Respiratory
Transcript of Respiratory

Respiratory system/ Khulood Shattnawi �
Alteration in Respiratory Function in Children
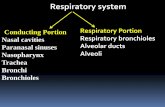
The respiratory system is made up of the organs involved in the interchanges of gases, and
consists of the nose, pharynx, larynx, trachea, bronchi, and lungs.
The upper respiratory tract includes the following: nose, nasal cavity, ethmoidal air cells, maxillary
sinus, larynx, and trachea. While the lower respiratory tract includes the following: lungs, bronchi
and alveoli.
Functions of respiratory system:
• Removal of CO2 and replacement of O2 needed for metabolism.
• Maintenance of acid-base balance (pH level).
• Maintenance of body H2O level and heat balance.
• Production of speech.
• Facilitate the sense of smell.
Respiratory differences in children:
• Tonsiller tissue is normally enlarged in early school-age.
• Respiratory mucus ( cleaning agent) :
• In newborn: is little makes them more susceptible to respiratory infections.
• Increase production of mucus up to 2 years of age lead to obstructions.
• After 2 years of age the right bronchus become shorter, wider, and more vertical than the
left bronchus, thus inhaled foreign bodies more often lodge in the right bronchus.
• Infants use their abdominal muscle for breathing, the change to thoracic begin around the
age of 2-3 years and completed at age of 7 years.
• Because accessory muscles are used more in children than in adult, weakness of these
muscles from diseases may lead to respiratory failure.
• In infants, the walls of the airways are small in size and have less cartilage than older
children and adults that’s why they are more likely to collapse after expiration.
• Infants are obligatory nasal breathers.
Assessment of Respiratory function
Information of the child’s respiratory status is obtained from observations of physical
signs and behavior. Respiration, the configuration of the chest, the pattern of respiratory movement,
including rate, regularity, symmetry of movement, depth, effort expended in respiration, and use of
accessory muscles of respiration, should be assessed. Respiration is best determined when the child is
sleeping or quietly awake.
Palpation and percussion provide information regarding areas of pain and tissue density.
Auscultation of the lung fields is helpful in identifying specific pathologies and in assessing the
child’s responses to treatment. Auscultation is essential when determining airway patency.
Noisy breathing
Noisy breathing has been described as abnormal breath sounds that are audible without the use of a
stethoscope. These sounds result from blockage of the airway anywhere along the pathway from the
nose to the bronchioles. Blockage at these points could be the result of foreign object inhalation,
inflammation, airway constriction or external compression of the airways. In general, respiratory
obstruction tends to occur more often in younger patients because the larynx is smaller in younger
infants.
Noisy breathing in a child/infant can cause great distress for the caregiver. It is a complaint that
should be investigated immediately and thoroughly.
Noisy breathing can be classified into three main types: snoring, stridor and wheezing.

Respiratory system/ Khulood Shattnawi �1. Snoring
Snoring is an abnormal breath sound that occurs while the child sleeps. Snoring is usually the
result of a partial obstruction of the upper respiratory tract that in turn causes vibration of air
as it passes through the nasopharynx and oropharynx. This obstruction may cause a child to
momentarily stop breathing during his/her sleep (sleep apnea). This sleep disturbance may
occur several times during the night and although the child may not be able to recall their
waking, sleep apnea can lead to fatigue and irritability throughout the day.
2. Stridor Stridor is a harsh, continuous, crowing sound that is caused by variable airway obstruction
that is an obstruction which blocks flow in one direction but not the other. Most commonly,
stridor occurs on inspiration and is caused by an extrathoracic variable airway obstruction.
Expiratory stridor can also be heard however this sound results from an intrathoracic variable
airway obstruction. It should be noted that an expiratory stridor may often resemble a wheeze.
A Biphasic stridor implies midtracheal involvement. If stridor occurs with hoarseness then an
obstruction of the larynx is indicated.
An acute onset of nocturnal stridor combined with a barky cough and hoarse voice should
point you towards croup. On the other hand, a chronic stridor from early infancy indicates an
underlying congenital abnormality.
3. Wheeze A wheeze is a continuous sound that is mainly heard on expiration. It indicates an
intrathoracic airway obstruction, resulting from dynamic compression of the bronchi.
Wheezing can be accompanied by feelings of tightness in the chest and labored breathing. It
is important to distinguish wheezing (a sound heard on expiration) from stridor (a sound
heard primarily on inspiration). Although anything that causes compression of the airways
can potentially cause wheezing, however in most cases wheezing is caused by asthma.
Specific questions should therefore be asked about environmental factors (grass, pollen,
trees), factors within the home (inhalants, moldy basements, dusty areas, sprays, perfumes,
parents occupation), school-related factors (dust, chalk) and pets. You should also ask about
family history, and whether the child or family members smoke.
**Remember, a child can start smoking at an early age, and will not feel comfortable telling
you this while parents are present.**
Children who are having difficult time breathing often show signs that they are not getting
enough oxygen, indicating respiratory distress. It is important to learn the signs of respiratory
distress to know how to respond appropriately.
Signs of respiratory distress:
•••• Breathing rate: An increase in the number of breaths per minute, usually > 60 breath/minute
in infants.
•••• Retractions: The chest appears to sink with each breath - one way of trying to bring more air
into the lungs. In severe airway obstruction, retraction becomes extreme. Subcostal retraction,
observed anteriorly at the lower costal margins, indicates a flattened diaphragm, since it not
only lowers the floor of the thorax, but also pulls on the rib cage in response to a greater than
normal decrease in intrathoracic pressure. In severe obstruction, retractions extend to the
supraclavicular areas and the suprasternal notch.
• Color changes: cyanosis seen around the mouth, on the inside of the lips, or on the
fingernails may occur when a person is not getting as much oxygen as needed. Cyanosis
become apparent when PaO2 is lower than 40 mmHg, or with increased of unoxygenated
level of hemoglobin (Hgb). The color of the skin may also appear pale or gray.
• Grunting: A grunting sound can be heard each time that the child exhales. This grunting is
the body's way of trying to keep air in the lungs so they will stay open. Grunting is frequently

Respiratory system/ Khulood Shattnawi �a sign of chest pain, suggesting acute pneumonia or pleural
involvement. It is also observed in pulmonary edema and is
a characteristic of respiratory distress syndrome.
• Nasal flaring: It is a sign of respiratory distress and a very
significant finding in an infant.
The openings of the nose spreading open while breathing
may indicate that a child is having to work harder to
breathe. The enlargement of the nostrils helps reduce nasal
resistance and maintain airway patency.
• Wheezing: A tight, whistling or musical sound heard with
each breath may indicate that the air passages may be
smaller, making it more difficult to breathe. Other abnormal
lung sounds that could be heard are rales (or crackles: short,
popping; sudden inflation of alveoli), ronchi (or gurgles:
continuous rattle; fluid in large airways) and pleural friction
rub (grating, leathery; inflamed pleura).
Associated observations:
• Cough, sound of coughing is caused by rapid expiration
past the glottis. Cough serves as a protective mechanism,
initiated by stimulation of the nerves of the respiratory tract
mucosa by the presence of dust, chemicals, mucus, or
inflammation. It is a useful procedure to
clear excess mucus or foreign bodies, but
becomes harmful and needs suppression
when there is no mucus or debris to be
expelled. Paroxysmal coughing is a series of
expiratory coughs after a deep inspiration (as
in case of pertussis), continuous coughing
increases the chest pressure, which cause the
venous return to heart to be decreased
(decreased cardiac output), that may lead to
fainting.
A cough is most often a symptom of lower respiratory disease, but can arise from a variety of
central nervous, pulmonary, and nonpulmonary origins (e.g., congenital heart disease). Asthma and
respiratory infections, usually viral, are the cause in most cases, but cystic fibrosis and psychological
problems are significant causes in older children. Ask the patient or parent for as much information
about the cough as possible, emphasizing the following points:
1. Quality of cough. It is extremely important to characterize the sound of the cough, since
certain diseases produce very distinctive coughs. Although it can be very helpful to obtain and
examine a sample of any sputum that is produced, infants and younger children usually
swallow sputum since they have generally not yet learned to spit. Determination of whether
the cough is productive or not can therefore be based on whether the cough sounds ‘dry’
(nonproductive) or ‘loose’ (productive).
2. Timing and duration of cough. A variety of timing patterns can provide clues as to the
origin of the cough. Ask about the cough’s occurrence with feeding, at night, in early
morning, and seasonal variations. Also determine whether the cough is of an acute or chronic
nature, the latter usually having lasted more than 3 to 4 weeks. Among those coughs that are
chronic, distinguishing between recurrent and persistent coughs may help to narrow the
differential diagnosis by pointing to relevant triggers or the possibility of recurrent infections.

Respiratory system/ Khulood Shattnawi �3. Aggravating factors. Certain stimuli can often be pin-pointed as cough-inducing factors.
Possibilities range from known infection, exercise, cigarette smoke, and weather changes (e.g.
cold air), to laughing, crying, or the presence of allergens. Environmental irritants associated
with molds on walls, air pollution, exhaust fumes, and wood-fire smoke should also be noted.
4. Associated clinical findings. Cough can present in association with several related signs and
symptoms. Be sure to obtain information regarding fever, hemoptysis, stridor, wheezing and
chest pain.
5. History. Evidence of a patient or family history of conditions such as asthma, eczema,
urticaria, or allergic rhinitis suggests a potential allergic
etiology.
• Clubbing: proliferation of tissue about the terminal phalanges,
accompanies a variety of conditions, frequently those associated with
chronic hypoxia, primarily cardiac defects and chronic pulmonary
disease. The change of the angle of the nail to the fingertip is occur
because of the increase of capillary growth in the fingertips, which
occur as the body attempts to supply more oxygen to the distal body
cells.
• Restlessness and apprehension: when children or infants have difficulty securing adequate
oxygen (hypoxia), they become anxious and restless. Restlessness and tachypnea in infants
are the first signs of airway obstruction.
• Increasing use of accessory muscles of respiration.
Diagnostic Procedures
Several procedures are available for assessing respiratory function and diagnosing respiratory
disease. All of these procedures require preparation and support of the child and the family to ensure
cooperation and accurate results. These procedures not only are useful in diagnosis, but also provide
information that guide nursing interventions, such as positioning, use of supplemental oxygen, and
assistance with coughing or deep breathing.
• Pulmonary function tests: noninvasive pulmonary mechanics are often measured at the
bedside of infants and children with the use of spirometry, a device that records the air exchange.
These tests are useful to evaluate the severity and course of a disease and to study the effects of
treatment. Pulmonary function tests used in children are:
• Forced vital capacity (FVC): maximum amount of air that can be expired
after maximum inspiration.
• Forced expiratory volume in 1 (FEV1) or 3 (FEV3) seconds: amount of air
that can be forced from lungs after maximum inspiration in 1 and 3 seconds.
• Tidal volume (TV): amount of air inhaled and exhaled during any respiratory
cycle.
• Functional residual volume (FRV); Functional residual capacity (FRC):
volume of air remaining in lungs after passive expiration.
• Radiologic examination:
• Radiography: x-rays produces images of internal structures of chest, including
air-filled lungs, airways, vascular marking, hearts, and great vessels.
• Bronchography: contrast medium is instilled directly into bronchial tree
through opaque catheter inserted via orotracheal tube. Detects distal bronchial
obstructions and malformations. Carried out with child under general anesthesia or
sedation
• Computed tomography (CT): sequence of x-rays, each representing a cross
section through lung tissue at different depth. Useful in identifying presence of
calcium or a cavity within a lesion, adenopathy, masses, or abnormalities.

Respiratory system/ Khulood Shattnawi �
• Magnetic resonance imaging (MRI): use of large magnet and radio waves to produce two or
three-dimensional image. It clearly identifies soft tissues, and requires cooperation or
sedation of child.
• Angiography: injection of dye to produce image of pulmonary vasculature. It
investigates pulmonary vascular anomalies and pulmonary hypertension. Performed
with child under general anesthesia.
• Other diagnostic procedures:
• Tracheal aspiration: sputum obtained by direct aspiration from trachea for examination
and culture.
• Bronchoscopy: direct observation of tracheobronchial tree via bronchoscope.
• Lung puncture: needle aspiration of lung fluid via syringe and needle through intercostal
space for histologic study or culture.
• Lung biopsy: removal of lung tissue via open thoracotomy or closed-needle procedures.
Used for diagnosis of protracted pulmonary disease unexplained by other means.
• Blood gas determination: blood gas measurements are sensitive indicators of change in
respiratory status in acutely ill patients. They provide valuable information regarding lung
function, lung adequacy, and tissue perfusion and are essential for monitoring conditions
involving hypoxemia, CO2 retention, and PH.
• Pulse oximetry: provides a continuous or intermittent noninvasive method of
determining O2 saturation (SaO2).
• Arterial blood gas (ABG) sampling: may be performed on blood from an artery
or a capillary. The blood samples are obtained by taking a deep heel stick after
dilation of the vascular bed by warming, or through an indwelling catheter
(arterial line) or by arteriopuncture. Although ABG values are similar for children
and adults, neonates can have slightly lower values and still be considered
normal. The significance of ABG determination is related primarily to the
relationships among three parameters: pH, Po2, and Pco2. Any change in a blood
gas value must be compared with the other values and with previous readings, as
well as with the child’s clinical appearance and behavior, medical history, and
associated physiologic factors. Clinical indicators for blood gas analysis include
changes in color, depth or rate of respiration, behavior, and vital signs.
Common Therapeutic Techniques used in the Treatment of Respiratory Illness in Children
• Oxygen therapy: the indication of administration of O2 is hypoxemia. O2 is delivered by
mask, nasal cannula, tent, hood, face tent, or ventilator. The mode of delivery is selected on the
basis of the concentration needed and the child’s ability to cooperate in its use. The concentration
of O2 delivered should be regulated according to the individual child’s needs. There are hazards
related to its use; therefore O2 should be continued only as long as needed (oxygen is a drug and
should not be administered or adjusted without a doctor's order, and is only administered as prescribed by dose, typically in liters per minute). Humidification of the gas before
administration to the patient is essential.
• Aerosol therapy: using the airway as the route of administration can be useful in avoiding
the systemic side effects of certain drugs and in reducing the amount of drug necessary to achieve
the desired effect. Medications can be aerosolized or nebulized with air or with O2-enriched gas.
Hand-held nebulizers are frequently used. The medicated mist is discharged into a small plastic
mask, which the child holds over the nose and mouth. To avoid particle deposition in the nose
and pharynx, the child is instructed to take slow, deep breaths through an open mouth during
treatment. The metered dose inhaler (MDI) is a self-contained, hand-held device that allows for
intermittent delivery of a specified amount of medication. Many bronchodilators are available in
this form. A major nursing responsibility during aerosol therapy is to assess the effectiveness of
the treatment and the patient’s tolerance of the procedure. Assessment of breath sounds and work
of breathing should be performed before and after treatment.

Respiratory system/ Khulood Shattnawi �
• Postural (Bronchial) drainage: is indicated whenever normal ciliary activity and cough are
not removing excessive fluid or mucus in the bronchi. Positioning the child to take maximum
advantage of gravity facilitate removal of secretions. Postural drainage is most effective in
children with chronic lung disease characterized by thick mucus secretions, such as cystic
fibrosis. Postural drainage is carried out three to four times daily and is more effective when it
follows other respiratory therapy, such as bronchodilator and/or nebulization medication.
Bronchial drainage is generally performed before meals (or 1-1½ hours after meals) to minimize
the chance of vomiting and repeated at bedtime. The length and duration of treatment depend on
the child’s condition and tolerance level-usually 20-30 minutes. There are positions to facilitate
drainage from all major lung segments, but all positions are not used at each session. Children
will usually cooperate for four to six positions, but more than six tend to exceed their limits of
tolerance.
• Chest Physiotherapy (CPT): CPT usually refers to the use of postural drainage in
combination with adjunctive techniques that are thought to enhance the clearance of mucus from
the airway.
• Percussion: The most common technique used in association with postural
drainage is manual percussion of the chest wall. The patient is dressed in a light
shirt and placed in a postural drainage position. The nurse then gently but firmly
strikes the chest wall with a cupped hand. A “popping” hollow sound (not a
slapping sound) should be the result. Percussion should be done over the rib cage
only and should be painless. Percussion can be performed with a soft, circular
mask.
• Vibration: can be used to help move secretions during exhalations. Hand-held
vibrators should be approved for use in an O2-enriched environment (tent, head
hood). CPT is contraindicated when patients have pulmonary hemorrhage,
pulmonary embolism, end-stage renal disease, or increased intracranial pressure.
• Deep breathing: is often encouraged when the child is relaxed and in the
desired position for drainage. The child is directed to take several deep breaths
using diaphragmatic breathing. The use of deep breathing enlarges the
tracheobronchial tree, enabling air to circulate around and through secretions that
are not affected by usual tidal volume. Expirations after these deep breaths often
carry secretions and may stimulate a cough. Other methods that can be employed
to stimulate deep breathing are the use of blow method that extends the expiratory
time and increases expiratory pressure. For example, play may include blowing
pinwheel toys, moving small items by blowing through a straw, blowing up
balloons, singing loudly, or blowing soap bubbles.
• Coughing exercise: with or without stimulation, children are also encouraged
to cough one or two hard coughs after a deep breath are efficient.
• Tracheostomy: consist of surgical opening in the trachea between the second and fourth
tracheal rings. It may be required in an emergency situation for epiglottitis, croup, or foreign
body aspiration. These tracheostomies remain in place for a short time. An infant or child
requiring long-term ventilatory support may also have a tracheostomy. Children who have
undergone a tracheostomy must be closely monitored for complications such as hemorrhage,
edema, aspiration, accidental decannulation, tube obstruction, and the entrance of free air into the
pleural cavity. The focus of nursing care is maintaining a patent airway, facilitating the removal
of pulmonary secretions, providing humidified air or O2, cleansing the stoma, monitoring the
child’s ability to swallow, and teaching while simultaneously preventing complications.

Respiratory system/ Khulood Shattnawi �Respiratory dysfunction:
• Upper respiratory tract infections:
– Otitis media (OM)
– Croup (Laryngotracheobronchitis (LTB))
– Epiglottitis
• Lower respiratory tract infections:
– Acute Bronchitis
– Bronchiolitis/ Respiratory Syncytial Virus (RSV)
– Pneumonia
• Long-term respiratory dysfunction:
– Asthma
– Cystic fibrosis (CF)
• Conditions caused by physical defects:
– Esophageal atresia and tracheoesophageal fistula
– Diaphragmatic hernia
UPPER RESPIRATORY TRACT INFECTIONS (URTI)
Otitis media (OM)
OM is one of the most prevalent diseases of early childhood. Approximately 70% of children
have had at least one episode and 33% have had three or more episodes by 3 years of age. The
incidence is highest in children ages 6 months to 2 years; it then decreases with age.
Acute OM is frequently caused by Streptococcus pneumoniae or Haemophilus influenza. The
etiology of the noninfectious type is unknown, although it is frequently the result of blocked
Eustachian tubes from the edema of URIs, allergic rhinitis, or hypertropic adenoids. Passive smoking
has been established as a significant factor in the development of OM. A relationship has been
observed between the incidence of OM and infant feeding methods. Infants fed breast milk have
lower incidence of OM compared with formula-fed infants. Beside the protective effects of breast
milk, reflux of milk up the eustachian tubes is less likely in breast-fed infants because of the
semivertical positioning during breast-feeding compared with bottle-feeding. There is a definite link
between the supine position during feeding and the reflux of fluid into the middle ear.
Mechanical or functional obstruction of the Eustachian tube causes accumulation of
secretions in the middle ear. Drainage is inhibited by sustained negative pressure and impaired ciliary
transport within the tube.
Complications: the consequences of prolonged middle ear disorders can be either functional or
structural. The principal functional consequence is hearing loss, although loss in most children is
conductive in nature and mild in severity. The causes of hearing loss are negative middle ear
pressure, the presence of effusion in the middle ear, or structural damage to the tympanic membrane.
However, the most feared consequence of hearing loss is its adverse effect on development of speech,
language, and cognition.
Structural complications involve primarily the tympanic membrane. Tympanic membrane
retraction occurs when continued negative middle ear pressure draws the tympanic membrane
inward. This retraction may result in impaired sound transmission, perforation of the thinned-out
areas, or infection.
Clinical manifestations:
As purulent fluid accumulates in the small space of the middle ear chamber, pain results from
the pressure on surrounding structures. Infants become irritable and indicate their discomfort by
holding or pulling at their ears and rolling their head from side to side. A temperature as high as 40 ْC
is common, and postauricular and cervical lymph glands may be enlarged. Rhinorrhea, vomiting, and
diarrhea, as well as signs of concurrent respiratory or pharyngeal infection, may also be present. Loss
of appetite typically occurs, and sucking or chewing tends to aggravate the pain. In children with OM

Respiratory system/ Khulood Shattnawi �with effusion exudates will accumulate and pressure will increase, with the potential for tympanic
membrane rupture. As a result of rupture, there is immediate relief of pain, a gradual decrease in
temperature, and the presence of purulent discharge in the external auditory canal.
In acute OM, otoscope reveals an intact membrane that appears bright red and bulging, with
no visible landmarks or light reflex. The usual landmarks of the bony prominence from the long and
the short process of the malleus are obscured by the outwardly bulging membrane. Diagnosis is
usually based on clinical manifestations, but if purulent discharge is present, it should be cultured and
a specific antibiotic chosen for that organism.
Treatment of acute OM involves a variety of antibiotics such as amoxicillin, sulfonamides,
erythromycin-sulfisoxazole, and cephalosporins (such as cefixime (suprax), Cefzil). For fever or
discomfort associated with OM, analgesic/antipyretic drugs such as acetaminophen or ibuprofen may
be given. Antihistamines, decongestants, or ear drops are not recommended. Children should be seen
after antibiotic therapy is complete to evaluate the effectiveness of the treatment and to identify
potential complications, such as effusion or hearing impairment.
Other treatments may include tympanostomy tubes where tiny tubes are inserted during a
relatively simple operation (myringotomy), allow the pressure to equalize on either side of the
eardrum by allowing free drainage of the fluid.
Nursing considerations:
Nursing objectives for the child with OM include (1) relieving pain, (2) facilitating drainage
when possible, (3) preventing complications or recurrence, (4) educating the family in care of the
child, and (5) providing emotional support to the child and family.
Analgesic are helpful to reduce severe earache. High fever should be reduced with antipyretic
drugs. If the ear is draining, the external canal may be cleansed with sterile cotton swabs soaked in
hydrogen peroxide.
Parents require anticipatory guidance regarding temporary hearing loss that accompanies OM
(they may need to speak louder, at closer proximity), and possible behavioral changes with hearing
loss.
Preventing recurrence requires adequate parent education regarding antibiotic therapy. Nurses
must emphasize that although the child may appear well in a couple of days, the infection is not
completely eradicated until all of the prescribed medication is taken (7-10 days). It is important to
stress the potential complications of OM, especially hearing loss, which can be prevented with
adequate treatment and follow-up care.
Croup (Laryngotracheobronchitis (LTB)):
LTB is one of the most frightening diseases of early childhood and primarily affects children
less than 5 years of age (peaks between 6 months and 3 years). The cause is usually viral, organisms
responsible for LTB are the parainfluenza virus (most common one), respiratory syncytial virus
(RSV), influenza A and B, and Mycoplasma pneumoniae. The disease is usually preceded by a URI,

Respiratory system/ Khulood Shattnawi which gradually descends to adjacent structures. It is characterized by the gradual onset of low-
grade fever.
Inflammation of the mucosa lining the larynx and trachea causes a narrowing of the airway.
When the airway is significantly narrowed, the child struggles to inhale air past the obstruction and
into the lungs, producing the characteristic inspiratory stridor and suprasternal retractions; other
classic manifestations include barking cough and hoarseness. The child may be in slight to
moderate respiratory distress, with mild wheezing and a low-grade fever. When the child is unable to
inhale a sufficient volume of air, symptoms of hypoxia become evident. As the work of forcing air
past the obstruction increases, negative pressure generated in the thoracic cavity also increases,
leading to leakage of pulmonary vascular fluid into interstitial spaces and causing uneven ventilation
and hypoxia. Obstruction severe enough to prevent adequate exhalation of carbon dioxide causes
respiratory acidosis, and respiratory failure.
Therapeutic management:
The major objective in medical management of infectious LTB is maintaining an airway and
providing for adequate respiratory exchange. Children with mild croup (no stridor at rest) are
managed at home. Parents are taught the signs of respiratory distress. High humidity with cool mist
provides relief for most children. A cool-air vaporizer can be used at home. In the hospital setting,
hoods for infants or mist tents for toddlers may be used to provide increased humidity and
supplemental oxygen.
The cool-temperature therapy modalities assist by constricting edematous blood vessels. In
the home environment, suggestions to provide cool air include taking the child outside to breathe in
cool night air, use of a cold-water vaporizer or humidifier, and standing in front of the open freezer. It
is also essential to allow children with mild croup to continue to drink encourage they like and to
encourage parents to use comforting measures with their child. If the child is unable to take oral
fluids, IV fluid therapy might be indicated. Children with severe respiratory distress (respiratory rate
more than 60 breaths/min for infants) should NOT be given anything by mouth to prevent aspiration
and decrease the work of breathing.
Nebulized epinephrine (5ml of 1:1000, cause mucosal vasoconstriction and subsequent
decreases subglottic edema) is often used in children with more severe disease, stridor at rest,
retractions, or difficulty breathing. The use of corticosteroids ( dexamethasone 0.6 mg/kg/dose IM
injection) is beneficial because the anti-inflammatory effects decrease subglottic edema. Intubation is
indicated in severe cases.
Nursing considerations:
The most important nursing function is continuous observation and accurate assessment of
respiratory status. Intubation equipment should be readily accessible at the bedside so that it can be
implemented whenever the nurse recognizes signs of impending respiratory failure. Early signs of
impending airway obstruction include increased pulse and respiratory rate; substernal, suprasternal,
and intercostal retractions; flaring nares; and increased restlessness.
Laryngo spasm with total occlusion of the airway may occur when child’s gag reflex is
elicited, or when the child is crying. It is important to comfort the child and do not elicit gag reflex
(DON’T GAG CHILD WITH TONGUE BLADE).
Epiglottitis
Acute epiglottitis is a serious obstructive inflammatory process that occurs principally in
children between 2 and 6 years of age but can occur from infancy to adulthood. The disorder requires
immediate attention. The responsible organism is usually Haemophilus influenzae.
The onset of epiglottitis is abrupt, less often preceded by cold symptoms and more often by a
sore throat, and it can rapidly progress to severe respiratory distress. The child usually goes to bed
asymptomatic to awaken later, complaining of sore throat and pain on swallowing. The child has a
fever, muffled voice, stridor, appears sicker than clinical findings suggest, and usually exhibits the
following behaviors: the child insists on sitting upright and leaning forward, with the chin thrust out,

Respiratory system/ Khulood Shattnawi �mouth open, and tongue protruding. Drooling of saliva is common because of the difficulty or
pain in swallowing and excessive secretions.
The child is irritable and extremely restless and has an anxious and frightened expression.
Suprasternal and substernal retractions may be visible. The pale color of mild hypoxia may progress
to frank cyanosis. The throat is red and inflamed, and a distinctive, large, cherry red, edematous
epiglottis is visible on careful throat inspection. Throat inspection should be attempted only when
immediate intubation can be performed if needed.
Therapeutic management:
In epiglottitis, obstruction appears suddenly. Progressive obstruction leads to hypoxia
(decreased O2 supply to tissue), hypercapnia (excess CO2 in blood), and acidosis followed by
decreases muscular tone, reduced level of consciousness and, when obstruction becomes more or less
complete, a rather sudden death.
Endotracheal intubation or tracheostomy is usually considered for the child with H.
influenzae epiglottits with severe respiratory distress. The epiglottal swelling usually decreases after
24 hours of antibiotic therapy, and the epiglottis is near normal by the third day. Children with
suspected bacterial epiglottitis are given antibiotics intravenously, followed by oral administration to
complete a 7- to 10-day course. The use of corticosteroids for reducing edema may be beneficial
during the early hours of treatment. Intravenous (IV) fluids, until the child can swallow again is
essential.
Nursing considerations:
It is important for the nurse to act quickly but calmly and provide support without increasing
anxiety. The child is allowed to remain in the position that provides the most comfort and security
and parents are reassured that everything possible is being done to obtain relief for their child. Nurses
who suspect epiglottitis should not attempt to visualize the epiglottis directly with a tongue depressor
or take a throat culture but should refer the child to a physician immediately. Continuous monitoring
of respiratory status, including blood gases, is part of nursing observations, and the IV infusion is
maintained.
Croup Epiglottitis
Age 6mo-3yr 2yr-6yr
Season Fall/winter Anytime
Worst s/s Night & am 24hours
History URI, gradual onset Sudden onset, no URI
Fever
Drooling
Cough
Position
Stridor
Voice
Low-grade
No
Yes
Sitting, lying
Inspir/Expir
Hoarse
Med-high
Yes
No
Tripod sit
Inspir
Muffled

Respiratory system/ Khulood Shattnawi ��
INFECTIONS OF THE LOWER AIRWAYS
Acute Bronchitis:
Bronchitis is an inflammation of the large airways (trachea and bronchi), which is frequently
associated with URI. Although there are several different types of bronchitis, the two most common
are acute and chronic (primarily affects adults). Acute bronchitis is the inflammation of mucous
membranes of the bronchial tubes. Viral agents usually cause this disease, although Mycoplasma
pneumoniae is a common cause in children older than 6 years of age. It may also be caused by
physical or chemical agents - dusts, allergens, strong fumes, and those from chemical cleaning
compounds, or tobacco smoke. (Acute asthmatic bronchitis may happen as the result of an asthma
attack, or it may be the cause of an asthma attack.).
Bronchitis is a mild, self-limiting disease that requires only symptomatic treatment, including
analgesics, antipyretics, and humidity. Cough suppressants may be useful to allow rest but can
interfere with clearance of secretions. Most patients recover in 5 to 10 days.
Bronchiolitis/ Respiratory Syncytial Virus (RSV):
Bronchiolitis is an infection of the lower respiratory tract that usually affects infants (rare in
children over 2 years of age). There is swelling in the smaller airways or bronchioles of the lung,
which causes obstruction of air in the smaller airways. The infection occurs primarily in winter and
spring. The most common cause of bronchiolitis is a virus, which is most frequently the respiratory
syncytial virus (RSV) (50% of cases). However, many other viruses may be involved, including
parainfluenza virus, adenovirus, and rhinovirus. Some bacteria can also cause bronchiolitis; these
include mycoplasma pneumoniae and chlamydia pneumoniae.
Initially, the virus causes an infection in the upper respiratory tract, and then spreads
downward into the lower tract. RSV affects the epithelial cells of the respiratory tract. The virus
causes inflammation and even death of the cells inside the respiratory tract. The bronchiole mucosa
swell and lumina are subsequently filled with mucus and exudate. The walls of the bronchi and
bronchioles are infiltrated with inflammatory cells. This leads to obstruction of airflow in and out of
the child's lungs. Dilation of bronchial passages on inspiration allows sufficient space for intake of
air, but narrowing of the passages on expiration prevents air from leaving the lungs. Thus air is
trapped distal to the obstruction and causes progressive overinflation (emphysema).
Clinical manifestations:
The younger the infant, the greater the likelihood that severe lower respiratory tract disease
requiring hospitalization will occur. The peak incidence for RSV is 2 to 5 months of age, but
reinfection with RSV is extraordinarily common at all ages, with the highest rates being reported
from daycare centers. The illness usually begins with URI after an incubation of about 5 to 8 days.
Symptoms such as rhinorrhea and low-grade fever often appear first. Otitis media and
conjunctivitis may also be present. In time, a cough may develop. If the disease progresses, it
becomes a lower respiratory tract infection and manifests typical symptoms, which are:
Initial symptoms:
• Rhinorrhea.
• Pharyngitis.
• Coughing/sneezing.
• Wheezing.
• Possible ear or eye infection.
• Intermittent fever.
With progression of illness:
• Increased coughing and wheezing.
• Air hunger.
• Tachypnea and retractions.
• Cyanosis.

Respiratory system/ Khulood Shattnawi ��Severe illness:
• Tachypnea > 70 breaths/min.
• Listlessness.
• Apneic spells.
• Poor air exchange; poor breath sounds.
With infants there may be several days of URI symptoms or no symptoms except slight lethargy,
poor feeding, or irritability.
Therapeutic management:
Bronchiolitis is treated symptomatically with high humidity, adequate fluid intake, rest, and
medications. Most children with bronchiolitis can be managed at home. The child who is tachypneic,
has marked retractions, seems listless, or has a history of poor fluid intake should be admitted. Mist
therapy is generally combined with oxygen by hood or tent in concentrations sufficient to alleviate
dyspnea and hypoxia, after which mist alone is continued for mild dyspnea. Fluids by mouth may be
contraindicated because of tachypnea, weakness, and fatigue; therefore, IV fluids are preferred until
the acute stage of the disease has passed.
Medical therapy for bronchiolitis is controversial. Bronchodilators, corticosteroids, cough
suppressants, and antibiotics have not proved to be effective in uncomplicated disease and are not
recommended for routine use. Corticosteroids, theophylline, and furosemide have all been used for
intubated and ventilated infants and children. Ribavirin, an antiviral agent may be used to treat RSV.
Pneumonia Pneumonia is an inflammation of the pulmonary parenchyma caused by bacteria, viruses, or chemical
irritants. It is a serious infection or inflammation in which the air sacs fill with exudate. Clinically,
pneumonia may occur either as a primary disease or as a complication of another illness. Pneumonia
can occur year round, but is usually seen in the winter and spring. Boys are affected by pneumonia
more often than girls. There is an increased chance of developing pneumonia in a crowded area. Ten
to 15 percent of children with a respiratory infection have pneumonia.
Types of pneumonia:
• Lobar pneumonia - affects one or more lobes of the lungs.
• Bronchial pneumonia (or bronchopneumonia) – begins in the terminal
bronchioles, which become clogged with mucopurulent exudate to form
consolidated patches throughout both lungs; also called lobular pneumonia.
• Interstitial pneumonia – the inflammatory process is more or less confined
within the alveolar walls and the peribronchial and interlobular tissues.
Viral Pneumonia Viral pneumonia is caused by various viruses, including respiratory syncytial virus (most commonly
seen in children under age 5), parainfluenza virus, influenza virus, adenovirus. Early symptoms of
viral pneumonia are the same as those of bacterial pneumonia. However, with viral pneumonia, the
respiratory involvement happens slowly. Wheezing may occur and the cough may worsen. Viral
pneumonias may make a child susceptible to bacterial pneumonia. Treatment of viral pneumonia will
be symptomatic, including: oxygenation (with cool mist), comfort, CPT and postural drainage, fluids
and family support.
Bacterial pneumonia Bacterial pneumonia is caused by various bacteria. Streptococcus pneumoniae (pneumococcus) is
the most common bacterium that causes bacterial pneumonia. Many other bacteria may cause

Respiratory system/ Khulood Shattnawi ��bacterial pneumonia including group B streptococcus, staphylococcus aureus, group A
streptococcus and Haemophilus influenza type b (Hib).
Bacterial pneumonia may have a quick onset and the following symptoms may occur:
• Productive cough
• Tachypnea.
• Fever.
• Breathe sounds: ronchi or fine crackles.
• Chest pain (increased with deep breathing).
• Retractions.
• Nasal flaring.
• Pallor to cyanosis (depends on severity)
• Chest x-ray film: diffuse or patchy infiltration, with peribronchial distribution.
• Behavior: irritable, restless and lethargic.
• Gastrointestinal: anorexia, vomiting, diarrhea, and abdominal pain.
Therapeutic management:
Antimicrobial therapy has significantly reduced the morbidity and mortality from bacterial
pneumonia. Therapy with penicillin G, intramuscularly or intravenously, or for penicillin-allergic
children, erythromycin, clindamycin, chloramphenicol, or a cephalosporin, is effective in the
treatment of pneumococcal pneumonia. Antibiotic therapy, bed rest, liberal oral intake or fluid, and
administration of antipyretic for fever constitute the principal therapeutic measures. In addition, IV
fluid administration is frequently necessary, and oxygen may be required if the child is in respiratory
distress.
Nursing considerations:
Nursing care of the child with pneumonia is primarily supportive and symptomatic but necessitates
thorough respiratory assessment and administration of oxygen and antibiotics. The child’s respiratory
rate and status, as well as general disposition and level of activity are frequently assessed. Isolation
procedures are instituted according to hospital policy; rest and conservation of energy are encouraged
by the relief of physical and psychologic stress. If the cough is disturbing, the use of antitussive,
especially before rest times and meals, is often helpful. To prevent dehydration, fluids are frequently
administered intravenously.
Children may be placed in a mist tent, with cool humidification moistening the airways and providing
an atmosphere that assists in temperature reduction. Fever is controlled by the cool environment and
administration of antipyretic drugs as prescribed.
Asthma:
Asthma is defined as a chronic inflammatory disorder of the airway. In susceptible children,
inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and cough,
particularly at night and/or in the early morning. These episodes are usually associated with variable
airflow limitation or obstruction that is reversible either spontaneously or with treatment. The
inflammation that occurs in asthma also causes an associated increase in bronchial
hyperresponsiveness to a variety of stimuli.
Triggers tending to precipitate and/or aggravate asthmatic exacerbation:
• Allergens:
• Outdoor: trees, grasses, molds, pollens, airpollution.
• Indoor: dust, mold, cockroach antigen.
• Irritants: tobacco smoke, wood smoke, odor sprays.
• Exposure to occupational chemicals.
• Exercise.
• Cold air.

Respiratory system/ Khulood Shattnawi ��
• Changes in weather or temperature.
• Environmental change: moving to new home, starting new school, etc.
• Colds and infections.
• Animals: cats, dogs, rodents, horses.
• Medications: aspirin, NSAIDs, antibiotics.
• Strong emotions: fear, anger, laughing, crying.
• Conditions: gastroesophageal reflux,
tracheoesophageal fistula.
• Food additives: sulfite preservatives.
• Foods: nuts, milk/dairy products.
• Endocrine factors: menses, pregnancy, and
thyroid disease.
The mechanisms responsible for the obstructive
symptoms in asthma include:
• Inflammation and edema of the mucus
membrane.
• Accumulation of tenacious secretions from
mucus glands.
• Spasm of the smooth muscle of the bronchi
and bronchioles, which decreases the diameter of
bronchioles.
Exacerbations are episodes of progressively worsening shortness of breath, cough, wheezing, chest
tightness, or some combination of these changes. They also are characterized by decreases in
expiratory airflow. Airways narrow because of bronchospasm, mucosal edema, and mucous
plugging, with air being trapped behind occluded or narrowed airways. Functional residual capacity
rises because the child is breathing close to total lung capacity; hyperinflation enables the child to
keep the airways open and permits gas exchange to occur. Hypoxemia (decrease O2 in blood) can
occur during episodes because of the mismatching of ventilation and perfusion. This is seen as
increasing oxygen tension levels.
Clinical manifestations:
The classic manifestations of asthma are dyspnea, wheezing, and coughing. However, the timing of
these symptoms varies among children. Bronchoconstriction in response to an allergen can have an
immediate, histamine-type pattern or a late response with airway hypersensitivity lasting for days,
weeks, or months. A second wave of symptoms can occur 6 to 8 hours after the initial antigen
exposure.
An asthmatic episode usually begins with children feeling uncomfortable or irritable and
increasingly restless. They may also complain of a headache, feeling tired, or their chest feeling
tight. Respiratory symptoms include a hacking, paroxysmal, irritative, and nonproductive cough
caused by bronchial edema. Accumulated secretions, acting as a foreign body, stimulate the cough.
As the secretions become more profuse, the cough becomes rattling and productive of frothy, clear,
gelatinous sputum. Bronchial spasm and mucosal edema reduce the size of the bronchial lumen, and
the bronchi may be occluded by mucus plugs.
Auscultation may reveal:
• Prolonged expiratory phase, usually with wheezing
• Inspiratory wheezing suggests secretions in large airways
• A silent chest may indicate such severe obstruction that flow rates are too low to
generate breath sounds

Respiratory system/ Khulood Shattnawi ��Therapeutic management:
Nonpharmacologic therapy: the goal of nonpharmacologic therapy is prevention and reduction of
the child’s exposure to allergens and irritants. Basic to any therapeutic plan is an evaluation of the
child’s general health and an assessment of the specific allergic factors and the nonspecific factors
that precipitate symptoms. Specific allergens are identified by skin testing, and steps are taken to
eliminate or avoid the offending allergens.
Pharmacologic: pharmacologic therapy is used to prevent and control asthma symptoms, reduce the
frequency and severity of asthma exacerbations, and reverse airflow obstruction. Medications used to
treat asthma are categorized into two general classes: long-term control medications (preventor
medications) to achieve and maintain control of inflammation and quick-relief medications (rescue
medications) to treat acute symptoms and exacerbations. Quick-relief ang long-term medications are
often used in combination. Corticosteroids, cromolyn sodium and nedocromil, methylxanthines, and
long-acting β2-agonists are used as long-term control medications. Short-acting β2-agonists,
anticholinergics, and systemic corticosteroids are used as quick-relief medications. Many
medications used to treat asthma are given by inhalation with a nebulizer or metered-dose inhaler
(MDI).
Corticosteroids are used to treat reversible airflow obstruction and to control symptoms and reduce
bronchial hyperreactivity in chronic asthma. Corticosteroids may be administered parenterally, orally,
or by aerosol. Cromolyn sodium is a nonsteroidal antiinflammatory drug. This drug blocks both the
early and late reaction to allergens. Nedocromil sodium has both antiallergic and antiinflammatory
properties. This drug inhibits the bronchoconstrictor response to inhaled antigens and inhibits the
activity of and release of histamine and prostaglandins from inflammatory cells associated with
asthma. The drug is used for maintainance therapy in asthma and is not effective for reversal of acute
exacerbations. β-adrenergic agonists (albuterol, metaproterenol, terbutaline) are used for quick relief
of acute exacerbations and for the prevention of exercise-induced bronchospasm. β-adrenergic
agonists can be given via inhalation or as oral or parenteral preparations. The methylxanthines,
principally theophylline, have been used for decades to relieve symptomes and prevent asthma
attacks. Theophylline, however, is now considered a third-line agent and perhaps even unnecessary
for treating asthma exacerbations. it is a weaker bronchodilator than the β-adrenergics, and because
inflammation contributes to asthma, other drugs are of increased benefit. Theophylline may be
administered intravenously, intramuscularly, orally, or rectally. In addition to its bronchodilator
effect, theophylline is a central respiratory stimulant and increases respiratory muscle contractility.
Anticholinergic therapy, the oldest form of bronchodilator therapy for asthma, reduces intrinsic
vagal tone to the airways and blocks reflex bronchoconstriction caused by inhaled irritants.
Anticholinergics are used for relief of acute bronchospasm. The primary drugs used are atropine or
its derivative, ipratropiun, which does not cross the blood-brain barrier and therefore elicits no central
nervous system effects.
n Avoid
– Sedatives
n Depress respiratory drive
– Antihistamines
n Decrease LOC, dry secretions
– Aspirin
n High incidence of allergy
Chest physiotherapy (CPT) includes breathing exercises and physical training. These therapies help
produce physical and mental relaxation, improve posture, strengthen respiratory musculature, and
develop more efficient patterns of breathing.

Respiratory system/ Khulood Shattnawi ��Nursing considerations:
• Airway
• Breathing
– Sitting position
– Humidified O2 by NRB mask
• Dry O2 dries mucus, worsens plugs
– Encourage coughing
– Be prepared for possible intubation, assisted ventilation
• Circulation
– IV
– Assess for dehydration
Also refer to nursing care plan/ the child with asthma.
Status Asthmaticus:
Status Asthmaticus is a severe, prolonged asthma exacerbation that has not been broken with
repeated doses of bronchodilators. It is a true emergency that requires early recognition and
immediate transport. Patients are in imminent danger of respiratory failure
The symptoms of status asthmaticus are extreme difficulty with breathing, which causes
restlessness and anxiety. Although coughing and wheezing are common symptoms of asthma, a child
with status asthmaticus may not cough or wheeze because there is not enough airflow. Advanced
symptoms include little or no breath sounds, inability to speak, cyanosis, and heavy sweating. Status
asthmaticus can lead to unconsciousness and cardiopulmonary arrest, which can be fatal. Status
asthmaticus is an emergency situation that can lead to death. Patient management is based upon
administering large doses of corticosteroid drugs and bronchodilators and ensuring that the patient is
receiving adequate oxygenation until the attack is completed
Cystic Fibrosis (CF):
CF, a condition characterized by exocrine (or mucus-producing) gland dysfunction that produces
multisystem involvement, is the most common lethal genetic illness among white children,
adolescents, and young adults. CF is inherited as autosomal recessive trait; the affected child inherits
the defective gene from both parents, with an overall
incidence of 1:4. The mutated gene responsible for CF
is located on the long arm of chromosome 7. CF is
characterized by several apparently unrelated clinical
features: increased viscosity of mucus gland secretions,
a striking elevation of sweat electrolytes, an increase in
several organic and enzymatic constituents of saliva,
and abnormalities in autonomic nervous system
function.
Patients with CF demonstrate decreased
pancreatic secretion of bicarbonate and chloride, and
the primary transport abnormality in CF involves an
electrogenic chloride channel or its regulation. An
increase in sodium and chloride in both saliva and
sweat is characteristic of children with CF and forms
the basis for one of the most reliable diagnostic
procedures, the sweat chloride test.
The sweat electrolyte abnormality is present from birth throughout life and is unrelated to the
severity of the disease or the extent to which other organs are involved. The sodium and chloride
content of sweat in children with CF is two to five times greater than that of the controls in 98% to
99% of affected children.
The primary factor, and the one responsible for the multiple clinical manifestations of the
disease, is mechanical obstruction caused by the increased viscosity of mucous gland secretions.

Respiratory system/ Khulood Shattnawi ��Instead of forming a thin, freely flowing secretion, the mucous glands produce a thick mucoprotein
that accumulates and dilates them. Small passages in organs such as the pancreas and bronchioles
become obstructed as secretions precipitate or coagulate to from concretions in glands and ducts.
Diagnosis of CF:
• The first indicator is often meconium ileus in newborn babies.
• Parents note that their baby " tastes salty" when kissed.
• The sweat chloride test is used to diagnose the disease; > 60mEq/L is diagnostic.
• Stool fat or enzyme analysis may be done.
• CXR : patchy atelactesis and obstructive emphysema.
Respiratory Tract: Because of the increased viscosity of bronchial mucus, there is greater resistance
to ciliary action, a slower flow rate of mucus, and incomplete expectoration, which also contributes
to the mucous obstruction. This retained mucus serves as an excellent medium for bacterial growth.
Reduced oxygen-carbon dioxide exchange causes variable degreed of hypoxia, hypercapnia, and
acidosis. In severe, progressive lung involvement, compression of pulmonary blood vessels and
progressive lung dysfunction frequently lead to pulmonary hypertension, cor pulmonale (cor
pulmonale is the term for CHF resulting from obstructive lung diseases), respiratory failure, and
death. Pulmonary complications are present in almost all children with CF, but the onset and extent
of involvement are variable. Symptoms are produced by stagnation of mucus in the airways, with
eventual bacterial colonization leading to destruction of lung tissue. The abnormally vicous and
tenacious secretions are difficult to expectorate and gradually obstruct the bronchi and bronchioles,
causing scattered area of atelectasis and emphysema.
Gastrointestinal Tract. In the pancreas of many patients, the thick secretions block the ducts, leading
to cystic dilations of the acini (small lobes of the gland), which then undergo degeneration and
progressive diffuse fibrosis. This event prevents essential pancreatic enzymes from reaching the
duodenum, which causes marked impairment in the digestion and absorption of nutrients, particularly
fats, proteins, and, to a lesser degree, carbohydrates. Disturbed absorption in reflected in excessive
stool fat (steatorrhea) and protein (azotorrhea). The endocrine function of the pancreas often
remains unchanged, since the islets of Langerhans are normal but may decrease in number as
pancreatic fibrosis progresses. Howevere, the incidence of diabetes mellitus is greater in these
children than in the general population.
Clinical manifestations:
Respiratory manifestations: initial manifestations are often wheezing respirations and a dry,
nonproductive cough. Diffuse bronchial and bronchiolar obstruction leads to irregular aeration with
progressive pulmonary disturbance and secondary infection. Dyspnea increases, the cough often
becomes paroxysmall, and the mucoid impactions within the small air passages cause a generalized
obstructive emphysema and patchy areas of atelactasis. Progressive pulmonary involvement with
hyperaeration of functioning alveoli produces the overinflated, barrel shaped chest. When ventilation
and subsequent diffusion and gas exchange are significantly impaired, cyanosis and clubbing of the
fingers and toes may occur.
Gastrointestinal manifestations: the earliest postnatal manifestation of CF is meconium ileus,
which occurs in 7% to 10% of newborns with the disease. Thick intestinal secretions continue to be a
problematic throughout life. Gumlike masses in the cecum can obstruct the bowel, causing pain,
nausea, and vomiting. As the disease progresses, obstruction of pancreatic ducts prevents digestive
enzymes (trypsin, lipase, chymotrypsin, & amylase) from being released into the duodenum, which
prevents conversion of ingested food into compounds that can be absorbed by the intestinal mucosa.
Consequently, the nondigested food is excreted (chiefly unabsorbed fats and proteins), increasing the
bulk of feces to two or three times the normal amount. Because so little is absorbed from the
intestine, affected children have difficulty maintaining weight despite a healthy appetite and diet.
Unable to compensate for the fecal losses, children lose weight and exhibit marked wasting of tissues

Respiratory system/ Khulood Shattnawi ��and failure to grow. The abdomen is distended, the extremities are thin, and the pale skin droops
from wasted buttocks. The impaired ability to absorb fats results in a deficiency of the fat-soluble
vitamins A, D, E, and K, which causes easy bruising. Anemia is a common complication.
Reproductive system: delayed puberty in females with CF is common even when their nutritional
and clinical status is good. Fertility can be inhibited by highly viscous cervical secretions, which act
as a plug, blocking sperm entry. With few exceptions, males are sterile, which may be caused by
blockage of the vas deferens with abnormal secretions or by failure of normal development of the
wolffian duct structures resulting in decreased or absent sperm production.
Integumentary system: parents frequently observe that their infants taste “salty” when they kiss
them. The chloride channel defect in sweat glands prevents reabsorption of sodium and chloride,
which leaves the affected person at risk for abnormal slat loss, dehydration, and hypochloremic and
hyponatremic alkalosis during hyperthermic conditions.
Therapeutic management:
Pulmonary problems: prevention of infection by a daily routine of chest physiotherapy (CPT) to
maintain pulmonary hygiene. Bronchodilator medication delivered in an aerosol helps open bronchi
for easier expectoration and is administered before CPT. Pulmonary infections are treated as soon as
they are recognized. Oxygen administration is usually recommended for children with acute
episodes.
GI problems: replacement of pancreatic enzymes (enteric-coated products) are administered with
meals and snacks to ensure that digestive enzymes are mixed with food in the duodenum. Usually
one to five capsules are administered with a meal, and a smaller amount is taken with snacks. The
amount of enzyme is adjusted to achieve normal growth and a decrease in the number of stools to
two or three per day. Children with CF require a well-balanced, high-protein, high-calorie diet. Since
the uptake of fat-soluble vitamins is decreased, water-miscible forms of these vitamins (A, D, E, K)
are given. When high-fat foods are eaten, the child is encouraged to add extra enzymes. Pancreatic
enzymes should be taken within 30 minutes of eating, and the beads should not be chewed or
crushed.
Salt depletion through sweating can be a problem during hot weathers or physical exertion.
Salt supplementation is often needed during hot weather or febrile periods and should include use of
fluids.
Esophageal atresia and tracheoesophageal fistula
• Atresia: absence of a normal opening
• Fistula: abnormal passage from a body organ to the body surface or between two internal
body organs.
Congenital esophageal atresia (EA) represents a failure of the esophagus to develop as a
continuous passage. Instead, it ends as a blind pouch. Tracheoesophageal fistula (TEF) represents an
abnormal opening between the trachea and esophagus. EA and TEF can occur separately or together.
EA and TEF are diagnosed in the ICU at birth and treated immediately.
The presence of EA is suspected in an infant with excessive salivation (drooling) and in a
newborn with drooling that is frequently accompanied by choking, coughing and sneezing. When
fed, these infants swallow normally but begin to cough and struggle as the fluid returns through the
nose and mouth. The infant may become cyanotic (the 3 C's: coughing, choking & cyanosis) and may
stop breathing as the overflow of fluid from the blind pouch is aspirated the trachea. The cyanosis is
a result of laryngospasm. Aspiration and pneumonia will be common complication, and over time
respiratory distress will develop.
If any of the above signs/symptoms are noticed, a catheter is gently passed into the esophagus to
check for resistance. If resistance is noted, other studies will be done to confirm the diagnosis. A
catheter can be inserted and will show up as white on a regular x-ray film to demonstrate the blind

Respiratory system/ Khulood Shattnawi �pouch ending. Sometimes a small amount of barium is placed through the mouth to diagnose the
problems.
Treatment of EA and TEF is surgery to repair the defect. If EA or TEF is suspected, all oral feedings
are stopped and intravenous fluids are started. The infant will be positioned to help drain secretions
and decrease the likelihood of aspiration. Babies with EA may sometimes have other problems.
Types of esophageal atresia/ tracheoesophageal fistula. The most common type is the left-most
diagram. In each diagram 1=esophagus (upper and lower portions) and 2=trachea
Nursing considerations: refer to nursing care plan/the infant with esophageal atrasia and
tracheoesophageal fistula.
Congenital Diaphragmatic hernia:
Congenital Diaphragmatic Hernia (CDH) occurs in about one in every 2,500 live births.
Absence of the diaphragm may occur on the left, right or both sides, but the left side is most
common. This defect allows abdominal organs to move into the chest cavity. With the heart, lungs,
and abdominal organs all taking up space in the chest cavity, the lungs do not have space to develop
properly. This underdevelopment of the lungs is called pulmonary hypoplasia. Diaphragmatic hernia
is a multifactorial condition, which means that many factors, both genetic and environmental, are
involved.
Further (careful) fetal evaluation is indicated to rule out other birth defects as well as
chromosomal anomalies, since they may adversely affect the outcome. Important prognostic
predictors (for survival) include the degree of fetal liver herniation into the chest, the presence or
absence of other anomalies. Prenatal evaluation consists of an ultrasound, fetal MRI, fetal
chromosome studies, as well as a fetal echocardiogram.
Whether a family chooses to terminate the pregnancy or carry to term for postnatal
management, accurate counseling regarding the expected outcome is crucial. For CDH fetuses with
chromosomal anomalies, survival would be rare. Postnatal management strategies include planned
delivery, immediate stabilization, and immediate access to specialized ventilation techniques. Once
the infant is stabilized, the diaphragmatic hernia is repaired with an operation. The stomach,
intestine, and other abdominal organs are moved from the chest cavity back to the abdominal cavity
and the hole in the diaphragm is repaired. Many babies will need to remain in the neonatal intensive
care unit for a while after surgery. Although the abdominal organs are now in the right place, the
lungs still remain underdeveloped. The baby will usually need to have breathing support for a period
of time after surgery.
The symptoms of diaphragmatic hernia are often observable soon after birth. The following
are the most common symptoms:
• Difficulty in breathing.
• Tachycardia.
• Cyanosis.
• Abnormal chest development, with one side being larger than the other.
• Concave abdomen.
Management: repairing the herniated diaphragm

Respiratory system/ Khulood Shattnawi �Foreign Body Aspiration
• Risk among older infants & children age 1 – 3 years.
• Severity is determined by:
– Location
– Type of object aspirated
– Extent of obstruction
What do they aspirate?
• Anything that can fit in the mouth
• Most common
– Food matter
• Peanut = most common
• Common, but less than food matter
– Inorganic matter
• Balloons = most lethal
• Toy parts
• Crayons
• Coins
Manifestations • Symptoms depends on the site of obstruction
• Initially, choking, gagging, or coughing
• laryngotracheal obstruction: dyspnea, cough, stridor, hoarseness because of decreased air
entry. Cyanosis may occur if obstruction becomes worse
• Bronchial obstruction: paroxysmal cough, wheezing, asymmetric breath sounds, decreased air
entry, dyspnea.
• With progressive obstruction: child’s face become discolored, child becomes unconscious and
dies of asphyxiation
• If the obstruction is partial, hours, days, or even weeks may pass without symptoms after the
initial period.
• secondary symptoms are related to the anatomic location of FB and usually caused by a
persistent respiratory infection
Therapeutic management • abdominal thrust older than 1 year, back blows and chest thrusts younger than 1, Heimlich
• What IF…child conscious but cannot speak or cough?
– Look for object in mouth/oropharynx
• If visible – Remove it
• NO blind finger sweeps
– <12mo old
• 5 Back blows
then
• 5 Chest thrusts
– >12mo old
• Heimlich maneuver
• Until object removed or child unconscious
Back blows to relieve foreign
body obstruction in the infant.

Respiratory system/ Khulood Shattnawi ��
Infant is held lying face up along
the length of an adult thigh while
a hand administers chest thrusts
in the proper direction to relieve
a complete foreign body airway
obstruction
Back slaps and Heimlich maneuver
for older child
If child is Unconscious
• <12mo old
– ABC
– Tongue-jaw lift – look for object
– Attempt to ventilate
– Continue 5 back blows and 5 chest thrusts
– CPR as needed
• >12mo old
– Lie child on floor
– ABC
– Tongue-jaw lift – look for object
– Attempt to ventilate
– 5 Abdominal thrusts
– CPR if needed
Nursing consideration
• Recognition signs of FB aspiration and distress.
– Not every child who gags or coughs while eating is truly choking
• The child in distress (truly choking):
– Cannot speak
– Becomes cyanostic
– Collapses
• Follow-up care after removal of FB include monitoring for signs of airway edema and
respiratory distress
• Place child in a high-humidity atmosphere.
• Antibiotic: for secondary infection

Respiratory system/ Khulood Shattnawi ��
NURSING CARE PLAN
The Child with Acute Respiratory Infection
Nursing Diagnosis: Ineffective breathing pattern related to inflammatory process
Patient Goal 1: Will exhibit normal respiratory function
• NURSING INTERVENTIONS/RATIONALES
Position for maximum ventilation (i.e., open airway and permit maximum lung expansion)
Allow position of comfort (e.g., tripod position of child with epiglottitis or maintain head elevation of
at least 30 degrees)
Check child's position frequently to ensure child does not slide down to avoid compressing the
diaphragm
Avoid constricting clothing or bedding
Use pillows and padding to maintain open airway (e.g., in infant or child with hypotonia)
Provide increased humidity and supplemental oxygen by placing child in small tent or hood (infant)
or administer via nasal cannula or mask (preferred methods for children older than infancy because of
safety issues)
Promote rest and sleep by scheduling appropriate activity and rest periods
Encourage relaxation techniques
Teach child and family measures to ease respiratory efforts (i.e., appropriate positioning)
For most respiratory illnesses use cool-mist humidifier in child's room
For spasmodic croup create warm mist by running hot water in a closed bathroom (warm mist,
often used for children with spasmodic croup, may be helpful because of its relaxing effect, but
mostly because child is being held upright in the shower)
• EXPECTED OUTCOMES
Respirations remain within normal limits (see inside back cover for normal variations)
Respirations are unlabored
Child rests and sleeps quietly
Patient Goal 2: Will receive optimum oxygen
supply
• NURSING INTERVENTIONS/RATIONALES
Position for maximum ventilatory efficiency (see Goal 1, above)
Use pulse oximetry to monitor oxygen saturations
Place in cool, humidified environment, using appropriate oxygen delivery system
Provide oxygen as prescribed and/or needed
• EXPECTED OUTCOMES
Child breathes easily
Respirations remain within normal limits (see inside back cover for normal variations)
Oxygen saturation is >95%
Nursing Diagnosis: Fear/anxiety related to difficulty breathing, unfamiliar procedures, and possibly
environment (hospital)
Patient Goal 1: Will experience reduction of fear/anxiety
• NURSING INTERVENTIONS/RATIONALES

Respiratory system/ Khulood Shattnawi ��Explain unfamiliar procedures and equipment to child in developmentally appropriate terms
Establish rapport with child and parents
Remain with child and parent during procedures
Use calm, reassuring manner
Provide frequent attendance during acute phase of illness
Provide comfort measures child prefers (e.g., rocking, stroking, music)
Provide attachment objects (e.g., familiar toy, blanket)
Encourage family-centered care with increased parental attendance and, when possible, involvement
Do nothing to make child more anxious or fearful
Instill confidence in both parents and child
Try to avoid any intrusive or painful procedures
Be aware of child's rest/sleep cycle or pattern in planning nursing activities
Assess and implement appropriate pain management therapy (i.e., sedatives and/or analgesics) (see
Pain Assessment; Pain Management, Chapter 26)
Provide diversional activities appropriate to child's cognitive ability and condition
Administer medications that promote improved ventilation (e.g., bronchodilators, expectorants) as
prescribed
• EXPECTED OUTCOMES
Child exhibits no signs of respiratory distress or physical discomfort
Parents remain with child and provide comfort
Child engages in quiet activities appropriate for age, interest, condition, and cognitive level
Nursing Diagnosis: Ineffective airway clearance related to mechanical obstruction, inflammation,
increased secretions, pain
Patient Goal 1: Will maintain patent airway
• NURSING INTERVENTIONS/RATIONALES
Position child in proper body alignment to allow better lung expansion and improved gas exchange,
as well as to prevent aspiration of secretions (prone, semiprone, side lying; for infants not at risk for
aspiration, use supine or side-lying position for sleeping)
Suction secretions from airway as needed
Limit each suction attempt to 5 seconds with sufficient time between attempts to allow
reoxygenation
Position supine with head in "sniffing" position with neck slightly extended and nose pointed to
ceiling
Avoid neck hyperextension
Assist child in expectorating sputum
Administer expectorants if prescribed
Perform chest physiotherapy
Give nothing by mouth to prevent aspiration of fluids (e.g., child with severe tachypnea)
Administer appropriate pain management
Have emergency equipment available to avoid delay in treatment if needed
Avoid throat examination and culture with suspected epiglottitis, because it could cause airway
obstruction
Assist child in splinting any incisional/injured area to maximize effects of coughing and chest
physiotherapy
• EXPECTED OUTCOMES
Airways remain clear
Child breathes easily; respirations are within normal limits (see inside back cover)

Respiratory system/ Khulood Shattnawi ��
Patient Goal 2: Will expectorate secretions adequately
• NURSING INTERVENTIONS/RATIONALES
Ensure adequate fluid intake to liquefy secretions
Provide humidified atmosphere to prevent crusting of nasal secretions and drying of mucous
membranes
Explain importance of expectoration to child and family
Assist child in coughing effectively; provide tissues
Remove accumulated mucus; suction if needed
Administer pain medications as indicated before attempt to clear airway
Provide nebulization with appropriate solution and equipment as prescribed
Assist with splinting so child will experience minimal discomfort
Perform percussion, vibration, and postural drainage to facilitate drainage of secretions
• EXPECTED OUTCOME
Older child expectorates secretions without undue stress and fatigue; younger child will be able to
have a productive cough
Nursing Diagnosis: Risk for infection related to presence of infective organisms
Patient Goal 1: Will exhibit no signs of secondary infection
• NURSING INTERVENTIONS/RATIONALES
Maintain aseptic environment, using sterile suction catheters and good handwashing
Isolate child as indicated to prevent nosocomial spread of infection
Administer antibiotics as prescribed to prevent or treat infection
Provide nutritious diet according to child's preferences and ability to consume nourishment to support
body's natural defenses
Encourage good chest physiotherapy
Teach child and/or family manifestations of illness
• EXPECTED OUTCOME
Child exhibits evidence of diminishing symptoms of infection
Patient Goal 2: Will not spread infection to others
• NURSING INTERVENTIONS/RATIONALES
Use standard precautions (see Infection Control, Chapter 27)
Instruct others (parents, members of staff) in appropriate precautions
Teach affected children protective methods to prevent spread of infection (e.g., handwashing,
disposal of soiled tissues)
Limit the number of visitors/family members/siblings and screen for any recent illness in visitors
Try to keep infants and small children from placing hands and objects in contaminated areas
Assess home situation and implement protective measures as feasible in individual circumstances
Administer antimicrobial medications if prescribed
• EXPECTED OUTCOME
Others remain free from infection
Nursing Diagnosis: Activity intolerance related to inflammatory process, imbalance between oxygen

Respiratory system/ Khulood Shattnawi ��supply and demand
Patient Goal 1: Will maintain adequate energy
levels
• NURSING INTERVENTIONS/RATIONALES
Assess child's level of physical tolerance
Assist child in those activities of daily living that may be beyond tolerance
Provide diversional activities appropriate to child's age, condition, capabilities, and interest
Provide diversional play activities that promote rest and quiet but prevent boredom and withdrawal
Provide rest and sleep periods appropriate to age and condition
Instruct child to rest when feeling tired
Balance rest and activity when ambulatory
• EXPECTED OUTCOMES
Child plays and rests quietly and engages in activities appropriate to age and capabilities (specify)
Child exhibits no evidence of increased respiratory distress
Child tolerates increasingly more activity
Patient Goal 2: Will receive optimum rest
• NURSING INTERVENTIONS/RATIONALES
Provide quiet environment
Organize activities for maximum sleep time
Do not perform nonessential treatments or procedures to maximize rest
Schedule visiting to allow for sufficient rest
Encourage parents to remain with child
Schedule treatments or other activities around the needs of the child so that fatigue will be
minimized.
Administer sedatives and analgesics as indicated if ordered for restlessness and pain
Encourage frequent rest periods and regular sleep times
Follow child's usual routine for bedtime and nap time
Implement measures to ensure sleep, such as quiet, darkened room
• EXPECTED OUTCOMES
Child remains calm, quiet, and relaxed
Child rests a sufficient amount (specify)
Nursing Diagnosis: Pain related to inflammatory process, surgical incision
Patient Goal 1: Will experience no pain or reduction of pain/discomfort to level acceptable to child
• NURSING INTERVENTIONs/RATIONALES
Use local measures (gargles, troches, warmth or cold) to reduce throat pain
Apply heat or cold as appropriate to affected area
Administer analgesic as prescribed (see Pain Management, Chapter 26)
Assess response to pain control measures (see Pain Assessment, Chapter 26)
Encourage diversional activities appropriate to age, condition, capabilities
• EXPECTED OUTCOME

Respiratory system/ Khulood Shattnawi ��Child has no pain or acceptable level of pain
Nursing Diagnosis: Altered family processes related to illness and/or hospitalization of a child
Patient (family) Goal 1: Will experience reduction of anxiety and increased ability to cope
• NURSING INTERVENTIONS/RATIONALES
Recognize parental concern and need for information and support
Explore family's feelings and "problems" surrounding hospitalization and child's illness
Explain therapy and child's behavior
Provide support as needed
Encourage family-centered care and encourage family to become involved in their child's care
• EXPECTED OUTCOME
Parents ask appropriate questions, discuss child's condition and care calmly, and become involved
positively in child's care
See also
Nursing Care Plan: The Family of the Child Who Is Ill or Hospitalized, Chapter 26
Nursing Care Plan: The Child in the Hospital, Chapter 26
Data from Wong DL: Whaley & Wong's Nursing Care of Infants and Children, ed. 6, St. Louis,
1999, Mosby, Inc.

Respiratory system/ Khulood Shattnawi ��NURSING CARE PLAN
The Child with Asthma
Nursing Diagnosis: Risk for suffocation related to interaction between individual and allergen(s)
Patient Goal 1: Will experience no asthmatic episode
• NURSING INTERVENTIONS/RATIONALES
Teach child and family how to avoid conditions or circumstances that precipitate asthmatic episode
Assist parents in eliminating allergens or other stimuli that trigger exacerbation (see Box 32-17 for
complete listing), such as:
Meal planning to eliminate allergenic foods
Removal of pets
Modification of environment: "allergy-proof" home, especially no smoking in home
Avoid extremes of environmental temperature
When child is exposed to cold air, recommend breathing through nose (not mouth) and wearing a
mask or scarf, or cupping hand over nose and mouth to create a reservoir of warm air to breathe
Assist parents in obtaining and/or installing device to control environment (dehumidifier, air
conditioner, electronic air filter)
Teach child and family to recognize early signs and symptoms so that an impending episode can be
controlled before it becomes distressful
Teach child and family correct use of bronchodilators and antiinflammatory drugs (e.g.,
corticosteroids, cromolyn sodium), adverse effects, and dangers of overuse or underuse of drugs
Teach child to understand how equipment works
Teach child correct use of inhalers, nebulizers, and peak expiratory flow meters (PEFMs)
Teach child and family prophylactic treatment when appropriate (e.g., prevent exercise-induced
bronchospasm by using medication before exercise)
Explain to child and family possible benefits of hyposensitization therapy when allergen(s) can be
defined and cannot be avoided (e.g., pollen, mold) or controlled satisfactorally by drugs
Administer hyposensitization therapy if prescribed
• EXPECTED OUTCOMES
Family makes every effort to remove or avoid possible allergens or precipitating events
Child/family are able to detect signs of an impending episode early and implement appropriate
actions
Child/family are able to administer medications and use inhalers and other equipment
Patient Goal 2: Will experience optimum health
• NURSING INTERVENTIONS/RATIONALES
Encourage sound health practices to support body's natural defenses:
Balanced, nutritious diet
Adequate rest
Good hygiene
Appropriate exercise
Follow-up care
Prevent respiratory infection, since it can trigger an attack or aggravate the asthmatic state
Avoid exposure to infection
Take meticulous care of equipment to avoid bacterial and/or fungal growth
Use good handwashing
• EXPECTED OUTCOMES
Child and parents practice sound health practices

Respiratory system/ Khulood Shattnawi ��Child exhibits no evidence of infection
Nursing Diagnosis: Activity intolerance related to imbalance between oxygen supply and demand
Patient Goal 1: Will receive optimum rest
• NURSING INTERVENTIONS/RATIONALES
Encourage activities appropriate to child's condition and capabilities (specify)
Provide ample opportunities for sleep, rest, and quiet activities to conserve oxygen supply
• EXPECTED OUTCOMES
Child engages in appropriate activities (specify)
Child appears rested
Nursing Diagnosis: Altered family processes related to having a child with a chronic illness
Patient/Family Goal 1: Will exhibit positive adaptation to the condition
• NURSING INTERVENTIONS/RATIONALES
Foster positive family relationships
Reinforce positive coping mechanisms of child and family
Use every opportunity to increase parents' and child's understanding of the disease and its therapies,
since adequate knowledge is related to family's timely use of preventive and emergency intervention
Reinforce the need for responding to early signs of impending asthma episode using prescribed
medications as needed to decrease potential for a severe exacerbation
Intervene appropriately if there is evidence of maladaptation
Be alert to signs of parental rejection or overprotection
Be alert to signs that child is depressed and make appropriate referral for psychologic support, since
depressed children, especially adolescents, may not comply with therapies as a means of passive
suicide
Teach child and family how to give respiratory treatments to eliminate any confusion regarding
medication or inhalers/nebulizers
Encourage family to contact school personnel (e.g., nurse, teachers, coaches, principal) to develop a
consistent plan of care for school setting
Refer family to appropriate support groups and community agencies
• EXPECTED OUTCOMES
Family copes with symptoms and effects of the disease and provides a normal environment for the
child
See Nursing Care Plan: The Child with Chronic Illness or Disability, Chapter 22
Nursing Diagnosis: Risk for suffocation related to bronchospasm, mucus secretions, edema
Patient Goal 1: Will experience cessation of bronchospasm
• NURSING INTERVENTIONS/RATIONALES
Establish IV infusion for administration of medication and hydration
Administer aerosolized bronchodilators and either oral or IV corticosteroids with or without
epinephrine as prescribed to relieve bronchospasm
Carefully monitor IV aminophylline infusion or oral theophylline for maximum efficacy and
minimum side effects
Closely monitor vital signs before, during, and after administration for maximum efficacy and

Respiratory system/ Khulood Shattnawi �minimum side effects
Interview parents to determine medications given before admission to avoid possible overdose
Have emergency equipment and medications readily available to prevent delay in treatment
• EXPECTED OUTCOMES
Child breathes more easily
Child does not suffocate
Patient Goal 2: Will exhibit normal respiratory function
• NURSING INTERVENTIONS/RATIONALES
Administer humidified oxygen by tent, face mask, or cannula to maintain satisfactory oxygenation
Closely monitor oxygen saturations and blood gases via pulse oximetry to detect early or impending
hypoxia
Closely monitor percentage of oxygen delivered, since high levels may depress respirations
Position for optimum lung expansion
High-Fowler position
Provide overbed table with pillow on which to lean if more comfortable for child
Implement measures to reduce fear/anxiety to decrease respiratory efforts and oxygen consumption
Encourage relaxation techniques to decrease anxiety and promote lung expansion
Administer sedatives and tranquilizing agents, if prescribed, with extreme caution and when agitation
is not caused by anoxia, since these drugs can depress respirations and mask signs of anoxia
Organize activities to allow for rest, sleep, and minimum expenditure of energy
• EXPECTED OUTCOMES
Child's respirations are unlabored and within normal limits (see inside back cover)
Child rests and sleeps comfortably
Child does not experience decreased oxygen saturations
Patient Goal 3: Will successfully expel bronchial secretions
• NURSING INTERVENTIONS/RATIONALES
Provide adequate hydration, oral or IV, to liquefy secretions for easier removal
Maintain NPO, if necessary, to prevent aspiration of fluids and food
Provide humidified atmosphere to prevent drying of mucous membranes
Encourage child to cough effectively
Provide tissues
Explain need to remove secretions
Suction, using correct technique, only when necessary
Do not use chest physiotherapy (CPT) during an acute episode, since it will only agitate an already-
anxious, dyspneic child and aggravate the episode
Position, if necessary, to prevent aspiration of secretions
Semiprone
Side-lying
• EXPECTED OUTCOMES
Secretions are adequately and easily expelled
Child coughs effectively
Child does not aspirate secretions, food, or fluids
Nursing Diagnosis: Risk for fluid volume deficit related to difficulty taking fluids, insensible fluid
losses from hyperventilation, and diaphoresis

Respiratory system/ Khulood Shattnawi �
Patient Goal 1: Will exhibit adequate hydration
• NURSING INTERVENTIONS/RATIONALES
Maintain IV infusion at appropriate rate, since fluid therapy will enhance liquifaction of secretions
(IV usually run two-thirds to three-quarters maintenance [unless dehydration present] in order to
minimize the risk of pulmonary edema because of high inspiratory pressures)
Encourage oral fluids
Offer fluids when acute respiratory distress subsides to decrease risk of aspiration
Avoid cold liquids, since they can trigger reflex bronchospasm
Give fluids (and food) in small, frequent feedings to avoid abdominal distention that might interfere
with diaphragmatic excursion
Use play techniques appropriate to child's age to encourage fluid intake
Measure intake and output
Correct dehydration slowly, since overhydration can increase the accumulation of interstitial
pulmonary fluid, leading to increased airway obstruction
• EXPECTED OUTCOME
Child exhibits adequate hydration
Nursing Diagnosis: Risk for injury (respiratory acidosis, electrolyte imbalance) related to
hypoventilation, dehydration
Patient Goal 1: Will not experience acidosis
• NURSING INTERVENTIONS/RATIONALES
Closely monitor blood pH, since pH less than 7.25 impairs systemic, pulmonary, and coronary blood
flow, and normal pH enhances effect of bronchodilators
Administer sodium bicarbonate as ordered to prevent or correct acidosis
Maintain IV infusion for administration of emergency medications and to prevent dehydration
Prevent vomiting and subsequent dehydration; initially, child will experience alkalosis, but if
vomiting becomes severe or uncontrolled, can lead to acidosis
Implement measures to improve ventilation; hypoventilation may cause an accumulation of carbon
dioxide, which will decrease pH
• EXPECTED OUTCOME
Child exhibits no evidence of respiratory acidosis
Patient Goal 2: Will exhibit normal serum electrolytes
• NURSING INTERVENTIONS/RATIONALES
Closely monitor serum electrolytes, since dehydration, as well as medications, can alter normal
serum electrolytes
Maintain IV infusion at appropriate rate
Prevent dehydration and vomiting, since they cause electrolyte imbalances
• EXPECTED OUTCOME
Child exhibits normal serum electrolytes
Nursing Diagnosis: Altered family processes related to emergency hospitalization of child
Patient/Family Goal 1: Will experience reduction of anxiety

Respiratory system/ Khulood Shattnawi ��
• NURSING INTERVENTIONS/RATIONALES
Keep parents informed of child's condition
Encourage expression of feelings, especially severity of condition and prognosis
Allow parents to be with child as much as possible by encouraging family-centered care concepts
Point out any evidence of improvement to encourage positive coping behaviors
If/when possible, schedule treatments and care to child's routines
Reduce sensory stimuli by maintaining quiet, relaxed environment
• EXPECTED OUTCOMES
Family verbalizes concerns and spends time with child
Family exhibits no signs of distress
See also:
Nursing Care Plan: The Family of the Child Who Is Ill or Hospitalized, Chapter 26
Nursing Care Plan: The Child in the Hospital, Chapter 26
Nursing Diagnosis: Ineffective airway clearance related to allergenic response and inflammation in
the bronchial tree
Patient Goal 1: Will exhibit evidence of improved ventilatory capacity
• NURSING INTERVENTIONS/RATIONALES
Instruct and/or supervise breathing exercises and controlled breathing to promote proper
diaphragmatic breathing, side expansion, and improved chest wall mobility
Use play techniques for breathing exercises with young children (e.g., blow a pinwheel or blow
cotton balls on table to extend expiratory time and increase expiratory pressure)
Teach correct use of prescribed medications
Teach correct use of PEFM, nebulizer, and metered-dose inhaler (MDI) if indicated
Teach family to perform percussion and postural drainage and to encourage coughing if indicated
Encourage physical exercise
Recommend activities requiring short bursts of energy (e.g., baseball, sprints, skiing), since they
may be better tolerated than those requiring endurance exercise (e.g., soccer, distance running)
Recommend swimming because child breathes air saturated with moisture, and exhaling underwater
prolongs expiration and increases end-expiratory pressure
Restrict physical activity only when child's condition makes it necessary
Encourage good posture for maximum lung expansion
Assist child and family in selecting activities appropriate to child's capabilities and preferences
• EXPECTED OUTCOMES
Child breathes easily and without dyspnea
Child exhibits improved ventilatory capacity (specify)
Child engages in activities according to abilities and interest (specify)
Data from Wong DL: Whaley & Wong's Nursing Care of Infants and Children, ed. 6, St. Louis,
1999, Mosby, Inc.

Respiratory system/ Khulood Shattnawi ��
NURSING CARE PLAN
The Infant with Esophageal Atresia and Tracheoesophageal Fistula
Nursing Diagnosis: Ineffective airway clearance related to abnormal opening between esophagus and
trachea or obstruction to swallowing
Patient Goal 1: Will maintain patent airway
• Nursing Interventions/Rationales
Suction as necessary to remove accumulated secretions from oropharynx
Position supine with head elevated on an inclined plane (at least 30 degrees) to decrease pressure
against thoracic cavity and to minimize reflux of gastric secretions up distal esophagus and into
trachea and bronchi
Administer oxygen per unit guidelines (pulse oximetry, blood gases) to help relieve respiratory
distress
Do not use positive pressure (e.g., resuscitation bag/mask), since it may introduce air into stomach
and intestines, creating additional pressure in thoracic cavity
Administer nothing by mouth to prevent aspiration
Maintain intermittent or continuous suction of esophageal segment, if ordered preoperatively, to keep
blind pouch empty of secretions
Leave gastrostomy tube, if present, open to gravity drainage so that air can escape, minimizing risk of
regurgitation of gastric contents into trachea
• Expected Outcomes
Airway remains patent
Infant does not aspirate secretions
Respirations remain within normal limits
Nursing Diagnosis: Impaired (difficulty) swallowing related to mechanical obstruction
Patient Goal 1: Will receive adequate nourishment
• Nursing Interventions/Rationales
Administer gastrostomy feedings as prescribed to provide nourishment until oral feedings are
possible
Progress to oral feedings as prescribed according to infant's condition and surgical correction
Observe closely to make certain infant is able to swallow without choking
Monitor intake, output, and weight to assess adequacy of nutritional intake
Give infant pacifier to provide for nonnutritive sucking
Teach family appropriate feeding techniques to prepare for discharge
• Expected Outcome
Infant receives sufficient nourishment and exhibits a satisfactory weight gain
Patient Goal 2: Patient will learn to take oral feedings (following complete repair)
• Nursing Interventions/Rationales
Introduce foods one at a time to evaluate tolerance of food item
Provide age-appropriate foods with various textures and flavors to stimulate interest in eating
Begin with pureed foods and progress to more solid food as child shows readiness

Respiratory system/ Khulood Shattnawi ��Cut food in small, noncylindrical pieces to prevent choking
Avoid foods such as whole hot dogs or large pieces of meat to decrease risk of choking
Teach child to chew foods well to decrease risk of choking
Refer to speech or occupational therapist, if appropriate, to facilitate learning
• Expected Outcome
Child takes an adequate amount of nourishment and displays no evidence of feeding resistance,
malnutrition, or dysphagia
Nursing Diagnosis: Risk for injury related to surgical procedure
Patient Goal 1: Will not experience trauma to surgical site
• Nursing Interventions/Rationale
Suction only with catheter premeasured to a distance that does not reach to surgical site to prevent
trauma to mucosa
• Expected Outcome
Child does not exhibit evidence of injury to surgical site
Nursing Diagnosis: Anxiety related to difficulty swallowing, discomfort from surgery
Patient Goal 1: Will experience a sense of security without discomfort
• Nursing Interventions/Rationales
Provide tactile stimulation (e.g., cuddling, rocking) to facilitate optimum development and promote
comfort
Administer mouth care to keep mouth clean and mucous membranes moist
Offer pacifier frequently to provide nonnutritive sucking
Administer analgesics as prescribed
Encourage parents to participate in child's care to provide comfort and security
• Expected Outcomes
Infant rests calmly, is alert when awake, and engages in nonnutritive sucking
Mouth remains clean and moist
Child experiences no or minimal pain
Nursing Diagnosis: Altered family processes related to child with a physical defect
Patient (family) Goal 1: Will be prepared for home care of child
• Nursing Interventions/Rationales
Teach family skills and observations needed for home care
Positioning to prevent aspiration
Signs of respiratory distress to prevent delay in treatment
Signs of complications-refusal to eat, dysphagia, increased coughing-so practitioner can be notified
Acquiring needed equipment and services
Care of gastrostomy and esophagostomy when infant has staged surgery, including techniques such
as suctioning, feeding, care of operative site and/or ostomies, dressing changes, to ensure appropriate
care after discharge
• Expected Outcome

Respiratory system/ Khulood Shattnawi ��Family demonstrates ability to provide care to infant, an understanding of signs of complications,
and appropriate actions
See also:
Nursing Care Plan: The Family of the Child Who Is Ill or Hospitalized, Chapter 26
Nursing Care Plan: The High-Risk Infant, Chapter 10
Data from Wong DL: Whaley & Wong's Nursing Care of Infants and Children, ed. 6, St. Louis,
1999, Mosby, Inc.