PEFR Measurement and Spirometry - Respiratory Medicine | Fastbleep
-
Upload
nur-farhana -
Category
Documents
-
view
10 -
download
0
description
Transcript of PEFR Measurement and Spirometry - Respiratory Medicine | Fastbleep

FastbleepRevision NotesEventsSchoolsBlogAboutSign in
Search Fastbleep..
Medical Notes
Respiratory Medicine ArticlesRevision Notes/ Medical Notes/ Heart Lungs & Blood/ Respiratory Medicine
PEFR Measurement and SpirometryWritten by: Michael Patrick Johnston from Manchester University,
What is peak flow?
PEFR (peak expiratory flow rate) is a form of pulmonary function test. It measures the fastestrate of air that can be expired.
The convenient size of the peak flow meter makes regular measurement of forced expirationpossible at home. The significance of its moderate 'pocketability' is that patients can write downmultiple readings in a day, recording them in a peak flow diary. This provides information on:
diurnal variabilityresponse to bronchodilatorsmonitoring severity of disease
The main use of peak flow is in asthma. Although it reveals some information about COPD ittends to underestimate the severity and therefore is unreliable.

What is spirometry?
Spirometry is a form of pulmonary function test. Patients blow into a tube as strongly aspossible, expiring until they have no breath left.
What do all the acronyms mean?
FEV1: forced expiratory volume in one second
VC: vital capacity - how much air you can breath out after as deep a breath as possible.Crucially it is not 'forced'...
FVC: forced vital capacity. Essentially the vital capacity but blowing out as strongly as possible.
*In normal young people VC and FVC are most likely to be equal. However, in emphysematouslungs elasticity of the airways is lost. This elasticity is what normally keeps the airways patentduring expiration. If the elasticity is not present the airways can become closed on forcefulexpiration and so not all the air is expelled. The key word to describe this phenomenon inOSCEs is 'trapping'. It is important to be aware of this disparity between VC and FVC inemphysematous patients.
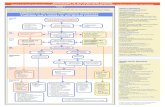
When is spirometry indicated?
Spirometry is a cheap, non-invasive, valuable investigation, available in both primary andsecondary care. It is also a dynamic investigation, with the following uses:
Confirm diagnosis of obstructive (e.g. COPD) or restrictive lung disease;Assessment of disease severityMeasuring deterioration of disease

Most general practices have their own spirometer. In secondary care formal request may benecessary but many thoracic departments have a spirometer in each ward. If this is the case inyour teaching hospital take the opportunity to do patients' pulmonary function. It is notuncommonly requested by the consultant. It is a basic piece of equipment so you only need todo it once to be covered for any potential OSCE station.
Interpretation - Part 1
1. Details
NameAgeSexHeightEthnicity
2. Reproducibility
Look at the variability (Var). BTS states that there must be at least two values within 3% of eachother for the result to be reliable.

3. Is it technicaly acceptable?
Did they cough during the expiration?Did they take an extra breath during expiration?Maybe they had a slow start?Was it a sub-maximal effort?
All of these produce dents and artefacts in the cruve produced. It may be difficult to achieve aperfectly accurate graph but the result should be as smooth as possible.

Interpretation - Part 2
Is the ratio FEV1/FVC <70%?
Yes: obstructive lung disease

No: may be restrictive lung disease
Our patient above appears to have an obstructive pattern. Another clue towards this is the shapeof the curve, which will have a flatter gradient the more obstruction there is.
Interpretation - Part 3 (Obstructive pattern)
Is this pattern reversible? Or is it fixed?
To test for reversibility either:
a) Repeat test 15 minutes after: salbutamol inhaler through spacer (400mcg)
b) Repeat test 15 minutes after: salbutamol nebuliser (5mg)
To determine reversibility it is the FEV1 figure we are interested in. Has the amount of air thepatient can forcefully blow out in one second increased after a bronchodilator? Is there'reversibility'? An increase of 400ml is said to be significant. Look in the 'Best spirometry result'section below (same patient again) and determine whether his obstructive disease is reversibleor not.
Our patient's FEV1 increased from 1.21L to 1.63L, a difference of greater than 400ml. His airway

disease follows a reversible obstructive pattern, e.g. asthma.
Interpretation - Part 3 (Restrictive pattern)
It is important to check for restrictive lung disease regardless of whether an obstructive patternis present or not. Clearly COPD patients and other obstructive disease individuals can have anelement of restrictive pattern as well.
Therefore:
Is the % predicted FVC < 80%?
Our 72 year old Caucasian man with reversible obstructive disease has a % predicted FVC of91%. This is greater than 80% and so there is no additional restrictive element.
Clearly, in other situations there will be patients with no obstructive disease but a restrictivepattern. These can be divided into pulmonary problems and non-pulmonary causes:
1. Pulmonary: fibrosis; pneumoconiosis; pulmonary oedema; parenchymal lung tumours;lobectomy/pneumectomy.
2. Non-pulmonary: neuromuscular disorders; postural problems (e.g. thoracic cage deformity orkyphoscoliosis); obesity; pregnancy.
Additional example

Is there satisfactory reproducibility?
Is it technically acceptable?
Is the pattern obstructive or restrictive, or combined?
If there is an obstructive pattern, is it reversible or fixed?
If the obstruction is fixed, what grade of severity is their COPD?
FEV1 ≥ 80% Stage 1 - Mild
FEV1 50-79% Stage 2 - Moderate
FEV1 30-49% Stage 3 - Severe
FEV1 < 30% Stage 4 - Very severe

SkillsABG Sampling and InterpretationMetered Dose Inhaler (MDI) UsageNebuliser UsageOxygen TherapyPEFR Measurement and SpirometryRespiratory ExaminationConditionsAsthmaBronchiectasisChronic Obstructive Pulmonary Disorder (COPD)Interstitial Lung DiseaseLung CancersPleural EffusionPneumoniaPneumothoraxPulmonary EmbolismTuberculosisPresentationsChest PainCoughCyanosisHaemoptysisShortness of BreathBasic PrinciplesControl of BreathingGas ExchangeVentilation
Related NewsBronchiectasis Patients Exhibit Higher Sedentary Lifestyles and Treatment ... - Bronchiectasis News Today (03 Jun15)(http://bronchiectasisnewstoday.com/2015/06/03/bronchiectasis-patients-exhibit-higher-sedentary-lifestyles-treatment-include-physical-activity-interventions/)The Effectiveness of Non-pharmacological Healthcare Interventions for Asthma ... - Medscape (04 May 14)(http://www.medscape.com/viewarticle/824182)Picture of Spirometer. Photo Courtesy of Getty Images, User Mario Tama - About.com: Health (25 May 08)(http://copd.about.com/od/copd/a/pfts.htm)When gout is caused by your medicine - Daily Mail (23 Jun 08)(http://www.dailymail.co.uk/health/article-1028838/When-gout-caused-medicine.html)E-Teaching Clinical Nursing Skills - Medscape (19 May 09)(http://www.medscape.com/viewarticle/702802)EPA's Smoke-and-Mirrors on Smog and Soot — Part 1 - Canada Free Press (10 Dec 10)(http://canadafreepress.com/article/30932)

About What we do and who we work with.T&Cs Terms and conditions of use.Powered by Software development at Fastbleep.
Get published Write an article for Fastbleep Notes.Volunteer For our Schools Programme.Contact us We like to talk.
Keepin
touchby
following us on Twitter (http://twitter.com/fastbleep) and finding us on Facebook (http://www.facebook.com/fastbleep) .
Copyright © 2015 Fastbleep Ltd.All rights reserved.
Happy Sunday.