Postural management for people with MS
-
Upload
ms-trust -
Category
Health & Medicine
-
view
119 -
download
3
Transcript of Postural management for people with MS
POSTURAL MANAGEMENT FOR
PEOPLE WITH MS
Wendy HendrieSpecialist physiotherapist in MS
Norwich MS Centre
Posture…
•is the shape and position our body adopts and is constantly changing
•provides balance and stability which is vital before we can function
•is a learned skill
Posture is complex•Adapting to the surface your body is resting on
•Organising body segments when sitting, lying and standing
•Being able to adjust quickly e.g. to the disturbance of moving a limb
•Being able to position the body for movement
Posture is complex
•Changing position•Taking the weight off limbs in order to move them – e.g. walking
•Allowing muscles to act by providing a fixed point to act against
•Keeping stable in order to function - balance
What is ‘good’ posture?•Stable base - supported and balanced
•A position from which we function effectively
•Uses as little energy as possible
•Causes the least damage to the body
What is ‘bad’ posture?
•Any position that causes damage to the body
•Asymmetrical postures can often cause the most damage
•Damage often occurs when bad postures are held for a long time
In people with MS…•Things go wrong when automatic andvoluntary postural control is lost
•Compensatory strategies maximise balance, stability and function
•Secondary complications inevitably arise
Secondary complications•Pain•Pressure•Contractures•Breathing difficulties•Speech and swallowing difficulties•Digestion problems•Inability to function effectively•Decreased quality of life
Why manage posture?
•Improve function
•Increase quality of life for pwMS and family/carers
•To minimise or avoid secondary complications
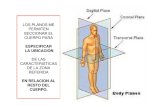
Assessment
•Subjective (rarely about posture!) •Pain•Pressure ulcer•Spasms•Speech or swallowing problems•Breathing difficulties•Handling or positioning problems•ADL problems
Assessment
•Objective•ROM•Active movement•Functional independence•Tissue damage•Infections – urinary/respiratory•Pain•Preferred posture
The ‘preferred’ posture
•The posture which the body customarily adopts when placed in any position.
•On release of passive correction the posture reverts to the original attitude indicating the existence of tissue adaptation.
Pelvis position – the key stone
Posterior pelvic tilt
Pelvic rotation – right ASIS forward
Pelvic obliquity – higher on left
Measure between the coracoid process and the ASIS – less useful if double curvature present in spine
Assessing sitting posture
•Lay the person on a flat bed
•Look at the preferred posture
•If the body is able to lay completely straight, a symmetrical posture can be achieved in sitting
Fixed postures
•The aim is to adapt the surface so that no further deformity can take place
•Referral to wheelchair service
•Consider Botox, antispasticity medication change
Goals
•Emphasis on function
•Aim for dynamic and/or static success
•Patient/family/carer led and agreed
Posture in lying
•Most damage done in this position•Keep body as straight and in-line as possible, hips in line with knees and shoulders and avoid twisting in the middle
•Keep knees apart and supported•Support arms and move them away from the sides of the body if possible
Summary•Often a compromise between posture and function
•Try to make people feel stable and balanced
•Change position regularly if possible
•Most damage done in lying position
Summary
•Pelvis is the keystone – correct pelvis first
•Dynamic and static success is good
•‘Sell’ the concept of good posture and ensure that people know what to do
24/7 management•Meeting of experts
•Care Plans that describe the correct positions
•Use digital cameras
•Family /carer awareness and training
What’s the point?
•Function and independence
•Prevention of unnecessary secondary complications which increase disability
•To improve quality of life for pwMS their family and carers