Posterior reversible encephalopathy syndrome
-
Upload
prashant-makhija -
Category
Health & Medicine
-
view
399 -
download
3
Transcript of Posterior reversible encephalopathy syndrome

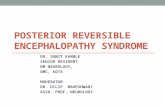
POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME
(PRES)
Dr Prashant Makhija

HISTORICAL BACKGROUND
In 1897, Vaquez and Nobecourt pointed out the correlation of toxemia of pregnancy and HTN
In1928, Oppenheimer and Fishberg introduced the term hypertensive encephalopathy
In 1996, Hinchey and colleagues first described the clinical condition- as reversible posterior leukoencephalopathy( RPLE)
1. Semin Neurol 2011;31:202–215
2. Crit Care & Shock (2009) 12:135-143

POSTERIOR REVERSIBLE ENCEPHALOPATHY
Is a Clinicoradiological entity Clinical features - headache, mental confusion, seizures and
visual disturbances Radiological features- pattern of bilateral white matter
abnormalities in the posterior regions of both cerebral hemispheres
Other terms reversible posterior leukoencephalopathy reversible posterior cerebral edema syndrome reversible occipital parietal encephalopathy “potentially reversible encephalopathy syndrome”
J Intensive Care Med 2012 27: 11
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

Dynamics of Cerebral Blood Flow
The normal cerebral blood flow ~ 50 ml/100gm/min
Cerebral blood flow varies directly with the cerebral perfusion pressure and inversely with the cerebral vascular resistance
CPP = MAP – CVP CBF=(MAP – CVP) / CVR
Cerebral resistance arterioles respond to the MAP rises with compensatory vasoconstriction that maintains a relatively constant cerebral blood flow
There is relative paucity of sympathetic innervation in posterior circulation
Semin Neurol 2011;31:202–215

Wide range of mean arterial pressures (MAP; 50 mm Hg to 150 mm Hg)
With chronic HTN, the resistance arterioles undergo proliferation of the muscular media adapting to the chronically high perfusion pressures
This results in a shift of the autoregulation curve to the right
This adaptation allows the maintenance of normal CBF at higher mean arterial pressures
The shift also limits vascular dilation and makes the CBF vulnerable to rapid lowering of the MAP
Semin Neurol 2011;31:202–215

NORMAL CEREBRAL AUTOREGULATION
Semin Neurol 2011;31:202–215

DYNAMICS OF CBF IN PTS WITH CHRONIC HTN
Semin Neurol 2011;31:202–215

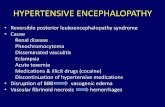
PATHOPHYSIOLOGY
Pathophysiology of PRES is poorly understood
Disruption of BBB → Vasogenic Edema
Cerebral Hyperperfusion- breakdown of Cerebral autoregulation due to rapid ↑ in BP
Cerebral Hypoperfusion- endothelial dysfunction
Pract Neurol 2011; 11: 136–144
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

Pathogenesis of PRES

COMORBID CONDITIONS/TRIGGERS
Pregnancy-related conditions Eclampsia Hydatidiform mole
Major medical illness Organ transplantation Thrombotic thrombocytopenic purpura Henoch-Scho¨nlein purpura Autoimmune inflammatory disease: systemic lupus, scleroderma,
Wegener’s, periarteritis nodosa Sepsis/systemic inflammatory response syndrome/multiple organ
failure Alcohol and drug withdrawal Hypomagnesemia, hypercalcemia, hypocholesterolemia
Semin Neurol 2011;31:202–215

Neurologic illness Guillain-Barre´ ’s syndrome Spinal cord injury with autonomic dysreflexia Head injury
Drugs that cause endothelial dysfunction Immunosuppressant agents - Cyclosporine A Chemotherapeutic agents, especially high-dose multidrug -
Tacrolimus (FK506), Cisplatin, Gemcitabine, Bevacizumab Erythropoietin Blood transfusion Indinavir Cytarabine IVIg
Semin Neurol 2011;31:202–215

CLINICAL FEATURES
Epidemiology Age- 4 to 90 years, most cases occur in young to middle-aged adults, the mean age
ranging across case series from 39 to 47 years Female predominance
Consciousness impairment severity from confusion, somnolence, and lethargy to coma reported in 13 % to 90 % of cases
Seizure Up to 92 % of cases rarely focal (23 %-28 %) ,Secondary generalized seizures are common (53–62 %) Status epilepticus, has been described in 3 % to 13 % of patients
Annual Update in Intensive Care and Emergency Medicine 2011

Headaches and nausea/vomiting were reported in 26 % to 53 % of patients
Visual abnormalities found in 26 % to 67 % of patients blurred vision (7 % -18 %) visual neglect (4 %-27 %) homonymous hemianopsia (4 % -20 %) visual hallucinations (3 % -5 %) cortical blindness (8 %-33 %)
Focal neurological signs None to 3-17% cases
Annual Update in Intensive Care and Emergency Medicine 2011

Distribution of clinical features in cohort studies of PRES
Clinical Features
Hinchey1996 (N=13)
Bartynski2007(N=136)
McKinney2007(N=76)
Lee2008(N=36)
Burnett2010(N=79)
Consciousnessimpairment
10 (67 %) 39 (26 %) 10 (13 %) 34 (94 %) 76 (90 %)
Seizure 11 (73 %) 97 (71 %) 58 (76 %) 33 (92 %) 56 (70 %)
Headaches 8 (53 %) 39 (26 %) 3 (4 %) 19 (53 %) 26 (31 %)
Visual abnormalities
10 (67 %) 39 (26 %) 3 (4 %) 13 (36 %) 24 (29 %)
Nausea/vomiting
8 (53 %) 39 (26 %) NR NR NR
Focal neurological signs
NR NR 2 (3 %) 1 (3 %) 14 (17 %)
Acute hypertension
12 (80 %) 91 (67 %) NR NR 62 (78 %)
Annual Update in Intensive Care and Emergency Medicine 2011

RADIOLOGICAL CHARACTERISTICS OF PRES
1. Holohemispheric watershed pattern (23 %) watershed zone between the anterior and posterior cerebral arteries,
on the one hand, and the middle cerebral artery, on the other confluent vasogenic edema extends through the frontal, parietal,
and occipital lobes
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

2. Superior frontal sulcus pattern (27 %) Patchy edema predominates in the frontal lobes along the superior
frontal sulci parietal and occipital lobes are variably involved
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

3. Dominant parietal-occipital pattern (22 %) previously thought to be typical of PRES posterior part of the parietal and occipital lobes is predominantly
involved
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

4. Partial / asymmetric expression of the primary patterns (28 %) absence of involvement of either the parietal or the occipital lobes
and asymmetric abnormalities in the affected parietal or occipital lobes
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

Complications diagnosed radiologically
Cerebral ischemia Reported to occur in 10 to 23% of pts. non-reversible damage associated with adverse outcomes
Cerebral herniation Posterior edema, particularly when located in the cerebellum and
brainstem, may cause transtentorial cerebral herniation
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

Cerebral hemorrhage uncommon in PRES- 5 to 17% of pts. parenchymal hematoma, subarachnoid hemorrhage, and focal
intraparenchymal hemorrhage measuring less than 5mm in diameter
more common among patients with allogeneic bone marrow transplantation or anticoagulant treatment
S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011

Radiological features in cohort studies of PRESRadiological Features
Hinchey1996 (N=13)
Casey2000N = 16
Bartynski2007(N=136
McKinney2007(N=76)
Lee2008(N=36)
Burnett2010(N=79)
Bilateral 15 (100 %) 11 (69 %) > 98 (> 72 %)
NR 36(100 %)
NR
Asymmetric 10 (67 %) NR 21 (15 %) 2 (3 %) NR NR
Confluent NR 2 (13 %) 31 (23 %) 44 (58 %) 2 (13 %) 12 (16 %)
Gray matter 4 (27 %) NR NR 22 (29 %) 16 (44 %) NR
Posterior > anterior
14 (93 %) 15 (94 %) 30 (22 %) NR NR NR
Occipital 14 (93 %) NR 134 (99 %) 75 (99 %) NR NR
Parietal 13 (87 %) 8 (50 %) 134 (99 %) 75 (99 %) NR 50 (67 %)
Frontal 7 (47 %) 14 (88 %) 93 (68 %) 60 (89 %) 22 (61 %) 61 (81 %)
Temporal 9 (60 %) 16 (100 %) 55 (40 %) 52 (68 %) NR 62 (83 %)
Brainstem 2 (13 %) NR 17 (13 %) 14 (18 %) 21 (58 %) NR
Cerebellum 1 (7 %) NR 41 (30 %) 26 (34 %) 21 (58 %) NR
Basal ganglia 1 (7 %) 3 (19 %) 19 (14 %) 9 (12 %) NR NR

DIFFERENTIAL DIAGNOSIS
Posterior circulation stroke usually no seizures infarction shows(cytotoxic oedema) hyperintensity on DWI with
low signal on the corresponding ADC map while, in contrast, PRES (vasogenic edema) shows the exact opposite on ADC mapping
Pract Neurol 2011; 11: 136–144

Reversible cerebral vasoconstriction syndrome Thunderclap headache PRES quickly progresses over a few hours, complications may
occur for several days with the RCVS Imaging PRES- Bilateral parieto-occipital lesions on MRI, typical
for PRES Imaging RCVS- classic pattern of ‘string of beads’ on
Angiography, at least two narrowings per artery on two different cerebral arteries at brain magnetic resonance angiography (MRA) or at conventional angiography
in about 10% of cases there seems to be overlap between this syndrome and PRES
Pract Neurol 2011; 11: 136–144

Primary CNS vasculitis Symptoms usually come on more insidiously CSF is abnormal, with more than 95% of cases showing an
inflammatory reaction MRI may show multiple infarcts of different ages
Encephalitis in PRES there are no systemic features of inflammation (fever,
blood tests, CSF)
Pract Neurol 2011; 11: 136–144

MANAGEMENT Principles of Management
General measures- aimed at maintaining ABC of the patient
Symptomatic therapy Antihypertensives Anticonvulsants
Correction/Removal of the underlying cause Withdrawl of offending drug Termination of pregnancy


MANAGEMENT OF BLOOD PRESSURE
No empirically established guidelines are available for the optimal degree of BP lowering
A 20% reduction in the MAP is a reasonable goal for immediate reduction in hypertensive crises
The above goal should be reached within the first 2 hours and to bring the blood pressure down to 160/100 mmHg within the first 6 hours
Ideal agent - IV administration, has a rapid onset and short duration of action allowing rapid titration to effect, and be free of limiting side effects- labetolol, hydralazine, nicardipine, or fenoldopam
Semin Neurol 2011;31:202–215
Annual Update in Intensive Care and Emergency Medicine 2011


PROGNOSIS
Brain lesions are reversible
Most studies- excellent short term and long term outcome
symptoms usually seem to resolve in about 3–8 days while recovery of the MRI abnormalities takes longer—several days to weeks
The ideal timing of repeat MRI is about 7–10 days after onset of symptoms when there should usually be clear improvement of the MRI abnormalities
Pract Neurol 2011; 11: 136–144

Occasionally poor neurological outcome has been mentioned as being due to conversion from primary vasogenic into cytotoxic oedema
Poor outcome may also be related to associated comorbidity (sepsis) or intracerebral haemorrhage
A retrospective review of PRES cases between 1998 and 2005 suggested recurrent PRES episodes occur in ~ 4% of cases
Studies report up to 15 % mortality rate
Pract Neurol 2011; 11: 136–144
Annual Update in Intensive Care and Emergency Medicine 2011

CONCLUSION
PRES is a clinicoradiological syndrome and its symptoms and signs develop over hours—a combination of seizures, disturbed vision, altered mental function and headache
MRI is the diagnostic gold standard. There is predominant affection of parieto-occipital subcortical white matter of both hemispheres.Typical PRES lesions on MRI are thought to represent vasogenic oedema
There are many different trigger factors, most commonly abrupt hypertension, renal failure, immunosuppressive therapy, eclampsia, autoimmune disease and infections

The prognosis is good and recurrence rare. Symptoms generally resolve within a week. MRI lesions resolve somewhat more slowly
Treatment consists of antihypertensive drugs, withdrawal of medication such as chemotherapy, and treatment of any underlying disease

THANK YOU