Platelet Hyperaggregability Idiopathic Recurrent Deep Vein...
Transcript of Platelet Hyperaggregability Idiopathic Recurrent Deep Vein...

IDIOPATHIC RECURRENT DEEP VEIN THROMBOSIS/Wu el al.
The documentation that platelet survival time may be par-tially or completely corrected with available drugs, sulfin-pyrazone and clofibrate," affords the opportunity toevaluate the use of these drugs in patients who undergo cor-onary bypass surgery.
Acknowledgment
The authors appreciate the expert technical assistance of Mrs. GloriaSmith, Jan Lacher, Ann Burns and of Miss Jean Baughman and the secre-tarial assistance of Mrs. Peggy Corbin.
References
1. Johnson WD, Felmma RJ, LePley DJR: Direct coronary surgery utiliz-ing multiple-vein bypass grafts. Ann Thorac Surg 9: 436, 1970
2. Effler DB, Favaloro RG, Groves LK: Coronary artery surgery utilizingsaphenous vein graft techniques: Clinical experience with 224 operations.J Thorac Cardiovasc Surg 59: 147, 1970
3. Alderman EL, Matlof HJ, Wexler L: Results of direct coronary-arterysurgery for the treatment of angina pectoris. N Engl J Med 288: 535,1973
4. Lesperance J, Bourassa MG, Biron P, Campeau L, Saltiel J: Aorta tocoronary artery saphenous vein grafts. Preoperative angiographic criteriafor successful surgery. Am J Cardiol 30: 459, 1972
5. Allard C, Goulet C, Grondin CM, Lesperance J, Bourassa MG: Patencyof aorto-coronary vein grafts and serum triglycerides. Three year follow-up study. Am J Cardiol 33: 679, 1972
6. Kern WH, Dermer GB, Lindesmith GG: The intimal proliferation inaortic-coronary saphenous vein grafts. Light and electron microscopicstudies. Am Heart J 84: 771, 1972
7. Vlodavor Z, Edwards JE: Pathologic changes in aortic-coronary arterialsaphenous vein grafts. Circulation 44: 719, 1971
8. Unni KK, Kottke BA, Titus JL, Frye RL, Wallace RB, Brown AL:Pathologic changes in aorto-coronary saphenous vein grafts. Am J Car-diol 34: 526, 1974
9. Brody WR, Angell WW, Kosek JC: Histologic fate of the venous cor-onary artery bypass in dogs. Am J Pathol 66: 111, 1972
10. Steele PP, Weily HS, Davies H, Genton E: Platelet function studies incoronary artery disease. Circulation 48: 1194, 1973
11. Steele P, Battock D, Genton E: Effect of clofibrate and sulfinpyrazone onplatelet survival in coronary artery disease. Circulation 52: 473, 1975
12. Aster RH: Effect of anticoagulant and ABO incompatibility on recoveryof transfused human platelets. Blood 26: 732, 1965
13. Weily HS, Steele PP, Davies H, Pappas G, Genton E: Platelet survival inpatients with substitute heart valves. N Engl J Med 290: 534, 1974
14. Sokal RR, Rohlf FJ: Biometry. San Francisco, WH Freeman & Co.,1969, pp 140-493
15. Henry RJ: Clinical Chemistry, Principles and Techniques, ed. 4,Evanston, Ill., Hoeber Medical Division, Harper and Row, 1967, p 838
16. Fletcher MJ: A colorimetric method for estimating serum triglycerides.Clin Chem Acta 22: 393, 1968
17. Lees RS, Hatch FT: Sharper separation of lipoprotein species by paperelectrophoresis in albumin-containing buffer. J Lab Clin Med 61: 518,1963
18. Fredrickson DS, Levy RI, Lees RS: Fat transport in lipoproteins. Anintegrated approach to mechanisms and disorders. N EngI J Med 276:150, 1967
19. Bousvaros G, Piracha AR, Chaudhry MA, Grant C, Older TM, PifarreR: Increase in severity of proximal coronary disease after successful dis-tal aorto-coronary grafts. Its nature and effects. Circulation 46: 870,1972
20. Aldridge HE, Trimble AS: Progression of proximal coronary arterylesions to total occlusion after aorto-coronary saphenous vein bypassgrafting. J Thorac Cardiovasc Surg 62: 7, 1971
21. Griffith LSC, Achuff SC, Conti CR, Humphries JO, Brawley RK, GottVL, Ross RS: Changes in intrinsic coronary circulation and segmentalventricular motion after saphenous-vein coronary bypass graft surgery. NEngl J Med 288: 589, 1973
22. Spaet TH, Gaynor E, Stemerman MB: Thrombosis, atherosclerosis andendothelium. Am Heart J 87: 661, 1974
23. Baumgartner HR, Stemerman MB, Spaet TH: Adhesion of platelets tosubendothelial surface: Distinct from adhesion to collagen. Experientia27: 283, 1971
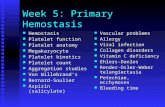
Platelet Hyperaggregability in IdiopathicRecurrent Deep Vein Thrombosis
KENNETH K. Wu, M.D., ROBERT W. BARNES, M.D., AND JOHN C. HOAK, M.D.
SUMMARY Studies of platelet function were performed in 30patients with idiopathic recurrent venous thrombosis. Evidence ofplatelet hyperactivity was found in 14 patients who exhibited spon-taneous platelet aggregation and in 13 patients who had evidence ofcirculating platelet aggregates. No other differences in clinicalcharacteristics or coagulation parameters could be elucidatedbetween these two subgroups. In nine patients who had 5"Cr-labeledplatelet survival studies, there was a good correlation between theplatelet hyperactivity and shortened platelet survival. Spontaneousplatelet aggregation was inhibited both in vivo and in vitro by aspirin.
ALTHOUGH IT HAD BEEN THOUGHT earlier thatplatelets did not play a significant role in the pathogenesis ofdeep vein thrombosis (DVT), several recent studies havereported shortened platelet survival in patients withrecurrent venous thrombosis.1' 2 These observations haverevived interest in the possible pathogenetic relationship
From the Venous Thrombosis Laboratory, Departments of Medicine andSurgery, University of Iowa Medical Center, Iowa City, Iowa.
Address for reprints: Kenneth K. Wu, M.D., Department of Medicine,University of Iowa Hospitals, Iowa City, Iowa 52242.
Received September 3, 1975; revision accepted for publication October 31,1975.
In addition, the circulating platelet aggregates were normalized bycombination treatment with aspirin and dipyridamole. The resultsindicate that the idiopathic recurrent venous thrombosis patient pop-ulation could be differentiated by the platelet function tests intosubgroup I, in which no platelet abnormality could be detected,and subgroup II, where platelet hyperaggregability was present.These results indicate that the role of platelets should be consideredin the pathogenesis of recurrent venous thrombosis and therapy withagents which inhibit platelet aggregation may be beneficial in thepatients with platelet hyperaggregability.
between platelets and venous thromboembolic disorders. Inorder to help elucidate this problem, the present study wasperformed to assess the platelet aggregability in 30 patientswith idiopathic recurrent deep vein thrombosis and toevaluate the effects of antiplatelet agents.
Patients and Methods
All patients were evaluated at the University of IowaMedical Center. Only patients with recurrent idiopathicdeep vein thrombosis were included. Criteria for the selec-tion of patients in this prospective study included 1) objec-
687
by guest on May 19, 2018
http://circ.ahajournals.org/D
ownloaded from

VOL. 53, No. 4, APRIL 1976
tive evidence of deep vein thrombosis demonstrated by theDoppler ultrasound technique, venography, and the 125-Ifibrinogen test; 2) recurrent deep vein thrombosis andpulmonary embolism, arbitrarily defined as having at leastthree episodes of well documented thromboembolic dis-orders in the previous years; 3) absence of known predis-posing factors or underlying diseases to account for the re-currence. A detailed history and physical examination wereperformed on each potential patient. Patients whose re-currence was associated with surgery, trauma, oral con-traceptive agents, pregnancy, delivery, or long-term im-mobilization were excluded. In addition, a complete bloodcount, battery of blood chemistry tests, urinalysis and chestX-ray were obtained. Patients with obvious neoplastic dis-eases, hematological disorders including paroxysmal noctur-nal hemoglobinuria and myeloproliferative disorders, andrenal failure were excluded. From September 1973, to June1975, 30 patients were selected. Their ages ranged from 19to 64 years (mean, 39 years). Nineteen were men. At thetime platelet function studies were performed, none had ex-perienced acute thromboembolic episodes within theprevious month. Fifteen normal subjects, matched for sexand age, were included to serve as controls (table 1). None ofthe subjects or patients took aspirin for at least seven daysprior to the platelet studies. None of the patients receivedoral anticoagulants or heparin during the study.Tests for spontaneous platelet aggregation (SPA) were
performed using a platelet aggregometer (Payton Assoc-iates, Inc., Buffalo, N.Y.) following the principle of Born.3Nine volumes of free flowing venous blood were drawn intoa siliconized glass tube containing one volume of 3.8%sodium citrate. After thorough mixing, the sample was im-mediately centrifuged at 220 X g at 220 C for 8 min to ob-tain platelet-rich plasma (PRP). The remaining sample wascentrifuged at 1800 x g for 15 min to obtain platelet poorplasma (PPP). The platelet concentration of the PRP sam-ple was determined with a Coulter counter.4 Since theplatelet counts of all patients were normal and the plateletconcentrations of the PRP were within the range of 300,000to 500,000 per cu mm, adjustment of the platelet concen-trations was unnecessary. For the determination of SPA, 0.4ml of PRP from a patient or a normal subject was placed ina cuvette containing a siliconized stirring bar and was stirredat 370 C at 1000 RPM for 10 min. The interval from time ofvenipuncture to the performance of platelet aggregationstudies was less than 1 hour. The plasma samples were keptat room temperature during the interval. The aggregometerwas so standardized that the platelet poor plasma blank
TABLE 1. Platelet Function Studies in 30 Patients with Re-current Venous Thrombosis and 15 Healthy Subjects
DVT Normal P
Total number 30 1.5Age (years) 39 (19-64)* 37 (23-53)*Sex (M/F) 19/11 9/6Platelet count(X103/mm3) 33.6 - 20.4 35.7 - 16.6
CPA 0.73 - 0.02 0.91 = 0.01 <0.01SPA (%.) 17.0 ,. 5.5 0.7 i 0.4 <0.01
*The number in the parenthesis indicates the range of the age.Abbreviations: DVT deep vein thrombosis; CPA = circulating
platelet aggregates; SPA spontaneous platelet aggregation.
would indicate 100% light transmission and the platelet richplasma 0% light transmission. At the end of 10 min, the ex-tent of the aggregation of the test PRP samples as measuredby the height of the curve on the chart was determined andthe result was expressed as follows:
% of increase in light transmission -extent of SPA (cm) x 100%.PPP blank (cm)
The result was confirmed further by examinations for thepresence of gross and microscopic platelet aggregates.
Circulating platelet aggregates (CPA) were measured by amethod described previously by Wu and Hoak.5 Free-flowing venous blood (0.5 ml) was drawn directly into twoseparate syringes through a 19 gauge siliconized needle. Onesyringe contained 2 ml of buffered formalin-EDTA solutionand the other buffered EDTA solution. After thorough mix-ing, they were transferred into siliconized glass tubes andkept at room temperature for 15 min. They were again mix-ed and centrifuged at 220 C at 220 x g for 8 min. Plateletcounts were then determined on the supernatant platelet richplasma (PRP) samples. The result was expressed as the ratioof the platelet count in the formalin-EDTA PRP to that ofthe EDTA PRP. This method was based upon the conceptthat formalin would fix existing platelet aggregates whichwould then be centrifuged out, causing the platelet count tobe decreased in the formalin-EDTA sample. The conceptalso involves the ability of EDTA to deaggregate the non-fixed platelet aggregates in the EDTA sample. Most plateletaggregation is calcium dependent, but irreversible plateletaggregates would not be detected by this method. Thegreater number of platelet aggregates in a given sample, thelower the ratio. This method was reproducible. When fivesets of CPA were performed on three normal subjects, thevariation of the results was minimal: i.e., 1.09, 1.09, 1.09,1.00, 1.00 in subject A; 0.94, 0.93, 0.87, 0.96, 0.85 in subjectB; and 1.00, 1.00, 1.00, 1.04, and 0.88 in subject C. Day-to-day variability was determined on two normal subjects forfour consecutive days. The daily CPA ratios were 0.90, 0.84,0.81, and 0.89 in one subject and 0.95, 0.85, 0.84, and 0.88 inthe other. Spontaneous platelet aggregation was repeatedlynegative in both subjects throughout the study.
Platelet survival studies were performed with 51Cr-labeledautologous platelets following the principle of Aster.6Platelet half-life (T½/2) was determined with a computer-assisted program using the least-squares technique.7To study the in vitro effect of aspirin on spontaneous
platelet aggregation, 10 gA I of aspirin solution (MerckChemical Division, Rahway, N.J.) with final concentrationsranging from 10 gg/ml to 100 ,g/ml was added to the PRPwhich was incubated at 370 C for 5 min before the aggrega-tion study. To study the in vivo effect of aspirin, a patientwas given aspirin 1200 mg in divided doses and the spon-taneous aggregation study was repeated in 24 hours. In addi-tion, a combination of aspirin (1200 mg daily) anddipyridamole (200 mg daily) was given to eight patients andthe platelet aggregate ratio was repeated 3-7 days later.
Statistical evaluation was carried out by the Student's t-test.8 Mean values were expressed together with the standarderror of the mean (SEM) unless otherwise specified.
688 CIRCULATION
by guest on May 19, 2018
http://circ.ahajournals.org/D
ownloaded from

IDIOPATHIC RECURRENT DEEP VEIN THROMBOSIS/Wu et al.
Results
Spontaneous Platelet Aggregation in Recurrent DVT
The mean SPA value in 30 patients with idiopathicrecurrent DVT was 16.5% ± 5.5, which was significantly in-creased from the controls (P < 0.01) (fig. 1). The normalrange (mean ± 3 SD) of the SPA value as determined in ourlaboratory from 150 normal subjects was 0 to 6.76%. Apositive SPA result was defined as an increase in lighttransmission of more than 7% with the presence of grossplatelet clumps. By this definition, 14 of the 30 patients hadincreased SPA. Their values ranged from 8% to 100%.
Platelet Aggregates in Recurrent DVT
The mean platelet aggregate ratio in 30 patients withrecurrent DVT was 0.73 ± 0.02 which was significantlylower than that of normals (P < 0.01), indicative of in-creased aggregates in these patients (fig. 2). The normalrange of CPA (mean ± 2 SD) obtained from 15 normalsubjects was 0.77 to 1.00. Thirteen (43%) patients had in-creased platelet aggregates. The comparison of SPA andCPA values in these patients was shown in table 2. Both testswere found to be positive in ten patients and both werenegative in 13.
Simultaneous determinations of SPA, CPA, and plateletsurvival time were performed on nine patients (table 3).These patients were randomly selected mainly because oftheir cooperation to participate in the study. In six patientsin whom both SPA and CPA were increased, the plateletsurvival was all decreased. On the other hand, platelet half-life was normal in two patients whose CPA and SPA valueswere also normal. The platelet half-life was shortened in onepatient whose CPA was abnormal but SPA was normal.
Effects of Aspirin on Spontaneous Aggregation
The in-vitro inhibition of spontaneous platelet aggrega-tion was dose-related. The SPA was not inhibited at the con-centration of 10 ,ug/ml, partially inhibited at 25 Atg/ml and,completely inhibited at 50,ug/ml. In this same patient, the
100po
TABLE 2. Comparison of Circulating Platelet Aggregates(CPA) and Spontaneous Platelet Aggregation (SPA) Resultsin Patients with Recurrent Venous ThrombosisSPA CPA N
+ + 1013
+ 4+ 3
+ = positive, indicating increased values as compared with normalmean data.- = negative, indicating values commensurate with normal mean data.N = number of patients.
spontaneous aggregation was completely inhibited 24 hoursafter aspirin, 1200 mg, was given. On the other hand,dipyridamole (200 mg daily) alone did not normalize theplatelet aggregation.
Persistence and Response of Increased CPA toAntiplatelet Agents
The platelet aggregate ratio was repeated from eight to164 days later in nine patients who were found to have in-creased aggregates initially. The condition of these patientswas stable during the study. The platelet aggregate ratiosremained low in all patients and the SPA remained littlechanged (table 4). However, CPA returned to normal inthree to seven days after combination of aspirin anddipyridamole was given in all patients except W.T. who hadan episode of pulmonary embolism at the end of the plateletsurvival study. He was therefore removed from the studyand treated with intravenous heparin. Spontaneous plateletaggregation returned to normal in six of seven patients. Thiscombination antiplatelet therapy failed to reduce the SPAvalue in one patient (E.M.).
Four patients were followed adequately and the clinicalresponse could be assessed. Three of the four patients (C.L.,R.W., and R.S.) had had no recurrence within one year afterthe start of antiplatelet therapy. These patients had two tofour episodes of deep vein thrombosis per year previously.The fourth patient (T.S.) had a recurrence of deep veinthrombosis and pulmonary embolism when he was treatedwith aspirin and dipyridamole. Despite an initial normaliza-tion of the CPA and SPA values one week following the an-
- 80
40
z20
r1.0-
0.8
Q)% 0.6
"Zs,
Q:- 0.4
: 02..
..,.. .. . .. . ....._,,..,,,,,..,.,_ ._, .,,._,,_,,,.. _._..._...... ....*s-. ..
Normal D.V.T(N -15) (N = 30)
FIGURE 1. Spontaneous platelet aggregation in 30 patients withrecurrent deep vein thrombosis and 15 healthy subjects.
I j Normal
I
;F
1--
I-
N=15 N=30Normal D.V.T.
FIGURE 2. Platelet aggregates in patients with recurrent venousthrombosis. The area above the dotted line represents the normalrange.
689
*-0
by guest on May 19, 2018
http://circ.ahajournals.org/D
ownloaded from

VOL. 53, No. 4, APRIL 1976
Function and Survival
SPA Platelet T'2Patient CPA (%) (days)
R.S. 0.39 10 1.2C.F. 0.68 12.5 - 3.2T.S. 0.63 8 3.0R.W. 0.57 100 2.9C.L. 0.67 100 3.8W.T. 0.61 43 3.0B.C. 0.90 0 4.0M.H. 0.88 0 4.1A.P. 0.65 3 3.0
Normal range 0.77 - 1.0 <7 3.3 - 4.9
tiplatelet therapy in this patient, both SPA and CPA hadbecome abnormal when the venous thrombosis recurred. Hewas subsequently treated with intravenous heparin.
Discussion
In this study of patients with idiopathic recurrent deepvein thrombosis, both spontaneous platelet aggregation andcirculating platelet aggregates were enhanced in almost 50%of the patients. The platelet function studies were performedwhile they were free from active thrombosis and while theywere not taking any anticoagulant or antiplatelet agents.The abnormal platelet function persisted from weeks tomonths and became normal when dipyridamole and/oraspirin were given. These findings suggest that platelethyperaggregability may play an important role in therecurrence of venous thrombosis in these patients.From this study, it also appears that idiopathic recurrent
deep vein thrombosis represents a heterogeneous group ofpatients which can be divided into two subgroups: group I inwhich a platelet abnormality could not be detected andgroup II in which platelet hyperaggregability was detected.The clinical manifestations, as well as the platelet count,fibrinogen concentration, partial thromboplastin and pro-thrombin times were similar in both groups of patients. Theabsence of hyperaggregability in group I patients suggeststhat the pathogenetic mechanisms for the initiation andrecurrence of venous thrombosis may involve abnormalitiesin the coagulation or fibrinolytic systems. Although recentstudies have found decreased fibrinolytic activity9 and anti-thrombin 11110, " in patients with deep vein thrombosis, theirimportance with respect to the pathogenesis remains to befurther studied. On the other hand, the pathogenesis of
TABLE 4. Persistence and Response of CPA and SPA toAntiplatelet Agents
CPA ratio SPA(%o)Patient Initial Follow-up Post-therapy Initial Follow-up Post-therapy
C.L. 0.67 0.60 0.90 100 100 2R.W. 0.57 0.57 0.91 100 96 3R.S. 0.39 0.43 0.85 10 12 3T.S. 0.63 0.70 0.93 9 15 4B.H. 0.59 0.64 0.85 11 12 1G.W. 0.69 0.69 0.80 9 9 4E.M.' 0.73 0.77 0.80 25 23 20W.F. 0.73 0.74 0.85 4 4 3W.T. 0.61 0.70 ND 43 14 NDND = not done.
recurrent deep vein thrombosis in group II patients is morereadily understood on the basis of enhanced SPA, increasedCPA, and shortened platelet survival. However, questionsconcerning the etiology of platelet hyperaggregability re-main to be answered. Does the increase in platelet functionmerely reflect the fact that the platelet population in thesepatients may be abnormally young and metabolicallyhyperactive? What are the roles of extrinsic factors such asimmune complexes, bacterial and viral injuries, etc.12 intriggering platelet hyperaggregability? Could the platelet ab-normality be related to intrinsic platelet defects, particularlythe altered platelet surface? Pertinent to the last question arerecent observations that removal of surface sialic acid withneuraminidase enhances platelet aggregability to aggregat-ing agents and shortens platelet survival"3 while addition ofsialic acid decreases platelet aggregability." It has also beenshown that platelet sialotransferase may play an importantrole in the platelet aggregation and platelet adhesiveness.'5Alteration of the enzyme activity should also be consideredas a possible mechanism for platelet hyperaggregability.That the SPA was inhibited with aspirin in vivo and in
vitro was consistent with the observation of Vreeken andVanAken."1 Additional studies performed in our laboratoryrevealed the SPA could also be inhibited with 2-chloro-adenosine, prostaglandin E, or apyrase in a dose-relatedmanner.'7 These indirect evidences and the demonstration ofincreased ADP release by direct measurement indicate thatthe phenomenon involved the release of endogenous ADPfrom the stirred platelets.'8The rationale for using the aspirin-dipyridamole therapy
in this study was based on the observation by Harker andSlichter'9 that aspirin may potentiate the effect of dipyri-damole on the prevention of platelet consumption in patientswith arterial thromboembolic disorders. On the other hand,aspirin alone has little modifying effect on platelet consump-tion. After treatment with this combination regimen, CPAreturned to normal in all eight patients and SPA returned tonormal in six of the seven patients. Three of the four patientswho were followed for at least a year did not haverecurrence. This is quite an improvement considering thatthey usually had two episodes of deep vein thrombosisand/or pulmonary embolism per year. These preliminarydata suggest that CPA and SPA tests may be useful in theselection of patients who may benefit from therapy withagents that inhibit platelet aggregation.
AcknowledgmentsThe authors wish to thank Mrs. Trudi Krapf, Mrs. Donna Haycraft, and
Mr. Don Harmon for their excellent technical assistance.
References
1. Harker LA, Slichter SJ: Platelet and fibrinogen consumption in man. NEngl J Med 287: 999, 1972
2. Steele PP, Weily HS, Genton E: Platelet survival and adhesiveness inrecurrent venous thrombosis. N Engl J Med 288: 1148, 1973
3. Born GVR: Aggregation of blood platelets by adenosine diphosphate andits reversal. Nature 194: 927, 1962
4. Bull BS, Schneiderman MA, Brecher G: Platelet counts with the Coultercounter. Am J Clin Pathol 44: 678, 1965
5. Wu KK, Hoak JC: A new method for the quantitative detection ofplatelet aggregates in patients with arterial insufficiency. Lancet 2: 924,1974
6. Aster RH: Effect of anticoagulant and ABO incompatibility on recovery
TABLE 3. Correlation of PlateletStudies in Nine Patients
690 CIRCULATION
by guest on May 19, 2018
http://circ.ahajournals.org/D
ownloaded from

HEPARIN KINETICS IN THROMBOEMBOLISM/Hirsh et al.
of transfused human platelets. Blood 26: 732, 19657. Paulus JM: Platelet Kinetics. Amsterdam, North Holland Publishing Co,
1971, ch 58. Hill AG: Principles of Medical Statistics. London, The Lancet Limited,
1961, ch XII9. Isacson S, Nilsson IM: Defective fibrinolysis in blood and vein walls in
recurrent "idiopathic" venous thrombosis. Acta Chir Scand 138: 313,1972
10. Bergstrom K, Lahnborg G: The effect of major surgery, low doses ofheparin and thromboembolism on plasma antithrombin. Comparison ofimmediate thrombin inhibiting capacity and the antithrombin III con-tent. Thromb Res 6: 223, 1975
11. Marciniak E, Farley CH, DeSimone PA: Familial thrombosis due to an-tithrombin III deficiency. Blood 43: 219, 1974
12. Mustard JF: Platelets in thromboembolic disease. Adv Cardiol 4: 131,1970
13. Greenberg J, Packham MA, Cazenave J, Mustard JF: Effects on platelet
function of removal of platelet sialic acid by neuraminidase. Lab Invest32: 476, 1975
14. Mester L, Szabados L, Born GVR, Michal F: Changes in the aggregationof platelets enriched in sialic acid. Nature New Biol 236: 213, 1972
15. Bosman HB: Platelet adhesiveness and aggregation. II. Surface sialicacid, glycoprotein: N-acetylneuraminic acid transferace and neur-aminidase of human blood platelets. Biochim Bioph Acta 279: 456, 1972
16. Vreeken J, Van Aken WG: Spontaneous aggregation of blood platelets asa cause of idiopathic thrombosis and recurrent painful toes and fingers.Lancet 2: 1394, 1971
17. Wu KK, Hoak JC: Spontaneous platelet aggregation in arterial insuf-ficiency: Mechanisms and implications. Blood 44: 934, 1974
18. Weiss HJ, Aldort LM, Kochwa S: The effect of salicylates on thehemostatis properties of platelets in man. J Clin Invest 47: 2169, 1968
19. Harker LA, Slichter SJ: Arterial and venous thromboembolism: Kineticcharacterization and evaluation of therapy. Thromb Diath Haemorrh 31:188, 1974
Heparin Kinetics in Venous Thrombosisand Pulmonary Embolism
JACK HIRSH, M.D., WILLEM G. VAN AKEN, M.D., Ph.D.,
ALEXANDER S. GALLUS, M.B.B.S., COLIN T. DOLLERY, M.B.Ch.B.,
JOHN F. CADE, M.D., Ph.D., AND WILLIAM L. YUNG, B.Sc.
SUMMARY The response to a standard dose of heparin wasstudied in 20 patients with venous thromboembolism. The heparinregimen consisted of intravenous injection of 70 units per kg, followedafter 90 minutes by a maintenance dose of 400 units per kg per 24hours given by continuous infusion. Plasma heparin activity and theactivated partial thromboplastin time (APTT) were measured at in-tervals to determine clearance of the initial injection and the responseto maintenance dose. Large inter-individual variations were found in
HEPARIN IS GENERALLY CONSIDERED to be thedrug of choice in the treatment of venous thromboembo-lism. The aim of heparin treatment is to prevent local exten-sion of venous thrombosis and subsequent recurrentpulmonary embolism without causing bleeding. The fre-quency of death, recurrent thromboembolism and bleedingduring heparin treatment has varied greatly in the manyreports of treatment of patients with venous thrombo-embolism and it is likely that this variation is related, atleast in part, to the heparin regimen used. Recent evidencesuggests that both recurrent thromboembolism and bleedingcan best be prevented if the heparin dose is adjusted in eachpatient to maintain the results of an in vitro test of bloodcoagulation within a defined range.'
From the Departments of Pathology and Medicine, McMaster University,Hamilton, Ontario, Canada, and the Department of Clinical Pharmacology,Royal Postgraduate Medical School, London, England.Supported in part by the Province of Ontario and the Canadian Heart
Foundation. Dr. van Aken is a Visiting Research Fellow of the Ontario HeartFoundation and was supported by a grant from the Ontario Heart Founda-tion of Canada and by a Travel Grant from the Nils Stensen Foundation,Amsterdam. Professor Dollery was the R. Samuel McLaughlin VisitingProfessor at McMaster University when this work was done.Address for reprints: J. Hirsh, M.D., Department of Pathology, Room
3N18, McMaster University Medical Centre, Hamilton, Ontario, Canada.Received August 14, 1975; revision accepted for publication October 28,
1975.
the anticoagulant effect and these were due in part to differences inheparin clearance and in part to differences in the APTT response togiven amounts of heparin (heparin effect index). The heparin half-lifewas 63 ± 15 minutes when plasma heparin activities were used forthis calculation and 84 ± 71.5 minutes when the APTT was used.These results are similar to values previously reported in normalvolunteers. Four of the 20 patients had pulmonary embolism and inthese heparin half-life was significantly shortened (P < 0.005).
A number of studies' have now demonstrated that the in-dividual response to a standard dose of heparin differs con-siderably among patients with venous thromboembolism.The reason for this variation is uncertain. It could be due tointer-individual differences in heparin inactivation orclearance, to variations in the levels of circulating coagula-tion factors which modify the coagulation test response toheparin, or to a combination of both of these factors.The present study was undertaken to investigate some of
the mechanisms for the variation in heparin response ofpatients with venous thromboembolism by measuring theplasma heparin activity, the activated partial thrombo-plastin time (APTT), and heparin kinetics in these patientsfollowing the administration of a standard heparin dosageregimen.
Patients and MethodsTwenty patients with venous thromboembolism were
studied before and during the administration of heparin.Details of age, sex and diagnosis are shown in table 1. Theclinical diagnosis of venous thrombosis was confirmed byascending venography in all but two patients, both of whomhad a history of allergy to contrast medium. The diagnosisof pulmonary embolism was suspected on clinical groundsand confirmed by the results of chest X-ray and either lung
691
by guest on May 19, 2018
http://circ.ahajournals.org/D
ownloaded from

K K Wu, R W Barnes and J C HoakPlatelet hyperaggregability in idiopathic recurrent deep vein thrombosis.
Print ISSN: 0009-7322. Online ISSN: 1524-4539 Copyright © 1976 American Heart Association, Inc. All rights reserved.
is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231Circulation doi: 10.1161/01.CIR.53.4.687
1976;53:687-691Circulation.
http://circ.ahajournals.org/content/53/4/687the World Wide Web at:
The online version of this article, along with updated information and services, is located on
http://circ.ahajournals.org//subscriptions/
is online at: Circulation Information about subscribing to Subscriptions:
http://www.lww.com/reprints Information about reprints can be found online at: Reprints:
document. Permissions and Rights Question and Answer information about this process is available in the
located, click Request Permissions in the middle column of the Web page under Services. FurtherEditorial Office. Once the online version of the published article for which permission is being requested is
can be obtained via RightsLink, a service of the Copyright Clearance Center, not theCirculationpublished in Requests for permissions to reproduce figures, tables, or portions of articles originallyPermissions:
by guest on May 19, 2018
http://circ.ahajournals.org/D
ownloaded from