Inside.indd 26 21/6/06 12:12:3
-
7
COMMENCEMENT OF LONG-TERM PREVENTIVE MEASuRES
*
**
***
#
Secondaryprophylaxis
Obtainconsentfromcaregiver/caseforIMpenicillintreatment
Firstdoseofsecondaryprophylaxisshouldbedeliveredinhospital
Notification
Caseshouldbenotifiedtoa localARFregister ifavailable(seeSection10.3).Thereshouldbeaneasymeanstodothis,viaa standardnotificationform,telephonecallorotherwise
Inaddition,asARFisanotifiablediseaseinNewZealand,eachcaseshouldbenotifiedtothelocalpublichealthunitfornational infectiousdiseasesurveillance
Contactcommunityservicestoensurefollow-up
Theregistercoordinator (ifavailable)shouldnotifycommunityhealthstaffaboutARFcases in theirarea. Thenotifyingmedical practitionershouldalsomakedirectcontactwiththoseinthecommunityresponsibleforprophylaxisdeliveryinordertoensurethat theyareawareofthediagnosis,theneedforsecondaryprophylaxisandanyotherspecificfollow-uprequirements.Thismayinclude districtnurses,publichealthnurses,medicalofficerofhealthandotherpublichealthstaff
Acommunitynurseand/orcommunityhealthworkerfortheareawherethecaseresidesshouldalsodoawardand/orfamilyvisitif possiblebeforedischarge
Whererelevant,itisalsoimportantforconsenttobeobtainedfromthecase(orcaregiver)fortheirlocalMa-oriorPacificproviderto knowabouttheillness
Education
Atthetimeofdiagnosis,itisessentialthatthediseaseprocessbeexplainedtothepatientandtheirfamilyinaculturallyappropriate way,usingavailableeducationalmaterialsandinteractivediscussion.Furthereducation,usingculturallyappropriateeducational materialsshouldfollowoncethecasehasreturnedhome
ForfurtherinformationregardingeducationseeSection10.2
Organisedentalcheckandongoingdentalcare
Thisiscriticalinthepreventionofendocarditis.Asthosewithoutrheumaticvalvedamagemaystillbeatlong-termriskofdeveloping RHD,particularlyintheeventofrecurrentepisodesofARF,dentalcareisessential,regardlessofthepresenceorabsenceofcarditis
Eachcaseshouldbenotifiedtotheappropriateschooldentalserviceordentist
Contactmanagement
Allsymptomaticandasymptomatichouseholdcontactsoftheindexcaseaged3yearsandoldershouldhaveathroatswabifthe contactwasnolongerthanonemonthbeforetheonsetofARFintheindexcase.Thisshouldbeorganisedthroughtheappropriate publichealthunitandallcontactswithpositiveGASculturesshouldbeofferedantibiotictreatment.Streptococcalacquisitionrates of25%orgreaterhavebeenrecordedinfamilycontactsofstreptococcalpharyngitis78,95,96
Opportunisticcare
ItisimportanttonotethisopportunitytoprovideinformationandotherservicesforARFcases,whomfrequentlyhaveotherchallenges to theirgeneralwellbeing. Thismay includepromotingahealthydiet,exerciseandhygiene,aswellasassistancewithsocio- economicstressors,andtheopportunityforongoingsupport.
Occasionally, when the diagnosis has already been confi rmed and the case is not unwell (e.g. mild recurrent chorea in a child with no other symptoms or signs), outpatient management may be appropriate. In such cases health staff must ensure that investigations, treatment, health education, registration (where available) and notifi cation are all completed and prophylaxis commenced
Controlled studies have failed to show that treating ARF with large doses of penicillin affects the outcome of rheumatic valvular lesions 1 year later.97,98 Despite this, most authorities recommend a course of penicillin, even if throat cultures are negative, to ensure eradication of streptococci that may persist in the upper respiratory tract (Grade D)
Most people labelled as being allergic to penicillin are not. Because penicillin is the best antibiotic choice for secondary prophylaxis it is recommended that those with stated penicillin allergy be investigated carefully, preferably with the help of an allergist, before being accepted as truly allergic (Grade D) (Section 6)
If the symptoms and signs do not remit substantially within 3 days of commencing anti-infl ammatory medications, a diagnosis other than ARF should be considered
NHF0239 80pp Inside.indd 27 21/6/06 12:12:3
-
The use of glucocorticoids and other anti-inflammatory medications in rheumatic carditis has been studied in two meta-analyses.74,75 All of these studies of glucocorticoids were performed more than 40 years ago, and did not use drugs in common use today. These meta-analyses failed to suggest any benefit of glucocorticoids or IVIG over placebo, or of glucocorticoids over salicylates, in reducing the risk of long-term heart disease (Level I). The available evidence suggests that salicylates do not decrease the incidence of residual RHD (Level IV).78,79,80 Therefore, salicylates are not recommended to treat carditis (Grade C). Glucocorticoids may be considered for those with heart failure in whom acute cardiac surgery is not indicated (Grade D). This recommendation is not supported by evidence, but is made because many clinicians believe that glucocorticoids may lead to more rapid resolution of cardiac compromise, and even be life-saving in severe acute carditis.75,99 The potential major adverse effects of short courses of glucocorticoids, including gastrointestinal bleeding and worsening of heart failure as a result of fluid retention, should be considered before they are used. If glucocorticoids are used, the drug of choice is oral prednisone or prednisolone (1-2mg/kg/day, to a maximum of 80mg once daily or in divided doses). Intravenous methyl prednisolone may be given in very severe cases. If a week or less of treatment is required, the medication can be ceased when heart failure is controlled, and inflammatory markers are improving. For longer courses (usually no more than 3 weeks is required), the dose may be decreased by 20-25% each week. Treatment should be given in addition to the other anti-failure treatments outlined below. Mild to moderate carditis does not warrant any specific treatment. As glucocorticoids will control joint pain and fever, salicylates can usually be discontinued, or the dose reduced, during glucocorticoid administration. Salicylates may need to be recommenced after glucocorticoids are discontinued to avoid rebound joint symptoms or fever
Side effects of carbamazepine include CNS adverse reactions (dizziness, headache, ataxia, drowsiness, fatigue and diplopia); gastrointestinal disturbances (nausea and vomiting), as well as allergic skin reactions. Uncommon side effects include abnormal involuntary movements (e.g. tremor, asterixis, dystonia and tics) and nystagmus. Rarely carbemazapine can cause orofacial dyskinesia, oculomotor disturbances, speech disorders (e.g. dysarthria and slurred speech), choreoathetotic disorders, peripheral neuritis, paresthesia, muscle weakness and paretic symptoms100
Side effects of valproic acid include pancreatitis, hepatic toxicity, hyperammonaemia and thrombocytopaenia.100
Observation and general hospital careGuidelinesforgeneralin-hospitalcareareprovidedinTable11(GradeD).
Table 11. Guidelines For General In-Hospital Care
NuRSING RECORDINGS
Temperature,pulse,RR,BP4timesdailySleepingpulse(e.g.0200hrs)Ifpulse>100bpm,recordapicalHR
DIET
Freefluids(ifnoheartfailure)Normaldiet(limitextras)Earlydietaryadviceifoverweightandinfailure,toavoidfurtherweightgainWeeklyweight
BED REST AND GENERAL CARE
Examinedailyforthepatternofarthritisandthepresenceofheartmurmur,choreiformmovements,skinrashandsubcutaneous nodulesIfclinicalcarditispresent: Documentcardiacsymptomsandsigns Dailyweightandfluidbalancechart Medicationsasappropriate(seeTable10andAppendixD) Seegeneralguidelinesforbedrest(Table10) CardiologyopinionRepeatinvestigationsasnecessaryProvideculturalsupport(asrelevant)PlancaretoproviderestperiodsProvideage-appropriateactivitiesNotifyschoolteacherInvolvefamilyincare.
+
Source: Adapted from Lennon D. 2004.32
Note: RR = respiratory rate; BP = blood pressure; HR = heart rate.
NHF0239 80pp Inside.indd 28 21/6/06 12:12:4
-
9
DischargeTiming of discharge
Thedurationoftreatmentisdictatedbytheclinicalresponseandimprovementininflammatorymarkers(ESRandCRP).MostcasesofARFwithoutseverecarditiscanbedischargedfromhospitalafterapproximatelytwoweeks.Thelengthofadmissionwillpartlydependonthesocialandhomecircumstances.Ifcasescomefromremotecommunitiesorothersettingswithlimitedaccesstohighqualitymedicalcare,itisadvisabletodiscussdischargetimingwiththeperson,familyandthelocalprimaryhealthcareteam(particularlyMa-oriorPacifichealthproviderswherepossible).Insomecases,itmaybeadvisabletoprolongthehospitalstayuntilrecoveryiswelladvanced.
Advice on discharge
Allcasesshouldhaveagoodunderstandingofthecauseofrheumaticfeverandtheneedtohavesorethroatstreatedearlyinotherfamilymembers.Contactmanagement(asperTable10)shouldbediscussed.
CasesandtheirfamiliesshouldunderstandthereasonforsecondaryprophylaxisandtheconsequencesofmissingaBPGinjection.ThefirstdoseofBPGisusuallygiveninahospitalsetting.Arrangementsforthefirstinjectionpostdischargeshouldbemade.Theyshouldbegivenclearinformationaboutwheretogoforsecondaryprophylaxisoncedischarged,knowwhotocontactwithquestionsconcerningtheirfollow-uporsecondaryprophylaxis,andbegivenwritteninformationonappointmentsforfollow-upwiththeirlocalmedicalpractitioner,physician/paediatricianandcardiologist(ifneeded).Theyshouldbeadvisedoftheappropriateactivityleveluntiltheirnextclinicappointment.
Casesandtheirfamiliesshouldalsoberemindedoftheimportanceofadditionalantibioticprophylaxisfordentalandotherprocedurestoprotectagainstendocarditis(AppendixH).
Copiesofthedischargesummaryshouldgotothefollowingservices:communitynursingstaffresponsibleforprophylaxisdelivery(suchasdistrictnurse,publichealthnurse),rheumaticfeversecretaryorstaffresponsiblefortheregister(whereapplicable),primarycareproviderandthefamily.
NHF0239 80pp Inside.indd 29 21/6/06 12:12:4
-
30
NHF0239 80pp Inside.indd 30 21/6/06 12:12:4
-
31
[SecondaryPrevention]
NHF0239 80pp Inside.indd 31 21/6/06 12:12:5
-
3
[6. Prophylaxis Regimes]
SECONDARY PREVENTIONSecondarypreventionofrheumaticfeverisdefinedasthecontinuousadministrationofantibioticstocaseswhohavehadapreviousattack of ARF orwell-documented RHD. The purpose is to prevent infection of the upper respiratory tract withGAS and thedevelopmentofrecurrentrheumaticfever.28
TheregularadministrationofantibioticstopreventinfectionwithgroupAstreptococcal(GAS)andrecurrentARFisrecommendedforallpeoplewithahistoryofARForRHD.3ThisstrategyhasbeenproveninrandomisedcontrolledtrialstopreventstreptococcalpharyngitisandrecurrentARF.
PenicillinInearlystudiesofARFprophylaxisusingsulphonamides,1.5%oftreatedcasesdevelopedARFrecurrences,comparedto20%ofuntreatedcases.Subsequently,penicillinwasfoundtobemoreefficaciousthansulphonamides(LevelI).35,83
ArecentCochranemeta-analysis101concludedthattheuseofpenicillin(comparedtonotherapy) isbeneficial inthepreventionofrecurrentARF,andthatintramuscularbenzathinepenicillinG(BPG)issuperiortooralpenicillininthereductionofbothrecurrentARF(8796%reduction)andstreptococcalpharyngitis(71-91%reduction)(LevelI)(AppendixE).
SecondaryprophylaxisalsoreducestheseverityofRHD.Itisassociatedwithregressionofheartdiseaseinapproximately50-70%ofthosewithadequateadherenceoveradecade(LevelIII2),56,102,103andreducesmortality(LevelIII2).104
DoseTheinternationallyacceptedstandarddoseofBPGforthesecondarypreventionofARFinadultsis1,200,000U.3,38,105Thedoseforchildrenislessclear.InNewZealand,itisrecommendedthat1,200,000UofBPGshouldbeusedforsecondaryprophylaxisforallpersonsweighing20kgormore(LevelIII-2,GradeB),and600,000Uforthoseweighinglessthan20kg(GradeD).106
FrequencyWhile BPG is usually administered every four weeks (28 days), serum penicillin levels may be low or undetectable 28 daysfollowingadoseof1,200,000U.107 Fewerstreptococcal infectionsandARFrecurrencesoccurredamongthosereceiving three-weeklyBPG(LevelI).101,108,109Moreover,thethree-weeklyregimenresultedingreaterresolutionofmitralregurgitationinalong-termrandomised study in Taiwan (66%vs46%) (Level II).110 Prospective data fromNewZealandhowever, showed that recurrenceswere rare among people who were fully adherent to a four-weekly BPG regimen. In Auckland (1993 to 1999), the rate ofrecurrenceinfullyadherentindividualsona28dayregimewas0.07per100patientyears.Failureontheprophylaxisprogramme(i.e. including thosewhowere less than fully adherent) was 1.4 per patient years.16,17 This compares favourably to prophylaxisfailure reported in Taiwan of 0.25 (21-day programme) and 1.29 (28-day programme) per 100 patient years.111 Furthermore, afour-weekly regime is preferable to a three-weekly regime because of the resource and compliance implications (Grade D).InNewZealand,threeweekly(21-day)BPGisrecommendedonlyforthosewhohaveconfirmedrecurrentARFdespitefulladherencetofour-weekly(28-day)BPGdelivery(GradeC).16,17
AnalternativestrategyistheadministrationoflargerdosesofBPG,leadingtoahigherproportionofpeoplewithdetectableserumpenicillinlevelsfourweeksafterinjection.112However,untilmoredataareavailable,thisstrategycannotberecommended.
NHF0239 80pp Inside.indd 32 21/6/06 12:12:5
-
33
Table 12. Recommended Antibiotic Regimens for Secondary Prevention of Acute Rheumatic Fever/Rheumatic Heart Disease
ANTIBIOTIC
First line
DOSE ROuTE FREQuENCY
BenzathinepenicillinG(BPG)
1,200,000U20kg600,000U20kg450mg(600,000U)20kg
REGIMEN
Singledose
DuRATION
PenicillinVPO
or
250mgbd 10days
ErythromycinethylsuccinatePO
40mg/kgperdayin2-4divideddosesmaximum1g/day(children)
400mgbd(adolescentsandadults)
10days
ParacetamolPO Arthritisorarthralgia-mildoruntildiagnosisconfirmed
60mg/kg/day(max4g)givenin4-6doses/day.Mayincreaseto90mg/kg/dayifneeded,undermedicalsupervision
UntilsymptomsrelievedorNSAIDstarted
CodeinePO Arthritisorarthralgiauntildiagnosisconfirmed
0.5-1.0mg/kg/dose(adults15-60mg/dose)4-6h
AspirinPO Arthritisorseverearthralgia(whenARFdiagnosisconfirmed)
80-100mg/kg/day(4-8g/dinadults)givenin4-5doses/day
Reduceto60-70mg/kg/daywhensymptomsimprove
Considerceasinginthepresenceofacuteviralillness,andconsiderinfluenzavaccineifadministeredduringautumn/winter
Untiljointsymptomsrelieved
NaproxenPO Arthritis(ifaspirin-intolerant)
10-20mg/kg/day (max1250mg)givenbd
Asforaspirin
PrednisoneorPrednisolonePO
Severecarditis,heartfailure,pericarditiswitheffusion
1-2mg/kg/day(max80mg).Ifused>1week,taperby20-25%perweek
Usually1to3weeks
FrusemidePO/IV(canalsobegivenIM)
Heartfailure Children:1-2mg/kgstat,then0.5-1mg/kg/dose6-24hrly(max6mg/kg/dose)
Adults:20-40mg/dose12-24hrlyupto250-500mg/day
Untilfailurecontrolledandcarditisimproved
NHF0239 80pp Inside.indd 68 21/6/06 12:12:21
-
9
SpironolactonePO
MEDICATION
Heartfailure
INDICATION
1-3mg/kg/day(max100-200mg/day)in1-3doses.Rounddosetomultipleof6.25mg(quarterofatab)
REGIMEN
Asforfrusemide
DuRATION
EnalaprilPO Children:0.1mg/kg/dayin1-2dosesincreasedgraduallyover2wkstomaxof1mg/kg/dayin1-2doses
AdultsInitial:2.5mgdailyMaintenance:10-20mgdaily(max40mg)
Asforfrusemide
LisinoprilPO Heartfailure Children:0.1-0.2mg/kgoncedailyupto1mg/kg/dose
Adults:2.5-20mgoncedaily(max40mg/day)
Asforfrusemide
DigoxinPO/IV Heartfailure/atrialfibrillation
Children:15mcg/kgstatandthen5mcg/kgafter6hrs,then3-5mcg/kg/dose(max125mcg)12-hourly.
Adults:125-250mcgdaily
Checkserumlevels
CarbamazepinePO Severechorea 7-20mg/kg/day(7-10mg/kg/dayusuallysufficient)giventds.
Untilchoreacontrolledforseveralweeks,thentrialoffmedication
Heartfailure
Seekadvicefromspecialist
ValproicacidPO Severechorea(mayaffectsalicylatemetabolism)
Usually15-20mg/kg/day(canincreaseto30mg/kg/day)giventds
Asforcarbamazepine.
NHF0239 80pp Inside.indd 69 21/6/06 12:12:21
-
70
Appendix E: Comparison of intramuscular penicillin and oral penicillin for secondary prevention
AsearchwasconductedbyManyembaandMayosi(2002).101ThesearchstrategyincludedtheControlledTrialsRegister(CochraneLibrary Issue2,2001),Medline (January1996toJuly2000),Embase (January1985toJuly2000), reference listsofarticlesandconsulatationwithexperts.
Randomisedandquasi-randomisedstudiescomparing:(i)oralwithintramuscularpenicillin;and(ii)two-weeklyorthree-weeklywithfour-weeklyintramuscularpenicillininpatientswithpreviousARF.Tworeviewersindependentlyassessedthetrialqualityandextractedthedataofsixincludedstudies(1,707patients).
Fourtrials(1,098patients)comparedIMwithoralpenicillinandallshowedthatIMpenicillinwasmoreeffectivethanoralinreducingrecurrenceofARFandstreptococcalthroatinfections.
Onetrialcomparedtwo-weeklywithfour-weeklyIMpenicillin.PenicillingiveneverytwoweekswasbetteratreducingARFrecurrence(relativerisk(RR)0.52,95%confidenceinterval(CI)0.33-0.83)andstreptococcalthroatinfections(RR0.60,95%CI0.42-0.85).
Onetrial(249patients)showedthatthree-weeklyIMpenicillininjectionsweremoreeffectivethanfour-weeklyIMpenicillinatreducingstreptococcalthroatinfections(RR0.67,95%CI0.48-0.92).
TheconclusionsmadethereforewerethatIMpenicillinseemedtobemoreeffectivethanoralpenicillininpreventingARFrecurrenceandstreptococcalthroatinfections.Two-weeklyorthree-weeklyinjectionsappearedtobemoreeffectivethanfour-weeklyinjections.However,theevidencewasbasedonpoor-qualitytrialsandtheuseofoutdatedformulationsoforalpenicillin.101
NHF0239 80pp Inside.indd 70 21/6/06 12:12:21
-
71
Appendix F: Anaphylaxis recognition and management
Thesignsandsymptomsofananaphylacticreactioninclude:rapidweakpulse,wheeze,tightnessinchest,pruritis,urticaria,giddinessorheadache,flushingand/orperiorbitaloedema.
Response procedure: donotleavethepatientalone
callforassistance
liepatientinrecoveryposition(maybebettersittingupifsevererespiratorydistress)
ensureairwayisclear,applyoxygenifavailable
giveadrenaline(Table25)
ring111forambulance
checkvitalsigns,notecolour,toneandperfusion
ifsignsoffurtherdeterioration,repeatadrenalineafter10minutes
upto3dosesofadrenalinecanbegiven.
Adrenaline dosage:Table 25. Recommended Dose of Adrenaline in Anaphylaxis*
0.5mlof1:1000adrenaline,deepIMinjection
12 YEARS OF AGE AND OVER
Approximately0.01ml/kgof1:1000adrenaline,deepIMinjection
Age0-3years:0.1ml
Age4-6years:0.2ml
Age6-8years:0.3ml
Age9-12years:0.4ml
uNDER 12 YEARS OF AGE
Source: StarshipHospitalClinicalPracticeManual,AucklandDistrictHealthBoard(2006).
* Up to 3 doses of adrenaline can be given
NHF0239 80pp Inside.indd 71 21/6/06 12:12:22
-
7
Appendix G: Protocol for follow-up of non-compliant cases
Case is non-compliant with injections on 3-4 concurrent occasions. All attempts at contact are clearly documented in the patients fi le. These attempts should include the use of multiple modalities for contact including telephone
calls, visits, texting and the use of the local knowledge of community health workers
Discuss with primary nurse and refer to community health worker, public health nurse, or other community staff as fi tting in the area for follow up. Note also opportunity to involve staff from Ma-ori or Pacifi c
primary health providers, if appropriate
Community health worker (or other community staff responsible) follows up with case (and family) to determine reason for non-
compliance. Where necessary and appropriate, provides on going support, education, and arranges appointments for review at
outpatient clinic
If compliance is no longer a problem, continue routine
secondary prophylaxis
At the end of the holding period, the primary nurse and community health
worker review the case and ifconsidered appropriate a discharge
letter is to be sent to the case, with a copy to the patient fi le, GP, and rheumatic
fever register (if available)
If non-compliance continues, letter of planning to discharge is copied to the
case, case fi le, and GP after discussion with primary nurse and community
health worker
Case fi le goes on holdfor up to six months
(local area policy may suggest regular attempts at contact while
case is on hold)
NHF0239 80pp Inside.indd 72 21/6/06 12:12:23
-
73
Appendix H: Wallet card for infective endocarditis prevention
Information For Patient/Parents/Guardians
has a heart disorder and therefore needs antibiotic protection to be given before some of the procedures that dentists and doctors may need to do.
YOU MUST SHOW THIS CARD TO ANY DENTIST/DENTAL THERAPIST OR DOCTOR BEFORE TREATMENT IS STARTED.
General Advice
1 Regular teeth cleaning and avoiding sugary foods and drinks will reduce the need for dental surgery.2 Regular dental check ups will help keep teeth healthy.
HOSPITAL CHECK UPS DO NOT REPLACE VISITS TO YOUR LOCAL DENTIST/ DENTALTHERAPIST.
3