rheumatic fever
-
Upload
kapil-dhital -
Category
Documents
-
view
11.729 -
download
2
Transcript of rheumatic fever

RheumaticRheumatic feverfever

Rheumatic fever bacterial infection affecting joints, heart and blood vessels;febrile disease occurring as a delayed sequela of infections with group A hemolytic streptococci and characterized by multiple focal inflammatory lesions of the connective tissue structures, especially of the heart, blood vessels, and joints (polyarthritis), and by the presence of Aschoff bodies in the myocardium and skin; a severe disease chiefly of children and characterized by painful inflammation of the joints and frequently damage to the heart valves.

The Etiology RF only develops in children and adolescents following GABHS pharyngitis, and only infections of the pharynx initiate or reactivate RF.
At least some rheumatogenic strains of GAS have antigenic domains similar to antigens in components of the human heart, and some authors have proposed that anti-M antibodies against the streptococci may cross-react with heart tissue, causing the pancarditis that is observed in RF. So-called molecular mimicry between streptococcal and human proteins is felt to involve both the B and T cells of peripheral blood, with infiltration of the heart by T cells. Some believe that an increased production of inflammatory cytokines is the final mechanism of the autoimmune reaction that causes damage to cardiac tissue in RHD. An insufficiency of interleukin-4 (IL-4)–producing cells in the valve tissue may also contribute to the valve lesions.
Streptococcal antigens, which are structurally similar to those in the heart, include hyaluronate in the bacterial capsule, cell wall polysaccharides (similar to glycoproteins in heart valves), and membrane antigens that share epitopes with the sarcolemma and smooth muscle.

Who is at risk for rheumatic fever?
Fewer than 0.3% of people who have strep throat also get rheumatic fever. Rheumatic fever is most common among children aged 5 to 15, but adults may have the condition as well. Doctors think that a weakened immune system may make some people more likely to get rheumatic fever. And, although antibiotic medicines have reduced the number of cases of rheumatic fever in developed countries, there are still thousands of reported cases.

Types of Rheumatic fever:Subtypes of Rheumatic fever: Acute rheumatic fever, Chronic rheumatic fever Parent types of Rheumatic fever: Group A Streptococcal Infections, Rheumatic conditions, Blood vessel conditions, Heart conditions, Bacterial diseases
Organs Affected by Rheumatic fever: joints, heart, blood vessels
Patient Profile for Rheumatic fever: Mostly children and teens; typically children 5-15
Deaths for Rheumatic fever: 3,767 deaths reported in USA 1999 for acute rheumatic fever and chronic rheumatic conditions (NVSR Sep 2001)

Diagnosis methods for rheumatic fever
There are no specific tests to diagnose rheumatic fever. Instead, physicians rely on a constellation of symptoms that may appear following an infection with streptococcus bacteria. Over time, a model has been developed to help guide physicians while diagnosing rheumatic fever. A diagnosis can be made if a patient has two major manifestations, or one major and two minor manifestations.

Signs of the condition that may be identified by a physician include: Carditis. Approximately 50 percent of patients show this
swelling of the heart walls. Damage to a valve and/or chordae, which attach the valve to the heart wall, will mostly affect the mitral valve or aortic valve.

Aortic valve showing active valvulitis. The valve is slightly thickened and displays
small vegetations – "verrucae"

Chest radiograph of an 8 year old patient with acute carditis
before treatment

Same patient after 4 weeks

Signs of the condition that may be identified by a physician include:
Chorea. Occurring in about 20 percent of cases, chorea is a rheumatic inflammation in the central nervous system. Surprisingly, this condition, which can bring rapid involuntary movements, may not begin until more than 90 days after the onset of the initial streptococcal infection.
Lumps under the skin (subcutaneous nodules).

Subcutaneous nodule on the extensor surface of elbow of a patient
with acute RF

Erythema marginatum on the trunk, showing erythematous lesions with pale centers and rounded or serpiginous
margins

Closer view of erythema marginatum in the same patient

Guidelines for the diagnosis of initial attack of rheumatic fever
(Jones Criteria, 1992 Update)
Major manifestations: Carditis; Fever; Polyarthritis; Arthralgia; Sydenham’s chorea
Minor manifestations Elevated acute phase reactants; Erythema marginatum; Prolonged PR interval; Subcutaneous nodules

The major manifestations The major manifestations ((Jones criteriaJones criteria)) include:include:
Carditis. Carditis may be detected during a physical examination if the physician hears a valvular murmur while listening to the heart through a stethoscope. Heart damage may also be identified with an echocardiogram (a form of ultrasound imaging that takes pictures of the heart’s structures and functions) or with an electrocardiogram (a test that measures the heart’s electrical activity).

The major manifestations include:The major manifestations include:
Arthritis in the joints.
Chorea. This describes inflammation of the central nervous system.
Rash (Erytema marginatum).
Lumps under the skin (subcutaneous nodules).

The minor manifestations include:The minor manifestations include:
Fever
Arthralgia
Elevated acute phase reactants
Prolonged PR interval
There is some evidence that a test for C-reactive protein (CRP) may also help physicians diagnose rheumatic fever. Because rheumatic fever is an inflammatory disease, blood levels of C-reactive protein are abnormal during the rheumatic process.

Signs and symptoms of rheumatic fever
Swelling, tenderness and arthritis-like pain in several larger joints (polyarthritis) Migratory arthritis that travels from one joint to another Rash Difficulty with speech Fatigue Lack of appetite Abdominal pain Nosebleeds Fever

Other clinical manifestationsAbdominal pain: Abdominal pain usually occurs at the onset of acute RF, resembles other conditions with acute microvascular mesenteric inflammation, and may mimic acute appendicitis. Arthralgias: Patients may report arthralgias upon presentation. In the history, determining if the patient has taken aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) is important because these may suppress the full manifestations of the disease. Arthralgia cannot be considered a minor manifestation if arthritis is present. Epistaxis: Epistaxis may be associated with severe protracted rheumatic carditis. Fever: Fevers greater than 39°C with no characteristic pattern are present initially in almost every patient with acute RF. The fever may be low grade (38.0-38.5°C) in children with mild carditis or absent in patients with pure chorea. The fever decreases without antipyretic therapy in approximately 1 week, but low-grade fevers persist for 2-3 weeks. Rheumatic pneumonia: Patients present with the same signs as an infectious pneumonia. Differentiate rheumatic pneumonia from respiratory distress related to CHF.

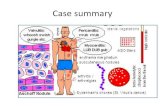
Conditions related to Conditions related to rheumatic feverrheumatic fever
Rheumatoid arthritis. Pain, inflammation and soreness in the joints. Mitral stenosis. A narrowing of the mitral valve (located between the left atrium and left ventricle), which can affect the function of the mitral valve. Pericarditis. Inflammation of the pericardium, the sac that encloses the heart. Endocarditis. Inflammation of the lining of the heart’s chambers or valves, often due to a bacterial infection. Myocarditis. Inflammation of the heart muscle. Heart failure. A serious condition in which the heart is not pumping well enough to meet the body’s demand for oxygen. It received its name because the heart is failing to pump efficiently, which often results in congestion in the lungs.

Differential diagnosis of rheumatic fever
Juvenile rheumatoid arthritisSystemic lupus erythematosus Infective endocarditis Reactive arthritis Sickle cell disease Drug reactions Other connective tissue diseases Septicaemia LeukaemiaGonoccocal arthritis Tuberculosis Lyme disease Serum sickness

Lifestyle ChangesIf rheumatic fever has led to rheumatic heart disease or damage to your heart valves, your doctor may recommend that you take antibiotic medicines continuously for many years. Some patients with rheumatic fever need to take antibiotics for the rest of their lives. In any case, you should always tell your doctor or dentist about your history of rheumatic fever before you have a surgical or dental procedure. Such procedures may cause bacteria to enter the bloodstream and infect your heart valves.

Penicillin is given to eradicate any organisms still present. In allergy to penicillin, erythromycin or a cephalosporin are recommended. Penicillin appears to be the drug of choice both in initial infection and to prevent recurrence.5 It may be more effective given by the IM route but the quality of the evidence is poor.6 For recurrent pharyngitis a second 10 days of penicillin may be given but carriage is difficult to eradicate with conventional penicillin therapy. Oral clindamycin is recommended. Aspirin usually relieves arthritis within a few days. High doses are required and other NSAID's like naproxen may be safer.7 There is no evidence that NSAIDs, steroids or immunoglobulin reduce the severity of heart disease but trials are rather old and newer methodology would be valuable.8 Heart failure will require diuretics, ACE inhibitors, and digoxin. If this fails consider cardiac surgery even in acute failure. Mitral valve repair or replacement may save the life. Chorea may be treated with haloperidol although this drug can cause extrapyramidal effects.