Pulmonary Disfunction in Chronic Liver Disease
-
Upload
adel-hamada -
Category
Documents
-
view
216 -
download
0
Transcript of Pulmonary Disfunction in Chronic Liver Disease

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 1/7
C inica C a enge
Pulmonary Dysfunction in Chronic Liver Disease
MICHAEL B. FALLON AND GARY A. ABRAMS
Pulmonary abnormalities and symptoms are common inpatients with chronic liver disease. If questioned, up to 70% of cirrhotic patients undergoing evaluation for liver transplanta-tion complain of dyspnea.1 In screening studies of patientswith chronic liver disease, arterial blood gas abnormalities arefound in as many as 45% and abnormal pulmonary functiontests in as many as 50%.2 A variety of causes for pulmonarydysfunction in liver disease have been identified and includeintrinsic cardiopulmonary disorders not specifically related toliver disease as well as unique problems associated with thepresence of liver disease and/or portal hypertension (Table 1).The recognition that a subset of patients with hepatic disease
develop significant pulmonary vascular alterations, either mi-crovascular dilation leading to the hepatopulmonary syn-drome (HPS) or arteriolar vasoconstriction leading to porto-pulmonary hypertension, indicates that unique changes in thepulmonary vasculature may occur in liver disease. These pul-monary vascular syndromes significantly impact morbidityand mortality in affected patients and influence candidacy forliver transplantation. This review will focus on the most com-mon abnormality in the pulmonary vasculature in liver dis-ease: HPS. It will address the differential diagnosis, clinicalfeatures, diagnostic evaluation, therapy, and pathogenesis of this increasingly well-recognized syndrome.
HEPATOPULMONARY SYNDROME
HPS is caused by intrapulmonary microvascular dilationthat occurs in a subgroup of patients with liver disease and/orportal hypertension. It is defined by the presence of hepaticdysfunction or portal hypertension, a widened age-correctedalveolar-arterial oxygen gradient on room air with or withouthypoxemia and intrapulmonary vasodilation.3,4 Although theassociation between pulmonary dysfunction and liver diseasehas been recognized for more than 100 years,5 the term “hepa-topulmonary syndrome” was not used until 19776 as the con-cept that intrapulmonary vasodilation caused the gas ex-change abnormalities in these patients emerged. At present,studies have shown that as many as 40% of cirrhotic patientshave detectable intrapulmonary vasodilation7 and that up to8% to 15% will develop impaired oxygenation, which resultsin significant functional limitations.3 Early definitions empha-
sized that the exclusion of intrinsic cardiopulmonary diseaseor hepatic hydrothorax were required to make the diagnosis ofHPS.4 However, it is now clear that HPS may occur in thesetting of other cardiopulmonary abnormalities8,9 and con-tribute significantly to gas exchange abnormalities in thesepatients.
CLINICAL SIGNIFICANCE OF HPS
The importance of detecting HPS in patients with liver dis-ease and/or portal hypertension derives from a number ofclinical observations in patients who have both hepatic andpulmonary dysfunction. First, what is known about the natu-ral history of HPS suggests that most patients develop progres-sive intrapulmonary vasodilation and worsening gas ex-change over time10 and that spontaneous improvement israre.11 Mortality is significant in this group10 and may be duein part to causes related to intrapulmonary vasodilation. Inaddition, many patients with moderate to severe HPS havecomparatively well-preserved hepatic synthetic function(Child’s-Pugh class A or B7). Consequently, it is likely thatover time HPS will significantly alter the quality of life andsurvival in affected patients. Second, liver transplantation hasemerged as an effective therapy for HPS and over 80% ofpatients transplanted to date have had resolution or markedimprovement in intrapulmonary vasodilation.12 However,
significant postoperative morbidity and mortality occurs inthese patients12 and may be anticipated and more effectivelymanaged if the diagnosis is made before transplantation. Inaddition, moderate to severe portopulmonary hypertension,in contrast to HPS, significantly increases liver transplant–related mortality and is considered a contraindication.13
Thus, distinguishing these two entities is extremely impor-tant, especially if liver transplantation is being contemplated.Finally, the recognition that HPS may coexist with intrinsiccardiopulmonary disease8 emphasizes the need to be able todefine the relative contribution of intrapulmonary vasodila-tion to gas exchange abnormalities in these patients. Specifi-cally, transplant candidacy or the use of experimental thera-pies for HPS may be influenced by this information.
CLINICAL FEATURES
HPS is usually diagnosed in patients with concomitant cir-rhosis and portal hypertension. However, no specific etiologyof cirrhosis has been found to increase the risk of developingHPS, and it has been observed in noncirrhotic portal hyper-tension as well.14 The majority of noncirrhotic patients havesome degree of liver injury that may include nodular regener-ative hyperplasia, congenital hepatic fibrosis, or Budd-Chiarisyndrome.15 These findings suggest that both liver injury andportal hypertension contribute to the development of in-trapulmonary vasodilation in most cases. A single case of HPShas been noted in a patient with metastatic carcinoid, normal
Abbreviations: HPS, hepatopulmonary syndrome; CT, computerized tomography;
TIPS, transjugular intrahepatic portosystemic shunt.
From the Liver Center, University of Alabama at Birmingham, Birmingham, AL.
Received February 9, 2000; accepted March 14, 2000.
Address reprint requests to: Michael B. Fallon, M.D., Associate Professor, Liver Cen-
ter, University of Alabama at Birmingham, Chief, Gastroenterology and Hepatology,
Birmingham VeteransAdministration Medical Center, 410LHRB, 701South 19thStreet,
Birmingham, AL 35294-0007. E-mail: [email protected]; fax: 205-975-9393.
Copyright © 2000 by the American Association for the Study of Liver Diseases.
0270-9139/00/3204-0027$3.00/0
doi:10.1053/jhep.2000.7519
859

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 2/7
liver function, and no evidence of portal hypertension.16 Thisobservation raises the possibility that vasoactive substances,possibly released from the tumor, may have triggered in-trapulmonary vasodilation in the absence of liver disease orportal hypertension.
Most patients with HPS complain of the insidious onset of dyspnea. Classically, an increase in dyspnea when standing(platypnea), caused by the predominance of vasodilation inthe lung bases in HPS, has been described. However, no stud-ies have assessed the frequency or usefulness of this observa-tion in the diagnosis of HPS. In addition, poor physical con-ditioning, smoking, ascites, and/or intrinsic lung disease areoften present in cirrhosis and may also cause dyspnea. There-fore, the diagnosis of HPS is often delayed and identified aftersevere arterial hypoxemia has ensued. In preliminary work,we have found that 72% of 112 cirrhotic patients undergoingevaluation for liver transplantation complained of dyspneawhen specifically questioned.1 Most of these patients had nor-
mal arterial oxygenation and did not have HPS. However, inpatients found to have HPS, dyspnea was present in over 95%.These findings suggest that dyspnea is a reasonably sensitivebut poorly specific indicator of the presence of HPS. Using anindex that quantifies dyspnea may improve the diagnosticusefulness of this common symptom in identifying patientswith HPS.1
Spider angiomata, digital clubbing, and cyanosis are clinicalfeatures commonly described in patients with HPS. However,these features have not been prospectively investigated as in-dicators of the presence of HPS. In our unpublished observa-tions, spider angiomata were noted in 11 of 15 patients withHPS compared with 42 of 112 cirrhotic patients without HPS,
providing a sensitivity and specificity of 73% and 63%, respec-tively. Clubbing was observed in 7 of 15 patients with HPScompared with only 2 of 112 cirrhotic patients without HPS,providing a sensitivity and specificity 47% and 98%, respec-tively. Cyanosis was observed in 5 of 15 HPS patients and innone of 112 cirrhotic patients without HPS, providing a sen-sitivity of 33% and a specificity of 100%. These findings sug-gest that the presence of spider angiomata is not a usefulclinical marker for HPS, although clubbing and cyanosis,when present in cirrhosis, appear to be specific.
DIAGNOSTIC EVALUATION
The diagnosis of HPS rests on documenting the presence of arterial deoxygenation and intrapulmonary vasodilation. In
patients in whom symptoms (dyspnea) or clinical findings(clubbing, cyanosis) raise the possibility of HPS, further diag-nostic evaluation is warranted to assess gas exchange andintrapulmonary vasodilation.
Pulmonary Gas Exchange Abnormalities. Arterial hypoxemia isarbitrarily defined when an arterial blood gas reveals an arte-rial pO2 of less than 70 mm Hg. However, diagnostic criteriafor HPS frequently include a widened alveolar-arterial oxygengradient (Ͼ20 mm Hg) alone as sufficient to indicate the
presence of gas exchange abnormalities.4 Although such adefinition maximizes the potential for detecting “early” HPS,it is important to recognize that the alveolar-arterial oxygengradient normally widens with age. In our cohort of 207 con-secutive liver transplant candidates who underwent arterialblood gas screening, 66% had alveolar-arterial oxygen gradi-ents greater than 15 mm Hg (unpublished observations).However, after correcting for age [normalϭ 10ϩ 0.43(age Ϫ20)], alveolar-arterial oxygen gradients remained abnormal inonly 35%. Therefore, a significant overestimation of HPS maybe reported if age is not taken into consideration when eval-uating the alveolar-arterial oxygen gradient. In addition, ob-taining arterial blood gases in the standing position may en-
hance the detection of arterial deoxygenation in HPS, becausevasodilation is often maximal in the lower lung fields andstanding will increase intrapulmonary shunting throughthese regions. Studies of 100% oxygen shunt are also oftenused in patients with documented or suspected HPS. In thistest, an arterial blood gas is performed with the patient breath-ing 100% oxygen. Accurate results require the use of a noseclip and a mouth piece to inspire the oxygen. Breathing 100%oxygen helps to distinguish “functional” shunting character-ized by microvascular dilation in gas exchange regions and anormal increase in the pO2 on 100% oxygen from “anatomic”shunting characterized by dilation outside of gas exchangeregions and a significantly diminished increase in the pO2 on
100% oxygen. Both functional and anatomic shunting may beseen in HPS. However, 100% oxygen shunt study results arereported as positive only if anatomical shunting is observed.Therefore, a “normal” 100% oxygen shunt study may be seenin HPS.
Pulse oximetry is a noninvasive modality that indirectlymeasures oxygen saturation and provides a screening test forhypoxemia. From a practical standpoint, it could provide arapid and inexpensive screen for HPS in patients with symp-toms or clinical findings. However, no prospective studiesusing pulse oximetry to detect hypoxemia in cirrhosis havebeen published. In preliminary studies, we have comparedpulse oximetry with oxyhemoglobin saturation levels deter-mined by arterial blood gases in 207 liver transplantation can-didates.17 We found that pulse oximetry significantly overes-timated the arterial oxyhemoglobin saturation, an effect notinfluenced by serum bilirubin levels. Using a pulse oximetrylevel of Յ97% provided a sensitivity of 96% and a specificity of76% for detecting mild hypoxemia (pO2 Ͻ70 mm Hg) andwould have limited the need for arterial blood gas testing to32% of the cohort. It would have missed one hypoxemic pa-tient (pO2 ϭ 69 mm Hg). Using a pulse oximetry value ofՅ94% would have identified all patients with moderate tosevere hypoxemia (pO2Ͻ60 mm Hg) and would have limitedarterial blood gas testing to only 9% of the total cohort. Ofnote, 8 of 13 patients with mild hypoxemia (pO2ϭ 60-69 mmHg) would have been missed using an oximetry value of 94%.
TABLE 1. Causes of Pulmonary Abnormalities in Chronic Liver Disease
Intrinsic cardiopulmonary disease
Chronic obstructive pulmonary disease
Congestive heart failure
Pneumonia
Asthma
Specific to liver disease
Associated with specific liver diseases
Panacinar emphysema: alpha-1 antitrypsin deficiency
Fibrosing alveolitits, pulmonary granulomas: primary biliary cirrhosis
Fluid retention complicating portal hypertension
Ascites
Hepatic hydrothorax
Pulmonary Vascular abnormalities
Hepatopulmonary syndrome
Portopulmonary hypertension
860 FALLON AND ABRAMS HEPATOLOGY October 2000

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 3/7
These findings indicate that pulse oximetry may be a usefulscreening test for hypoxemia and HPS in cirrhosis, but revealthat the threshold value for obtaining an arterial blood gas ishigher than typically expected.
Intrapulmonary Vasodilation. Contrast echocardiography,lung perfusion scanning, and pulmonary angiography are thediagnostic modalities that have been used to detect intrapul-monary vasodilation. Two-dimensional transthoracic con-trast echocardiography is the most commonly used technique.
Typically, agitated saline, which creates microbubbles visibleon echocardiography, is used as a contrast agent. A positivetest for intrapulmonary vasodilation occurs when delayed vi-sualization of intravenously administered microbubbles areobserved in the left heart (3rd heartbeat after injection18-20).Immediate visualization of injected contrast in the left heartindicates intracardiac shunting. Transthoracic echocardiogra-phy is more sensitive than lung perfusion scanning in detect-ing intrapulmonary vasodilation.7 Transesophageal contrastechocardiography may increase the sensitivity of detectingintrapulmonary vasodilation compared with transthoracicechocardiography21 because it improves visualization of theheart and may identify early HPS that is missed by transtho-
racic echocardiography.22 However, no study has proven it tobe advantageous compared with transthoracic echocardiogra-phy in detecting intrapulmonary vasodilation in hypoxemicpatients with HPS. Transesophageal echocardiography is alsoinvasive and more expensive than transthoracic echocardiog-raphy and is not generally used as the initial screening test forHPS. Contrast echocardiography, using either technique, ispositive in up to 40% of cirrhotic patients with normal arterialblood gases,7 suggesting that mild intrapulmonary vasodi-lation insufficient to alter gas exchange and cause HPS iscommon in cirrhosis. The natural history of pulmonary vaso-dilation in these patients is unknown. Thus, a positive trans-thoracic echocardiography or transesophageal echocardiogra-
phy in a hypoxemic patient with a concomitant pulmonarydisorder (pleural effusion, chronic obstructive pulmonarydisease) is insufficient to establish the diagnosis of HPS, be-cause either intrapulmonary vasodilation or the underlyingpulmonary process could be responsible for gas exchange ab-normalities.
Radionuclide lung perfusion scanning, using technetium-labeled macroaggregated albumin particles, is also commonlyused to detect intrapulmonary shunting.23,24 A significant ad-vantage of the radionuclide lung perfusion scan over contrastechocardiography is that a positive lung scan is specific for thepresence of HPS even in the setting of coexistent intrinsic lungdisease.9 Additionally, it can be used to quantify intrapulmo-nary shunting and is useful for following the progressionand/or resolution of disease prospectively. However, radionu-clide lung perfusion scanning is less sensitive than contrastechocardiography in detecting intrapulmonary vasodilation,and cannot evaluate cardiac function, intracardiac shuntingor assess pulmonary artery pressure. Therefore, the radionu-clide lung perfusion scan is not an optimal screening test forHPS.
Pulmonary angiography is an invasive and insensitive diag-nostic modality for detecting intrapulmonary vasodilation inHPS25 and is not useful as a screening test. Two types of angiographic findings have been reported: type 1—a diffuse“spongy form” appearance of pulmonary vessels during thearterial phase and type 2—small discrete arteriovenous com-
munications. However, many patients have normal angio-grams in the setting of clinically significant HPS. Angiographymay have a therapeutic role in therareHPS patient with a poorresponse to 100% oxygen (arbitrarily defined as a pO 2 Ͻ150mm Hg) and anatomic shunting due to type 2 lesions that maybe amenable to embolization.26
A recent study has shown that high-resolution chest com-puterized tomography (CT) may be a less invasive radiologicmethod to detect dilated pulmonary vessels in the lung inHPS.27 The degree of dilation observed on CT correlated with
the severity of gas exchange abnormalities in these patientswith HPS, suggesting that quantitation of intrapulmonary va-sodilation was possible. Further studies are warranted to de-fine if chest CT will be useful in assessing the presence andseverity of HPS.
DIAGNOSTIC ALGORITHM FOR PULMONARY
DYSFUNCTION IN CIRRHOSIS
Figure 1 presents one approach to evaluating pulmonaryabnormalities in liver disease. Patients with dyspnea are tar-geted for screening because virtually all patients in our studieswith hypoxemia complain of this symptom. Pulse oximetry,with a cutoff value of 97%, is used to screen for hypoxemia to
detect patients with a pO2 less than 70 mm Hg. If the pulseoximetry is greater than 97%, an arterial blood gas is notobtained. A chest radiograph is ordered to exclude pleuraleffusions or cardiopulmonary disease as a cause for dyspnea.If the chest radiograph is normal, we assess if poor condition-ing, smoking, ascites, or obesity may account for the symp-toms. Patients are treated where possible and followed to de-fine if changes in pulse oximetry or progressive dyspneaoccur. Patients with progressive symptoms undergo contrastechocardiography to assess cardiac function, evaluate for in-trapulmonary shunting, and estimate pulmonary artery sys-tolic pressures and consider the possibility of portopulmonaryhypertension. Portopulmonary hypertension is found in ap-proximately 2% to 5% of patients with cirrhosis and is defined
FIG. 1. Evaluation of pulmonary dysfunction in cirrhosis. ABG, arterialblood gas; CE, contrast echocardiography; (ϩ) CE, positive intrapulmonaryshunting, (Ϫ) CE, no evidence for intrapulmonary shunting; CXR, chestx-ray; HPS, hepatopulmonary syndrome; HTN, hypertension; MAA, macro-aggregated albumin radionuclide lung perfusion scan;nl, normal; abn, abnor-mal; PFTs, pulmonary function tests.
HEPATOLOGY Vol. 32, No. 4, 2000 FALLON AND ABRAMS 861

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 4/7
by the presence of a mean pulmonary artery pressure greaterthan 25 mm Hg and a normal pulmonary capillary wedgepressure.13 Estimated pulmonary artery systolic pressuresgreater than 50 mm Hg on echocardiography warrant rightheart catheterization. If contrast echocardiography is positivefor delayed intrapulmonary shunting or pulse oximetry de-clines, an arterial blood gas is obtained to determine if HPS ispresent.
If the pulse oximetry is Յ97% an arterial blood gas is ob-tained. If gas exchange abnormalities are detected (widenedalveolar-arterial oxygen gradient or hypoxemia), then con-trast echocardiography and pulmonary function tests are per-formed. In HPS, the chest radiograph is typically normal, butincreased interstitial markings caused by vascular distentionmay be found and mistaken for interstitial fibrosis. In patientswhere contrast echocardiography shows intrapulmonaryshunting and chest radiograph and pulmonary function tests
are normal, the diagnosis of HPS is confirmed. If contrastechocardiography is positive but the chest radiograph or pul-monary function tests show a significant abnormality, thenthe diagnosis of HPS is uncertain because intrinsic cardiopul-monary disease rather than HPS could be responsible for hy-poxemia. In this situation, we perform a radionuclide lungperfusion scan, which, if abnormal, indicates that HPS is con-tributing significantly to the decreased pO2. If contrast echo-cardiography is normal, then other causes for gas exchangeabnormalities are evaluated.
TREATMENT
No clearly effective medical therapy for HPS has been found
(Table 2). Somatostatin, amiltrine, indomethacin, L-NAME,and plasma exchange have all been tried unsuccessfully.15
Aspirin increased arterial oxygenation in 2 children withHPS28 and a case report29 and subsequent open-label trial30
using garlic also suggested a beneficial effect. In the later trial,garlic powder was administered for a minimum of 6 months,and 6 of 15 HPS patients had improvements greater than 10mm Hg in the pO2 and 1 subject had resolution of hypoxemia(pO2: 46 mm Hg to 80 mm Hg) over a 1.5-year period. Arandomized, placebo-controlled trial will be necessary to con-firm these preliminary findings.
Three case reports have suggested that transjugular intra-hepatic portosystemic shunt (TIPS) may improve gas ex-change in HPS. However, short duration of follow-up in one31
and the presence of coexistent hepatic hydrothorax, alsotreated with TIPS in another,32 limit evaluation of the use ofTIPS in these cases. A third report clearly showed an increasein arterial oxygenation of 20 mm Hg 6 months after TIPSplacement.33 However, significant intrapulmonary shuntingpersisted based on radionuclide lung perfusion scanning andthe cardiac output increased after TIPS. These findings sug-gest that improved oxygenation was not caused by reversal ofintrapulmonary vasodilatation but was more likely caused bya redistribution of pulmonary blood flow to normal ventila-tion to perfusion ratio regions induced by an increase in car-diac output. This observation raises the possibility that TIPSmay be detrimental in patients who cannot further increasecardiac output after stent placement. In addition, there is areported observation that TIPS did not improve oxygenationin one patient with HPS and that HPS developed in two pa-tients with functioning TIPS.34 Taken together, these findings
support that TIPS should be considered an experimental treat-ment for HPS and its use confined to the setting of clinicaltrials so that efficacy may be judged.
Liver transplantation is the only proven therapy for HPSbased on the total resolution or significant improvement ingas exchange postoperatively in more than 85% of reportedpatients.12 However, the length of time for arterial hypoxemiato normalize after transplantation varies and may be morethan 1 year.35 In addition, mortality is increased after trans-plantation in HPS patients compared with subjects withoutHPS,12 and unique postoperative complications includingpulmonary hypertension,36 cerebral embolic hemorrhages,37
and immediate postoperative deoxygenation requiring pro-
longed mechanical ventilation38
have been reported. Innova-tive approaches such as frequent body positioning39 orinhaled nitric oxide40,41 have been used to improve postoper-ative gas exchange. Further research focused on the perioper-ative medical management of HPS patients is needed to opti-mize survival.
PATHOGENESIS
The pathogenesis of intrapulmonary vasodilation in HPS isan area of active investigation. Studies in humans have impli-cated enhanced pulmonary production of nitric oxide in thedevelopment of vasodilation by assessing exhaled nitric oxideproduction.42-44 However, what triggers the increase in pul-monary nitric oxide, how it relates to the presence of portal
TABLE 2. Medical Therapies for HPS
Year Medication Patients Outcome Reference
1977 Phenylephrine/isoproterrnol. 2 No improvement 24
1987 Almitrine 5 1/5 Better 58
1990 Plasma exchange 6 No improvement 59
1991 PGF/indomethacin 1 Mild improvement 60
1992 Garlic 1 Improvement 29
1992 Cyclophosp./pred. 1 Improved after 1 yr 61
1992 Somatostatin analogue 3 No improvement 62
1993 Almitrine 6 Minimal change PO2 631993 Indomethacin 6 No improvement 64
1993 Somatostatin analogue 7 No improvement 10
1994 Somatostatin analogue 2 No improvement 65
1994 Methylene blue 1 Improved 66
1994 L-NAME 1 No improvement 67
1996 Aspirin 3 Improved 28
1998 Garlic 15 6/15 pO2 increaseϾ10 mm Hg 30
862 FALLON AND ABRAMS HEPATOLOGY October 2000

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 5/7
hypertension, the hyperdynamic circulation and the degree of liver injury, and why only 8% to 15% of cirrhotic patients areaffected remain undefined. Reports of HPS in patients withprehepatic portal hypertension14 and in the presence of infer-ior vena cava obstruction without cirrhosis45 suggest that thepresence of severe hepatic dysfunction is not a prerequisite forthe development of intrapulmonary vasodilation. In addition,although most patients reported with HPS have a picture con-sistent with portal hypertension and a hyperdynamic circula-tory state, reports that HPS has developed after portal decom-pression34 and the recognition that only a subset of all patientswith cirrhosis and a hyperdynamic circulation develop HPS,suggest that other factors contribute to the onset of intrapul-monary vasodilation.
The development of an animal model of HPS (common bileduct ligation in the rat46) has provided a system to investigatethe mechanisms of intrapulmonary vasodilation. Early studiessuggested that altered pulmonary eicosanoid production andan influx of intravascular macrophages triggered pulmonaryvascular alterations.47,48 However, more recent work hasshown that the endothelial form of nitric oxide synthase isincreased in the pulmonary microcirculation and contributesto enhanced nitric oxide activity and vasodilation in affectedanimals.49,50 Changes in lung endothelial nitric oxide syn-thase and intrapulmonary vasodilation were found only incommon bile duct ligated animals and not in animals withprehepatic portal hypertension alone, suggesting that a com-bination of liver injury and portal hypertension contribute to
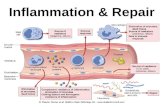
FIG 2. Endothelin-1 effects inthe normal and HPS pulmonary mi-crovasculature. In the normal vascu-lature, endothelin-1 (ET-1), pro-duced locally in endothelial cells,acts as a paracrine vasoconstrictorthrough activation of the endothelin
A (ETA) receptor on smooth musclecells. To a lesser extent, luminal re-lease of ET-1 stimulates nitric oxide(NO) production by endothelial ni-tric oxide synthase (eNOS) throughactivation of the endothelin B (ETB)receptor on endothelial cells. InHPS, ET-1 reaches the lung throughthe pulmonary circulation and actsas an endocrine vasodilator by stim-ulating theETB receptor on thelumi-nal surface of the endothelial celland preferentially increasing NOproduction.
HEPATOLOGY Vol. 32, No. 4, 2000 FALLON AND ABRAMS 863

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 6/7
the pathogenesis of pulmonary vascular changes in thissystem.
Subsequent studies focused on determining how hepaticinjury contributes to intrapulmonary vasodilation, revealedthat an unexpected potential mediator of HPS, endothelin-1(classically known as a vasoconstrictor), is overproduced inthe common bile duct ligated liver and found in the systemiccirculation.51,52 Endothelin-1 production occurred in part inbiliary epithelium in these animals, and plasma levels corre-
lated with the increase in pulmonary endothelial nitric oxidelevels and intrapulmonary vasodilation.51 Further work hasshown that endothelin-1 can directly stimulate endothelialnitric oxide production in cultured pulmonary vascular endo-thelial cells and when infused chronically at low levels intoanimals with isolated portal hypertension can trigger pulmo-nary endothelial nitric oxide production, intrapulmonary va-sodilation, and gas exchange abnormalities indicative of HPS.53 These studies support the hypothesis that certainforms of hepatic injury may trigger the production and releaseof hepatic endothelin-1, which contributes to the onset of intrapulmonary vasodilation.
Whether the observations in common bile duct–ligated an-
imals are also found in human HPS and whether other factors,in addition to endothelin-1, contribute to vasodilation in thissystem are undefined. However, biliary endothelin-1 produc-tion54 and increased plasma endothelin-1 levels have beendescribed in human cirrhosis.55,56 Figure 2 provides a work-ing model of the potential effects of endothelin-1 in the pul-monary microcirculation after common bile duct ligation.Under normal conditions, endothelin-1 is a paracrine vaso-constrictor that regulates vascular tone.57 In this situation,endothelin-1 is released from vascular endothelial cells, pre-dominately in an abluminal direction, where it targets theendothelin A receptor on vascular smooth muscle cells andinitiates vasoconstriction. To a lesser degree, endothelin-1released into the lumen targets the endothelin B receptor on
endothelial cells and triggers nitric oxide production, whichcounterbalances vasoconstrictive effects. After common bileduct ligation, endothelin-1 reaches the pulmonary circulationfrom the liver and may preferentially interact with the endo-thelin B receptor on the luminal surface of the pulmonaryvascular endothelium. In this setting, endothelin-1 may act asan endocrine vasodilator triggering enhanced endothelial ni-tric oxide production and intrapulmonary vasodilation.
CONCLUSION
HPS has become a well recognized complication of liverdisease and portal hypertension over the last 15 years. Al-though symptoms and clinical features of HPS are non-
specific, a diagnostic algorithm for detecting gas exchangeabnormalities and intrapulmonary vasodilation is proposed.Because a widened alveolar-arterial oxygen gradient on arte-rial blood gas testing, in the setting of intrapulmonary vaso-dilation, is sufficient to make the diagnosis of HPS, it is im-portant to correct the alveolar-arterial oxygen gradient for ageto avoid unwarranted evaluation for HPS. Distinguishing por-topulmonary hypertension from HPS and defining the contri-bution of HPS to gas exchange abnormalities in patients whoalso have intrinsic lung disease has become critical as livertransplantation has emerged as a successful treatment for thesyndrome. Medical therapies for HPS are suboptimal, but mayimprove as the pathogenetic mechanisms of intrapulmonaryvasodilation are elucidated. Use of TIPS for HPS remains ex-
perimental. Liver transplantation reverses HPS in more than80% of patients, but unique postoperative complications mayoccur and should be anticipated when transplantation is un-dertaken.
REFERENCES
1. Sood G, Fallon MB, Niwas S, Tutton T, van Leeuwen DJ, Bloomer JR,McGuire BM, et al. Utility of a dyspnea-fatigue index for screening livertransplant candidates for hepatopulmonary syndrome [Abstract]. HEPA-
TOLOGY 1998;28(Suppl):742A.2. Hourani J, BellamyP, Tashkin D, Simmons M. Pulmonary dysfunction in
advanced liver disease: frequent occurrence of an abnormal diffusionCapacity. Am J Med 1991;90:693-700.
3. Lange PA, Stoller JK. The hepatopulmonary syndrome. Ann Int Med1995;122:521-529.
4. Rodriguez-Roison R, Agusti A, Roca J. The hepatopulmonary syndrome:new name, old complexities. Thorax 1992;47:897-902.
5. Fluckiger M. Vorkommen von trommelschagel formigen fingerendpha-langen ohne chronische veranderungen an der lungen oder am herzen.
Wien Med Wochenschr 1884;34:1457.6. Kennedy TC, Knudson RJ. Exercise aggregated hypoxemia and orthode-
oxia in cirrhosis. Chest 1977;72:305.7. Abrams GA, Jaffe CC,Hoffer PB, Binder HJ, FallonMB. Diagnostic utility
of contrast echocardiography and lung perfusion scan in patients withhepatopulmonary syndrome. Gastroenterology 1995;109:1283-1288.
8. Martinez G, Barbera J, Navasa M, Roca J, Visa J, Rodriguez-Roisin R.Hepatopulmonary syndrome associated with cardiorespiratory disease.
J Hepatol 1999;30:882-889.9. Abrams G, Nanda N, Dubovsky E, Krowka M, Fallon M. Use of macro-
aggregated albumin lung perfusion scan to diagnose hepatopulmonarysyndrome: a new approach. Gastroenterology 1998;114:305-310.
10. Krowka MJ, Dickson ER, Cortese DA. Hepatopulmonary syndrome.Clinical observations and lack of therapeutic response to somatostatinanalogue. Chest 1993;104:515-521.
11. Saunders KB, Fernando SSD, Dalton HR, Joseph A. Spontaneous im-provement in a patient with the hepatopulmonary syndrome assessed byserial exercise tests. Thorax 1994;49:725-727.
12. Lange PA, Stoller JK. The hepatopulmonary syndrome: effect of livertransplantation. Clin Chest Med 1996;17:115-123.
13. Mandell M, Groves B. Pulmonary hypertension in chronic liver disease.Clin Chest Med 1996;17:17-33.
14. DimandRJ, HeymanMB, Bass NM,Lavine JE,Lake JR,Roberts JP,AscherNL. Hepatopulmonary syndrome: response to hepatic transplantation[Abstract]. HEPATOLOGY 1991;141(Suppl):55A.
15. Abrams G, Fallon M. The hepatopulmonary syndrome. Clin Liver Dis1997;1:185-200.
16. Lee D, Lepler L. Severe intrapulmonary shunting associated with meta-static carcinoid. Chest 1999;115:1203-1207.
17. Abrams GA, Fallon MB, Nail C, McGuire BM, van Leeuwen DJ, EckhoffDE, Bynon SJ, et al. Pulse oximetry: utility in detecting arterial hypox-emia in subjects with cirrhosis [Abstract]. HEPATOLOGY 1999;30(Suppl):435A.
18. Hopkins WE, Waggoner BA, Barzilai B. Frequency and significance ofintrapulmonary right-to-left shunting in end-stage hepatic disease. Am JCardiol 1992;70:516-519.
19. Krowka MJ, Tajik AJ, Dickson ER, Wiesner RH, Cortese DA. Intrapul-monary vascular dilatations (IPVD) in liver transplant candidates.
Screening by two-dimensional contrast-enhanced echocardiography.Chest 1990;97:1165-1170.
20. Park S, Beerman L, Gartner C, Zitelli BJ, Malatack J, Fricker FJ, FischerDR, et al. Echocardiographic Findings Before and After Liver Transplan-tation. Am J Card 1985;55:1373-1378.
21. Vedrinne JM,Duperret S, Bizollon T, MagninC, Motin J, Trepo C, DucerfC. Comparison of transesophageal and transthoracic contrast echocardi-ography for detection of an intrapulmonary shunt in liver disease. Chest1997;111:1236-1240.
22. Aller R, Moya JL, Moreira V, Boixeda D, Cano A, Picher J, Garcia-Rull S,et al. Diagnosis of hepatopulmonary syndrome with contrast transesoph-ageal echocardiography: advantages over contrast transthoracic echocar-diography. Dig Dis Sci 1999;44:1243-1248.
23. Genovesi MG, Tierney DF, Taplin GV, Eisenberg H. An intravenousradionuclidemethod to evaluate hypoxemia caused by abnormal alveolarvessels. Am Rev Resp Dis 1976;114:59-65.
864 FALLON AND ABRAMS HEPATOLOGY October 2000

7/28/2019 Pulmonary Disfunction in Chronic Liver Disease
http://slidepdf.com/reader/full/pulmonary-disfunction-in-chronic-liver-disease 7/7
24. Wolfe JD, Tashkin DP, Holly FE, Brachman MB, Genovesi MG. Hypox-emia of cirrhosis: detection of abnormal small pulmonary vascular chan-nels by a quantitative radionuclide method. Am J Med 1977;63:746-754.
25. MacNee W, Buist T, Finlayson N, Lamb D, Miller HC, Muir AL, DouglasAC. Multiple microscopic pulmonary arteriovenous connections in thelungs presenting as cyanosis. Thorax 1985;40:316-318.
26. Poterucha JJ, Krowka MJ, Dickson ER, Cortese DA, Stanson AW, KromRAF. Failure of hepatopulmonary syndrome to resolve after liver trans-plantation and successful treatment with embolotherapy. HEPATOLOGY
1995;21:96-100.27. Lee KN, Lee HJ, Shin WW, Webb WR. Hypoxemia and liver cirrhosis
(hepatopulmonary syndrome) in eight patients: comparison of thecentral and peripheral pulmonary vasculature. Radiology 1999;211:549-553.
28. Song JY, Choi JY, Ko JT, Bae EJ, Kim HS, Noh CI, Yoon YS. Long-termaspirin therapy for hepatopulmonary syndrome. Pediatrics 1996;97(6 Pt1):917-920.
29. Caldwell SH, Jeffers LJ, Narula OS, Lang EA, Reddy KR, Schiff ER. An-cient remedies revisited: does Allium sativum (garlic) palliate the hepa-topulmonary syndrome? J Clin Gastroenterol 1992;15:248-250.
30. Abrams GA, Fallon MB. Treatment of hepatopulmonary syndrome withallium sativum L. (garlic): a pilot trial. J Clin Gastro 1998;27:232-235.
31. Reigler JL, Lang KA, Johnson SP, Westerman JH. Transjugular intrahe-patic portosystemic shunt improves oxygenation in hepatopulmonarysyndrome. Gastroenterology 1995;109:978-983.
32. Selim KM, Akriviadis EA, Zuckerman E, Chen D, Reynolds TB. Trans- jugular intrahepatic portosystemic shunt: a successful treatment forhepatopulmonary syndrome. Am J Gastroenterol 1998;93:455-458.
33. Allgaier HP, Haag K, Ochs A, Hauenstein KH, Jeserich M, Krause T,Heilmann C, et al. Hepatopulmonary syndrome: successful treatment bytransjugular intrahepatic portosystemic stent-shunt (TIPS). J Hepatol1995;23:102-105.
34. Corley DA, Scharschmidt B, Bass N, Sonnenberg K, Gold W. Lack of efficacy of TIPS for hepatopulmonary syndrome. Gastroenterology 1997;113:728-731.
35. Philit F, Wiesendanger T, Gille D, Boillot O, Cordier J. Late resolution of hepatopulmonary syndrome after liver transplantation. Respiration1997;64:173-175.
36. Mandell MS, Groves BM, Duke J. Progressive plexogenic pulmonary hy-pertension following liver transplantation. Transplantation 1995;59:1488-1490.
37. Abrams GA, Rose K, Fallon MB, McGuire BM, Bloomer JR, van LeeuwanDJ, Tutton T, et al. Hepatopulmonary syndrome and venous embolicausing intracerebral hemorrhages after liver transplantation: a case re-
port. Transplantation 1999;68:1-3.38. Scott V, Mira A, Kang Y, DeWolf A, Bellary S, Martin M, Kramer D, et al.
Reversibility of the hepatopulmonary syndrome by orthotopic livertransplantation. Transplant Proc 1993;25:1787-1788.
39. Meyers C, Low L, Kaufman L, Druger G, Wong LL. Trendelenburg posi-tioning and continuous lateral rotation improve oxygenation in hepato-pulmonary syndrome after liver transplantation. Liver Transpl Surg1998;6:510-512.
40. Alexander J, Greenough A, Baker A, Rela M, Heaton N, Potter D. Nitricoxide treatment of severe hypoxemia after liver transplantation in hepa-topulmonary syndrome. Liver Transpl Surg 1997;3:54-55.
41. Durand P, Baujard C, GrosseAL. Reversal of hypoxemia by inhaled nitricoxide in children with severehepatopulmonary syndrome,type 1, duringand after liver transplantation. Transplantation 1998;65:437-439.
42. Cremona G, Higenbottam TW, Mayoral V, Alexander G, DemoncheauxE, Borland C, Roe P, et al. Elevated exhaled nitric oxide in patients withhepatopulmonary syndrome. Eur Respir J 1995;8:1883-1885.
43. Rolla G, Brussino L, Colagrande P, Dutto L, Polizzi S, Scappaticci E,Bergerone S, et al. Exhaled nitric oxide andoxygenation abnormalities inhepatic cirrhosis. HEPATOLOGY 1997;26:842-847.
44. Rolla G, Brussino L, Colagrande P. Exhaled nitric oxide and impairedoxygenation in cirrhotic patients before and after liver transplantation.Ann Intern Med 1998;129:375-378.
45. Binay KD, Sen S, Biswas PK, Sanyal R, Majumbar D, Biswas J. Hepato-pulmonary syndrome in inferior vena cava obstruction responding tocavoplasty. Gastroenterology 2000;118:192-196.
46. Chang S-W, O’Hara N. Pulmonary circulatory dysfunction in rats withbiliary cirrhosis. Am Rev Respir Dis 1992;148:798-805.
47. Chang SW, Ohara N. Increased pulmonary vascular permeability in ratswith biliary cirrhosis: role of thomboxane A2. Am J Physiol 1992;264:L245-L252.
48. Chang SW, Ohara N. Chronic biliary obstruction induces pulmonaryintravascular phagocytosisand endotoxinsensitivity in rats. J Clin Invest1994;94:2009-2019.
49. Fallon MB, Abrams GA, McGrath JW, Hou Z, Luo B. Common bile ductligation in the rat: a model of intrapulmonary vasodilatation and thehepatopulmonary syndrome. Am J Physiol 1997;272:G779-G784.
50. Fallon MB, Abrams GA, Luo B, Hou Z, Dai J, Ku DD. The role of endo-thelial nitric oxide synthase in the pathogenesis of a rat model of hepa-topulmonary syndrome. Gastroenterology 1997;113:606-614.
51. Luo B, Abrams G, Fallon M. Endothelin-1 in the bile duct ligation modelof hepatopulmonary syndrome: correlation with pulmonary dysfunc-tion. J Hepatol 1998;28:571-578.
52. Rockey D, Fouassier L, Chung J, Carayon A, Vallee P, Rey C, Housset C.Cellular localization of endothelin-1 and increased production in liverinjury in the rat: potential for autocrine and paracrine effects on stellatecells. Hepatology 1998;27:472-480.
53. Zhang M, Luo B, Chen S, Abrams G, Fallon M. Endothelin-1 stimulationof endothelial nitric oxide synthase in the pathogenesis of hepatopulmo-nary syndrome. Am J Physiol 1999;277 (Gastrointest Liver Physiol 40):G944-G952.
54. Pinzani M, Milani S, DeFranco R, Grappone C, Caligiuri A, Gentilini A,
Tosti-Guerra C, et al. Endothelin 1 is overexpressed in human cirrhoticliver and exerts multiple effects on activated hepatic stellate cells. Gas-troenterology 1996;110:534-548.
55. Asbert M, Gines A, Gines P, Jimenez W, Claria J, Salo J, Arroyo V, et al.Circulating Levels of Endothelin in Cirrhosis. Gastroenterology 1993;104:1485-1491.
56. Moore K, Wendon J, Frazer M, Krani J, Williams R, Badr K. Plasmaendothelin immunoreactivity in liver disease and the hepatorenal syn-drome. N Engl J Med 1992;327:1774-1777.
57. Filep JG. Endothelin peptides: biological actions and pathophysiologicalsignificance in the lung. Life Sci 1992;52:119-133.
58. KrowkaMJ, Cortese DA.SevereHypoxemia associated with liver disease:Mayo Clinic experience and the experimental use of almitrine bismesy-late. Mayo Clin Proc 1987;62:164-173.
59. Krowka MJ, Cortese DA. Hepatopulmonary syndrome: an evolving per-spective in theera of liver transplantation. HEPATOLOGY 1990;11:138-141.
60. Shijo H, Sasaki H, Yuh K, Okumura M. Effects of indomethacin onhepatogenic pulmonary angiodysplasia. Chest 1991;99:1027-1029.
61. Cadranel J, Milleron B, Cadranel J-R, Fermand J-P, Andriuet P, Brouet J-C, Adnot S, et al. Severe hypoxemia associated intrapulmonary shunt ina patient with chronic liver disease: improvement after medical treat-ment. Am Rev Respir Dis 1992;146:526-527.
62. Schwartz SM, Pound DC. Hepatopulmonary syndrome: failure of re-sponse to somatostatin analogue [Abstract]. Gastroenterology 1992;102(Suppl):882A.
63. Nakos G, EvrenoglouD, Vassilakis N, Lampropoulos S. Haemodynamicsand gas exchange in liver cirrhosis: the effect of orally administeredalmitrine bismesylate. Respir Med 1993;87:93-98.
64. Andrivet P, Cadranel J, Housset B, Herigault R, Harf A, Adnot S. Mecha-nisms of impaired arterial oxygenation in patient with liver cirrhosis andsevere respiratory insufficiency. Effects of indomethacin. Chest 1993;103:500-507.
65. Hobeika J, Houssin D, Bernard O, Devictor D, Grimon G, Chapuis Y.Orthotopic liver transplantation in children with chronic liver diseaseand severe hypoxemia. Transplantation 1994;57:224-228.
66. Rolla G, Bucca C, Brussino L. Methylene blue in the hepatopulmonarysyndrome. N Eng J Med 1994;331:1098.
67. Boker KHW, Hoper M, Lehman M, Fabel H, Manns MP. Effect of nitricoxide synthase inhibitor L-NAME on vascular resistance and arterialoxygenation in patients with hepatopulmonary syndrome [Abstract]HEPATOLOGY 1994;20(Suppl):333A.
HEPATOLOGY Vol. 32, No. 4, 2000 FALLON AND ABRAMS 865