R. Ribes · A. Luna · P. Ros - download.e-bookshelf.de · cine, bone densitometry, and...
-
Upload
truongliem -
Category
Documents
-
view
217 -
download
0
Transcript of R. Ribes · A. Luna · P. Ros - download.e-bookshelf.de · cine, bone densitometry, and...

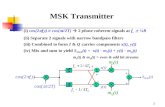
Learning Imaging
Series Editors:R. Ribes · A. Luna · P. Ros

R. Ribes · J. C. Vilanova (Eds.)
Learning Musculoskeletal Imaging

Ramón Ribes MD, JD, PhDPlatero Martinez 1914012 Córdoba [email protected]
Joan C. Vilanova , MD, PhDUniversity of GironaChief MRI UnitClínica GironaLorenzana, 3617002 [email protected]
ISBN: 978-3-540-87999-2 e-ISBN: 978-3-540-88000-4DOI: 10.1007/978-3-540-88000-4
Springer Heidelberg Dordrecht London New York
Library of Congress Control Number: 2010921306
© Springer-Verlag Berlin Heidelberg 2010
This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, spe-cifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other way, and storage in data banks. Duplication of this publication or parts thereof is permitted only under the provisions of the German Copyright Law of September 9, 1965, in its current version, and permission for use must always be obtained from Springer-Verlag. Violations are liable for prosecution under the German Copyright Law.
The use of general descriptive names, registered names, trademarks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use.
Product liability: The publishers cannot guarantee the accuracy of any information about dosage and application contained in this book. In every individual case the user must check such information by consulting the relevant literature.
Cover design: eStudioCalamar, Figueres/Berlin
Printed on acid-free paper
9 8 7 6 5 4 3 2 1
Springer is part of Springer Science+Business Media (www.springer.com)

“To Manuel Sánchez Gálvez, my first
hero.”
Ramón Ribes
“To my wife Cris and my children
Cristina and Eduard for their love
and for accommodating the sacrifices of
personal time.”
Joan C. Vilanova

Preface
Musculoskeletal (MSK) radiology is a radiological subspecialty that has expanded its
knowledge base and imaging capabilities with the advent of MRI, multi/detector CT, ultra-
sound, and PET. Prior to the advent of MRI, MSK radiologists used plain film X-rays and
arthrograms as their primary tools. The subspecialty has progressed from primary imag-
ing of osseous structures and indirect imaging of joint spaces, to direct imaging of soft
tissue structures with direct visualization and fine definition of MSK structures.
A specialized MSK radiologist requires a sound knowledge of anatomy, pathophysiol-
ogy, orthopedic surgical techniques, and advancements in imaging modalities. MSK imag-
ing involves all aspects about anatomy, function, disease states, and aspects of interventional
radiology appertaining to the MSK system including imaging in orthopedics, trauma,
rheumatology, metabolic and endocrine diseases, as well as aspects of pediatrics, oncology,
and sports imaging.
Subspecialty training in MSK radiology must ensure competence to obtain experience
in the following techniques: plain radiography, ultrasonography, CT, MRI, nuclear medi-
cine, bone densitometry, and fluoroscopic procedures including arthrography. MSK radi-
ologists must be aware of the strengths and weaknesses of the different imaging methods
in each pathological condition and choose the appropriate imaging technique and/or the
appropriate sequence in the investigation of specific clinical problems.
A MSK radiologist should be prepared to assure an in-depth understanding of disease
of the MSK system and understand the role of imaging in the diagnosis and treatment of
MSK disease. Moreover, because of innovation and new medical imaging modalities, there
are increasingly demanding requirements by clinical specialists. If radiologists do not or
cannot keep up with increasing demands for MSK interpretations, clinicians will be forced
to compete with radiologists in providing interpretations.
From the beginning of the subspecialty in the 1970s with the foundation of the
International Skeletal Society, multiple multidisciplinary or dedicated skeletal radiology
societies have been founded and organized from international or national societies.
We will try to expand the development of MSK radiology through complete prepared
radiologists, in order to develop the ability to transmit the knowledge and assume the con-
tinuity and evolution of radiological diagnosis in the field of MSK radiology.
Córdoba, Spain Ramon Ribes
Girona, Spain Joan C. Vilanova

1 Infection and ArthritisJosé A. Narváez, Matias De Albert, and Joan C. Vilanova . . . . . . . . . . . . . . . . . . . . . . . 1
Case 1.1 Femur Osteomyelitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2Case 1.2 Rheumatoid Arthritis of the Cervical Spine. . . . . . . . . . . . . . . . . 4 Case 1.3 Ankylosing Spondylitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6Case 1.4 Enthesitis in Psoriatic Arthritis . . . . . . . . . . . . . . . . . . . . . . . . . . . 8Case 1.5 Calcium Pyrophosphate Crystal Deposition Disease . . . . . . . . . 10Case 1.6 Muscular Abscess . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12Case 1.7 Septic Arthritis of the Pubic Symphysis . . . . . . . . . . . . . . . . . . . . 14Case 1.8 Facet Joint Arthritis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16Case 1.9 Cellulitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18Case 1.10 Pyogenic Spondylodiscitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22
2 TumorsGuadalupe Garrido-Ruiz, Antoino Luna-Alcalá, and Joan C. Vilanova . . . . . . . . . . . 23
Case 2.1 Osteoblastoma of the Rib . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24Case 2.2 Ewing’s Sarcoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26Case 2.3 Intraosseous Lipoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28Case 2.4 Giant Cell Tumor of Bone . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30Case 2.5 Skeletal Muscle Metastases . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32Case 2.6 Synovial Sarcoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34Case 2.7 Synovial Hemangioma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 36Case 2.8 Brown Tumor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38Case 2.9 Intramuscular Myxoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40Case 2.10 Soft-Tissue Liposarcoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44
3 Tendons and MusclesRosa Mónica Rodrigo, Mario Padrón, and Eugenia Sanchez-Lacalle . . . . . . . . . . . . 45
Case 3.1 Tennis Leg Injury . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46Case 3.2 Hamstring Muscle Injury . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 48Case 3.3 Indirect Rectus Femoris Strain Injury . . . . . . . . . . . . . . . . . . . . . 50Case 3.4 Adductor Muscle Strain Injury . . . . . . . . . . . . . . . . . . . . . . . . . . . 52Case 3.5 External Hip Rotator Muscle Injury . . . . . . . . . . . . . . . . . . . . . . . 54Case 3.6 Chronic Avulsion of the Ischial Tuberosity . . . . . . . . . . . . . . . . . 56Case 3.7 Acute Avulsion of the Anteroinferior Iliac Spine . . . . . . . . . . . . . 58Case 3.8 Patellar Tendinopathy: Partial Tear . . . . . . . . . . . . . . . . . . . . . . . . 60Case 3.9 Posterior Tibial Tendon Dysfunction . . . . . . . . . . . . . . . . . . . . . . 62Case 3.10 Partial Rupture of the Aquilles Tendon with Tendinosis . . . . . . 64Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 66
Contents

X Contents
4 Bone MarrowJoan C. Vilanova, Mercedes Roca, and Sandra Baleato . . . . . . . . . . . . . . . . . . . . . . . . 67
Case 4.1 Bone Metastasis of Melanoma in the Femoral Head Mimicking Avascular Necrosis . . . . . . . . . . . . . . . . . . . . . . . . . . . 68
Case 4.2 Bone Marrow Necrosis Due to Nonhodgkin’s Lymphoma . . . . . 70Case 4.3 Systemic Mastocytosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72Case 4.4 Bone Crisis in Gaucher’s Disease . . . . . . . . . . . . . . . . . . . . . . . . . . 74Case 4.5 Non-Hodgkin’s (Diffuse Large B-Cell) Lymphoma . . . . . . . . . . . 76Case 4.6 Shoulder Arthropathy Secondary to Gaucher’s Disease . . . . . . . 78Case 4.7 Multifocal Osteonecrosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 80Case 4.8 Multiple Myeloma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 82Case 4.9 Bone Metastases . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 84Case 4.10 Regional Migratory Osteoporosis . . . . . . . . . . . . . . . . . . . . . . . . . 86Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 88
5 SpineEva Llopis, Victoria Higueras, Elena Belloch, and María Vañó . . . . . . . . . . . . . . . . . 89
Case 5.1 Congenital Scoliosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 90Case 5.2 Herniated Disc Migration with Spontaneous Regression . . . . . 92Case 5.3 Ligamentum Flavum Cyst . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 94Case 5.4 Primary Vertebral and Epidural Lymphoma . . . . . . . . . . . . . . . . 96Case 5.5 Osteoid Osteoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 98Case 5.6 Meningioma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 100Case 5.7 Myeloma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 102Case 5.8 Fracture Dislocation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 104Case 5.9 Spondylo discitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 106Case 5.10 Sacral Chordoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 108Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 110
6 ShoulderFernando Idoate-Saralegui, and Joan C. Vilanova . . . . . . . . . . . . . . . . . . . . . . . . . . . . 111
Case 6.1 Adhesive Capsulitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 112Case 6.2 Parsonage: Turner Syndrome . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 114Case 6.3 Bankart Lesion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 116Case 6.4 Perthes Lesion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 118Case 6.5 Alpsa + Hill–Sachs Lesion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 120Case 6.6 Glad Lesion and Calcified Loose Body . . . . . . . . . . . . . . . . . . . . . 122Case 6.7 Slap Lesion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 124Case 6.8 Posterior Labral Tear + Paraglenoid Labral Cyst . . . . . . . . . . . . 126Case 6.9 Ambrii + Bilateral Labral Tears . . . . . . . . . . . . . . . . . . . . . . . . . . . 128Case 6.10 Posterosuperior Impingement (Throwing Shoulder + GIRD) . 130Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 133
7 Elbow, Hand, and WristJuan de Dios Berná, Ana Canga, and Luis Cerezal . . . . . . . . . . . . . . . . . . . . . . . . . . . . 135
Case 7.1 Slac Wrist . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 136Case 7.2 Scaphoid Avascular Necrosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 138

Contents XI
Case 7.3 Intraosseous Ganglia of the Lunate (“Pseudo-Kienböck” Disease) . . . . . . . . . . . . . . . . . . . . . . . . . . . . 140
Case 7.4 Glomus Tumor in the Thumb . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 142Case 7.5 Carpal Boss . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 144Case 7.6 De Quervain Tenosynovitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 146Case 7.7 Distal Biceps Tendon Rupture . . . . . . . . . . . . . . . . . . . . . . . . . . . . 148Case 7.8 Posterior Dislocation of the Elbow . . . . . . . . . . . . . . . . . . . . . . . . 150Case 7.9 Occult Fracture of the Radial Head . . . . . . . . . . . . . . . . . . . . . . . . 152Case 7.10 Pigmented Villonodular Synovitis of the Elbow . . . . . . . . . . . . . 154Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 156
8 Hip and PelvisAra Kassarjian, José Martel-Villagrán, and Ángel Bueno-Horcajadas . . . . . . . . . . 157
Case 8.1 Postpartum Sacral Fracture . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 158Case 8.2 Acute Avulsion Fracture of the Ischial Apophysis . . . . . . . . . . . . 160Case 8.3 Transient Osteoporosis of the Hip . . . . . . . . . . . . . . . . . . . . . . . . . 162Case 8.4 Osteolysis Associated with Total Hip Arthroplasty . . . . . . . . . . . 164Case 8.5 Osteomalacia with Looser Zones . . . . . . . . . . . . . . . . . . . . . . . . . . 166Case 8.6 Femoroacetabular Impingement (Predominantly Cam Type) . 168Case 8.7 Pubalgia Due to Common Adductor Tendon Microavulsion . . 170Case 8.8 Osteopoikilosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 172Case 8.9 Rapidly Destructive Osteoarthritis . . . . . . . . . . . . . . . . . . . . . . . . 174Case 8.10 Osteonecrosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 176Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 178
9 KneeJoan C. Vilanova, Sandra Baleato, and Joaquim Barceló . . . . . . . . . . . . . . . . . . . . . . . 179
Case 9.1 Lipoma Arborescens . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 180Case 9.2 Pigmented Villonodular Synovitis . . . . . . . . . . . . . . . . . . . . . . . . . 182Case 9.3 Spontaneous Osteonecrosis of the Knee . . . . . . . . . . . . . . . . . . . . 184Case 9.4 Discoid Meniscus . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 186Case 9.5 Osgood-Schlatter Disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 188Case 9.6 Chondromalacia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 190Case 9.7 Meniscal Tear . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 192Case 9.8 Osteochondritis Dissecans . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 194Case 9.9 Mucoid Degeneration of the Anterior Cruciate
Ligament with Ganglion Bone Cyst . . . . . . . . . . . . . . . . . . . . . . . . 196Case 9.10 Acute Meniscal and Ligament Tears of the Knee . . . . . . . . . . . . . 198Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 200
10 Ankle and FootXavier Tomas and Ana Isabel Garcia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 201
Case 10.1 Osteochondral Talar Lesion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 202Case 10.2 Calcaneal Fracture . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 204Case 10.3 Complete Achilles Tendon Tear . . . . . . . . . . . . . . . . . . . . . . . . . . . 206Case 10.4 Lateral Collateral Ligament Sprain . . . . . . . . . . . . . . . . . . . . . . . . 208Case 10.5 Syndesmotic Ankle Sprain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 210

Case 10.6 Plantar Fasciitis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 212Case 10.7 Plantar Fibromatosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 214 Case 10.8 Tarsal Tunnel Syndrome . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 216 Case 10.9 Diabetic Foot . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 218 Case 10.10 Intermetatarsal Bursitis and Morton’s Neuroma . . . . . . . . . . . . 220Further Reading . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 222
ContentsXII

Sandra BaleatoDepartment of RadiologyCHOP Complexo Hospitalario de Pontevedra PontevedraSpain
Joaquim BarcelóDepartment of RadiologyClínica Girona-Hospital Sta. CaterinaGironaSpain
Elena BellochDepartment of RadiologyHospital de la RiberaCarretera de Corbera km146600 ValenciaSpain
Ángel Bueno-HorcajadasHospital Universitario Fundación AlcorcónAlcorcón (Madrid)Spain
Juan de Dios Berná-MestreDepartment of RadiologyVirgen de la Arrixaca University Hospital30120 El Palmar (Murcia)Spain
Ana CangaDepartment of RadiologyMarqués de Valdecilla University HospitalRadiologic Anatomy39008 SantanderSpain
Luis CerezalDiagnóstico Médico Cantabria (DMC)Manuel Cacicedo 9139012 SantanderSpain
Matias de AlbertDepartment of RadiologyHospital Universitario de BellvitgeHospitalet de LlobregatBarcelonaSpain
Ana Isabel GarcíaRadiology DepartmentMuscle-Skeletal UnitHospital ClínicBarcelonaSpain
Guadalupe Garrido-RuizHospital Vall d’HebronBarcelonaSpain
Victoria HiguerasDepartment of RadiologyHospital de la RiberaCarretera de Corbera km146600 ValenciaSpain
Fernando Idoate-SaraleguiDepartment of RadiologyClínica San MiguelPamplonaSpain
Contributing Authors

XIV Contributing Authors
Ara KassarjianMassachusetts General HospitalBoston, MAUSA
Eva LlopisDepartment of RadiologyHospital de la RiberaCarretera de Corbera km146600 ValenciaSpain
Antonio Luna-AlcaláClínica Las Nieves Sercosa23007 JaénSpain
José Martel-VillagránCorades, S.L.Majadahonda (Madrid)Spain
Rosa Mónica RodrigoResonancia BilbaoBilbaoSpain
José A. NarváezDepartment of RadiologyHospital Universitario de BellvitgeHospitalet de LlobregatBarcelonaSpain
Mario PadrónRadiology DepartmentClínica CemtroMadridSpain
Mercedes RocaCiberer. Instituto Aragonés de Ciencias de la Salud I+D+IZaragozaSpain
Eugenia Sanchez-LacalleRadiology DepartmentClínica CemtroMadridSpain
Xavier TomasRadiology DepartmentMuscle-Skeletal UnitHospital ClínicBarcelonaSpain
Maria VañóDepartment of RadiologyHospital de la RiberaCarretera de Corbera km146600 ValenciaSpain,
Joan C. VilanovaUniversity of GironaChief MRI UnitClínica GironaLorenzana, 3617002 GironaSpain

Infection and Arthritis
José A. Narváez, Matias De Albert, and Joan C. Vilanova
1

J. A. Narváez, M. De Albert, and J. C. Vilanova2
Case 1.1
Femur Osteomyelitis
Fig. 1.1.1
Fig. 1.1.3
Fig. 1.1.4
Fig. 1.1.5
Fig. 1.1.2

Infection and Arthritis 3
A 9-year-old boy presented with a 3-week history of left hip pain. Four weeks prior, the patient
had suffered a superficial injury to his abdomen, which required a subcutaneous suture.
At admission, he had intermittent fever. He was reluctant to bear weight on his left limb
and had gait disturbances. Plain-film pelvic radiographs performed in the emergency
room were suspicious for a bone tumor of the left ischium. CT, bone scintigraphy, and MRI
examinations were requested to rule out bone tumor.
Acute hematogenous osteomyelitis usually occurs during skeletal growth when the growth
plate is open. Early detection of osteomyelitis is essential to enable therapy to be started
before bone devitalization.
Hematogenous osteomyelitis may not be evident on plain films until at least 10 days
after the onset of symptoms. The evolution of the infection can manifest radiographically
as soft-tissue swelling with obliteration of adjacent muscle planes, subperiosteal calcifica-
tion, and resorption of bony trabeculae.
Bone scintigraphy is highly sensitive for the diagnosis of osteomyelitis. Bone scintigra-
phy scans are sensitive indicators of altered osteoblastic activity, but local disturbances in
vascular perfusion, clearance rate, permeability, and chemical binding also affect imaging.
CT should be used only as a third-line technique for visualizing bony destruction, gas
within the bone, or bony sequestration.
MRI is highly sensitive as an indicator of disease because pathological findings are evi-
dent much earlier in the course of the disease. The MRI diagnosis of osteomyelitis is based
on its capability to detect bone marrow abnormalities within the physis.
Active osteomyelitis foci appear as low signal intensity areas on T1-weighted images and
high signal intensity areas on T2-weighted images, fat-suppression, or STIR sequences.
MRI is an excellent technique for the detection of osteomyelitis and the depiction of its
extent.
It is important to understand the limitations of each imaging technique to avoid delays
in the diagnosis and management of osteomyelitis and prevent possible complications.
The differential diagnosis of pelvic osteomyelitis in children should include septic
arthritis, Legg-Calve-Perthes disease, toxic synovitis, and less commonly, collagen-vascular
diseases, neoplasms involving bone, and retroperitoneal abscess.
Plain film of the pelvis (Fig. 1.1.1) shows no pathologic findings for bone infection in the
left femur. A swollen left ischiopubic synchondrosis was found incidentally (open arrow)
and was at first interpreted as the reason for the patient’s complaint. Bone scintigraphy
(Fig. 1.1.2) scan shows increased uptake within the left femoral head (arrow) and slight
uptake in the left ischiopubic synchondrosis (open arrowhead).
CT (Fig. 1.1.3) shows a round annular area in the left femoral head corresponding to the
focal site of infection.
Axial T1-weighted MRI (Fig. 1.1.4) shows diffuse low signal intensity within the proxi-
mal metaphysis of the left femur. Coronal STIR MRI (Fig. 1.1.5) reveals high signal inten-
sity in the bone marrow of the proximal femoral growth plate, with edema in the surrounding
soft-tissues. Note the hypertrophy of the ischiopubic synchondrosis (arrowhead).
Comments
Imaging Findings

J. A. Narváez, M. De Albert, and J. C. Vilanova4
A 58-year-old woman with a 10-year history of rheumatoid arthritis (RA) pre-
sented hyperreflexia and neck pain unresponsive to conventional treatment. No
sensory or motor deficits were found at neurologic examination. Radiographs and
MRI of the neck were requested to rule out cervical spinal canal compromise.
The cervical spine, particularly the craniocervical junction, is one of the most
common sites of RA involvement. The prevalence of cervical spine lesions of any
kind among RA patients ranges from 43 to 86%.
Cervical spine involvement can lead to severe pain and disability, as well as a
variety of neurological complications.
RA attacks the synovium; the atlantoaxial joint, where most of the synovial
tissue in the cervical spine is located, is where the disease is most prevalent and
Case 1.2
Rheumatoid Arthritis of the Cervical Spine
Fig. 1.2.4
Fig. 1.2.1
Fig. 1.2.2
Fig. 1.2.3
Comments

Infection and Arthritis 5
where characteristic changes are most evident at imaging. Atlantoaxial joint synovitis
erodes the transverse ligament that holds the odontoid process to the atlas and causes lax-
ity, resulting in anterior atlantoaxial subluxation. This is the most common pattern of
atlantoaxial instability.
Radiographs are the initial imaging method in these cases. The normal anterior atlanto-
odontoid interval is less than 3 mm. Anterior atlantoaxial subluxation may be not detected
in radiographs obtained in a neutral position, and lateral views with the neck flexed should
be obtained. When the anterior atlanto-odontoid interval is greater than 9 mm, the risk of
cord compression increases.
A more severe manifestation of atlantoaxial rheumatoid disease is vertical subluxation,
in which the odontoid process migrates upward, protruding into the foramen magnum.
This condition results from destruction of the lateral atlantoaxial joints or of bone around
the foramen magnum.
Subaxial (below C2 level) involvement is less common in RA. In this cervical spine segment,
the most common rheumatoid manifestation is anterior subluxation, caused by apophyseal
joint destruction. An anterior vertebral body displacement greater than 3 mm is diagnostic of
anterior subaxial subluxation. End-plate erosions, sclerosis, and destructive changes are
apparently due to extension of the inflammatory process from adjacent neurocentral joints
(the joints of Luschka, which are lined by synovium) into the discovertebral area
Magnetic resonance imaging (MRI) is the imaging modality of choice for assessing
involvement of the cervical spine in RA. It permits evaluation of the anatomical relation-
ships of the occiput, atlas, and axis, and it is therefore useful to define the extent of sublux-
ation of this spinal segment. It also permits direct visualization of periodontoid synovitis
formation, spinal cord, and brainstem.
MRI of the cervical spine is mandatory when spinal cord compression is clinically suspected.
In asymptomatic patients, MRI of the cervical spine should be considered when radiographs
show vertical subluxation, an anterior atlanto-odontoid interval greater than 9 mm, a posterior
atlanto-odontoid interval of 14 mm or less, or a subaxial canal diameter of 14 mm or less.
Lateral view of the cervical spine in neutral position (Fig. 1.2.1) shows a normal anterior
atlanto-odontoid interval (open arrow). Disc space narrowing, end-plate erosions, and sub-
chondral erosions are seen in the anterior region of C3–C4; the rest of the disc space is
spared and no associated osteophytes, which correspond to discovertebral rheumatoid
involvement, are present.
Lateral view of the cervical spine with the neck in flexion (Fig. 1.2.2) reveals anterior
atlantoaxial subluxation (anterior atlanto-odontoid interval of more than 3 mm) (arrows).
Sagittal T1-weighted (Fig. 1.2.3) and T2-weighted (Fig. 1.2.4) MRIs show periodontoid
synovitis, which presents low signal intensity on T1-weighted and high signal intensity on
T2-weighted images (open arrows). Periodontoid synovitis causes a mild mass effect on the
anterior thecal sac (arrowheads), but there is no cord compression. MRI was performed in
the neutral position, so the anterior atlantoaxial subluxation is not evident.
Note the small erosions and subchondral low signal intensity changes (open arrow-
heads) in the anterior region of the C3–C4 disc space.
Imaging Findings

J. A. Narváez, M. De Albert, and J. C. Vilanova6
A 47-year-old man presented with long-standing low back pain and stiffness.
Several years earlier, he was diagnosed with “probable degenerative disc disease.”
Radiographs of the lumbar and cervical spine and pelvis were obtained.
Ankylosing spondylitis is a chronic inflammatory disorder that mainly affects
the axial skeleton. It is more common in males, with a male-to-female ratio of
5:1. It is seen predominantly between the ages of 15 and 35 years.
Case 1.3
Ankylosing Spondylitis
Comments
Fig. 1.3.1 Fig. 1.3.2
Fig. 1.3.3 Fig. 1.3.4

Infection and Arthritis 7
The most common and characteristic initial symptoms are chronic, inflammatory low back
pain, and stiffness. Occasionally, back pain is too mild to impel the patient to seek medical care,
or it is misdiagnosed as sciatica due to degenerative disc disease, as occurred in our case.
Ankylosis spondylitis is characterized by bilateral sacroiliac and spinal involvement.
The sacroiliac joint is the first joint involved. The disease initial involves the spine in the
thoracolumbar junction and progresses to the lumbar and thoracic spine. Cervical spine
involvement is less frequent.
Radiographs are the initial imaging technique in these patients.
Radiographic signs of sacroiliitis are included in the diagnostic criteria of ankylosing
spondylitis. Small erosions are the initial radiographic abnormality, initially on the iliac
side and then on the sacral side. Usually, erosions are surrounded by subchondral sclerosis.
The anterior, synovial aspect of the joint ankyloses relatively early, but ankylosing of the
posterior, ligamentous aspect of the joint is common.
When radiographic findings are normal or inconclusive, CT can demonstrate these
destructive and reparative changes better.
Initially, radiographs of the spine show erosion of the anterior corners of the vertebral
body with secondary reactive sclerosis and a “squared” appearance of the vertebral body.
Ossification of the longitudinal ligaments is called syndesmophyte and involves the spine
in a symmetrical fashion. Spine ankylosis is associated to disc calcification. Ankylosing of
the apophyseal joints and ossification of the interspinous ligaments may be present. The
resulting appearance is called “bamboo spine.”
The axial distribution and the bone reparative changes with progression to ankylosis in
a short period of time allow a confident diagnosis in most cases.
In the last decade, MRI has been increasing used to study the inflammatory process in
ankylosing spondylitis and the other spondyloarthropathies. In contrast to radiographs
and CT, which detect destructive and reparative changes as mentioned above, MRI can
detect inflammatory changes at joints before these destructive-reparative changes take
place. MRI signs of early sacroiliitis are subchondral bone marrow edema and increased
signal on T2-weighted images and increased contrast-enhancement of the joint cavity, cor-
responding to synovitis. Bone marrow edematous changes at the ligamentous insertions
(entheses) in the spine are the hallmark of early disease.
Radiograph of the pelvis (Fig. 1.3.1) reveals complete ankylosis of both sacroiliac joints.
Ossification of the ligaments in the posterior superior portion of the joints is called the
“star” sign (open arrows).
Radiographs (AP and lateral views) of the lumbar spine (Figs. 1.3.2 and 1.3.3) demon-
strate bilateral, succinct syndesmophytes. Note also disk calcification and partial ankylosis
of the apophyseal joints.
Radiograph (lateral view) of the cervical spine (Fig. 1.3.4) shows anterior syndesmo-
phytes at some disc spaces (closed arrows), disc space calcification, and partial ankylosis of
the apophyseal joints.
Imaging Findings

J. A. Narváez, M. De Albert, and J. C. Vilanova8
Case 1.4
Enthesitis in Psoriatic Arthritis
Fig. 1.4.2
Fig. 1.4.3
Fig. 1.4.1

Infection and Arthritis 9
A 26-year-old man complained of a painful left heel for several months. Pain did not sub-
side with rest. Conservative treatment with relative rest, nonsteroidal antiinflammatory
drugs, and a soft rubber heel pad was ineffective.
Initially, radiographs were obtained. MR imaging study was requested to better evaluate
the soft-tissue structures of the heel.
The enthesis is the point where a tendon, ligament, or joint capsule attaches to bone.
Inflammation at the enthesis, or enthesitis, is considered the hallmark of the spondyloar-
thropathies, which are a group of inflammatory arthropathies that share some common
genetic, pathologic, and clinical features. This group includes ankylosing spondylitis, pso-
riatic arthritis, reactive arthritis (e.g., Reiter syndrome), arthritis associated with inflam-
matory bowel disease (e.g., Crohn disease or ulcerative colitis), and undifferentiated
spondyloarthritis.
Psoriatic arthritis has been defined as an inflammatory arthritis associated with psoria-
sis. Peripheral enthesitis is a common manifestation of psoriatic arthritis. The most com-
mon locations are at the enthesis of the Achilles tendon and plantar fascia in the calcaneus.
Enthesitis is usually bilateral and may be the initial manifestation of the disease.
Radiographs show erosions and bone proliferations at the enthesis of the Achilles ten-
don and plantar fascia, creating irregular and ill-defined spurs. The spurs tend to point
upward toward the calcaneus rather than downward along the course of the plantar aponeu-
rosis as occurs in normal heel spurs.
MRI not only identifies the destructive and reparative changes, but it also reveals the
inflammatory changes at the entheses. MRI signs of enthesitis include edematous changes
in the bone marrow adjacent to the insertion of the tendon or fascia and in the Achilles
tendon and plantar fascia themselves, which show increased signal intensity and variable
thickening. Edematous changes are also seen in the adjacent soft-tissues.
Erosions are seen as irregularity and defects of the bony margins, and sclerosis shows
low signal intensity on all pulse sequences. Precisely the aim of the MRI study is to identify
enthesitis before erosions and reparative sclerosis appear, making it possible to start effec-
tive treatment as early as possible.
Lateral view plain-film radiograph of the ankle (Fig. 1.4.1) shows erosion and bone forma-
tion at the attachment of the Achilles tendon (open arrow). There is also sclerosis and for-
mation of a calcaneus spur (closed arrow), which points upward toward the calcaneus.
T1-weighted (Fig. 1.4.2) and STIR (Fig. 1.4.3) MRI demonstrates extensive edematous
changes in bone marrow at the insertions of the Achilles tendon and plantar fascia (open
arrowheads). Note also the edematous changes in the adjacent soft-tissues, with small ret-
rocalcaneal bursitis (closed arrowheads).
Comments
Imaging Findings

J. A. Narváez, M. De Albert, and J. C. Vilanova10
Case 1.5
Calcium Pyrophosphate Crystal Deposition Disease
Fig. 1.5.1
Fig. 1.5.2
Fig. 1.5.3 Fig. 1.5.4
Fig. 1.5.5

Infection and Arthritis 11
A 73-year-old man complained of inflammatory cervical pain for 1 month. Cervical pain
increased progressively and required fentanyl treatment. After radiographs of the cervical
spine were inconclusive, a CT study of the cervical spine was requested.
Calcium pyrophosphate dehydrate (CPPD) crystal deposition is characterized by a constel-
lation of clinical manifestations, which can be grouped in five discrete patterns: pseudogout,
pseudoosteoarthritis with synovitis, pseudoosteoarthritis without synovitis, monoarthrop-
athy, and pseudorheumatoid arthritis.
CPPD crystals may be deposited as soft-tissue masses, a condition known as tophaceous
pseudogout. Commonly affected sites of deposition include the temporomandibular and
atlantoaxial joints, ligamentum flavum, and the finger joints.
Involvement of the atlantoaxial joint is primary related to ligamentous CPPD crystal
deposition, which is associated with periodontoid synovitis and bony erosions and cysts,
mainly in the odontoid process. Erosion of the odontoid process can produce a pathologic
fracture. Retrodental synovial masses with calcification can cause cervical cord compres-
sion. This syndrome of acute neck pain associated with calcification surrounding the
odontoid process has been described as “crowned dens syndrome.”
Symptomatic spinal involvement of the ligamentum flavum of the cervical and lumbar
spine has been reported.
Ligamentous calcification can be detected by radiographs, but CT is usually necessary to
identify calcifications in the periodontoid synovial masses, allowing a correct diagnosis.
MRI is useful to assess the relationships between these periodontoid masses and the
cervical cord.
Lateral view radiograph of the cervical spine (Fig. 1.5.1) shows small calcifications located
below the anterior rim of the atlas (open arrow), with ill-defined erosions of the odontoid
process.
Axial CT scans (Figs. 1.5.2 and 1.5.3) demonstrate calcified deposits (closed arrow) and
odontoid erosions (open arrowhead).
Coronal multidetector CT reconstruction of the cervical spine (Fig. 1.5.4) shows the
periodontoid calcifications.
Coronal multidetector CT reconstruction of the pelvis (Fig. 1.5.5) demonstrates a linear
calcification of the symphysis pubis as well as irregular calcifications at the adductor mus-
cle insertions (closed arrowheads).
Comments
Imaging Findings

J. A. Narváez, M. De Albert, and J. C. Vilanova12
Case 1.6
Muscular Abscess
Fig. 1.6.1
Fig. 1.6.2
Fig. 1.6.3 Fig. 1.6.4

Infection and Arthritis 13
A 52-year-old alcoholic man presented at the emergency department with disorientation
and depressed level of consciousness. Signs of malnutrition, hypotension, and generalized
edema were detected. Laboratory tests showed pancytopenia. Blood cultures were positive
for Streptococcus equisimilis, though no clear source of infection was identified. Five days
after admission, a cellulitic plaque appeared on his right thigh. He underwent ultrasonog-
raphy and CT.
Although most bacterial infections in the soft-tissues remain localized, depending on the
immunologic status of the patient, these infections can extend and may form an abscess.
The most commonly isolated pathogen in soft-tissue abscesses is S aureus, especially
methicillin-resistant S aureus.
Ultrasonography plays a major role in the detection and management of superficial
abscesses, but deeper fluid collections usually require MRI or CT. MRI and CT are the ideal
techniques to display the soft-tissue abnormalities and can be quite specific and helpful in
detecting the presence and extent of infection, which generally is suspected clinically on
the basis of physical and laboratory findings.
At ultrasonography, soft-tissue abscesses are demonstrated as an irregular fluid-filled
anechoic or diffusely hypoechoic area with posterior acoustic enhancement containing a
variable amount of echogenic debris. Color Doppler imaging may be used to demonstrate
hyperemia at the periphery of the mass and absence of flow in its center.
CT shows a well-demarcated fluid collection, with a peripheral pseudocapsule showing
rim enhancement.
MRI shows a well-demarcated fluid collection that is hypointense on T1-weighted
images and hyperintense on T2-weighted and STIR images, surrounded by a pseudocap-
sule with low signal intensity in all sequences and peripheral rim enhancement after intra-
venous administration of gadolinium-based contrast material.
Needle aspiration biopsy is mandatory if an abscess is suspected. Abscesses are treated
with antibiotics and percutaneous drainage.
Ultrasonographic image of the posterior compartment of the right thigh (Fig. 1.6.1) shows
a well-circumscribed hypoechoic subcutaneous cavity (open arrow) with internal echoes
(arrow) displacing the fat lobules (open arrowhead). The echogenic material filling the
abscess fluctuated on compression.
Power Doppler ultrasound image (Fig. 1.6.2) shows hyperemic blood flow within the
abscess wall (open arrow). No flow was seen in the center.
CT (Fig. 1.6.3) shows septations of the subcutaneous fat (open arrow), skin thickening
(arrow), and a small rim-enhancing, well-demarcated fluid collection adjacent to the biceps
femoris muscle (open arrowhead).
Coronal MPR CT (Fig. 1.6.4) shows the intramuscular location of the abscess, inside the
biceps femoral muscular fibers (open arrow).
Comments
Imaging Findings