Point of Care Ultrasound versus Chest X-ray in Detection ...
Transcript of Point of Care Ultrasound versus Chest X-ray in Detection ...
Point of Care Ultrasound versus Chest X-ray in Detection of Pneumothorax Prior to Removal of Tube
Thoracostomy in Trauma Patients
Benjamin Mati, MD | Javier Romero, MDVentura County Medical Center
Ventura CA
Next
Ultrasound
• Well-validated for ruling out pneumothorax (PTX)– Lung sliding and comet tails
• Compared to chest X-Ray (CXR) for detection of traumatic PTX– More sensitive
– More specific
– Less expensive
– Faster
NextMore
Clinically significant PTX (CS-PTX):
• CXR: >10% per attending radiologist• Ultrasound: loss of comet tails and/or sliding sign at >1 intercostal space (ICS)
Prospective non-inferiority study
Inclusion criteria:
• Trauma patients with tube thoracostomy (TT)
Exclusion criteria:
• Severe subcutaneous emphysema• Adhesions of pleura• Thoracic skin injuries• Restrictive lung diseases• Painful skin lesions• Painful fractures
Methods
Blinded to CXR, POCUS operator made binary decisions
Final management decided by trauma team based on CXR
POCUS prior to CXR to assess for residual PTX when:• TT to water seal for 12-24 hr• < 200mL drained over 12-24 hr
More Next
POCUS operators were POCUS trained family medicine residents:• 30min focused lung ultrasound training and• At least 10 proctored lung US exams (including 5 positive for PTX)
• 7 CS-PTX reaccumulations were found on subsequent CXR:
• 3 pre-removal exams were POCUS negative and CXR negative
• 3 pre-removal exams were POCUS positive and CXR negative
• 1 pre-removal exam was POCUS positive and CXR positive
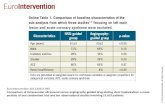
Table 1:
Total Subjects 42
Total Studies 62
Avg BMI 26
Subjects w/confirmed rib Fx 29
Avg POCUS time 4min
ResultsTable 2:
CS-PTXCXR
CS-PTX No CS-PTX
POCUSCS-PTX 4 16
No CS-PTX 0 42
• No CS-PTX seen on CXR were missed on POCUS
• 10 non CS-PTX were seen on CXR but not seen on POCUS
• 16 CS-PTX seen on POCUS were not seen on CXR
More Next
Table 2:
Total PTXCXR
PTX No PTX
POCUSPTX 19 18
No PTX 10 42
Clinically significant PTX (CS-PTX):• CXR: >10% per attending radiologist• Ultrasound: loss of comet tails and/or sliding sign at >1 intercostal space (ICS)
Table 3:
Pre-removal exam for Subsequent CS-PTX Reaccumulations
CXR
CS-PTX No CS-PTX
POCUSCS-PTX 1 3
No CS-PTX 0 3
Table 3:
Pre-removal exam when all PTXReaccumulation Occurred
CXR
PTX No PTX
POCUSPTX 1 4
No PTX 0 12
Conclusions
• No CS-PTX seen on CXR were missed by POCUS
• POCUS is non-inferior to CXR in detecting CS-PTX prior to the removal of TT in simple (ie: single TT) trauma patients
• A POCUS-based algorithm assessing for PTX prior to removal of TT deserves further considerations
More Next
References1. Ball CG, Kirkpatrick AW, Feliciano DV. The occult pneumothorax: what have we learned?. Can J Surg. 2009;52(5):E173-9.2. Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad
Emerg Med. 2005;12(9):844-9.3. Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011;140(4):859-66.4. Galbois A, Ait-oufella H, Baudel JL, et al. Pleural ultrasound compared with chest radiographic detection of pneumothorax resolution after drainage. Chest.
2010;138(3):648-55.5. Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with
Sonography for Trauma (EFAST). J Trauma. 2004;57(2):288-95.6. Kwan RO, Miraflor E, Yeung L, Strumwasser A, Victorino GP. Bedside thoracic ultrasonography of the fourth intercostal space reliably determines safe removal of
tube thoracostomy after traumatic injury. J Trauma Acute Care Surg. 2012;73(6):1568-73.7. Lavingia, Kedar S., et al. "Basic ultrasound training can replace chest radiography for safe tube thoracostomy removal." The American Surgeon80.8 (2014): 783-786.8. Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134(1):117-25.9. Nagarsheth K, Kurek S. Ultrasound detection of pneumothorax compared with chest X-ray and computed tomography scan. Am Surg. 2011;77(4):480-4.10. Nandipati KC, Allamaneni S, Kakarla R, et al. Extended focused assessment with sonography for trauma (EFAST) in the diagnosis of pneumothorax: experience at a
community based level I trauma center. Injury. 2011;42(5):511-4.11. Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT-
-initial experience. Radiology. 2002;225(1):210-4.12. Saucier S, Motyka C, Killu K. Ultrasonography versus chest radiography after chest tube removal for the detection of pneumothorax. AACN Adv Crit Care.
2010;21(1):34-8.13. Soldati G, Testa A, Sher S, Pignataro G, La sala M, Silveri NG. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency
department. Chest. 2008;133(1):204-11.14. Soult MC, Collins JN, Novosel TJ, Weireter LJ, Britt LD. Thoracic ultrasound can predict safe removal of thoracostomy tubes. J Trauma Acute Care Surg.
2014;77(2):256-61.15. Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma.
Acad Emerg Med. 2010;17(1):11-7.16. Wilson H, Ellsmere J, Tallon J, Kirkpatrick A. Occult pneumothorax in the blunt trauma patient: tube thoracostomy or observation?. Injury. 2009;40(9):928-31.17. Younes RN, Gross JL, Aguiar S, Haddad FJ, Deheinzelin D. When to remove a chest tube? A randomized study with subsequent prospective consecutive validation. J
Am Coll Surg. 2002;195(5):658-62.
END























![Clinical Study High Intensity Focused Ultrasound versus ... · Clinical Study High Intensity Focused Ultrasound versus ... Nazareno Suardi ... ca-tion system [ ].](https://static.fdocuments.in/doc/165x107/5af97c097f8b9aff288d3dc0/clinical-study-high-intensity-focused-ultrasound-versus-study-high-intensity.jpg)
