Resistant Gram-negative Infections 21 st March 2013 Acute Medicine Study Day Dr Sarah Glover...
-
Upload
gabriel-randle -
Category
Documents
-
view
213 -
download
0
Transcript of Resistant Gram-negative Infections 21 st March 2013 Acute Medicine Study Day Dr Sarah Glover...

Resistant Gram-negative Infections
21st March 2013
Acute Medicine Study Day
Dr Sarah Glover
Consultant in Medical Microbiology and Infectious Diseases

Overview
• Resistance in Enterobacteriaceae (‘coliforms’ e.g. E coli, Klebsiella, Enterobacter)
• ESBLs – what they are• ESBLs – why they matter• Epidemiology• Carbapenemases

Case 1
• 90M• Background of DM, CRF, previous pneumonia• Care home resident, bed bound fully dependent, long
term urinary catheter• Admitted SOB, CRP >250 WCC 35 ?LRTI• Started cefuroxime plus clarithromycin as hx of penicillin
allergy• 24 hrs into admission, blood cultures flagged positive
with Gram negative bacilli• Looking at previous microbiology: MSU from a month
earlier: ESBL-positive E coli• Changed to meropenem

Case 1
• Following day, BC isolate confirmed as ESBL producing E coli, resistant to trimethoprim, co-amoxiclav, cefuroxime, ciprofloxacin. Sensitive to meropenem and gentamicin
• CSU from admission, mixed growth of 3 organisms including ESBL-producing E coli with the same sensitivity pattern
• Good clinical response to carbanepenem treatment

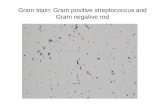
β-lactams & β-lactamases
• β-lactam antibiotics: -penicillins
-cephalosporins-carbapenems
• Inhibit cell wall formation• β lactamases = bacterial enzymes that
hydrolyse β lactam antibiotics rendering them inactive

β-lactams

β-lactamases
• Resistance to penicillins such as ampicillin or amoxicillin very common among coliforms, due to β lactamases (TEM or SHV)– E.g. 60% of invasive E coli isolates in UK are
amp-/amoxicillin-resistant)

β-lactamases
Urine culture Auth
10^5 Escherichia coli /ml
Amoxicillin R Nitrofurantoin S Cefalexin/cefradine S Ciprofloxacin SCo-amoxiclav S Gentamicin STrimethoprim S

Extended-spectrum β-lactamases (ESBLs)
• ESBLs are a group of β lactamases which are capable of hydrolysing (and therefore causing resistance to) not only penicillins, but many other β lactams, including 2nd and 3rd generation cephalosporins
• Initially recognised in clinical isolates of Klebsiella pneumoniae in the 1980s, derived from TEM or SHV β lactamases by point mutation
• Until 2000, most were TEM/SHV

ESBLs
• Since then, CTX-M increasingly prevalent – more than 50 distinct enzymes identified – transferred via plasmids from environmental bacteria (Kluyvera)
• Initially found in South America, now global problem, including in community acquired E coli
• Increasing due to plasmid spread plus clonal expansion eg CTX-M-15 in UK

ESBLs
Urine culture Auth
10^5 Escherichia coli /ml
Amoxycillin R Cefalexin/cefradine R
Cefuroxime R
Cefotaxime R
Ceftazidime R

Clinical relevance – Antibiotic management
• Now present in the most common Gram-negative infector of humans (E.coli)
• Difficult to treat• Resistant to most beta-lactams including 3rd
generation cephalosporins • ESBL + isolates often display co-resistance
to other classes of antibiotics e.g. trimethoprim, fluoroquinolones, aminoglycosides
• Penicillin-inhibitor combinations (e.g. co-amoxiclav, pip-tazo) may appear sensitive in vitro but often result in treatment failure

ESBLs
Urine culture Auth
10^5 Escherichia coli /ml
Amoxycillin R Trimethoprim R Cefuroxime R Ciprofloxacin R
Cefalexin/cefradine R Gentamicin R
Cefotaxime R Augmentin (S) Ceftazidime R Tazocin (S)

Clinical relevance – Antibiotic management
• Outpatient management of uncomplicated UTI – limited oral & once-daily IV options

Clinical relevance – Antibiotic management
• Surviving sepsis – early initiation of appropriate antimicrobials important factor in determining outcome
• Studies have shown that mortality from sepsis due to multi-resistant bacteria is double that of sensitive bacteria

Clinical relevance – Epidemiology
• E. coli and Klebsiella pneumoniae are the major ESBL producers worldwide
• E. coli is primary commensal of the human bowel and the commonest causes in community and hospital settings of:– UTI– Intra-abdominal sepsis– Bacteraemia

Clinical relevance – Epidemiology
• Gram negative infection is increasingly common
• Bacteraemia due to coliforms, particularly E coli, is increasing:
E coli is the commonest cause of bacteraemia in England

Bacteraemia

35% increase in E coli bacteraemias in England, Wales and N Ireland between 2007-2011, compared with a 7% decrease in all bacteraemias

E coli bacteraemia by ageHPA voluntary data
Livermore, D. Tracing, tracking and tackling the big beasts of bacteraemia - Resistance and treatment issues in bloodstream infections ? E. coli. in Federation of Infection Societies (FIS) Scientific Meeting. 2012. Liverpool, UK, Abstract. SA62

Local data2
00
5-Q
tr1
20
05
-Qtr
2
20
05
-Qtr
3
20
05
-Qtr
4
20
06
-Qtr
1
20
06
-Qtr
2
20
06
-Qtr
3
20
06
-Qtr
4
20
07
-Qtr
1
20
07
-Qtr
2
20
07
-Qtr
3
20
07
-Qtr
4
20
08
-Qtr
1
20
08
-Qtr
2
20
08
-Qtr
3
20
08
-Qtr
4
20
09
-Qtr
1
20
09
-Qtr
2
20
09
-Qtr
3
20
09
-Qtr
4
20
10
-Qtr
1
20
10
-Qtr
2
20
10
-Qtr
3
20
10
-Qtr
4
20
11
-Qtr
1
20
11
-Qtr
2
20
11
-Qtr
3
20
11
-Qtr
4
20
12
-Qtr
1
20
12
-Qtr
2
20
12
-Qtr
3
20
12
-Qtr
4
0
10
20
30
40
50
60
70
80
90
100
UHSFT E. coli Bacteraemias
No
. of
Pa
tie
nt
Iso
late
s/1
4 d
ay
pe
rio
d

Local data2
00
5-Q
tr2
20
05
-Qtr
3
20
05
-Qtr
4
20
06
-Qtr
1
20
06
-Qtr
2
20
06
-Qtr
3
20
06
-Qtr
4
20
07
-Qtr
1
20
07
-Qtr
2
20
07
-Qtr
3
20
07
-Qtr
4
20
08
-Qtr
1
20
08
-Qtr
2
20
08
-Qtr
3
20
08
-Qtr
4
20
09
-Qtr
1
20
09
-Qtr
2
20
09
-Qtr
3
20
09
-Qtr
4
20
10
-Qtr
1
20
10
-Qtr
2
20
10
-Qtr
3
20
10
-Qtr
4
20
11
-Qtr
1
20
11
-Qtr
2
20
11
-Qtr
3
20
11
-Qtr
4
20
12
-Qtr
1
20
12
-Qtr
2
20
12
-Qtr
3
20
12
-Qtr
4
0
10
20
30
40
50
60
70
80
90
100
UHSFT E. coli Bacteraemias
Hospital Acquired Community Acquired
No
. of
Pa
tie
nt
Iso
late
s/1
4 d
ay
pe
rio
d

Resistance
• 10% of E coli bacteraemia isolates from UK were resistant to 3rd generation cephalosporins in 2011

Resistance in E coli bacteraemia HPA voluntary data
Livermore, D. Tracing, tracking and tackling the big beasts of bacteraemia - Resistance and treatment issues in bloodstream infections ? E. coli. in Federation of Infection Societies (FIS) Scientific Meeting. 2012. Liverpool, UK, Abstract. SA62

Risk factors for resistance
• Elderly• Antibiotic exposure (third generation
cephalosporins, quinolones)• Healthcare contact• Travel from higher prevalence areas• But many pts have no risk factors

2007
2011

Local data2
00
6-Q
tr1
20
06
-Qtr
2
20
06
-Qtr
3
20
06
-Qtr
4
20
07
-Qtr
1
20
07
-Qtr
2
20
07
-Qtr
3
20
07
-Qtr
4
20
08
-Qtr
1
20
08
-Qtr
2
20
08
-Qtr
3
20
08
-Qtr
4
20
09
-Qtr
1
20
09
-Qtr
2
20
09
-Qtr
3
20
09
-Qtr
4
20
10
-Qtr
1
20
10
-Qtr
2
20
10
-Qtr
3
20
10
-Qtr
4
20
11
-Qtr
1
20
11
-Qtr
2
20
11
-Qtr
3
20
11
-Qtr
4
20
12
-Qtr
1
20
12
-Qtr
2
20
12
-Qtr
3
20
12
-Qtr
4
0
500
1,000
1,500
2,000
2,500
3,000
3,500
4,000
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Antibiotic Resistance in E. coli Urine Isolates
Total Isolates % Cefotaxime or Ceftazidime Resistant % Resistant to Gentamicin % Resistant to Ciprofloxacin
% Resistant to Trimethoprim % Resistant to Nitrofurantoin
No
. o
f U
rin
e I
so
late
s
Pe
rce
nta
ge
Re
sis
tan
ce

ESBL-E.coli in urine (UHS, 2009-2012)
Concomitant resistance to:• Trimethoprim 83%• Ciprofloxacin 69%• Nitrofurantoin 5%• Gentamicin 25%
Local data

Antibiotic options• Carbapenems widely considered antibiotic of
choice for severe ESBL infection: good clinical outcome data when compared with other agents with in-vitro susceptibility
• Aminoglycosides, if susceptible• Quinolones, if susceptible• Nitrofurantoin, if susceptible, for uncomplicated
UTI only• Other orals: fosfomycin, pivmecillinam• Tigecycline

So why not give everyone meropenem?

UHS broad-spectrum antibiotic prescribing
0
1000
2000
3000
4000
5000
6000Q
tr1
Qtr
2
Qtr
3
Qtr
4
Qtr
1
Qtr
2
Qtr
3
Qtr
4
Qtr
1
Qtr
2
Qtr
3
Qtr
4
Qtr
1
Qtr
2
Qtr
3
Qtr
4
Qtr
1
Qtr
2
Qtr
3
Qtr
4
Qtr
1
Qtr
2
Qtr
3
Qtr
4
Qtr
1
2006 2007 2008 2009 2010 2011 2012
Sta
nd
ard
tre
atm
en
t d
ay
s p
er
qu
art
er
Meropenem
Piperacillin/Tazobactam
Sum of Total DDD
Years Issue Date
Drug Type
Kieran Hand, Consultant pharmacist UHS


Case 2
• 28M with congenital biliary dilatation• Presented Sept 2012 with biliary sepsis• Recurrent sepsis with bacteraemia since then• Not amenable to drainage, awaiting liver transplant• Klebsiella pneumoniae recurrently isolated: sensitive
only to ertapenem, meropenem, amikacin and colistin• Repeated courses of carbapenem treatment• Frequent relapses after standard courses therefore
treated with 6 week course of ertapenem

• During 6th week of treatment, fever recurred with breakthrough bacteraemia
• Isolate now ertapenem resistant• Treated with meropenem for 2 weeks• Developed eosinophilia and itch, meropenem
stopped• Recurrent symptoms within 48 hours of
stopping, with recurrent bacteraemia on admission 2 days later

• Isolate showing reduced susceptibility to carbapenems: ref lab report suggests possible metallo-carbapenamase
• Pt is antibiotic dependent• Source control impossible without
transplant• Very limited antibiotic options



Dangers of meropenem overuse
Emergence of carbapenem resistance, esp. K. pneumoniae
• Carbapenemases:– E.g. KPC, NDM-1, VIM, OXA-48
• Other mechanisms:– Accumulation of different β-lactamases – Hyper-production of β-lactamases – Cell membrane porin loss (loss of permeability)– Combinations of the above

Carbapenemase-producing Enterobacteriaceae referred to Health Protection Agency (Colindale) 2003 to 2011

• KPC most prominent – first reported in USA, since 2006 has spread across US, Israel, Greece, Italy with outbreaks in China, Brazil, other European countries. 40% prevalence in Klebsiella pneumoniae bacteraemia in Greece
• NDM occurs in 2-8% of Enterobacteriaceae in teaching hospitals in India, and 27% of inpatients at two military hospitals in Pakistan were carriers

Antibiotic suceptibilities of carbapenemase-producing Enterobacteriaceae from the UK
Health Protection Agency

• Colistin – nephrotoxic and neurotoxic
• Tigecycline – low blood concentrations, unsuitable for UTI as only 22% excreted in urine
• Fosfomycin – borderline susceptibility common in Klebsiella. Not marketed in UK but can import

Control
• Organisms present in gut• Selected for by use of carbapenems, become
predominant flora: judicious use of antibiotics• Control spread: isolation (particularly diarrhoea),
handwashing, identification of carriers, ANTT of drains, environmental cleaning
• Controlling source of infection – pts with undrainable abdominal sepsis present high risk for breeding resistance

Take home points
1. E coli causing a rising number and proportion of bacteraemias
2. Resistance to carbapenems a genuine threat
3. Look at previous microbiology results when choosing empirical treatment regimens for sepsis
4. Carbapenems should be used judiciously




Health Protection Agency

Local data2
00
6-Q
tr1
20
06
-Qtr
2
20
06
-Qtr
3
20
06
-Qtr
4
20
07
-Qtr
1
20
07
-Qtr
2
20
07
-Qtr
3
20
07
-Qtr
4
20
08
-Qtr
1
20
08
-Qtr
2
20
08
-Qtr
3
20
08
-Qtr
4
20
09
-Qtr
1
20
09
-Qtr
2
20
09
-Qtr
3
20
09
-Qtr
4
20
10
-Qtr
1
20
10
-Qtr
2
20
10
-Qtr
3
20
10
-Qtr
4
20
11
-Qtr
1
20
11
-Qtr
2
20
11
-Qtr
3
20
11
-Qtr
4
20
12
-Qtr
1
20
12
-Qtr
2
20
12
-Qtr
3
20
12
-Qtr
4
0
500
1,000
1,500
2,000
2,500
3,000
3,500
4,000
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Antibiotic Resistance in E. coli Urine Isolates
Total Isolates % Cefotaxime or Ceftazidime Resistant % Resistant to Gentamicin % Resistant to Ciprofloxacin
% Resistant to Trimethoprim % Resistant to Nitrofurantoin % Resistant to Co-amoxiclav
No
. o
f U
rin
e I
so
late
s
Pe
rce
nta
ge
Re
sis
tan
ce