Parental balanced chromosomal rearrangement leading to ...
Transcript of Parental balanced chromosomal rearrangement leading to ...

RESEARCH NOTE
Parental balanced chromosomal rearrangement leading to majorgenomic imbalance and an autosomal trisomy resulting in consecutivepregnancy loss: a case report
ANUSHKA SHRIVASTAVA1,2, SEEMA THAKUR3, TARA NATH2, ABHIPSA V. F. DEBNATH1
and SONAL R. BAKSHI1*
1Institute of Science, Nirma University, Ahmedabad 382 481, India2Advanced Genomic Institute and Laboratory Medicine (Labassure), New Delhi 110 003, India3Department of Clinical Genetics and Fetal Medicine, Fortis Hospital, New Delhi 110 088, India*For correspondence. E-mail: [email protected].
Received 8 November 2020; revised 9 February 2021; accepted 23 March 2021
Abstract. Chromosomal aberrations such as parental balanced translocation contribute to a significant proportion of recurrent pregnancylosses. These have extreme genetic implications on the foetus which can either cause physical and/or mental retardation or early death. Inthis study, we report a unique clinical case of a couple with three consecutive pregnancy losses and we aim to determine the geneticabnormalities causing the miscarriages. Conventional cytogenetic and molecular genetic analysis were performed on the products ofconception as well as for the parents. Chromosomal analysis was performed based on the ISCN 2016 guidelines. This was followed byChromosomal microarray analysis carried out using ISCA consortium probe set (8X60K). Genetic testing for the 1st product of conceptionwas not performed. However, the 2nd and 3rd products of conception indicated an autosomal trisomy 22 and a 3.7 Mb deletion of 2p(cytoband p25.3) along with 13.6 Mb duplication of 16p (cytoband p13.3p13.12), respectively. The paternal karyotype was normal butmother showed a balanced translocation 46,XX,t(2;16)(p25.3;p13.3). This was parallel to the products of conception microarray findings,unbalanced chromosomal abnormality in the foetus. Balanced translocation carriers are susceptible for meiotic nondisjunction processesand early detection of genetic anomalies can be informative to parents trying to conceive. Genetic analysis of the abortus after the 1st losscan be helpful to understand the cause of miscarriage. A combined approach with microarray and karyotyping of the products of conceptioncan be important to determine the specific aberrations in the foetal chromosomes leading to abortion.
Keywords. spontaneous abortions; balanced translocation; chromosomal analysis; microarray; trisomy.
Introduction
Recurrent spontaneous abortion is defined as two or moreconsecutive loss of clinically established intrauterine preg-nancy before 20 weeks of gestation. Early pregnancy lossoccurs in 15% of all clinically recognized pregnancies. Thechromosomal abnormalities make a significant contributionin recurrent spontaneous abortions, accounting for *50% offirst trimester foetal loss (Van den Berg et al. 2012). Studiesof couples who are balanced translocation carriers indicatethat as many as 80% of the pregnancies may end up inspontaneous miscarriage (Sheth et al. 2013). Balancedtranslocations occur in 0.2% of the neonatal population, in0.6% of infertile couples and in up to 9.2% of patients with
recurrent abortions (Stern et al. 1999). The translocationcarrier have a risk to have a child with birth defects in termsof intellectual development and other phenotypic anomalydue to a segmental aneusomy (Gardner et al. 2012).
In case of couples with balanced translocation carrier, thereproductive risk of an abnormal foetus depends on theextent of genetic imbalance caused, also on the number andbreakpoints of the chromosome involved (Mackie andScriven 2004).
Balanced translocation is defined as rearrangement ofsegments of chromosomes with no loss of critical geneticmaterial or no lethal fusion gene formation, resulting in aphenotypically normal individual whereas, unbalancedtranslocation is defined as chromosomal rearrangement
Journal of Genetics (2021)100:54 � Indian Academy of Scienceshttps://doi.org/10.1007/s12041-021-01304-3 (0123456789().,-volV)(0123456789().,-volV)

resulting in loss or gain of genetic material which producesan altered phenotype (Sadler and Langman 2011).
Balanced chromosomal translocation carriers may havemore risk of recurrent spontaneous abortion and/or childrenwith serious birth defects due to unbalanced chromosomecomplements (Kunwar and Bakshi 2016).
Materials and method
Case report
The present study reports a case of a young couple presentedwith a history of three recurrent abortions in the first tri-mester of pregnancy (figure 1). The couple themselves didnot show any evidence of genetic abnormality. Genetictesting of the 1st product of conception (POC) was notperformed, and thus analysis of genetic basis of the next tworecurrent abortions was necessary. A conventional chromo-some analysis of the 2nd POC was done first followed byChromosomal microarray for 3rd POC specifically to findout the genetic defects in the abortus to determine the reasonbehind previous pregnancy failures. The results frommicroarray lead to the cytogenetic study of the parents. Thecouple did not approach us for the 4th pregnancy, so it isassumed that it would have been a successful pregnancy.
The POC samples were transported in sealed and sterilesample collection vial containing RPMI media with antibi-otics at room temperature. The samples were then processedfor culture. Abortus material (preferably villi) was washed,enzyme treated and cultured in T-Flask in Amniomax media
(GIBCO). Harvesting of cells was done after the properconfluency of the culture appeared using standard cytoge-netic methods (Jobanputra et al. 2002). Karyotype analysiswas done using Cytovision software (Leica Microsystems)as per ISCN 2016.
For further analysis, chromosomal microarray CMA(Agilent) (whole genome microarray-based hybridization)was performed on the DNA isolated from product of con-ception. This array contains *60,000 CGII probes, whichconsists of the entire ISCA (International standards forCytogenetic Arrays) consortium 8X60K version probe set.The array can detect gain and losses at a minimum of 400 kbto 200 kb, respectively across the genome, or smaller (C50kb) for clinically relevant deletion/duplication syndromes inthe subtelomere and pericentromere regions or targetedgenes.
Results
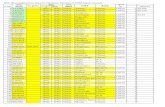
Table 1 combines the genetic findings from chromosomalanalysis and microarray analysis of the products of con-ception. The karyotype of the 2nd POC showed the presenceof trisomy 22 (47,XX,?22) (figure 2). The product of con-ception from the couple was collected for CMA studies at 7weeks of gestation from the 3rd abortion. The array reportfrom this POC [arr[hg19] 2p25.3(17019-3729241)x1,16p13.3p13.12(106271-13792996)x3] showed a clinicallysignificant genomic deletion of 3.7 Mb on short arm ofchromosome 2p25.3 and a clinically significant genomicduplication of 13.6 Mb on short arm of chromosome 16p13.3p13.12 (figure 3). Parental karyotyping revealed anormal karyotype for the father (46,XY) but the mother wasa carrier of balanced translocation involving chromosomes 2and 16 [46,XX,t(2;16)(p25.3;p13.3)] (figure 4).
Discussion
A 25 year old female presented with a history of threeconsecutive spontaneous abortions, clinically indicated asG4P0A3. The cytogenetic studies were carried out onproducts of conception to identify any constitutional geneticanomaly in the aborted foetus. Genetic testing was not
Figure 1. Pedigree showing three consecutive abortions and onelive pregnancy.
Table 1. Details of recurrent abortions and clinically significant genetic findings in POCs.
Gravida Status Gestation (weeks) Ultrasound finding Genetic finding
First Spontaneous abortion 7 No Gestational sac seen –Second Spontaneous abortion 8 Cardiac activity not seen Trisomy 22Third Spontaneous abortion 7 Cardiac activity present but
disappeared after 2 days3.7 Mb deletion on chromosome 2pand 13.6 Mb duplication onchromosome 16p
Fourth Current pregnancy 7 Anembryonic conception,no yolk sac seen
–
54 Page 2 of 6 Anushka Shrivastava et al.

Figure 2. Karyotype from 2nd POC showing trisomy 22, 47,XX,?22. POC, product of conception.
Figure 3. Graph showing genomic deletion on short arm of chromosome 2 and genomic gain on short arm of chromosome 16.
Balanced translocation causing recurrent pregnancy loss Page 3 of 6 54

performed on the 1st POC. The second consecutive abortionoccurred at 8 weeks of gestation with no cardiac activityobserved on ultrasound. The karyotype revealed an
autosomal trisomy of chromosome 22 (47,XX,?22). Themiscarriages occurring before 10 weeks of gestation aremajorly due to chromosomal aneuploidies arising from new
Figure 4. Karyotype from the mother showing balanced chromosome translocation 46,XX,t(2;16)(p25.3;p13.3).
Table 2. List of genes involved in the critical region of chromosome 2p25.3 (as listed in www.Omim.org).
Location Gene Gene nameGenenumber Phenotype
2:38,8132p25.3
FAM110C Family with sequencesimilarity 110, member C
611395
2:218,1352p25.3
SH3YL1 SH3 domain- and SYLFdomain-containing protein 1
617314
2:663,8762p25.3 TMEM18 Transmembrane protein 18 6132202:1,631,8862p25.3
PXDN, D2S448E, KIAA0230,PRG2, PXN, COPOA,ASGD7
Peroxidasin 605158
2:3,497,3652p25.3
ADI1, SIPL Acireductone dioxygenase 1 613400
2:1,789,1122p25.3
MYT1L, KIAA1106, MRD39 Myelin transcription factor 1-like 613084 Mental retardation, autosomal dominant 39
2:1,413,2872p25.3
TPO, TPX, TDH2A Thyroid peroxidase 606765 Thyroid dyshormonogenesis 2A
2:3,188,9242p25.3
EIPR1, TSSC1 EARP complex and GARPcomplex interacting protein 1
608998
2:3,379,2442p25.3
TRAPPC12, TTC15, PEBAS Trafficking protein particlecomplex, subunit 12
614139 Encephalopathy, progressive, early-onset,with brain atrophy and spasticity
2:3,594,8312p25.3
COLEC11, CLK1, 3MC2 Collectin 11 612502 3MC syndrome 2
2:3,531,8122p25.3
RNASEH1, PEOB2 Ribonuclease H1 604123 Progressive external ophthalmoplegiawith mitochondrial DNA deletions,autosomal recessive 2
2:3,575,2592p25.3
RPS7, DBA8 Ribosomal protein S7 603658 Diamond-Blackfan anemia 8
54 Page 4 of 6 Anushka Shrivastava et al.

nondisjunctional events, which are even more frequent invery early miscarriages (Sierra and Stephenson 2006). Apartfrom the common autosomal trisomies involving chromo-somes 13, 18 and 21 reported in early pregnancy loss, tri-somy 22 is also reported along with other uncommonautosomal trisomies (Choi et al. 2014; Pylyp et al. 2018).
Chromosomal microarray studies are informative regard-ing sub-microscopic deletions and duplications commonlymissed by conventional cytogenetic analysis. The product ofconception from this couple was collected for CMA studiesat 7 weeks of gestation for the 3rd pregnancy. The cardiacactivity was recorded at 7th week on ultrasound scan whichstopped after two days. The deletion of 3.7 Mb on short armof chromosome 2p25.3 and duplication of 13.6 Mb on shortarm of chromosome 16 p13.3p13.12 was observed.
Both these regions on chromosomes 2 and 16 are generich and hence can be critical. There are numerous genesinvolved in genomic deletion of 3.7 Mb on chromosome2p25.3 (table 2) which are reported to be associated withvarious clinical conditions including mental retardation,encephalopathy with brain atrophy and spasticity.
The genomic duplication of 13.6 Mb on chromosome 16palso involves multiple genes (table 3). The clinical featuresof duplication 16p syndrome includes critical region of ter-minal 16p13.1-p13.3 reported to be associated with specificfacial anomalies, mental retardation, congenital cardiac andvascular defects, urinary malformations and hypoplasticdistal phalanges of hands (Digilio et al. 2009).
The findings of CMA from third POC prompted parentalkaryotype study for which the mother was a carrier of abalanced translocation 46,XX,t(2;16)(p25.3;p13.3). It hasbeen reported that around two-third of balanced autosomal
translocation carriers had two or more pregnancy losses(Sheth et al. 2013). Various reports of cytogenetic studiesshow 2 to 8% cases with recurrent spontaneous abortionshad chromosomal abnormalities (Ghazaey et al. 2015).Parental chromosomal abnormalities play an important rolein the pathogenesis of recurrent abortion (Flynn et al. 2014).
A chromosomal break can cause loss of function of geneif it disrupts the coding sequence (Kunwar and Bakshi2016). According to OMIM database, results frommicroarray are suggestive of 2p25.3 deletion syndrome and16p duplication syndrome involving multiple genes. Thegenomic imbalance detected using chromosomal microarraycan be responsible for the foetal loss. The earlier miscarriagein this case was found to be associated with trisomy ofchromosome 22. The autosomal trisomy is reported in43–54% of cases in recurrent miscarriages (Choi et al.2014). Autosomal trisomies commonly associated withrecurrent spontaneous abortions are trisomy 13, 16, 18 and21, apart from these trisomy, 15 and 22 have also beenreported. The mispairing of translocated chromosomes dur-ing the first meiotic division can give rise to different formsof segregation, resulting in aneuploidy of the translocatedchromosomes (Pourjafari et al. 2012). Couples with bal-anced reciprocal translocation have 50% chance of recurrentspontaneous abortions and 20% risk of progeny with geneticimbalance (De et al. 2015). The formation of balanced,unbalanced, and normal gametes depends on the breakpointsof the chromosomes involved.
Chromosomal abnormality is one of the major causes ofrecurrent abortions; however, genetic testing is routinelyindicated after two or three consecutive abortions. Ourresults indicate importance of genetic study on the first
Table 3. List of a few genes involved in the critical region of chromosome 16p (as listed in www.Omim.org).
Location Gene Gene nameGenenumber Phenotype
16:016p13.3
DEL16p13.3, RSTSS Chromosome 16p13.3 deletionsyndrome (Rubinstein–Taybi deletionsyndrome)
610543 Chromosome 16p13.3deletion syndrome
16:016p13.3
DUP16p13.3, C16DUPq13.3 Chromosome 16p13.3 duplicationsyndrome
613458 Chromosome 16p13.3duplication syndrome
16:016pter-p13.3
HBHR, ATR1 Alpha-thalassaemia/mental retardationsyndrome, type 1
141750 Alpha-thalassaemia/mentalretardation syndrome, type 1
16:016p13.3
MCOPCT1 Microphthalmia with cataract 1 156850 Microphthalmia with cataract 1
16:016p13.3
PKDTS Polycystic kidney disease, infantilesevere, with tuberous sclerosis
600273 Polycystic kidney disease,infantile severe, with tuberoussclerosis
16:1,984,19216p13.3
GFER, ERV1, ALR Growth factor, erv1, S. cerevisiae,homolog of (augmenter of liverregeneration)
600924 Myopathy, mitochondrialprogressive, with congenitalcataract, hearing loss, anddevelopmental delay
16:2,155,77716p13.3
TRAF7, RFWD1, CAFDADD TNF receptor-associated factor 7 606692 Cardiac, facial and digital anomalieswith developmental delay
Balanced translocation causing recurrent pregnancy loss Page 5 of 6 54

instance of miscarriage to provide better informed clinicalintervention. The presence or absence of genomic imbalancewhen confirmed early using high resolution genetic analysislike CMA can avoid trauma and distress in couples. Con-ventional karyotyping is informative for microscopic geno-mic imbalance but also has its own limitations, one of thembeing culture failure. Hence we recommend includingchromosomal microarray even for the first pregnancy loss torule out cryptic translocation or sub microscopic deletionand duplication. The chromosomal microarray is reported tobe a reliable and comprehensive technique with highersuccess rates for detecting genomic imbalance in products ofconception (Levy et al. 2014; Zhu et al. 2018).
In conclusion, Conventional cytogenetic provides a robustplatform to study early pregnancy loss, whereas molecularcytogenetic methods have overcome the problem of tissueculture failure and provide more specific diagnostic yields. Acombined approach of microarray and conventional cyto-genetic methods to study POC can optimise findings ofrecurrent pregnancy loss. Genetic counselling for suchpatients is must to understand the risk in planning furtherpregnancies. Also prenatal cytogenetic analysis will behelpful for future pregnancies in such cases. Clinical inter-ventions like in vitro fertilization and preimplantationgenetic diagnosis in such cases can be most fruitful whenoffered earlier to the couple preventing recurring agony ofpregnancy loss.
Acknowledgements
Authors acknowledge support from Advanced Genomics Instituteand Laboratory Medicine, AGILE, New Delhi. Authors are gratefulto the patients for the kind support and consent for the study.
References
Choi T. Y., Lee H. M., Park W. K., Jeong S. Y. and Moon H. S.2014 Spontaneous abortion and recurrent miscarriage: a com-parison of cytogenetic diagnosis in 250 cases. Obstet. Gynecol.Sci. 57, 518–525.
De P., Chakravarty S. and Chakravarty A. 2015 Novel balancedchromosomal translocations in femaleswith recurrent spontaneousabortions: two case studies. J. Hum. Reprod. Sci. 8, 114–117.
Digilio M. C., Bernardini L., Capalbo A., Capolino R., Gagliardi M.G.,MarinoB. et al. 2009 16p subtelomeric duplication: a clinicallyrecognizable syndrome. Eur. J. Med. Genet. 17, 1135–1140.
Flynn H., Yan J., Saravelos S. H. and Li T. C. 2014 Comparison ofreproductive outcome, including the pattern of loss, betweencouples with chromosomal abnormalities and those with unex-plained repeated miscarriages. J. Obstet. Gynaecol. Res. 40,109–116.
Gardner R. J. M., Sutherland G. R. and Shaffer L. G. 2012Chromosome abnormalities and genetic counseling, 4th edition.Oxford University Press, Oxford, UK.
Ghazaey S., Keify F., Mirzaei F., Maleki M., Tootian S., AhadianM. and Abbaszadegan M. R. 2015 Chromosomal analysis ofcouples with repeated spontaneous abortions in NortheasternIran. Int. J. Fertil. Steril. 9, 47–54.
Jobanputra V., Sobrino A., Kinney A., Kline J. and Warburton D.2002 Multiplex interphase fish as a screen for commonaneuploidies in spontaneous abortions. Hum. Reprod. 17,1166–1170.
Kunwar F. and Bakshi S. R. 2016 Familial constitutionalrearrangement of chromosomes 4 & 8: phenotypically normalmother and abnormal progeny. J. Clin. Diagn. Res. 10, Gd01–Gd04.
Levy B., Sigurjonsson S., Pettersen B., Maisenbacher M. K., HallM. P., Demko Z. et al. 2014 Genomic imbalance in products ofconception: single-nucleotide polymorphism chromosomalmicroarray analysis. Obstet. Gynecol. 124, 202–209.
Mackie Ogilvie C. and Scriven P. N. 2004 Preimplantation geneticdiagnosis (PGD) for reciprocal translocations. Prenat. Diagn. 24,553–555.
Pourjafari B., Pour-Jafari H., Farimani M., Ghahramani S. andSaleh E. K. 2012 Genetic counseling in carriers of reciprocaltranslocations involving two autosomes. Indian J. Hum. Genet.18, 250–253.
Pylyp L. Y., Spynenko L. O., Verhoglyad N. V., Mishenko A. O.,Mykytenko D. O. and Zukin V. D. 2018 Chromosomalabnormalities in products of conception of first-trimester mis-carriages detected by conventional cytogenetic analysis: a reviewof 1000 cases. J. Assist. Reprod. Genet. 35, 265–271.
Sadler T. W. and Langman J. 2011 Langman’s medical embryology,12th edition. Wolters Kluwer Health/Lippincott Williams &Wilkins, Philadelphia.
Sheth F. J., Liehr T., Kumari P., Akinde R., Sheth H. J. and Sheth J.J. 2013 Chromosomal abnormalities in couples with repeatedfetal loss: an Indian retrospective study. Indian J. Hum. Genet.19, 415–422.
Sierra S. and Stephenson M. 2006 Genetics of recurrent pregnancyloss. Semin. Reprod. Med. 24, 17–24.
Stern C., Pertile M., Norris H., Hale L. and Baker H. 1999Chromosome translocations in couples with in-vitro fertilizationimplantation failure. Hum. Reprod. 14, 2097–2101.
van den Berg M. M., van Maarle M. C., van Wely M. and GoddijnM. 2012 Genetics of early miscarriage. Biochim. Biophys. ActaMol. Basis Dis. 1822, 1951–1959.
Zhu X., Li J., Zhu Y., Wang W., Wu X., Yang Y., Gu L. et al. 2018Application of chromosomal microarray analysis in products ofmiscarriage. Mol. Cytogenet. 11, 44.
Corresponding editor: B. K. THELMA
54 Page 6 of 6 Anushka Shrivastava et al.