PowerPoint Presentation/media/Files/Providence OR PDF...Herbal Cannabis >400 legal strains ... No...
Transcript of PowerPoint Presentation/media/Files/Providence OR PDF...Herbal Cannabis >400 legal strains ... No...
2017-11-17
1
Medical Cannabis & Cannabinoids
Dept of Internal Medicine, cross appt in Hematology/bone marrow transplant @ VGHDept of Internal Medicine @ UBC hospital Cannabis Authorization & Research @ Greenleaf Medical Clinic
Dr. Caroline MacCallum MD, FRCPC (Internal Medicine), B Sc. PharmacyClinical Instructor, Faculty of Medicine, UBC
Email: [email protected] Web: www.drcarolinemaccallum.com
@camaccallum
© Caroline MacCallum 2017
I have the following Relationships with commercial interests:
• Advisory Board: Emerald Health Botanicals, Shoppers Drug Mart, Vitality Biopharma
• CME content: MD Briefcase, Canopy Growth
• Speaker Fees: Canopy Growth, Shoppers Drug Mart
• Other: Medical Director, Greenleaf Medical Clinic
Presenter Disclosure
© Caroline MacCallum 2017
1. Endocannabinoid system and cannabis mechanism of action
2. Evidence for medical cannabis, “Indications” and contraindications
3. Cannabinoid products, routes, side effects and monitoring
4. Clarifying common cannabis myths – smoking vs. vaporization, CBD vs. THC, medical vs. recreational cannabis, illegal vs. legal medical cannabis sources in Canada.
Learning Objectives
© Caroline MacCallum 2017
Socioeconomic Consequences
• Healthcare costs
• Disability
• Lost workdays
Social Consequences
• Marital/family relations
• Intimacy/sexual activity
• Social isolation
Biopsychosocial Impact of Complex disease
Quality of Life• Physical functioning• Ability to perform
activities of daily living• Work• Recreation
Psychological Morbidity• Depression• Anxiety, anger• Sleep disturbances• Loss of self-esteem
© Caroline MacCallum 2017
Medication Deaths/ Toxicity Other Notes
Acetaminophen ~ 36 / yr
287 deaths 2005-13
4500 admission in
Canada / year
Health Canada
NSAIDs 16,500 / yr
(in OA & RA pt only)
103,000 hospital
admissions/yr in US
Singh 2000
(US stat)
Alcohol 29,001 TI = 10:1 US CDC 2013
Opioids (Rx) >14,000 TI = 70:1 US CDC 2014
Cannabis 0
LD50 = inhale 1500 lbs
in 15 min
TI = 1000:1 CDC & Health
Canada
Morbidity & Mortality of Pain “treatments”
Therapeutic Index - Williamson EM, Evans FJ. Cannabinoids in clinical practice. Drugs. 2000 Dec;60(6):1303-14. Review. PubMed PMID: 11152013.
© Caroline MacCallum 2017
76 F living independently at home
• RFR: neuropathic pain
• PmHx: DM, HTN, anxiety, OP, OA, DDD
• Rx: metformin, glyburide, ramipril, alendronate, gabapentin, morphine
• Previous Rx: pregabalin, citalopram, venlafaxine, T3, amitriptyline
• Complex Pain Symptoms: pain, nausea, anxiety, insomnia
• ADE: opioid, TCA, gaba = sedation, constipation, dry mouth, urinary retention
Case 1
2017-11-17
2
© Caroline MacCallum 2017 © Caroline MacCallum 2017
CarbamazepineOxcarbazepineTricyclic antidepressantTopiramateLamotrigineLidocaine*Cannabinoids (via 1° afferent, nonneuronal etc, not via Na+)
Na+
Peripheral
Sensitization
SpinalCord
*MacCallum, modified from Beydoun 2003
Ca++: Gabapentin
LevetiracetamOxcarbazepineLamotriginePregabalin
*Cannabinoids
NMDA: Ketamine
DextromethorphanMethadoneMemantine
*Cannabinoids
Central Sensitization
Descending Inhibitory Pathways
TCA5HT/ NE reuptake inhibitors SSRI Alpha adrenergic agentsOpioidsTramadol*Cannabinoids (via 5HT, PGD, NE + others)
Cannabis vs. Rx for Neuropathic Pain
Glial Cell Health Palmitoylethanolamide (PEA) Low Dose Naltrexone (LDN) ? Cannabis
✔
✔
✔
✔
✔NE/5HT, enkephalinsEndocannabinoid Tone? cannabis
✔
© Caroline MacCallum 2017
Cannabinoids are a class of compounds that act on cannabinoid receptors in the human body
Endocannabinoids are cannabinoids that are naturally produced in the body (endogenous)
Phytocannabinoids are cannabinoids produced by the cannabis plant
Synthetic cannabinoids are laboratory-synthesized compounds that bind to cannabinoid receptors
Definitions
© Caroline MacCallum 2017
Lipid signaling system in human body
Involved in most physiologic and pathophysiologic processes in the human body including:
PAIN
Appetite/digestion
Sleep/Wake
Psychiatric disease
Immune function
AND many many more ….
The Endocannabinoid System
© Caroline MacCallum 2017
Distribution of CB1 &2 in body
http://www.fundacion-canna.es/en/endocannabinoid-system © Caroline MacCallum 2017
How Do Cannabinoids work ?
Russo & Hohmann 2013 Role of cannabinoids in pain management, http://cannabiscoalition.ca/info/Russo-Hohmann-Role-of-cannabinoids-in-pain-management-2013.pdf
* Justone MOA
2017-11-17
3
© Caroline MacCallum 2017
• 450 compounds in Cannabis plant
• > 100 Cannabinoids with medical value
• Nonpsychoactive = CBD (cannabidiol), CBG, CBC etc.
• Psychoactive = Δ-9-THC (tetrahydrocannabinol)
• Non cannabinoids (nonpsychoactive & medical value)
• Terpenes & Flavonoids
• Cannabis species
• Sativa (energizing) & Indica (relaxing)
• THCA/CBDA (raw plant) heat decarboxylate THC/ CBD
Phytocannabinoids Basics
© Caroline MacCallum 2017
THC: Analgesic, muscle relaxant, anti anxiety, anti depressant, psychoactive*, antiemetic
CBD : Anti inflammatory, analgesic, antiemetic, anti anxiety, anti psychotic, anti depressant, may counteract THC and help “reduce the high”
*CBD + THC = “high” of THC + “entourage effect”
*Ratio of CBD : THC influences the therapeutic effects.
Cannabis has Multiple Actions
© Caroline MacCallum 2017
• CB1 is 10 times more abundant than μ opioid receptors
• Coanalgesic Effects - Cannabinoids exhibit analgesic effects and may potentiate the anti-nociceptive effects of opioids.
• So the same dose of opioids may be more potent. This may make it easier to wean down/off opioids.
• * I provide referred patients with a taper regimen which they can work on with their GP.
Cannabis & Polypharmacy Reduction
© Caroline MacCallum 2017
Cannabis & Pain
© Caroline MacCallum 2017
Can prevent peripheral nociception:
Decreasing nociceptor sensitizers
Decreasing nociceptor activators
Hyperpolarizing nociceptor
Central analgesia via:
Inhibition of GABA, glycine, and glutamate release
Blocking NMDA in dorsal horn cell
Local analgesia via:
Inhibition of mast cell function
inflammatory action of PG
substance P
MOA of Cannabis in Pain
2017-11-17
4
© Caroline MacCallum 2017
CBD
Boost natural ECS (AEA & 2AG)
inflammatory cytokines TNF and IL6 etc
Influence psychoimmunoglogy
Stress hormones & HPA axis
Decrease anxiety and depression
Decrease PTSD (and painful / fearful memory)
Action on δ and μ opioid receptors
MOA of Cannabis in Pain (cont.) Cannabinoids & Nociceptor
Photo credit: Dr. John Mcpartland
© Caroline MacCallum 2017
RCT in Cannabinoids in Pain
© Caroline MacCallum 2017
• DB, placebo controlled, RCT• NP pain patients on traditional rx• Vaporized cannabis , 8-12 puffs over 3 h. • Significant reduction in NP pain (VAS, NP pain scale etc)
p<0.0001 at 3h , p=0.0018 at 5h • Psychoactive effects were minimal• Low dose = medium dose for pain efficacy ***
© Caroline MacCallum 2017
• Cannabis does not have a DIN and therefore not approved by HC
• This document Reviews safety data and research
• Does not provide day to day practical direction or clinical information on “how to” authorize cannabis
Cannabis Guidance Documents (ref)
http://www.hc-sc.gc.ca/dhp-mps/alt_formats/pdf/marihuana/med/infoprof-eng.pdf
© Caroline MacCallum 2017
I take issue with these topics in the document:
• Nabilone should be used pre-cannabis
• Cannabis “should not be used” for:
• Fibromyalgia, Back Pain, Anxiety, insomnia
• “should” use 9% THC or less (based on compass study)
Cannabis “Guidance” Documents (ref)
http://www.cfpc.ca/uploadedFiles/Resources/_PDFs/Authorizing%20Dried%20Cannabis%20for%20Chronic%20Pain%20or%20Anxiety.pdf
2017-11-17
5
© Caroline MacCallum 2017
Potential Therapeutic Uses of Cannabis
? Future uses: DM, CAD, NASH, COPD, asthma, psoriasis, autism, pyrodermagangrenosum
© Caroline MacCallum 2017
CFPC Cannabis Guidance Document “Relative Contraindications”
*Adverse events are due to THC and are dose dependent. I have successfully used cannabis in these patients by using CBD only or low dose THC
**Resp concern is due to smoking cannabis (not oil/vap)
CFPC = College of Family Physicians of Canada
© Caroline MacCallum 2017
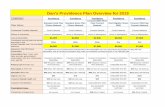
Natural vs. Synthetic Cannabinoids (ref) Advantages Disadvantages
Nabilone
Cesamet®
D.I.N
Long acting
Doses: 0.25, 0.5, 1mg capsules
Indication: chemo N/V
Clinical experience/ trials
Insurance coverage
++Side effects (mimics THC)
Long acting = 10+h
Cost: 5mg d = 300$/mo
Herbal
Cannabis
>400 legal strains in Canada
Short acting (vaporization) vs.
Long acting (oil)
Entourage effect
THC < 1 % - > 29 %, CBD < 1% to
> 20 % (can get CBD only or THC
only and combinations in
between)
No D.I.N
No approved indications in
Canada
No coverage
Need more studies
No standardization
Dose =“start low and go slow”
Cost: 75 - 300$ +/ mo
Nabiximols
Sativex ®
1:1 (2.5 : 2.7%)
THC:CBD
D.I.N
Delivery: Spray/SL (short acting)
Indication: NP pain, MS,
Clinical experience/trials
Entourage effect
Dose: Single formulation
No coverage
Cost: 5 sprays/day = ~ 375$
/ month (250$/bottle, sold in
3pack = 750$ up front)
Table created by Dr. MacCallum © Caroline MacCallum 2017
Source of Cannabis (in Canada)
Issue LP Dispensary
Health Canada Regulated ✔ ✖
Legal Cannabis ✔ ✖
“Medical Card” (does not imply patient is “legal”)
✔ ✔
Strict testing for metal, toxins, pesticides, fungus, contaminants etc
✔ ✖
Consistency of THC & CBD % ✔ ✖
Authorized by MD ✔ ✔ & ✖
Onsite distribution ✖ ✔
© Caroline MacCallum 2017
Routes of Administration
* flower/oil are legal herbal sources of cannabis is canada
MacCallum C, Russo E. "Practical Considerations in Medical Cannabis Administration and Dosing". Europ
J Intl Med 2018 (submission in progress).
© Caroline MacCallum 2017
• Smoking @ 600-900C CO + carcinogens
• Vap @ 180-200C little, if any CO (Abrams et al 2007)
• Vap = more efficient, $ saving (30-50% less) & safer
• So far, 2 vaporizers = medical devices by HC
• 1 cannabis cig = x4 tar of nicotine cig. Also
many patients mix tobacco with cannabis.
Vaporizing vs. Smoking
2017-11-17
6
© Caroline MacCallum 2017
• Medical goal = lowest dose of THC for symptom control and functional improvement
• “Start low, go slow and stay low ”
• THC start = 2.5 mg5mg 7.5mg 10mg
• Self titrate to lowest THC dose (max benefit & min ADE)
• No real dosing guidelines for CBD
• Avg dose cannabis = 1-3 g/day (5% use > 3g / day - Ware et al)
• Tolerance to adverse effects but NOT to benefit
Dosing
MacCallum C, Russo E. "Practical Considerations in Medical Cannabis Administration and
Dosing". Europ J Intl Med 2018 (submission in progress).
© Caroline MacCallum 2017
Side Effects (2°THC)
MacCallum C, Russo
E. "Practical
Considerations in
Medical Cannabis
Administration and
Dosing". Europ J Intl
Med 2018 (submission
in progress).
© Caroline MacCallum 2017
• Largest study (prospective) of the long term safety of MC use by patients with chronic pain
• NO serious ADE vs control • NO harm on cognitive function, PFT, biochem (Cr, LFT, CBC)• Significant improvement in their levels of pain, symptom
distress, mood and quality of life
© Caroline MacCallum 2017
• Most DI are associated with concurrent use of other CNS depressants
• Clinically significant drug interactions are unlikely
•Exception - ↑ clobazam levels with very high dose CBD
• “In clinical trials where SATIVEX® (CBD 2.5mg/THC 2.7mg per spray) has been taken concomitantly with other drugs metabolized by the CYP450 enzyme system, no clinically apparent drug-drug interactions have been seen in these trials at clinical doses.”
• SATIVEX has been studied for > 10 years with 6000 patient year data.
• Extensive DI studies have not been done. Existing studies have not demonstrated toxicity/ loss of effect of concomitant medications, but still theoretically possible (Health Canada 2013)
Metabolism & Drug Interactions (ref)
© Caroline MacCallum 2017
• THC is oxidized by (CYP) 2C9, 2C19, and 3A4
• ↑ THC – with inhibitors (fluoxetine, omeprazole, macrolides, ketoconazole, diltiazem, verapamil, HIV proteases, amiodarone)
• ↓ THC - 2C9, 3A4 inducers (rifampicin, phenytoin, St. John’s Wort)
• THC inhibits CYP 1A1, 1A2, 1B1
• ↑ amitriptyline, theophylline, granisetron, flutamide
Animal / Invitro Studies (ref)
© Caroline MacCallum 2017
• Response/efficacy
• Strains /dose (? % CBD/THC)
• Route (change to oil?)
• Potential drug interactions
• Review meds & consider a slow taper (opioids, benzo etc)
• Repeat anxiety GAD-7, depression PHQ-9, pain BPI scale, Q of L and functional improvement
Monitoring
2017-11-17
7
© Caroline MacCallum 2017
• Cannabis intoxication (THC) increases the risk of collision related morbidity and mortality up to 3 fold
• Similar to caution with other medications which impair judgment including; opioids, muscle relaxants, alcohol
• If using cannabis daily, THC tolerance will develop and there may be minimal impairment (similar to tolerance to prescription opioids)
• BOTTOM LINE: If impaired DO NOT drive /do safety sensitive job
Driving Considerations
http://www.cfpc.ca/uploadedFiles/Resources/_PDFs/Authorizing%20Dried%20Cannabis%20for%20Chronic%20Pain%20or%20Anxiety.pdf
© Caroline MacCallum 2017
1. Multiple concurrent diseases
2. Symptom clusters (sleep, mood, anxiety, nausea etc)
3. Multiple prescription Rx failures
4. Reduce Adverse Drug Events
5. Reduce Polypharmacy
6. Co-analgesia Effect of Cannabis & Opioid opioid
7. Help with withdrawal SE when tapering opioids, SSRI, TCA etc
8. > 20 Mechanism of Action for Pain. Can help multiple pain generators ie. neuropathic, nociceptive, mechanical
Back to the case…. Why cannabis?
© Caroline MacCallum 2017
1. Focus on Sleep – THC helps with pain, anxiety and insomnia. If sleep improves , so will daytime pain, anxiety, mood etc.
• Strategy for bedtime dosing: • THC Oil for ingestion for “long acting” relief
• THC Vaporization for “short acting” relief
• Use “sedating” (indica) THC
2. Daytime - CBD oil to minimize impairment
3. “Energizing” (sativa) vaporization “short acting” for severe daytime pain (counsel on driving/ potential impairment).
4. Follow up visit: Slow Taper off opioids/Rx if appropriate.
Cannabis Rx Treatment Approach to Chronic Pain
*TREAT COEXISTING DISORDERS: sleep, mood, anxiety & CSS.
**TREAT COEXISTING “PAIN GENERATORS”: ie mech, inflam,
nociceptive/neuropathic. (EACH may need different Rx approaches)
Ie. NP meds, Methadone,
Cannabis, Complimentry & Alternative tx
+ Gentle Exercise; Yoga, Tai Chi, swim,
walk, (not strenuous cardio)
+ Neuromodulation, Neuroablation, or
Surgery*
+ CBT, pacing, groups, stress management
+ TPI, IMS, accupuncture,
prolotherapy
Ie. IV ketamine, lidocaine
Diet
Education
© Caroline MacCallum 2017
• Vaporizing ≠ Smoking
• Lowest THC dose = benefit & ADE
• CBD & Terpenes = medical benefit & NOT psychotropic
• CBD + THC = “high” of THC (+ ”entourage effect”)
• Recreational users ≠ Medical users (symptom control vs. euphoria)
• Safer than opioids ( > 100,000 deaths vs. 0 since 2000)
• Driving issues = similar to opioids
• LP = consistent, safe and leg medicinal cannabis
Take Home Points
2017-11-17
8
© Caroline MacCallum 2017
Resources on www.drcarolinemaccallum.com
© Caroline MacCallum 2017
Email: [email protected] Tel: 1-877-513-4769Web: www.drcarolinemaccallum.com @camaccallum
Resources:
© Caroline MacCallum 2017
Other Resources:
http://www.ccic.net/index.php?id=335,0,0,1,0,0 https://www.youtube.com/watch?v=ohMeUJPyRiQ © Caroline MacCallum 2017
Extra Slides on Opioids & Pain
© Caroline MacCallum 2017
No more than 10% reduction every 1-2 week
May require 5% reduction every 1-2 week when at lower doses
Opioid taper WILL result in withdrawal pain with EACH reduction in dose (each “cycle” of withdrawal will resolve within 5 days).
For unpleasant withdrawal symptoms, consider:
Clonidine/propranolol (anxiety, tremors, palpitations)
Loperamide (diarrhea)
Oxybutynin (sweating)
Antihistamines (runny eye/nose)
Cannabis (has co-analgesic/synergistic effects when used with opioids which can make it even more favourable when tapering off opioids specifically)
Education on Opioids Tapering
© Caroline MacCallum 2017
CSS - http://thischangedmypractice.com/hope-for-patients-with-fatigue-pain-and-unexplained-symptoms/
CFS - http://thischangedmypractice.com/chronic-fatigue-syndrome-disease/
Opioid Withdrawl -http://thischangedmypractice.com/managing-opioid-withdrawal/
UBC “This Changed My Practice”
2017-11-17
9
© Caroline MacCallum 2017
The Anxiety and Phobia workbook, Edmund J Bourne (~20$)
The Chronic Pain Care Workbook, Michael J Lewandowski (~20$)
Holistic Pain Relief Dr. Heather Tick Integrative pain medicine
Living Well with Pain and Illness Vidyamala Burch
How to be Sick: A Buddhist Inspired Guide for the Chronically Ill and their Caregivers (Toni Bernhard)
Meditation Exercises to Enlighten the Mind and Heal the Body Tulku Thondup
Jon Kabat-Zinn is one of the better known authors on mindfulness
Neil Pearson's "Understand Pain, Live Well Again" book
http://www.lifeisnow.ca/pain-management-products/
Explain Pain by Moseley is always a good choice too, it's a classic
http://www.amazon.ca/Explain-Pain-David-S-Butler/dp/097509100X
Books for Patients
© Caroline MacCallum 2017
• Pain Toolkit
https://www.painbc.ca/sites/default/files/PainBC-PainToolbox-2016-Digital.pdf
• CSS handout
http://med-fom-tcmp.sites.olt.ubc.ca/files/2015/10/Central-Sensitivity-Syndromes-CSS.pdf
• Opioid withdrawal
http://med-fom-tcmp.sites.olt.ubc.ca/files/2014/06/For-Patients-TCMP-2014-Managing-Opioid-Withdrawal.pdf
Handouts For Patients
© Caroline MacCallum 2017
Extra Cannabis Slides
Cannabis Evidence (ref)
MacCallum C, Russo E. "Practical Considerations in Medical Cannabis Administration and Dosing".
Europ J Intl Med 2018 (submission in progress).
MacCallum C, Russo E. "Practical Considerations in Medical Cannabis Administration and Dosing". Europ J Intl Med 2018
(submission in progress).
Cannabis Mechanism of Action in Chronic Pain
Prevention peripheral nociception ● Decreasing nociceptor sensitizers
● Decreasing nociceptor activators
● Hyperpolarizing nociceptor
Central analgesia via ● Inhibition of GABA, glycine, and glutamate release
● Blocking NMDA in dorsal horn cell
Local analgesia via ● Inhibition of mast cell function
● Inflammatory action on PG & substance P
CBD ● Boost natural ECS (Increase AEA & 2AG)
● Decrease inflammatory cytokines TNF and IL6, etc.
Influence psychoimmunology ● Stress hormones & HPA axis
● Decrease anxiety and depression
● Decrease PTSD (and painful/fearful memory)
● Action on δ and μ opioid receptors
TMCI. 2017. “Clinical Cannabinoid Medicine Curriculum.” Accessed June 5. https://themedicalcannabisinstitute.org/product/clinical-cannabinoid-medicine-curriculum-2/.
2017-11-17
10
Conditions and Cannabis Evidence (ref)
MDBriefcase 2017:http://www.advancingpractice.com/p-98-medical-cannabis-iq-the-
fundamentals.aspx?utm_source=MCIQ_website&utm_medium=referral&utm_campaign=MCIQ&utm_content=MC_medicalcannabis
Whiting et al. 2015. “Cannabinoids for Medical Use: A Systematic Review and Meta-Analysis.” Jama 313 (24): 2456–73.
Nausea and vomiting due to
chemotherapy
• A greater average number of patients showing a complete nausea and vomiting response
with cannabinoids (47% vs 20%; odds ratio [OR], 3.82 [95% CI, 1.55-9.42])
Chronic pain • Reduction in pain (37% vs 31%; OR, 1.41 [95% CI, 0.99-2.00])
• A greater average reduction in numerical rating scale pain assessment (on a 0-10-point
scale; weighted mean difference [WMD], −0.46 [95% CI, −0.80 to −0.11])
Spasticity • An average reduction in the Ashworth spasticity scale (WMD, −0.36 [95% CI, −0.69 to
−0.05])
Adverse effects • Higher risk of adverse effects
• Common AEs included dizziness, dry mouth, nausea, fatigue, somnolence, euphoria,
vomiting, disorientation, drowsiness, confusion, loss of balance, and hallucination
A partial list of peer-reviewed double-blind, RCT Cannabis Studies (ref)
Year Reference Title Number of
Participants
2007 (Abrams et al. 2007) Cannabis in Painful HIV-Associated Sensory Neuropathy a Randomized Placebo-Controlled Trial 50
2010 (Collin et al. 2010) A Double-Blind, Randomized, Placebo-Controlled, Parallel-Group Study of Sativex, in Subjects with Symptoms of Spasticity due to
Multiple Sclerosis
337
2009 (Ellis et al. 2009) Smoked Medicinal Cannabis for Neuropathic Pain in HIV: A Randomized, Crossover Clinical Trial 34
2010 (Johnson et al. 2010) Multicenter, Double-Blind, Randomized, Placebo-Controlled, Parallel-Group Study of the Efficacy, Safety, and Tolerability of THC:
CBD Extract and THC Extract in Patients with Intractable Cancer-Related Pain
144
2013 (Langford et al. 2013) A Double-Blind, Randomized, Placebo-Controlled, Parallel-Group Study of THC/CBD Oromucosal Spray in Combination with the
Existing Treatment Regimen, in the Relief of Central Neuropathic Pain in Patients with Multiple Sclerosis
339
2011 (Novotna et al. 2011) A Randomized, Double-blind, Placebo-controlled, Parallel-Group, Enriched-Design Study of nabiximols*(Sativex®), as Add-on
Therapy, in Subjects with Refractory Spasticity Caused by Multiple Sclerosis
572
2007 (Nurmikko et al. 2007) Sativex Successfully Treats Neuropathic Pain Characterised by Allodynia: A Randomised, Double-Blind, Placebo-Controlled Clinical
Trial
125
2011 (Schoedel et al. 2011) A Randomized, Double-blind, Placebo-Controlled, Crossover Study to Evaluate the Subjective Abuse Potential and Cognitive
Effects of Nabiximols Oromucosal Spray in Subjects with a History of Recreational Cannabis Use
58
2010 (Ware et al. 2010) Smoked Cannabis for Chronic Neuropathic Pain: A Randomized Controlled Trial 23
2008 (Wilsey et al. 2008) A Randomized, Placebo-Controlled, Crossover Trial of Cannabis Cigarettes in Neuropathic Pain 44
2010 (Hazekamp and
Grotenhermen 2010)
Review on clinical studies with cannabis and cannabinoids 2005-2009 Review
2016 (Kowal, Hazekamp, and
Grotenhermen 2016)
Review on clinical studies with cannabis and cannabinoids 2010-2014 Review
© Caroline MacCallum 2017
• Cost: minimum 5$/g x 1g/d = 150$/mo.
• Compassionate pricing for patients on disability or <30K/year. Usually 6-8$/g.
• Lock box: Patient has been advised to use a locked box to so store his cannabis if there are children visiting/living in the home.
• Safety: safety sensitive occupation & activities, as well as implications of work urine drug screening were discussed.
• Urine drug screen: can be + for 3 wk after THC use.
Cannabis “fine print”
© Caroline MacCallum 2017
• Income tax: Patient can use receipts for vaporizers, medical cannabis, clinic fees etc as medical expenses Some medical plans cover the cost of cannabis
• Travel: Within Canada, keep legal cannabis in original packaging along with Rx from MD. Cannabis is federally illegal in the US, and a number of other countries. Options for travel would include rx nabilone or sativex.
• Treatment Agreement: signed by patient
Cannabis “fine print”
© Caroline MacCallum 2017
• Dried Product/bud: get from an LP which uses GAMMA RADIATION to kill fugus/bacterial. So that these contaminants are not inhaled.
• Oil: the extraction process of CBD/THC from dried product into oil should kill fungus/bacteria, therefore gamma radiation is not as big an issue.
Neutropenic / Immunosuppressed Patients
© Caroline MacCallum 2017
• I DO NOT recommend as main route of administration
• Trendy you tube videos
• Being used as anti-nauseant, anti-inflammatory and for health prevention
• THCA/CBDA have little effect vs THC/CBD and require MASSIVE quantities Ie 20-200g of leaves/bud for 1 drink
• My concern is that this quantity may be diverted.
• May be an option for patients who grown their own cannabis as they have left over leaves/trimmings which they may not want to waste.
Juicing
2017-11-17
11
© Caroline MacCallum 2017
Increased risk of addiction
In those at risk, younger age of first cannabis use is associated with younger age of schizophrenia and bipolar disorder and worse outcomes
Regular users < 18 years old have increased risk of persistent cognitive effects
Regular use in youth associated with increased social dysfunction, anxiety and depression
Cannabis and Youth
1. Urbanoski KA et al. Eur Addict Res 2005;11(3):115-232. Nocon A, et al. J Psychiatr Res 2006;40(5):394-4033. Dragt S, et al. Acta Psychiatr Scand 2012;125(1):45-534. Crean RD et al. J Adddict Med 2011;5(1):1-85. Fergusson DM et al. Addiction 2001;97(9):1123-35
© Caroline MacCallum 2017
• CBD alone may be a useful therapy for children (or adults) with sever developmental/self harm, schizophrenia , seizures, brain tumors, refractory or rare diseases
• In these conditions, CBD (and low or no THC) can be more efficacious with less SE than traditional therapies. (ie opioids, antiepileptic etc)). Risks and benefits needs to be considered.
• FYI Normal neuronal maturation and synaptic change occur up to mid 20s, there is NO evidence for an age cut-off at 25 years any more than 18 or 21.
Cannabis & Youth (cont)
© Caroline MacCallum 2017
Is Cannabis Addictive?
http://www.drugwarfacts.org/cms/Addictive_Properties#sthash.EQ3MjDzT.dpbs © Caroline MacCallum 2017
There is evidence of a statistical association between cannabis use and the development of schizophrenia or other psychoses, with the highest risk among the most frequent users. (Abrams 2017)
“...an increased familial morbid risk for schizophrenia may be the underlying basis for schizophrenia in cannabis users and not cannabis use by itself.” (Proal et al. 2014)
“...cannabis does not induce schizophrenia in non-vulnerable individuals.” (Hill 2015)
In individuals with schizophrenia and other psychoses, a history of cannabis use may be linked to better performance on learning and memory tasks. (Abrams 2017)
Schizophrenia
© Caroline MacCallum 2017
Extra Cannabis Studies • Chronic pain – MSK, post traumatic, arthritis, cancer, FM,
migraine, MS, sickle cell, thoracic outlet syndrome
• 21 Cannabis non-naïve subjects on LA morphine/oxycodone
• 5 day study = vaporized cannabis in the PM day 1, TID on
days 2–4, and in the AM of day 5
• Statistically significant 27% [95% CI 9 – 46] in pain score
• No significant effect on opiate metabolism
• Limitations: sm size, short duration, not randomized, No
placebo
Abrams DI et al. Clin.Pharmacol.Ther. 90: 844-851.
2017-11-17
12
• First placebo controlled, DB, RCT in RA
• 1 spray = THC 2.7% & 2.5% CBD (=CBDM)
• CBM produced statistically significant improvement in pain
on movement, pain at rest, quality of sleep , DAS28, and SF-
MPQ pain
• Majority of AE were mild/mod
• No withdrawal/serious AE
• RCT, DB, placebo controlled crossover design• 37 cannabis naïve or exposed MS patients with moderate
spasticity• Avg of 4 puffs of 4% THC vs. placebo cigarettes• Primary outcome = Significantly improved spasticity (p< 0.001)• Also significantly improved pain (P=0.008), significant reduction
in cognitive function (p=0.003)• No significant change in physical function
Corey-Bloom et al CMAJ. 2012 Jul 10;184(10):1143-50
© Caroline MacCallum 2017