Repetitive blast exposure in mice and combat veterans ... · Here, blast-exposed veterans reported...
Transcript of Repetitive blast exposure in mice and combat veterans ... · Here, blast-exposed veterans reported...

R E S EARCH ART I C L E
TRAUMAT I C BRA IN IN JURY
http://sD
ownloaded from
Repetitive blast exposure in mice and combat veteranscauses persistent cerebellar dysfunctionJames S. Meabon,1,2 Bertrand R. Huber,3 Donna J. Cross,4 Todd L. Richards,4 Satoshi Minoshima,5
Kathleen F. Pagulayan,1,2 Ge Li,1,2,6 Kole D. Meeker,6 Brian C. Kraemer,6,7 Eric C. Petrie,1,2
Murray A. Raskind,1,2 Elaine R. Peskind,1,2 David G. Cook6,7,8*
Blast exposure can cause mild traumatic brain injury (TBI) in mice and other mammals. However, there are importantgaps in our understanding of the neuropathology underlying repetitive blast exposure in animal models compared tothe neuroimaging abnormalities observed in blast-exposed veterans. Moreover, how an increase in the number of blastexposures affects neuroimaging endpoints in blast-exposed humans is not well understood. We asked whether there is adose-response relationship between the number of blast-related mild TBIs and uptake of 18F-fluorodeoxyglucose (FDG),a commonly used indicator of neuronal activity, in the brains of blast-exposed veterans with mild TBI. We found that thenumber of blast exposures correlated with FDG uptake in the cerebellum of veterans. In mice, blast exposure producedmicrolesions in the blood-brain barrier (BBB) predominantly in the ventral cerebellum. Purkinje cells associated withthese BBBmicrolesions displayed plasmamembrane disruptions and aberrant expression of phosphorylated tau protein.Purkinje cell loss was most pronounced in the ventral cerebellar lobules, suggesting that early-stage breakdown of BBBintegrity may be an important factor driving long-term brain changes. Blast exposure caused reactive gliosis in mousecerebellum, particularly in the deep cerebellar nuclei. Diffusion tensor imaging tractography of the cerebellum of blast-exposed veterans revealed that mean diffusivity correlated negatively with the number of blast-related mild TBIs.Together, these results argue that the cerebellum is vulnerable to repetitive mild TBI in both mice and humans.
tm.sc
by guest on Novem
ber 20, 2020iencem
ag.org/
INTRODUCTION
There is mounting concern that blast exposure may initiate latent patho-logical processes leading to chronic traumatic encephalopathy or other re-lated neurodegenerative disorders (1–6). Detonation of high explosives caninflict brain injury in at least three ways: primary blast effects due to blastoverpressure, secondary blast effects caused by fragmented objects or shrap-nel inflicting trauma when hitting the head, and tertiary effects causedby the head striking other objects (7). Even without direct blunt impactsor significant head acceleration/deceleration from secondary and tertiaryimpacts (8), blast overpressure is capable of injuring the brain (7, 9–15).
The prevalence of repetitive blast-related mild traumatic brain injuries(TBIs) among Iraq and Afghanistan veterans (16, 17) has spurred intensiveefforts to understand its cognitive and pathological consequences in bothhumans and animal models. Studies in mice, rats, swine, and other mam-mals have demonstrated that the intense energy imparted by blastoverpressure is sufficient to induce an array of neuropathological and be-havioral disturbances (7, 9–14, 18–21).
Neuroimaging studies of military service members and veterans havedocumented chronic abnormalities on 18F-fluorodeoxyglucose (FDG)positron emission tomography (PET) imaging, which assesses glucosemetabolic activity in the brain (4, 22, 23). Abnormalities of brain white mat-ter tract structural integrity andmyelin density in these veteran populations
1Mental Illness Research, Education, and Clinical Center, VA Puget Sound Health CareSystem (VA Puget Sound), Seattle, WA 98108, USA. 2Department of Psychiatry andBehavioral Sciences, University of Washington, Seattle, WA 98195, USA. 3VA Jamaica Plain,Department of Neurology, Boston University School of Medicine, Jamaica Plain, MA02130, USA. 4Department of Radiology, University of Washington, Seattle, WA 98195, USA.5Department of Radiology, University of Utah, Salt Lake City, UT 84132, USA. 6GeriatricResearch Education and Clinical Center, VA Puget Sound Health Care System, Seattle, WA98108, USA. 7Department of Medicine, University of Washington, Seattle, WA 98195, USA.8Department of Pharmacology, University of Washington, Seattle, WA 98195, USA.*Corresponding author. E-mail: [email protected]
www.Scien
have also been characterized using magnetic resonance diffusion tensorimaging (DTI) and macromolecular proton fraction mapping (5, 24–26).
Multiple research groups, including ours, have shown that blast exposurein mice permits study of well-characterized mild to moderate effects of blastoverpressure with attenuated secondary and tertiary injury components,thereby affording new opportunities for mechanistic pathological and ge-netic investigations that are difficult to achieve in any other species (7, 9–15).Nonetheless, it remains challenging to assess potential correlations betweenthis animal model and neuroimaging findings in patients with blast-relatedmild TBIs and blast-induced neuropathology in specific anatomicalbrain regions. This is due in part to interspecies differences in cerebralcortical gray matter and subcortical white matter anatomy betweenhumans (a gyrencephalic species) and rodents (a lissencephalic species).
The cerebellum, however, is gyrencephalic in both humans and rodentsand has broadly similar structural organization in both species. Findingsfrom previous neuropathological studies in rodents (7, 9–15, 27) andneuroimaging studies in human subjects (3–5, 26, 28–31) suggest thatthe cerebellum is susceptible to blast injury. A growing body of data sug-gest that the cerebellum, in addition to controlling motor-related func-tions, subserves important cognitive and affective functions that maybe specifically related to cognitive and behavioral symptoms in blast-exposed individuals (32–35). Therefore, we investigated the consequencesof repetitive blast exposure in the cerebellum of mice and humans.
RESULTS
An increase in the number of blast exposures is associatedwith lower cerebellar glucose metabolism in veterans withblast-related mild TBISeveral FDG-PET studies have demonstrated lower metabolic activityin a number of brain regions including the cerebellum in veterans with
ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 1

R E S EARCH ART I C L E
by guesthttp://stm
.sciencemag.org/
Dow
nloaded from
blast-related mild TBI compared to veterans without blast exposure (5, 22)or nonmilitary controls (4, 36). Nonetheless, the significance of gradedincreases in the number of blast exposures on subsequent chronic brainglucose hypometabolism has not been addressed directly. Among ourstudy cohort of blast-exposed veterans with mild TBI (Table 1), thenumber of blasts experienced by each individual varied considerably,ranging from 1 to >100 reported blast events that caused acute symptomsconsistent with mild TBI. This wide range in the number of blast-relatedmild TBIs in a well-characterized cohort (5) presented an opportunity totest the hypothesis that an increasing number of blast events would beassociated with a greater degree of chronic brain glucose hypometabolismand would allow us to address the possibility that the cerebellum may bevulnerable to injury from repetitive blast exposure.
Here, blast-exposed veterans reported experiencing an average of21 (median, 11; range, 1 to 102) blast-related mild TBIs during the en-tire period of their military service (Table 1). Among this group, 21, 52,and 27% reported 1 to 5, 6 to 20, and 21 to 102 blast-related mild TBIs,respectively. The number of mild TBIs associated with loss of con-sciousness from any cause was relatively low (average of 2.3 lifetime mildTBIs; Table 1). The average time from the last blast-related mild TBIto imaging with FDG-PET was 3.6 years.
Figure 1A shows a statistical parametric map of the mean voxel-wise correlations between brain metabolic activity (normalized to globalactivity) and log10-transformed number of blast exposures among the33 blast-exposed veterans. The brightest colors (yellow, z score rangefrom −4 to −5) denote brain regions with the strongest negative corre-lations between blast number and glucose metabolism. Statistical sig-nificance following correction for multiple comparisons was achievedin three brain areas, all of which were localized within the right in-ferior semilunar lobule of the cerebellum (z scores, 4.02, 4.09, and4.37, respectively; P ≤ 0.05; see Supplementary Methods).
Using an alternative, independent analytical approach, we also cor-related blast number (log10) versus mean metabolic activity in regions
www.Scien
on Novem
ber 20, 2020
of interest circumscribing the entire left and right cerebellar hemi-spheres. Figure 1B shows that this method also revealed a statisticallysignificant negative correlation between the number of blast-relatedmild TBIs and cerebellar metabolism [Spearman r = −0.433 (P ≤0.012) and −0.406 (P ≤ 0.019) for left and right cerebellar hemispheres,respectively].
Because posttraumatic stress disorder (PTSD), depression, and al-cohol use are common in this cohort of blast-exposed veterans (4, 37)and may contribute to hypometabolism in the central nervous system(CNS), we performed multivariate regression analysis to control for po-tential confounding effects. We modeled FDG uptake in the left andright cerebellar hemispheres as a function of blast number (log10)and controlled for PTSD with the Clinician-Administered PTSD (CAPS)total score, Patient Health Questionnaire-9 (PHQ-9), and alcoholuse with the Alcohol Use Disorders Identification Test—Consumption(AUDIT-C). The associations between blast number and decreasedFDG uptake in both left and right hemispheres of the cerebellum re-mained statistically significant (log10 blast exposure, P ≤ 0.01, andlog10 blast exposure, P < 0.02, left and right cerebellar hemispheres, re-spectively). Also, none of these factors was significantly correlated withmetabolic activity in either cerebellar hemisphere (P > 0.05). Thus, theassociations between the number of blast-related mild TBIs and re-duced normalized FDGuptake in the cerebellum of veterans exposedtomild TBIswere not likely to be due to comorbid PTSD, depression, oralcohol use.
Repetitive blast exposure causes chronic neuronal loss andpersistent synaptic disturbances in murine cerebellumOur FDG-PET findings (Fig. 1) suggested the possibility that the cer-ebellum may be especially vulnerable to the cumulative effects of repetitiveblast exposure. In addition, the correlation of the number of blast exposuresand glucose hypometabolism in the cerebellum (Fig. 1A) raised the pos-sibility of subregional vulnerability within the cerebellum to blast exposure.
To address these issues in more detail, we used a mouse model ofblast-induced TBI that mimics battlefield-relevant blast overpressure inkeeping with well-established approaches.We used blast overpressure param-eters consistent with mild to moderate blast exposure (9, 38, 39). Brief-ly, 3-month-old male C57BL/6 mice were exposed to blasts using a shocktube and exposure parameters described in detail elsewhere (9). Here,mice were exposed either to one (1×) or three (3×) blast overpressureevents (24-hour interblast intervals), which were highly reproducible,with a mean peak intensity of 19.2 psi ± 0.21, initial peak wave dura-tion of 5.8 ± 0.028 ms, and a calculated impulse of 30.7 pressure persquare inch per millisecond (Fig. 2A). Under these experimentalconditions, the overall survival rate was 99%, with blast-exposed mice ap-pearing comparable to sham-exposed animals by inspection 2 hours afterblast exposure. Sham-exposed control mice were treated identically toanimals exposed to blast overpressure events: animals were anesthetized for3 to 5 min with isoflurane and mounted in the same shock tube restraintharness for the same amount of time. Each sham-exposed control animalwas yoked to a blast-exposed animal, thereby receiving either one or threesham treatments.
First, we examinedmice exposed to one blast that were administeredTexas Red–conjugated 10-kD dextran immediately before treatment. Asagittal section of the brain following clearance of peripheral circulatingdextran revealed domains of breakdown in the blood-brain barrier(BBB) as shown by regions of parenchymal dextran accumulation(Fig. 2B). At lower magnification, dextran accumulation was most
Table 1. FDG-PET (n = 33). PSQI, Pittsburgh Sleep Quality Index; NSI,Neurobehavioral Symptom Inventory.
Demographics
Mean (SD), rangeAge (years)
31.5 (9.4), 23–60Education (years)
13.7 (1.5), 11–16Race, nonwhite, n (%)
8 (24.2%)APOE-&4–positive (%)
8 (25.8%)Blast exposures
Number of blast-related mild TBIsduring military service (lifetime)
21.2 (26.7), 1–102Median = 11
Number of lifetime mild TBIs withloss of consciousness
2.3 (2.5), 0–11Median = 2
Time since last blast-related mildTBI (years)
3.6 (1.5), 1–7Median = 4
Behavioral and neurological measures
CAPS score (3 missing)
55.6 (30.5), 4–106PHQ-9 score
9.6 (7.4), 0–25PSQI score (4 missing)
9.3 (5.1), 1–19AUDIT-C score
4.8 (2.4), 0–10NSItotal score
29.4 (17.8), 2–77ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 2

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
obvious in the cerebellum, particularly in the more ventral regions(Fig. 2B). Figure 2C shows cerebellar lobule 9 of a blast-exposed mousedisplaying distinct regions of BBB breakdown.
Four-channel confocal microscopy (Fig. 2D) carried out in thesedomains of BBB breakdown revealed that within 1 to 4 hours aftera single blast, individual cerebellar Purkinje cells took up dextran(red staining) that had crossed the BBB. It has been reported previ-ously that neuronal uptake of dextran exogenously applied directlyonto the brain following TBI is associated with disturbances of theneuronal plasma membrane (40). Consistent with this, in our study,dextran uptake by Purkinje cells was evident in blast-exposed but notsham-treated animals (Fig. 2D). In addition, within the same domainin which dextran had crossed the BBB, other Purkinje cells immediatelyadjacent to the dextran-positive neuron were also exposed to parenchy-mal dextran but did not accumulate it. Although the dextran-positivePurkinje cell in Fig. 2D appeared morphologically normal followingblast exposure, accumulation of extracellular parenchymal dextran indi-cated early-stage neuronal dysfunction. To obtain initial insight into theloss of BBB integrity in different cerebellar lobules, Fig. 2E shows theresults of an analysis where a line of interest (see SupplementaryMethods) was traced along the cerebellar molecular layer of sagittalbrain sections from dextran-treated blast-exposed and sham-treated
www.ScienceTranslationalMedicine.org 1
animals. Figure 2E shows that lobule bylobule, relative to sham-treated mice, theamount of Texas Red–conjugated 10-kDdextran that crossed the BBB into thebrain parenchyma was greater in blast-exposed animals, with lobule 9 showingthe greatest effect (t12 = 2.15, P ≤ 0.05,n = 7, blast-exposed and sham-exposed,respectively). Figure 2F shows represent-ative confocal images from a sham-exposedand a blast-exposed animal, where TexasRed–conjugated dextran crossed the BBBinto the cerebellar parenchyma with subse-quent Purkinje cell dextran uptake 1 hourafter a single blast exposure. This was ac-companied by aberrant expression of phos-phorylated tau in brain parenchyma.Aberrant expression of phosphorylatedtau was further confirmed using a differ-ent rabbit anti-tau antibody in the samemice (Fig. 2G). In addition, Western blotanalysis confirmed that a single blast in-duced increased expression of multiplephosphorylated tau species in the cere-bellum within 1 hour (Fig. 2H). Threedays after a single blast exposure, 1,4,5-trisphosphate receptor type 1 (IP3R1) im-munostaining (a morphological markerof Purkinje cells) in lobule 9 (Fig. 2I) re-vealed dystrophic Purkinje cells (blackarrowheads). Together, these data sug-gest that blast exposure disturbs cerebel-lar BBB integrity, which is associatedwith early accumulation of aberrantphosphorylated tau and neuronal plasmamembrane dysfunction.
The FDG-PET findings in the blast-exposed veterans argue thatthe chronic consequences of repetitive blast exposure are demonstrablein the cerebellum (Fig. 1). The findings in blast-exposed mice indicatethat even a single blast is sufficient to evoke aberrant phosphorylatedtau accumulation and uptake of microvessel-derived dextran indicativeof neuronal injury (Fig. 2). To address directly whether repetitive blastexposure causes permanent and specific subregional cerebellar Purkinjecell loss, we quantified “empty baskets” (a term referring to the denseaxonal terminals from basket cells enveloping Purkinje cell bodies thatpersist long after Purkinje cells have been lost) in mice 30 days afterthey were exposed to either one or three blasts.
Fixed cerebellar sections (50 mm) were serially imaged by confocalmicroscopy (22 scans at 2.27-mm intervals in the z plane). Figure 3Ashows a merged maximum field projection with orthogonal views oflobule 9 in the x-y plane with basket cell processes (immunostainedgreen with anti-neurofilament heavy chain antibodies) envelopingthe soma of Purkinje cells (immunostained red with anti-IP3R1 anti-bodies). The corresponding serially reconstructed z-plane image stacksalong the indicated image planes (white lines) are depicted above andto the right of merged x-y images. We observed distributed, patchymicrodomains of empty baskets in mice exposed to three blasts com-pared to sham-exposed animals 30 days after exposure.
Fig. 1. Number of blast exposures is associated with decreased FDG uptake in the cerebellum ofveterans with mild TBI. (A) Distribution and relative magnitude of negative correlations between log
10number of blast exposures and FDG uptake by the human brain (normalized to global activity) overlaid onmagnetic resonance template images for anatomical orientation. Shown are right lateral (RT LAT), leftlateral (LT LAT), right medial (RT MED), left medial (LT MED), and inferior (INF) aspects of the human brain.Scale bar indicates z scores. A greater number of log10 blast exposures were associated with decreasedmetabolic activity in three adjacent loci within the right inferior semilunar lobule by whole-brain voxel-wise analyses. (B) Scatter plots of the mean activity in predefined cerebellar hemisphere volumes of interest(VOIs; left and right cerebellum) versus log10 number of blast exposures during military service. There was astatistically significant negative correlation between the number of blast exposures (log10) and FDG uptakein each cerebellar hemisphere VOI (Spearman r correlations, n = 33).3 January 2016 Vol 8 Issue 321 321ra6 3

R E S EARCH ART I C L E
www.S
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
l
-
r
--
r
r
-
-
l-
-
-
--
--.:
-
t
Thirty days after treatment, empty baskets were quantified in eachof the eight major cerebellar lobules (Fig. 3B) in 1× blast– and 3× blast–exposed mice. Quantification of empty baskets in sham-exposed micerevealed no statistically significant differences between 1× and 3×animals in any cerebellar lobule. Therefore, these groups were combinedas a single composite sham group for each lobule. Results among the 1×blast– and 3× blast–exposed mice are presented as a ratio of empty basketsin blast-exposed versus sham-exposed mice (Fig. 3, C and D). Analysis ofthe results shown in Fig. 3C revealed a statistically significant effect of re-petitive blast exposure in both the ventral cerebellar lobules (7 to 10) andthe dorsal cerebellar lobules (1 to 6) (F2,26 = 14.997, P ≤ 0.0001, andF2,26 = 6.356, P ≤ 0.01, respectively). This confirmed that repetitive
cien
blast exposure produced chronic cerebellar Purkinje cell loss. Furtherinspection also revealed that although 3× blast exposure caused Pur-kinje cell loss throughout the cerebellum, the ventral lobules appearedto be more vulnerable to Purkinje cell loss after a single blast exposure.This was confirmed by a planned Helmert comparison test of blast (1×and 3×) versus sham, which showed statistically significant differences inPurkinje cell loss in the ventral (P < 0.01) but not the dorsal cerebellum.
ANOVA tests of empty baskets in cerebellar lobules of sham-, 1×blast–, and 3× blast–exposed mice (Fig. 3D) further confirmed thatrepetitive blast exposure caused Purkinje cell loss throughout the cer-ebellum. However, the more ventral subregions of the cerebellum weremore vulnerable to Purkinje cell loss: lobules 1/2, F2,22 = 2.678, n.s.;
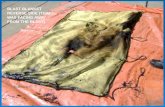
Fig. 2. A single blast causes inferior cerebellar BBB dysfunction andPurkinje cell injury in amousemodel ofmild TBI. (A) Shock tube–generated
highly reproducible battlefield-relevant blast overpressure. The red traceshows the time (ms) versus pressure (psi) measured 5 cm above the animaaveraged among n = 32 blast overpressure waveforms that were collectedover a randomly selected 2-day period (black bars indicate ±SEM). Superimposed blue Friedlander waveform illustrates the close correspondenceof the shock tube–generated blast overpressure to thewaveformexpectedfrom an open-field detonation of about 22.4 kg of trinitrotoluene (TNT) at adistance of 6.1m. (B) Blast-exposed mice were retro-orbitally loaded with10-kDdextran labeledwith Texas Red; theywere allowed to recover for 1 o4 hours after a single blast exposure, and brain slices were observed usingconfocal microscopy. Blast-specific dextran (red) labeling was most frequently observed in the cerebellum (white arrowheads). Shown is an example of amouse brain slice (50 mmthickness) 1 hour after treatment. (C) TexasRed–labeled dextran in the blood that crossed the BBB into the cerebellaparenchymawas observed at both 1 and 4 hours after blast exposure (redhighlights). Extravasated dextran was most noticeable in the cerebellamolecular layer. DAPI, 4′,6-diamidino-2-phenylindole. (D) Blast-exposedPurkinje cells that internalized dextran that had crossed the BBB were associated with morphologically distinct microglia (green) that appeared to beactivated. (n = 20 blast-treated animals, 19 of 73 brain slices had dextranlabeled Purkinje cells with only one cell (a granule cell) labeled in theupper half of the cerebellum; n= 20 sham-treated animals, with 0 of 75 slicesshowing dextran-positive Purkinje cells. GFAP, glial fibrillary acidicprotein. (E) To assess regional BBB breakdown, the linear pixel-by-pixemean dextran fluorescence intensity within themolecular layer of the cerebellum was measured across each lobe and plotted. Results show themean normalized with respect to values for seven sham-treated and seven blast-treated animals. Only lobule 9 showed evidence of increaseddextran fluorescence (P ≤ 0.05, two-tailed t test; mean = 1.65 and 1.0for blast- and sham-treated animals, respectively). (F) Confocal microscopy revealed elevated aberrant tau phosphorylated at Ser396 (detectedwith mouse monoclonal anti-tau396 antibody) in blast-treated versussham-treated cerebellum. (G) Confocal microscopy revealed elevated aberrant tau phosphorylated at Ser396 (detected with rabbit anti-tau396 antibody) in blast-treated versus sham-treated cerebellum. (H) In mousecerebellum, multiple pathological forms of phosphorylated tau were observed 1 to 4 hours after blast exposure. Representative Western blots illustrate blast-induced elevation of phosphorylated tau in mouse cerebellumEach lane corresponds to one sham-treated or blast-exposed animal (1 hourn = 4, 4 hours: n = 4; n = 3 sham-treated and n = 4 blast-exposed). Pyruvatekinase (PK) was the gel protein loading control. (I) Three days after experimental treatment, Purkinje cell injury (black arrowheads) was observed inthe form of swollen cell bodies, cell membrane breakdown, and aberranIP3R1 staining in two of three blast-exposed animals. Similar Purkinje cell dys- morphologywas not observed in sham-treated animals (n= 0/3). Images are representative examples from lobule 9, taken at 20×. Slideswere prepared usingantibodies against IP3R1 and standard immunohistochemistry. Scale bars, 500 mm (B), 250 mm (C), and 50 mm (D, F, and G). (F) and (G) represent data from fivesham-treated and five blast-exposed animals. Error bars represent SEM. *P ≤ 0.05, two-tailed t test.ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 4

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
lobule 3, F2,25 = 3.617, P ≤ 0.042; lobules 4/5, F2,23 = 2.372, n.s.; lobule6, F2,26 = 1.857, n.s.; lobule 7, F2,23 = 3.562, P ≤ 0.045; lobule 8, F2,26 =4.369, P ≤ 0.023; lobule 9, F2,22 = 6.738, P ≤ 0.005; lobule 10, F2,24 =7.298, P ≤ 0.003.
In keeping with the Purkinje cell loss findings, Fig. 4 shows that 30 daysafter blast exposure, the mice showed impaired rotarod performancein the 3× but not the 1× blast group (F1,37 = 0.423, n.s., 1× blast; F1,6 =7.477, P ≤ 0.034, 3× blast). In addition, a two-way mixed between/within-subjects ANOVA comparing 1×, 3×, and sham controls (1× sham–and 3× sham–treated mice were not significantly different and thus werepooled) further confirmed that repetitive blast exposure decreasedmotor performance on the rotarod test (F2,44 = 5.603, P ≤ 0.007).
To address the consequences of blast exposure on synaptic proteins,we examined the expression of the glutamatergic synaptic scaffold-ing protein PSD-95 (postsynaptic density-95) (41) and of GABAB-R1
(g-aminobutyric acid B receptor 1) by Western blotting (Fig. 5, A andB). Onemonth after a single blast exposure, PSD-95 protein expression,
www.Scien
but not GABAB-R1 expression, was significantly reduced compared tosham-treated animals (t8 = −5.988, P≤ 0.0003; t8 = −0.003, n.s., respec-tively). Additional experiments in Fig. 5C showed that blast-inducedloss of PSD-95 expression in the cerebellum developed slowly. Therewere no significant differences between sham-treated and 1× blast–exposed animals at 1 day after exposure (F1,7 = 0.262, n.s.). However,at the 30-day time point, PSD-95 expressionwas significantly reduced in1× blast– and 3× blast–exposed animals compared to sham-treatedcontrols (F2,26 = 6.392, P ≤ 0.006). Confocal microscopy carried out120 days after 3× blast exposure also indicated that PSD-95 expressionwithin the cerebellar molecular layer was reduced compared to 3× shamcontrols (Fig. 5, D and E).
Repetitive blast exposure causes persistent cerebellar whitematter and glial neuropathologyTo investigate the consequences of repetitive blast exposure on cere-bellar white matter tracts in mice, we first performed Bielschowsky
Fig. 3. Purkinje cell loss increases with the number of blast exposuresin mice. (A) Representative confocal images of cerebellar lobule 9 in sham-
baskets observed in sham-treated mice (n = 10, 7, and 12 for sham-treated, 1×blast–exposed, and 3× blast–exposedmice, respectively). In both dorsal/superior
and 3× blast–treated mice 30 days after treatment. Images show a mergedmaximumprojection of 22 scans acquired at 2.27-mm intervals in the z planeimmunostained for neurofilament heavy chain (NF-HC)–positive basket cells(green) and IP3R1-positive Purkinje cells (red). Blast-exposed cerebellumdisplayed prominentmicrodomains of Purkinje cell loss (empty baskets) thatwere also apparent when viewed along the z plane for highlighted regions(white boxes) projected above and to the right of themerged x-y images. (B)For illustrative purposes, this sagittal section denotes cerebellar lobule anat-omy(lobules1/2to10). (C)Histogramshowsemptybasket frequencies in1×blast–and 3× blast–exposed mice normalized with respect to the number of empty
(lobules 1 to 6) and ventral/inferior (lobules 7 to 10) regions of the cerebellum,blast exposure caused an overall increase in empty baskets [P < 0.01 and P <0.0001, analyses of variance (ANOVAs), respectively]. 3× blast exposure causedmarked Purkinje cell loss throughout the cerebellum. However, the ventral/inferior lobules appearedmore vulnerable to Purkinje cell loss after a single blastexposure. **P < 0.01, Helmert test. (D) Histogram shows normalized emptybaskets for each lobule in the same sham-treated, 1× blast–exposed, and 3×blast–exposedmice. *P<0.05, **P<0.01, ANOVA. n.s., nonsignificant. Scale bars,50 mm (A) and 500 mm (B). Data represent mean normalized to values forsham-treated mice, with error bars indicating ±SEM.
ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 5

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
silver staining, which revealed aberrant axonal varicosities and thick-ened neuronal processes within the granule layer adjoining the deepwhite matter tracts and the Purkinje cell layer 24 hours after a singleblast exposure (Fig. 6, A and B). To further investigate the effects ofrepetitive blast exposure in cerebellar white matter, we also measuredamyloid precursor protein (APP) expression, which was easier toquantify than Bielschowsky staining (42, 43). At both 24 hours and7 days after a single blast exposure, APP expression was increasedcompared to sham-exposed animals but then returned to sham levelsby 30 days after exposure (Fig. 6, C and D). However, 30 days after a3× blast exposure, APP expression in the cerebellum remainedelevated. A two-factor ANOVA comparing treatment groups (sham-treated, 1× blast, and 3× blast) with respect to time after exposure (1, 7,and 30 days) confirmed that blast exposure significantly increasedAPP expression in the cerebellum (treatment group factor: F2,31 =9.923, P ≤ 0.0005; time post-exposure factor: F2,31 = 1.310, n.s.). Inaddition, a one-factor ANOVA comparing the overall effects of thenumber of blast exposures (sham, 1× blast, and 3× blast) was alsostatistically significant (F2,35 = 8.048, P ≤ 0.001).
To investigate prolonged consequences of blast exposure, we nextexamined GFAP immunoreactivity in the mouse cerebellum by con-focal microscopy 30 days after one or three blast exposures. Persistentlyelevated GFAP, an indication of inflammatory reactive astrocytes, wasapparent throughout the cerebellar white matter tracts (Fig. 7A). Quan-tification of relative GFAP immunoreactivity (Fig. 7B) circumscribingboth the lobular and peri-deep cerebellar nuclei white matter tracts con-firmed that GFAP expression was significantly increased 30 days afterblast exposure (F2,18 = 21.055, P < 0.001). In addition, at higher mag-nification (Fig. 7C), GFAP expression was found in white matter re-gions adjacent to deep cerebellar nuclei with statistically significantincreases in blast-exposed mice compared to sham-exposed animals(F2,18 = 25.990, P < 0.001) (Fig. 7D).
To further investigate blast-induced neuroinflammation-related re-sponses, we also carried out Iba-1 immunostaining of the mouse cer-ebellum. Figure 7E shows that 3× blast exposure evoked distinctpatches of microglia/macrophages with a morphology indicative of ac-tivation. Figure 7F shows the cumulative anatomical distribution ofthese microglial patches in 1× blast, 3× blast, and sham controls at
www.Scien
14 and 30 days after treatment. Blast-induced microglial responseswere particularly prominent in regions near the cerebellar pedunclesof mice exposed to 3× blast at 14 days after exposure.
To address this in more detail, a neuropathologist blind to treat-ment condition evaluated 13 pairs of Iba-1–immunostained confocalimages from the white matter superior to the deep cerebellar nuclei(1× blast, 3× blast, and corresponding shams, n = 5, n = 8, and n =13, respectively). Blinded pairwise (sham versus blast) comparisonswere judged on the basis of an expected overall appearance of reducedmicroglial process length/arborization and increased soma size inblast-exposed mice. The rater correctly assigned condition (blast ver-sus sham) in 84.6% of comparisons (11 of 13 correct group assign-ments; c2 = 4.9231, df = 1, P ≤ 0.027; with 4 of 5 and 7 of 8 correctresponses for the 1× and 3× blast/sham groups, respectively). As afurther confirmation, overall size of microglial processes was alsoexamined by convex hull volume analysis that calculated the volumecreated by forming a convex envelope containing all of the cellularfilaments associated with a given Iba-1–immunostained microglialcell. Figure 7G (right panel) shows convex hull volumes calculatedusing Imaris software from the representative Iba-1–immunostainedconfocal images in the left panel fromwhitematter tracts superior to thedeep cerebellar nuclei 2 weeks after sham, 1× blast, or 3× blast expo-sure. The summary histogram (Fig. 7H) indicates that convex hull vol-ume was statistically significantly reduced in Iba-1–immunostainedcells in blast-exposed animals (1× and 3×) compared to sham controls[F1,24 = 4.718, P ≤ 0.040; average number of cells examined per ani-mal = 23 (range, 15 to 34); n = 8, n = 6, n = 12; 1× blast, 3× blast, andsham controls, respectively; with sham controls from 1× and 3× groupspooled together because they were not statistically different].
Together, these data argue that blast exposure provokes amore con-tracted morphology of microglia, suggesting that the microglia wereactivated. Consistent with this, we also observed a significant increasein CD68 expression, an indication ofmicroglia/macrophage activation,on Western blots of cerebellum protein lysates obtained 2 weeks afterblast exposure (Fig. 7I) (F2,16 = 6.359, P≤ 0.01). Double-labeled fluores-cent immunostaining also showed that Iba-1–immunopositivemicroglia/macrophages coexpressed CD68, further suggesting that blast exposureprovoked microglial activation (Fig. 7J).
Number of blast-related mild TBIs correlates with meandiffusivity in deep cerebellar tracts of combat veteransThe findings in mice indicate that blast exposure can give rise topersistent neuropathology in cerebellar deep peri-peduncular/deepcerebellar nuclei regions. The results in Fig. 7 suggest that this area,which is the major route of fiber passage in and out of the cerebellum,is susceptible to injury caused by blast exposure. This prompted us tohypothesize that an increase in the number of blast exposures in com-bat veterans might correlate with structural neuroimaging measuresthat are sensitive to disturbances in the deep white matter tractstraversing the cerebellum.
To test this hypothesis, DTI tractography was carried out to definefiber tracts derived from a seed region located in areas surroundingthe bilateral dentate nuclei. Out of the total cohort of blast-exposedveterans in this study, 19 participants had magnetic resonance imag-ing (MRI) scans that were suitable for tractography analysis (Table 2).Mean diffusivity, fractional anisotropy radial diffusivity, and axial dif-fusivity were calculated for three spherical 1-cm3 volumes of interest(VOIs) within fiber tracts arising from the seed point near the dentate
Fig. 4. Repetitive blast exposure impairs motor performance in mice.(A) Single blast exposure (1×) did not alter rotarod performance in mice at
30 days after treatment (n = 20 sham-treated, n = 19 blast-exposed mice).(B) In contrast, mice exposed to 3× blast exposure showed significant im-pairment in rotarod performance compared to sham-treated mice (n = 4sham-treated, n = 5 blast-exposed; P ≤ 0.034, ANOVA). Data representmean, with error bars indicating ±SEM.ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 6

R E S EARCH ART I C L E
www.S
http://stm.scie
Dow
nloaded from
.r
lf
-
-
--,
)--
by guest on Novem
ber 20, 2020ncem
ag.org/
nucleus (see Materials and Methods). In keeping with the findings inblast-exposed mice, VOI1 and VOI2 were located in the white mattertracts near the left and right dentate nuclei, and VOI3 was located inthe middle cerebellar peduncle, a region that contains white mattertracts contiguous with those crossing through VOI1 and VOI2 (Fig. 8A)(44). The three VOIs were averaged together for each subject. Figure 8Bshows that there was a statistically significant negative correlation betweenaverage mean diffusivity–VOI(1–3) and log10 number of blast exposures(rank-order Spearman r = −0.487, P≤ 0.034). Fractional anisotropy, radialdiffusivity, and axial diffusivity, as well as average track density were notsignificantly correlated with the number of blast exposures (Spearman r =−0.201, −0.340, −0.278, and −0.106, respectively; all n.s. P > 0.05).
Whereas increasedmean diffusivity ismost often associatedwith de-myelination and neuronal loss, recent reports suggest that presympto-matic inflammation-related processes, including gliosis occurring inadvance of overt neurodegeneration, can restrict water diffusivity, thusresulting in reduced mean diffusivity (45) (see Discussion). Figure. 8 (Band C) shows representative DTI tractography images from two blast-exposed individuals, onewith 5 and the otherwith >100 blast exposures.Tract colors correspond to mean diffusivity values, with green indicat-ing a lowermean diffusivity. In this example, the whitematter tracts de-picted in the subject exposed to more blasts appear to be more green inthe highlighted region (arrow), indicative of lower mean diffusivity. Asnoted above, overall average track density for VOI(1–3) was not signifi-cantly correlated with the number of blast exposures. This suggests thatapparent tract density differences in these two examples in this angle ofview may not be representative of tract density in the group as a whole.An axial presentation of mean diffusivity with the tractography removedin the same two subjects (Fig. 8D) further corroborates that the tracto-graphy mean diffusivity observations (Fig. 8C) in the subject with >100blast exposures were lower compared to those in the subject reportingonly 5 blast exposures. The number of blast exposures (log10) did not
cien
correlate significantly with scores measuring PTSD (CAPS), depression(PHQ-9), and alcohol use (AUDIT-C) (Spearman correlation coeffi-cients = −0.012, −0.027, and −0.199, respectively; all P > 0.05; Sup-plementary Materials). Multivariate regression analysis modeling ofthe averagemean diffusivity–VOI(1–3) as a function of the number of blastexposures (log10) accounting for PTSD symptoms and PTSD-relatedfactors (CAPS, PHQ-9, AUDIT-C) still resulted in a statistically sig-nificant correlation between log10 number of blast exposures and meandiffusivity (P ≤ 0.012), thus further strengthening the conclusion thatincreasing numbers of blast exposures may be associated with reducedmean diffusivity in white matter tracts of the inferior cerebellum.
Number of blast-related mild TBIs correlates with symptomsof impaired sensorimotor integration in combat veteransSensorimotor integration is a critical function of the cerebellum. To ad-dress whether symptoms related to impaired sensorimotor integration
Fig. 5. Blast exposure reduces PSD-95 expression in mouse cerebellum(A) Western blots for PSD-95 and GABAB-R1 performed at 30 days afte
treatment showed reduced PSD-95, but not GABAB-R1, in 1× blast-exposedmice compared to sham-treated animals. Each lane shows Triton X-100–solublecerebellar protein lysates (20 mg), with one animal per lane using PK as a geprotein loading control. (B) Histograms show densitometric quantification oWestern blots in (A) normalized to sham-treated mice, which are consideredto be 1.0 (that is, 100%). Expression of PSD-95, but not GABAB-R1, was reducedby blast exposure (P ≤ 0.0003, t test; n = 5 sham-treated and n = 5 blastexposed mice). (C) Histogram shows normalized PSD-95 expression fromWestern blot experiments. One day after 1× blast exposure, PSD-95 expression was not different from sham controls (ANOVA, n.s.; n = 5 sham-treatedand n = 4 blast-exposed mice). However, 30 days after blast exposure, PSD95 expression was significantly reduced in blast-exposed animals compared to sham controls [P ≤ 0.006, ANOVA; n = 14, 11, and 4, sham-treated1× blast–exposed, and 3× blast–exposed mice, respectively; includes datapooled from (B) and (C)]. (D) Confocal microscopy confirmed decreasedPSD-95 immunostaining in cerebellum of 3× blast–exposed mice 4 monthsafter treatment. (E) At higher magnification, different sections from (Dshowed reduced PSD-95 immunopositive puncta in the cerebellar molecular layer (white arrows) of 3× blast–exposed mice 4 months after treatment compared to sham-treated mice. Results are representative of n = 5blast-exposed and n = 5 sham-treated mice. Scale bars, 500 mm (D) and50 mm (E).ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 7

R E S EARCH ART I C L E
by guest on No
http://stm.sciencem
ag.org/D
ownloaded from
correlate with an increase in the number of blast exposures, we corre-lated symptoms of dizziness, loss of balance, and poor coordination(items of the NSI) in 41 blast-exposed veterans, with the number ofblast-relatedmild TBIs (ranging from 1 to >100). Symptoms were ratedby participants as none to severe (0 to 4). Table 3 shows that the numberof blast exposures significantly correlated with sensorimotor symptomsof dizziness, loss of balance, and poor coordination (Spearman corre-lation: P≤ 0.016, P≤ 0.005, and P≤ 0.019, respectively), as well as totalsymptoms (Spearman correlation: P≤ 0.004). In addition, the associa-tion between total symptoms and the number of blast exposures re-mained statistically significant after adjusting for PTSD symptoms,depression, and alcohol use by multivariate regression analysis (P ≤0.02), thus arguing that these impairments are not likely to be theresult of comorbid PTSD, depression, or alcohol use.vember 20, 2020
DISCUSSION
Numerous reports indicate that blast-exposed individuals exhibit ab-normalities in the brain after imaging with FDG-PET, DTI, DTI tracto-graphy, or macromolecular proton fraction mapping (3–5, 26, 31, 46, 47).This raises concerns that repetitive blast exposure may set in motionlatent pathological processes that place these individuals at risk for de-veloping neurodegenerative disorders in mid-to-late life, as has beenargued for repetitive impact-related mild TBIs (48–53).
A number of obstacles currently limit our understanding of thesignificance of aberrant neuroimaging findings in veterans with blast-related mild TBIs. First, with one exception (28), most of the subjectsstudied experienced multiple mild TBIs. Second, it can be challengingto assess the relative contributions of primary blast overpressure andsecondary/tertiary (impact) injury to overall TBI symptoms andpersisting neuroimaging abnormalities. Third, little is known regard-ing early-stage pathology among individuals who currently have onlysubtle cognitive symptoms yet nonetheless have abnormal neuroima-ging findings (5).
To begin closing these important knowledge gaps, we studied theeffects of increasing numbers of blast exposures on neuronal activity
www.Scien
Fig. 6. Blast exposure induces persistent axonal injury in mice. (A)Bielschowsky silver staining of cerebellar slices from single blast-exposed
mice at 24 hours shows thickened axonal varicosities evident in axonsemanating from the Purkinje cell layer (n = 5/6 blast-exposed and n =1/5 sham-treated mice). (B) Enlarged insets from (A) numbered 1 to 4 (ar-rowheads denote axonal varicosities). (C) Representative Western blotanalyses from individual blast-treated and sham-exposed mice showedthat blast exposure increased APP expression in cerebellum. Each lane re-presents Triton X-100–soluble protein lysates (20 mg total protein per lane)for a single animal using PK or SYPRO-Ruby (SR) as a total protein loadingcontrol. (D) Histogram indicates APP normalized to values for sham-treatedmice, which are considered to be 100%. A two-factor ANOVA comparing allgroups (sham-treated, 1× blast–exposed, and 3× blast–exposed mice) withrespect to posttreatment delay (1, 7, and 30 days) confirmed that blastexposure increased APP in the cerebellum (ANOVA: treatment group,P ≤ 0.0005). Each group n = 5, except 1× blast–exposed and 1× sham–treated, which were n = 4. Error bars indicate ±SEM. Scale bars, 50 mm(A) and 10 mm (B).ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 8

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
-
)-
r-trr
,-
.--
-
-;
-
t
-
/
).
-r--
t
Fig. 7. Blast exposure inducespersistent reactive gliosis in
mouse cerebellum. (A) Representative confocal images (20 mergedscans at 2.5 mm along the z axisshow persistently elevated GFAP expression (red) in cerebellar whitematter 30 days after 1× and 3×blast–exposure. White lines indicateareas of interest (AOI) delineated bythe interior border of the cerebellagranule cell layer. (B) GFAP immunoreactivity (normalized with respecto sham-treated mice) in cerebellaAOIs circumscribing overall cerebellawhite matter was increased in theblast-exposed animals (P ≤ 0.001ANOVA; n = 8, 10, and 3 shamtreated, 1× blast–exposed and 3×blast–exposed mice, respectively)(C) In these slices, GFAP immunostaining in white matter surrounding deep cerebellar nuclei/dentatenuclei (DCN/DN) was increased (seeinsets). (D) GFAP immunoreactivity(normalized with respect to shamtreated) in cerebellum surroundingthe deep cerebellar nuclei/dentatenuclei was increased in the blastexposed animals (P ≤ 0.001, ANOVAn= 8, 10, and 3 sham-treated, 1×blast–exposed, and3×blast–exposedmice, respectively). (E) Fourteendays after treatment, Iba-1 staining(green) in the brains of 3× blast–exposed mice shows clusters of Iba1–positive cells (green). Highlightedregions (white boxes) are shownat higher magnification (far righpanels). Iba-1 immunoreactivitydoes not colocalize with GFAPpositive astrogliosis (red). (F) Thecumulative distribution of microglialmacrophage clusters was observedin the brains of individual animals(with sample size noted in panelsat 14 and 30 days after exposureAt 14 days, microglial clusterswere observed with a predominant distribution in the cerebellanuclei and white matter, with occurrences increasing near the peduncle. The number of clustersincreased with the number of blasexposures and diminished 30 days after exposure. (G) The overall volume of microglial processes was quantifiedby calculating the convex hull volume (right panels) of the Iba-1 immuno-positive cells in 285-mm2 (x, y plane) × 50-mm (z plane) images from deepcerebellar white matter from sham-treated, 1× blast–exposed, and 3× blast–exposed animals 14 days after treatment (left panel shows representativemaximum field projections). (H) Histogram shows that microglial convex hullvolume was reduced in blast-exposed animals compared to sham-treatedmice (P ≤ 0.04; n = 8, 6, and 12, 1× blast, 3× blast, and sham-treated mice,respectively). (I) Histogram of Western blot densitometry of CD68 expressionwww.Scien
(an indication of microglial/macrophage activation) in cerebellar protein ly-sates in blast-exposed mice (ANOVA: P ≤ 0.01; n = 9, 5, and 5, sham-treated,1× blast–exposed, and 3× blast–exposed mice, respectively) 14 days afterexposure. Total protein was normalized with respect to reprobing of PK im-munoreactivity. (J) Double-label confocal microscopy shows Iba-1–positivemicroglial cells (green) coexpressing CD68 (red). Data represent mean (nor-malized to sham values), with error bars indicating ± SEM. Scale bars, 250 mm(A and C), 100 mm (E, left panels, and G), 50 mm (E, right panels), and 25 mm (J).WM, white matter; ML, molecular layer; GCL, granule cell layer.
ceTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 9

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
measured by FDG-PET. We also carried out DTI tractography to assessthe structural integrity of tracts in the inferior cerebellum. We focusedon the impact of repetitive blast in the cerebellum to facilitate potentialtranslational correspondence between the neuropathological findings inblast-exposed mice and findings in blast-exposed veterans.
That unbiased whole-brain voxel-wise analyses demonstrated amarked dose-response relationship between increasing numbers ofblast-related mild TBIs and decreased metabolic activity specificallyin the cerebellum argues that the cerebellummay be particularly vulner-able to graded increases in the number of blast exposures. Our findingsin the repetitive blast-exposed mice support this notion. We found thatan increase in the number of blasts produced graded increases in Purkinjecell loss (Fig. 3). Although Purkinje cell loss was statistically significant,any specific injured neuron was surrounded by neighboring Purkinjecells that appeared, at least initially, to be intact. More extensive subclus-ters of empty baskets became apparent 30 days after mice received threeblast exposures. Although the absolute number of lost Purkinje cells wassmall compared to the number of remaining morphologically intactcells, the extensive synaptic arbors supported by each Purkinje cellmight be expected to amplify the functional consequences of individualPurkinje cell loss. In keeping with this, we observed slowly developingblast-induced reductions in the synaptic scaffolding protein, PSD-95, atleast 4 months after blast exposure, further supporting that synapses inthe cerebellum are lost or become chronically structurally abnormal.
We found that the ventral lobules (7 to 10) of the murine cerebel-lum are more vulnerable to blast-related injury compared to other re-gions of the cerebellum. This highly specific pattern of neuron losscorresponded with the overall pattern of BBB dysfunction and alteredPurkinje cell plasma membrane integrity occurring within 1 to 4 hoursof blast exposure. This suggested that early-occurring BBB distur-bances may play a key role in subsequent chronic CNS injury. Thisemphasizes the importance of developing early treatment strategies to
www.Scienc
limit the pathophysiological consequences of even limited BBB inju-ry to prevent long-term neuron loss.
The negative dose-response relationship between mild TBIs fromblast exposure and metabolic activity assessed by FDG-PET wasmost pronounced in the inferior aspect of the cerebellum in blast-exposed veterans. Nonetheless, these correlations may also includecontributions from more superior cerebellar domains, which maynot be distinguishable due to the inherently lower spatial resolutionand lack of neuroanatomical discrimination of FDG-PET imaging inhuman brains, particularly in inferior brain regions where slight co-registration mismatches may reduce localization specificity.
In landmark neuropathological studies, Corsellis and colleaguesmapped Purkinje cell loss (54) in former boxers and found an ana-tomical pattern of loss that was strikingly similar to our findings inblast-exposed mice. Specifically, they found the most prominent Pur-kinje cell loss in the inferior/ventral aspects and, to a lesser extent,limited losses in more superior domains of the cerebellum (54). Pur-kinje cell damage was one of the most prominent neuropathologicalfindings in nonhuman primates after exposure to explosive blasts thatcaused behavioral changes similar to humans with mild TBIs (55).
The neuroanatomical correspondence between blast-exposedmice and veterans with repetitive blast-related mild TBIs or formerboxers with impact-related mild TBIs raises interesting questionsabout the mechanisms by which blast injures the cerebellum. Ithas been argued that the anatomical structure of the cerebellummay render it vulnerable to injury from shear stress or rapid accel-
eration/deceleration impacts (26, 56–59), particularly impacts of theinferior cerebellar lobules against the posterior fossa and/or herniationof the cerebellar tonsils through the magnum foramen itself (54, 60).In the mouse model of blast-induced mild TBI used in this study, headmovements were attenuated (9), consistent with previous studies usingcomparably restrained movement models of blast that produce neu-ropathology and behavioral deficits (7, 11–13, 19, 39, 61–67). The blastparameters we used were comparable to those estimated to be sufficientto produce brain injury in humans without substantial acceleration/de-celeration (8). Nonetheless, it is not possible to rule out acceleration/de-celeration as a contributing injury mechanism.
Factors other than biomechanical insults may also contribute toblast-related cerebellar injury. The high basal metabolic activity ofPurkinje cells may influence their susceptibility to injury (68). Thismay partially explain their vulnerability to injury by ischemia and hy-poxia (69). The microvasculature of the Purkinje cell layer renders itvulnerable to the development of ischemia during episodes of hypoper-fusion (70), and vasospasm is uniquely associated with blast-related versusimpact-related TBI (71). Thus, these factors also may contribute to cere-bellar vulnerability to blast-related mild TBIs. In addition, unrelated todisplacement or shear stress, the cerebellum is predisposed to CNS in-sults that involve susceptibility to BBB breakdown in the experimentalautoimmune encephalomyelitis mouse model (72). Also, a large numberof human genetic diseases target the cerebellum (73). Thus, it would bepremature to conclude that any one factor governs susceptibility of thecerebellum to blast-related mild TBI. It is more likely that complex inter-actions among multiple factors underlie the correspondence we havefound between blast-exposed mice and veterans with blast-related mildTBI, and that have previously been found in former boxers (54).
In addition to Purkinje cell and synaptic disturbances, we also ob-served increased cerebellar expression of APP, axonal varicosities incerebellar white matter tracts, and persistent reactive gliosis in white
Table 2. DTI tractography (n = 19).
Demographics
Mean (SD), rangeAge (years)
33.2 (7.7), 22–52Education (years)
14.6 (1.6), 12–18Race, nonwhite, n (%)
5 (26.3%)APOE-&4 positive (%)
6 (33.3%)Blast exposures
Number of blast-related mild TBIsduring military service (lifetime)
27.1 (28.3), 3–102 Median = 15
Number of lifetime mild TBIs withloss of consciousness
2.6 (2.7), 0–11 Median = 2
Time since last blast-related mildTBI (years)
5.7 (2.2), 1–8 Median = 6
Behavioral and neurological measures
CAPS score
64.1 (28.7), 13–111PHQ-9 score
10.6 (7.9), 0–25PSQI score
10.5 (4.3), 3–17AUDIT-C score
3.4 (2.3), 0–9NSItotal score
29.5 (13.4), 4–57eTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 10

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
matter tracts in proximity to the deep cerebellar nuclei. In keepingwith previous findings in both humans and blast-exposed animals(26, 39, 55, 66, 74), these data suggest that deep cerebellar white matter tractsin blast-exposed veterans may also exhibit graded vulnerability toincreasing numbers of blast-related mild TBIs. The DTI tractographyresults (Fig. 8) were consistent with this notion, as we observed a sta-tistically significant negative correlation between blast number and meandiffusivity in these tracts.
In this regard, it is often reported that white matter damage, typ-ically exemplified by distinct myelin disruption and axonal loss, is as-sociated with increased, rather than decreased, mean diffusivity,because the loss of overall white matter integrity allows for more freelymoving water molecules in all directions (75–77). However, a growing
www.Scienc
body of data support that different types of white matter tract pathol-ogy can result in complex and sometimes opposing changes in meandiffusivity. For example, inflammatory processes such as reactive gli-osis and microgliomatosis accompanied by increased cellularity canrestrict water diffusivity (78). In some instances, a CNS insult resultsin an initial decrease in mean diffusivity or the apparent diffusion co-efficient of water (ADCw), followed by increased diffusivity (79). Simi-lar observations have recently been reported among individuals withpresenilin-1 (PS1) mutations (45). Compared to normal controls,mean diffusivity was reduced in PS1 mutation carriers before onsetof symptoms. However, mean diffusivity was increased in symptomaticAlzheimer’s disease (AD) patients with PS1 mutations compared tocontrols, thereby raising the possibility that the initial mean diffusivitydecrease may reflect early-occurring glial activation or cellular swellingpreceding overt AD-related pathology (45). Additional support for the ideathat reactive gliosis attending neurodegenerative disease processes could beassociated with decreased mean diffusivity comes from recent findings inpatients with sporadic Creutzfeldt-Jakob disease (CJD) in whomDTI analy-ses revealed widespread decreased mean diffusivity in white matter tracts(80, 81). In addition, among a limited number of CJD cases in which itwas possible to relate the mean diffusivity findings to histopathological ex-aminations, reactive astrocytic gliosis and microglial activation appeared tobe roughly associated with the degree of reduction in mean diffusivity (80).
These reports raise the possibility that our finding of lower meandiffusivity in deep cerebellar white matter in veterans with the largest
Table 3. Correlation between number (log10) blast exposures andsymptoms related to sensorimotor integration (n = 41). D, dizziness;LB, loss of balance; PC, poor coordination.
Symptom
Spearman r PDizziness
0.374 0.016Loss of balance
0.431 0.005Poor coordination
0.365 0.019Total (D + LB + PC)
0.438 0.004Fig. 8. Decreasedmean diffusivity in human cerebellum correlates withan increase in the number of blast-related TBIs. (A) Approximate spatial
posures (lower panel). Color scale represents the maximum eigenvalue ofthe tensor that is related to mean diffusivity (MD). Compared to the subject
locations of three VOIs (1 to 3) used for quantification of DTI parameters areshown on a reference T1-weighted MRI scan (Montreal Neurological Insti-tute −32 mm in z axis). (B) Scatter plot reveals a statistically significant neg-ative correlation between log10 number of blast-related mild TBIs andmean diffusivity calculated as the average of VOI 1 to 3 (Spearman r, P ≤0.034, n = 19). (C) Examples of DTI fiber tracts arising from the seed pointdefined near the dentate nucleus for one VOI in a subject with 5 reportedblast exposures (upper panel) and a subject with >100 reported blast ex-
with five blasts, the greater amount of green color in the highlighted re-gions (white arrows) in the >100 blast-exposed subject indicates a lowermean diffusivity. (D) Mean diffusivity axial images from the same twosubjects shown in (C) depicted as a mean diffusivity map. The ovals highlightthe same regions shown in (C), demonstrating lower mean diffusivity(more green) in the subject with >100 blast-related mild TBIs comparedto the subject with 5 blast exposures. Color bars represent mean diffusivityvalues (mm2/s).
eTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 11

R E S EARCH ART I C L E
by guest on Novem
bhttp://stm
.sciencemag.org/
Dow
nloaded from
number of blast exposures may indicate chronic subacute reactive gli-osis and microgliomatosis. Nonetheless, in the absence of more directneuropathological evidence and with the lack of correlated changes infractional anisotropy, this possibility remains to be confirmed. Alter-natively, the relationship between mean diffusivity and the number ofblast exposures could be due to other factors that include impairedaxonal transport, cellular swelling, or changes in crossing fiber anatomy(78, 80). It also remains unclear whether or not such underlying whitematter DTI abnormalities in these blast-related mild TBI subjects are anearly indication of latent disease processes that may later give rise toneurological symptoms.
Our study has limitations with respect to estimates of the numberof blast exposures, which relied on retrospective recollection facilitatedby a semistructured interview. However, unbiased whole-brain voxel-wiseanalysis yielded a correlation between the number of recalled blast ex-posures and glucose hypometabolism in the cerebellum. The numberof blast exposures also correlated with self-reported sensorimotor symp-toms. Another important limitation is that the possible link between de-creased mean diffusivity on diffusion tensor images in the blast-exposedveterans and mild, chronic white matter neuroinflammation-related pro-cesses is only suggestive. Nonetheless, this possibility is supported by re-cent PET translocator protein imaging data in former National FootballLeague players, suggesting that neuroinflammation is associated withrepetitive impact mild TBI (82). Despite the cell loss seen in the cerebel-lum of blast-exposed mice, which is indicative of lasting CNS injury(Fig. 3), the microglial and astrocytic pathology we observed 30 days afterrepetitive blast exposure in the mice requires further study.
The deep cerebellar white matter tracts imaged here subserve func-tional networks connecting the cerebellum with brain regions that arecritical to both cognitive and emotional function, including the prefrontalcortex and limbic regions (33, 83, 84). Thus, it is possible that the cere-bellar white matter and Purkinje cell abnormalities observed in our studycould disrupt cerebellar-cortical connections and thereby contribute tothe chronic behavioral and postconcussive symptoms that are frequent-ly observed in this population, as well as impaired sensorimotor integra-tion. Continued longitudinal investigation of the veterans in this study iscurrently under way in an effort to address this important question.
er 20, 2020
MATERIALS AND METHODS
Study designThe overall aim of this study was to investigate the neurologicalconsequences of repetitive mild TBI in the cerebellum and to testthe correlation between cerebellar injury in a mouse model of repeti-tive blast-induced mild TBI and neuroimaging findings in veteranswith multiple blast-related mild TBI. A total of 41 veterans reportingfrom 1 to greater than 100 blast-related mild TBI events were studied.All participants were male. Females were eligible for study inclusion,but no females with blast-related mild TBI were enrolled. Inclusioncriteria for all veteran participants included documented hazardousduty in Iraq and/or Afghanistan with the U.S. Armed Forces duringOperation Iraqi Freedom and/or Operation Enduring Freedom. Ve-terans with mild TBI must have had exposure to at least one blast withacute symptoms that meet VA/Department of Defense/AmericanCongress of Rehabilitation Medicine criteria for mild TBI. Exclusioncriteria for all participants included moderate-severe TBI, seizure dis-order, insulin-dependent diabetes, current DSM-IV (Diagnostic and
www.Scienc
Statistical Manual of Mental Disorders, 4th Edition) diagnosis of alco-hol abuse or other substance abuse, schizophrenia or other psychoticdisorders, bipolar disorder, or dementia, and taking medications likelyto affect cognitive performance such as opiates, benzodiazepines, andsedating antihistamines. Veterans with retained shrapnel or metalfragments or foreign objects in the eyes, skin, or body that would con-traindicate a brain MRI scan were excluded from MRI. All partici-pants who had undergone FDG-PET scanning were included in thereported FDG-PET analysis. A subset of these underwent MRI scan-ning; all of those with MRI scans of sufficient quality for DTI tractogra-phy were included in this study. Sensorimotor-related NSI symptoms forall participants in this report are included.
A total of 175male wild-type C57BL/6mice ranging in age from 3to 4 months were studied. Animals were randomly assigned to ex-perimental (blast) and control (sham) groups. Experimental groupsample sizes were based on previous pathological findings (9). ForWestern blots, entire flash-frozen cerebellum samples were analyzedand reported. Fixed floating tissue sections from each brain were col-lected into buffer holding tubes for each animal. For each experiment,fixed sections from each brain were randomly pulled from the holdingtubes; subjected to immunostaining, mounting, and confocal micros-copy; and analyzed under identical conditions for both blast-exposedversus sham control samples with subsequent data reported, includingsections with missing lobules. Except where indicated, analyses wereperformed nonblinded using identical experimental procedures fordata/image collection andwith image adjustments limited only to linearcontrast and brightness adjustments applied identically to data fromblast- and sham-treated animals in each experiment.
Human subjectsThese studies were approved by the VA Puget Sound Health CareSystem Human Subjects Committee. Participants provided writteninformed consent before study. The study conformed to institutionalregulatory guidelines and principles of human subject protection inthe Declaration of Helsinki. Veterans with mild TBI were character-ized by physical and neurological examination. Behavioral assessmentswere made for PTSD using CAPS (85), for depression using PHQ-9(86), for alcohol consumption using AUDIT-C (87), and for potentialpostconcussive symptoms using NSI. A lifetime history of both blast-related and impact-related mild TBI was obtained using a semi-structured interview by two expert clinicians [described in detailelsewhere (5)]. FDG-PET and DTI were performed within 3 monthsof clinical evaluation. Participants with retained shrapnel did notundergo DTI.
Animal subjectsThis study used wild-type C57BL/6 male, 3- to 4-month-old mice(The Jackson Laboratory) that were group-housed with access to foodand water ad libitum. All animal experiments were conducted in ac-cordance with Association for Assessment and Accreditation of Lab-oratory Animal Care guidelines and were approved by the VA PugetSound Institutional Animal Care and Use Committee.
Statistical analysesStandard ANOVAs or t tests were used (two-tailed). Where noted,following a statistically significant overall ANOVA, Helmert tests wereused to carry out a priori, planned comparisons (88, 89). Rank-orderSpearman correlations (two-tailed P values) were performed using
eTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 12

R E S EARCH ART I C L E
log10-transformed number of blast exposures to linearize blast num-ber. Subsequent multivariate linear regression analyses reported corre-lations (two-tailed) adjusted for CAPS, PHQ-9, and AUDIT-C scores.Using established methods (90), NEUROSTAT performed an r-to-ztransform, with statistical significance of resultant z-score values eval-uated using randomGaussian fields and a Euler characteristic algorithm(91) to control for multiple comparisons and maintain a type I errorrate of P < 0.05 (corresponding to z > 4.0). All reported P values de-note two-tailed critical values defined as P≤ 0.05. Statistical likelihoodof correctly identifying the conditions for treatment pairs (sham ver-sus blast) was performed using a test for one proportion. Statisticalanalyses were done using SPSS software (IBM) and R version 3.2.2(R Core Team).
Dow
nloaded f
SUPPLEMENTARY MATERIALS
www.sciencetranslationalmedicine.org/cgi/content/full/8/321/321ra6/DC1MethodsTabulated data for Figs. 1B, 2E, 3 (C and D), 4 (A and B), 5 (B and C), 6D, 7 (B, D, H, and I), and 8.References (92–101)
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
rom
REFERENCES AND NOTES
1. I. Cernak, Blast-induced neurotrauma models and their requirements. Front. Neurol. 5,128 (2014).
2. J. E. Karr, C. N. Areshenkoff, E. C. Duggan, M. A. Garcia-Barrera, Blast-related mild traumaticbrain injury: A Bayesian random-effects meta-analysis on the cognitive outcomes of concus-sion among military personnel. Neuropsychol. Rev. 24, 428–444 (2014).
3. C. L. Mac Donald, A. M. Johnson, D. Cooper, E. C. Nelson, N. J. Werner, J. S. Shimony,A. Z. Snyder, M. E. Raichle, J. R. Witherow, R. Fang, S. F. Flaherty, D. L. Brody, Detection ofblast-related traumatic brain injury in U.S. military personnel. N. Engl. J. Med. 364, 2091–2100(2011).
4. E. R. Peskind, E. C. Petrie, D. J. Cross, K. Pagulayan, K. McCraw, D. Hoff, K. Hart, C.-E. Yu,M. A. Raskind, D. G. Cook, S. Minoshima, Cerebrocerebellar hypometabolism associatedwith repetitive blast exposure mild traumatic brain injury in 12 Iraq war Veterans withpersistent post-concussive symptoms. Neuroimage 54 (Suppl. 1), S76–S82 (2011).
5. E. C. Petrie, D. J. Cross, V. L. Yarnykh, T. Richards, N. M. Martin, K. Pagulayan, D. Hoff,K. Hart, C. Mayer, M. Tarabochia, M. A. Raskind, S. Minoshima, E. R. Peskind, Neuroima-ging, behavioral, and psychological sequelae of repetitive combined blast/impact mildtraumatic brain injury in Iraq and Afghanistan war veterans. J. Neurotrauma 31, 425–436(2014).
6. A. C. McKee, M. E. Robinson, Military-related traumatic brain injury and neurodegenera-tion. Alzheimers Dement. 10, S242–S253 (2014).
7. M. A. Mayorga, The pathology of primary blast overpressure injury. Toxicology 121, 17–28(1997).
8. W. C. Moss, M. J. King, E. G. Blackman, Skull flexure from blast waves: A mechanism forbrain injury with implications for helmet design. Phys. Rev. Lett. 103, 108702 (2009).
9. B. R. Huber, J. S. Meabon, T. J. Martin, P. D. Mourad, R. Bennett, B. C. Kraemer, I. Cernak,E. C. Petrie, M. J. Emery, E. R. Swenson, C. Mayer, E. Mehic, E. R. Peskind, D. G. Cook, Blastexposure causes early and persistent aberrant phospho- and cleaved-tau expression ina murine model of mild blast-induced traumatic brain injury. J. Alzheimers Dis. 37, 309–323(2013).
10. I. Cernak, Blast injuries of the lung: Development, prognosis and possible therapy.Vojnosanit. Pregl. 54, 91–102 (1997).
11. I. Cernak, J. Savic, Z. Malicevic, G. Zunic, P. Radosevic, I. Ivanovic, L. Davidovic, Involvement ofthe central nervous system in the general response to pulmonary blast injury. J. Trauma 40(Suppl. 3), S100–S104 (1996).
12. I. Cernak, Z. Wang, J. Jiang, X. Bian, J. Savic, Ultrastructural and functional characteristicsof blast injury-induced neurotrauma. J. Trauma 50, 695–706 (2001).
13. I. Cernak, Z. Wang, J. Jiang, X. Bian, J. Savic, Cognitive deficits following blast injury-inducedneurotrauma: Possible involvement of nitric oxide. Brain Inj. 15, 593–612 (2001).
14. J. M. K. Murthy, J. S. Chopra, D. R. Gulati, Subdural hematoma in an adult following a blastinjury. Case report. J. Neurosurg. 50, 260–261 (1979).
15. I. Cernak, L. J. Noble-Haeusslein, Traumatic brain injury: An overview of pathobiology withemphasis on military populations. J. Cereb. Blood Flow Metab. 30, 255–266 (2010).
www.Scienc
16. R. S. Bell, A. H. Vo, C. J. Neal, J. Tigno, R. Roberts, C. Mossop, J. R. Dunne, R. A. Armonda,Military traumatic brain and spinal column injury: A 5-year study of the impact blast andother military grade weaponry on the central nervous system. J. Trauma 66 (Suppl. 4),S104–S111 (2009).
17. B. D. Owens, J. F. Kragh Jr., J. C. Wenke, J. Macaitis, C. E. Wade, J. B. Holcomb, Combatwounds in Operation Iraqi Freedom and Operation Enduring Freedom. J. Trauma 64,295–299 (2008).
18. F. Ahmed, A. Gyorgy, A. Kamnaksh, G. Ling, L. Tong, S. Parks, D. Agoston, Time-dependentchanges of protein biomarker levels in the cerebrospinal fluid after blast traumatic braininjury. Electrophoresis 33, 3705–3711 (2012).
19. R. A. Bauman, G. Ling, L. Tong, A. Januszkiewicz, D. Agoston, N. Delanerolle, Y. Kim, D. Ritzel,R. Bell, J. Ecklund, R. Armonda, F. Bandak, S. Parks, An introductory characterization of acombat-casualty-care relevant swine model of closed head injury resulting from exposureto explosive blast. J. Neurotrauma 26, 841–860 (2009).
20. L. E. Goldstein, A. M. Fisher, C. A. Tagge, X. L. Zhang, L. Velisek, J. A. Sullivan, C. Upreti,J. M. Kracht, M. Ericsson, M. W. Wojnarowicz, C. J. Goletiani, G. M. Maglakelidze, N. Casey,J. A. Moncaster, O. Minaeva, R. D. Moir, C. J. Nowinski, R. A. Stern, R. C. Cantu, J. Geiling,J. K. Blusztajn, B. L. Wolozin, T. Ikezu, T. D. Stein, A. E. Budson, N. W. Kowall, D. Chargin,A. Sharon, S. Saman, G. F. Hall, W. C. Moss, R. O. Cleveland, R. E. Tanzi, P. K. Stanton,A. C. McKee, Chronic traumatic encephalopathy in blast-exposed military veteransand a blast neurotrauma mouse model. Sci. Transl. Med. 4, 134ra60 (2012).
21. R. De Gasperi, M. A. Gama Sosa, S. H. Kim, J. W. Steele, M. C. Shaughness, E. Maudlin-Jeronimo,A. A. Hall, S. T. Dekosky, R. M. McCarron, M. P. Nambiar, S. Gandy, S. T. Ahlers, G. A. Elder,Acute blast injury reduces brain ab in two rodent species. Front. Neurol. 3, 177 (2012).
22. R. P. J. Stocker, M. A. Cieply, B. Paul, H. Khan, L. Henry, A. P. Kontos, A. Germain, Combat-related blast exposure and traumatic brain injury influence brain glucose metabolismduring REM sleep in military veterans. Neuroimage 99, 207–214 (2014).
23. M. F. Mendez, E. M. Owens, G. Reza Berenji, D. C. Peppers, L.-J. Liang, E. A. Licht, Mildtraumatic brain injury from primary blast vs. blunt forces: Post-concussion consequencesand functional neuroimaging. NeuroRehabilitation 32, 397–407 (2013).
24. J. J. Bazarian, K. Donnelly, D. R. Peterson, G. C. Warner, T. Zhu, J. Zhong, The relationbetween posttraumatic stress disorder and mild traumatic brain injury acquired duringOperations Enduring Freedom and Iraqi Freedom. J. Head Trauma Rehabil. 28, 1–12(2013).
25. R. E. Jorge, L. Acion, T. White, D. Tordesillas-Gutierrez, R. Pierson, B. Crespo-Facorro,V. A. Magnotta, White matter abnormalities in veterans with mild traumatic braininjury. Am. J. Psychiatry 169, 1284–1291 (2012).
26. C. Mac Donald, A. Johnson, D. Cooper, T. Malone, J. Sorrell, J. Shimony, M. Parsons, A. Snyder,M. Raichle, R. Fang, S. Flaherty, M. Russell, D. L. Brody, Cerebellar white matter abnormalitiesfollowing primary blast injury in US military personnel. PLOS One 8, e55823 (2013).
27. A. Kamnaksh, M. D. Budde, E. Kovesdi, J. B. Long, J. A. Frank, D. V. Agoston, Diffusiontensor imaging reveals acute subcortical changes after mild blast-induced traumaticbrain injury. Sci. Rep. 4, 4809 (2014).
28. D. L. Warden, L. M. French, L. Shupenko, J. Fargus, G. Riedy, M. E. Erickson, M. S. Jaffee,D. F. Moore, Case report of a soldier with primary blast brain injury. Neuroimage 47(Suppl. 2), T152–T153 (2009).
29. W. Liu, B. Wang, R. Wolfowitz, P.-H. Yeh, D. E. Nathan, J. Graner, H. Tang, H. Pan, J. Harper,D. Pham, T. R. Oakes, L. M. French, G. Riedy, Perfusion deficits in patients with mild trau-matic brain injury characterized by dynamic susceptibility contrast MRI. NMR Biomed. 26,651–663 (2013).
30. B. L. Fischer, M. Parsons, S. Durgerian, C. Reece, L. Mourany, M. J. Lowe, E. B. Beall, K. A. Koenig,S. E. Jones, M. R. Newsome, R. S. Scheibel, E. A. Wilde, M. Troyanskaya, T. L. Merkley, M. Walker,H. S. Levin, S. M. Rao, Neural activation during response inhibition differentiates blast frommechanical causes of mild to moderate traumatic brain injury. J. Neurotrauma 31, 169–179(2014).
31. P.-H. Yeh, B. Wang, T. R. Oakes, L. M. French, H. Pan, J. Graner, W. Liu, G. Riedy, Postcon-cussional disorder and PTSD symptoms of military-related traumatic brain injury asso-ciated with compromised neurocircuitry. Hum. Brain Mapp. 35, 2652–2673 (2014).
32. F. Van Overwalle, K. Baetens, P. Marien, M. Vandekerckhove, Social cognition and thecerebellum: A meta-analysis of over 350 fMRI studies. Neuroimage 86, 554–572 (2014).
33. R. L. Buckner, The cerebellum and cognitive function: 25 years of insight from anatomyand neuroimaging. Neuron 80, 807–815 (2013).
34. C. J. Stoodley, The cerebellum and cognition: Evidence from functional imaging studies.Cerebellum 11, 352–365 (2012).
35. C. J. Stoodley, E. M. Valera, J. D. Schmahmann, Functional topography of the cerebellumfor motor and cognitive tasks: An fMRI study. Neuroimage 59, 1560–1570 (2012).
36. M. F. Mendez, E. M. Owens, E. E. Jimenez, D. Peppers, E. A. Licht, Changes in personalityafter mild traumatic brain injury from primary blast vs. blunt forces. Brain Inj. 27, 10–18(2013).
37. E. C. Petrie, D. J. Cross, V. L. Yarnykh, T. Richards, N. M. Martin, K. Pagulayan, D. Hoff, K. Hart,C. Mayer, M. Tarabochia, M. Raskind, S. Minoshima, E. Peskind, Neuroimaging, behavioral,
eTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 13

R E S EARCH ART I C L E
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from
and psychological sequelae of repetitive combined blast/impact mild traumatic brain injury inIraq and Afghanistan war veterans. J. Neurotrauma 31, 425–436 (2014).
38. I. Cernak, A. C. Merkle, V. E. Koliatsos, J. M. Bilik, Q. T. Luong, T. M. Mahota, L. Xu, N. Slack,D. Windle, F. A. Ahmed, The pathobiology of blast injuries and blast-induced neurotrau-ma as identified using a new experimental model of injury in mice. Neurobiol. Dis. 41,538–551 (2011).
39. V. E. Koliatsos, I. Cernak, L. Xu, Y. Song, A. Savonenko, B. J. Crain, C. G. Eberhart, C. E. Frangakis,T. Melnikova, H. Kim, D. Lee, A mouse model of blast injury to brain: Initial pathological,neuropathological, and behavioral characterization. J. Neuropathol. Exp. Neurol. 70,399–416 (2011).
40. O. Farkas, J. Lifshitz, J. T. Povlishock, Mechanoporation induced by diffuse traumaticbrain injury: An irreversible or reversible response to injury? J. Neurosci. 26, 3130–3140(2006).
41. E. Kim, M. Sheng, PDZ domain proteins of synapses. Nat. Rev. Neurosci. 5, 771–781(2004).
42. K. J. McKenzie, D. R. McLellan, S. M. Gentleman, W. L. Maxwell, T. A. Gennarelli, D. I. Graham, Isb-APP a marker of axonal damage in short-surviving head injury? Acta Neuropathol. 92,608–613 (1996).
43. S. H. Friess, R. N. Ichord, J. Ralston, K. Ryall, M. A. Helfaer, C. Smith, S. S. Margulies, Repeatedtraumatic brain injury affects composite cognitive function in piglets. J. Neurotrauma 26,1111–1121 (2009).
44. K. Oishi, A. Faria, P. C. M. van Zijl, S. Mori, MRI Atlas of Human White Matter (AcademicPress, Amsterdam, 2nd ed., 2011).
45. N. S. Ryan, S. Keihaninejad, T. J. Shakespeare, M. Lehmann, S. J. Crutch, I. B. Malone,J. S. Thornton, L. Mancini, H. Hyare, T. Yousry, G. R. Ridgway, H. Zhang, M. Modat, D. C. Alexander,M. N. Rossor, S. Ourselin, N. C. Fox, Magnetic resonance imaging evidence for presympto-matic change in thalamus and caudate in familial Alzheimer’s disease. Brain 136, 1399–1414(2013).
46. R. A. Morey, C. C. Haswell, E. S. Selgrade, D. Massoglia, C. Liu, J. Weiner, C. E. Marx; MIRECCWork Group, I. Cernak, G. McCarthy, Effects of chronic mild traumatic brain injury onwhite matter integrity in Iraq and Afghanistan war veterans. Hum. Brain Mapp. 34,2986–2999 (2013).
47. K. H. Taber, R. A. Hurley, C. C. Haswell, J. A. Rowland, S. D. Hurt, C. D. Lamar, R. A. Morey,White matter compromise in veterans exposed to primary blast forces. J. Head TraumaRehabil. 30, E15–E25 (2015).
48. D. M. Erlanger, K. C. Kutner, J. T. Barth, R. Barnes, Neuropsychology of sports-related headinjury: Dementia pugilistica to post concussion syndrome. Clin. Neuropsychol. 13, 193–209(1999).
49. A. C. McKee, R. C. Cantu, C. J. Nowinski, E. T. Hedley-Whyte, B. E. Gavett, A. E. Budson,V. E. Santini, H.-S. Lee, C. A. Kubilus, R. A. Stern, Chronic traumatic encephalopathy inathletes: Progressive tauopathy after repetitive head injury. J. Neuropathol. Exp. Neurol. 68,709–735 (2009).
50. B. I. Omalu, S. T. DeKosky, R. L. Minster, M. I. Kamboh, R. L. Hamilton, C. H. Wecht, Chronictraumatic encephalopathy in a National Football League player. Neurosurgery 57, 128–134;discussion 128-34 (2005).
51. A. C. McKee, T. D. Stein, C. J. Nowinski, R. A. Stern, D. H. Daneshvar, V. E. Alvarez, H.-S. Lee,G. Hall, S. M. Wojtowicz, C. M. Baugh, D. O. Riley, C. A. Kubilus, K. A. Cormier, M. A. Jacobs,B. R. Martin, C. R. Abraham, T. Ikezu, R. R. Reichard, B. L. Wolozin, A. E. Budson, L. E. Goldstein,N. W. Kowall, R. C. Cantu, The spectrum of disease in chronic traumatic encephalopathy. Brain136, 43–64 (2013).
52. Z. Yang, F. Lin, C. S. Robertson, K. K. W. Wang, Dual vulnerability of TDP-43 to calpain andcaspase-3 proteolysis after neurotoxic conditions and traumatic brain injury. J. Cereb.Blood Flow Metab. 34, 1444–1452 (2014).
53. C. M. Baugh, C. A. Robbins, R. A. Stern, A. C. McKee, Current understanding of chronictraumatic encephalopathy. Curr. Treat. Options. Neurol. 16, 306 (2014).
54. J. A. N. Corsellis, C. J. Bruton, D. Freeman-Browne, The aftermath of boxing. Psychol. Med.3, 270–303 (1973).
55. J. Lu, K. C. Ng, G. Ling, J. Wu, D. J. F. Poon, E. M. Kan, M. H. Tan, Y. J. Wu, P. Li, S. Moochhala,E. Yap, L. K. H. Lee, M. Teo, I. B. Yeh, D. M. B. Sergio, F. Chua, S. D. Kumar, E.-A. Ling, Effectof blast exposure on the brain structure and cognition in Macaca fascicularis. J. Neuro-trauma 29, 1434–1454 (2012).
56. P. A. Taylor, C. C. Ford, Simulation of blast-induced early-time intracranial wave physicsleading to traumatic brain injury. J. Biomech. Eng. 131, 061007 (2009).
57. U. Krave, M. Al-Olama, H.-A. Hansson, Rotational acceleration closed head flexion traumagenerates more extensive diffuse brain injury than extension trauma. J. Neurotrauma 28,57–70 (2011).
58. L. E. Goldstein, A. M. Fisher, C. A. Tagge, X. L. Zhang, L. Velisek, J. A. Sullivan, C. Upreti,J. M. Kracht, M. Ericsson, M. W. Wojnarowicz, C. J. Goletiani, G. M. Maglakelidze, N. Casey,J. A. Moncaster, O. Minaeva, R. D. Moir, C. J. Nowinski, R. A. Stern, R. C. Cantu, J. Geiling,J. K. Blusztajn, B. L. Wolozin, T. Ikezu, T. D. Stein, A. E. Budson, N. W. Kowall, D. Chargin,A. Sharon, S. Saman, G. F. Hall, W. C. Moss, R. O. Cleveland, R. E. Tanzi, P. K. Stanton,
www.Scienc
A. C. McKee, Chronic traumatic encephalopathy in blast-exposed military veteransand a blast neurotrauma mouse model. Sci. Transl. Med. 4, 134ra160 (2012).
59. D. C. Viano, I. R. Casson, E. J. Pellman, L. Zhang, A. I. King, K. H. Yang, Concussion inprofessional football: Brain responses by finite element analysis: Part 9. Neurosurgery57, 891–916 (2005).
60. P. W. Lampert, J. M. Hardman, Morphological changes in brains of boxers. JAMA 251,2676–2679 (1984).
61. A. Säljö, F. Bao, K. G. Haglid, H.-A. Hansson, Blast exposure causes redistribution of phos-phorylated neurofilament subunits in neurons of the adult rat brain. J. Neurotrauma 17,719–726 (2000).
62. I. Cernak, V. Savic, J. Kotur, V. Prokic, B. Kuljic, D. Grbovic, M. Veljovic, Alterations in mag-nesium and oxidative status during chronic emotional stress. Magnes. Res. 13, 29–36(2000).
63. J. B. Long, T. L. Bentley, K. A. Wessner, C. Cerone, S. Sweeney, R. A. Bauman, Blastoverpressure in rats: Recreating a battlefield injury in the laboratory. J. Neurotrauma26, 827–840 (2009).
64. H. Bayir, V. E. Kagan, R. S. B Clark, K. Janesko-Feldman, R. Rafikov, Z. Huang, X. Zhang, V. Vagni,T. R. Billiar, P. M. Kochanek, Neuronal NOS-mediated nitration and inactivation of manganesesuperoxide dismutase in brain after experimental and human brain injury. J. Neurochem. 101,168–181 (2007).
65. S. T. Ahlers, E. Vasserman-Stokes, M. C. Shaughness, A. A. Hall, D. A. Shear, M. Chavko,R. M. McCarron, J. R. Stone, Assessment of the effects of acute and repeated exposureto blast overpressure in rodents: Toward a greater understanding of blast and the potentialramifications for injury in humans exposed to blast. Front. Neurol. 3, 32 (2012).
66. Y. Wang, Y. Wei, S. Oguntayo, W. Wilkins, P. Arun, M. Valiyaveettil, J. Song, J. B. Long,M. P. Nambiar, Tightly coupled repetitive blast-induced traumatic brain injury: Developmentand characterization in mice. J. Neurotrauma 28, 2171–2183 (2011).
67. E. Rostami, J. Davidsson, K. C. Ng, J. Lu, A. Gyorgy, J. Walker, D. Wingo, S. Plantman,B.-M. Bellander, D. V. Agoston, M. Risling, A model for mild traumatic brain injury that induceslimited transient memory impairment and increased levels of axon related serum bio-markers. Front. Neurol. 3, 115 (2012).
68. W. T. Thach, Cerebellar output: Properties, synthesis and uses. Brain Res. 40, 89–102(1972).
69. J. R. Sarna, R. Hawkes, Patterned Purkinje cell death in the cerebellum. Prog. Neurobiol.70, 473–507 (2003).
70. H. Nonaka, M. Akima, T. Hatori, T. Nagayama, Z. Zhang, F. Ihara, The microvasculature ofthe human cerebellar meninges. Acta Neuropathol. 104, 608–614 (2002).
71. R. A. Armonda, R. S. Bell, A. H. Vo, G. Ling, T. J. DeGraba, B. Crandall, J. Ecklund, W. W. Campbell,Wartime traumatic cerebral vasospasm: Recent review of combat casualties. Neurosurgery 59,1215–1225; discussion 1225 (2006).
72. J. R. Tonra, Cerebellar susceptibility to experimental autoimmune encephalomyelitis inSJL/J mice: Potential interaction of immunology with vascular anatomy. Cerebellum 1, 57–68(2002).
73. S. Jayadev, T. D. Bird, Hereditary ataxias: Overview. Genet. Med. 15, 673–683 (2013).74. R. H. Garman, L. W. Jenkins, R. C. Switzer III, R. A. Bauman, L. C. Tong, P. V. Swauger, S. A. Parks,
D. V. Ritzel, C. E. Dixon, R. S. B. Clark, H. Bayir, V. Kagan, E. K. Jackson, P. M. Kochanek, Blastexposure in rats with body shielding is characterized primarily by diffuse axonal injury.J. Neurotrauma 28, 947–959 (2011).
75. C. Pierpaoli, A. Barnett, S. Pajevic, R. Chen, L. R. Penix, A. Virta, P. Basser, Water diffusionchanges in Wallerian degeneration and their dependence on white matter architecture.Neuroimage 13, 1174–1185 (2001).
76. F. Agosta, E. Pagani, M. Petrolini, D. Caputo, M. Perini, A. Prelle, F. Salvi, M. Filippi, Assess-ment of white matter tract damage in patients with amyotrophic lateral sclerosis: A dif-fusion tensor MR imaging tractography study. AJNR Am. J. Neuroradiol. 31, 1457–1461(2010).
77. S.-K. Song, S.-W. Sun, M. J. Ramsbottom, C. Chang, J. Russell, A. H. Cross, Dysmyelinationrevealed through MRI as increased radial (but unchanged axial) diffusion of water. Neuroimage17, 1429–1436 (2002).
78. Y. Wang, Q. Wang, J. P. Haldar, F.-C. Yeh, M. Xie, P. Sun, T.-W. Tu, K. Trinkaus, R. S. Klein,A. H. Cross, S.-K. Song, Quantification of increased cellularity during inflammatorydemyelination. Brain 134, 3590–3601 (2011).
79. M. Anderova, I. Vorisek, H. Pivonkova, J. Benesova, L. Vargova, M. Cicanic, A. Chvatal,E. Sykova, Cell death/proliferation and alterations in glial morphology contribute to changesin diffusivity in the rat hippocampus after hypoxia–ischemia. J. Cereb. Blood Flow Metab. 31,894–907 (2011).
80. E. Caverzasi, M. L. Mandelli, S. J. DeArmond, C. P. Hess, P. Vitali, N. Papinutto, A. Oehler,B. L. Miller, I. V. Lobach, S. Bastianello, M. D. Geschwind, R. G. Henry, White matter involve-ment in sporadic Creutzfeldt-Jakob disease. Brain 137, 3339–3354 (2014).
81. E. Caverzasi, R. G. Henry, P. Vitali, I. V. Lobach, J. Kornak, S. Bastianello, S. J. DeArmond,B. L. Miller, H. J. Rosen, M. L. Mandelli, M. D. Geschwind, Application of quantitativeDTI metrics in sporadic CJD. Neuroimage Clin. 4, 426–435 (2014).
eTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 14

R E S EARCH ART I C L E
by gueshttp://stm
.sciencemag.org/
Dow
nloaded from
82. J. M. Coughlin, Y. Wang, C. A. Munro, S. Ma, C. Yue, S. Chen, R. Airan, P. K. Kim, A. V. Adams,C. Garcia, C. Higgs, H. I. Sair, A. Sawa, G. Smith, C. G. Lyketsos, B. Caffo, M. Kassiou,T. R. Guilarte, M. G. Pomper, Neuroinflammation and brain atrophy in former NFL players:An in vivo multimodal imaging pilot study. Neurobiol. Dis. 74, 58–65 (2015).
83. C. J. Stoodley, J. D. Schmahmann, Evidence for topographic organization in the cerebel-lum of motor control versus cognitive and affective processing. Cortex 46, 831–844(2010).
84. J. A. Bernard, S. J. Peltier, B. L. Benson, J. L. Wiggins, S. M. Jaeggi, M. Buschkuehl, J. Jonides,C. S. Monk, R. D. Seidler, Dissociable functional networks of the human dentate nucleus.Cereb. Cortex 24, 2151–2159 (2014).
85. D. D. Blake, F. W. Weathers, L. M. Nagy, D. G. Kaloupek, F. D. Gusman, D. S. Charney,T. M. Keane, The development of a Clinician-Administered PTSD Scale. J. Trauma. Stress 8,75–90 (1995).
86. K. Kroenke, R. L. Spitzer, J. B. Williams, The PHQ-9: Validity of a brief depression severitymeasure. J. Gen. Intern. Med. 16, 606–613 (2001).
87. K. Bush, D. R. Kivlahan, M. B. McDonell, S. D. Fihn, K. A. Bradley, The AUDIT alcohol con-sumption questions (AUDIT-C): An effective brief screening test for problem drinking.Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identifi-cation Test. Arch. Intern. Med. 158, 1789–1795 (1998).
88. B. J. Winer, D. R. Brown, K. M. Michels, Statistical Principles in Experimental Design(McGraw-Hill Inc., New York, ed. 3, 1991), p. 1057.
89. A. Field, Discovering Statistics Using SPSS (Sage Publications, London, ed. 2, 2005), p. 777.90. E. C. Petrie, D. J. Cross, D. Galasko, G. D. Schellenberg, M. A. Raskind, E. R. Peskind,
S. Minoshima, Preclinical evidence of Alzheimer changes: Convergent cerebrospinal fluid bio-marker and fluorodeoxyglucose positron emission tomography findings. Arch. Neurol. 66,632–637 (2009).
91. K. J. Worsley, A. C. Evans, S. Marrett, P. Neelin, A three-dimensional statistical analysisfor CBF activation studies in human brain. J. Cereb. Blood Flow Metab. 12, 900–918(1992).
92. J. Talairach, P. Tournoux, Co-Planar Stereotaxic Atlas of the Human Brain. 3-Dimensional Pro-portional System: An Approach to Cerebral Imaging (Thieme Medical Publishers, New York,1988).
93. S. Minoshima, R. A. Koeppe, K. A. Frey, M. Ishihara, D. E. Kuhl, Stereotactic PET atlas of thehuman brain: Aid for visual interpretation of functional brain images. J. Nucl. Med. 35,949–954 (1994).
94. S. Minoshima, R. A. Koeppe, K. A. Frey, D. E. Kuhl, Anatomic standardization: Linear scalingand nonlinear warping of functional brain images. J. Nucl. Med. 35, 1528–1537 (1994).
95. S. Minoshima, K. A. Frey, R. A. Koeppe, N. L. Foster, D. E. Kuhl, A diagnostic approach inAlzheimer’s disease using three-dimensional stereotactic surface projections of fluorine-18-FDG PET. J. Nucl. Med. 36, 1238–1248 (1995).
www.Scienc
96. S. Minoshima, K. A. Frey, N. L. Foster, D. E. Kuhl, Preserved pontine glucose metabolism inAlzheimer disease: A reference region for functional brain image (PET) analysis. J. Comput.Assist. Tomogr. 19, 541–547 (1995).
97. I. Oguz, M. Farzinfar, J. Matsui, F. Budin, Z. Liu, G. Gerig, H. J. Johnson, M. Styner, DTIPrep:Quality control of diffusion-weighted images. Front. Neuroinform. 8, 4 (2014).
98. I. Cernak, J. Savic, D. Ignjatovic, M. Jevtic, Blast injury from explosive munitions. J. Trauma47, 96–103; discussion 103–104 (1999).
99. J. S. Meabon, A. Lee, K. D. Meeker, L. M. Bekris, R. K. Fujimura, C.-E. Yu, G. S. Watson, D. V. Pow,I. R. Sweet, D. G. Cook, Differential expression of the glutamate transporter GLT-1 in pancreas.J. Histochem. Cytochem. 60, 139–151 (2012).
100. N. W. Dunham, T. S. Miya, A note on a simple apparatus for detecting neurological deficitin rats and mice. J. Am. Pharm. Assoc. Am. Pharm. Assoc. 46, 208–209 (1957).
101. B. J. Jones, D. J. Roberts, The quantitative measurement of motor inco-ordination in naivemice using an accelerating rotarod. J. Pharm. Pharmacol. 20, 302–304 (1968).
Funding: This work was supported by the Department of Veterans Affairs Office of Researchand Development Medical Research Service (D.G.C. and B.C.K.); VA Rehabilitation Research &Development Service (E.R.P.); University of Washington Friends of Alzheimer’s Research (D.G.C.and E.R.P.); University of Washington Royalty Research Fund (D.G.C.); Northwest Network MentalIllness Research, Education and Clinical Center (J.S.M., B.R.H., K.F.P., E.C.P., M.A.R., and E.R.P.);Office of Academic Affiliations Advanced Fellowship Program Mental Illness Research andTreatment, Department of Veterans Affairs (B.R.H.); NIH T32 AG000258 (J.S.M.); and VA ClinicalScience R&D Career Development Award Program #CX00516 (K.F.P.). Author contributions: J.S.M.and B.R.H. conducted blast procedures, biochemistry experiments, and microscopy. K.D.M.conducted biochemistry experiments. J.S.M., B.R.H., D.J.C., T.L.R., S.M., G.L., E.C.P., M.A.R., E.R.P.,and D.G.C. contributed to study design. J.S.M., D.J.C., E.R.P., G.L., E.R.P., M.A.R., and D.G.C. performeddata analysis and data interpretation. J.S.M., D.J.C., T.L.R., K.F.P., G.L., B.C.K., E.C.P., M.A.R., E.R.P.,and D.G.C. drafted the manuscript and/or edited it critically for important intellectual content.Competing interests: J.S.M. is chief operations officer of Neurogenix Pharmaceuticals. Theother authors declare no competing interests.
Submitted 2 March 2015Accepted 17 December 2015Published 13 January 201610.1126/scitranslmed.aaa9585
Citation: J. S. Meabon, B. R. Huber, D. J. Cross, T. L. Richards, S. Minoshima, K. F. Pagulayan,G. Li, K. D. Meeker, B. C. Kraemer, E. C. Petrie, M. A. Raskind, E. R. Peskind, D. G. Cook, Repetitiveblast exposure in mice and combat veterans causes persistent cerebellar dysfunction. Sci.Transl. Med. 8, 321ra6 (2016).
t o
eTranslationalMedicine.org 13 January 2016 Vol 8 Issue 321 321ra6 15
n Novem
ber 20, 2020

dysfunctionRepetitive blast exposure in mice and combat veterans causes persistent cerebellar
Ge Li, Kole D. Meeker, Brian C. Kraemer, Eric C. Petrie, Murray A. Raskind, Elaine R. Peskind and David G. CookJames S. Meabon, Bertrand R. Huber, Donna J. Cross, Todd L. Richards, Satoshi Minoshima, Kathleen F. Pagulayan,
DOI: 10.1126/scitranslmed.aaa9585, 321ra6321ra6.8Sci Transl Med
veterans.correspond to abnormal brain imaging findings obtained in similar cerebellar regions in blast-exposed combatintegrating sensory information and movement, is injured by blast exposure in mice in specific areas that
report that the cerebellum, a brain structure important foret al.correspond to humans with mild TBI. Meabon causes persistent brain injuries. There is also limited insight into how blast-induced brain injuries in animal modelsAfghanistan. Most of these TBIs are blast-related. Currently, there is limited understanding of how mild blast
Mild traumatic brain injury (TBI) is often referred to as the ''signature injury'' of the wars in Iraq andThe cerebellum is vulnerable to blast injury in mice and combat veterans
ARTICLE TOOLS http://stm.sciencemag.org/content/8/321/321ra6
MATERIALSSUPPLEMENTARY http://stm.sciencemag.org/content/suppl/2016/01/11/8.321.321ra6.DC1
CONTENTRELATED
http://stm.sciencemag.org/content/scitransmed/12/526/eaay1769.fullhttp://stm.sciencemag.org/content/scitransmed/11/508/eaaw1993.fullhttp://science.sciencemag.org/content/sci/352/6288/881.full
REFERENCES
http://stm.sciencemag.org/content/8/321/321ra6#BIBLThis article cites 97 articles, 6 of which you can access for free
PERMISSIONS http://www.sciencemag.org/help/reprints-and-permissions
Terms of ServiceUse of this article is subject to the
registered trademark of AAAS. is aScience Translational MedicineScience, 1200 New York Avenue NW, Washington, DC 20005. The title
(ISSN 1946-6242) is published by the American Association for the Advancement ofScience Translational Medicine
Copyright © 2016, American Association for the Advancement of Science
by guest on Novem
ber 20, 2020http://stm
.sciencemag.org/
Dow
nloaded from