Pulmonary Drug Delivery Originated as a More Relevant Alternative for Delivering Drugs to the Lungs
-
Upload
rajesh-akki -
Category
Documents
-
view
214 -
download
0
description
Transcript of Pulmonary Drug Delivery Originated as a More Relevant Alternative for Delivering Drugs to the Lungs
1. Pulmonary drug delivery originated as a more relevant alternative for delivering drugs to the lungs. Respiratory conditionssuch as asthma, chronic obstructive pulmonary(COPD) and emphysema are therapeutic areas of the pulmonary space.2. Recent technological advancements have Pulmonary Drug Delivery Systems: Technologies and Global Markets MarketWatchapplied the application of pulmonary devices to thetreatment of nonrespiratory conditions also such as diabetes and migraines.3. The recent trends and research in theformulating sector have grown tremendously and increased sales of dry powder inhalers (DPIs), and slowly replacedmetereddoseinhalers (MDIs). 4. Pulmonary delivery of drugs for the treatment of respiratory diseases gives a faster,simpler and easier therapeutic effect compared to systemic treatments for these indications. In addition, it also reducesside effects associated with many drugs. Lungs are an attractive target for the pulmonary administration of active pharmaceutical ingredients(APIs) in the form of various drug delivery systems [13]. Additionally, this route offers manyadvantages over conventional per oral administration, such as a high surface area with rapid absorption1. due to high vascularization and circumvention of the first pass effect [2].
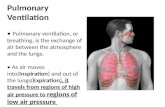
2. Anatomy and Physiology of the Lungs2.1. Anatomy of the LungsLungs are responsible for the gas exchange and supply of oxygen to all the cells. The lungs consistof a total of five lobes, the right lung consisting of three and the left lung of two lobes. The interior ofthe lungs is comprised of bronchi and smaller air passages, alveoli, blood vessels and lymph tissue.The bronchi are further divided into primary and secondary bronchi and bronchioles and, finally, thealveoli. Lungs have over 300 million alveoli. Furthermore, each alveolus is lined with pulmonarycapillaries, thus forming a vast network comprising over 280 billion capillaries, giving rise to a vastsurface area of almost 70 m2 available as the blood-gas barrier. The alveolar gas exchange majorlyoccurs at the interface consisting of alveolar epithelium, endothelium and interstitial cell layers. Thealveolar wall is made up of two types of alveolar epithelial cells, namely (pneumonocytes) Type I andType II. Between the capillaries and the alveolar epithelium, there exists a single endothelial layer. Thedistance between the alveoli and capillaries is so small, about 0.5 m, that owing to this extremethinness of the blood-gas interface, gas exchange is facilitated by diffusion at the interface. The alveoliare coated with a layer of alveolar fluids and mucus, which is majorly composed of phospholipids andsurface proteins. This phospholipid surfactant layer at the alveoli reduces the surface tension and isessential for the proper functioning of the gas exchange. These distal respiratory passages aresupported by a thin layer of connective tissue. This layer is surrounded with different cells, likemacrophages, fibroblasts, nerves, as well as lymph vessels. This serves as an ideal location for theadministration of drugs with access to the pulmonary, as well as the lymphatic system [14,15].
2.2. Deposition of the ParticlesThe deposition of particles in the different regions of the lungs depends on the particle size of theformulation. Based on the particle size, three different mechanisms of drug deposition are defined,namely impaction, sedimentation and diffusion [16]. In impaction, the aerosol particles pass throughthe oropharynx and upper respiratory passages at a high velocity. Due to the centrifugal force, theparticles collide with the respiratory wall and are deposited in the oropharynx regions. This mechanismis generally observed for dry powder inhalation (DPI) and metered dose inhalators (MDI), withparticles sizes greater than 5 m. In case of the DPI, the inspiratory effort of the patient plays animportant role in the deposition. If the force of inhalation is insufficient, the dry powder deposits in theupper airways, owing to the mass of the particles and the inertial forces. For the MDI and despitethe high speed of the generated aerosol, high particle sizes also tend to lead to the deposition of theparticles mostly in the upper respiratory tract region. Gravitational forces are predominantlyresponsible for the sedimentation of particles. Particles with sufficient mass and sizes between one to5 m are deposited in the smaller airways and bronchioles, where they are deposited slowly, provideda sufficiently long time span. Therefore, sedimentation is also influenced by the breathing pattern.Slow breathing provides a sufficient time span for sedimentation. Apart from impaction andsedimentation, Brownian motion plays a major role in the deeper alveolar areas of the lungs. TheBrownian motion of the surrounding molecules of the aqueous lung surfactant causes a randommovement of the particles. Upon contact with the lung surfactant, the dissolution of API in alveolarInt. J. Mol. Sci. 2014, 15 5855fluid is essential for diffusion. Additionally, the concentration gradient also influences the diffusionprocess. Particles smaller than one to 0.5 m are deposited in the alveolar region, while most of theparticles, owing to smaller sizes, are exhaled [17]. For nanoparticulate systems, sedimentation is themost attractive method of particle deposition. Nanoparticulate systems, after being released from anaerosol, form aggregates in the micrometer size range. These aggregates are believed to have asufficient mass to sediment and stay in the bronchiolar region for a longer time, hence achieving thedesired effect. Apart from the mechanisms, parameters, such as the particle size of the aerosol, particlemorphology and geometry, along with surface properties, play an important role in depositionphenomena. Furthermore, breathing frequency and the holding of breaths, humidity, air velocity andtidal volume also are vital factors influencing the deposition [17].