Rheumatic Fever
-
Upload
princessisma -
Category
Documents
-
view
221 -
download
0
Transcript of Rheumatic Fever

Rheumatic feverFrom Wikipedia, the free encyclopedia
• Ten things you didn't know about images on Wikipedia •Jump to: navigation, search
Rheumatic feverClassification & external resources
ICD-10 I 00. -I 02. ICD-9 390–392
DiseasesDB 11487MedlinePlus 003940
eMedicine med/3435 med/2922 emerg/509 ped/2006
MeSH D012213
Rheumatic fever is an inflammatory disease which may develop after a Group A streptococcal infection (such as strep throat or scarlet fever) and can involve the heart, joints, skin, and brain.
Contents[hide]
1 General information 2 Diagnosis: modified Jones criteria
o 2.1 Major criteria o 2.2 Minor criteria o 2.3 Other signs and symptoms
3 Pathophysiology 4 Treatment
o 4.1 Infection o 4.2 Inflammation o 4.3 Heart failure
5 Prevention 6 Notable people affected or killed by rheumatic fever 7 References
8 External links
[edit] General informationRheumatic fever is common worldwide and responsible for many cases of damaged heart valves. In the Western countries, it became fairly rare since the 1960s, probably due to widespread use of antibiotics to treat streptococcus infections. While it is far less

common in the United States since the beginning of the 20th century, there have been a few outbreaks since the 1980s. Although the disease seldom occurs, it is serious and has a mortality of 2–5%.
Rheumatic fever primarily affects children between ages 6 and 15 years and occurs approximately 20 days after strep throat or scarlet fever. In up to a third of cases, the underlying strep infection may not have caused any symptoms.
The rate of development of rheumatic fever in individuals with untreated strep infection is estimated to be 3%. The rate of development is far lower in individuals who have received antibiotic treatment. Persons who have suffered a case of rheumatic fever have a tendency to develop flare-ups with repeated strep infections.
The recurrence of rheumatic fever is relatively common in the absence of maintenance of low dose antibiotics, especially during the first three to five years after the first episode. Heart complications may be long-term and severe, particularly if valves are involved.
[edit] Diagnosis: modified Jones criteriaT. Duckett Jones, MD, first published these criteria in 1944.[1] They have been periodically revised by the American Heart Association in collaboration with other groups.[2] Two major criteria, or one major and two minor criteria, when there is also evidence of a previous strep infection, support the diagnosis of rheumatic fever.[3][4]
[edit] Major criteria
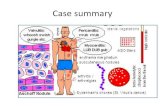
Carditis: inflammation of the heart muscle which can manifest as congestive heart failure with shortness of breath, pericarditis with a rub, or a new heart murmur.
Migratory polyarthritis : a temporary migrating inflammation of the large joints, usually starting in the legs and migrating upwards.
Sydenham's chorea (St. Vitus' dance): a characteristic series of rapid movements without purpose of the face and arms. This can occur very late in the disease.
Erythema marginatum : a long lasting rash that begins on the trunk or arms as macules and spread outward to form a snakelike ring while clearing in the middle. This rash never starts on the face and is made worse with heat.
Subcutaneous nodules (a form of Aschoff bodies): painless, firm collections of collagen fibers on the back of the wrist, the outside elbow, and the front of the knees. These now occur infrequently.
[edit] Minor criteria
Fever : temperature elevation Arthralgia : Joint pain without swelling

Laboratory abnormalities: increased Erythrocyte sedimentation rate, increased C reactive protein, leukocytosis
Electrocardiogram abnormalities: a prolonged PR interval Evidence of Group A Strep infection: positive culture for Group A Strep,
elevated or rising Antistreptolysin O titre Previous rheumatic fever or inactive heart disease
[edit] Other signs and symptoms
Abdominal pain Nosebleeds
[edit] PathophysiologyRheumatic fever is a systemic disease affecting the peri-arteriolar connective tissue and can occur after an untreated Group A streptococcal pharyngeal infection. It is believed to be caused by antibody cross-reactivity. This cross-reactivity is a Type II hypersensitivity reaction and is termed molecular mimicry. Usually, self reactive B cells remain anergic in the periphery without T cell co-stimulation. During a Strep. infection activated antigen presenting cells such as macrophages present the bacterial antigen to helper T cells. Helper T cells subsequently activate B cells and induce the production of antibodies against the cell wall of Streptococcus. However the antibodies may also react against the myocardium and joints[5], producing the symptoms of Rheumatic fever.
Group A streptococcus pyogenes has a cell wall composed of branched polymers which sometimes contain "M proteins" that are highly antigenic. The antibodies the immune system generates against the "M proteins" may cross react with cardiac myofiber sarcolemma and smooth muscle cells of arteries, inducing cytokine release and tissue destruction. This inflammation occurs through direct attachment of complement and Fc receptor-mediated recruitment of neutrophils and macrophages. Characteristic Aschoff bodies, composed of swollen eosinophilic collagen surrounded by lymphocytes and macrophages can be seen on light microscopy. The larger macrophages may become Aschoff giant cells. Acute rheumatic valvular lesions may also involve a cell-mediated immunity reaction as these lesions predominantly contain T-helper cells and macrophages.[6]
In acute RF, these lesions can be found in any layer of the heart and is hence called pancarditis. The inflammation may cause a serofibrinous pericardial exudates described as “bread-and-butter” pericarditis, which usually resolves without sequelae. Involvement of the endocardium typically results in fibrinoid necrosis and verrucae formation along the lines of closure of the left-sided heart valves. Warty projections arise from the deposition, while subendothelial lesions may induce irregular thickenings called MacCallum plaques.
Chronic rheumatic heart disease is characterized by repeated inflammation with fibrinous resolution. The cardinal anatomic changes of the valve include leaflet thickening,

commissural fusion and shortening and thickening of the tendinous cords. RHD cause 99% of mitral stenosis often resulting in a “fish mouth” gross appearance.[7]
[edit] TreatmentThe management of acute rheumatic fever is geared toward the reduction of inflammation with anti-inflammatory medications such as aspirin or corticosteroids. Individuals with positive cultures for strep throat should also be treated with antibiotics. Another important cornerstone in treating rheumatic fever includes the continuous use of low dose antibiotics (such as penicillin, sulfadiazine, or erythromycin) to prevent recurrence.
[edit] Infection
Patients with positive cultures for streptococcus pyogenes should be treated with penicillin as long as allergy is not present. This treatment will not alter the course of the acute disease.
[edit] Inflammation
Patients with significant symptoms may require corticosteroids. Salicylates are useful for pain.
[edit] Heart failure
Some patients develop significant carditis which manifests as congestive heart failure. This requires the usual treatment for heart failure: diuretics and digoxin. Unlike normal heart failure, rheumatic heart failure responds well to corticosteroids.
[edit] PreventionPrevention of recurrence is achieved by eradicating the acute infection and prophylaxis with antibiotics. The American Heart Association recommends prophylaxis continue at least 10 years.
Nurses also have a role in prevention, primarily in screening school-aged children for sore throats that may be caused by Group A streptococci(especially Group A β Hemolytic Streptococcus pyogenes).