Potential of CXCR4 antagonists for the treatment of metastatic … in lung cancer... ·...
Transcript of Potential of CXCR4 antagonists for the treatment of metastatic … in lung cancer... ·...

621
Review
www.expert-reviews.com ISSN 1473-7140© 2011 Expert Reviews Ltd10.1586/ERA.11.11
The CXCR4 chemokine receptor & its ligand, CXCL12Chemokines induce the directional migration of cells towards a gradient of the chemokine (chemotaxis) by binding to seven-transmem-brane G-protein-coupled (chemokine) recep-tors. Chemokines are small (~8–14 kDa) secreted proteins that are divided into the two main chemokine subfamilies on the basis of the arrangement of two N-terminal cysteine residues. These cysteine residues either have an amino acid between them, or they are adja-cent, defining CXC or CC chemokines [1]. In a more functional sense, chemokines can also be classified as inflammatory or homeostatic chemokines that are induced during inflamma-tion to attract inflammatory cells or are consti-tutively secreted by stromal cells (homeostatic chemokines). Homeostatic chemokines, such as CXCL12, coordinate cell trafficking and hom-ing, which is essential during development, and for homeostasis and function of the immune and stem cell systems.
The chemokine CXCL12, previously called stromal cell-derived factor-1 (SDF-1) or pre-B-cell growth-stimulating factor [2], signals through the CXCR4 chemokine receptor. In 1996, the coreceptor function of CXCR4 for entry of T-tropic (X4) HIV-1 strains into CD4+ T cells was discovered [3,4]. Subsequently, CXCL12 and CXCR4 gene-deleted mice were described with an identical, lethal phenotype, suggesting a monogamous relationship between CXCL12 and CXCR4. The phenotype of these mice is characterized by deficient hematopoiesis with defects in B-cell development and myelo-poiesis, and abnormal neuronal and cardiovas-cular development [5,6]. More recently, CXCR7 has been described as an alternate receptor for CXCL12, which appears to function by seques-tering CXCL12 [7] and modifying CXCR4 signaling rather than displaying autonomous signaling in response to CXCL12 [8]. Inherited heterozygous autosomal-dominant mutations of
the CXCR4 gene, which result in the trunca-tion of the C-terminus (C-tail) of the receptor,
Jan A Burger†1, David J Stewart2, Ori Wald3 and Amnon Peled4
1Department of Leukemia, Unit 428, The University of Texas MD Anderson Cancer Center, PO Box 301402, Houston, TX 77230-1402, USA 2Department of Thoracic/Head and Neck Medical Oncology, University of Texas MD Anderson Cancer Center, Houston, TX, USA 3Department of Cardiothoracic Surgery, Goldyne Savad Institute of Gene Therapy, Hadassah Hebrew University Hospital, Jerusalem, Israel 4Goldyne Savad Institute of Gene Therapy, Hadassah Hebrew University Hospital, Jerusalem, Israel †Author for correspondence:Tel.: +1 713 563 1487 Fax: +1 713 794 4297 [email protected]
Despite advances in surgery, chemotherapy and radiotherapy over the last decades, the death rate from lung cancer has remained largely unchanged, which is mainly due to metastatic disease. Because of the overall poor prognosis, new treatment strategies for lung cancer patients are urgently needed, and targeting CXCR4 constitutes such a novel, attractive strategy. Tumor cell migration and metastasis share many similarities with leukocyte trafficking, which is critically regulated by chemokine receptors and adhesion molecules. Lung cancer cells express CXCR4 (CD184), a seven-transmembrane G-protein-coupled chemokine receptor. Stromal cells within the tumor microenvironment constitutively secrete stromal cell-derived factor-1 (SDF-1/CXCL12), the ligand for CXCR4. Activation of CXCR4 induces lung cancer cell migration and adhesion to stromal cells, which in turn provides growth- and drug-resistance signals to the tumor cells. CXCR4 antagonists, such as Plerixafor (AMD3100) and T140 analogues (TN14003/BKT140), can disrupt CXCR4-mediated tumor cell adhesion to stromal cells and sensitize lung cancer cells to cytotoxic drugs. Therefore, targeting the CXCR4–CXCL12 axis is a novel, attractive therapeutic approach in small-cell lung cancer and non-small-cell lung cancer. In this article, we summarize data about the cellular and molecular microenvironment in small-cell lung cancer and non-small-cell lung cancer, as well as the role of CXCR4 in tumor–stroma crosstalk. In addition, we review the current status of the preclinical and clinical development of CXCR4 antagonists.
Keywords: CXCL12 • CXCR4 • CXCR4 antagonists • NSCLC • SCLC • tumor microenvironment • tumor stem cells
Potential of CXCR4 antagonists for the treatment of metastatic lung cancerExpert Rev. Anticancer Ther. 11(4), 621–630 (2011)
THeMed ArTICLe y Lung Cancer
For reprint orders, please contact [email protected]

Expert Rev. Anticancer Ther. 11(4), (2011)622
Review Burger, Stewart, Wald & Peled
are associated with a rare disease known as warts, hypogamma-globulinemia, immunodeficiency and myelokathexis (WHIM) syndrome [9].
Bone marrow stromal cells and other mesenchymal stromal cells (MSCs) are considered the major source for CXCL12 in adult individuals. CXCL12-secreting stromal cells can be found in various tissues, such as the liver, lungs, lymphatic tissues and the marrow [10]. Constitutive high-level CXCL12 secretion by reticular stromal cells and endothelial cells in the marrow is essen-tial for homing, retention [11] and maintenance of hematopoietic stem cells (HSCs) in distinct vascular and endosteal niches for their development and growth [12]. Via CXCL12, these stromal cells also attract circulating hematopoietic progenitor cells [11] or leukemia cells [13] for homing to the marrow. CXCR4 is the only functional chemokine receptor on hematopoietic progenitor cells [14], emphasizing the predominant role of this chemokine receptor for homing and maintenance of HSCs in marrow niches. Current clinical trials with AMD3100 utilized this mechanism of CXCR4-mediated homing to the marrow in order to mobilize HSCs to the peripheral blood for HSC collection for autologous stem cell transplantation. In Phase II trials, mobilization with the combination of AMD3100 and granulocyte–colony-stimulating factor (G-CSF) results in the collection of higher numbers of progenitor cells than with G-CSF alone [15]. The peptide CXCR4 antagonist 4F-benzoyl-TN14003 is also a potent mobilizing agent of HSC alone and in combination with G-CSF [16].
CXCR4 has also been described to function as a key migration factor for targeted cancer cell metastasis to organs that secrete CXCL12, the ligand for CXCR4. In the tumor microenviron-ment, the CXCR4–CXCL12 axis furthermore supports cancer cell survival and growth, and participates in tumor angiogenesis [17].
CXCR4 & the tumor microenvironment Compelling evidence has emerged in recent years indicating that accessory cells, collectively referred to as ‘stromal cells’, play a critical role in disease progression in various cancers of both the hematopoietic and nonhematopoietic system. The importance of the microenvironment, defined as tissue niches where pro-genitor cells reside and are maintained by accessory ‘feeder’ cells, was initially recognized for hematopoietic stem cells, based upon the observation that transplanted hematopoietic progenitor cells specifically home to the marrow microenvironment where they find conditions necessary for their maintenance and propagation. More recently, the architecture of distinct niches for hematopoi-etic and various tissue stem cells, and the mechanisms that govern stem cell homeostasis within these niches, are emerging [18,19]. Regulated migration and homing of stem cells to tissue niches is a critical step during embryonic development or tissue repair, but also in cancer (stem) cell dissemination [20].
The interactions of cancer cells with components of their tumor microenvironment are bidirectional and crucial for cancer pro-gression [21–23]. In order to organize their microenvironment, tumor cells communicate with their surrounding microenviron-ment via a network of secreted growth factors, cytokines and chemokines [24,25].
Among the various cells that compose reactive infiltrates into tumors, MSCs [26,27], monocyte/macrophage lineage cells and T lymphocytes [28], along with the extracellular matrix (ECM) and blood vessels, are key cellular players in tumor–microenviron-ment crosstalk. When associated with epithelial cancers, MSCs are oftentimes called carcinoma-associated fibroblasts (CAFs) [17] or myofibroblasts, and can be identified by staining with a-smooth muscle actin antibodies.
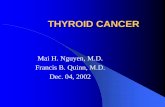
Different types of cancers express different chemokines and chemokine receptors [25,29]. However, the chemokine receptor CXCR4 is the only one that is expressed by the majority of cancer types. Tumor cells from at least 23 different types of cancers express CXCR4 [25]. Furthermore, MSCs/CAFs consti-tutively secrete the chemokine CXCL12 (SDF-1), which in turn promotes tumor progression via direct and indirect mechanisms (Figure 1) [30]. Cells of monocyte/macrophage lineage are another highly important cell type in the tumor microenvironment [31]. When associated with tumor, lymphoma or chronic lymphocytic leukemia cells, monocytes/macrophages are referred to as tumor-associated macrophages, lymphoma-associated macrophages or nurse-like cells, respectively. These cells support cancer progres-sion by inducing cancer cell motility and metastasis, and angio-genesis. Among many others, CXCL12 is a prominent mediator accounting for tumor-associated macrophage/lymphoma-associ-ated macrophage accumulation in tumors [32]. Increased num-bers of regulatory T cells in the tumor microenvironment can be detected by forkhead box P3 staining, and are thought to suppress immune recognition and response to the neoplastic cells [28]. Among the many molecular pathways of tumor–stroma crosstalk, the CXCL12–CXCR4 axis plays a critical role, as dem-onstrated in solid and hematologic tumors [17,33]. MSCs/CAFs are well known for constitutive secretion of CXCL12. CXCL12 promotes carcinoma cell growth directly through the CXCR4 receptor expressed on tumor cells, and indirectly by recruitment of endothelial progenitor cells into tumors, thereby causing neoangiogenesis [17].
Vascular endothelial growth factor is one of the most potent and specific regulators of angiogenesis, and is required for viabil-ity and growth of various solid tumors. VEGF can induce the perivascular expression of CXCL12 by myofibroblasts, which, in turn, positions monocyte–macrophages in the target tissue, where they promote proliferation of tumor cells [34]. Recently, the VEGFR antagonist Avastin® was approved in combination with carboplatin and paclitaxel for the initial systemic treat-ment of patients with unresectable, locally advanced, recur-unresectable, locally advanced, recur- advanced, recur-rent or metastatic, non-squamous non-small-cell lung cancer (NSCLC) [35].
In addition, abnormal expression or function of EGF fam-ily members may stimulate tumor progression and can affect CXCR4 expression and function. The EGF receptor (EGFR) HER2 increases CXCR4 expression and inhibits CXCR4 degra-dation, which could explain increased invasion and metastasis of HER2-positive breast cancer cells [36]. A substantial percentage of lung cancers express cell surface EGFRs, and similar interactions between EGFRs and CXCR4 may also exist in lung cancer.

www.expert-reviews.com 623
ReviewPotential of CXCR4 antagonists for the treatment of metastatic lung cancer
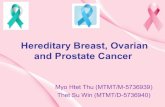
CXCR4 in NSCLCIn all major subtypes of NSCLC, the tumor cells expressed CXCR4 by immunohisto-chemistry (Figure 2), and NSCLC patients with higher CXCR4 surface-expressing tumors are more likely to have metastatic disease [37]. Spano and colleagues reported that strong CXCR4-positive nuclear stain-ing was associated with a better outcome in early-stage NSCLC [38], which was con-firmed by Wagner et al. [39]. Based on a large sample size, these authors proposed high CXCR4 surface expression as an independent high-risk factor in NSCLC, whereas nuclear staining conferred a sur-vival benefit [39]. The primary sites of NSCLC metastasis (the lymph nodes, bone, liver, adrenal glands and brain) are all sites of high-level CXCL12 expression [10], and therefore CXCR4 is considered a key guidance mechanism for NSCLC metas-tasis. Phillips and colleagues demonstrated that anti-CXCL12 antibodies abrogated metastasis in a murine NSCLC model [40]. Oonakahara et al. demonstrated a correlation between CXCR4 expression and NSCLC dissemination into the pleu-ral space [41]. Chen et al. recently reported that high-level CXCR4 expression cor-relates with brain-specific metastasis of NSCLC [42].
Some studies suggested a link between high-level CXCL12 expression and a more advanced disease stage [39,43]. We have pre-viously shown that CXCL12 is expressed in the majority of NSCLC tissue sections (up to 80%) obtained from stage IA–IIB disease patients [43]. Both neoplastic cells and stromal cells (CAFs and vascular endothelial cells) stained positive for CXCL12. CXCL12-expressing CAFs and other stromal cells were mostly detected in proximity to CXCL12-negative tumor tissues, and vice versa. In vitro stimu-lation of NSCLC cells with CXCL12 increased their colony-forming capacity and induced ERK phosphorylation. These findings indicate that CXCL12–CXCR4 interactions in NSCLC occur in situ and act locally to support tumor growth. CXCL12 levels in NSCLC tumors were elevated compared with peripheral blood, and high CXCL12 expression correlated with increased tumor infiltration by acces-sory cells, including regulatory T-cell
Blood vessel
Angiogenesis
CXCR4
Endothelial progenitor cells
Endocrine
CXCL12
CXCL12
SCLC/NCSLC cells
Paracrine
Blood vessel
Bone marrow
Bone
HPC
Marrow stromal cells
CAFs
CXCL12
Expert Rev. Anticancer Ther. © Future Science Group (2011)
pO2
CXCR4
CXCL12
Figure 1. Importance of the CXCR4 chemokine receptor and its ligand, CXCL12, in the tumor microenvironment and for targeted metastasis. Within hypoxic areas of tumors, both CXCL12 expression by fibroblasts and CXCR4 expression on tumor cells, such as SCLCs and NSCLCs, increases, which stimulates tumor cell motility and invasiveness. These relationships are indicated by the triangles in the top part of the figure. CAFs stimulate tumor progression by CXCL12 secretion. Two major mechanisms by which fibroblast-derived CXCL12 promotes tumor progression have been identified. First, CXCL12 promote tumor cell growth in a paracrine fashion by directly stimulating tumor cell growth via CXCR4. Second, CXCL12 from CAFs induces recruitment of endothelial progenitors, which allow for tumor angiogenesis (endocrine effect of CXCL12). Targeted metastasis to the marrow or other sites of high CXCL12 expression involves CXCR4 activation on circulating tumor cells that ‘hijack’ the CXCR4–CXCL12 axis for homing to microenvironments that are normally restricted to HPCs. CXCL12 gradients attract CXCR4-positive tumor cells to the marrow and other sites where stromal cells secrete high levels of CXCL12. As a consequence, tumor cells can displace HPCs from their protective microenvironment, resulting in hematopoietic dysfunction. Moreover, tumor cells may invade adjacent tissues, resulting in bone destruction. CAF: Carcinoma-associated fibroblast; HPC: Hematopoietic progenitor cell; NSCLC: Non-small-cell lung cancer; pO
2: Partial pressure of oxygen; SCLC: Small-cell
lung cancer. Adapted from [33].

Expert Rev. Anticancer Ther. 11(4), (2011)624
Review Burger, Stewart, Wald & Peled
lymphocytes [43]. Overall, the CXCL12–CXCR4 axis appears to be a key player in NSCLC pathogenesis, acting in an autocrine and paracrine fashion in the tumor microenvironment, and as a chemoattractant and growth-promoting factor at primary and metastatic sites.
CXCR4 in small-cell lung cancer Extensive-stage small-cell lung cancer (SCLC), which accounts for approximately 70% of all SCLC cases, is primarily treated with chemotherapy with a high initial response rate of 60–70%.
Despite this high initial response rate, the median survival of extensive SCLC is only 10 months, because the vast majority of patients relapse from minimal residual disease [44].
There is growing evidence suggesting that interactions with accessory stromal cells, which are dispersed with SCLC cells in pri-mary tumors and at metastatic sites, promote SCLC growth, drug resistance and overall disease progression [45,46]. Like NSCLC, SCLC cells are engaged in a complex crosstalk with accessory cells (mesenchymal fibroblasts, inflammatory cells, vasculature and others), soluble factors and ECM components. SCLC immuno-histochemistry reveals an infiltration by stromal cells, consisting of either fine fibrous septa or a desmoplastic response [47]. This stroma in SCLC also reveals high levels of the ECM, including fibronectin, collagen IV and tenascin [45,48]. Adhesive interactions between SCLC cells and the ECM confer survival- and drug-resistance signals that are mediated through adhesion molecules, in particularly b1 integrins [45]. This SCLC cell adhesion-medi-ated drug resistance is also termed cell adhesion-mediated drug resistance (CAM-DR) [49], and can be targeted, for example by b1 integrin-targeting antibodies [48].
The marrow microenvironment, an example of a microenviron-ment into which SCLC cells preferentially metastasize, includes ECM-diffusible growth factors, chemokines and other cytokines, and a heterogeneous population of adherent cells, including mes-enchymal fibroblasts (also called MSCs), osteoblasts, endothe-lial cells and others, and they create distinct marrow niches that normally support hematopoiesis [50]. CXCR4 is highly expressed on SCLC cells [46,51], and its activation induces firm adhesion of SCLC cells to marrow stromal cells [46], which in turn con-fers drug resistance and integrin activation [52], and enhances the invasiveness of lung cancer cells by increasing matrix metallo-proteinase-9 expression [53]. CXCL12-induced integrin activation resulted in an increased adhesion of SCLC cells to fibronectin and collagen [52]. This CXCR4-induced adhesion was mediated by a2, a4, a5 and b1 integrins, and could be inhibited by CXCR4 antagonists. Stromal cells protected SCLC cells from chemother-apy-induced apoptosis, and this protection/CAM-DR could also be antagonized by CXCR4 inhibitors. Therefore, we concluded that the activation of integrins and CXCR4 chemokine receptors co-operate in mediating adhesion and survival signals in SCLC.
Lung cancer stem cellsThere is evidence suggesting that cancer growth is driven by a subpopulation of cells referred to as cancer stem cells (CSCs) that are more tumorigenic than other tumor cells of the same clone. CSCs oftentimes share phenotypic and functional characteristics with their normal counterparts, and the hierarchical organization of the neoplastic clone mimics differentiation and cell turnover as part of homeostasis or tissue repair, nurtured by infrequent stem cells [54,55]. This concept was initially developed in acute myelo-genous leukemia where leukemia-initiating (stem) cells account for approximately 1 in 250,000 leukemia cells in the peripheral blood [56]. Normal and malignant stem cells apparently have a particular affinity for homing to distinct niches: HSCs local-ize to CXCL12+ stromal cells that are in close proximity to the
Figure 2. CXCL12 expression in non-small-cell lung cancer. Sections of (A) lung adenocarcinoma and (B) squamous cell carcinoma samples were stained with anti-CXCL12 monoclonal antibodies (R&D Systems), and counterstained. Photomicrographs were taken at (A) 100× or (B) 200× magnification. (A) CXCL12-positive adenocarcinoma cells are highlighted by the long black arrows, whereas the short black arrows point to tumor vasculature. The black arrowheads point to fibroblasts (carcinoma-associated fibroblasts), and the white arrowheads point towards lymphocytes. (B) CXCL12-positive and -negative squamous cell cancer cells are highlighted by the black (CXCL12-positive) or the white arrows (CXCL12-negative), respectively.

www.expert-reviews.com 625
ReviewPotential of CXCR4 antagonists for the treatment of metastatic lung cancer
marrow vasculature (vascular niche) or the endosteum (osteoblast niche) [12]. Interestingly, brain tumor stem cells also reside in vas-cular niches adjacent to blood vessels [57], suggesting that normal stem cells and CSCs have fundamentally similar requirements towards their niches [58]. Highly tumorigenic lung cancer cells with stem-like features have recently been described as a rare sub- have recently been described as a rare sub-population of cells expressing CD133 [59,60], an antigen expressed by primitive cells of various lineages. Other markers expressed on lung cancer progenitor cells include efflux of the Hoechst dye (side population) cells [61], keratin 14 (an antigen on epithelial progenitor cells) [62], multidrug-resistance transporters and stem cell markers [63,64]. Bertolini et al. recently provided robust evi-dence for a connection between lung cancer progenitor cells and CXCR4. Cisplatin treatment of lung cancer cells in vitro resulted in enrichment of the CD133+ fraction, and a consistent enrich-consistent enrich-ment of a CD133+/CXCR4+ population after cisplatin treatment of tumor xenografts [60], providing the first in vivo evidence for a highly tumorigenic and metastatic subpopulation in lung cancer, characterized by expression of CD133+ together with CXCR4+.
Blocking CXCR4 in lung cancerCXCR4 chemokine receptors are expressed by various solid and hematologic tumors, such as breast cancer, lung cancer, prostate cancer, and acute and chronic leukemias. In general, CXCR4 expression by the tumor cells allows for tumor cell migration and homing to sites where nonmalignant stromal cells express CXCL12. This concept implies that tumor cell metastasis is guided by the expression of chemokine receptors and adhesion molecules on the neoplastic cells, and expression of respective ligands in target tissues [10,65]. Tumor cells exploit this mecha-nism to access microenvironments, such as the marrow, that provide factors that favor their growth and protect them from conventional cytotoxic agents. Lung cancer cells, both primary tumors and cell lines, express high levels of CXCR4 [40,51], and rapidly adhere to MSCs in a CXCR4-dependent fashion [46]. Furthermore, CXCR4 activation induces activation of signaling pathways in lung cancer cells that are linked to cell survival and growth, such as the p44/42 MAPK (ERK-1/2) [46] and the PI3K pathway with phosphorylation of Akt and p70 S6 kinase [51]. MSCs protected SCLC cells from etoposide-induced cell death, and this protective effect was antagonized by the CXCR4 antago-nist TN14003 [52]. CXCL12 also promotes tumor progression by recruiting endothelial progenitor cells to tumors for angiogen-esis [17]. As such, the rationale for CXCR4 antagonists is based on the presence of CAFs/MSCs in the tumor microenvironment, both at primary and metastatic sites. Constitutive secretion of CXCL12 by the stromal cells induces migration and adhesion of SCLC cells to the stromal cells via CXCR4 activation and CXCR4-dependent integrin activation [46,52]. Specific CXCR4 antagonists, such as TN14003, can block stromal cell adhesion, antagonize CAM-DR and thereby sensitize SCLC to drugs such as etoposide [52]. In vivo, we assume that tumor cells that are adherent to stromal cells via CXCR4 could, at least partially, be sensitized to chemotherapy, and therefore CXCR4 antago-nists may help to reduce minimal residual disease and relapses in
SCLC. The enrichment of CXCR4+ cells in chemoresistant CSC populations in vivo [60] provides further strong rationale to target CXCR4 in lung cancer.
CXCR4 antagonistsCXCR4 antagonists were initially developed for treatment of HIV-1 infection. At the time of their discovery in the early 1990s, the mechanism of anti-HIV activity of the CXCR4 antagonists T140 and its analogues [66,67], AMD3100 [68,69] and ALX-4C [70], was unknown. However, rapidly following the discovery of the coreceptor function of CXCR4 for T-tropic HIV-1, the activity of the different CXCR4 antagonists was demonstrated to be due to specific binding of these drugs to CXCR4 [70–72]. In gen-eral, four major classes of CXCR4 antagonists and agonists can be distinguished:
• Nonpeptide CXCR4 antagonists, such as the bicyclam AMD3100;
• Small-peptide CXCR4 antagonists, such as T140 and its analogues (TN14003 and others);
• Antibodies to CXCR4;
• Modified agonists and antagonists for SDF-1/CXCL12, which will be discussed later.
Nonpeptide CXCR4 antagonistsAMD3100 is a bicyclam, in which two cyclam rings are linked through an aromatic bridge. AMD3100 was among a series of bi cyclams that were synthesized in the early 1990s and found to have high anti-HIV activity [73]. AMD3100, a specific antagonist of CXCR4, binds to CXCR4, inhibits CXCL12-induced chemotaxis and GTP-binding, and does not crossreact with other chemokine receptors [74,75]. Initially, AMD3100 was developed at Johnson Matthey (NJ, USA) in collaboration with the Rega Institute for Medical Research (Leuven University, Brussels, Belgium), and therefore this compound was first called JM3100. The name then changed to AMD3100 after a new company, AnorMED (BC, Canada), took over the development. The anti-HIV-1 activity of AMD3100 and the blocking function of AMD3100 on gp120 interaction with CXCR4 during viral entry was the initial focus during the early development of this drug [76]. However, a rapid, transient leukocytosis was noticed during Phase I/II clinical trials of AMD3100 in volunteers and HIV-infected patients, caused by the mobilization of various hematopoietic cells (including CD34+ HSCs) to the blood [77,78]. Overall, safety and pharmacokinetic issues, and a relatively low effect on the viral load, precluded further development of AMD3100 in HIV. Instead, AnorMED explored AMD3100 as a mobilizing agent for HSCs [79], and a sub-sequent series of preclinical and clinical trials demonstrated that AMD3100 alone and in combination with G-CSF is an effective mobilizing agent for HSCs [79–82]. The precise mechanism through which AMD3100 mobilizes HSCs is still under investigation. AMD3100 (recently renamed as Plerixafor or Mozobil™) is now owned by Genzyme (MA, USA) after acquisition of AnorMED by Genzyme in 2006. Plerixafor was approved by the US FDA

Expert Rev. Anticancer Ther. 11(4), (2011)626
Review Burger, Stewart, Wald & Peled
for subcutaneous injection for use in combination with G-CSF to mobilize hematopoietic stem cells to the peripheral blood for col-lection and subsequent autologous transplantation in patients with non-Hodgkin’s lymphoma and multiple myeloma, based upon the data of two randomized Phase III trials [83,84]. Currently, Plerixafor is also used in leukemia patients for leukemia cell mobilization and subsequent targeting by conventional drugs. The activity of Plerixafor to inhibit CXCR4 activation in various tumor models, such as inhibition of CXCL12-induced tumor cell migration and downstream signaling, and activity in animal models has been reported. These studies demonstrate activity of Plerixafor in vitro and in animal models of breast cancer, NSCLC, pancreatic cancer, cholangiocarcinoma, colorectal cancer, malignant melanoma, gli-oma, ovarian cancer, glioblastoma and medulloblastoma (reviewed in [85]). AMD070 is another orally bioavailable small-molecule CXCR4 antagonist with anti-HIV activity [86]. KRH-1636 is an orally available, nonpeptide CXCR4 antagonist that inhibits infec-tion by X4 HIV-1 virus and blocks responses to stimulation with CXCL12, such as calcium mobilization.
Small-peptide antagonist of CXCR4Initially, this group of small-peptide CXCR4 antagonists was discovered by screening naturally occurring peptides for anti-HIV activity. In that process, the self-defense peptides tachyple-sin (from the Japanese horseshoe crab Tachypleus tridentatus) and polyphemusin (from the American horseshoe crab Limulus polyphemus) were discovered and chemically modified, leading to the synthesis of the anti-HIV peptides T22 [67], T134 and T140 [87]. Initially, these compounds were thought to function by inhibiting HIV-1–T-cell fusion or viral uncoating. T22 specifi-cally binds to CXCR4 and blocks CXCR4 receptor regions that are critical for HIV-1 entry and for activation by CXCL12 [72]. T140 is considered the most active CXCR4 peptide antagonist among the initially synthesized peptides, but lacks serum stabil-ity due to cleavage of the C-terminal arginine (Arg). Therefore, C-terminally amidated T140 analogues were developed to over-come serum instability [88], leading to the synthesis of TN14003 and TC14012. Further work revealed the binding regions for T140 within the extracellular domains and regions of the hydro-phobic core of CXCR4, which are distinct from the binding region for AMD3100 [89]. In addition, in a series of experiments to elucidate the mechanism of CXCR4 signaling, it was noticed that T140 decreased autonomous CXCR4 signaling in CXCR4 wild-type or constitutively active CXCR4 mutants, characteriz-ing T140 as an inverse CXCR4 agonist, whereas AMD3100 and ALX40-4C displayed partial agonist activity in this study [90]. This is, however, a controversial issue, because other investigators have not found any (partial) agonistic activity of AMD3100 [74,75].
The efficacy of T140 and its analogues for blocking CXCR4 in vitro and in vivo has been documented in numerous preclinical studies, including in vitro and in vivo models for SCLC, breast cancer and melanoma, rheumatoid arthritis, and stem cell mobi-lization [85]. Other studies explored the activity of these agents in acute and chronic leukemias, multiple myeloma, malignant mela-noma, and pancreatic cancer [85]. Besides these disease-oriented
studies, T140 and its analogues have been used in basic stud-ies exploring the function of CXCR4 in dendritic cell develop-ment [91] and migration [92], B-cell homing and germinal cen-ter positioning within lymphatic tissues [93], and hematopoietic stem cell homing [94]. Currently, the T140 analogue TN14003 (BKT140) is under clinical development for patients with multiple myeloma by Biokine Therapeutics Ltd (Rehovot, Israel).
ALX40-4C is a polypeptide of nine Arg residues that is stabi-lized by terminal protection and the inclusion of d-amino acids. ALX40-4C is a specific CXCR4 antagonist [70], and was the first CXCR4 antagonist clinically used in Phase I and Phase I/II tri-als in HIV patients conducted by the Canadian company Allelix Biopharmaceuticals (ON, Canada) [95]. This peptide is no longer under development, particularly because of formulation diffi-culties, lack of efficacy, and because it is unlikely that an oral formulation of this complex peptide can be produced.
Development antibodies to CXCR4 Neutralizing the interaction between CXCL12 (the ligand for CXCR4) and CXCR4 by using the anti-CXCR4 antibody 12G5 significantly inhibits HIV infection and tumor cell migration in vitro [96]. Furthermore, anti-human CXCR4 or CXCL12 anti-bodies also significantly impair metastasis and progression of non-Hodgkin’s lymphoma, breast, lung and prostate tumors in animal models [40,97,98]. Development of therapeutic monoclonal antibod-ies (mAbs) to CXCR4 is complicated because of the conforma-tional heterogeneity of CXCR4. Using a panel of mAbs to CXCR4, it was found that CXCR4 on both primary and transformed T, B and myeloid cells exhibited considerable conformational hetero-geneity [99]. This heterogeneity of CXCR4 explains the cell type-dependent ability of CXCR4 antibodies to block chemotaxis to its ligand CXCL12. In addition, the mAb most commonly used to study CXCR4 expression, 12G5, recognizes only a sub population of CXCR4 molecules on all primary cell types analyzed. As a result, CXCR4 concentrations on these important cell types have been underestimated to date. The factors responsible for altering CXCR4 conformation are largely unknown. However, CXCR4 can be post-translationally modified by sulfation of its N-terminal tyrosines, and by a chondroitinsulfate chain at serine 18 [100]. This phenomenon may in part explain the difference in confirmation, antibody specificity and function of CXCR4. Altered glycosylation patterns, neoexpression, and underexpression or overexpression of glycans are a hallmark of cancer and may significantly affect the activity of various CXCR4 antagonists in development.
Other CXCR4-targeting agentsCTCE-9908 [101] and CTCE-0214 [102] are peptide analogues of CXCL12 with inhibitory and agonist activity, respectively. CTCE-9908 has received orphan drug status by the FDA for the treat-ment of osteogenic sarcoma. CTCE-9908 decreases growth and adhesion of osteosarcoma cells and the metastatic dissemination of cancer cells in two murine models [103]. CTCE-9908 is devel-oped by Chemokine Therapeutics (BC, Canada). Compounds from the family of chalcones [104] and Spiegelmer technology are under development for neutralization of CXCL12.

www.expert-reviews.com 627
ReviewPotential of CXCR4 antagonists for the treatment of metastatic lung cancer
Another potential approach is RNA-mediated CXCR4 silenc-ing by RNAi. This typically involves siRNA that directs the cleav-age and degradation of complementary mRNA target molecules [105]. In breast cancer cells, siRNA targeting CXCR4 inhibited breast cancer cell migration in vitro [106]. Finally, Jähnichen et al. recently characterized immunoglobulin single variable domains against CXCR4 called nanobodies. Two highly selective monova-lent nanobodies, 238D2 and 238D4, displayed strong antiretro-viral activity against T-cell-tropic and dual-tropic HIV-1 strains, blocked CXCR4 activation by CXCL12, and induced CD34+ stem cell mobilization in Cynomolgus monkeys [107].
ConclusionCXCR4 is a chemokine receptor expressed on lung cancer cells and lung CSCs. CXCR4 mediates lung cancer cell migration and adhesion to stromal cells (CAFs) that are present within the tumor microenvironment. CAFs constitutively secrete the ligand for CXCR4 – CXCL12 – and thereby attract and activate lung cancer cells. Adhesion to stromal cells provides lung cancer cells with growth- and drug-resistance signals that could be responsible for residual disease after conventional chemotherapies for SCLC. Persistence of CD133+/CXCR4+ CSCs after conventional che-motherapy in vivo further emphasizes that CXCR4 is a valid new therapeutic target in lung cancer. Targeting CXCR4 in lung can-cer could help to overcome primary drug resistance (CAM-DR) and eradicate residual disease, and potentially improve response rates to current treatments.
Expert commentaryCXCR4 antagonists provide a new, targeted tool to inhibit lung cancer cell adhesion to stromal cells (CAFs) that secrete CXCL12. Thereby, CXCR4 antagonists can reverse CAM-DR, making lung cancer cells more accessible to conventional drugs. Moreover, this approach can reverse direct CXCR4-derived growth and sur-vival signals and indirect, proangiogenic circuits between CAFs and endothelial progenitors. As such, this strategy may help to overcome residual disease and relapses that account for the high
mortality in lung cancer. Because of the relatively high expression of CXCR4, its high propensity for metastasis to target organs that express CXCL12, and the limited therapeutic options for lung cancer patients, we propose that lung cancer represents a very suitable disease to start investigating the therapeutic activ-ity of CXCR4 antagonists in solid cancers. Currently, CXCR4 antagonists are explored in proof-of-principle studies in leukemia patients in which leukemia cell mobilization can be easily assessed and monitored. However, given the expression and function of CXCR4 receptors in lung cancer, and particularly in lung CSCs, the clinical efficacy of CXCR4 antagonists in lung cancer should be explored.
Five-year viewIncreasing emphasis will be placed over the coming years towards targeting the microenvironment, and not only the tumor cells. CXCR4 and its ligand CXCL12 represent a key receptor–ligand pair involved in the complex crosstalk between tumor cells and their microenvironment in various cancers, including lung can-cer (SCLC and NSCLC). Significant further benefit for lung cancer patients from new chemotherapeutic strategies or chemo-therapy combinations is not expected. Instead, combinations of conventional chemotherapeutic drugs with drugs that target the tumor microenvironment, for example CXCR4 antagonists, could improve response rates and outcome, and should be pursued fur-ther in the treatment of lung cancer. Additional preclinical studies in lung cancer, both in vivo and in vitro studies, will accelerate the development of these new therapeutic concepts and will help define the best drug combinations.
Financial & competing interests disclosureJan A Burger is supported by an ASCO Career Development Award and a CLL Global Research Foundation grant. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
ReferencesPapers of special note have been highlighted as:•ofinterest
1 Zlotnik A, Yoshie O. Chemokines: a new classification system and their role in immunity. Immunity 12(2), 121–127 (2000).
2 Nagasawa T, Kikutani H, Kishimoto T. Molecular cloning and structure of a pre- B- cell growth-stimulating factor. Proc. Natl Acad. Sci. USA 91(6), 2305–2309 (1994).
3 Bleul CC, Farzan M, Choe H et al. The lymphocyte chemoattractant SDF-1 is a ligand for LESTR/fusin and blocks HIV-1 entry. Nature 382(6594), 829–833 (1996).
4 Oberlin E, Amara A, Bachelerie F et al. The CXC chemokine SDF-1 is the ligand for LESTR/fusin and prevents infection by T-cell-line-adapted HIV-1 [published erratum appears in Nature 1996 Nov 21;384(6606):288]. Nature 382(6594), 833–835 (1996).
Key issues
• Lung cancer cells express CXCR4 chemokine receptors.
• These receptors are involved in lung cancer cell dissemination and adhesion to stromal cells that express the CXCR4 ligand, CXCL12.
• CXCL12-expressing stromal cells, also called carcinoma-associated fibroblasts, promote tumor progression via direct (promotion of growth and drug-resistance) and indirect effects (angiogenesis).
• Lung cancer cells can also express CXCL12, and can thereby promote tumor progression in an autocrine and paracrine fashion.
• CXCR4 antagonists can block activation of lung cancer cells via CXCL12, and therefore represent a new, targeted approach towards blocking tumor-promoting signals within the lung cancer microenvironment.

Expert Rev. Anticancer Ther. 11(4), (2011)628
Review Burger, Stewart, Wald & Peled
5 Nagasawa T, Hirota S, Tachibana K et al. Defects of B-cell lymphopoiesis and bone-marrow myelopoiesis in mice lacking the CXC chemokine PBSF/SDF-1. Nature 382(6592), 635–638 (1996).
6 Tachibana K, Hirota S, Iizasa H et al. The chemokine receptor CXCR4 is essential for vascularization of the gastrointestinal tract [see comments]. Nature 393(6685), 591–594 (1998).
7 Boldajipour B, Mahabaleshwar H, Kardash E et al. Control of chemokine-guided cell migration by ligand sequestration. Cell 132(3), 463–473 (2008).
8 Sierro F, Biben C, Martinez-Munoz L et al. Disrupted cardiac development but normal hematopoiesis in mice deficient in the second CXCL12/SDF-1 receptor, CXCR7. Proc. Natl Acad. Sci. USA 104(37), 14759–14764 (2007).
9 Hernandez PA, Gorlin RJ, Lukens JN et al. Mutations in the chemokine receptor gene CXCR4 are associated with WHIM syndrome, a combined immunodeficiency disease. Nat. Genet. 34(1), 70–74 (2003).
10 Muller A, Homey B, Soto H et al. Involvement of chemokine receptors in breast cancer metastasis. Nature 410(6824), 50–56 (2001).
• FirstpapertodescribetheCXCL4–CXCR12axisasakeyplayerinmetastasisofsolidtumors(breastcancer).
11 Peled A, Petit I, Kollet O et al. Dependence of human stem cell engraftment and repopulation of NOD/SCID mice on CXCR4. Science (New York, NY) 283(5403), 845–848 (1999).
12 Sugiyama T, Kohara H, Noda M, Nagasawa T. Maintenance of the hematopoietic stem cell pool by CXCL12–CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity 25(6), 977–988 (2006).
13 Sipkins DA, Wei X, Wu JW et al. In vivo imaging of specialized bone marrow endothelial microdomains for tumour engraftment. Nature 435(7044), 969–973 (2005).
14 Wright DE, Bowman EP, Wagers AJ, Butcher EC, Weissman IL. Hematopoietic stem cells are uniquely selective in their migratory response to chemokines. J. Exp. Med. 195(9), 1145–1154 (2002).
15 Cashen AF, Nervi B, Dipersio J. AMD3100: CXCR4 antagonist and rapid stem cell-mobilizing agent. Future Oncol. 3(1), 19–27 (2007).
16 Abraham M, Biyder K, Begin M et al. Enhanced unique pattern of hematopoietic cell mobilization induced by the CXCR4 antagonist 4F-benzoyl-TN14003. Stem Cells 25(9), 2158–2166 (2007).
17 Orimo A, Gupta PB, Sgroi DC et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell 121(3), 335–348 (2005).
• Definedthetumor-promotingroleofcancer-associatedfibroblasts(CAFs)andthekeyroleoftheCXCL4–CXCR12axisinthiscrosstalk.Inaddition,itdefinedthatCAF-derivedCXCL12playsmultiplerolesintumorprogressionthroughdirectandindirectmechanisms.
18 Moore KA, Lemischka IR. Stem cells and their niches. Science (New York, NY) 311(5769), 1880–1885 (2006).
19 Morrison SJ, Spradling AC. Stem cells and niches: mechanisms that promote stem cell maintenance throughout life. Cell 132(4), 598–611 (2008).
20 Laird DJ, Von Andrian UH, Wagers AJ. Stem cell trafficking in tissue development, growth, and disease. Cell 132(4), 612–630 (2008).
21 De Visser KE, Coussens LM. The inflammatory tumor microenvironment and its impact on cancer development. Contrib. Microbiol. 13, 118–137 (2006).
22 Raman D, Baugher PJ, Thu YM, Richmond A. Role of chemokines in tumor growth. Cancer Lett. 256(2), 137–165 (2007).
23 Ben-Baruch A. The multifaceted roles of chemokines in malignancy. Cancer Metas. Rev. 25(3), 357–371 (2006).
24 Vicari AP, Caux C. Chemokines in cancer. Cytokine Growth Factor Rev. 13(2), 143–154 (2002).
25 Balkwill F. Cancer and the chemokine network. Nat. Rev. 4(7), 540–550 (2004).
26 Kalluri R, Zeisberg M. Fibroblasts in cancer. Nat. Rev. 6(5), 392–401 (2006).
27 Orimo A, Weinberg RA. Stromal fibroblasts in cancer: a novel tumor-promoting cell type. Cell Cycle 5(15), 1597–1601 (2006).
28 Liyanage UK, Moore TT, Joo HG et al. Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J. Immunol. 169(5), 2756–2761 (2002).
29 Murphy PM. Chemokines and the molecular basis of cancer metastasis. N. Engl. J. Med. 345(11), 833–835 (2001).
30 Allinen M, Beroukhim R, Cai L et al. Molecular characterization of the tumor microenvironment in breast cancer. Cancer Cell 6(1), 17–32 (2004).
31 Lewis CE, Pollard JW. Distinct role of macrophages in different tumor microenvironments. Cancer Res. 66(2), 605–612 (2006).
32 Kioi M, Vogel H, Schultz G, Hoffman RM, Harsh GR, Brown JM. Inhibition of vasculogenesis, but not angiogenesis, prevents the recurrence of glioblastoma after irradiation in mice. J. Clin. Investig. 120(3), 694–705 (2010).
33 Burger JA, Kipps TJ. CXCR4: a key receptor in the crosstalk between tumor cells and their microenvironment. Blood 107(5), 1761–1767 (2006).
• ExtensivereviewofthefunctionofCXCR4incancerbiologyanditspotentialroleasatherapeutictarget.
34 Grunewald M, Avraham I, Dor Y et al. VEGF-induced adult neovascularization: recruitment, retention, and role of accessory cells. Cell 124(1), 175–189 (2006).
35 Sandler A, Yi J, Dahlberg S et al. Treatment outcomes by tumor histology in Eastern Cooperative Group Study E4599 of bevacizumab with paclitaxel/carboplatin for advanced non-small cell lung cancer. J. Thorac. Oncol. 5(9), 1416–1423 (2010).
36 Li YM, Pan Y, Wei Y et al. Upregulation of CXCR4 is essential for HER2-mediated tumor metastasis. Cancer Cell 6(5), 459–469 (2004).
37 Su L, Zhang J, Xu H et al. Differential expression of CXCR4 is associated with the metastatic potential of human non-small cell lung cancer cells. Clin. Cancer Res. 11(23), 8273–8280 (2005).
38 Spano JP, Andre F, Morat L et al. Chemokine receptor CXCR4 and early-stage non-small cell lung cancer: pattern of expression and correlation with outcome. Ann. Oncol. 15(4), 613–617 (2004).
39 Wagner PL, Hyjek E, Vazquez MF et al. CXCL12 and CXCR4 in adenocarcinoma of the lung: association with metastasis and survival. J. Thorac. Cardiovasc. Surg. 137(3), 615–621 (2009).
40 Phillips RJ, Burdick MD, Lutz M, Belperio JA, Keane MP, Strieter RM. The stromal derived factor-1/CXCL12–CXC chemokine receptor 4 biological axis in non-small cell lung cancer metastases. Am. J. Respir. Crit. Care Med. 167(12), 1676–1686 (2003).

www.expert-reviews.com 629
ReviewPotential of CXCR4 antagonists for the treatment of metastatic lung cancer
41 Oonakahara K, Matsuyama W, Higashimoto I, Kawabata M, Arimura K, Osame M. Stromal-derived factor-1a/CXCL12–CXCR 4 axis is involved in the dissemination of NSCLC cells into pleural space. Am. J. Respir. Cell. Mol. Biol. 30(5), 671–677 (2004).
42 Chen G, Wang Z, Liu XY, Liu FY. High-level CXCR4 expression correlates with brain-specific metastasis of non-small cell lung cancer. World J. Surg. 35(1), 56–61 (2011).
43 Wald O, Izhar U, Amir G et al. CD4+CXCR4highCD69+ T cells accumulate in lung adenocarcinoma. J. Immunol. 177(10), 6983–6990 (2006).
44 Simon Gr, Turrisi A. Management of small cell lung cancer: ACCP evidence-based clinical practice guidelines (2nd Edition). Chest 132(3 Suppl.), 324S–339S (2007).
45 Sethi T, Rintoul RC, Moore SM et al. Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: a mechanism for small cell lung cancer growth and drug resistance in vivo. Nat. Med. 5(6), 662–668 (1999).
• Introducestheconceptofstroma-mediateddrugresistanceinlungcancer.
46 Burger M, Glodek A, Hartmann T et al. Functional expression of CXCR4 (CD184) on small-cell lung cancer cells mediates migration, integrin activation, and adhesion to stromal cells. Oncogene 22(50), 8093–8101 (2003).
• HighlightsexpressionandfunctionofCXCR4onsmall-celllungcancer(SCLC)cellsandexplorestheactivityofCXCR4antagonistsfordisruptingSCLC–stromainteractions.
47 Nicholson SA, Beasley MB, Brambilla E et al. Small cell lung carcinoma (SCLC): a clinicopathologic study of 100 cases with surgical specimens. Am. J. Surg. Pathol. 26(9), 1184–1197 (2002).
48 Hodkinson PS, Mackinnon AC, Sethi T. Extracellular matrix regulation of drug resistance in small-cell lung cancer. Int. J. Radiat. Biol. 83(11–12), 733–741 (2007).
49 Damiano JS, Cress AE, Hazlehurst LA, Shtil AA, Dalton WS. Cell adhesion mediated drug resistance (CAM-DR): role of integrins and resistance to apoptosis in human myeloma cell lines. Blood 93(5), 1658–1667 (1999).
50 Nagasawa T. Microenvironmental niches in the bone marrow required for B-cell development. Nat. Rev. Immunol. 6(2), 107–116 (2006).
51 Kijima T, Maulik G, Ma PC et al. Regulation of cellular proliferation, cytoskeletal function, and signal transduction through CXCR4 and c-Kit in small cell lung cancer cells. Cancer Res. 62(21), 6304–6311 (2002).
52 Hartmann TN, Burger JA, Glodek A, Fujii N, Burger M. CXCR4 chemokine receptor and integrin signaling co-operate in mediating adhesion and chemoresistance in small cell lung cancer (SCLC) cells. Oncogene 24(27), 4462–4471 (2005).
53 Tang CH, Tan TW, Fu WM, Yang RS. Involvement of matrix metalloproteinase-9 in stromal cell-derived factor-1/CXCR4 pathway of lung cancer metastasis. Carcinogenesis 29(1), 35–43 (2008).
54 Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat. Med. 3(7), 730–737 (1997).
55 Lessard J, Sauvageau G. BMI-1 determines the proliferative capacity of normal and leukaemic stem cells. Nature 423(6937), 255–260 (2003).
56 Lapidot T, Sirard C, Vormoor J et al. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 367(6464), 645–648 (1994).
57 Calabrese C, Poppleton H, Kocak M et al. A perivascular niche for brain tumor stem cells. Cancer Cell 11(1), 69–82 (2007).
58 Yang Zj, Wechsler-Reya Rj. Hit ‘em where they live: targeting the cancer stem cell niche. Cancer Cell 11(1), 3–5 (2007).
59 Eramo A, Lotti F, Sette G et al. Identification and expansion of the tumorigenic lung cancer stem cell population. Cell Death Differ. 15(3), 504–514 (2008).
60 Bertolini G, Roz L, Perego P et al. Highly tumorigenic lung cancer CD133+ cells display stem-like features and are spared by cisplatin treatment. Proc. Natl Acad. Sci. USA 106(38), 16281–16286 (2009).
61 Salcido CD, Larochelle A, Taylor BJ, Dunbar CE, Varticovski L. Molecular characterisation of side population cells with cancer stem cell-like characteristics in small-cell lung cancer. Br. J. Cancer 102(11), 1636–1644 (2010).
62 Ooi AT, Mah V, Nickerson DW et al. Presence of a putative tumor-initiating progenitor cell population predicts poor prognosis in smokers with non-small cell lung cancer. Cancer Res. 70(16), 6639–6648 (2010).
63 Donnenberg VS, Luketich JD, Landreneau RJ, Deloia JA, Basse P, Donnenberg AD. Tumorigenic epithelial stem cells and
their normal counterparts. Ernst Schering Found. Symp. Proc. 5, 245–263 (2006).
64 Levina V, Marrangoni AM, Demarco R, Gorelik E, Lokshin AE. Drug-selected human lung cancer stem cells: cytokine network, tumorigenic and metastatic properties. PLoS ONE 3(8), e3077 (2008).
65 Liotta LA. An attractive force in metastasis. Nature 410(6824), 24–25 (2001).
66 Nakashima H, Masuda M, Murakami T et al. Anti-human immunodeficiency virus activity of a novel synthetic peptide, T22 ([Tyr-5,12, Lys-7]polyphemusin II): a possible inhibitor of virus-cell fusion. Antimicrob. Agents Chemother. 36(6), 1249–1255 (1992).
67 Masuda M, Nakashima H, Ueda T et al. A novel anti-HIV synthetic peptide, T-22 ([Tyr5,12,Lys7]-polyphemusin II). Biochem. Biophys. Res. Commun. 189(2), 845–850 (1992).
68 De Clercq E, Yamamoto N, Pauwels R et al. Potent and selective inhibition of human immunodeficiency virus (HIV)-1 and HIV-2 replication by a class of bicyclams interacting with a viral uncoating event. Proc. Natl Acad. Sci. USA 89(12), 5286–5290 (1992).
69 De Clercq E. The AMD3100 story: the path to the discovery of a stem cell mobilizer (Mozobil). Biochem. Pharmacol. 77(11), 1655–1664 (2009).
70 Doranz BJ, Grovit-Ferbas K, Sharron MP et al. A small-molecule inhibitor directed against the chemokine receptor CXCR4 prevents its use as an HIV-1 coreceptor. J. Exp. Med. 186(8), 1395–1400 (1997).
71 Schols D, Struyf S, Van Damme J, Este JA, Henson G, De Clercq E. Inhibition of T-tropic HIV strains by selective antagonization of the chemokine receptor CXCR4. J. Exp. Med. 186(8), 1383–1388 (1997).
72 Murakami T, Nakajima T, Koyanagi Y et al. A small molecule CXCR4 inhibitor that blocks T cell line-tropic HIV-1 infection. J. Exp. Med. 186(8), 1389–1393 (1997).
73 De Clercq E. The bicyclam AMD3100 story. Nat. Rev. Drug Discov. 2(7), 581–587 (2003).
74 Hatse S, Princen K, Bridger G, De Clercq E, Schols D. Chemokine receptor inhibition by AMD3100 is strictly confined to CXCR4. FEBS Lett. 527(1–3), 255–262 (2002).

Expert Rev. Anticancer Ther. 11(4), (2011)630
Review Burger, Stewart, Wald & Peled
75 Fricker SP, Anastassov V, Cox J et al. Characterization of the molecular pharmacology of AMD3100: a specific antagonist of the G-protein coupled chemokine receptor, CXCR4. Biochem. Pharmacol. 72(5), 588–596 (2006).
76 Donzella GA, Schols D, Lin SW et al. AMD3100, a small molecule inhibitor of HIV-1 entry via the CXCR4 co-receptor. Nat. Med. 4(1), 72–77 (1998).
77 Hendrix CW, Flexner C, Macfarland RT et al. Pharmacokinetics and safety of AMD-3100, a novel antagonist of the CXCR-4 chemokine receptor, in human volunteers. Antimicrob. Agents Chemother. 44(6), 1667–1673 (2000).
78 Hendrix CW, Collier AC, Lederman MM et al. Safety, pharmacokinetics, and antiviral activity of AMD3100, a selective CXCR4 receptor inhibitor, in HIV-1 infection. J. Acquir. Immune Defic. Syndr. 37(2), 1253–1262 (2004).
79 Liles WC, Broxmeyer HE, Rodger E et al. Mobilization of hematopoietic progenitor cells in healthy volunteers by AMD3100, a CXCR4 antagonist. Blood 102(8), 2728–2730 (2003).
80 Devine SM, Flomenberg N, Vesole DH et al. Rapid mobilization of CD34+ cells following administration of the CXCR4 antagonist AMD3100 to patients with multiple myeloma and non-Hodgkin’s lymphoma. J. Clin. Oncol. 22(6), 1095–1102 (2004).
81 Devine SM, Vij R, Rettig M et al. Rapid mobilization of functional donor hematopoietic cells without G-CSF using AMD3100, an antagonist of the CXCR4/SDF-1 interaction. Blood 112(4), 990–998 (2008).
82 De Clercq E. Recent advances on the use of the CXCR4 antagonist plerixafor (AMD3100, Mozobil) and potential of other CXCR4 antagonists as stem cell mobilizers. Pharmacol. Therap. 128(3), 509–518 (2010).
83 Dipersio JF, Stadtmauer EA, Nademanee A et al. Plerixafor and G-CSF versus placebo and G-CSF to mobilize hematopoietic stem cells for autologous stem cell transplantation in patients with multiple myeloma. Blood 113(23), 5720–5726 (2009).
84 Dipersio JF, Uy GL, Yasothan U, Kirkpatrick P. Plerixafor. Nat. Rev. Drug Discov. 8(2), 105–106 (2009).
85 Burger JA, Peled A. CXCR4 antagonists: targeting the microenvironment in leukemia and other cancers. Leukemia 23(1), 43–52 (2009).
86 Stone ND, Dunaway SB, Flexner C et al. Multiple-dose escalation study of the safety, pharmacokinetics, and biologic activity of oral AMD070, a selective CXCR4 receptor inhibitor, in human subjects. Antimicrob. Agents Chemother. 51(7), 2351–2358 (2007).
87 Tamamura H, Xu Y, Hattori T et al. A low-molecular-weight inhibitor against the chemokine receptor CXCR4: a strong anti-HIV peptide T140. Biochem. Biophys. Res. Commun. 253(3), 877–882 (1998).
88 Tamamura H, Omagari A, Hiramatsu K et al. Development of specific CXCR4 inhibitors possessing high selectivity indexes as well as complete stability in serum based on an anti-HIV peptide T140. Bioorg. Med. Chem. Lett. 11(14), 1897–1902 (2001).
89 Trent JO, Wang ZX, Murray JL et al. Lipid bilayer simulations of CXCR4 with inverse agonists and weak partial agonists. J. Biol. Chem. 278(47), 47136–47144 (2003).
90 Zhang WB, Navenot JM, Haribabu B et al. A point mutation that confers constitutive activity to CXCR4 reveals that T140 is an inverse agonist and that AMD3100 and ALX40-4C are weak partial agonists. J. Biol. Chem. 277(27), 24515–24521 (2002).
91 Kohara H, Omatsu Y, Sugiyama T, Noda M, Fujii N, Nagasawa T. Development of plasmacytoid dendritic cells in bone marrow stromal cell niches requires CXCL12–CXCR4 chemokine signaling. Blood 110(13), 4153–4160 (2007).
92 Kabashima K, Shiraishi N, Sugita K et al. CXCL12–CXCR4 engagement is required for migration of cutaneous dendritic cells. Am. J. Pathol. 171(4), 1249–1257 (2007).
93 Allen CD, Ansel KM, Low C et al. Germinal center dark and light zone organization is mediated by CXCR4 and CXCR5. Nat. Immunol. 5(9), 943–952 (2004).
94 Petit I, Szyper-Kravitz M, Nagler A et al. G-CSF induces stem cell mobilization by decreasing bone marrow SDF-1 and up-regulating CXCR4. Nat. Immunol. 3(7), 687–694 (2002).
95 Doranz BJ, Filion LG, Diaz-Mitoma F et al. Safe use of the CXCR4 inhibitor ALX40–4C in humans. AIDS Res. Hum. Retroviruses 17(6), 475–486 (2001).
96 Endres MJ, Clapham PR, Marsh M et al. CD4-independent infection by HIV-2 is mediated by fusin/CXCR4. Cell 87(4), 745–756 (1996).
97 Bertolini F, Dell’agnola C, Mancuso P et al. CXCR4 neutralization, a novel therapeutic approach for non-Hodgkin’s lymphoma. Cancer Res. 62(11), 3106–3112 (2002).
98 Engl T, Relja B, Marian D et al. CXCR4 chemokine receptor mediates prostate tumor cell adhesion through a5 and b3 integrins. Neoplasia 8(4), 290–301 (2006).
99 Baribaud F, Edwards TG, Sharron M et al. Antigenically distinct conformations of CXCR4. J. Virol. 75(19), 8957–8967 (2001).
100 Farzan M, Babcock GJ, Vasilieva N et al. The role of post-translational modifications of the CXCR4 amino terminus in stromal-derived factor 1 a association and HIV-1 entry. J. Biol. Chem. 277(33), 29484–29489 (2002).
101 Wong D, Korz W. Translating an antagonist of chemokine receptor CXCR4: from bench to bedside. Clin. Cancer Res. 14(24), 7975–7980 (2008).
102 Perez LE, Alpdogan O, Shieh JH et al. Increased plasma levels of stromal-derived factor-1 (SDF-1/CXCL12) enhance human thrombopoiesis and mobilize human colony-forming cells (CFC) in NOD/SCID mice. Exp. Hematol. 32(3), 300–307 (2004).
103 Kim SY, Lee CH, Midura BV et al. Inhibition of the CXCR4/CXCL12 chemokine pathway reduces the development of murine pulmonary metastases. Clin. Exp. Metastasis 25(3), 201–211 (2008).
104 Hachet-Haas M, Balabanian K, Rohmer F et al. Small neutralizing molecules to inhibit actions of the chemokine CXCL12. J. Biol. Chem. 283(34), 23189–23199 (2008).
105 Kim DH, Rossi JJ. Strategies for silencing human disease using RNA interference. Nat. Rev. Genet. 8(3), 173–184 (2007).
106 Chen Y, Stamatoyannopoulos G, Song CZ. Down-regulation of CXCR4 by inducible small interfering RNA inhibits breast cancer cell invasion in vitro. Cancer Res. 63(16), 4801–4804 (2003).
107 Jähnichen S, Blanchetot C, Maussang D et al. CXCR4 nanobodies (VHH-based single variable domains) potently inhibit chemotaxis and HIV-1 replication and mobilize stem cells. Proc. Natl Acad. Sci. USA 107(47), 20565–20570 (2010).


![Aquaporins as diagnostic and therapeutic targets in cancer ...cancer, Laryngeal cancer, Lung cancer [43], Nasopharyngeal cancer, Ovarian cancer [37] Tumor grade, prognosis, tumor angiogenesis,](https://static.fdocuments.in/doc/165x107/5ffa8fafa51a2a21db58011f/aquaporins-as-diagnostic-and-therapeutic-targets-in-cancer-cancer-laryngeal.jpg)








![[Ghiduri][Cancer]Gastric Cancer](https://static.fdocuments.in/doc/165x107/55cf9399550346f57b9de771/ghiduricancergastric-cancer.jpg)