Pure Sensory Stroke Caused by a Small Cortical Infarct in ...€¦ · infarct in the middle...
Transcript of Pure Sensory Stroke Caused by a Small Cortical Infarct in ...€¦ · infarct in the middle...

660 STROKE VOL 15, No 4, JULY-AUGUST 1984
tors. Geriatrics 23: 135-141, 196825. Kuller L, Reisler DM: An explanation for variation in distribution
of stroke and artenosclerotic heart diseases among population and 29racial groups. Am J Epidemiol 93: 1-9, 1971
26. Kieffer SA, Amplatz K, Takeya Y: Stroke USA and Japan. Angio-graphic study Geriatrics 24: 100-110, 1969
27. Kameyama M, Yamanouchi H: Study of the causes of cerebral 30.infarction by site. Jpn J Geriatrics — Nippon Ronen Igakkai Zasshi14: 375, 1977 31.
28. Kato H: Epidemiological survey of cerebral apoplexy — Compari-
son of Japanese and Japanese-Americans. Modern Medicine —Saishm Igaku 32: 2229-2234, 1977Mitsuyama Y, Thompson LR, Hayashi T, Lee KK, Keehn RJ,Resch JA, Steer A: Autopsy study of cerebrovascular disease inJapanese man who lived in Hiroshima, Japan and Honolulu, Ha-waii. Stroke 10: 389-395, 1979Hatano S: Epidemiological study of cerebral apoplexy. Jpn J IntMed — Naika Vol 22: 1204-1211, 1968Takeshita M: Vascular diseases of the brain and prevention. Jpn JClin Exp Med — Rinsho to Kenkyu 51: 981-988, 1974
Pure Sensory Stroke Caused by a Small CorticalInfarct in the Middle Cerebral Artery Territory
CHRISTIAN DEROUESNE, M.D., JEAN-LOUIS MAS, M.D., FRANCIS BOLGERT, M.D.,
AND PAUL CASTAIGNE, M.D.
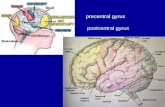
SUMMARY A patient with the sudden onset of a pure sensory deficit involving cortical modalities in hisleft hand and foot is described. CT scan suggested the lesion responsible for the deficit was a small corticalinfarct in the middle cerebral artery territory, involving the middle part of the post-central gyrus andinterrupting thalamo-cortical pathways in the corona radiata.
Stroke Vol 15. No 4. 1984IN 1965, Fisher1 coined the term "pure sensorystroke" (PSS) for the sudden onset of a unilateral iso-lated sensory deficit involving the face, arm and leg.He attributed this syndrome to a lacunar infarct in theventroposterior nucleus (VPN) of the thalamus. Morerecently, examples of this clinical syndrome caused bythalamic hemorrhage and by infarct or hemorrhage inthe corona radiata have been documented.2-3 Pure sen-sory transient ischemic attacks associated with occlu-sive vascular disease of the internal carotid, middlecerebral or posterior cerebral arteries are well known,4
but a PSS caused by a cortical infarct has not yet beenreported. We have had the opportunity to observe aPSS involving the left hand and foot, which proved onCT scan to be caused by a small cortical infarct in theterritory of the right middle cerebral artery.
Report of a CaseA 50-year-old, white, right-handed man, with no
history of systemic hypertension, had undergone a bi-lateral sympathectomy for peripheral occlusive diseasetwo years before admission to the Hopital de la Salpe-triere. Two days prior to admission (PTA) he suddenlydeveloped numbness in his left thumb, index and mid-dle fingers: they felt as if they had "gone to sleep" orwere frozen. He could move his fingers normally butdropped small objects held in his left hand. One dayPTA, on awakening, he experienced numbness in thedistal part of his left foot and clumsiness while putting
From the Clinique des Maladies du Systeme Nerveux. Hopital de laSalpetriere. Paris. France.
Address correspondence to: Professor Christian Derouesnd. Hopitalde la Salpetriere. 47 Bd de IHopital. 75651 Paris CEDEX 13. France.
Received September 30. 1983. revision #1 accepted January 9.1984.
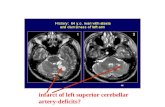
his slipper on his foot. On the day of admission, ex-amination revealed that his muscular strength wasgood and deep tendon reflexes were normal and equal;plantar responses were flexor. Pinprick, light touch,heat and cold, vibration were appreciated perfectly.However, fine movements of the left fingers and toeswere inaccurately perceived, and stereognosis, graph-estesia and two-point discrimination were severelyimpaired. Visual fields were full to confrontation.Copying and drawing were normal. His blood pressurewas 150/100 mm Hg, equal in both arms. The righttibial pulse was not palpable. No neck bruit was heard.Clinical examination of the heart and ECG showed noabnormalities. These data were consistent with a diag-nosis of PSS and, because the patient had no history ofhypertensive disease, treatment with calcium heparin-ate (5000 U I x 3/day) was initiated without delay. CTscan (fig. I A) performed on the 17th day after theonset of the condition, revealed a discrete cortico-sub-cortical hypodense area in the middle of the right pari-etal region, enhanced with contrast, and consistentwith a recent infarct in the superficial middle cerebralartery territory. The thalamic regions were normal.Echo-tomography of the cervical arteries revealed anatheromatous stenosis of the initial segment of the rightinternal carotid artery. This was confirmed by cerebralangiography which also demonstrated a severe (morethan 75%) stenosis of the intracranial segment of theinternal carotid artery and a moderate stenosis of theorigin of the right vertebral artery. Short-latency soma-tosensory evoked potentials (EPS) produced by stimu-lation of the median and tibial nerves, were performed30 and 56 days after the clinical onset. The latencies ofthe thalamocortical components: N 19 P 22 (recordedfrom a scalp electrode over the parietal sensory cortex
by guest on Novem
ber 4, 2016http://stroke.ahajournals.org/
Dow
nloaded from

PURE SENSORY STROKE/Derouej/i<< et al
F.GURE I. CT scans performed after contrast injection 17 days {A) and 2 months (B) after the clinical onset
contralateral to the stimulated limbs) were equal onboth sides but their amplitude was significantly re-duced when stimulating the left median or tibial nerves(fig. 2). Symptoms disappeared in three weeks. Thepatient was discharged with advice to take long termaspirin therapy (1 g/day). Two months later, on fol-low-up examination, the sensory deficit persisted un-changed. CT scan showed a hypodense area in the pa-rietal region without contrast enhancement (fig. I, B).
DiscussionIn a patient with PSS, a recent cortico-subcortical
infarct in the territory of the middle cerebral artery wasdemonstrated by CT scan. The infarct was presumablycaused by embolization from an atheromatous andstenotic internal carotid artery. The CT scan abnor-malities were consistent with an infarct of the samedate as the clinical symptoms. A simultaneous thalam-ic infarct cannot be totally ruled out by the normalappearance of the thalamic region on CT scan,4 nor bythe normal latencies of the short-latency somatosen-sory EPS.5 This hypothesis, however, is very unlikely.
The sensory deficit in the hand was of a corticaltype,6 ie: distal with a "pseudoradicular" distributionand characterized by exclusive loss of joint positionsense, stereognosis, graphesthesia and two-points dis-crimination. The CT scan data are consistent with aninfarct involving the middle part of the post-centralgyrus which, according to Penfield, is the site of sen-sory projections from the opposite hand. This area isvascularized by the anterior parietal artery,7 a branch
either of the central artery (as cerebral angiographyshowed in the case reported here), or of the trunk ofthe middle cerebral artery, or rarely of the posteriorparietal artery. The superior and inferior parts of thepost central gyrus have a different blood supply.8 Ac-cordingly, the limited sensory deficit in the hand canbe explained by embolization to the anterior parietalartery.
The involvement of the foot is more difficult toexplain. The most plausible explanation would be thatthe same cortical infarct also interrupted the corre-sponding sensory pathways between the thalamus andparacentral lobule in the corona radiata. These fibersappear to be supplied by cortical perforating arteries.
This hypothesis is congruent with isolated reportsthat an infarct in the anterior parietal artery territorywas found responsible for contralateral hemianesthe-sia.'' " Somatotopic identification of lhalamocorticalpathways has remained obscure2 but the data presentedhere indicates that the sensory fibers corresponding tothe distal part of the foot might be located more lateral-ly than the fibers corresponding to the rest of the leg.Lastly, the normal latencies and decreased amplitudeof the thalamocortical (N 19 — P 22) EPS componentsare consistent with a pure cortico-subcortical lesion.5
In a recent survey of PSS, Fisher4 reaffirmed hisearlier belief in the predominance of thalamic lesionswhen there is a contralateral sensory deficit, involvingthe face, arm and leg. He also stated that, when onlyone or two parts of the side are involved, the localisa-tion of the lesion might be questionable. However,
by guest on Novem
ber 4, 2016http://stroke.ahajournals.org/
Dow
nloaded from

662 STROKE VOL 15, No 4, JULY-AUGUST 1984
20,20
3t,80
FIGURE 2. Short-latency somatosensory evoked potentialsperformed 30 days after the clinical onset. Upper: stimulationof the right median nerve; amplitude of the NJ9-P22 compo-nents = 4,40 V. Lower: stimulation of the left median nerve;amplitude of the N19-P22 components = 1,25 V. Quite similarresults were observed on the 56th day.
discrete infarcts of the VPN of the thalamus have beendocumented with sensory deficits individually involv-ing the face and hand; the mastoid region, arm andleg;4 the face; the arm; the leg; the oral cavity; theperibuccal area and forearm; and the peribuccal areaand radial edge of forearm.'2 On the other hand, senso-ry deficits involving face, arm and leg ("pseudo-tha-lamic") have been described in partial middle cerebralartery territory infarcts.9 l0 It is, therefore, not possibleto locate the lesion from the physical findings alone.
Fisher believed that the lesion responsible for PSSwas a lacunar infarct, usually due to lipohyalinoticocclusion related directly to hypertensive disease.11
However, in one pathological case,2 the lesion consist-ed of a small hemorrhage found in the posterior limbsof the internal capsule. Of three other cases1 of PSS,one was related by CT scan to a thalamic hemorrhage;a second, to a lacunar infarct located in the thalamo-
cortical projection area; and a third to a small thalamicinfarct associated with occlusive disease of the posteri-or cerebral artery.
In the case here, PSS was due to a small infarct inthe cortical territory of the middle cerebral arterycaused, presumably, by embolization from an athero-matous stenosis of the internal carotid artery. There-fore it seems that PSS might not be a specific manifes-tation of a lacunar lesion in the thalamus. In this way itis comparable to the syndrome of pure motor hemiple-gia which cannot be reported as a manifestation only ofcapular lesions infarction.14 Assessment of patient,with the syndrome of PSS should be the same as forany other minor stroke, and should include CT scan,doppler, ECG and ancillary investigations to verify thetopographical and etiological diagnosis.
References
8
1. Fisher CM: Pure sensory stroke involving face, arm and leg. Neu-rology 15: 76-80, 1965
2. Groothuis DR, Duncan GW, Fisher CM: The human thalamocorti-cal sensory path in the internal capsule: evidence from a smallcapsular hemorrhage causing a pure sensory stroke. Ann Neural 2:328-331. 1977
3. Rosenberg NL. Koller R. Computerized tomography and pure sen-sory stroke Neurology 31: 217-220, 1981
4. Fisher CM: Pure sensory stroke and allied conditions Stroke 13:434-437. 1982
5. Chiappa KH. Ropper AH: Evoked potentials in clinical medicine(second of two parts). N Eng J Med 306: 1205-1210, 1982
6. Dejerine J: Sdmeiologie des affections du systeme nerveux Mas-son. Paris 1914
7. Damasio H: A computed tomographic guide to the identification ofcerebral vascular territories. Arch Neural 40: 138-142, 1983Salamon G, Huang YP: Radiologic anatomy of the brain. SpringerVerlag; Berlin, 1976
9 Foix C, Chavany JA, Levy M: Syndrome pseudo-thalamiqued'ori-gine pari&ale. Lesion de I'artere du sillon interparidtal (Pa PI P2antgrieures. petit territoire insulo-capsulaire). Rev Neural (Paris)35: 68-76. 1927
10. Waddington MM. Ring BA: Syndromes of occlusions of middlecerebral artery branches. Angiographic and clinical correlation.Brain 91: 685-696. 1968
11. Lhermitte F, Daisi M. Signoret JL, Deloche G: Aphasic kinesthisi-que associee a un syndrome pseudo-thalamique. Rev Neurol (Par-is) 136: 675-688, 1980Lapresle J, Haguenau M: Anatomico-clinical correlation in focalthalamic lesions. Z. Neurol 205: 29-46, 1973Fisher CM: Thalamic pure sensory stroke: a pathologic study.Neurology 28: 1141-1144. 1978Rascol A. Clanet M. Manelfe C. Guiraud B. Bonafe A: Pure motorhemiplegia: CT study of 30 cases. Stroke 13: 11-17, 1982
12
13
14
by guest on Novem
ber 4, 2016http://stroke.ahajournals.org/
Dow
nloaded from

C Derouesné, J L Mas, F Bolgert and P CastaignePure sensory stroke caused by a small cortical infarct in the middle cerebral artery territory.
Print ISSN: 0039-2499. Online ISSN: 1524-4628 Copyright © 1984 American Heart Association, Inc. All rights reserved.
is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231Stroke doi: 10.1161/01.STR.15.4.660
1984;15:660-662Stroke.
http://stroke.ahajournals.org/content/15/4/660World Wide Web at:
The online version of this article, along with updated information and services, is located on the
http://stroke.ahajournals.org//subscriptions/
is online at: Stroke Information about subscribing to Subscriptions:
http://www.lww.com/reprints Information about reprints can be found online at: Reprints:
document. Permissions and Rights Question and Answer available in the
Permissions in the middle column of the Web page under Services. Further information about this process isOnce the online version of the published article for which permission is being requested is located, click Request
can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.Stroke Requests for permissions to reproduce figures, tables, or portions of articles originally published inPermissions:
by guest on Novem
ber 4, 2016http://stroke.ahajournals.org/
Dow
nloaded from