Regulatory Natural Killer T Cells Protect against Spontaneous and Recurrent Type 1 Diabetes
-
Upload
shayan-sharif -
Category
Documents
-
view
212 -
download
0
Transcript of Regulatory Natural Killer T Cells Protect against Spontaneous and Recurrent Type 1 Diabetes
PDFlib PLOP: PDF Linearization, Optimization, Protection
Page inserted by evaluation versionwww.pdflib.com – [email protected]
77
Ann. N.Y. Acad. Sci. 958: 77–88 (2002). © 2002 New York Academy of Sciences.
Regulatory Natural Killer T Cells Protect against Spontaneous and Recurrent Type 1 Diabetes
SHAYAN SHARIF,a GUILLERMO A. ARREAZA,a PETER ZUCKER,a
AND TERRY L. DELOVITCHa,b
aAutoimmunity/Diabetes Group, The John P. Robarts Research Institute,London, Ontario N6G 2V4, CanadabDepartment of Microbiology and Immunology and Department of Medicine, University of Western Ontario, London, Ontario N6A 5C1, Canada
ABSTRACT: Autoimmune diseases, especially type 1 diabetes (T1D), may becaused by dysregulation of the immune system, which leads to hyporesponsive-ness of regulatory T helper 2 (Th2) cells and promotion of autoimmune Th1cells. Natural killer T (NKT) cells, which comprise a minor subpopulation of Tcells, play a critical role in immunoregulation as a result of a rapid burst of IL-4 and IFN-� secretion. These cells are functionally and numerically deficient inindividuals at risk of T1D, as well as in nonobese diabetic (NOD) mice. It is con-ceivable that protection from T1D may be achieved by correction of this defi-ciency. Alpha-galactosylceramide (�-GalCer) specifically binds to NKT cells ina CD1-dependent manner and stimulates these cells to proliferate and to pro-duce various cytokines, including IFN-�, IL-4, and IL-10. In this review, wepresent evidence that a multiple-dose �-GalCer treatment regimen, which isknown to promote a dominant Th2 environment, can prevent the onset of spon-taneous and cyclophosphamide (CY)-accelerated T1D. This protection is asso-ciated with elevated IL-4 and IL-10 in the spleen and pancreas of protectedfemale NOD mice. Concomitantly, IFN-� levels are reduced in both tissues.More importantly, the protective effect of �-GalCer in CY-accelerated T1D isabrogated by the in vivo blockade of IL-10 activity. We also show that �-GalCertreatment significantly prolongs syngeneic islet graft survival in recipientdiabetic NOD mice. These findings raise the possibility that �-GalCer treat-ment may be used therapeutically to prevent the onset and recurrence of hu-man T1D.
KEYWORDS: NOD; type I diabetes; NKT; alpha-galactosylceramide; islettransplantation
Address for correspondence: Dr. Terry L. Delovitch, Director, Autoimmunity/Diabetes Group,The John P. Robarts Research Institute, 1400 Western Road, London, Ontario, Canada N6G 2V4.Voice: 519-663-3972; fax: 519-663-3847.
78 ANNALS NEW YORK ACADEMY OF SCIENCES
INTRODUCTION
A failure in immune regulation in nonobese diabetic (NOD) mice or human sub-jects at risk of type 1 diabetes (T1D), which stems from deficient T cell–mediatedregulation and T helper 2 cell (Th2) anergy, may be causal to the onset of autoim-mune T1D.1 While diabetogenic effector T cells are CD4+ cells with a Th1 cytokinesecretion profile, regulatory T cells that modulate the function of these effector Tcells, appear to express a Th2 phenotype.1 We previously demonstrated that thymicand peripheral T cells in young NOD mice display a proliferative hyporesponsive-ness (anergy) upon TCR ligation, which is associated with a large reduction in se-cretion of IL-2 and IL-4. Importantly, this stage of anergy in NOD T cells may bereversed in vitro by stimulation with exogenous IL-4,2 and the early administrationof IL-4 in vivo prevents T1D in NOD mice.2,3 Furthermore, immunotherapeutic ap-proaches, including anti-CD28 stimulation,4 that promote and enhance the functionof intraislet Th2 cells and secretion of IL-4 by these cells can effectively prevent theonset of T1D.
Thus, it is conceivable that immune dysregulation in NOD mice may be causedby defects in the expansion and/or function of populations of regulatory T cells, in-cluding Th2 cells that suppress the effector function of diabetogenic Th1 cells. Theexact nature of regulatory T cells in autoimmune disease in general, and in T1D inparticular, has remained elusive. Nonetheless, several types of regulatory cells haveemerged as candidates that mediate protection against T1D, including natural killerT (NKT), CD4+CD25+ T, CD8+TCRγδ+ T, Tc2 and CD4+CD62L+ T cells. This re-view will focus on the potential role of NKT cells in the regulation of autoimmunityand prevention of T1D.
NKT CELLS: PHENOTYPE, DEVELOPMENT, AND SPECIFICITY
NKT cells comprise a unique subset of T cells that coexpress an invariant T cellreceptor (TCR) and NK cell–related surface markers, including NK1.1.5 The major-ity of these cells are restricted to the MHC-I–related molecule CD1, preferentiallyuse an invariant TCRα chain consisting of the Vα14-Jα281 gene segments, and alsohave a bias in TCRβ gene usage.5,6 Cells that preferentially use the invariant Vα24-JαQ TCR gene segments with similar phenotypic characteristics have been de-scribed in humans.7 NKT cells are most frequent in the liver and bone marrow, butare also detected in the thymus and spleen and to a lesser extent in lymph nodes.5 Itappears that subsets of NKT cells exist that are CD1 independent and fail to expressthe invariant TCR. While the thymus and liver are enriched for CD1-dependent NKTcells, spleen and bone marrow are the main sites for CD1-independent NKT cells.8
Based on the expression of CD4 and CD8 markers, three subsets of NKT cellsmay be identified the distribution of which is tissue dependent.9 Although, the ma-jority of NKT cells in liver and lymphoid organs are CD4+ or CD4−CD8−, a smallpopulation of CD8+ NKT cells is present in the spleen.9 The latter population differsfrom conventional NKT cells in that it fails to rapidly produce IL-4 upon primarystimulation and is not CD1- or Jα281 dependent.9 The identification of NKT cells,especially in mouse strains that do not express the NK1.1 allele, was recently facil-
79SHARIF et al.: MODULATION OF AUTOIMMUNE DIABETES BY NKT CELLS
itated by the introduction of CD1 tetramers loaded with the NKT cell ligand α-Gal-Cer.10,11 This reagent identifies a subset of NKT cells that are CD1 dependent andexpress the invariant TCR. Interestingly, a new subset was discovered that was CD1tetramer–positive but NK1.1− and was found only in lymph nodes and the intestine,which was previously thought to lack NKT cells.11 In contrast, CD1 tetramer–nega-tive NKT cells were detected in the spleen and bone marrow that were NK1.1+.11
These results signify the complexity of this cell population and call into question thevalidity of the markers (coexpression of TCRαβ and NK1.1) commonly used toidentify NKT cells.
The development of NKT and T cells appears to be differentially regulated.12 Forexample, interactions with membrane lymphotoxin expressing cells and Fyn signal-ing are required for the development of NKT cells but not for the development ofconventional T cells.12 NKT cell development may be thymus dependent or indepen-dent, and liver serves as a candidate site for the extrathymic development of thesecells.13 The fetal development of Vα14+ NKT cells starts at day 9 of gestation inmice, before the fetal thymus is formed, and their development can occur indepen-dently of the yolk sac.14 A model of NKT development was recently proposed.15
This model predicts that NKT and T cells share the same progenitors and that thestochastic rearrangement of the Vα14 segment with Jα281 followed by interactionwith CD1-expressing cells determines the fate of undifferentiated thymocytes to be-come NKT cells. Another aspect of this model is its prediction that cells should passthrough a CD4+CD8+ stage prior to lineage commitment. Cells that encounter CD1prior to lineage commitment become CD4−CD8− NKT cells, whereas those that en-counter CD1 after lineage commitment become CD4+ NKT cells.15
The natural ligand of NKT cells appears to be glycosylphosphatidylinositol,16 butthis issue remains controversial.17 However, a glycolipid derived from marinesponges, α-GalCer, has been identified as a specific ligand for both mouse and hu-man NKT cells.18 Presentation of α-GalCer by CD1 invokes a vigorous response byNKT cells marked by their proliferation, expression of activation molecules, in-crease in cytotoxic activity, and secretion of various cytokines.18,19 Secretion ofTh1- or Th2-type cytokines may be differentially regulated by the regime of α-Gal-Cer administration in vivo. While a single dose of α-GalCer stimulates a Th1 re-sponse, a multiple-dose regime promotes a Th2 response.20 Although NKT cells aretriggered primarily by α-GalCer, bystander cells, including NK, CD8+, CD4+, andB cells, may also become nonspecifically activated as a consequence of NKT cell ac-tivity.21 This observation raises the possibility that α-GalCer may act as a bridge be-tween the innate and acquired arms of the immune system.
IMMUNOREGULATION BY NKT CELLS
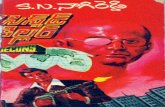
The role of NKT cells in the regulation of several types of immune responses hasreceived much attention. This attention stems mostly from the propensity of NKTcells to secrete various cytokines very early in the course of an immune response.Depending on the type and intensity of the stimulus and the microenvironment ofNKT cells, these T cells may trigger a Th1 or Th2 response (FIG. 1). In fact, earlyinvestigations pointed to the crucial role of NKT cells in triggering Th2-type re-
80 ANNALS NEW YORK ACADEMY OF SCIENCES
sponses.22 Despite these findings, it has been argued that the role of NKT cells in thedevelopment of a Th2 response is dispensable.23 These discrepancies between therelative role of NKT cells in the development of Th1 vs. Th2 cells likely depend onthe particular immunological environment of the NKT cells.
Several in vivo studies have attributed an immunoregulatory function to NKTcells in the amelioration of allogeneic graft-versus-host disease, induction of anteri-or chamber–associated immune deviation (ACAID), and induction of tolerance inrecipients of hepatic and cardiac allografts.24–27 In the ACAID model, which is per-haps one of the best-studied models of antigen-specific immunoregulation, the pres-ence of NKT cells is absolutely necessary for the induction of systemic tolerance.25
Moreover, the induction of tolerance in ACAID is dependent on NKT cell–derivedIL-10,28 and NKT cells are recruited to the site of immunoregulation (spleen) by theCC chemokine macrophage inflammatory protein–2 (MIP-2).29
FIGURE 1. Model of NKT regulation and activation. NKT cells are stimulated byCD1-bearing antigen presenting cells (APCs) that are loaded with α-GalCer. NKT cells andAPCs interact via interactions between costimulatory molecules and their ligands (CD40-CD40L, B7-CD28), and reciprocally regulate each other’s activity by secretion of IL-12 andIFN-γ. Upon stimulation, NKT cells exert effector (e.g., cytotoxicity via Fas-FasL and per-forin-dependent pathways) and immunoregulatory (e.g., secretion of cytokines: IL-4, IL-10,TGF-β and IFN-γ) functions. The early burst of cytokine secretion by NKT cells may be crit-ical in the differentiation of Th0 cells to Th1 or Th2 cells. B cells and NK cells may alsobecome activated by NKT cells.
81SHARIF et al.: MODULATION OF AUTOIMMUNE DIABETES BY NKT CELLS
NKT CELLS IN AUTOIMMUNITY
A potential role for NKT cells in the regulation of autoimmunity was initially rec-ognized in SJL mice that are susceptible to experimental allergic encephalomyelitis(EAE), a Th1-mediated autoimmune disease. SJL mice are deficient in their Th2-mediated responses, and their NKT cells are significantly reduced in number andfunction in various tissues.22 A functional deficit in NKT cells, especially in the pro-duction of IL-4 and other regulatory cytokines, in autoimmune disease–prone mousestrains can lead to a dominant pathogenic autoreactive Th1 response. The impor-tance of NKT cells in the recovery from acute EAE induced by a myelin oligoden-drocyte glycoprotein peptide (MOG 35–55) was recently reported. TCRβ-/-
recipients of a MOG 35–55–specific encephalitogenic T cell line can be rescuedfrom acute EAE by transfer of splenic NKT cells from wild-type donors.30 However,this is in contrast to the finding that transfer of NKT cells into RAG−/− antimyelinbasic protein TCR transgenic C57BL/6 (B6) mice fails to protect them against spon-taneous EAE. This finding raises the possibility that NKT cell protection againstEAE is antigen dependent. Notably, protection conferred by α-GalCer–stimulatedNKT cells in the EAE model induced by MOG 35–55 in B6 mice is costimulationdependent.31 While blockade of B7.2 costimulation results in polarization of NKTcells towards Th2 cytokine production and suppression of EAE, CD40-activated an-tigen presenting cells (APCs) induce polarization of NKT cells towards Th1 cytok-ine production and enhancement of EAE.31 The involvement of NKT cells in theregulation of systemic lupus erythematosus (SLE) in SLE-susceptible strains, suchas MRL lpr/lpr, C3H gld/gld, and (NZB/NZW)F1 mice, has remained controversial.Taniguchi and coworkers32 previously reported that Vα14+ NKT cells are reducedin SLE-prone mice in an age-dependent manner and that this reduction precedes dis-ease development. However, the antibody employed in this study to detect Vα14+
NKT cells was deemed to be nonspecific for NKT cells.12 Nevertheless, the impor-tance of NKT cells in the regulation of autoimmunity has been substantiated by dem-onstration of their involvement in several human autoimmune diseases. Patients withsystemic sclerosis,33 rheumatoid arthritis,34 and multiple sclerosis35 have a reducedfrequency of peripheral blood NKT (Vα24-JαQ+) cells.
NKT CELLS AND AUTOIMMUNE TYPE 1 DIABETES
The strongest evidence in support of a role for NKT cells in the regulation of au-toimmunity is provided by studies of T1D in humans,36 NOD mice,38,39 and BBrats.40 Considerable evidence suggests that NOD mice38,39 and T1D patients36 suf-fer from numerical and functional deficiencies in NKT cells.
NKT Cells in Human T1D
In studies of a group of twin/triplet sets discordant for T1D, the diabetic sibs hada lower frequency of CD4−CD8− NKT cells in their peripheral blood in comparisonto their nondiabetic nonprogressor sibs.36 More importantly, CD4−CD8−Vα24JαQ+
NKT cell clones from these discordant sets differed appreciably in their production
82 ANNALS NEW YORK ACADEMY OF SCIENCES
of IL-4 and IFN-γ. Whereas all clones from diabetic siblings produced only IFN-γ,76 of 79 clones derived from at-risk nonprogressor siblings simultaneously producedIL-4 and IFN-γ.36 A follow-up study of these NKT clones pointed to distinct geneexpression patterns following TCR cross-linking.37
NKT Cells in NOD Mice
In NOD mice between three and five weeks of age, the proportion of NKT-likethymocytes is reduced, and TCR cross-linking–induced IL-4 production is signifi-cantly impaired.38 It is noteworthy that these qualitative and quantitative deficien-cies appear at an age that represents an important checkpoint in the progression toT1D—immediately prior to the development of insulitis.1 The impaired IL-4 pro-duction in NOD may be corrected by IL-7,41 albeit IL-7 fails to protect from T1D.44
This deficiency in NKT cell number and function is restored to normal by 12–15weeks of age in the thymus, but not in the spleen.38 More supportive evidence for aregulatory role of NKT cells in T1D has been obtained by the demonstration thattransfer of NKT-like thymocytes from (BALB/c × NOD)F1 donors into young NODmice prevents T1D in an IL-4– and IL-10–dependent manner.42 Moreover, transgen-ic expression of the Vα14-Jα281 TCR protects NOD mice from spontaneous as wellas cyclophosphamide (CY)-accelerated T1D.43 This protection is associated withthe number of NKT cells and the level of IL-4 secretion by anti-CD3ε–stimulatedNKT cells. Furthermore, these Vα14-Jα281 TCR transgenic NOD mice display el-evated levels of IL-4 and decreased levels of IFN-γ mRNA transcripts in islets, re-spectively.44 There was also a dominant Th2 response (higher IgG1/IgG2c ratio)response to the glutamic acid decarboxylase 65 (GAD65) islet autoantigen. Impor-tantly, in vivo administration of IL-12 abrogated the protective effects of the Vα14-Jα281 TCR transgene.44 In contrast to these findings, TCR- or IL-12–stimulatedNOD NKT cells were reported to be severely deficient in the production of IFN-γbut not IL-4.45 In the latter studies, purified NOD NKT cells stimulated by IL-7 notonly did not prevent T1D, but rather accelerated the onset of T1D. The reason for thisapparent discrepancy may be attributed to the choice of surrogate markers(CD3+CD122+Ly49A+) used to identify NOD NKT cells in this study.12 This furthersupports the significance of using α-GalCer– loaded CD1 tetramers to track NKT cellpopulations in NOD mice and other strains that do not express the NK1.1 marker.
In view of the recent discovery that α-GalCer interacts with Vα14 NKT cells ina CD1-depndent manner, we tested whether NOD NKT cells display deficient IL-4production in response to a CD1-restricted stimulation. We discovered that spleno-cytes of female NOD mice treated with α-GalCer in vivo produce less IL-4 thanthose from T1D-resistant male NOD and female NOR mice upon restimulation invitro with α-GalCer. This deficiency was consistently detected in 6-, 8-, and 12-week-old female NOD mice. Thus, peripheral NKT cells of female NOD mice aredeficient in their IL-4 response to TCR ligation by both a nonspecific (anti-CD3ε)and specific (α-GalCer) CD1-restricted stimulus, and this defect is present through-out critical checkpoints in the pathogenesis of T1D (see TABLE 1 and Ref. 46). De-spite previous reports,45 we did not detect any deficiency in IFN-γ production byperipheral NKT cells of NOD mice in response to α-GalCer (our unpublished obser-vations). These results have been corroborated by other groups of investigators.47,48
83SHARIF et al.: MODULATION OF AUTOIMMUNE DIABETES BY NKT CELLS
INHIBITION OF T1D DEVELOPMENT BY THENKT CELL LIGAND �-GALCER
It is conceivable that correction of quantitative and qualitative deficiencies ofNKT cells in individuals at risk for T1D may prevent occurrence or recurrence ofdisease. Indeed, our results46 as well as those obtained by others47,49 indicate that a
TABLE 1. Immunoregulation of tolerance, transplantation, and autoimmunity byNKT cells
Immunological setting Ref.
Anterior chamber-associated immune deviation (ACAID)
• NKT cells are required for induction of ACAID 25
• IL-10 derived from NKT cells is required for induction of ACAID 28
• MIP-2 recruits NKT cells to the site of immunoregulation (spleen) 29
Graft versus host disease (GVHD)
• NKT cells suppress GVHD in an IL-4–dependent manner 24
Induction of tolerance to grafts
• Induction of cardiac allograft tolerance by LFA-1/ICAM-1 or CD28/B7 blockadeis abrogated in NKT deficient mice
27
• NKT cells are required for acceptance of Rat → mouse islet xenografts 51
Autoimmunity
Experimental allergic encephalomyelitis (EAE) and multiple sclerosis (MS)
• NKT cells in EAE-prone SJL mice are functionally and numerically deficient 22
• Transfer of splenic NKT cells protects against EAE in recipients of a MOG 35–55specific T cell line
30
• α-GalCer–stimulated NKT cells protect against MOG 35–55 induced EAE in aco-stimulation dependent manner
31
• NKT cells are reduced in frequency in MS patients 35
Rheumatoid arthritis (RA) and systemic sclerosis (SS)
• NKT cells are reduced in frequency in RA and SS patients
Type 1 diabetes (T1D) 33,34
• NKT cells are less frequent and display deficient IL-4 production in human T1D
• patients as well as in NOD mice 36,38,39
• Activation of NKT cells by their specific ligand (α-GalCer) protects NOD miceagainst the onset of spontaneous and cyclophosphamide-induced T1D
46,47
• Protection against T1D conferred by α-GalCer is associated with a dominant Th2response in the spleen and pancreas
46,49
• α-GalCer induced protection against T1D is IL-10 dependent 46
• Regulation of development of T1D by NKT cells occurs upstream of the pancreasin the spleen and/or pancreatic lymph nodes
46
• Syngeneic islets grafted into overtly diabetic recipients are protected from a recur-rent autoimmune response and onset of T1D by α-GalCer treatment
46
84 ANNALS NEW YORK ACADEMY OF SCIENCES
multidose α-GalCer treatment administered prior to or after the establishment of in-sulitis (4 and 10 weeks of age, respectively) significantly protects against spontane-ous T1D. Importantly, we discovered that a multidose regime of α-GalCer on days0, 2, 4, 6, and 8 post–CY challenge results in protection of female NOD mice againstthe onset of CY-accelerated T1D (TABLE 1 and Ref. 46). This protection is associatedwith a polarized Th2 environment that is marked by elevated IL-4 and IL-10 and re-duced IFN-γ levels in the spleen and pancreas (TABLE 1 and Ref. 46). To gain moreinsight into the mechanism of α-GalCer–mediated protection in the CY-acceleratedmodel, the effect of α-GalCer treatment was examined after the activity of IL-10 wasneutralized by an anti-IL-10 receptor (anti-IL-10R) mAb (1B1.3a) in vivo. Treat-ment of NOD mice with the latter mAb abrogated the protective effect of α-GalCer(TABLE 1 and Ref. 46), consistent with the recent reports of an immunoregulatoryrole for IL-10 derived from NKT cells.28,42
We tested the hypothesis that α-GalCer regulates progression of T1D indirectlyby modulating the activity of CD4+CD25+ regulatory T cells. It is noteworthy that adecreased frequency of the latter T cell subset may be associated with susceptibilityto T1D.48 We examined this subset in the spleen and pancreatic lymph nodes (PLN)of NOD mice using a short-term or chronic protocol of α-GalCer treatment, but didnot find an increase in the frequency of this subset (TABLE 1 and Ref 46). Thus, α-GalCer does not seem to activate or expand CD4+CD25+ regulatory T cells.
To determine whether α-GalCer promotes the expansion of NKT cells in second-ary lymphoid organs as well as in the pancreas, we examined this population in thespleen, PLN, and islet-infiltrating mononuclear cells of NOD mice following long-term α-GalCer therapy. NKT cells were tracked by double staining with an anti-TCRαβ mAb and CD1d tetramers loaded with α-GalCer. The frequency of NKTcells in α-GalCer–treated mice was increased threefold in the PLN and twofold inthe spleen, whereas these cells were absent from the islet-infiltrating cells regardlessof the treatment (TABLE 1 and Ref. 46). These findings suggest that the NKT-medi-ated immunoregulation can occur upstream of the pancreas, in the spleen and/orPLN. The detection of an α-GalCer–mediated expansion of NKT cells in the spleenand PLN may be due to the recruitment of monocyte-derived CD8α+ dendritic cellsto these lymphoid sites induced by α-GalCer treatment.49
NKT CELLS IN TRANSPLANTATION
Considering the in vivo immunoregulatory activities of NKT cells, it is temptingto speculate that they might mediate tolerance to allo- or xenografts. Recently, NKTcells were shown to mediate the induction of tolerance to cardiac allografts achievedby the blockade of CD28/B7 and lymphocyte function-associated antigen–1 (LFA-1)/intercellular adhesion molecule–1 (ICAM-1) interactions.27 Importantly, induc-tion of tolerance in this model was dependent on NKT-derived IFN-γ. NKT cells mayalso play a role in the induction of tolerance to hepatic allografts in rats.26 Prolon-gation of pancreaticoduodenal graft survival in nonrecurrent spontaneous diabeticBB rats is associated with the proliferation of donor-derived NKT cells in hepaticand splenic tissues and higher serum levels of IL-4.50 NKT cells are also requiredfor the acceptance of xenogeneic islet grafts in mice.51 In this model, which involvesgrafting Lewis rat islets into streptozotocin-induced diabetic C57BL/6 recipients,
85SHARIF et al.: MODULATION OF AUTOIMMUNE DIABETES BY NKT CELLS
administration of an anti-CD4 mAb results in prolongation of graft survival from 7days in control to as long as 60 days in the treatment group. Notably, the protectiveeffects of this treatment were abrogated in Jα281−/− mice, which lack Vα14+ NKTcells.51 It appears that neither IFN-γ nor IL-4 are involved in mediating the protec-tive effects of Va14 + NKT cells in this model.
Normoglycemia may be achieved in overtly diabetic NOD mice by grafting syn-geneic islets in the subcapsular region of their kidney. However, the grafted tissue isnot protected against the recurrent autoimmune response. Therefore, by day 10 post-transplantation, grafts are destroyed by the autoimmune response in most if not allthe recipients, and these recipients become hyperglycemic again. In this context, ex-ogenously added Th2 cytokines, including IL-4 and IL-10, can prolong islet graftsurvival in NOD recipients.52 Since we noted that α-GalCer polarizes NKT cells to-ward IL-4 and IL-10 production, we tested whether treatment of spontaneous diabet-ic NOD mice with α-GalCer prolongs graft function in recipients of islet transplants.While islet grafts failed in 90% of control vehicle-treated recipients by day 8 post-transplantation, grafts in over 80% of α-GalCer treated mice were still functional, asevidenced by the maintenance of euglycemia (TABLE 1 and Ref. 46). By day 10 post-transplantation, islet grafts in all control mice had failed, whereas this period was ex-tended to as long as 22 weeks in α-GalCer–treated mice. However, α-GalCer hasfailed thus far to prolong graft function in diabetic NOD recipients of allogeneic isletgrafts from B6 donors (our unpublished observations). In this model, both autoim-mune and allogeneic responses play a role in the destruction of grafted islets.
CONCLUSIONS
NKT cells, which are quantitatively and qualitatively deficient in diabetes-proneNOD mice and humans, provide an excellent target for future immunotherapeuticapproaches aimed at the prevention or reversal of human T1D. Since these cells playa major role in the early induction of Th1 and Th2 immune responses, appropriateactivation of NKT cells—for example, towards a Th2 response—may correct im-mune dyresgulation and prevent the pathogenesis of T1D. Indeed, our results indi-cate that activation of NKT cells by their ligand, α-GalCer, even when initiated afterthe onset of insulitis, protects NOD mice from T1D and prolongs pancreatic isletgraft survival significantly in overtly diabetic NOD mice. Protection from T1D is as-sociated with a dominant Th2-like immune response in the spleen and pancreas ofα-GalCer–treated diabetes-resistant NOD mice. Considering the proved lack of se-vere toxicity of α-GalCer in humans53 and the phylogenetic conservation of humanand mouse NKT cell response to α-GalCer,54 the use of this compound in clinicaltrials of human T1D may be warranted.
ACKNOWLEDGMENTS
We thank Drs. Luc Van Kaer, André Herbelin, Jean-François Bach, and BrianWilson for sharing their findings prior to publication. This work was supported bygrants from the Juvenile Diabetes Research Foundation International, the CanadianInstitutes of Health Research, and the London Health Sciences Center Multi-Organ
86 ANNALS NEW YORK ACADEMY OF SCIENCES
Transplant Program (to T.L.D.). S.S. is the recipient of a postdoctoral fellowshipfrom the Canadian Diabetes Association.
REFERENCES
1. DELOVITCH, T.L. & B. SINGH. 1997. The nonobese diabetic mouse as a model ofautoimmune diabetes: immune dysregulation gets the NOD. Immunity 7: 727–738.
2. RAPOPORT, M.J. et al. 1993. Interleukin 4 reverses T cell proliferative unresponsive-ness and prevents the onset of diabetes in nonobese diabetic mice. J. Exp. Med. 178:87–99.
3. CAMERON, M.J. et al. 1997. IL-4 prevents insulitis and insulin-dependent diabetes mel-litus in nonobese diabetic mice by potentiation of regulatory T helper-2 cell function.J. Immunol. 159: 4686–4692.
4. ARREAZA, G.A. et al. 1997. Neonatal activation of CD28 signaling overcomes T cellanergy and prevents autoimmune diabetes by an IL-4-dependent mechanism. J. Clin.Invest. 100: 2243–2253.
5. BENDELAC, A. et al. 1997. Mouse CD1-specific NK1 T cells: development, specificity,and function. Annu. Rev. Immunol. 15: 535–562.
6. TANIGUCHI, M. et al. 1996. Essential requirement of an invariant V alpha 14 T cell anti-gen receptor expression in the development of natural killer T cells. Proc. Natl.Acad. Sci. USA 93: 1125–1128.
7. PORCELLI, S. et al. 1993. Analysis of T cell antigen receptor (TCR) expression byhuman peripheral blood CD4-8- alpha/beta T cells demonstrates preferential use ofseveral V beta genes and an invariant TCR alpha chain. J. Exp. Med. 178: 1–16.
8. EBERL, G. et al. 1999. Tissue-specific segregation of CD1d-dependent and CD1d-inde-pendent NK T cells. J. Immunol. 162: 6410–6419.
9. HAMMOND, K.J. et al. 1999. NKT cells are phenotypically and functionally diverse.Eur. J. Immunol. 29: 3768–3781.
10. BENLAGHA, K. et al. 2000. In vivo identification of glycolipid antigen-specific T cellsusing fluorescent CD1d tetramers. J. Exp. Med. 191: 1895–1903.
11. MATSUDA, J.L. et al. 2000. Tracking the response of natural killer T cells to a gly-colipid antigen using CD1d tetramers. J. Exp. Med. 192: 741–754.
12. GODFREY, D.I. et al. 2000. NKT cells: facts, functions and fallacies. Immunol. Today21: 573–583.
13. LEGENDRE, V. et al. 1999. Selection of phenotypically distinct NK1.1+ T cells uponantigen expression in the thymus or in the liver. Eur. J. Immunol. 29: 2330–2343.
14. MAKINO, Y. et al. 1996 Development of Valpha4+ NK T cells in the early stages ofembryogenesis. Proc. Natl. Acad. Sci. USA. 93: 6516–6520.
15. MACDONALD, H.R. 2000. CD1d-glycolipid tetramers: a new tool to monitor naturalkiller T cells in health and disease. J. Exp. Med. 192: F15–20.
16. JOYCE, S. et al. 1998. Natural ligand of mouse CD1d1: cellular glycosylphosphatidyli-nositol. Science 279: 1541–1544.
17. MOLANO, A. et al. 2000. Cutting edge: the IgG response to the circumsporozoite pro-tein is MHC class II-dependent and CD1d-independent: exploring the role of GPIs inNK T cell activation and antimalarial responses. J. Immunol. 164: 5005–5009.
18. KAWANO, T. et al. 1997. CD1d-restricted and TCR-mediated activation of Valpha14NKT cells by glycosylceramides. Science 278: 1626–1629.
19. KITAMURA, H. et al. 1999. The natural killer T (NKT) cell ligand alpha-galactosylcera-mide demonstrates its immunopotentiating effect by inducing interleukin (IL)-12production by dendritic cells and IL-12 receptor expression on NKT cells. J. Exp.Med. 189: 1121–1128.
20. BURDIN, N., L. BROSSAY & M. KRONENBERG. 1999. Immunization with alpha-galacto-sylceramide polarizes CD1-reactive NK T cells towards Th2 cytokine synthesis. Eur.J. Immunol. 29: 2014–2025.
21. SINGH, N. et al. 1999. Activation of NK T cells by CD1d and alpha-galactosylceramidedirects conventional T cells to the acquisition of a Th2 phenotype. J. Immunol. 163:2373–2377.
87SHARIF et al.: MODULATION OF AUTOIMMUNE DIABETES BY NKT CELLS
22. YOSHIMOTO, T. et al. 1995. Defective IgE production by SJL mice is linked to theabsence of CD4+, NK1.1+ T cells that promptly produce interleukin 4. Proc. Natl.Acad. Sci. USA. 92: 11931–11934.
23. GUERY, J.C. et al. 1996. Selective development of T helper (Th)2 cells induced by con-tinuous administration of low dose soluble proteins to normal and beta(2)-microglo-bulin-deficient BALB/c mice. J. Exp. Med. 183: 485–497.
24. ZENG, D. et al. 1999. Bone marrow NK1.1(-) and NK1.1(+) T cells reciprocally regu-late acute graft versus host disease. J. Exp. Med. 189: 1073–1081.
25. SONODA, K.H. et al. 1999. CD1-reactive natural killer T cells are required for develop-ment of systemic tolerance through an immune-privileged site. J. Exp. Med. 190:1215–1226.
26. OHKAWA, A. et al. 1999. Immunological characteristics of intragraft NKR-P1+ TCRalpha beta+ T (NKT) cells in rat hepatic allografts. Transplant. Proc. 31: 2699–2700.
27. SEINO KI, K. et al. 2001. Requirement for natural killer T (NKT) cells in the inductionof allograft tolerance. Proc. Natl. Acad. Sci. USA 98: 2577–2581.
28. SONODA, K.H. et al. 2001. NK T cell-derived IL-10 is essential for the differentiationof antigen-specific T regulatory cells in systemic tolerance. J. Immunol. 166: 42–50.
29. FAUNCE, D.E. K.H. SONODA & J. STEIN-STREILEIN. 2001. MIP-2 recruits NKT cells tothe spleen during tolerance induction. J. Immunol. 166: 313–321.
30. FRITZ, R.B. & M.L. ZHAO. 2001. Regulation of experimental autoimmune encephalo-myelitis in the C57BL/6J Mouse by NK1.1(+), DX5(+), alphabeta(+) T cells. J.Immunol. 166: 4209–4215.
31. PAL, E. et al. 2001. Costimulation-dependent modulation of experimental autoimmuneencephalomyelitis by ligand stimulation of V alpha 14 NK T cells. J Immunol. 166:662–668.
32. MIEZA, M.A. et al. 1996. Selective reduction of V alpha 14+ NK T cells associatedwith disease development in autoimmune-prone mice. J. Immunol. 156: 4035–4040.
33. SUMIDA, T. et al. 1995. Selective reduction of T cells bearing invariant V alpha 24Jalpha Q antigen receptor in patients with systemic sclerosis. J. Exp. Med. 182: 1163–1168.
34. YANAGIHARA, Y. et al. 1999. Natural killer (NK) T cells are significantly decreased inthe peripheral blood of patients with rheumatoid arthritis (RA). Clin. Exp. Immunol.118: 131–136.
35. ILLES, Z. et al. 2000. Differential expression of NK T cell V alpha 24J alpha Q invari-ant TCR chain in the lesions of multiple sclerosis and chronic inflammatory demyeli-nating polyneuropathy. J. Immunol. 164: 4375–4381.
36. WILSON, S.B. et al. 1998. Extreme Th1 bias of invariant Valpha24JalphaQ T cells intype 1 diabetes. Nature 391: 177–181.
37. WILSON, S.B. et al. 2000. Multiple differences in gene expression in regulatory Valpha24Jalpha Q T cells from identical twins discordant for type I diabetes. Proc. Natl.Acad. Sci. USA 97: 7411–7416.
38. GOMBERT, J.M. et al. 1996. Early quantitative and functional deficiency of NK1+-likethymocytes in the NOD mouse. Eur. J. Immunol. 26: 2989–2998.
39. BAXTER, A.G. et al. 1997. Association between alphabetaTCR+CD4-CD8- T-cell defi-ciency and IDDM in NOD/Lt mice. Diabetes 46: 572–582.
40. IWAKOSHI, N.N. et al. 1999. Diabetes prone BB rats are severely deficient in naturalkiller T cells. Autoimmunity 31: 1–14.
41. GOMBERT, J.M. et al. 1996. IL-7 reverses NK1+ T cell-defective IL-4 production in thenon-obese diabetic mouse. Int. Immunol. 8: 1751–1758.
42. HAMMOND, K.J.L. et al. 1998. α/β-T cell receptor (TCR)+CD4-CD8- (NKT) thy-mocytes prevent insulin-dependent diabetes mellitus in nonobese diabetic (NOD)/Ltmice by the influence of interleukin (IL)-4 and/or IL-10. J. Exp. Med. 187: 1047–1056.
43. LEHUEN, A. et al. 1998. Overexpression of natural killer T cells protects Valpha14-Jalpha281 transgenic nonobese diabetic mice against diabetes. J. Exp. Med. 188:1831–1839.
44. LALOUX, V. et al. 2001. NK T Cell-induced protection against diabetes in Valpha14-Jalpha281 transgenic nonobese diabetic mice is associated with a Th2 shift circum-
88 ANNALS NEW YORK ACADEMY OF SCIENCES
scribed regionally to the islets and functionally to islet autoantigen. J. Immunol. 166:3749–3756.
45. FALCONE, M. et al. 1999. A defect in interleukin 12-induced activation and interferongamma secretion of peripheral natural killer T cells in nonobese diabetic mice sug-gests new pathogenic mechanisms for insulin-dependent diabetes mellitus. J. Exp.Med. 190: 963–972
46. SHARIF, S. et al. 2001. Activation of NKT cells by alpha galactosylceramide treatmentprevents the onset and recurrence of autoimmune type I diabetes. Nature Med. 7:1057–1062.
47. HONG, S. et al. 2001. Prevention of autoimmune diabetes in NOD mice by the naturalkiller T cell ligand α-galactosylceramide. Nature Med. 7: 1052–1056.
48. SALOMON, B. et al. 2000. B7/CD28 costimulation is essential for the homeostasis ofthe CD4+CD25+ immunoregulatory T cells that control autoimmune diabetes.Immunity 12: 431–440.
49. NAUMOV, Y. et al. 2001. Activation of CD1d-restricted T cells protects NOD mice fromdeveloping diabetes by regulating dendritic cell subsets. Proc. Natl. Acad. Sci. USA98: 13838–13843.
50. TORI, M. et al. 2000. Importance of donor-derived lymphocytes in the protection ofpancreaticoduodenal or islet grafts from recurrent autoimmunity: a role forRT6+NKR-P1+ T cells. Transplantation 70: 32–38.
51. IKEHARA, Y. et al. 2000. CD4(+) Valpha14 natural killer T cells are essential for accep-tance of rat islet xenografts in mice. J. Clin. Invest. 105: 1761–1767.
52. RABINOVITCH, A.O. et al. 1997. Combination therapy with cyclosporine and interleu-kin-4 or interleukin-10 prolongs survival of syngeneic pancreatic islet grafts in non-obese diabetic mice: islet graft survival does not correlate with mRNA levels of type1 or type 2 cytokines, or transforming growth factor-beta in the islet grafts. Trans-plantation 64: 1525–1531.
53. VAN DER VLIET, H.J. et al. 1999. Effects of alpha-galactosylceramide (KRN7000),interleukin-12 and interleukin-7 on phenotype and cytokine profile of humanVA24+Vβ11+ T cells. Immunology 98: 557–563.
54. BROSSAY, L. et al. 1998 CD1d-mediated recognition of an alpha-galactosylceramide bynatural killer T cells is highly conserved through mammalian evolution. J. Exp. Med.188: 1521–1528.