Perioperative Interstitial Brachytherapy for Soft Tissue Sarcomas: Prognostic Factors and Long-Term...
-
Upload
siddhartha-laskar -
Category
Documents
-
view
228 -
download
0
Transcript of Perioperative Interstitial Brachytherapy for Soft Tissue Sarcomas: Prognostic Factors and Long-Term...

Perioperative Interstitial Brachytherapy for Soft TissueSarcomas: Prognostic Factors and Long-Term Results of
155 Patients
Siddhartha Laskar, MD,1 Gaurav Bahl, MD,1 Ajay Puri, MS,2 Manish G. Agarwal, MS,2
MaryAnn Muckaden, MD,1 Nikhilesh Patil, MD,1 Nirmala Jambhekar, MD,3
Sudeep Gupta, DM,4 Deepak D. Deshpande, PhD,5 Shyam K. Shrivastava, MD,1 andKetayun A. Dinshaw, FRCR1
1Department of Radiation Oncology, Tata Memorial Hospital, Dr. Ernest Borges Road, Parel, Mumbai, India2Department of Surgery, Tata Memorial Hospital, Mumbai, India
3Department of Pathology, Tata Memorial Hospital, Mumbai, India4Department of Medical Oncology, Tata Memorial Hospital, Mumbai, India5Department of Medical Physics, Tata Memorial Hospital, Mumbai, India
Background: The goal of this study was to evaluate the efficacy of temporary interstitialbrachytherapy (BRT) for patients undergoing combined modality management of soft tissuesarcomas (STS).Methods: From January 1990 to December 2003, 155 adults 18–88 years of age (median =
42 years) with STS who had received BRT as part of locoregional treatment were included inthis review. Sixty-four percent were males. Sixty-nine percent had primary lesions. Sixtypercent had lesions involving the lower extremities. Spindle cell sarcoma (28%) and synovialsarcoma (16%) were the most common histologic types and 51% had grade III lesions.Treatment included wide local excision of primary tumor with BRT with or without externalbeam radiotherapy (EBRT).Results: After a median followup of 45 months, the local control (LC), disease-free survival
(DFS), and overall survival (OS) for the entire cohort was 71%, 57%, and 73%, respectively.DFS was superior for superficial tumors compared with that for deep tumors (96% vs. 54%,P =.02). Patients with a tumor less than 5 cm had superior OS (88% vs. 63%, P =.05).Cumulative radiotherapy dose greater than 60 Gy had a significant positive impact on LC(P = .003), DFS (P =.003), and OS (P =.048). Subcutaneous fibrosis (21%) was the majorcomplication.Conclusions: Temporary perioperative iridium-192 interstitial BRT with or without EBRT
after function-preserving surgery results in satisfactory outcome in patients with STS. Bothlow dose rate and high dose rate BRT are equivalent in terms of disease control and com-plications when used alone or in combination with EBRT. BRT results in fewer complicationscompared with the combination of BRT and EBRT.Key Words: Soft tissue sarcoma—Radiotherapy—Interstitial brachytherapy..
Soft tissue sarcomas (STS) are a heterogeneousgroup of malignant tumors arising from the sup-porting extraskeletal mesenchymal tissues of thebody. They are a group of relatively uncommon, butaggressive, neoplasms that represent approximately1% of all cancers. Local management of adult STS
Received April 12, 2006; accepted June 19, 2006; publishedonline November 11, 2006.Address correspondence and reprint requests to: Siddhartha
Laskar, MD; E-mail: [email protected]
Published by Springer Science+Business Media, Inc. � 2006 The Society ofSurgical Oncology, Inc.
Annals of Surgical Oncology 14(2):560–567
DOI: 10.1245/s10434-006-9137-2
560

includes surgery combined with radiotherapy. Opti-mal therapy aims at eradicating local disease withminimal functional disability. Although surgicalresection remains the primary therapeutic modalityfor all localized tumors, it is now established thatconservative function-preserving excision followed byadjuvant irradiation provides adequate local controlwith good cosmetic and functional outcome andquality of life.Postoperative external beam radiotherapy (EBRT)
has played a pivotal role in the local control of thesetumors and is an integral component of most treat-ment protocols. However, there are significant latetoxicities associated with the high doses of EBRTrequired to achieve satisfactory local control (LC),such as tissue fibrosis, loss of joint motion, neuritis,and limb edema. Brachytherapy (BRT) has emergedas an attractive modality by which these complica-tions may be reduced without compromising ade-quate irradiation of the tumor bed. This treatmentapproach, used alone or in combination with EBRT,delivers high doses of radiation to the tumor volumein a very precise and localized manner while sparingthe nearby normal tissues. Furthermore, the overalltreatment time is significantly shortened while main-taining a comparable high rate of LC. The ability tospare normal tissues significantly allows BRT to beused postoperatively with recurrent disease in previ-ously irradiated patients. In an attempt to furtherdefine the efficacy of BRT, we reviewed our experi-ence with BRT in adults with STS.
PATIENTS AND METHODS
From January 1990 to December 2003, 155 adultswith nonmetastatic STS underwent conservativeorgan- and function-preserving surgery and periop-erative interstitial BRT with or without EBRT at ourinstitution. Patients were 18–88 years of age with amedian age of 42 years at presentation. There were99(64%) males and 56(36%) female patients.Approximately one-third (31%) were treated forrecurrent disease. The lower extremities were mostcommonly involved (60%), followed by the upperextremities (19%), the chest and abdominal walls(19%), and the head and neck region (1%). The mostcommon histologic types in this study were spindlecell sarcoma (28%) and synovial sarcoma (16%), fol-lowed by a diverse group of histologies, includingliposarcoma (14%), malignant fibrous histiocytomas(9%), fibrosarcoma (7%), malignant peripheralnerve sheath tumor (6%), rhabdomyosarcoma (5%),
lieomyosarcoma (5%), and various other soft tissuesarcomas. Seventy-nine patients (51%) had grade III,38 (25%) had grade II, and 38 (25%) had grade I le-sions. The diameter of the tumors ranged from 2 to 20cm (median = 7 cm). Sixty-seven patients (43%) hadtumors less than 5 cm in maximum diameter. In eightpatients (5%) the surgical margins were positive and insix (4%) they were close. The tumor size was deter-mined from the gross pathologic description whenavailable, or else from the initial clinical description.Tumor grade, histologic subtype, and margins wereobtained from the microscopic description by expe-rienced pathologists. Table 1 presents the pertinentclinical and pathologic patient information.All patients received treatment consisting of con-
servative surgery in the form of wide local excision(WLE) of the tumor followed by postoperativeradiotherapy. The skin closure was primary in 142(91%) of patients while 11 (7%) underwent recon-struction of the skin defect with a pedicle graft andtwo patients had a split skin graft. Fifty-five patients(36%) were treated with radical BRT alone while 100patients (64%) received a combination of BRT andEBRT (EBRT dose range = 20–50 Gy, median = 46Gy). While in 98 (63%) patients BRT was deliveredusing low dose rate (LDR), 57 (37%) were treatedwith high dose rate (HDR) BRT. The BRT dosevaried depending on whether the patient would re-ceive further EBRT. The median cumulative dose ofradiation in the group receiving BRT and EBRT was69.9 Gy. In the group receiving BRT alone, themedian doses were 39 Gy and 34.5 Gy in the LDRand HDR groups, respectively.
Brachytherapy Technique
All patients included in this study were treated withtemporary perioperative interstitial BRT using irid-ium-192. After WLE the tumor bed was demarcatedby both the surgeon and the radiation oncologistusing radiopaque surgical clips. Plastic afterloadingcatheters were introduced into the tumor bed using16-gauge stainless-steel needles. The implanted areagenerally included the tumor bed with a 2-cm radialmargin. The longitudinal margin depended on theintent of BRT. When BRT was intended to be usedas a boost along with EBRT, the margin was 2 cmbeyond the tumor bed, while the margin was increasedto 3–4 cm if the plan was to use radical BRT alone.The catheters were placed parallel to each other at adistance of 1.0–1.5-cm intervals. No effort was madeto include the drain sites within the implanted volume.A single-plane arrangement was used for all patients.
INTERSTITIAL BRACHYTHERAPY FOR ADULT STS 561
Ann. Surg. Oncol. Vol. 14, No. 2, 2007

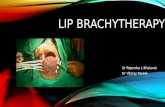
Catheters were inserted at at a depth of approximately5 mm into the tumor bed to avoid underdosage of thetumor bed. In situations in which the catheters couldnot be anchored to the tumor bed, resorbable sutureswere used to secure the catheters onto the tumor bed.If required, gel-foam or thin muscle flaps were inter-posed between the catheter plane and neighboringcritical structures. Finally, catheters were secured inposition using stainless-steel buttons and plastic beads(Figs. 1 and 2). After the procedure, the surgicalincision was closed either by primary closure or, ifnecessary, with the reconstruction of the surgical de-fect with regional or microvascular free flaps.Orthogonal radiographs were taken on the fourth or
fifth postoperative day for dosimetry and treatmentplanning. Treatment was generally started on thesame day as dosimetry. The EBRT + BRT dose wasbased on the intent of BRT (radical vs. boost) and theBRT dose rate (HDR vs. LDR).
Statistical Analysis
Followup information was abstracted from pa-tients� hospital records and from an existing databaseof patients undergoing BRT. Because BRT is pri-marily a local treatment, disease control at the primarysite/tumor bed was the primary endpoint evaluated inthe study. Local failure was defined as recurrence or
TABLE 1. Tumor characteristics
Histologic type (WHO)
Histologic grade Tumor depth Tumor size Site of primary tumor
Trunk andhead and neck
Gr
Superficial Deep £5 cm >5 cmUpperextremity
LowerextremityGr I Gr II Gr III
Fibromatoses 2 0 0 1 1 1 1 1 1 0Fibrosarcoma 3 3 4 3 7 5 5 1 3 6DMFP 5 1 1 7 0 5 2 0 1 6MFH 1 5 8 3 11 6 8 5 7 2Liposarcoma 6 5 11 2 20 8 14 3 16 3Leiomyosarcoma 0 3 4 2 5 4 3 2 4 1Synovial sarcoma 7 8 9 6 18 11 12 5 17 2MPNST 1 2 6 2 7 4 5 4 5 0Extraskeletal chondrosarcoma 0 1 0 0 1 1 0 1 0 0Alv soft part sarcoma 0 1 0 0 1 0 1 0 1 0Epithelioid sarcoma 0 1 1 0 2 1 1 0 2 0Neurofibroma 1 0 0 0 1 1 0 1 0 0Spindle cell sarcoma 9 6 28 9 34 17 25 6 29 8Undifferentiated 0 0 2 1 1 0 2 0 1 1RMS 2 2 3 1 6 2 5 1 5 1Others 1 0 2 0 3 1 2 0 1 2Total 38 38 79 37 118 67 86 30 93 32
DMFP, dermatofibrosarcoma protuberans; MFH, malignant fibrous histiocytoma; MPNST, malignant peripheral nerve sheath tumor;Alv, alveolar; RMS, rhabdomyosarcoma.
FIG. 1. Tumor bed with 16-gauge stainless-steel needles in situ. FIG. 2. Stainless-steel needles replaced by plastic catheters.
S. LASKAR ET AL.562
Ann. Surg. Oncol. Vol. 14, No. 2, 2007

progression within or at the margin of the irradiatedfield. Disease-free survival (DFS) was calculated fromthe date of registration to the date of recurrence ofdisease at any site, and overall survival (OS) was cal-culated from the date of registration to the date ofdeath due to any cause. LC, DFS, and OS rates werecalculated using the Kaplan–Meier method. Multiple-covariate analysis was performed using the stepwiseCox proportional hazards regression model. Thehazard ratios (HR) with the 95% confidence interval(CI) were calculated. Complications were recorded aseither acute or chronic if they occurred within threemonths or more than 3 months after completion oftreatment, respectively. Events were scored accordingto the Radiation Therapy Oncology Group (RTOG)late radiation morbidity scoring system.
RESULTS
After a median followup of 45 months (range =1-132 months), 125 (81%) patients were alive with-out disease, 12 (8%) patients were alive with disease,and 18 (11%) patients had died due to disease. The
LC, DFS, and OS for the whole cohort were 71%,57%, and 73%, respectively. The overall results/prognostic factors are summarized in Table 2.Table 3a and 3b highlights the patterns of failureaccording to tumor characteristics and type ofradiotherapy treatment.
Local Control
Of the 155 patients treated, 10 developed recurrentdisease within the BRT site. The 5-year LC rate forthe whole group was 71%. Patients with a maximumtumor diameter less than or equal to 5 cm had a LCof 87% vs. 62% for those with a tumor diametergreater than 5 cm (P = .79). Patients with superficialand deep tumors had LC rates of 96% and 54%,respectively (P = .20). Age at presentation, gender,site of primary tumor (upper extremities vs. lowerextremities vs. trunk), grade of the tumor, and type oftumor (primary vs. recurrent) did not significantlyinfluence the LC (Table 2). Furthermore, patientswith microscopically positive and negative surgicalmargins had similar LC rates of 45% and 51%,
TABLE 2. Results
Prognostic factors n
Local control Disease-free survival Overall survival
% Significance % Significance % Significance
Overall 155 71 57 73Age £40 yr 69 81 P = .32 65 P = .33 58 P = .27
>40 yr 85 59 48 81Gender Male 99 80 P = .63 60 P = .17 72 P = .11
Female 56 61 56 78Size £5 cm 67 87 P = .79 78 P = .22 88 P = .05
> 5cm 86 62 46 63Depth Superficial 37 96 P = .20 90 P = .05 93 P = .18
Deep 118 54 42 67Site Upper limb 30 84 P = .91 69 P = .46 70 P = .33
Lower limb 93 60 47 67Trunk 32 72 62 92
Tumor Primary 106 90 P = .19 71 P = .61 61 P = .46Recurrent 48 52 44 85
Grade Gr I 38 83 P = .89 78 P = .31 81 P = .72Gr II 38 72 59 84Gr III 79 67 49 67
Surgical margin + ve 8 45 P = .29 66 P = .70 46 P = .07Close 6 100 100 100) ve 141 51 63 72
Symptom duration £3 mo 52 83 P = .51 67 P = .72 73 P = .43>3 mo 102 69 56 73
RT type BRT 54 63 P = .13 50 P = .38 52 P = .76EBRT + BRT 100 74 59 79
EBRT + BRT Group:Dose rate LDR 57 73 P = .72 58 P = .73 78 P = .84
HDR 43 97 84 89Cumulative dose £60 Gy 7 0 P = .0003 0 P = .003 36 P = .048
>60 Gy 93 97 79 84Radical BRT Alone Group:Dose rate LDR 40 65 P = .44 52 P = .58 56 P = .0016
HDR 14 50 44 40
INTERSTITIAL BRACHYTHERAPY FOR ADULT STS 563
Ann. Surg. Oncol. Vol. 14, No. 2, 2007

respectively (P = .29). Patients receiving a combi-nation of BRT and EBRT had LC of 74% comparedwith 63% (P = .13) for those receiving BRT alone.Among the 100 patients treated with a combinationof BRT and EBRT, the cumulative radiation dosesignificantly influenced the incidence of local diseaserecurrence. The LC rate was significantly superior inthe group receiving cumulative radiation doses equalto or greater than 60 Gy (P = .003) (Fig. 3). Thisretained significance on multivariate analysis, and thehazard ratio (HR) for local failure in the group ofpatients receiving a cumulative RT dose of less than60 Gy was 3.72 (95% CI: 1.35-9.51) (Table 5). In thissame subgroup, there was no statistically significantdifference in the LC rates between the patients whoreceived BRT using HDR versus those receivingLDR BRT (96% vs. 73%, P =.72). Of the 55 patientswho received radiotherapy in the form of radicalBRT alone, the LC rates were 65% and 50% in thegroups receiving LDR and HDR BRT, respectively(P =.44).
Disease-Free and Overall Survival
The 5-year DFS and OS for the entire group were57% and 73%, respectively. Eighteen patients (12%)
died due to disease, 10 (6%) were alive with disease,and the remaining 127 (82%) were alive without evi-dence of disease at the time of analysis. Fifteen of the20 (75%) patients who had developed distant metas-tasis died due to the disease. All three patients whohad developed distant metastasis as well as a localrecurrence died of their disease. Five of the sevenpatients (71%) who had failed locally were alive withdisease, and the other two patients with local recur-rence, who had been treated with salvage surgery andfurther radiotherapy, were alive without disease. Themost common site of distant metastases was thelungs.Patients with a maximum tumor diameter less than
or equal to 5 cm had an OS of 88% vs. 63% for thosewith lesions greater than 5 cm (P = .05). Althoughthere was a clear difference in the DFS between thesetwo groups (78% vs. 46%), this did not attain statis-tical significance (P = .22). Patients with superficialtumors had a better outcome than those with deepones, the DFS and OS being 90% vs. 42% (P = .05)(Fig. 4) and 93% vs. 67% (P = .18), respectively. Ageat presentation, gender, site of primary tumor (upperextremities vs. lower extremities vs. trunk), grade ofthe tumor, and type of tumor (primary vs. recurrent)did not significantly influence the DFS or OS(Table 2). The DFS was 50% vs. 59% (P = .38) andOS was 52% vs. 79% (P = .76) for patients receivingBRT alone and. BRT + EBRT, respectively. In pa-tients treated with a combination of BRT and EBRT,those who had received a cumulative dose greaterthan 60 Gy had a significant improvement in DFScompared with those receiving doses less than 60 Gy(P = .003). Similarly, the OS was 36% vs. 84% be-tween those receiving doses less than 60 Gy versus
TABLE 3A. Tumor characteristics vs. patterns of failure
Localrecurrence
Distantmetastasis
Local anddistant failure
Tumor size£5 cm (n = 67) 3 (4%) 6 (9%) 1 (1%)> 5cm (n = 85) 4 (5%) 14 (16%) 2 (2%)DepthSuperficial (n = 37) 1 (3%) 2 (5%) 0 (0%)Deep (n = 117) 6 (5%) 18 (15%) 3 (3%)SiteUpper limb (n = 30) 2 (7%) 3 (10%) 1 (3%)Lower limb (n = 92) 3 (3%) 14 (15%) 2 (2%)Trunk (n = 32) 2 (2%) 3 (9%) 0 (0%)Tumor typePrimary (n = 107) 3 (3%) 15 (14%) 2 (2%)Recurrent (n = 48) 4 (8%) 5 (10%) 1 (2%)GradeI (n = 38) 1 (3%) 2 (5%) 1 (3%)II (n = 38) 2 (5%) 5 (5%) 0 (0%)III (n = 78) 4 (5%) 13 (17%) 2 (3%)
TABLE 3B. Radiotherapy vs. patterns of failure
Radiotherapytype
Localrecurrence
Distantmetastasis
Local anddistant failure
BRT aloneLDR (n = 41) 3 (7%) 5 (12%) 1 (2%)HDR (n = 14) 1 (7%) 0 1 (7%)BRT + EBRTLDR (n = 57) 3 (5%) 9 (16%) 1 (2%)HDR (n = 43) 1 (2%) 5 (12%) 0
FIG. 3. Kaplan-Meier curve for local control comparingcumulative RT dose as a factor.
S. LASKAR ET AL.564
Ann. Surg. Oncol. Vol. 14, No. 2, 2007

more (P = .04) (Fig. 5). On multivariate analysis, thehazard ratio (HR) for death in the group of patientsreceiving a cumulative RT dose of less than <60 Gywas 3.39 (95% CI: 0.98–6.39) (Table 4). Within thissame subgroup, the patients who received LDR BRThad a DFS of 58% vs. 84% for HDR (P = .73).Similarly, the OS was 78% vs. 89% (P = .84),respectively, between the two groups. Among the 55patients receiving radiotherapy in the form of BRTalone, the DFS was 52% vs. 44% (P = .58) betweenLDR and HDR BRT, respectively. Similarly, the OSwas 56% vs. 40% (P = .16) between LDR and HDRBRT.Complications (Table 5 Subcutaneous fibrosis was
the major late sequelae (21%) followed by distal limbedema (10%) and wound dehiscence (6%). Impairedjoint mobility was documented in 5% patients. Theincidence of subcutaneous fibrosis, distal limb edema,wound dehiscence, and impairment of joint mobilitywas more in the group receiving BRT + EBRTcompared to BRT alone (30% vs. 5%, 15% vs. nil, 7%vs. 5%, and 8% vs. nil. respectively).
DISCUSSION
Treatment strategies for adults with soft tissuesarcomas have evolved over the years. Withimprovement in surgical and radiotherapeutic tech-niques and with better understanding of the naturalhistory of these tumors, the focus now is on organand function preservation with improvement ofquality of life of the patients. More ablative proce-dures like amputation and compartmental excision
have given way to conservative approaches like WLEand radiation therapy without compromising ondisease control.1–4 Radiation therapy in the form ofEBRT and BRT, used either alone or in combination,has been established as an important component ofthese multimodal approaches in the management ofSTS. Experiences of Suit et al.,5 Martin et al.,3 andLindberg et al.6 lead to the concept of limited surgeryand high-dose radiation therapy in STS resulting inLC rates of 80%-90%. In our earlier publication fromthe Tata Memorial Hospital,7 we had reported two-year local control rates of 86% and 82%, respectivelyfor patients receiving BRT + EBRT and BRT alone,respectively. In our current series we report LC, DFS,and OS of 71%, 57%, and 73%, respectively, after alonger median followup of 45 months. Pisters et al.,8
in a randomized trial comparing WLE versus WLE+ BRT, showed superior results in the groupreceiving BRT. They reported a LC rate of 91%which is comparable to local control rates reported inother series using postoperative EBRT.9,10 Thecurrent series reports LC rates of 62.8% and 73.7%(P = .1) for patients receiving BRT alone and BRT+ EBRT, respectively. Brennen et al.,11 Harrison
TABLE 5. Late toxicity
Complications Pts. (%) BRT (%) BRT + EBRT (%)
Subcutaneous fibrosis 33 (21%) 3/55 (5%) 30/100 (30%)Distal limb oedema 15 (10%) – 15/100 (15%)Wound dehiscence 10 (6%) 3/55 (5%) 7/100 (7%)Impaired joint movement 8 (5%) – 8/100 (8%)
FIG. 4. Kaplan-Meier curve for disease-free survival comparingtumor depth as a factor.
TABLE 4. Multiple-covariate Cox regression analysis for prognostic factors
Variable
Local control Disease-free survival Overall survival
P value HR 95.0% CI P value HR 95.0% CI P value HR 95.0% CI
Size > 5 cm 0.48 2.94 0.14–2.52 0.12 2.07 0.48–3.41 0.07 2.79 0.92–8.51Deep tumor 0.26 3.65 0.39–13.34 0.77 2.91 0.88–9.77 0.29 2.12 0.24–10.3Recurrent tumor 0.49 1.62 0.39–6.60 0.95 1.97 0.43–219 0.44 1.68 0.20–1.99BRT alone 0.37 1.29 0.71–1.10 0.68 1.33 0.32–1.46 0.61 1.31 0.46–3.74Cumulative RT dose > 60 Gy 0.024 3.72 1.35–9.51 0.047 3.39 1.02–9.44 0.055 3.10 0.98–6.38
CI, confidence interval; HR, hazard ratio; BRT, brachytherapy.
INTERSTITIAL BRACHYTHERAPY FOR ADULT STS 565
Ann. Surg. Oncol. Vol. 14, No. 2, 2007

et al.,12 and Habrand et al.13 have also demonstratedsimilar LC rates with the use of BRT. However, inmost of their trials the advantage of BRT was re-stricted primarily to high-grade tumors. The possibleexplanation for the absence of LC advantage withBRT for low-grade tumors has been ascribed to theslower progress along the cell cycle for these tumorscompared to the high-grade tumors. As a conse-quence, the total duration of the BRT treatment (4–5days) may not be able to catch all the tumor cells intheir radiosensitive phase. In the randomized trial byPisters et al.,8 the authors reported no additionaladvantage of interstitial BRT for disease control inlow-grade tumors. In the current study a significantproportion of patients received HDR BRT (over 4–5days). Suit et al.14 reported a strong correlation be-tween tumor grade and disease-free survival, withDFS of 83% for grade I and 17% for grade III tu-mors. In a study from the Memorial Sloan KetteringCancer Centre (MSKCC) by Alekhteyar et al.,15
there was no difference in the two-year actuarial LCrate between the BRT + EBRT group (90%) and theBRT-alone group (82%) (P = .32). However, forpatients with positive resection margins, the use ofBRT + EBRT produced better local control thanBRT alone (P = .08). In our study only 8 of the 155patients had positive resection margins and we ob-served no difference in outcome compared with thosewith negative margins. However, statistical interpre-tation of this small number of patients with micro-scopically positive margins may be erroneous and wedo not base any conclusions on this finding.It has been well established that large tumor size is
associated with poor DFS and OS.16,17 Authors havereported inferior LC rates in patients with tumors
equal to or greater than 5 cm compared with tumorsless thanor equal to 5 cm. It has also beenobserved thattumors equal to or greater than 10 cm were associatedwith a greater rate of distant metastasis. In our presentseries we observed a higher rate of distant metastasesamong patients with tumors equal to or greater than 5cm compared with smaller tumors, resulting in aninferior OS (63.3% vs. 88%, P =.05). Our results alsoshowed better DFS in patients with superficial tumorscompared to deep-seated tumors (90.3% vs. 41.5%,P= .05). The incidence of distant metastasis is higheramong patients with local failure compared with thosewith disease locally controlled (30% vs. 14%, P= .17).Although this difference did not achieve statisticalsignificance, there seems to be a definite trend towardincreased incidence of distant metastasis in patientswith local failure. Other investigators have also ob-served a reduction in the incidence of distantmetastasiswith improvement in local disease control.12,18,19
The impact of radiation therapy on wound com-plication rates has been widely evaluated in the past.In the current study the most significant complicationwas subcutaneous fibrosis (21%). There was no dif-ference in the complication rates between patientsundergoing primary wound closure versus those whounderwent reconstructive surgery. In a randomizedtrial from MSKCC20 of BRT vs. no further RT aftercomplete tumor excision, the authors reported woundcomplication rates of 24% in the BRT group and 14%in the no-BRT group (P = .13). However, theyhighlighted that wound reoperation rates after BRTwere higher if the width of the skin excised duringsurgery was more than 4 cm. Arbeit et al.21 reported asignificantly higher complication rate in the BRTversus the no-BRT groups (48% vs. 16%, P = .01),whereas Ormsby et al.22 found no difference in thecomplication rates between the two arms (14% vs.10%). This difference in complication rates betweenthe two studies was attributed to the difference in thedelay in loading the radioactive sources after thesurgery in the two studies. In the Arbeit et al. study21
the mean time for loading was 4.3 days comparedwith 6.1 days in the Ormsby et al. study.22 The time-dependent effect of radiation damage on woundhealing has been demonstrated in animal models.Devereux et al.23 showed that timing of radiationtherapy and the combination of antineoplastic agentscould impair normal wound healing. They suggestedthat radiation or antineoplastic drugs used seven daysbefore or after surgery could inhibit wound healing.This was attributed to the inhibition of newly syn-thesized collagen as determined using hydroxyprolineassays and force tension curves. In a randomized trial
FIG. 5. Kaplan-Meier curve for overall survival comparing tumorsize as a factor.
S. LASKAR ET AL.566
Ann. Surg. Oncol. Vol. 14, No. 2, 2007

of preoperative versus postoperative radiotherapyreported by O�Sullivan et al.,24 the authors reported ahigher acute wound complication rate in the preop-erative versus the postoperative group (35% vs. 17%,P = .01). At our institute the policy is to start radi-ation treatment on the fourth or fifth day after sur-gery.In conclusion, we state that interstitial BRT with or
without EBRT is an effective modality in the con-servative management of STS. Future studies usingBRT should try to stratify patients into treatmentgroups based on clinicopathologic factors so thatselected patients could be treated with BRT alonewithout compromising on disease control rates,especially in the current context of increasing use ofsystemic chemotherapy along with radiation therapyin patients with high-grade extremity STS.
REFERENCES
1. Liebel SA, Tranbaugh RF, Wara WM, et al. Soft tissuesarcomas of the extremities. Survival and patterns of failurewith conservative surgery and postoperative irradiation com-pared to surgery alone. Cancer 1987; 50:1076–1083.
2. Cantin J, McNeer GP, Chu FC, et al. The problem of localrecurrence after treatment of soft tissue sarcoma. Ann Surg1968; 168:47–3.
3. Martin RG, Butler JJ, Albores-Saavedra. J. (1965) Soft tissuetumors: surgical treatment and results. Tumors of bone and softtissue. Chicago: Year Book Medical Publishers, pp 333–48.
4. Shiu HN, Castro EB, Hajdu SI, et al. Surgical treatment of 297soft tissue sarcoma of the lower extremity. Ann Surg 1975;182:597–02.
5. Suit HD, Russel WO, Martin RG, et al. Management of pa-tients with sarcomas of soft tissue in an extremity. Cancer 1973;31:1255–297.
6. Lindberg RD, Martin RG, Romsdhal MM. Surgery and post-operative radiotherapy in the treatment of soft tissue sarcomain adults. AJR Am J Roentgenol 1975; 123:123–29.
7. Chaudhary AJ, Laskar S, Badhwar R. Interstitial brachyther-apy in soft tissue sarcomas: The Tata Memorial HospitalExperience. Strahlenther Onkol 1998; 174(10):522–28.
8. Pisters PW, Harrison LB, Woodruff JM, et al. A prospectiverandomised trial of adjuvant brachytherapy in the manage-ment of low grade soft tissue sarcomas of the extremity andsuperficial trunk. J Clin Oncol 1994; 12:1150–1155.
9. Suit HD, Mankin HJ, Wood WC, et al. Treatment of the pa-tient with stage M0 soft tissue sarcoma. J Clin Oncol 1998;6:854–63.
10. Karakousis CP, Emrich IJ, Rao U, et al. Feasibility of limbsalvage and survival in soft tissue sarcomas. Cancer 1988;57:484–491.
11. Brennan MF, Hilaris B, Shiu MH, et al. Local recurrencein adult soft tissue sarcoma. Arch Surg 1987; 122:1289–1293.
12. Harrison LB, Franzese F, Gaynor JJ, et al. Long-term resultsof a prospective randomized trial of adjuvant brachytherapy inthe management of completely resected soft tissue sarcomas ofthe extremity and superficial trunk. Int J Radiat Oncol BiolPhys 1993; 27(2):259–265.
13. Habrand JL, Gerabaulet A, Pejovic MH, et al. Twenty yearsexperience of interstitial iridium brachytherapy in the man-agement of soft tissue sarcomas. Int J Radiat Oncol Biol Phys1991; 20:405–411.
14. Suit HD, Russel RO, Martin RG. Sarcomas of soft tissue:clinical and histologic parameters and response to treatment.Cancer 1975; 35:1478–1483.
15. Alekhteyar KM, Leung DH, Brennan MF, et al. The effect ofcombined external beam radiotherapy and brachytherapy onlocal control and wound complications in patients with high-grade soft tissue sarcomas of the extremity with positivemicroscopic margin. Int J Radiat Oncol Biol Phys 1996;36(2):321–324.
16. Tepper JE, Rosenberg SA, Glatstein E. Radiation therapytechnique in soft tissue sarcomas of the extremity—policies oftreatment at the NCI. Int J Radiat Oncol Biol Phys 1983;8:263–293.
17. Torosian MH, Fredrick C, Godbold J, et al. Soft tissue sar-comas. Initial characteristics and prognostic factors in patientswith or without metastatic disease. Semin Surg Oncol 1980;4:13–19.
18. Rosenberg SA, Tepper J, Glatstein E, et al. The treatment ofsoft-tissue sarcomas of the extremities: prospective randomizedevaluations of (1) limb-sparing surgery plus radiation therapycompared with amputation and (2) the role of adjuvant che-motherapy. Ann Surg 1982; 196(3):305–315.
19. Strotter AT, A�Herm RP, Fisher C, et al. The influence of localrecurrence of extremity soft tissue sarcoma on metastasis andsurvival. Cancer 1990; 65:1119–1129.
20. Alektiar KM, Zelefsky MJ, Brennan MF. Morbidity of adju-vant brachytherapy in soft tissue sarcoma of the extremity andsuperficial trunk. Int J Radiat Oncol Biol Phys 2000;47(5):1273–1279.
21. Arbeit J, Hilaris B, Brennan M. Wound complications in themultimodality treatment of extremity and superficial truncalsarcomas. J Clin Oncol 1987; 5:480–488.
22. Ormsby M, Hilaris B, Nori D, et al. Wound complications ofadjuvant radiation therapy in patients with soft tissue sarco-mas. Ann Surg 1989; 210:93–99.
23. Devereux D, Kent H, Brennan M. Time dependent effects ofadriamycin and x-ray therapy on wound healing in the rat.Cancer 1980; 45:2805–2810.
24. O�Sullivan B, Davis AM, Turcotte R, et al. Preoperative versuspostoperative radiotherapy in soft-tissue sarcoma of the limbs:a randomised trial. Lancet 2002; 359(9325):2235–2241.
INTERSTITIAL BRACHYTHERAPY FOR ADULT STS 567
Ann. Surg. Oncol. Vol. 14, No. 2, 2007