Platelet activation as a novel mechanism of atherothrombotic risk in chronic obstructive pulmonary...
-
Upload
gian-carlo -
Category
Documents
-
view
214 -
download
1
Transcript of Platelet activation as a novel mechanism of atherothrombotic risk in chronic obstructive pulmonary...

Review
BackgroundChronic obstructive pulmonary disease (COPD) is an important cause of mortality worldwide and is projected to be the fifth most prevalent disease and the third leading cause of death by 2020. Its prevalence in adults aged >40 years is about 9–10%, and estimated to be 20–30% in patients aged >70 years, which suggests a posi-tive correlation with age. An important aspect of this disease is its clinical and pathophysiologi-cal inflammatory heterogeneity, involving both pulmonary and extrapulmonary aspects. Indeed, the presence of concomitant chronic conditions, in particular cardiovascular and metabolic dis-eases, is reported invariably high in this pop-ulation of patients [1], which also refer to the need of a more complex approach and clinical management.
Systemic inflammation has been considered the main determinant of multimorbidities in COPD patients. In particular, systemic inflam-mation has been identified as one of the main
causal factor for atherosclerosis [2], and indeed COPD is an independent risk factor for cardio-vascular diseases [3], although the mechanisms leading to these are still unclear. The low-grade systemic inflammation, hypoxia and oxidative stress typical of these patients may together explain this increase in cardiovascular risk and mortality [4,5]. Inflammatory pathways are fur-ther upregulated during acute exacerbation and may plausibly precipitate an acute cardiovascu-lar event [6]. Inflammatory cells and cytokines have been proved to be involved in atheromatous plaque formation and coronary thrombosis [7].
Platelet activation: pro-atherothrombotic & inflammatory mechanisms in smokers and COPDPlatelets (PTLs) have multiple functions. First, they are involved in coagulation, which prevents blood loss, and promote the atherothrombotic process. Second, they have immune system-modulating properties and promote the release
Mario Malerba*1, Enrico Clini2, Michele Malagola3 and Gian Carlo Avanzi4
1Dipartimento di Medicina Interna – Az. Spedali Civili di Brescia e Università di Brescia2DU di Scienze Mediche e Chirurgiche Università Studi di Modena e Reggio Emilia – Ospedale Villa Pineta UO Pneumologia e Riabilitazione, Pavullo n/F (MO)3Dipartimento di Medicina Interna – Sez. di Ematologia – Az. Spedali Civili di Brescia e Università di Brescia4Dipartimento di Medicina Traslazionale, Università del Piemonte Orientale, Novara*Author for correspondence: Tel.: +39 030 3995250 [email protected]
Chronic obstructive pulmonary disease (COPD) is characterized by pulmonary and systemic inflammation. In particular, the clinical course of this disease typically leads to periodic exacerbation involving inflammatory response and both respiratory and cardiovascular symptoms. Even though the exact mechanisms underlying the pathogenesis of COPD and its chronic and acute inflammation have not yet been fully understood, many studies have been highlighting the role of the endothelium, platelets (PTL) and other circulating blood cells. PLT are crucial for hemostasis and, once activated by a number of different factors, will mediate endothelium adhesion, and the rolling and activation of other circulating cells, such as neutrophils, which become a cause of tissue damage during the inflammatory process. The aim of this review is to highlight the onset of activation, thrombus formation and inflammatory amplification with particular regard to the COPD patients and the course of their acute exacerbations.
Keywords: acute exacerbation • chronic obstructive pulmonary disease • inflammation • platelet activation
Platelet activation as a novel mechanism of atherothrombotic risk in chronic obstructive pulmonary diseaseExpert Rev. Hematol. 6(4), 475–483 (2013)
Expert Review of Hematology
© 2013 Informa UK Ltd
10.1586/17474086.2013.814835
1747-4086
1747-4094
Review
10.1586/17474086.2013.814835 475ISSN 1747-4086© 2013 Informa UK Ltdwww.expert-reviews.com

Review
of cytokines and chemokines. Hemostasis is mediated by two mutually related elements: cells (PLT and vascular endothelial cells, which normally inhibit thrombosis) and plasma proteins, that is, coagulation cascade [8].
When the endothelium is damaged, PLT become active and interact with each other and/or with other cells, such as neu-trophils and monocytes. This phenomenon requires very com-plex links between adhesion molecules, some specific receptors and the cytokine network [9]. In light of this, PLT activation and hemostasis are very strongly related to inflammation, which means that the natural course of chronic and inflammatory non-hematological diseases, such as COPD, may also have relations with PLT activation and function [10].
Multiple pathways lead to PLT activation as shown in Table 1 [11]. The cumulative action of these activators results in recruit-ment of PLT from the blood, which then results in a number of particular signs of activation. Their change in shape, the expres-sion of proinflammatory molecules such as P-selectin and soluble CD40 ligand (sCD40L), the expression of procoagulant activity and the conversion of GPIIb/IIIa (αIIβ3-integrin) into one of its
active forms, allow for PLT aggregation and thus increase their potential for pathologic thrombosis.
Another promising biomarker for COPD exacerbations and comorbidities is blood fibrinogen, an acute phase glycoprotein which is present in plasma and which has the role of converting thrombin into fibrin during blood coagulation [12]. Recent stud-ies have shown that levels of blood fibrinogen have a relationship with forced expiratory volume (FEV
1) % pred., independent of
smoking status, in a cohort of a little less than 9000 subjects [13], with risk of exacerbations, in 2138 patients with COPD [14] and with cardiovascular comorbidities of COPD in a cohort little over 2500 subjects [15].
PLT-derived chemokines can potentiate thrombosis and inflammation [16]. Earlier studies had already shown an elevated PLT aggregation in 23 hypoxemic COPD patients studied [17]. More recently, PLT aggregation has been indirectly proved in vivo by assessing the urinary level of 11-dehydro-thromboxane B2 (11-d-TxB2), the metabolite of thromboxane A2 (TxA2), as a marker of biosynthesis [18], involved in both PLT aggregation and smooth muscle constriction and proliferation [19]. Very impor-
tantly, urinary 11-d-TxB2 values are notably higher in the 29 patients with stable COPD than in the 29 controls included in the study and are inversely correlated with arterial oxygen tension and directly correlated with acute oxygen supplementation irrespective of smoking status [20]. These data suggest a link between hypoxia and PLT activation, since hypoxia induces metabolic changes on the PLT mem-brane that in turn lead to increased activation of cyclooxygenase-1 and increased thromboxane formation [21]. In addition, as in a vicious cycle, the activation of coagulation (associated with the generation of thrombin) is able to determine a further activation of PLT, with a consequent increase of the biosynthesis of thromboxane [22].
It has been demonstrated that activated PLT secrete reactive oxygen species (ROS), which may enhance PLT recruitment to a growing thrombus and lipid peroxidation of cell-membrane phospholipids and circulating low-den-sity lipoproteins [23], thus leading to atherothrombosis. The onset and course of COPD is closely linked with oxida-tive stress and a decrease in antioxidant response [24]. Elevated level of hydrogen peroxide in exhaled breath condensate is a marker of oxidative stress in the lungs of COPD patients irrespective of smok-ing status [25], as well as in non-COPD
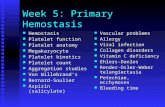
Table 1. Agonists involved in platelet activation and their effects on platelets.
PLT activator Receptor(s) Effect on PLT
ADP P2Y1P2Y12
PLT shape change (P2Y1)Transient aggregation (P2Y1)Sustained irreversible aggregation (P2Y12)Expression of P-selectin (P2Y12)Release of TxA2 (P2Y1 and P2Y12)PLT recruitment to sites of injury (P2Y12)Induction of procoagulant activity and aggregation(P2Y12)
Thromboxane A2 TPαTPβ
PLT recruitment and aggregation to a primary PLT plug (TP-α)
Serotonin 5HT-2A PLT recruitment to sites of injuryInduction of procoagulant activity via retention of fibrinogen and thrombospondin on PLT surface
Epinephrine α2a Supplementary role overlapping P2Y12 receptor signaling
Collagen GPIb (high shear via vWF)GPIIb/IIIa (high shear via vWF)GPIa/IIa (low shear)GPVI (low shear)
Activation of GPIIb/IIIaRelease of ADP and TxA2PLT spreadingPLT aggregationInduction of procoagulant activity via release of Ca2+
Thrombin PAR-1PAR-4
PLT aggregation (PAR-1)Release of ADP, TxA2 (PAR-4), serotonin (PAR-1) and epinephrine (PAR-1)Activation/mobilization of P-selectin and CD40L (PAR-1)Induction of PLT procoagulant activity (PAR-1)
Receptors primarily responsible for activation in PLT are indicated in bold.ADP: Adenosine diphosphate; GP: Glycoprotein; PAR: Protease-activated receptor; PLT: Platelet; vWF: von Willebrand factor.
Expert Rev. Hematol. 6(4), (2013)476
Malerba, Clini, Malagola & Avanzi

Review
smokers [26]. Oxidative stress can promote the peroxidation of polyunsaturated fatty acids. F2-isoprostanes are the stable prod-ucts of the peroxidation of arachidonic acid and provide a reliable measure of systemic in vivo oxidative stress. Irrespective of cur-rent smoking habits, the excretion of F2-isoprostane significantly increases in COPD and peaks during exacerbations [27]. This may suggest susceptibility to low-density lipoproteins oxidation [28], a potential determinant of plaque formation. Therefore, PLT activa-tion and hemostasis are closely linked with chronic inflammation, which means that inflammatory diseases such as COPD may be influenced by PLT activation and function.
P-selectin expression, a marker of PLT activation, is increased in smokers compared to non-smokers [29]. Basal PLT-dependent thrombin generation appears to be significantly greater in smokers than in non-smokers and further rises on direct cigarette smoke inhalation [30] and at higher heart rates [31]. Moreover, smokers appeared to have increase CD40 ligand (CD40L) expression on PLT and CD40 expression on monocytes [32] that may lead to both atheroma formation and thrombosis.
In addition, sCD40L levels were shown to be elevated in smok-ers. The sCD40L has recently been suggested as a predictor of car-diovascular events in 221 patients with acute coronary syndrome
[33]. Although produced by cells other than PLT, such as CD4-T lymphocytes, it is thought that sCD40L is mainly the result of PLT activity [34] and inversely relates with FEV
1 in patients with
cystic fibrosis [35]. The CD40–CD40L interaction promotes cytokine release and adhesion of molecules, metalloproteinases and tissue factor [36].
In summary, upregulation of the CD40/CD40L may lead to what we term ‘the atherothrombotic consequences of smoking’. Overall, these data confirm the role of cigarette smoke-related PTL activation which determines an enhancement of coagulation and finally leads to increased thrombin generation [37].
Consequences of PLT–immune system interactionThe induction of inflammatory mediators by activated PLT cul-minates in the recruitment of leukocytes. PLT P-selectin is crucial for the recruitment of immune cells through its adhesive activity and signaling properties [38,39] and it is also necessary for the for-mation of regulated on activation, normal T cell expressed and secreted deposits on the inflamed endothelium [40]. The interac-tion between PLT, leukocytes, and the endothelium may occur in various forms. First, PLT can aggregate with leukocytes and support leukocyte recruitment to the endothelium via activation
Figure 1. Mechanisms and markers related with atherothrombosis in chronic obstructive pulmonary disease. COPD: Chronic obstructive pulmonary disease; CRP: C-reactive protein; MMP: Matrix metalloproteinase; oxLDL: Oxidized low-density lipoprotein; ROS: Reactive oxygen species. Adapted with permission from [45].
Atherosclerotic plaqueHeart attack and stroke
Smooth muscle cells (layer)
ICAM-1VCAM-1
Foam cells oxLDL
Monocyte
Lung inflammation
Systemic inflammation
Blood vessel activation
Endothelial dysfunction
Oxidative stress Pro-thrombotic status
COPD, asthma, infection
exposure to air pollution
Fibrinogen
Endothelialcells (layer)
Destabilize plaques:
Adhesion molicule expression→
Monocyte recruitment→
Plaque cellurality→
Foam cells and plaque lipid content→
Smooth muscle cell proliferation→
Proteinase activity (MMPs)→
Fibrose cap of plaques
→
CRP and fibrinogenCytokines (TNF-α, IL-1β, IL-6)Leukocytes and platelets
→→
→
Endothelial permeabilityROS and uptaken of oxLDL
Vasodilatation
→→
→→ ET-1, NO
→
477www.expert-reviews.com
COPD & platelet activation

Review
of leukocyte adhesion receptors. Alternatively, PLTs adherent on the endothelium can chemoattract leukocytes and provide a sticky surface for neutrophil–endothelium interaction. The net result of these events is cell infiltration in atherosclerotic plaque [41]. PLT, therefore, are not only implicated in vessels occlusion but, in fact, they also play additional role beyond hemostasis and thrombosis and may provide the basis for plaque formation.
In animal model, the Gas6/TAM system (growth arrest-specific factor, namely Gas6 and its receptors Tyro3–Axl–Mer, namely TAM) plays a role in the phagocytosis of apoptotic cells and in the regulation of innate immune response [42], preserving vessel integrity and mediating the response to injury. Interestingly, poly-morphisms in human Gas6 and Mer genes are protective against stroke [43] and carotid atherosclerosis [44], respectively.
PLT activation & COPD: which measure can be useful in clinical practice?At least four factors seem to play a significant role in the patho-genesis of COPD and atherothrombosis: chronic systemic inflam-mation, susceptibility to hypercoagulation, PLT activation and oxidative stress (Figure 1 & Table 2) [45].
Enhanced inflammatory pathways during an episode of acute exacerbation are more likely to precipitate an acute cardiovascular event [5]. In light of the main role that activated PTLs play in the pathogenesis of atherothrombosis (see above), this further underlines the importance of this process in COPD patients. PTL reactivity is higher in COPD patients [46] and may follow the increased PLT oxidation [47]. Indeed, plasma levels of P-selectin are significantly higher in the 40 COPD patients than in the 20 healthy controls analyzed, and inversely relate with FEV
1 [48].
PTL activation is a reliable predictor of adverse outcomes in patients with stable coronary disease [49–51], is of help in identifying
patients likely to experience recurrent cardiovascular events fol-lowing percutaneous coronary bypass surgery [52], is linked with structural remodeling of the pulmonary vasculature and is thought to play a role in the pathogenesis of all forms of pulmonary arterial hypertension [53]. All these factors are potentially of relevance to the pulmonary vascular system in COPD patients; indeed, COPD patients have shown arterial stiffness rates higher than controls [54].
Recently, Maclay et al. demonstrated that 18 COPD patients studied showed an increase in circulating PLT-monocyte aggre-gates even during exacerbations [46]. Some authors have suggested that several factors may be involved, including increased systemic inflammation, hypoxemia and hemodynamic stress, which are enhanced during an acute episode. In this condition, mono-cyte recruitment, PLT–monocyte interaction and adherence to denuded endothelium are driven by upregulation of adhesion molecules and increased chemokine release by activated PLT [47]. Leukocytes recruited through chemotaxis also cause PLT activa-tion [55]. Circulating leukocyte and neutrophil concentrations depend on PLT-monocyte aggregates, supporting the hypoth-esis that the level of systemic inflammation may contribute to PTL activation in COPD. This mechanism is thought to play an equally fundamental role in other chronic inflammatory conditions typically characterized by increased PLT-monocyte aggregates such as rheumatoid arthritis and type-1 diabetes. In addition, enhanced systemic inflammation such as during exac-erbation or infection can induce activation of PTLs through the Gas6 /TAM system. Increased levels of circulating Gas6 have been demonstrated in severe sepsis and in septic shock [56] or during acute pulmonary embolism [57].
Finally, activation of circulating PLT in COPD patients during an acute exacerbation may also depend on other factors such as hypoxia, tachycardia and hyperglycemia [58]. These conditions enhance inflammatory response, thus potentially explaining the occurrence of respiratory symptoms and the acute ischemic events [59].
In a preliminary report, PLT counts were found to be higher in COPD than in matched controls, with the number of PTL count significantly correlated with the degree of airway obstruction as measured through the global initiative for chronic obstructive lung disease Global Initiative for Chronic Obstructive Lung Disease standard. In fact, Crisafulli et al. studied 196 patients with stable COPD and found an increase in PLT according to the GOLD classes and that PLT count is correlated with FEV
1 [60]. A
higher PTL count has been associated with adverse cardiovascular outcomes in both healthy individuals and patients with acute myocardial infarction [61].
High mean platelet volume (MPV) as well can be regarded as a marker of PTLs activation, as it has been detected in acute myo-cardial infarction, hypercholesterolemia, diabetes mellitus, hyper-tension and stroke [62]. Recently, a study on 85 COPD patients and 34 healthy smokers enlightened that MPV, as well as white blood cells count, was higher in COPD patients but not in healthy smokers [63]. A recent study by Cui et al. found high MPV levels and impaired cardiopulmonary function to be linked in elderly male COPD patients [64]. For the first time, these authors found that high MPV was inversely correlated with FEV
1% predicted
Table 2. Mechanisms and biomarkers involved during the atherothrombotic process in chronic obstructive pulmonary disease.
Pro-atherothrombotic mechanisms in COPD
Biomarkers involved
Systemic inflammation Increased C-reactive protein (even during acute exacerbations)Increased fibrinogen (even during acute exacerbations)Increased IL-6Increased IL-8Increased TNF-α
Hypercoagulable state HypoxiaIncreased fibrinogenIncreased D-dimerIncreased prothrombin fragment F 1.2Polycythemia
PLT activation Increased PLT aggregability in hypoxemic patients (11-d-TxA2/11-d-TxB2)
Oxidative stress Increased F2-isoprostanes in the urine (marker of LDL oxidation)
COPD: Chronic obstructive pulmonary disease; LDL: Low-density lipoprotein.
Expert Rev. Hematol. 6(4), (2013)478
Malerba, Clini, Malagola & Avanzi

Review
in the COPD population; consequently, high MPV levels may be indicative of disease severity. Moreover, MPV was higher in patients with decreased left ventricular ejection fraction, which means that high MPV may serve as an early predictive marker of impaired cardiopulmonary function in those individuals.
In literature only two studies reported that a lower MPV is cor-related to COPD; in particular, the study by Ulasli et al. [65] showed that patients with acute exacerbations have lower MPV than in patients with stable COPD and in controls [65]; while the study by Biljak et al. showed that COPD patients have lower MPV compared with healthy controls [66]. However, the first paper has not been widely cited because it was published on a Polish journal, the number of patients considered by this study was little (47 COPD patients and 40 controls) and the controls were not cigarette smoking-matched. The second paper was a short communication; the study group was small and they did not consider subgroups of GOLD stages or patients with acute exacerbation of COPD and did not exclude the confounding effects of the drugs used by patients, as inhaled corti-costeroids. One study [67] showed the prevalence of left ventricular systolic dysfunction (to range) from 10 to 46% among patients with exacerbated COPD, and a prevalence of 21% of previously unknown heart failure cases was reported in conjunction with histories positive of COPD or asthma. In that study, the prevalence of left ventricular diastolic dysfunction in COPD patients was 53.4%. Overall, find-ings warrant that we should not ignore the role of high MPV in COPD patients with impaired cardiac function.
Thus, PTL counts, PLT-monocyte aggregates and MPV may serve as simple markers of cardiovascular risk, being a potential target of pharmacological therapy. Despite aggregates forming independently on the cyclooxygenase pathway [68], no study was designed till date to assess whether aspirin or other agents are effective anti-PTLs therapies specifically in the COPD popu-lation, or if the regular use of anti-PTL agents might prevent cardiovascular accidents in these patients.
Clinical implications & treatmentThe anti-PLT agents used in preventing atherothrombosis are aimed at blocking the TxA2 (e.g., aspirin) and interfering with P2Y12-mediated adenosine diphosphate (ADP) stimulation (e.g., clopidogrel). These agents, used either individually or combined, significantly decrease the risk of atherothrombotic events, but a significant residual risk of recurrent ischemic events still remains. According to mainstream literature, this may be due to the persis-tence of elevated PLT reactivity, regardless of whether these agents are used [69,70]. Several novel anti-PLT agents are currently under clinical development, with the goal to achieve higher efficacy [71]. These include agents, such as the P2Y12 receptor antagonists, that block TxA2-mediated effects or that inhibit the protease-activated receptor-1 PLT activation pathway [72].
In the COPD population, the occurrence of PLT hyperreactiv-ity has been demonstrated in ex vivo studies where PLT proved more sensitive to various agonists and elevated levels of plasma b-TG and soluble P-selectin of PLT origin occurred [48]. These reports reflect the presence of in vivo PLT activation as meas-ured by increased synthesis of TxA2 in COPD patients and the
improved respiratory distress in patients with chronic pulmonary emphysema after administering a TxA2 antagonist [20].
Owing to the occurrence of COPD-related vascular events associ-ated with high levels of systemic inflammation, the inhaled corticos-teroids have been considered to have a therapeutical role. These drugs are commonly used in combination with long-acting β-agonists or antimuscarinic agents to specifically lower the lung inflammation.
Although the effect of inhaled steroids does not automatically translate into a reduction of inflammatory biomarkers in the blood stream, withdrawal of inhaled corticosteroids increased baseline C-reactive protein levels by 71%, while 2-week inhala-tion of fluticasone reduced C-reactive protein levels by 50% in stable COPD patients [73].
Overall, the mortality of COPD patients may be positively modified by assumption of inhaled corticosteroids. Patient data from seven randomized trials involving more than 5000 patients has so far shown that inhaled steroids reduced all-cause mortal-ity by about 25% relative to controls on placebo [74]. This rate reduction is similar to that observed after a 3-year therapy with simvastatin in patients with coronary heart disease [75].
This data suggest the potential use of anti-inflammatory agents for improving cardiovascular outcomes in COPD. The improved survival rate may be the consequence of a reduction in cardiovas-cular deaths, which are the effect of inhaled corticosteroids on the vascular plaque inflammation. This intriguing hypothesis enjoys the support of some other observational studies [76].
Recently, the effect of inhaled corticosteroids on mortality has been questioned by the results of an important trial, the ‘Toward a Revolution in COPD Health’ study, which analyzed 6112 patients [77]. In that study, the 3-year mortality rate in the fluticasone group (16%) was comparable to the one observed in the placebo group (15.2%). In patients treated with the combination therapy of fluticasone and long-acting β2-agonist salmeterol, an interesting 17.5% reduction in the risk of death was observed, when compared with placebo. However, the relative impact of these two drugs on the cardiovascular mortality was not reported. Notwithstanding, β2-agonists are known to activate glucocorticoid receptors in the lung [78]. Therefore, these studies have shown that inhaled cor-ticosteroids can modify the expression of membrane proteins on different types of lung cells and that these alterations may induce a reduction of PLT activation and may thus lead to a reduction of cardiovascular mortality in patients with COPD.
In fact, the only treatment that improves the survival in COPD is long-term oxygen therapy in hypoxemic patients [79]. Indeed, oxygen therapy per se might prevent the hypoxia-induced PLT activation and blood clotting and part of its clinical benefit may be the result of a reduction in atherothrombotic fatal events.
Expert commentaryThe recent body of evidence suggests that PTL reactivity is enhanced in COPD patients and that PTL activation is increased both in patients with stable disease and during an acute exacerbation, when compared with age and cigarette smoke exposure-matched controls.
Recent data show a link between high MPV, a marker of PTLs activation, and impaired cardiopulmonary function in the COPD
479www.expert-reviews.com
COPD & platelet activation

Review
population. PTL activation represents a novel mechanism linking COPD, inflammation and cardiovascular diseases. Indeed, PTL activation is central to the development of atherosclerotic plaques, structural remodeling of pulmonary vasculature and changes in systemic vascular function (namely increased arterial stiffness) typical of COPD.
The Rotterdam Study [80] has recently shown that elderly patients with COPD had a higher prevalence of carotid artery plaques, and that COPD per se is an independent risk factor for vulnerable plaques, confronting 253 patients with COPD and 920 healthy subjects. In this perspective, PTLs function may change as a direct consequence of COPD; therefore, identifying PTL activation as an important prothrombotic manifestation of the disease may provide a useful therapeutic target in these patients.
Whether the addition of acetyl-salicylic acid or other anti-PTL agents to the pharmacological therapies of COPD may act as the primary prevention against the vascular diseases, still needs to be elucidated in long-term prospective clinical trials.
Five-year viewNotwithstanding the actual body of evidence, gaps are still present, thus making it still difficult to draw any firm conclusion on the exact role of PLT function within the natural course of COPD.
The natural evolution of research in this field will need to cover unexplored or unclear aspects before translating the messages into clinical practice.
First, the exact mechanism of PTL activation in these patients has yet to be fully investigated. Indeed, the exact role of increased systemic inflammation, hypoxemia and hemody-namic stress should be carefully assessed in the pathogenesis of PTLs activation.
Second, since circulating leukocyte and neutrophil concentra-tions depend on the occurrence of PLT-monocyte aggregates, the heterogeneity of inflammation that occurs in the COPD popula-tion and the different level of systemic inflammatory response might significantly influence the likely activation of PTLs in the individual patient.
Third, the validity of markers, such as PLT-monocyte aggre-gation, PLT count and MPV, still have to be validated in large samples to confirm their potential role as simple, sensitive and use-ful biomarkers of PTL activation with the aim to better estimate and possibly prevent the amount of disease-specific cardiovascular risk both in the stable phase or during acute exacerbations of the disease.
Financial & competing interests disclosureThe authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending or royalties.
No writing assistance was utilized in the production of this manuscript.
Key issues
• Platelet (PLT) activation is likely to occur early in chronic obstructive pulmonary disease patients and is even likely to increase during acute exacerbation, thus increasing their cardiovascular mortality risk.
• Direct and indirect biomarkers may be useful in assessing the PLT activation in these patients.
• Anti-PLT agents might act in chronic obstructive pulmonary disease patients as a primary prevention against the associated cardiovascular diseases.
ReferencesPapers of special note have been highlighted as:• of interest•• of considerable interest
1 Vanfleteren LW, Spruit MA, Groenen M et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 187, 728–735 (2013).
• Evidencedthatmultimorbidityisacommonconditioninchronicobstructivepulmonarydisease(COPD)patientsandthatalowgradeofinflammationispresentinallthedifferentgroupsofcomorbiditiesthattheyfoundinthesepatients.
2 Ridker PM, Hennekens CH, Buring JE et al. C-reactive protein and other markers of inflammation in the prediction of
cardiovascular disease in women. N. Engl. J. Med. 342, 836–843 (2000).
3 Curkendall SM, DeLuise C, Jones JK et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann. Epidemiol. 16, 63–70 (2006).
4 MacNee W, Maclay J, Mcallister D. Cardiovascular injury and repair in chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 5, 824–833 (2008).
•• EvidencedincreasedcardiovascularriskinCOPD,suggestingthathypoxia,systemicinflammationandoxidativestressinCOPDpatientsmaycontributetocausecardiovasculardiseases.
5 Sin DD, Anthonisen NR, Soriano JB et al. Mortality in COPD: role of comorbidities. Eur. Respir. J. 28, 1245–1257 (2006).
6 McAllister DA, Maclay JD, Mills NL et al. Diagnosis of myocardial infarction following hospitalisation for exacerbation of COPD. Eur. Respir. J. 39,1097–1103 (2012).
7 Donaldson GC, Hurst JR, Smith CJ et al. Increased risk of myocardical infarction and stroke following exacerbation of COPD. Chest 137(5), 1091–1097 (2010).
8 Hoffman M. Remodeling the blood coagulation cascade. J. Thromb. Thrombolysis, 16(1–2), 17–20 (2003).
9 Di Santo A, Amore C, Dell'Elba G et al. Glycogen synthase kinase-3 negatively regulates tissue factor expression in monocytes interacting with activated platelets. J. Thromb. Haemost. 9(5), 1029–1039 (2011).
10 Schumacher A, Liebers U, John M, et al. P-selectin glycoprotein ligand-1 (PSGL-1)
Expert Rev. Hematol. 6(4), (2013)480
Malerba, Clini, Malagola & Avanzi

Review
is up-regulated on leucocytes from patients with chronic obstructive pulmonary disease. Clin. Exp. Immunol. 142(2), 370–376 (2005).
11 Davi G, Patrono C. Platelet activation and atherothrombosis. N. Engl. J. Med. 357, 2482–2494 (2007).
12 Duvoix A, Dickens J, Haq I et al. Blood fibrinogen as a biomarker of chronic obstructive pulmonary disease. Thorax 68, 670–676 (2013) .
• Themeta-analysisanalyzednumerousstudiesaboutCOPDandplasmaleveloffibrinogenandconcludedthatthereisanassociationbetweenhighorlowriskofCOPDexacerbationandleveloffibrinogen,sofibrinogenmaybeusedasapredictivebiomarkerofriskofexacerbationandmortalityinCOPDpatients.
13 Dahl M, Tybjaerg-Hansen A, Vestbo J et al. Elevated plasma fibrinogen associated with reduced pulmonary function and increased risk of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 164, 1008–1011 (2001).
14 Hurst JR, Vestbo J, Anzueto A et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N. Engl. J. Med. 363, 1128–1138 (2010).
15 Stec JJ, Silbershatz H, Tofler GH et al. Association of fibrinogen with cardiovascu-lar risk factors and cardiovascular disease in the Framingham Offspring Population. Circulation 102, 1634–1638 (2000).
16 Lambert MP, Sachais BS, Kowalska MA. Chemokines and thrombogenicity. Thromb. Haemost. 97, 722–729 (2007).
17 Wedzicha JA, Syndercombe-Court, Tan KC. Increased platelet aggregate formation in patients with chronic airflow obstruction and hypoxaemia. Thorax 46, 504–507 (1991).
18 Patrono C, Patrignani P, Rocca B et al. Characterization of biochemical and functional effects of antiplatelet drugs as a key to their clinical development. Thromb. Haemost. 74, 396–400 (1995).
19 Rolin S, Masereel B, Dogne JM. Pros-tanoids as pharmacological targets in COPD and asthma. Eur. J. Pharmacol. 533, 89–100 (2006).
20 Davì G, Basili S, Vieri M et al. Enhanced thromboxane biosynthesis in patients with chronic obstructive pulmonary disease. The Chronic Obstructive Bronchitis and Haemostasis Study Group. Am. J. Respir. Crit. Care Med. 156, 1794–1799 (1997).
21 Ponicke K, Sternitzky R, Mest HJ. Stimulation of aggregation and thrombox-ane A2 formation of human platelets by hypoxia. Prostaglandins Leukot Med. 29, 49–59 (1987).
22 Patrono C. Thromboxane synthesis inhibitors and receptor antagonists. Thromb. Res. Suppl. 11, 15–23 (1990).
23 Gawaz M, Langer H, May AE. Platelets in inflammation and atherogenesis. J. Clin. Invest. 115, 3378–3384 (2005).
24 Boots AW, Haenen GR, Bast A. Oxidant metabolism in chronic obstructive pulmonary disease. Eur. Respir. J. Suppl. 46, 14s–27s (2003).
25 Nowak D, Kasielski M, Antczak A et al. Increased content of thiobarbituric acid-reactive substances and hydrogen peroxide in the expired breath condensate of patients with stable chronic obstructive pulmonary disease: no significant effect of cigarette smoking. Respir. Med. 93, 389–396 (1999).
26 Nowak D, Kalucka S, Bialasiewicz P et al. Exhalation of H2O2 and thiobarbituric acid reactive substances (TBARs) by healthy subjects. Free Radic. Biol. Med. 30, 178–186 (2001).
27 Praticò D, Basili S, Vieri M et al. Chronic obstructive pulmonary disease is associated with an increase in urinary levels of isoprostane F2alpha-III, an index of oxidant stress. Am. J. Respir. Crit. Care Med. 158, 1709–1714 (1998).
28 Devaraj S, Hirany SV, Burk RF et al. Divergence between LDL oxidative susceptibility and urinary F(2)-isopros-tanes as measures of oxidative stress in type 2 diabetes. Clin. Chem. 47, 1974–1979 (2001).
29 Pernerstorfer T, Stohlawetz P, Stummvoll G et al. Low-dose aspirin does not lower in vivo platelet activation in healthy smokers. Br. J. Haematol. 102, 1229–1231 (1998).
30 Hioki Y, Aoki N, Kawano K et al. Acute effects of cigarette smoking on platelet-dependent thrombin generation. Eur. Heart J. 22, 56–61 (2001).
31 Hung J, Lam JYT, Lacoste L et al. Cigarette smoking acutely increases platelet thrombus formation in patients with coronary artery disease taking aspirin. Circulation, 92, 2432–2436 (1995).
32 Harding SA, Sarma J, Josephs DH et al. Upregulation of the CD40/CD40 ligand dyad and platelet–monocyte aggregation in cigarette smokers. Circulation 109, 1926–1929 (2004).
33 Heeschen C, Dimmeler S, Hamm CW et al.; CAPTURE Study Investigators. Soluble CD40 ligand in acute coronary syndromes. N. Engl. J. Med. 348, 1104–1111 (2003).
34 Andre´ P, Nannizzi-Alaimo L, Prasad SK et al. Platelet-derived CD40L: the switch-hitting player of cardiovascular disease. Circulation 106, 896–899 (2002).
35 Falco A, Romano M, Iapichino L et al. Increased solubile CD40 ligand levels in cystic fibrosis. J. Thromb. Haemost. 2, 557–560 (2004).
36 Fimognari FL, Scarlata S, Conte ME et al. Mechanisms of atherothrombosis in chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 3(1), 89–96 (2008).
37 Miller GJ, Bauer KA, Cooper JA et al. Activation of the coagulant pathway in cigarette smokers. Thromb. Haemost. 79, 549–553 (1998).
38 Dominick J. Angiolillo, Goto S. Basic principles of platelet biology and clinical implications. Circ. J. 74, 597–607 (2010).
39 da Costa Martins PA, van Gils JM, Mol A et al. Platelet binding to monocytes increases the adhesive properties of monocytes by up-regulating the expression and functionality of beta1 and beta2 integrins. J. Leukoc. Biol. 79, 499–507 (2006).
40 Schober A, Manka D, von Hundelshausen P et al. Deposition of platelet RANTES triggering monocyte recruitment requires P-selectin and is involved in neointima formation after arterial injury. Circulation 106, 1523–1529 (2002).
41 Zarbock A, Polanowska-Grabowska RK, Ley K. Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Rev. 21, 99–111 (2007).
42 Alciato F, Sainaghi PP, Sola D et al. TNF-alpha, IL-6, and IL-1 expression is inhibited by GAS6 in monocytes/macrophages. J. Leukoc. Biol. 87(5), 869 (2010).
43 Muñoz X, Sumoy L, Ramírez-Lorca R et al. Human vitamin K-dependent GAS6: gene structure, allelic variation, and association with stroke. Hum. Mutat. 23(5), 506–512 (2004).
44 Hurtado B, Abasolo N, Muñoz X et al. Association study between polymorphims in GAS6-TAM genes and carotid atherosclerosis. Thromb. Haemost. 104(3), 592–598 (2010).
45 van Eeden SF, Sin DD. Chronic obstruc-tive pulmonary disease: a chronic systemic
481www.expert-reviews.com
COPD & platelet activation

Review
inflammatory disease. Respiration 75, 224–238 (2008).
46 Maclay JD, McAllister DA, Johnston S et al. Increased platelet activation in patients with stable and acute exacerbation of COPD. Thorax 66, 769–774 (2011).
•• ThisoriginalpaperwasoneofthefirsttoobservethatpatientswithstableCOPDhaveincreasedcirculatingplatelet(PLT)-monocyteaggregatescomparedwithwell-matchedcontrols.PLTactivationisfurtherincreasedinpatientswithCOPDduringanacuteexacerbation.
47 De Castro J, Hernandez-Hernandez A, Rodriguez MC et al. Comparison of changes in erythrocyte and platelet phospholipid and fatty acid composition and protein oxidation in chronic obstruc-tive pulmonary disease and asthma. Platelets 18, 43–51 (2007).
48 Ferroni P, Basili S, Martini F et al, Soluble P-selectin as a marker of platelet hyperac-tivity in patients with chronic obstructive pulmonary disease. J. Invest. Med. 48, 21–27 (2000).
49 Walter RE, Wilk JB, Larson MG et al. Systemic inflammation and COPD: the Framingham Heart Study. Chest 133, 19–25 (2008).
50 Sarma J, Laan CA, Alam S et al. Increased platelet binding to circulating monocytes in acute coronary syndromes. Circulation 105, 2166–2171 (2002).
51 Christie DJ, Kottke-Marchant K, Gorman RT. Hypersensitivity of platelets to adenosine diphosphate in patients with stable cardiovascular disease predicts major adverse events despite antiplatelet therapy. Platelets 19, 104–110 (2008).
52 Gianetti J, Parri MS, Sbrana S et al. Platelet activation predicts recurrent ischemic events after percutaneous coronary angioplasty: a 6 months prospective study. Thromb. Res. 118, 487–493 (2006).
53 Humbert M, Morrell N, Archer S et al. Cellular and molecular pathobiology of pulmonary arterial hypertension. J. Am. Coll. Cardiol. 43, 13–24 (2004).
54 Maclay JD, McAllister DA, Mills NL et al. Vascular dysfunction in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 180, 513–520 (2009).
• Inthisoriginalpaperinvolving18COPDpatientsand17controls,COPDwasassociatedwithincreasedarterialstiffnessthatmayrepresentthemechanisticlinkbetweenCOPDandtheincreasedriskofcardiovasculardiseaseassociatedwiththiscondition.
55 Gawaz M, Langer H, May AE. Platelets in inflammation and atherogenesis. J. Clin. Invest. 115, 3378–3384 (2005).
56 Borgel D, Clauser S, Bornstain C et al. Elevated growth-arrest-specific protein 6 plasma levels in patients with severe sepsis. Crit. Care Med. 34, 219–222 (2006).
57 Sainaghi PP, Alciato F, Carnieletto S et al. Gas evaluation in patients with acute dyspnea due to suspected pulmonary embo-lism. Respir. Med. 103(4), 589–594 (2009).
58 Vaidyula VR, Boden G, Rao AK. Platelet and monocyte activation by hyperglycemia and hyperinsulinemia in healthy subjects. Platelets 17, 577e85 (2006).
59 Smeeth L, Thomas SL, Hall AJ et al. Risk of myocardial infarction and stroke after acute infection or vaccination. N. Engl. J. Med. 351, 2611e18 (2004).
60 Crisafulli E, Marietta M, Venturelli E et al. Platelets count in chronic obstructive pulmonary disease [abstract]. Eur. Respir. J. 40(Suppl.), 76s (2012).
61 Ly HQ, Kirtane AJ, Murphy SA et al. Association of platelet counts on presenta-tion and clinical outcomes in ST-elevation myocardial infarction (from the TIMI Trials). Am. J. Cardiol. 98, 1–5 (2006).
62 Vizioli L, Muscari S, Muscari A. The relationship of mean platelet volume with the risk and prognosis of cardiovascular diseases. Int. J. Clin. Pract. 63, 1509–1515 (2009).
•• Meanplateletvolume(MPV)couldbeanewindependentcardiovascularriskfactorandconsideredanindicatorofPLTfunction.Inthispaper,MPVwaspredictiveofstroke,acutemyocardialinfarctionandrestenosisofcoronaryangioplastyandwasincreasedinthepresenceofobesity,diabetesmellitusandmetabolicsyndrome.
63 Steiropoulos P, Papanas N, Nena E et al. Mean platelet volume and platelet distribution width in patients with chronic obstructive pulmonary disease: the role of comorbidities. Platelets 23, 447–454 (2012).
64 Cui H, Liu L, Wei Z et al. Clinical value of mean platelet volume for impaired cardiopulmonary function in very old male patients with chronic obstructive pulmo-nary disease. Arch. Gerontol. Geriatr. 54(2), 109–112 (2012).
•• Inthisoriginalpaper,theauthorsshowedthathighMPVmayberegardedasanearlypredictivemarkerofimpairedcardiopulmonaryfunctioninCOPD.MPVwasnegativelycorrelatedwithleftventricularejectionfractionandthe
predictedvalueFEV1;moreover,MPVwas
positivelycorrelatedwithrightpulmonaryarterialdiameter.
65 Ulasli SS, Ozyurek BA, Yilmaz EB et al. Mean platelet volume as an inflammatory marker in acute exacerbation of chronic obstructive pulmonary disease. Pol. Arch. Med. Wewn. 122(6), 284–290 (2012).
66 Biljak VR, Pancirov D, Cepelak I et al. Platelet count, mean platelet volume and smoking status in stable chronic obstructive pulmonary disease. Platelets 22(6), 466–470 (2011).
67 Rutten FH, Cramer MJ, Lammers JW et al. Heart failure chronic obstructive pulmonary disease: an ignored combina-tion? Eur. J. Heart Fail. 8, 706–711 (2006).
68 Klinkhardt U, Bauersachs R, Adams J et al. Clopidogrel but not aspirin reduces P-selectin expression and formation of platelet-leukocyte aggregates in patients with atherosclerotic vascular disease. Clin. Pharmacol. Ther. 73, 232–241 (2003).
69 Pettersen AÅ, Seljeflot I, Abdelnoor M et al. High on-aspirin platelet reactivity and clinical outcome in patients with stable coronary artery disease: results from ASCET (Aspirin Nonresponsiveness and Clopidogrel Endpoint Trial). J. Am. Heart Assoc. 1(3), e000703 (2012).
70 Mora S, Wenger NK, Demicco DA et al. Determinants of residual risk in secondary prevention patients treated with high- ver-sus low-dose statin therapy: the Treating to New Targets (TNT) study. Circulation 125(16), 1979–1987 (2012).
71 Briasoulis A, Tousoulis D, Bakogiannis C et al. Novel anti-platelet agents for the treatment of stable angina pectoris. Curr. Pharm. Des. 19(9), 1581–1586 (2013).
72 Barrett NE, Holbrook L, Jones S et al. Future innovations in anti-platelet therapies. Br. J. Pharmacol. 154, 918–939 (2008).
73 Sin DD, Lacy P, York E et al. Effects of fluticasone on systemic markers of inflammation in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 170, 760–765 (2004).
74 Sin DD, Wu L, Anderson JA, et al. Inhaled corticosteroids and mortality in chronic obstructive pulmonary disease. Thorax 60, 992–997 (2005).
• Inthispooledanalysis,patientdatafromsevenrandomizedtrials(involving5085patients)werecollected:inhaledcorticosteroidsreducedall-causemortalitybyabout25%relativetoplacebo.This
Expert Rev. Hematol. 6(4), (2013)482
Malerba, Clini, Malagola & Avanzi

Review
beneficialeffectwasespeciallynoticeableinwomenandformersmokers.
75 Pedersen TR, Kjekshus J, Berg K et al. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Atheroscler. Suppl. 5(3), 81–87 (2004).
76 Macie C, Wooldrage K, Manfreda J et al. Inhaled corticosteroids and mortality in COPD. Chest 130, 640–646 (2006).
77 Calverley PM, Anderson JA, Celli B et al; TORCH investigators. Salmeterol and fl
uticasone propionate and survival in chronic obstructive pulmonary disease. N. Engl. J. Med. 356, 775–789 (2007).
78 Eickelberg O, Roth M, Lorx R et al. Ligand-independent activation of the glucocorticoid receptor by beta2-adrener-gic receptor agonists in primary human lung fi broblasts and vascular smooth muscle cells. J. Biol. Chem. 274, 1005–1010 (1999).
79 Afessa B, Morales IJ, Scanlon PD, Peters SG. Prognostic factors, clinical course, and
hospital outcome of patients with chronic obstructive pulmonary disease admitted to an intensive care unit for acute respiratory failure. Crit. Care Med. 30, 1610–1615 (2002).
80 Lahousse L, Van der Bouwhuijsen QJA, Loth DV et al. Chronic obstructive pulmonary disease and lipid core carotid artery plaques in the elderly. The Rotterdam Study. Am. J. Respir. Crit. Care Med. 187, 58–64 (2013).
483www.expert-reviews.com
COPD & platelet activation