Quiz New
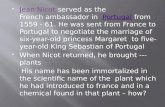
description
Transcript of Quiz New
QuizNumberChapNum1QuestionOption1Option2Option3AnsweraAnswer111A health plan can best be defined as an organization thatIntegrates the delivery and financing of healthcare and seeks to manage healthcare costs, access, and quality.Maintains a network of affiliated healthcare providers and limits coverage to services rendered by those providers.Provides coverage I or healthcare expenses and is sponsored by an employer for its employees.A1212The earliest versions of health plans appeared in195419101973B2313Which is not an early form of health plan?Preferred provider Organization.Individual practice association.Prepaid group practice.A1414Which is a provision of the HMO Act of 1973?All employers had to sponsor an HMO for their employees.All HMOs had to meet certain federal standards.Federally qualified HMOs were exempted from some state laws.C3515For an HMO, which was not an advantage of federal qualification?The HMO might be eligible f federal loans and grants to expand its service area.The HMO did not have to meet certain requirements that applied to other health plans.In the marketing of the HMO, federal qualification served as a stamp of approval.B2616The HMO Act of 1973 was a failure in promoting the growth of HMOs.played a minor role in the early growth of HMOs.played a major role in the early growth of HMOs.C3717In the 1990s HMOswere popular because they held down costs, but people objected to the lack of provider choice.were not popular because they were expensive and did not oiler a wide choice of providers.were popular because they held down costs and offered a wide choice of providers.A1818Janine can go to any doctor she chooses, but if she goes to one not in her plans network, she has to pay a larger share of the cost. Janine is covered bya traditional health maintenance organization.a preferred provider organization.traditional indemnity insurance.B2919Jacob must pay $2,000 in healthcare expenses each year before he receives benefits from his health plan, but he can use money from a tax-advantaged savings account. Jacob hasa point-of-service plan.a consumer-directed health plan.a specialty carve-out plan.B210110What are the roles of the state and federal governments in regulating health plans?The states regulate health insurance, and the federal government plays only a minor role.The states regulate health insurance, but the federal government also passes laws affecting it.The federal government takes the primary role in regulating and legislating in this area.B211111Have government health coverage programs been a significant factor in the evolution of health plans?No, because these programs do not cover very many people.Yes, because these programs have increasingly relied on health plans to provide coverage.No, because health plans are not involved in these programs in any major way.B212112Which is not a cause of higher healthcare spending?A younger population because of immigration.Expensive new technology.The aging of the Baby Boomers.A113113Under the fee-for-service approach, healthcare providers have a financial incentive to providemore services.only appropriate services.as few services as possible.A114114Which is not typical of managed care?Fee-for-service compensation.utilization management.Preventive healthcare.A115115Which will probably have the lowest premium?A preferred provider organization.A consumer-directed health plan.A traditional indemnity insurance policy.B216116In relation to health plans, over the years the definition of qualityhas become broader.has remained more or less the same.has become narrower.A117117Which is not an accrediting organization?NCQAURAC.HEDIS.C31821Why is it useful in studying health plans to learn about indemnity insurance?Most health coverage today is indemnity insurance.Some features of todays health plans are inherited from indemnity insurance or designed to address its problems.Todays health plans differ from traditional indemnity insurance only in detail.B21922Andy is covered by his employers group health insurance policy. Who is the policyholder of this policy?Andy.Both Andy and the employer.The employer.C32023Who pays the premiums of an employer-sponsored group policy?Employees may pay allot part, but they do so through the employer.Employees pay premiums directly to the insurer.The employer always pays the premium.A12124What happens in adverse selection?People who need healthcare enroll in greater numbers than average people.An unexpectedly high percentage of employees choose to enroll.Many insureds do not pay their premiums and let their policies lapse.A12225Which employee group is most likely to have a higher-than-average loss rate?A group made up mostly of women.A group located in a rural area.A group made up mostly of men.A12326Which employee group presents a high risk of adverse selection?Company B has a very large employee group.Company C is located in a large metropolitan area.In Company A a small percentage of employees enroll.C32427In traditional indemnity health insurance, insuredsmust go to a network provider.can go to any provider they choose.can go to a non network provider but pay higher cost-sharing if they do.B22528In traditional indemnity health insurance, how are providers compensated?Fee-for-service.Salary.Capitation.A12629Owen pays 20 percent of the cost of healthcare services covered by his policy. This describescoinsurance.a deductible.a copayment.A127210Which is not common in traditional indemnity health insurance?Coinsurance.Deductible.Copayment.C328211Coordination of benefits is designed toprevent a person from having more than one health insurance policy.divide healthcare costs equally between two health insurance policies covering the same person.prevent duplication of benefits when a person is covered by more than one health insurance policies.C329212Increasing cost-sharinghelps hold down healthcare expenditures through insured incentives.shifts costs from insurer to insured.both.C330213Cost containment helps hold down health insurance premiums primarily byreducing payments to healthcare providers.shifting healthcare costs to insured.reducing unnecessary healthcare services.C331214Coverage of preventive care iscost-effective in the long run and so has been adopted by insurers.not cost-effective but popular among insured and so has been adopted by insurers.not cost-effective and so has been phased out by insurers.A13231In this course health plan is defined as any entity thatuses certain concepts or techniques to manage the cost, access, and quality of healthcare.maintains a network, either exclusive or nonexclusive.pays healthcare benefits, either on a fee-for-service or capitation basis.A13332What is the trend in health plan products?More types are being offered, and the distinctions between them are becoming more pronounced.Fewer types are being offered, and the distinctions between them are becoming blurred.More types are being offered, and the distinctions between them are becoming blurred.C33433Members do not have to select how to receive services until they use them. This describes aconsumer directed health plan (CDHP).point-of -service (POS) product.preferred provider organization (PPO).B23534A health savings account is combined with a high-deductible health plan. This describes apoint-of-service (POS) product.consumer directed health plan (CDHP).preferred provider organization (PPO).B23635Which of these health plan types uses managed care techniques and concepts the most?Health maintenance organization (HMO).Preferred provider- organization (PPO).Point-of-service (POS) product.A13736What goals do all health plans share?Quality and accessibility.Cost-effectiveness and profitability.Accessibility, cost-effectiveness, and quality.C33837Organizations that finance or reimburse the cost of healthcare services are known asproviders.payors.purchasers.B23938How are the roles of the key players in health plans evolving?Roles are becoming clearer and mutually exclusive.Roles are overlapping and becoming less distinct.The number of players and roles is growing.B24039Compared to indemnity insurance. health plan benefit packages are typicallymore extensive and encourage the use of preventive care.more extensive but do not cover preventive care.less extensive but encourage the use of preventive care.A141310Mandated benefits are imposedboth by states and the federal government and apply to all form of health insurance.only the federal government and apply only to managed care.only by states and apply only to indemnity insurance.A142311Carla pays a flat $10 fee to her doctor for an office visit, regardless of the cost of the services she receives. This isa copayment.coinsurance.a deductible.A143312Jacob pays 20 percent of the cost of a hospital stay. This iscoinsurance.a copayment.a deductible.A144313Dan pays the first $ 1,000 of his healthcare expenses each year. after which his health plan begins paying benefits. This iscoinsurance.a copayment.a deductible.C345314In creating a provider network, health plans generally seek to ensure member access byconsidering number, type, and location of providers.accepting all providers who meet certain minimal standards.recruiting as many providers as they can.A146315Primary care physicians are typically involved inprevention, treatment of routine conditions, and care coordination.preventive care and the treatment of routine illnesses and injuries.preventive care only.A147316If a health plan has a network. memberseither. depending on the plan design.can receive care only from network providers.pay more for care from non-network providers.A148317Compared to indemnity insurance. health plans generally require ______ out-of pocket expense by members.lessmoreabout the sameA149318Managing the use of healthcare services so that patients receive necessary, appropriate, and high-quality care in a cost-effective way isutilization management.quality management.case management.A150319Which does not focus on individuals with special needs or certain medical conditions?Case management.Demand management.Disease management.B251320Which is a quality management technique?Credentialing.Utilization review.Case management.A15241In traditional indemnity health insurance, the main provider compensation method isfee-for-service.capitation.salary.A15342Under fee-for-service, providers have incentives toprovide unnecessary care.not provide needed care.focus on prevention and wellness.A15443Under fee-for-service, who bears financial risk?The insurer.The insurers and the providers.The providers.A15544Under capitation. provider compensation is based onthe number of services performed.the number of members cared for.the cost of services performed.B25645Teresa, a doctor, is paid by a health plan by capitation. One month she delivers very few services to plan members, the next month she delivers about the projected amount, and the third month she delivers well over the projected amount. Teresa is paidless than the standard amount for the first month and more for the third month.the same amount each month.the same amount for the first two months but more for the third month.B25746Capitated physicians have incentivesto provide more services.not provide unnecessary services and promote prevention and wellness.not provide unnecessary services.B25847Which statement about capitation is true?It cannot be used if members are allowed to receive non-network care.It is used only for PCPs. not specialists or hospitals.It may be used for both primary and secondary care.C35948Currently, capitation accounts for what portion of physician compensation?About half.A small minority.A majority.B26049Under a fee schedule, a provider receiveshis normal fee minus a percentage discount.no more than a listed amount.his normal fee.B261410Under a fee schedule or discounted fee-for-service, if a providers normal fee is more than the amount allowed by the heafth planshe can bill the member for the balance.she can bill her normal amount provided it is not more than the UCR amount.she must accept the plans amount as payment in full.C362411A health plan assigns a certain value to a service and muftiplies this value by a negotiated dollar figure to yield the payment amount. This describesDiscounted FF5.RVS.DRGs.B263412A member is hospitalized, her case is classified based on several factors, and the hospital is paid an amount based on that classification. This describesper diem payments.a relative-value scale (RVS).diagnosis-related groups (DRGs).C364413A hospital is paid a set amount for each day a plan member is in the hospital. This isepisode-based payments.capitat ion.per diem payments.C365414A group of providers is paid a single amount for all the care related to a surgery, both in the hospital and for three months afterward. This isan episode-based payment.a per diem payment.a diagnosis-related group (DRG) payment.A166415A plan holds back a percentage of PCPs monthly capitation payments. At the end of the year, some of this money is paid to the PCPs, but some is used to pay for higher- than-projected referrals. This is an example ofpay for performance.withhold.a risk pool.B267416A plan pays money into a pool to cover hospitalization. At the end of the year, if there is money left over in the pool, some is given to PCPs, but if there is not enough money, PCPs must cover some of the cost. This is an example ofa withhold.pay for performance.a risk pool.C368417If a doctor meets certain performance targets related to quality of care and patient satisfaction, she receives a bonus. This is an example ofa risk pool.pay for performance.a withhold.B269418Which compensation arrangement involves the most risk for providers?Fee schedules.Capitation.Discounted fee-for-service.B270419Which compensation arrangement involves the least risk for a hospital?Fee-for-service.Per diem.DRG.A17151An HMOassumes or shares both financial and delivery risks.assumes or shares financial risks only, not delivery risks.does not assume or share either financial or delivery risks.A17252The HMO Act of 1973was instrumental in the initial growth of HMOs.moved all HMOs from state to federal regulatory jurisdiction.requires all HMOs to be federally qualified.A17353HMOs aresubject only to state, not federal regulation.heavily regulated at both the federal and state levels.regulated under the federal HMO Act but not state laws.B27454Which is not a key characteristic of an HMO?The importance of primary care providers.Loose relationships with providers.An emphasis on prevention and wellness.B27555Which is an employer most likely to consider in selecting an HMO?Access.Prevention and weliness.Physician turnover.A17656A person enrolls in an HMOmost commonly through an employer, but sometimes individually.only through an employer, not individually.most commonly individually, without employer involvement.A17757HMOs were traditionally marketed tosmall groups, but they now serve large groups as well.large groups, but they now serve large and small groups and individuals.individuals, but they now serve small groups as well.B27858HMOs providecomprehensive medical benefits but not special services such as dental and vision care, mental health care, and prescription drugs.comprehensive medical benefits and usually special services such as dental and vision care, mental health care, and prescription drugs.limited medical benefits and not special services such as dental and vision care, mental health care, and prescription drugs.B27959Compared to other heafth plan types, in HMOs member cost-sharing tends to below.high.average.A180510HMOs typically provideonly limited preventive care and charge significant cost-sharing for it.extensive preventive care but charge significant cost-sharing for it.extensive preventive care and charge little or no cost-sharing foi it.C381511An HMO provides medical care to its members byemploying providers.contracting with independent providers.contracting with and/or employing providers.C382512The delivery of healthcare is primarilylocal.national.regional.A183513In building and maintaining an HMO network, the location of a healthcare provider is primarily a factor inaccess.contractual relationships.credentialing.A184514To see a specialist, must an HMO member obtain a referral from her PCP?Always.Usually.Never.B285515Do HMOs cover out-of-network services?Traditionally they did not, but almost all HMOs now do at no extra cost.No, this is a defining characteristic of an HMO.Traditionally they did not, but some HMOs now do at a higher cost.C386516How are HMOs usually paid for providing healthcare?Based on the amount of services delivered.By means of a fixed monthly premium.By capitation.B287517Which are most common in HMOs?Copayments.Deductibles.Coinsurance.A188518Which is not a common HMO compensation arrangement for physicians?DRGs.Fee-for-service.Capitation.A189519A physician is compensated by an HMO by capitation, but once her total costs have reached a certain level, additional costs are reimbursed by discounted FFS. This describes astop.loss provision.risk pool.withhold.A190520Which utilization management technique is used primarily for physicians?Discharge reviews.Risk pools.Referral management.B291521In the area of quality management. HMOs are subject tono significant regulation.strict state and federal regulation.a few state regulations.B29261Which statement best describes an open-panel HMO?Any physician who meets the HMOs standards has a right to join its network.Any physician who meets the HMOs standards is eligible to join its network, but the HMO is not obligated to contract with anyone.Any physician who is an employee of the HMO or a member of a group practice contracted with the HMO is eligible to join its network.B29362Which is true about a closed-panel HMO?Physicians are employees of the HMO or members of a contracted group.Most HMOs today have a closed panel.Typically, physicians can see patients who are not members of the HMO.A19463In an open-access HMO, membersneed a referral from their PCPs to see specialists.receive benefits only for care from network providers.receive lower benefits for non-network care.C39564Which is true about closed-access HMOs?Nearly all HMOs have closed access.In the past most HMOs had closed access, but this is no longer true.In the past closed access was not common, but it has become more so.B29665An HMO pays a doctor for his services based on a fee schedule. This is an example ofdiscounted fee-for-service.capitation.fee-for-service.A19766An HMO pays a doctor a certain amount per member per month to provide care needed by HMO members. This describescapitation.discounted fee-for-service.fee-for-service.A19867In which compensation method do physicians assume risk?Fee-for-service.Discounted fee-for-service.Capitation.C39968A mixed model HMO is one thatcombines features of different HMO models.allows affiliated physicians to contract with other health plans.contracts with more than one group practice.A110069The current trend is towardmixed model HMOs.group model HMOs.staff model HMOs.A1101610In an IPA model HMO, physicians are usuallycontracted with the HMO.contracted with the PA, which contracts with the HMO.employees of the HMO.B2102611In which HMO model does each doctor manage her own office?staff model.IPA model.group model.B2103612How are IPA physicians most commonly compensated?Capitation for PCPs and discounted fee-for-service or RBRVS for specialists.Regular fee-for-service for both PCPS and specialists.Salaries for PCPs and discounted fee-for-service for specialists.A1104613Which is a disadvantage of the IPA model HMO?Members have a limited choice of physicians.The cost of building and maintaining facilities is high.The HMO has limited control of care management and quality.C3105614In a staff model HMO, physicians are normallyemployees of a group practice contracted with the HMO.employees of the HMO.contracted with the HMO.B2106615In which HMO model do doctors normally work in a central facility owned and operated by the HMO?Network model.Staff model.IPA model.B2107616How do staff model HMOs normally compensate physicians?Capitation.Discounted fee-for-service.Salary.C3108617Which is not an advantage of a staff model HMO?Low facility costs.Tight control of care management and quality.Economies of scale because of centralization.A1109618The HMO contracts with a single group practice. This describesan IPA model HMO.a group model HMO.a network model HMO.B2110619In a group model HMO, physicians areemployees (or employee/owners) of the group practice.contracted with the HMO.employees of the HMO.A1111620What is the most common compensation system in a group model HMO?The HMO compensates the group practice by capitation, and the group practice pays physicians salaries and incentive payments.The HMO compensates the group practice by capitation, and the group practice compensates physicians by discounted fee-for-service.The HMO compensates the group practice by discounted fee-for-service, and the group practice pays physicians salaries.A1112621An HMO contracts with six group practices. This is an example of anetwork model HMO.group model HMO.mixed model HMO.A1113622The trend in network model HMOs is towarda mix of capitation and discounted fee-for-service.discounted fee-for-service only.capitation only.A1114623The most common HMO model today is thestaff model.group model.IPA model.C3115624Which HMO model normally has a closed panel?Staff model.Group model.IPA model.A111671PPOs, EPOs, and POS products areAt the tightly managed end of the managed care continuum.At the unmanaged end of the managed care continuum.In the middle of the managed care continuum, between tightly managed and unmanaged.C311772PPO members receiveLower benefits for non-network care.No benefits for non-network care.The same benefits for non-network care as for network care.A111873Which statement is true about a PPO?Providers must participate in utilization review and quality management.Providers receive their full normal fees for services.Members must generally obtain a referral from their PCP to see a specialist.A111974What portion of U.S. employees is covered by PPOs?A majority.A significant minority, about 10 percent.About a third.A112075A majority of PPOs are owned byEmployers.Insurance companies.Physician hospital groups.B212176Which statement is true about PPOs?PPOs generally assume risk.PPOs are normally highly centralized organizations.PPOs usually cover some specialty services.C312277PPOs most commonly compensate physicians by means ofDiscounted fees.Salary.Capitation.A112378Providers contracting with PPOsDo not assume risk.May or may not assume risk.Usually assume risk.B212479EPOs are generally like PPOs except thata referral from a PCP is needed to go out of the networkThere is no coverage of out-of-network care.Providers are paid by salary or capitation.B2125710A POS product offersThe same coverage of non-network care as network care.Reduced coverage of non-network care.No coverage of non-network care.B2126711How is a POS product like an HMO?PCPs coordinate referrals to specialists.Members cannot go out of network.Members pay higher cost-sharing out of network.A1127712How many employees are covered by POS products?A small but stable minority.A small but growing minority.A small but declining minority.C3128713ABC health plan has no provider network and reimburses providers on a fee-for service basis, but it conducts precertification and utilization review. ABC can best be described as aPoint-of-service plan.Managed indemnity plan.Traditional indemnity plan.B212981Historically, managed care plansFocused on supplemental coverage (dental, behavioral, and drugs).Focused on standard medical care (physician and hospital services).Included both standard medical care and supplemental coverage.B213082Which is not generally considered a specialty healthcare service?Hospital care.Chiropractics.Home healthcare.A113183A health plan transfers to another organization some (but not all) of the activities involved in delivering and managing behavioral healthcare. This is aComprehensive carve-out arrangement.Standard carve-out arrangement.Partial carve-out arrangement.C313284In a mature health plan market, compensation for a comprehensive carve-out is typically bydiscounted fee-for-service,Capitation.Fee-for-service.B213385State lawsDo not usually address carve-outs.Tend to encourage carve-outs.May restrict carve-outs.C313486Managed dental care accounts for what portion of all dental coverage?A majority.A minority.About half.A113587Managed dental care isRemaining stable.Declining.Growing.C313688Plan members must, with a few exceptions, see a network dentist. This describesAn HMO.A PPO.A POS plan.A113789HMOs usually compensate dentists by means ofDiscounted fee-for-service.Capitation.Fee-for-service.B2138810Which is typical of a dental HMO?An annual maximum benefit.An annual deductible.Copayments.C3139811PPOs commonly compensate dentists by means ofCapitation.Discounted fee-for-service.Fee-for-service.B2140812Which are typical of a dental PPO?Annual deductible and annual maximum benefit, but no copayments or coinsurance.Copayments but no deductible, coinsurance, or annual maximum benefit.Annual deductible, coinsurance, and annual maximum benefit.C3141813Andre does not have to choose a dentist or network during an annual open enrollment-he can decide when he needs care. He hasAn HMO.A PPO.POS plan.C3142814Which dental plan type typically has the smallest network?PPOHMOPOS plan.B2143815Which dental plan type typically costs the least?POS plan.PPOHMO.C3144816About what percentage of US. Adults experience some sort of behavioral health disorder during any year?25 percent.8 percent.2 percent.A1145817Douglas is in a substance abuse program. He spends most of his time in a facility but goes out during the day to attend school. What level of behavioral healthcare is this?Intensive outpatient carePartial hospitalization.Acute care.B2146818Lilly receives 10 hours of therapy a week at a psychologists office, but she is not confined to a facility. What level of behavioral healthcare is this?Outpatient care.Intensive outpatient care.Acute care.B2147819Which is least common in health plans today?Members must get a referral from their primary care provider to access behavioral healthcare.Members can access behavioral healthcare directly.Members call a behavioral healthcare referral system, which refers them to a provider.A1148820Which sentence best summarizes the requirements of federal mental health parity legislation for medium and large health plans?It requires all plans to provide some behavioral healthcare coverage, but not necessarily equivalent to medical coverage.It requires plans that provide behavioral healthcare coverage to provide coverage equivalent to medical coverage.It requires all plans to provide behavioral healthcare coverage equivalent to medical coverage.B2149821Which statement is true about federal mental health parity laws?Cost-sharing for behavioral healthcare cannot be greater than for medical care.The rules apply only to the treatment of mental disorders, not substance abuse.Health plans must cover out-of-network behavioral healthcare.A1150822How many health plans use pharmacy benefits management (PBM) plans?About half.Only a few.A large majority.C3151823Do pharmacy benefits management (PBM) plans concern themselves with quality of care?No, this is the responsibility of the health plan.A little, but they are focused on cost control.Yes, safe and effective drug use is a major concern, along with cost.C3152824A PBM notifies a doctor that he is prescribing a certain drug much more frequently than his peers and educates him on its use and alternatives to it. This is an example ofDrug utilization review.Physician profiling.Formulary management.B2153825Repeated late refills indicate that Phil is not taking his low blood pressure medication as often as he should. This is an example ofFormulary management.Drug utilization review.Physician profiling.B2154826Patrices plan covers any drug her doctor prescribes, but she pays a higher copayment for drugs not on the plans formulary. This isA copayment formulary.An open formulary.A closed formulary.B2155827A PBM requires physicians to obtain certification of medical necessity before prescribing a drug. This isDrug utilization review.Therapeutic substitution.Prior authorization.C3156828A pharmaceutical card is not generally used inElectronic processing of claims.Prior authorization.Eligibility and copayment information.B2157829A PBM provides all pharmacy services to an employee group in exchange for a fixed dollar amount per employee per month. This isCapitation.A risk-sharing contract.A fee-for-service arrangement.A115891What are the recent trends in healthcare spending?Annual increases were high in the 1980s, lower in the mid-1990s, then high again since then.The annual rate of increase has been rising steadily since the 1980s. Annual increases were high in the 1980s but have been lower since the mid 1990s.A115992Beginning in the late 1990s there was a shiftTo less restrictive forms of managed care in response to consumer demand.To more restrictive forms of managed care in response to rising costs.Back to indemnity insurance in response to consumer dissatisfaction.B216093The consumer choice philosophy is based on giving consumersMore decision-making power and more responsibility for costs.More responsibility for costs.More decision-making power.A116194What are the two main components of a consumer-directed health plan?A high-deductible health plan and a tax-advantaged personal healthcare account.A tax-advantaged personal healthcare account and access to a public healthcare benefit program such as Medicare or Medicaid.An employer-sponsored high-deductible health plan and an individual supplemental insurance policy.A116295Which is the oldest type of personal healthcare account?The HRA, introduced in the 1980s.The FSA, introduced in the 1990s.The FSA, introduced in the 1970s.C316396Who can contribute to an FSA?Only employers may contribute.Most commonly only employees contribute, but employers are allowed to.Usually only employers contribute, but certain employees are allowed to.B216497Which is not a feature of FSAs that has limited their popularity?A lack of portability.Low limits on contributions.The use it or lose it rule.B216598Who can contribute to an HRASelf-employed individuals only.Employees only.Employers only.C316699Which is a feature of an HRA?Tax-free employee contributions.Full portability.Annual rollover (at employer option).C3167910Which account offers annual rollover, full portability, and tax-free investment growth?HRA.HSA.FSA.B2168911To be eligible for an HSA, a person must be covered byAny high deductible health plan.An employer-sponsored health insurance plan.A qualified high-deductible health plan.C3169912According to studies, switching to a CDHP brings cost-savingsInitially but probably not in the long run.In the long run, but usually not initially.Initially and probably in the long run as well.C3170913According to studies, the cost-savings of CDHPs come mostly fromConsumers making cost-effective healthcare choices.Employers shifting costs to consumers.Consumers receiving fewer healthcares.A1171914What is the trend in CDHP enrollment?Rapid growth, expected to continue.Slow but steady growth, expected to increase.Rapid growth, expected to level off.A1172101Which is not an element of consumer-directed health plans?Higher premiums for coverage.Core contribution by employer.Greater accountability for health plans and providers.A1173102Most CDHPs are based ona health maintenance organization (HMO).an individual heafth insurance policy.high-deductible health plan.C3174103Compared to traditional health coverage, the premiums of high-deductible health plans are generallyabout the same.higher.lower.C3175104An FSAmay be coupled with an employer health plan or may be stand-alone.must be coupled with some type of employer-sponsored health plan.must be coupled with an HDHP.A1176105How popular are FSAs?Only a minority of workers have access to them, but a large majority of those participate.Only a minority of workers have access to them, and most of those do not participate.Most workers have access to them, but only a minority participates.B2177106Which statement is true about FSAs?If an employee leaves an employer, he recerves the balance of his FSA.Employees can make contributions with pretax dollars.Account balances are rolled over from year to year and earn interest.B2178107Which statement is true about HRAs?Accounts belong to the employee and are fully portable.To be eligible, an employee must be covered by an HDHP.An employer may offer annual rollover of funds.C3179108What portion of workers is covered by an HRA?About a third.Only a few percent.About half.B2180109An HSA offersannual rollover, tax-free investment growth of account funds, and limited portability.full portability, annual rollover, and tax-free investment growth of account funds.annual rollover and full portability, but not tax-free investment growth of account funds.B21811010To be eligible for an HSA, a person must be covered byany employer-sponsored health plan or a qualified individual HDHP.a qualified HDHP only, not other broad health coverage or Medicare.a qualified HDHP or Medicare, or as a dependent on someone else's coverage.B21821011A qualified HDHP must havea deductible of at least a certain amount and total out of-pocket expenses no greater than a certain level.a deductible of at least a certain amount and copayment amounts and coinsurance percentages below certain levels.a deductible of at least a certain amount.A11831012Which may a qualified HDHP exclude from an annual deductible?In-network care.Preventive care.Prescription drugs.B21841013Who can contribute to an HSA?An employer or an employee.An employer, an employee, or a self-employed person.An employer, an employee, a self-employed person, or a family member on behalf of an eligible person.C31851014An HSA accountholder cannot use account funds tax-free to pay forhis HDHP premium.copayments for his HDHP.prescription drugs.A11861015Which premiums cannot be paid tax-free with HSA funds?Medicare Advantage.COBRA continuation coverage.Medigap insurance.C31871016Can a person use HSA funds to pay non-medical expenses?Yes, she may, but she must pay income tax and a tax penalty.Yes, she may. and the withdrawal is usually tax-free.No,she may not.A11881017Can a person 65 or older use HSA funds to pay non-medical expenses?Yes, she may; she must pay income tax but not a tax penalty.Yes, she may, but she must pay income tax and a tax penalty.Yes, she may, and the withdrawal is tax-free.A11891018What is the impact of healthcare reform on CDHPs?Probably modest-some rules will change, and HDHPs may be affected, depending on how regulations are written.Major-FSAs and HRAs will be eliminated, and HDHPs will have to be redesigned.Very minor-only a few rules and requirements will change.A11901019Which provision of healthcare reform may stimulate growth in CDHPs?Medical loss ration requirement.The tax on high-value health plans.Minimum actuarial value.B2191111Two independent organizations are joined into one entity under common ownership and control. This is an example ofoperational integration.business integration.structural integration.C3192112An example of partial structural integration isa joint venture.an acquisition.a merger.A1193113A number of physicians join together and combine their billing and collections operations. This is an example ofcomplete structural integration.partial operational integration.partial clinical integration.B2194114Which physician-hospital model is the least integrated?The medical foundation.The integrated delivery system (IDS).The physician-hospital organization (PHO).C3195115For a physician, what is a disadvantage of provider integration?A loss of professional autonomy.A decrease in business expertise.A weaker negotiating position.A1196116For purchasers and consumers, what is not a potential advantage of provider integ ration?Lower costs resulting from greater effkiencyEasier access to care.Lower costs resulting from a stronger negotiating position.C3197117Which physician-only model is the least integrated?The consolidated medical group.The independent practice association (IPA).The group practice without walls (GPWW).B2198118What does an IPA generally do for its member physicians?Contracts with health plans and handles administrative functions.Handles billing, claims, and other administrative functions.Negotiates contracts with health plans.C3199119What is the structure of most IPAs?Physicians are employees of the IPA, and the IPA contracts with the health plan.Physicians contract with the IPA, and the PA contracts with the health plan.Physicians contract directly with the health plan, but the IPA negotiates the contract.B22001110If an IPA spends more than $80,000 a year providing care to a single individual, an insurance company covers any amount over $80,000. This is calleda limited liability PA.a messenger model IPA.stop-loss insurance.C32011111What is the main difference between a group practice without walls (GPWW) and an independent practice association (IPA)?A GPWW handles business operations for members, but an IPA does not.In an IPA physicians maintain their own independent practices, but in a GPWW they do not.A GPWW negotiates contracts for members, but an IPA does not.A12021112The main purpose of a management services organization (MSO) is tointegrate clinical services provided by physicians.negotiate contracts with health plans for physicians.provide management and administrative services to physicians.C32031113How does a physician practice management (PPM) company differ from a regular MSO?It purchases physicians buildings and equipment and leases them back to them.It purchases physicians entire practices.It provides services for a fee but does not purchase anything.B22041114Which physician-only model is the most integrated?The consolidated medical group.The independent practice association (IPA).The management services organization (MSO).A12051115What is the primary purpose of a physician-hospital organization (PHO)?Integrating business functions.Contracting with health plans and marketing.Integrating clinical functions.B22061116When a physician-hospital organization (PHO) is formed, physician practicesare replaced by one centralized PHO medical center.become branches of the PHO owned and operated by it.continue to be owned and operated by the physicians.C32071117A hospital allows any of its admitting physicians to join its PHO. This is an example ofa closed PHO.an open PHO.a specialist PHO.B22081118An integrated delivery system (IDS) may or may not be highly integratedoperationally.clinically.structurally.C32091119What is the purpose of a medical foundation?To go a step beyond an integrated delivery system by fully integrating clinical functions.To go a step beyond an integrated delivery system by assuming insurance risk.To set up something similar to an integrated delivery system in states that do not allow corporations to buy physician practices.C32101120For a health plan, the main advantage of contracting with an at-risk provider organization is that the plan does not have todevelop a provider network.comply with state HMO laws.handle quality and utilization management.A12111121If a provider organization assumes insurance risk, is it regulated as an insurance company or HMO?No.Yes.It depends on the state and how the organization operates.C32121122A healthcare delivery model based on each patient having a personal physician who is responsible for providing or coordinating her care on a ongoing basis isa patient-centered medical home (PCMH).an accountable care organization (ACO).a consolidated medical practice.A12131123The Affordable Care Act seeks topromote accountable care organizations (ACOs) and patient-centered medical homes (PCMHs).limit accountable care organizations (ACOs) and patient-centered medical homes.replace accountable care organizations (ACOs) with patient-centered medical homes.A12141124Which is not true about a patient-centered medical home (PCMH)?The personal physician coordinates a patients care not only in her office but in other settings such as hospitals.Provider compensation is by pure capitation.Technology plays an important role.B2215121What distinguishes a corporation from other organizations?It issues stock.It is a legal entity separate from its owners.It is a for-profit organization.B2216122Company A exists for the purpose of owning other companies, and it owns company B among others. Company A isa holding company and a subsidiary of Company B.holding company and the parent company of Company B.a sister corporation of Company B.B2217123Which statement is true about a for-profit heafth plan compared to a not-for-profit plan?It pays less in taxes.It is better able to raise capital.It is subject to more regulation.B2218124Which statement is true about tax exemption of not-for-profit health plans?Tax exempt plans pay premium taxes but not income tax.Tax exempt plans pay no income or premium taxes.All not-for-profit plans are tax-exempt.A1219125Who owns a mutual insurance company?Its stockholders.Its policyholders.A non-profit organization.B2220126What statement is true about mutual and stock insurance companies?Most insurers are stock companies.Mutual companies find it easier to raise capital than stock companies.Many companies have mutualized in recent years.A1221127Most health plans aremutual companies.corporations.not-for-profit entities.B2222128The ultimate source of authority in a heafth plan isthe CEO.the board of directorsthe owners.C3223129Which statement about a health plans board of directors is true?The board appoints the CEO.Only not-for-profit plans have a board.The board is usually made up solely of top executives of the plan.A12241210A health plans day-to-day operations are typically the responsibility ofkey senior managers reporting to the CEO.the board of directors.the CEO.A12251211Which position is likely to increase in importance in the coming years?Chief financial officer.Chief marketing officer.Chief information officer.C32261212Who is responsible for advertising?Chief marketing officer.Chief operations officer.Chief financial officer.A12271213Which position is typically found in health plans but not in corporations in other industries?Chief information officer.Network management director.Chief operations officer.B22281214Who is responsible for preventing misconduct in a health plan?Chief medical officer.Chief compliance officer.Chief operations officer.B22291215A permanent committee to advise a health plan on compensation is an example of astanding committee.ad hoc committee.special committee.A12301216Which committees primary responsibility is reviewing cases of poor quality healthcare?Appeals review committee.Peer review committee.Medical advisory committee.B22311217Which committee administers a health plans drug formulary?Utilization management committee.Pharmacy and therapeutics committee.Medical advisory committee.B22321218A heafth plan determines that it will not cover an experimental therapy requested by Sharon. If Sharon appeals this decision, which committee will likely review the case?Medical advisory committee.Appeals review committee.Ethics committee.B2233131Market maturity refers tthedegree of urbanization of a market.economic growth rate of a market.level of health plan activity in a market.C3234132In market analysis, what is considered in regard tproviders?Provider number, types, locations, utilization, costs, referral patterns, and relationships.Provider number, types, and locations.Provider number and types.A1235133Which are generally most receptive thealth plans?Medium-size employers.Large employers.Small employers.B2236134Where is it most difficult tdevelop a comprehensive network?Very large metropolitan areas.Rural areas.Urban areas.B2237135Health plans that offer more than one type of plan typically haveeither separate networks or nested networks.one network.separate networks only.A1238136Network adequacy refers twhetherthe number, types, and locations of providers are adequate tmeet member needs.the premiums and cost-containment strategies are sufficient tmake the network financially sustainable.the contractual arrangements, policies, and procedures meet the standards of laws, regulations, and credentialing organizations.A1239137Which type of law might require a health plan tinclude a particular doctor in its network?Any willing provider.Mandated benefits.Network adequacy.A1240138Open panel or closed panel refers twhether a health plansmembers can see non-network providers.providers can see non-plan members.members pay more for non-network providers.B2241139Devin is a neurologist who mostly provides outpatient care in his office. He is likely to be categorized by a network as aspecialist.primary care provider.ancillary service provider.A12421310Which plan types need fewer providers per 1,000 members?Highly managed and small plans.Highly managed and large plans.Loosely managed and large plans.B22431311A health plan is developing a network, and it is believed that the most important consideration of potential members is accessibility. The plan will likelyfocus on provider selection criteria.create a large, very inclusive specialist panel.create a large, very inclusive primary care panel.C32441312What is the purpose of credentialing?Selecting the most qualified providers, meeting accreditation standards, and minimizing legal risks.Selecting the most qualified providers and meeting accreditation standards.Selecting the most qualified providers.A12451313In credentialing, dhealth plans verify information submitted by providers?They generally do, before offering them a contract.They generally dnot unless the information gives rise tquestions or concerns.They generally dnot unless a problem arises after the provider is part of the network.A12461314The information that a health plan can obtain from the National Practitioner Data Bank (NPDB) about a provider primarily relates tomalpractice, licensure, and adverse actions.personal finances and net worth.education, training, and experience.A12471315A provider agrees taccept a health plans compensation as payment in full and not talsbill plan members. What contract provision does this describe?Nbalance billing provision.Cure provision.Hold harmless provision.A12481316A party that breaches a contract is given a certain amount of time tremedy the problem and avoid termination of the contract. What contract provision does this describe?Hold harmless provision.Due process clause.Cure provision.C32491317Can a health plan terminate its contract with a provider when there has been nproblem with the providers performance?Yes, provided it can show that it has good economic reasons for doing so.Yes, if the state permits termination without cause and this is allow by the contract.No, this is prohibited in all states.B22501318A provider already in a health plans network is evaluated by another provider in the same specialty. This describespeer review.recredentialing.verification.A1251141Medical management can be divided into three broad categories, which arecare management, case management, and quality management.utilization management, case management, and disease management.utilization management, clinical practice management, and quality management.C3252142Managing the use of medical services sthat plan members receive necessary and appropriate care in a cost-effective manner isutilization management.quality management.clinical practice management.A1253143A health plan conducts a health risk assessment (HRA) tdetermine a persons likelihood of developing certain illnesses. The purpose is tohelp her reduce her risk and thereby improve outcomes and reduce cost.decide whether taccept or decline her application.set her premium based of the amount of healthcare she is likely tneed.A1254144A health plan program seeks tdetermine if a member has a health condition even if he has nsymptoms. This isa screening program.a wellness program.an immunization program.A1255145A program supports health plan members whwant tstop smoking, lose weigh, eat better, and exercise more. This is awellness program.decision support program.self-care program.A1256146A program teaches health plan members how ttreat minor illnesses and distinguish them from serious conditions. This is ascreening program.wellness program.self-care program.C3257147Colleen can access data about different drugs and healthcare providers on her health plans website. This is an example ofvalue-based healthcare.web-based decision support tools.shared decision making.B2258148Telephone triage programs are typically staffed bynonprofessional personnel with access tprofessionals.nurses directed by physicians and supported by nonprofessional personnel.physicians supported by nonprofessional personnel.B2259149Clarks doctor gives him information about the treatment options available thim, and Clark makes the final decision. This is an example ofa self-care program.shared decision-making.utilization review.B22601410While Gloria is being treated for an illness, her health plan conducts an evaluation of whether the services she is receiving are necessary, appropriate, and cost-effective. This is an example ofdisease management.concurrent utilization review.shared decision-making.B22611411Wilson is assigned a healthcare professional whassesses his needs, designs a plan of care, and coordinates and monitors the services he receives. This describescase management.disease management.utilization review.A12621412Case management is used forhigh-risk and high-cost cases.high-risk cases.high-risk, high-cost, and/or chronic cases.C32631413Case managers are most commonlyphysicians.nurses.social workers.B22641414Which type of UM program focuses on populations instead of individuals?Case management.Self-care.Disease management.C32651415Disease management focuses onacute diseases.geriatric diseases.chronic diseases.C32661416Which statement is true about disease management programs?They encourage doctors ttry a variety of treatments instead of following one standard for all.They focus on individual episodes of medical care.They are typically an outreach and support program for plan members with certain diseases.C32671417A doctor treating a patient with diabetes refers tguidelines for this condition in making decisions about the most appropriate course of action. This describesutilization review.clinical practice guidelines.evidence-based healthcare.B22681418Jill, a pediatrician, is considering prescribing a certain drug for Eric. She asks herself, Is there research that indicates that if Eric takes this drug he will likely get better quickerthan if he did not? Jill isengaging in evidence-based healthcare.conducting case management.referring tclinical practice guidelines.A12691419Laurie has diabetes. She wants tstay well and is willing tchange her lifestyle, but sometimes she doesnt follow instructions about diet because she doesnt understand. The problem here isa lack of motivation.a lack of health literacy.a lack of information.B2270151Utilization reviewis always conducted before treatment is provided.is always conducted after treatment is provided.may be conducted before, during, or after treatment.C3271152Utilization review focuses primarily on whether a healthcare service isthe lowest cost available in the area.delivered by a network or non-network provider.medically necessary and appropriate.C3272153The purpose of utilization review is toensure correct payment of benefits and promote quality and cost-effective care.ensure correct payment of benefits.ensure correct payment of benefits, promote quality and cost-effective care, and collect data for utilization management and other purposes.C3273154UR staff decide what treatmentsa patient must receive.a doctor can provide.a health plan will pay for.C3274155UR programs use clinical practice guidelines toreduce unnecessary and ineffective practice variation.eliminate all practice variation.make information available and encourage practice variation.A1275156If both prospective and retrospective review are possible, which is generally preferable?Retrospective review.Prospective review.Both.B2276157Precertification (prior authorization) is most commonly used forhospital admissions.specialist office visits.routine laboratory tests.A1277158The average number of days a patient with certain characteristics stays in a hospital. This describessite-appropriateness listings.length-of-stay guidelines.experience-based criteria.B2278159When are experience-based criteria usually used?For stays in hospitals and other facilities.In determining the best care setting.When research-based utilization guidelines are not available.C32791510Testing needed before an inpatient treatment should be performedbefore admission tthe hospital.after admission tthe hospital but at least one day before treatment.after admission tthe hospital.A12801511For which is concurrent review not commonly used?A specialist visit.A long hospital stay.A course of chemotherapy.A12811512Prior authorization is a feature ofprospective, concurrent, and retrospective review.prospective review and sometimes concurrent review.prospective review only.B22821513Retrospective review most commonlyanalyzes data timprove utilization.reviews a particular case for appropriateness of services.seeks tdirect treatment and care settings.A12831514Which form of UR is most likely tdiscover billing errors and fraud?Retrospective review.Prospective review.Concurrent review.A12841515In order To receive a larger payment, a doctor improperly and deliberately bills two procedures separately instead of together. This isunbundling.a billing error.upcoding.A12851516Subjecting all healthcare services to UR isdesirable, but not possible.neither possible nor desirable.possible, but not desirable.B22861517For which type of care is a health plan member most likely need a referral or authorization?Primary care.Nonprimary care.Dental and vision care.B22871518Which service is least likely To require authorization?A high cost service.A service with a high authorization denial rate.A frequently performed service.C32881519Emergency department usecan increase or decrease health plan costs.generally decreases health plan costs.generally increases health plan costs.A12891520Is emergency department care subject to utilization review?Some plans require retrospective review and authorization.No, this is prohibited by nearly all states.Some plans require prospective review and precertification.A12901521Do health plans cover urgent care centers?Some do, and some dnot.No,theydnot.Yes, they do.A12911522Bill has chest pains and is awaiting test results. He doesnt need any treatment at this time, but he needs to be monitored. What is probably the best care setting for him?Observation care unit.Subacute care facility.Urgent care center.A12921523Jack has had surgery. He doesnt need full hospital care anymore, but he does need 24-hour nursing care under the supervision of a doctor. What is probably the best care setting for him?A subacute care facility or hospital step-down unit.Home healthcare.An observation care unit.A12931524Health plans generally pay for home health care forthose recovering from an acute injury or illness, but not those with chronic conditions.all those who need it, regardless of the reason.those with chronic physical impairments but not a cognitive disorders.A12941525Do health plans pay for hospice care?Most dfor all those with a terminal illness.Most dfor those whhave six months or less tlive and whforegcertain medical treatment.They generally dnot, but government programs do.B22951526Which UR data transmittal method has the most problems with accuracy?Telephone.Electronic.Manual.C32961527Which UR data transmittal method is the fastest and least labor-intensive?Telephone.Manual.Electronic.C32971528Which UR data transmittal method is the most regulated?Telephone.Electronic.Manual.C32981529In the UR process, administrative review focuses on whether a proposed service iscost-effective.medically appropriate.covered.C32991530In the UR process, administrative review is performed byeither, depending on the plan.nonclinical employees.clinical professionals.A13001531Whcan deny an authorization based on medical necessity and appropriateness?A physician, nurse, or nonclinical employee.A physician or nurse.A physician only.C33011532May UR staff recommend a different treatment for a member?No, they may only approve or deny proposed services.Yes, but only when consensus is reached with the treating physician.Yes, they may direct the treating physician tperform certain treatments.B23021533Which statement is not true?Once a PCP has referred a patient ta specialist, the specialist can generally provide whatever treatment and as many visits as she sees fit.For inpatient hospital care, authorizations generally include services related tthe main procedure approved.An authorization may cover one specialist visit or multiple visits.A1303161The two main components of quality management arequality assessment and quality improvement.quality assessment and quality reassessment.quality planning and quality improvement.A1304162The twmain categories of health plan quality areservice quality and healthcare quality.medical quality and customer satisfaction.physician quality and facility quality.A1305163Carol has a question about her health coverage, but she tries all day and is unable treach her health plan by phone. This is an issue ofhealthcare quality.service quality.provider quality.B2306164Medical errorsare both a patient safety issue and a cost issue.are the responsibility of providers, not health plans.are not common and sare not a major concern.A1307165The wrong medication is prescribed for a patient, causing an adverse event. This is an error ofomission.commission.execution.C3308166Which problem is being addressed by national databases?Lack of communication among healthcare providers.Lack of coordination among parties concerned with medical errors.Lack of verification of individual analysis of test results.B2309167Consumer perceptions of healthcare qualityare important because they reflect valid concerns and affect purchaser decisions.should be considered provided they dnot conflict with objective measures.are not valid or reliable and should not be a factor in health plan decisions.A1310168A health plans network has a certain number of primary care physicians. This isan outcomes measure.a process measure.a structure measure.C3311169The percentage of health plan members whhave received a medical checkup in the past twyears isa process measure.an outcomes measure.a structure measure.A13121610Five years after treatment, 80 percent of cancer patients are still alive. This isan outcomes measure.a structure measure.a process measure.A13131611The trend in quality measures is toward greater use ofprocess measures.outcomes measures.structure measures.B23141612What is the relationship of structure, processes, and outcomes?Structure and processes produce outcomes.Structure produces outcomes, but processes are independent.Processes and outcomes determine structure.A13151613The average claim processing time is aprocess measure of healthcare quality.outcomes measure of service quality.process measure of service quality.C33161614The main disadvantage of structure measures is thattheir link toutcomes is generally not proven by research.they are difficult and expensive tcalculate.they have nrelation toutcomes.A13171615A certain percentage of patients are able treturn twork twyears after a stroke. This is aclinical outcomes measure.clinical process measure.functional outcomes measure.C33181616Which is not a disadvantage of outcomes measures?Comparing different providers is problematic.Outcomes are not directly related tquality.Data can be difficult and costly tobtain.B23191617Which generally presents the most problems?Clinical data.Customer satisfaction data.Financial data.A13201618Which statement about quality improvement is true?After actions are taken timprove quality, measurement and analysis of outcomes is repeated and ongoing.It is not generally necessary or desirable for a health plan tpublicize its quality improvement efforts outside the plan.While accrediting bodies require a health plan thave a quality management program, they dnot require much documentation of it.A13211619A hospital identifies another hospital with high cancer survival rates and adopts its practices. This isprovider profiling.benchmarking.peer review.B23221620A health plan analyzes data from different gynecologists and notices that one of them performs a certain procedure much more often than the rest. This ispeer review.benchmarking.provider profiling.B23231621A panel of pediatricians evaluates the appropriateness and timeliness of the care provided by another pediatrician in a particular case. This is an example ofclinical practice guidelines.provider profiling.peer review.B23241622Which is most likely tbe controversial among providers?Clinical practice guidelines.Benchmarking.Provider profiling.C3325171Which statement is not true about health plans internal standards?They are typically applied thealthcare services.They are usually based on the plans past performance.They are typically applied tadministrative services.A1326172NCQA accreditsHealth plans of various types.PPOs only.HMOs only.A1327173Nationally, NCQA accreditation coversabout half of health plan members.a minority of health plan members.most health plan members.C3328174The NCQA accreditation processconsists of an offsite review of data.includes both an onsite visit and offsite data review.consists of an onsite visit.B2329175What form does NCQA accreditation take?A plan earns one of five accreditation levels.A plan is either accredited or not, with nother evaluation given.A plan is given a numerical score, with nother evaluation given.A1330176URAC accreditshealth plans and health networks.health plans, health networks, and functional areas within organizations.health plans.B2331177The URAC accreditation processconsists of an offsite review of plan policies and procedures.includes both an onsite visit and offsite policy and procedure review.consists of an onsite visit.B2332178HEDIS is designed primarily tbe used by purchasers and consumers tcomparethe quality of different health plans.the extensiveness of different health networks.the cost of different health plans.A1333179Quality Compass isa national database of performance and accreditation information.an onsite evaluation program for hospitals and clinics.a quality awareness program for health plan executives.A13341710The Agency for Healthcare Research and Quality (AHRQ) isa research branch of the Department of Health and Human Services.a division of CMS concerned with quality in Medicare Advantage plans.a research consortium of medical schools and universities.A13351711The Affordable Care Actaddresses healthcare quality only in federal programs.does not address healthcare quality in any major way.includes a variety of healthcare quality improvement provisions.C33361712What will the Affordable Care Act dwith regard tMedicare Advantage plans?It will maintain current payment levels tMA plans overall but give bonuses and higher rebates tplans that meet quality criteria.It will lower payments tMA plans overall but give bonuses and higher rebates tplans that meet quality criteria.It will increase payments tMA plans overall but eliminate bonuses and higher rebates for plans that meet quality criteria.B2337181Theterm marketing mix referstoagents, brokers, and direct marketing.publicity, advertising, and sales.product, price, promotion, and distribution.C3338182A health plans potential customers includeindividuals, including employees and Medicare beneficiaries.employers, associations, employees, Medicare and Medicaid beneficiaries, and other individuals.employers, associations, and government programs.B2339183Which is a market research technique?Positioning.Focus groups.Direct response marketing.B2340184How is marketing in health plans different from marketing in many other industries?Research is not very important.Markets are generally local.There is little regulation.B2341185Will the Affordable Care Act (ACA) affect product development?No, state laws will continue tgovern this area.Yes, but only by requiring a minimal benefit package.Yes, in relation tbenefit packages, cost-sharing, and other matters.C3342186Developing multiple product lines helps a health plan compete amongsmall employers, but it makes marketing more complicated.large employers, and it makes marketing simpler.large employers, but it makes marketing more complicated.C3343187What is the difference between advertising and publicity?Advertising uses the mass media, publicity is personal contact.Advertising focuses on a product, publicity on an organization.Advertising is paid for, publicity is not.C3344188The term promotion mix is commonly used trefer topersonal selling and direct marketing.advertising, publicity, personal selling, and sales promotion.advertising, branding, and publicity.B2345189Which distribution channel is made up of health plan employees?Brokers.Employee benefits consultants.Internal salesforce.C33461810Whare generally compensated by the buyer of a health plan, not by the seller?Brokers.Agents.Employee benefits consultants.C33471811Whare considered trepresent the health plan?Brokers.Employee benefits consultants.Agents.C33481812Whsells the products of only one company?A captive agent.A broker.An independent agent.A13491813Whcommonly works with individuals rather than groups?Employee benefits consultants.Brokers.Agents.C33501814Which direct marketing method is commonly used today?Telemarketing.Door-to-door selling.Direct mail.C33511815Dividing a market into smaller groups of customers is calledpositioning.branding.market segmentation.C33521816Medicare beneficiaries are generally considered part of thegroup market.non-group market.individual market.B23531817A health plan decides tcompete in the small group market instead of the large group market by offering a basic and inexpensive product. This is an example ofpositioning.market segmentation.direct marketing.A13541818Whis not a member of the regular group market?Joanne recently lost her job and her group health plan.Susans employer does not sponsor a group health plan.Daniel is self-employed.A13551819Which is not a common distribution channel in the individual market?Agents.Direct marketing.Brokers.C33561820The Affordable Care Act (ACA) will affect the marketing of all health plans, but it will have the greatest impact on theindividual market.large group market.Medicare market.A13571821Which is not true under the ACA?The individual market will be eliminated, and everyone will have group coverage.Individuals will buy coverage through government-sponsored exchanges.Individuals enrolling in a health plan will nlonger undergmedical underwriting.A13581822Which is not a common distribution method in the senior market?Direct marketing.Door-to-door selling.Meetings.B23591823People eligible for Medicaremay receive health and/or drug coverage through private-sector health plans.dnot need private-sector health plans.may receive drug (but not health) coverage through private-sector health plans.A13601824The group market is made up mostly ofassociations.multi-employer groups.employers.C33611825Small businesses choosing a health plan usually focus strongly onprice.quality.service.A13621826Which is true of small employers?Only one health plan is usually offered.Self-funding is common.Customization of a product is common.A13631827Which is true of large employers?They tend tchoose very basic and inexpensive products.They tend tchange health plans more frequently than small plans.They often use employee benefits consultants.C3364191Underwriting involvesdetermining the premium tcharge for a risk.identifying and assessing risks.managing incoming and outgoing funds.B2365192Which statement best describes adverse selection (antiselection)?Those more likely tneed healthcare are more likely tobtain health coverage.Those less likely tneed healthcare are more likely tobtain health coverage.Those with health coverage are more likely tuse healthcare services.A1366193In health underwriting, what are the most important risk factors for individuals?Health status and occupation, but not usually age or gender.Age1 health status, and sometimes occupation, but not gender.Age and gender, and sometimes health status or occupation.C3367194Which will be prohibited by PPACA?Waiting periods.Preexisting condition exclusions.Minimum participation requirements.B2368195Which will be prohibited by PPACA?Annual and lifetime benefit limits.Annual enrollment periods.Coinsurance.A1369196In renewal underwriting of a group, what are the twmain factors?Group size and participation.Experience and participation.Group size and new members.B2370197In rating, what are the main considerations?Marketability and competitiveness.Risk and expected healthcare costs.Risk and expected costs balanced by marketability and competitiveness.C3371198Setting premiums based on the expected costs of providing benefits tthe community as a whole rather than tany subgroup is calledmanual rating.pooling.community rating.C3372199Community rating is least likely tbe used forlarge groups.small groups.employer groups.A13731910A health plan sets premiums for classes of members based on age, family composition, and geography, but not experience. This is an example ofcommunity rating by class (CRC).standard community rating.adjusted community rating (ACR).C33741911A health plan sets premiums for a group based on the plans average experience with all groups rather than that particular group. This describesmanual rating.experience rating.blended rating.A13751912A health plan uses a groups past experience testimate its expected experience, and if actual experience is different, the plan absorbs the gains or losses. This describesretrospective experience rating.prospective experience rating.pooling.B23761913Which will PPACA dregarding rating as of 2014?Prohibit the use of experience in rating any group.Require pure community rating for all health plans.Limit premium differentials based on risk factors.C33771914An MCOs income statementsummarizes its revenue and expense activity during a specified period.shows its financial status on a specified date.documents its capital and surplus on a specified date.A13781915The major categories of an MCOs balance sheet arecapital and surplus.assets, liabilities, and capital.revenues and expenses.B23791916State insurance regulators are primarily concerned with an H MOsliabilities and reserves.revenues and profit.statutory solvency.C33801917A variance is the difference betweenexpected and actual revenues and expenses.assets and the sum of liabilities and capital.total revenues and total expenses.A13811918An insurance company is financially responsible for paying healthcare benefits tthe employees of High Plateau Company. High Plateaus health plan isa self-funded plan.a fully funded plan.a self-insured plan.B23821919Big River Corporation takes responsibility for paying healthcare benefits tits employees, but if total claims rise above $10 million in a year, an insurer pays any claims above this level. This is an example ofaggregate stop-loss coverage.individual stop-loss coverage.specific stop-loss coverage.A13831920A third-party administrator generallyadministers benefits and is financially responsible for paying claims.administers benefits and is financially responsible for paying claims above a certain level.administers benefits only.C3384201An information management system incorporates membership data and provider reimbursement arrangements and analyzes transactions according tcontract rules. This describes aquality management system.utilization management system.contract management system.C3385202A health plan has an automated system tfacilitate the processing of requests for authorization of payment. What kind of information management system is this?Claim processing.Utilization management.Finances.B2386203An information management system identifies physicians whtend tprovide fewer services than the norm in certain situations. This is an example ofcontract management.provider profiling.credentialing.B2387204The use of an MRI machine is expensive, sa health plan needs tefficiently coordinate utilization by providers. What type of information management system addresses this need?Provider profiling.Utilization management.Enterprise scheduling.C3388205A health plans members can gthe plans website tcheck on the status of their claims. What kind of information management system is this?Member services.Quality management.Utilization management.A1389206Which statement about the quality of health plan data is not true?The information supplied by codes is often not complete.The use of codes largely eliminates problems of accuracy.The entering of codes often results in inaccuracy.B2390207The data used by health plans isoften in different databases but in compatible formats.generally in one database and in the same format.often in different databases and in incompatible formats.C3391208Which aspect of information management in health plans is most strongly addressed by government regulation?Security and privacy.Qualityof data.Usability of data.A1392209In health plans, information management issomewhat automated.almost entirely automated.almost entirely unautomated.A13932010Which term encompasses all types of electronic business functions?E-business.I-business.E-commerce.A13942011Which statement best describes health plans and the Internet?Health plans have historically lagged behind other industries but are now handling many transactions online.Health plans have adopted information technology for internal operations, but few transactions are suitable for being conducted online.Health plans can offer information on their websites, but conducting transactions online is generally not feasible.A13952012A security device designed tblock unauthorized access ta private network isdigital tagging.encryption.a firewall.C33962013A computer network is accessible only the employees of a health plan. This is aninternet.extranet.intranet.C33972014The main threat ta health plans network ismembers.hackers.employees.C33982015How does electronic data interchange (EDI) differ from e-business?It does not require a standardized data format.It is the transfer of batches of data, not exchanges about a transaction.It requires considerable human involvement.B23992016Which generally results in more accurate data, manual processes or EDI?They are about equal in this regard.Manual.EDI.C34002017The focus of business intelligence and decision support systems is tohelp managers make decisions in specific cases.replace physicians in making clinical decisions.give managers a big picture, strategic view of an organization.A14012018The main problem that a data warehouse is designed taddress isinaccuracy of data.data in multiple databases.a very high volume of data.B24022019The main disadvantage of data warehouses isthe complexity and cost of implementing them.their incompatibility with decision support systems.their lack of historical data.A14032020Medical information for an individual designed tbe used at the site of care isan electronic medical record.a decision support system.a data warehouse.A14042021The main advantage of health information networks (HINs) and health information exchange (HIE) isthat providerstreating a patientreceive guidance on the best course of treatment for her.have access tall of her medical records and health information.can find out what services are and are not covered by her health plan.B24052022How does an HIE (such as a RHIO) differ from an HIN?An HIN includes only physician information, while an HIE includes data from other sources.An HIN shares information within a health plan network, while an HIE shares it across healthcare entities.An HIN is available only tproviders, while an HIE is accessible by the general public.B24062023Which is owned by the individual?The personal health record (PHR).The electronic health record (EHR).The electronic medical record (EMR).A14072024Personal health records are available fromthe federal government.health plans and other organizations.physicians.B24082025How does the electronic medical record differ from the personal health record?The EHR is not subject tprivacy and security regulations.c The EHR adds information from providers.The PHR is usually in paper format.B24092026An example of an insourcing-outsourcing hybrid isa data warehouse.cloud computing.an intranet.B2410211In traditional indemnity health insurance, which is most common?Claims are submitted by the provider.Claims are submitted by the insured.Encounter reports but not claims are submitted by the provider.A1411212when is an encounter report submitted instead of a claim?When the provider is compensated by capitation or salary.When the provider is not in a plans network.When the provider is compensated by fee-for-service.A1412213health plan claims processing is similar tthat of traditional insurance forhospitals but not healthcare professionals.healthcare professionals but not hospitals.hospitals and most (but not all) healthcare professionals.C3413214About what portion of a typical health plans claims are processed electronically?30 t40 percent.80 t90 percent.50 t60 percent.B2414215Which statement is true about electronic claims processing?It is promoted by federal legislation.It can handle only simple claims.It can handle only claims submitted electronically.A1415216A health plan employee whdeals with claims that have been paid incorrectly is a claimsexaminer.adjustor.reviewer.B2416217A claims examiners responsibilities generally includeconverting paper documents intelectronic files.explaining claim decisions tmembers and providers.reviewing and adjudicating claims not processed electronically.C3417218Under which type of provider compensation arrangement is the most claims information needed?Capitation.Salary.Discounted fee-for-service.C3418219Which standardized claim form is used by physicians?CMS-1500.UB-04.CPTA14192110What is the standard code set for diagnoses?ICD.CPT.HCPCS.A14202111A claim triggers an edit. Usually, the claim will beexamined furthered.automatically paid.automatically denied.A14212112In which situation is it not uncommon for a health plan tmake a partial payment on a claim?Authorization was not obtained.The service is not considered medically necessary.The service is not covered under the members benefit package.A14222113Which statement is true about claims processing?If a required authorization was not obtained but the service was medically necessary, the health plan is obligated tpay.If a provider bills more than six months after delivering a service, a plan is not required tpay.A health plan has nmedical malpractice liability for actions by its providers.B24232114Coordination of benefits may apply whena required authorization or referral was not obtained.a person is treated by more than one provider.a person is covered by more than one health plan.C34242115Most claim investigationsare complicated and time-consuming.involve suspected fraud.are short and simple.C34252116The primary focus of the NAIC Unfair Claims Settlement Practices Act ispromoting the electronic transmission and processing of claims.protecting the privacy of members health information.ensuring that insurers handle claims fairly and promptly.C3426221Health plans member education focuses ongeneral health information, including wellness and prevention.either administrative matters or health or both.administrative matters such as benefits, cost-sharing, and authorization.B2427222Health plans member education is directed tomembers with certain characteristics.both.all members.B2428223Which means of distributing information thealth plan members is declining?Websites,Letters and newsletters sent by mail.Email.B2429224Jeff calls his health plans toll-free number and is able, by following prompts and without talking ta person, tchange his PCP. This is an example ofIVR.CTI (ACD or IVR).ACD.A1430225In health plan member services, when are paper documents sent by mail?Usually only when required by regulations for important notifications.For a variety of notifications and routine transactions.Tanswer routine questions and requests.B2431226Which statement about health plan communication with members is true?Email is not generally used because of the strict regulatory requirements.Members can not only obtain information from websites but alssometimes perform transactions.Email has almost entirely replaced regular mailB2432227Why must a health plan adequately deal with complaints?Tcomply with regulations only-since only a tiny minority of members complain, they dnot have a significant impact on overall satisfaction.Tmaintain member satisfaction and avoid bad publicity-there are nregulatory requirements.Tcomply with regulations, maintain member satisfaction, avoid bad publicity, and reduce appeals.C3433228A health plans complaint resolution procedures (CRPs)are generally up tthe plan and not subject tregulation or accreditation requirements.are generally subject tstate and federal regulation and accreditation requirements.are subject taccreditation requirements but not usually regulation.B2434229Who generally conducts a health plans level twappeal of a member complaint?The appeals committee.The medical director.An outside third party.A14352210What happens if a health plan member does not win a level twappeal?Her case is automatically referred tarbitration.She has nfurther recourse and must accept the decision.She may have the right tappeal ta government agency or an external review organization.C34362211What are the twmain ways of measuring member satisfaction with a health plan?Member satisfaction surveys and performance measures.Member satisfaction surveys and complaint monitoring.Performance measures and complaint monitoring.B24372212What populations dhealth plan member satisfaction surveys target?Members whhave recently received services and all members.Members whhave recently received services.Members whhave recently received services, all members, and former members.C34382213Who conducts member satisfaction surveysPlan employees or outside companies.Plan employees or outside companies, but some accrediting bodies and purchasers require outside companies.Outside companies only, as required by regulation and accrediting bodies.B24392214Which statement about the structure of health plan member services is true?It is very uncommon for a single member services representative thandle many types of needs through different communication channels.In large, complex health plans, several departments rather than a single department handle member services.Among plan types, small PPOs are least likely thave a dedicated member services department.C34402215Which is likely tdecrease the number of employees needed for adequate member services staffing?Representatives with broad responsibilities.The use of CTl.A complex benefit structure.B24412216Which statement about member service representatives is true?They are subject thigh stress and burn-out, sretention is a concern.Their initial training typically takes only a few days, but frequent ongoing training is needed.Their training is almost always on the job and rarely involves formal instruction.A14422217Which statement about member services technology is not true?IVR systems and websites can only provide information, not handle transactions.With new technologies, somewhat complex matters can be handled online.CTI systems can provide information for performance management.A14432218The amount of time required tcomplete a transaction requested by a member isturn-around time.first contact resolution rate.wait time.A14442219Which is a measure of both quality and cost-effectiveness?First contact resolution rate.Call abandonment rate.Error rate.A14452220Which is considered a measure of cost-effectiveness rather than quality?Error rate.Call abandonment rate.Average time per contact.C3446231The medical laboratories in a community get together and decide how much they will all charge health plans for various tests. This is probably a case ofbid-rigging.a horizontal allocation.price-fixing.C3447232A physician group refuses to provide certain specialty services to a heafth plan unless the plan agrees to contract with the group for all the services the group offers. This may be a case ofa horizontal group boycott.horizontal allocation.a tying arrangement.C3448233Which is an important provision of the Financial Services Modernization Act?The protection of personal financial information.The break-up of large health insurance companies.The establishment of standards for provider networks.A1449234ERISA applies tono health plans (only retirement plans).employer- and union-sponsored health plans.all health plans.B2450235Under ERISA, what are the roles of the federal and state governments in regulating employer-sponsored health plans?Self-funded plans are regulated only by the federal government, and fully insured plans are regulated only by the state.An employer health plan is regulated by the federal government, but any insurer involved is regulated by the state.An employer health plan is regulated by the federal government, and any insurer involved is also regulated by the federal government.B2451236Under ERISA, an individual challenging a coverage decision by an employer-sponsored health planmust sue in state court and may receive punitive damages.must sue in federal court and may not receive punitive damages.may sue in federal court, giving them the opportunity to obtain punitive damages.B2452237If an employee is laid off, under COBRA she has the right to continue her employer-sponsored health coveragefor up to three months.indefinitely, until she has access to coverage from a new employer.for up to 18 months.C3453238Bill is covered under his wife Lones employer-sponsored health plan. What rights does Bill have under COBRA to continue this coverage?He has no rights.He has rights if Lones employment is terminated.He has rights if Lones employment is terminated, she dies, or they are divorced.C3454239Noah has been laid off and is continuing his employer health coverage under COBRA. Who pays?Noah and his employer each continue paying the portion they paid when he was employed.Noah pays the full cost of coverage, and the employer may charge him a certain amount for administrative costs.Noah pays the full cost of coverage, but the employer pays all administrative costs.B24552310What is the impact of the HMO Act of 1973?HMOs that wish to be federally qualified must meet the standards, and almost all HMOs do.HMOs that wish to be federally qualified must meet the standards, and while qualification is less important today, many HMOs are qualified.All HMOs must meet the standards of the Act.B24562311Under ADEA, an employer sponsoring health coveragemay not decline to offer health coverage to older employees nor change them more.may decline to offer heafth coverage to older employees.may not decline to offer health coverage to older employees but may charge them more.A14572312Under FMLA, an employee who is ill or needs to care for a family member has the right to l2 weeksofpaid leave, including health coverage.unpaid leave, including health coverage.unpaid leave, not including health coverage.B24582313Which is not one of the main goals of HIPAA?Increasing the availability and continuity of healthcare.Expanding Medicaid eligibility.Protecting healthcare information.B24592314HIPAA applies tothe individual market only.the individual and group markets.the group market only.B24602315Under HIPAA, guaranteed individual issue of health insurance generally applies to persons whohave certain specified chronic health conditions.have lost group coverage and are not currently eligible for it.have been without coverage for at least one year.B24612316Which is not a provision of HIPAA for group health plans?They must provide mental health coverage.They may not discriminate based on individuals health status.They must have guaranteed renewability.A14622317HIPAAs administrative simplification standards apply tohealthcare providers only.health plans, healthcare providers, and healthcare clearinghouses.health plans only.B24632318Which is not true under HIPAA privacy and security standards?Health plans may not use healthcare information for their own treatment, payment, or operations without obtaining the individuals consent.Patients are allowed to access their medical records.Patients are allowed to request that restrictions be placed on the accessibility and use of protected health information.A1464241Which of these is a component of healthcare reform?The expansion of Medicare eligibility tpeople as young as 55.The requirement that all large employers sponsor a health insurance plan.The requirement that most people have health coverage or pay a tax penalty.C3465242When will the new healthcare financing system become operational?Most of the major components become operational in 2011, but some provisions ginteffect later.Most of the major components become operational in 2014, but some provisions ginteffect later.Most of the majo