Page 1 of 41 - Queensland Children's Hospital · Overview of the face to face course structure...
Transcript of Page 1 of 41 - Queensland Children's Hospital · Overview of the face to face course structure...

Page 1 of 41

Page 2 of 41
Table of Contents Introduction ...................................................................................................................................................................... 4
What is OPTIMUS? ............................................................................................................................................................ 5
Who is SToRK?................................................................................................................................................................... 5
Safety in the Course .......................................................................................................................................................... 6
Learning Objectives ........................................................................................................................................................... 6
Faculty Resources ............................................................................................................................................................. 7
eLearning ........................................................................................................................................................................... 7
eLearning Flier ................................................................................................................................................................... 8
Overview of the F2F Course Structure .............................................................................................................................. 9
Group Rotation Options .................................................................................................................................................. 11
The Case Study ................................................................................................................................................................ 14
The Airway and Breathing Station .................................................................................................................................. 15
The Circulation Station .................................................................................................................................................... 18
CPR and Defibrillation Station ......................................................................................................................................... 20
Debriefing Scenarios : A Crash Course ............................................................................................................................ 24
Scenario 1 : Respiratory Deterioration and Apnoea ....................................................................................................... 27
Scenario 2 : Cardiac Arrest .............................................................................................................................................. 30
The Testing Station ......................................................................................................................................................... 33
Assessor’s Guide : Assessment Station Scenario Options............................................................................................... 35
Assessor’s Guide : Expected Standards of Achievement ................................................................................................ 36
Assessor’s Guide : Expected Defibrillation Knowledge ................................................................................................... 38
CPR Assessment Sheet (Core and Advanced Participants) ............................................................................................. 40
Defibrillation Assessment Sheet (Advanced Participants) .............................................................................................. 41

Page 3 of 41
Version 2.0
The State of Queensland (Queensland Health) 2014
Copyright protects this material. Except as permitted by the Copyright Act, reproduction by any means
(photocopying, electronic, mechanical, recording or otherwise) making available online, electronic
transmission or other publication of this material is prohibited without prior written permission of Queensland
Health.
Inquiries should be addressed to:
Email: [email protected]
Postal Address: The IP Officer, Office of Health & Medical Research,
Reform & Development Division, Queensland Health,
GPO Box 48, Brisbane, Qld, 4001. Statement of Indemnity
Material in this document cannot be reproduced in part or in whole without the expressed permission of Queensland Health and remains the intellectual property of Queensland Health. Queensland Health does not accept any responsibility for the use of this material outside the scope for which it has been designed.
The information provided in this document is for educational purposes only. It is not intended nor implied to be a
substitute for, or to be used as, the only resource in the provision of care to paediatric patients. Formal advice, consultation and collaboration with appropriate advisers and consultants should be sought in all matters relating to the
specific management of the health and well being of the paediatric patient. References to any non-governmental entity, product, service or source of information that may be contained in this package should not be considered as an
endorsement either direct or implied.
Version Control
This is version 2.0 of Opitimising Paediatric Training In eMergencies Using Simulation. Clinical Observation
and Response to Emergencies (OPTIMUS CORE) and will remain current until 2019.
Document Development History
Document
Development
Whom Date Review Date
Initial Document
RMDPP V1.0
Simulation Training on
Resuscitation for Kids
(SToRK)
Feb 2014 Feb 2016
Feb 2018
Document Review
OPTIMUS CORE V2.0
SToRK Statewide
Advisory Workgroup
May 2018

Page 4 of 41
Clinical Observation & Response to Emergencies
Introduction
Welcome to CORE.
It is a course on foundational knowledge for paediatric health care staff, with an emphasis on :
• Recognition of the deteriorating paediatric patient
• Orientation to local Medical Emergency Response Teams
• Paediatric basic life support
Unlike other OPTIMUS courses, CORE includes a formal BLS assessment. This has been incorporated to
allow CORE to be used to provide your local Paediatric BLS certication, while also incorporating the
Children’s Early Warning Tool and introductory paediatric clinical knowledge.
In order to create a shared mental model & team based approach to these issues CORE utilises a blend of :
• eLearning
• Case Based Discussion
• Practical skills stations
• Scenario based learning
CORE is the base of our spiral curriculum of OPTIMUS courses. It is best suited to those new to paediatric practice, or those who request a refresher after a period of time away.
Faculty requisites:
• Faculty should be interprofessional and include a combination of : o An acute paediatric medical specialist o An acute paediatric nursing specialist
• Some staff will require expertise in simulation technology and debriefing experience. o Any of the faculty may fill these roles. o It is recommended that the course workload is shared amongst at least three faculty
members.
Target Group :
• All health staff who might attend a paediatric emergency.
Face to Face Course Length : 4 Hours

Page 5 of 41
What is OPTIMUS?
OPTIMUS is a suite of courses designed to create a complete paediatric life support
training package.
It has been developed to address Queensland’s training needs in paediatric critical
care.
In line with the recommendations of NSQHS Standard 9 (recognition and response
to clinical deterioration), the suite of OPTIMUS courses cover :
• Recognition of Deterioration and Skills for First Responders (CORE)
• Advanced Resuscitative Care for Second Responders (PRIME)
• Ongoing learning through Spaced Practice via Simulation Modules (BONUS)
OPTIMUS has been designed by Children’s Health Queensland’s SToRK Team.
Who is SToRK?
SToRK is Children’s Health Queensland ‘Simulation Training on Resus for Kids’
Unit.
Founded in 2014, we aim to improve paediatric health care to all children in
Queensland.
Based in Queensland Children’s Hospital, the team’s achievements include :
• Rolling out the OPTIMUS CORE program statewide
• Creating and teaching on OPTIMUS PRiME statewide
• Teaching Crisis Resource Management and Paediatric Acute Trauma courses
locally

Page 6 of 41
Safety in the Course
• A safe environment must be maintained for the participants and other instructors:
o Be familiar with local emergency activation procedures
o Label all medications as use for training only
o Sharps bin available
o Closed in shoes are preferred to minimize risk of injury
o Be familiar with the safe use of a working defibrillator in the skills stations and
simulations. This includes:
▪ a compatible rhythm simulator and a charge dump device (ie mannequin,
manufacturers charge dump device) – checking of working order of
equipment prior to use, ie mannequin studs are tight, leads are attached.
▪ informing all participant’s and instructors that the defibrillator is ‘live’
▪ responsibility for the safety of participants when using defibrillator.
Learning Objectives
OPTIMUS CORE educates health workers to:
• Understand the importance of early recognition, management and escalation of care for the deteriorating child
• Use a structured approach in the assessment and management of a deteriorating paediatric patient
• Gain an understanding of and accurately use the state-wide Children’s Early Warning Tool (CEWT)
• Be able to provide basic life support (including defibrillation safety)
• Be able to provide advanced life support - recognise and manage the four cardiac arrest rhythms – and manage a team during this event (advanced life support providers)
• Gain knowledge and skills in paediatric airway management - optimal airway positioning, use of adjuncts, Laryngeal Mask Airways and Bag Mask Ventilation
• Gain knowledge and skills in management of circulation in the paediatric patient - intraosseous access, fluid resuscitation, resuscitation medications
• Gain hands on experience in managing critical events using crisis resource management principles through simulated learning events (teamwork, leadership, handover and communication)
OPTIMUS CORE will assist your health facility in fulfilling the requirements of the National Safety
and Quality Health Service Standards, particularly Recognition and Responding to Clinical
Deterioration in Acute Health Care and Clinical Handover.

Page 7 of 41
Faculty Resources
This OPTIMUS CORE Faculty Manual contains information on every station and simulation
on the course.
Please visit our SToRK Sharepoint site to :
• Find links for Participants, Instructors and Directors to prepare for the course
• Download the most up to date version of :
o The Case Study
o Printed Materials
o Participant and Faculty Certificates
• When visiting the website, Instructors can review video refreshers of any stations
they are teaching on.
Following each course please email [email protected] the Faculty Evaluation &
Participant Evaluations.
eLearning
The OPTIMUS CORE course begins with its eLearning course.
It is hosted on Queensland Health’s iLEARN package. This is available on the internet at :
https://ilearn.health.qld.gov.au/d2l/login .
iLEARN can be accessed from home via the internet, it doesn’t require a QHealth Intranet
connection, but does require users to sign up for an account.
A Flier that explains how to access the eLearning is attached on the next page of this
manual.
In CORE participants will meet 4 patients and as they progress through the elearning they
will manage each of these patients in order to reflect on : Respiratory Support, Circulatory
Support, CPR and Defibrillation.

Page 8 of 41
eLearning Flier

Page 9 of 41

Page 10 of 41
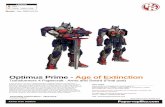
Overview of the face to face course structure
OPTIMUS CORE is structured to be delivered in 4 hrs.
A Faculty : Participant ratio of 1:4 is recommended to provide a quality learning experience.
Time Session Objectives NSQHS
10 min Welcome Introduction
Objectives & Course overview
30 min
Recognition of the
deteriorating patient Case study
9.2.3 –
9.2.4
9.3.3
9.4.1 –
9.4.3
9.5.1 –
9.5.2
90 min
3 x 30 min
rotations
Management of the
deteriorating patient
Skills stations
Airway/breathing:
9.4.1 –
9.4.3
9.6.1
CPR / Defibrillation
Circulation
20 min
90 min
3 x 30 min
rotations
Simulated Scenarios
Putting it all together
CPR assessment
Please complete
evaluations whilst
waiting for CPR
assessment
Scenario 1
9.3.3
9.4.1 –
9.4.3
9.6.1
Scenario 2
CPR assessment
Defibrillation assessment

Page 11 of 41
Group Rotation Options
The OPTIMUS CORE structure can be customised to your health facilities needs and participant
group size. On the following pages are some suggested course structures for different participant
group sizes. A Faculty : Participant ration of 1:4 is recommended to facilitate a quality learning
experience.
Suggested Course Structure for 1 Group of Participants
At least 2 faculty
Time SESSION
08:00 – 08:20 Introduction: objectives and course overview
08:20 – 08:50 Case Study
08:50 – 09:20 Airway/Breathing
09:20 – 09:50 Circulation
09:50 – 10:20 CPR/Defibrillation
10:20 – 10:30 Break
10:30 – 11:05 CPR/Defibrillation Assessment
11:05 – 11.40 Scenario 1
11:40 – 12:15 Scenario 2
12:15 End of Course

Page 12 of 41
Suggested Course Structure for 2 Groups of Participants – 6 - 8 participants
At least 1 Faculty Member Per Station
Time SESSION
08:00 – 08:20 Introduction: objectives and course overview
ALL GROUPS
08:20 – 08:50 Case Study
ALL GROUPS
Airway/Breathing
CPR/Defib Circulation
08:50 – 09:20 A - B
09:20 – 09:50 B - A
09:50 – 10:20 - A & B -
10:20 – 10:30 Break
Scenario 1 Scenario 2 CPR/Defib
assessment
10:30 – 11:05 A - B
11:05 – 11.40 B - A
11:40 – 12:15 - A & B -
12:15 End of Course

Page 13 of 41
Suggested Course Structure for 3 Groups of Participants – recommended for 9 – 24
participants
Minimum of 2 faculty per station for participant numbers > 12
Number of assessors needed for testing station will vary with participant numbers
Time SESSION
08:00 – 08:20 Introduction: objectives and course overview
ALL GROUPS
08:20 – 08:50 Case Study
ALL GROUPS
Airway/Breathing
CPR/Defib Circulation
08:50 – 09:20 A B C
09:20 – 09:50 C A B
09:50 – 10:20 B C A
10:20 – 10:30 Break
Scenario 1 Scenario 2 CPR/Defib
assessment
10:30 – 11:05 A B C
11:05 – 11.40 C A B
11:40 – 12:15 B C A
12:15 End of Course

Page 14 of 41
The Case Study Overview :
• The OPTIMUS CORE case study involves the presentation of a case involving a 6 month old in respiratory
distress.
• It involves recorded observations and videos of infants with moderate to severe work of breathing.
• It provides an opportunity to teach how to recognise, manage and appropriately escalate care for the
deteriorating paediatric patient.
Learning Objectives :
Upon conclusion of the case study participants should :
• Use clinical reflection and analysis to recognise the signs of deterioration in a child
• Be familiar with the signs of mild, moderate and severe respiratory distress.
• Understand using the CEWT chart and its role in recognising potential early deterioration through trends.
• Be empowered to use CEWT as a tool to ensure appropriate patient review and escalation of treatment.
• Know how to activate a Medical Emergency Response in their own hospital.
• Have practiced and reflected on clinical handover techniques both before and during resuscitation.
• Appreciate the benefit of preparation of the team in an emergency.
Equipment Required :
• Powerpoint projector
• Powerpoint file : ‘Case Study’ included in your trainer pack
• A large desk for each group of participants
• A laminated CEWT chart on each table that is consistent with the version that is used in your own
hospital.
• Laminated SBAR template on each table
• Whiteboard markers to fill out the CEWT chart
Layout :
Participants should be arranged into workgroups of 2 – 6 with access to a table for each group to work together.
Presenting the Case :
The 40 minute session involves :
• A brief initial overview of the structure of the course itself.
• A case based discussion of a 6 month old with laryngomalacia and respiratory distress who deteriorates
over the course of the session.
o 2 prompt points for participant workgroups to discuss the patients likely CEWT score, allowing
time for the group to fill out the CEWT chart at their table.
o Discussion on clinical handover to ward call staff using SBAR once the patient has deteriorated.
o Discussion on escalating to a medical emergency response according to the CEWT tool and your
local hospital protocols.
o Discussion on anticipating arrival of the medical emergency team :
▪ Institution of Basic Life Support
▪ Ward Team Allocation
▪ Clinical handover during a Resuscitation event.
• The case study PowerPoint presentation contains extra reference points for discussion in the notes pages
• Participant Groups should then be advised as to their next skill station location.

Page 15 of 41
The Airway and Breathing Station
Part 1. Setup
Equipment required: Ensure all equipment is in working order and similar to what is used in your
own hospital
(Mannequins not shown)
Paediatric airway head x 1
Infant ALS mannequin x 1
Infant BLS mannequin x 2 (1 per 2 participant)
Child BLS mannequin x 2 (1 per 2 participant)
Oropharyngeal airways size 00, 0, 1, 2, 3 x 1 each
Nasopharyngeal airways size 3.5, 4.5 x 1 each
Paediatric / 500mL self-inflating bag x 2 (1 per infant
mannequin)
Adult 1200mL self-inflating bag x 2 (1 per child mannequin)
Masks size 0/1, 2 x 2 (1 per infant mannequin)
Masks size 3/4 x 2 (1per child mannequin)
Suction catheters size 6, 8 x 1 each
Yankaeur sucker small and large x 1 each
Suction tubing x 1
Tongue depressors x 2
High-concentration oxygen mask large & small x 1 each
Airway laminates
T-piece bag 500mL x 1
LMA size 1, 1.5 x 1 each
Syringes 10mL x 2
Mannequin lubricant spray x 1
Resuscitation table x 1

Page 16 of 41
Figure 1. example layout of Bag and
Mask practice area
Participants should be spread around the
table to allow skills practice on the
mannequins.
Figure 2. example layout of Airway
Adjuncts practice area

Page 17 of 41
Part 2. Running the Station
Aim
The purpose of the airway skills station is for participants to learn how to perform basic airway skills in the
management of the deteriorating child. Identifying the appropriate escalation to advanced airway
management in the deteriorating child or cardiac arrest.
Objectives: By the end of the session, all participants have practiced:
Core/Advanced participants:
• Basic airway opening manoeuvres - positioning, suction, oropharyngeal / nasopharyngeal insertion
• Recognition of risks of bag-valve-mask ventilation in a spontaneously breathing child
• Effective bag-valve-mask ventilation Advanced participants:
• Effective ventilation using Ayres t-piece / anaesthetic bag
• Laryngeal mask insertion Facilitator: Medical / Nursing
Participants: max 8 per group, mix of core and advanced Identify core and advanced participants.
Facilitate group using a team approach of supportive practice – advanced practitioners to support core skill
practitioners.
Facilitator demonstrates the skill first and then supports participants practice.
Airway Scenario
Max is admitted with pneumonia. You are alerted by parent that Max has increased respiratory distress.
Demonstrate and practice – 30 minutes:
1. Airway positioning to open airway – head tilt-chin lift; jaw thrust 2. Suction 3. Oxygenation methods – nasal prongs, high-flow nasal prong therapy, Hudson mask vs non rebreather
mask Max stops breathing 4. Bag and mask ventilation – single and dual operator (2 handed mask technique)
- Self-inflating bag – NB danger of CO2 retention in the self ventilating patient - Anaesthetic bag - advanced participants
5. Oropharyngeal insertion 6. Nasopharyngeal insertion 7. Nasogastric tube insertion 8. LMA insertion – advanced participants

Page 18 of 41
The Circulation Station
Part 1. Setup
Equipment required: Ensure all equipment is in working order
Core / Advanced
BLS Mannequin (with intravenous access + drainage)
1L 0.9% sodium chloride
0.9% sodium chloride ampoules x 1
Rapid infuser / IV administration set x 1
60mL syringe x 1
3-way tap with extension x 2
10mL syringe x 1
2mL syringe x 2
Box gloves x 1
Adrenaline minijet x 1
Adrenaline 1:1000 x 1
3-way tap x 1
Drawing up needles x 1
Resuscitation / emergency drug table x 1
I/O leg x 2 OR crunchie bar IO x 2
Manual Intraosseous needle x 2
IO driver x 1
IO driver needles small & medium needles x 1
each
EZI I/O laminate of positions
Equipment required: Ensure all equipment is in working order
Figure 1. Layout of
Circulation Skills Station

Page 19 of 41
Part 2. Running the Station
Aim
To recognize the signs of a child in circulatory shock and to obtain access to administer an appropriate fluid
bolus and to calculate adrenaline doses appropriate to weight.
Objectives
To recognize signs of circulatory shock including importance of BP - To obtain early vascular access - To calculate a fluid bolus - To recognize when to use an IO - To understand how and where to insert an IO - To understand what drugs and fluids can be administered through an IO - To recognize potential complications in using an IO and appropriate care of IO site. - To calculate adrenaline doses to be used during cardiac arrest.
Facilitator: Medical / Nursing
Participants: max 8 per group, mix of core and advanced
Identify core and advanced participants.
Facilitate group using a team approach of supportive practice – advanced practitioners to support core skill
practitioners.
Facilitator demonstrates the skill first and then supports participants practice.
Circulation Scenario
Jeremy is admitted with vomiting and diarrhoea. How would you assess this child’s circulatory status?
(Tachycardic, BP normal, CRT 3 seconds, dry mucous membranes, +/- fontanelle sunken)
1. How would you administer a fluid bolus? (syringe / rapid infusion line + 3-way tap push technique)
2. How much fluid do you give to an 8 kg infant / 30 kg child? (resus table)
HR increases, CRT 5 secs, hypotensive for age, decreased LOC
IV access is unable to be obtained – how else can you obtain vascular access?
3. Identify the sites for I/O insertion 4. Demonstrate and practice I/O insertion
The child’s pulse is no longer able to be obtained and CPR has been commenced. What is the first line
drug in managing cardiac arrest? (IV adrenaline)
5. Demonstrate assembly of a minijet 6. What is the dose of adrenaline for an 8 month old / 30 Kg child?
For the child signs of anaphylaxis, how would you administer adrenaline?
7. What is the dose of IM adrenaline for an 8 month old / 30 Kg child? 8. How do you prepare this?

Page 20 of 41
CPR and Defibrillation Station
Part 1. Setup
Equipment required: Ensure all equipment is in working order and consistent with what is used in
your hospital.
Mannequins and Defibrillator not pictured.
Table 1: CPR
Infant BLS mannequin x 2 (1 per 2 participant)
Child BLS mannequin x 2 (1 per 2 participant)
Paediatric 500mL self-inflating bag x 2 (1 per infant
mannequin)
Adult 1200mL self-inflating bag x 2 (1 per child
mannequin)
Masks size 0/1, 2 x 2 (1 per infant mannequin)
Masks size 3/4 x 2 (1 per child mannequin)
Infant & adult defibrillator pads x 1 each
DRSABCD poster x 1
Table 2: Rhythms & Defibrillation
SimJunior/Megacode Kid x 1
Self-inflating bag and masks (suitable for
mannequin)
Rhythm simulator x 1 OR photos of rhythms x 4
(PEA, asystole, VT & VF)
Defibrillator x 1 OR photos of Defibrillator
Cardiac Arrest guideline poster x 1

Page 21 of 41
Figure 1. Layout of Core CPR Station
Figure 2. Layout of Advanced CPR
Station

Page 22 of 41
Part 2. Running the CPR Station
Aim
The purpose of the CPR and defibrillation skills station is for participants to learn how to perform
cardiopulmonary resuscitation, recognise cardiac arrest rhythms and safe defibrillation.
Objectives: By the end of the session, all participants have practiced:
Core participants:
• DRSABCD algorithm including:
• Effective cardiac compressions (ratio, rate, depth, minimise interruption)
• Application of defibrillation pads
• Safety in defibrillation
Advanced participants:
• Core elements
• Recognition and management of shockable and non-shockable cardiac arrest rhythms
• Team coordination and readiness for safe defibrillation
• Consideration of 4H’s & 4T’s in cardiac arrest management
Facilitator: Medical / Nursing
Participants: max 8 per group, mix of core and advanced
Identify core and advanced participants.
Facilitate group using a team approach of supportive practice – advanced practitioners to support core skill
practitioners.
Facilitator demonstrates the skill first and then supports participants practice.
CPR & defibrillation Scenario
You find a child lying in bed, looks very pale and is breathing irregularly. How would you approach this
child?
Ask each participant to provide information whilst instructor demonstrates.
D – danger – provide examples of danger to self, patient, others
R – assess response using verbal and tactile stimuli
S – shout / send for help – initiate local emergency response (NB decision at 1 min to seek help if none has
arrived)
A – open airway - discuss airway positions for different ages and interventions e.g. suction
B – assess breathing (maintaining airway patency) – not breathing normally or not breathing – 2 x rescue
breaths
C – check for pulse – discuss pulse check sites for different ages, pulse check for no longer than 10 secs
- Indications to start compressions – you can’t feel a pulse; pulse rate < 60 bpm with associated poor
perfusion; no “signs of circulation/signs of life’; if in doubt, commence compressions - Start Compressions – landmarks lower half of sternum, centre of chest; depth – 1/3 depth chest;
Two hands encircling / two fingers, one hand / two; rate 100 – 120 bpm; ratio 15:2, adults 30:2; allow full recoil of chest; no leaning or rocking
o Utilise metronome recording or defibrillator with metronome capability - CPR continues - How often should we change over? Change rescuer every two minutes to reduce
fatigue and maintain efficacy of compressions - Participants to assist with rotation of ventilation/compressions

Page 23 of 41
D – Defibrillation. Defibrillator arrives. Facilitator demonstrates pad placement: AP vs AL position, ensure implanted devices, GTN / medication patch, ECG dots and leads are not under the defib pads – Discuss the principles of safe defibrillation: metal, oxygen, water.
Rhythm recognition & safe defibrillation
Facilitator takes on defibrillator role to demonstrate process for safe defibrillation (VT). It is of high priority to maintain safe practice when teaching with a live defibrillator. Participants rotate around mannequin in roles or airway/breathing, compressions, defibrillation, drugs & Team leader. Advanced participants to take on defibrillation role and demonstrate rhythm recognition and safe defibrillation process. Team Leader coordinates roles and works through arrest algorithm. Core participants continue to rotate through compression : ventilation roles (focus on minimising interruption to compressions on rotations) Initial rhythm VF, change rhythms between VT, VF asystole & PEA
• Defib pads are insitu - maintain good quality CPR
• Select joules
• Charge defibrillator – immediately for 1st shock and then towards end of 2 min cycle – maintain CPR whilst charging
• Remove oxygen & maintain good quality CPR while charging
• Once charged, call – ‘Stand Clear’ team confirm ‘I’m clear’ - compressions person hands off but near enough to recommence compressions as soon as either shock delivered or discharged safely in the non-shockable pathway
• Confirm shockable rhythm – (VF or VT on rhythm simulator)
• Assess pulse prior to first shock and each time there is a change in rhythm
• Look around bed to ensure all clear
• Discharge asynchronous shock 4 joules / Kg
• Immediately recommence CPR for 2 minutes - NB Note: DC shock disrupts electrical conductivity of the heart which does not always restore immediately. Recommencing CPR immediately maintains blood flow to the brain and heart following the DC shock.
• Move through Shockable arrest algorithm as participants rotate through roles o Establish IV access o 2nd shock adrenaline 10 micrograms/ kg o 3rd shock amiodarone 5 mg/kg o Discuss 4H’s & 4 T’s - covering indications more commonly seen in the paediatric
population. Continue until all participants have rotated through ventilation & compressions and all advanced participants have performed defibrillation role.
• Change rhythm to PEA & discuss non-shockable management
• Demonstrate how to safely dump the shock

Page 24 of 41
Debriefing Scenarios : A Crash Course It is beyond the scope of this manual to provide in-depth training in the facilitation of a simulated scenario including debriefing. The simulated scenarios are an identified source of angst for some prospective trainers. As such, we have compiled a basic list of pointers and some resources for further reading about running simulation events and debriefing. This is not meant to be a prescriptive ‘script’ for those experienced to follow. Rather, the intent is to provide a basic guide for how a scenario might run.
Simulation Orientation and Pre-briefing :
• State the Learning Objectives: o Explain the learning objectives of the scenario and how it fits into the course eg. Consolidation of
skills and knowledge from previous sessions, putting the skills into context, etc
• It is important to create a safe environment for participants. o Before starting all scenarios, remind participants that it is not a formal assessment or test, but a
chance to practice and reconcile the skills they have learned during their course. o Nervous participants may benefit from further reassurance that there will be no tricks or traps, and
that this is a safe environment where they can feel comfortable making mistakes without judgement or consequence to real patients.
o Reinforce this by repeating the ‘essential premise’ of the course : ▪ “Everyone attending is committed to improving their own practice, we bring together
knowledge and experience and share those experiences to improve the care we provide to the children we care for.”
o Explain that a discussion will occur at the end of the scenario to explore how the event unfolded - debrief
• Orientate to the environment :
o Orientate to equipment and resources available. o Explain that both the faculty and the participants will need to work together to paint a picture of what
the “child” looks like. It’s Ok to ask for information that’s not clear to help with critical thinking. e.g. colour, vital signs on the monitor.
o Orientate to the capabilities of the mannequin being used – note, low technology mannequins work equally as well as a high technology mannequin
▪ eg. Does the chest rise and fall? Can they put an Intraosseus in? Can the mannequin be intubated? How do they safely shock the patient? How can fluids and medications be administered?
• Refer to the ‘Establishing a safe container’ paper in the resources list.
Running the Simulation :
• The 2 simulations in the OPTIMUS CORE both involve patient deterioration on the ward.
• As such, participants should be divided into groups to imitate the arrival of :
o Initial ward staff (core participants) – initial respondents
o Senior ward staff (core or advanced participants) – to arrive once initial respondents call for help
o Medical Emergency Response (advanced participants) – to arrive a few minutes after Medical
emergency call is made
▪ If there are no advanced participants the scenario ends with clinical handover to the medical
emergency team, played by faculty, ie announce team arrival – ‘please provide handover’. At
this stage – time permitting – the faculty can role model by recapping and stating a moving
forward plan.
• Begin the scenario with the initial ward staff, giving them the handover and call in other team members as
appropriate.
• Prompts should be given to participants to help them guage a picture of the clinical state – remember the
mannequin is not real and in a high state of stress they may not remember all you have mentioned during the
pre-brief. e.g. “they still look very blue”, or “they don’t seem to be breathing”. This is not a test for them, and
the more information they receive, the more real it will become and the more positive the experience will be.
• Once the scenario has reached its end point (either all learning objectives met or time is up), confirm this by
stating ‘end scenario’ and then direct participants to their debriefing area.

Page 25 of 41
Debriefing:
• It takes courage to perform simulated clinical care in front of your peers.
o As such, it is fundamentally important to remember that participants in simulation can feel
deeply vulnerable and that overt criticism or harsh feedback can result in an inability to take in
further constructive information, avoidance of future simulated teaching and other defensive
behaviour.
o Conversely, falsely ‘sugary’ feedback of poorly performed scenarios will ring true for neither the
participants nor their colleagues, and will not lead to adequate reflection or personal growth.
o We recommend the use of open questions that stimulate thought and discussion.
o Refer to the “PEARLS” paper in your resource material
• In the OPTIMUS CORE you will have 10 – 15 minutes to debrief, therefore the discussion will need to be
concise to utilise the time limitation efficiently.
Topics to consider when debriefing:
1. Teamwork in a Crisis :
o How were roles allocated?
o What impact did the clear (or unclear) allocation of roles have on the team?
o What Anticipation and Planning was demonstrated?
o What examples of good communication were seen?
o What impact did the environment/noise have on the resuscitation?
2. Clinical Handover :
o What handover points took place throughout the scenario?
o What would the new team members have liked to learn on arrival?
o Was there a transfer of leadership upon arrival of the MET team? What impact did this have
on the team?
3. Leadership :
o Who felt they were the team leader?
o Was that clear to the group?
o Who should be the team leader?
4. Clinical Knowledge and Skills :
o Eg..Was the CPR algorithm followed appropriately?
o How did the team ensure high quality CPR during the resuscitation?
o What were the initial cues that made the staff call for help?

Page 26 of 41
Further Simulation Delivery Resources : Queensland Clinical Skills Development Service : Simulation Provider Training
• Provides excellent courses including ‘The Fundamentals of Debriefing’ and ‘Simulation Provider training. Imperial College London, Handbook of Debriefing
• A downloadable handbook, includes the ‘SHARP’ structure for debriefing. NEHT Sim eLearning
NHET-Sim is designed for anyone who currently or intends to use simulation as an educational method to support the development of healthcare students and professionals.
Harvard Center for Medical Simulation
• Workshops for practicing clinicians that address the clinical and behavioral aspects of individual and team performance with a focus on crisis management and error prevention.
• Mostly run from Boston, but courses are provided in Queensland intermittently. Rudolph, J; Simon, R; Dufresne, R; Raemer, 2006. There’s no such thing as “Nonjudgemental” debriefing: a Theory and method for debriefing with good judgement: D Society for Simulation in Health Care Vol 1, No 1, pp 49 – 55.
An article on both the structure and content of high quality debriefing. Rudolph, JW, Raemer, DB, Simon, R 2014, ‘Establishing a Safe Container for Learning in Simulation: The Role of the Presimulation Briefing’. Simulation in Healthcare, Vol. 9, No. 6, pp 339 – 349.
• A useful article for pre-brief Eppich, W; Chen A. 2015 Promoting Excellence and Reflective Learning in Simulation (PEARLS): Society for Simulation in Health Care Vol. 10, No 2, pp 106 – 115.
A useful article for novice to expert Debriefers Cheng A, Palaganas J, Eppich W, Rudolph J, Robinson T, Grant V. 2015 Co-debriefing for Simulation-based Education: Society for Simulation in Health Care Vol. 10, No, 2, pp 69 – 75.
A useful article to help obtain the best value out of Co-debriefing Rutherford-Hemming, T 2012 ‘Simulation Methodology in Nursing Education and Adult Learning Theory’ Adult Learning Vol.23, No. 3, pp 129 – 137
• Covers some theories in relation to simulation as learning.

Page 27 of 41
Scenario 1 : Respiratory Deterioration and Apnoea
Part 1. Setup
Equipment Required:
• Simbaby/NewB or Infant ALS mannequin
• We recommend the use of a portable scenario box that can be used for both scenarios.
Layout:
• Lay out the manikin on a bed or a table to appear consistent with them lying on a hospital bed. Place Subnasal low flow Oxygen prongs on her.
• If a training resuscitation trolley is not available, the scenario equipment should be laid out on a broad table as an imitation ‘resus trolley’.
Table 11.1 Contents of the Scenario Box for Scenario 1 & 2
Airway Bag
Suction tubing
Yankauer sucker –small & large
1 x 6 & 8Fg, suction catheter
Oropharyngeal airways – 1x sizes 0, 1, 2
Infant nasal prongs (insitu on mannequin
for infant scenario)
Paediatric non-rebreather mask
1 x nasogastric tube size 8
1 x roll wide leucoplast tape
Breathing Bag
Self-inflating bag large & small
Masks 0/1, 2, 3-4
1 x Stethoscope
Intubation Bag
1 x size 3.0, 3.5, 4.0, 4.5, 5.0 cuffed ETT
1 x Laryngoscope handle
1 x Laryngoscope blades: size 1 & 2
straight & curved
1 x small intubation introducer
1 x Magill’s Forceps
1 x small & large pedi-cap
Circulation Bag
1 x IV cannula 22, 24 Fg
2 x Alco wipes
2 x 10ml, 5ml, 2ml, 1ml
2 x blunt 18g needles
2 x needless access device
4 x 0.9% N saline amp
1 x ‘teddy bear’ tegaderm
1 x tourniquet
1 x manual IO & EZ-IO needle (pink &
blue) & EZ-IO driver
1 x scissors
1 x blood gas syringe
Fluids and Lines
1 x 0.9 N saline 1L
1 x ‘pump’ IV line
1 x 3 way tap
1 x 50ml syringe
Drug Pack
2 x Adrenaline 1:10, 000
Miscellaneous
1 x Paediatric & adult Defib Pads
Infant & child BP cuff
Thermometer
Infant & child sats probe
2 x 3 way tap with extension + drainage
bag for IV access on manikin
Documentation
Scenario session plan
CEWT Form – age appropriate
Cardiac Arrest guidelines poster
Paediatric Resus Table / Emergency
Drug Preparation List
White Board markers
Remove contents from packets

Page 28 of 41
Part 2. Facilitator Instructions
Objectives:
1. Recognise and manage respiratory distress, impending respiratory failure and apnoea in an infant
• Clinical interventions: ➢ Suction, airway positioning, Nasopharyngeal airway ➢ Oxygen and ventilation: high-flow Nasal Prong oxygen / High concentration oxygen; bag-valve-mask;
intubation anticipation & preparation 2. Crisis resource management principles: Call for help early (local escalation process), effective leadership,
teamwork, role delineation, communication and handover.
Scenario synopsis:
2 month old admitted with bronchiolitis. Infant has history of Trisomy 21, is on nasal prong oxygen @ 1L/min. Sim
commences with Mother calling for help, is concerned that baby’s breathing is faster. Mother is covered in vomit
and needs to leave (removing the mother will reduce the cognitive load on the participants to allow them to focus on
managing the child). The infant has mod – severe resp effort. Respiratory compromise progresses with apnoea prior
to emergency responders arrival. Condition improves following intervention of airway clearance with suction and
supportive ventilation. Scenario concludes following handover to emergency responders and team coordination.
Sim Facilitator –instructions: 15 min scenario – 15 min debrief
• First rotation only, inform that there will be 3 rotations in this session - 2 scenarios and 1 PLS / defibrillation assessment.
• Remind participants that this scenario is a chance to consolidate what they have learnt in their e-Learning and face to face course, it is not new information and it is not a test
o Essential premise – “everyone attending is committed to improving their own practice, we bring together knowledge and experience and share those experiences to improve the care we provide to the children we care for.”
Orientate to mannequin and equipment and process:
Refer to OPTIMUS CORE Scenario PreBrief sheet in your course resource pack.
We know that this manikin is plastic, lets work together to paint a picture of what the child is like clinically.
This manikin can have a Guedel airway can be inserted, oxygen can be applied, it can be ventilated using a bag and
mask, fluids and drugs can be administered, and compressions can be done.
I will provide you with handover information for this child then I’d like you to assess the child, intervene where
necessary and evaluate interventions, I will give you additional information about the progress of the child condition on
request. If you need further clinical support please call for help.
We will have a discussion at the end of the scenario about how it unfolded.
• 1-2 participants commence scenario, the remaining participants are removed from the room and are fed into
the scenario as staff on the floor responding to initial call for assistance and then as emergency respondents.
If no critical care / advanced or medical staff participating facilitator takes on role of emergency responder
leader.
Facilitation Notes:
• Provide specific information about the case as it progresses.
• Discuss core learning objectives during debrief, refer to previous section on Debriefing (p 24).
• A debrief sheet is provided in your resource pack.

Page 29 of 41
Handover provided to initial participants prior to responding to call for help (remaining participants are
outside the room) :
Bronte 2month girl with Trisomy 21 (Down syndrome) admitted @ 0900hrs, with suspected RSV bronchiolitis. 3 day
history of respiratory symptoms.
A: Occasional suctioning of nares.
B: Resps 64, tracheal tug & intercostal recession (mild). Occasional moist cough. SaO2 >95% 1L/min NP O2.
C. P 150, CRT 2sec
D: Lethargic but responding to mother.
E: T 38˚C, Poor feeding – EBM, Weight – 4.5Kg.
You answer the call bell and are confronted by Bronte distressed mother, who states that Bronte has vomited
her feed and is now breathing faster. Mother leaves room to wash off vomit. Please assess Bronte.
Time States Patient Status Expected Actions Teaching Points
Recognition of
deterioration
in condition –
resp
compromise
A. Nasal secretions +++ B. RR 76, grunting, head
bob, subcostal recession; SaO2 91%
C. HR 170; BP 87/45; CRT 3, cool peripheries, very pale
D. Weak cry to pain E. T – 38.0
Assess ABCD • Early recognition of deterioration + call for help
• MET activation criteria
• Ward Role allocation
• Anticipation of resources required for management
Call for local assistance
Suction
High flow O2 - face mask + reservoir
Activate MET – Local emergency number
Allocate Ward Roles – team leader
15 second
apnoea
A. Nil noises B. RR 0; SaO2 86%; C. HR 190; BP 85/45;
CRT 4 Very pale, cold.
D. Nil response E. BGL – 6.8mmol/L
Airway positioning + Ventilatory support • Respiratory management
• Role responsibilities
Circ: prep IV access & fluids
Documenter: wt; resus table; resus record
Runner – assit as required
MET arrival
Condition
improves with
airway
clearing and
supportive
ventilation.
End scenario
A. Gurgled airway sounds B. RR 36; SaO2 no trace; C. HR 200; BP 70/40;
CRT 4; cold. D. Unresponsive
Handover to MET – SBAR • SBAR handover
• Leadership
• Role delineation, Team coordination
• Communication
Identify leader, coordinate roles
Respiratory support – prep for intubation

Page 30 of 41
Scenario 2 : Cardiac Arrest
Part 1. Setup
Equipment Required:
• SimJunior/Megacode Kid
• Resuscitation Equipment
• Training Defibrillator with Rhythm Selector
• We recommend the use of a portable scenario box that can be used for both scenarios.
• The scenario box should contain the equipment listed in the Table 12.1.
Layout:
• Lay out the manikin on a bed or a table to appear consistent with them lying on a hospital bed. An IV should be marked as ‘in situ’ in one cubital fossa.
• If a training resuscitation trolley is not available, the scenario equipment should be laid out on a broad table as an imitation ‘resus trolley’.
• A training defibrillator should be set up very near the patient, for use when the emergency responders arrive.
Refer to Table 11.1 for equipment list

Page 31 of 41
Part 2. Facilitator Instructions
Objectives:
1.Emergency management of the child with circulatory compromise and cardiac arrest in the context of hypovolaemic
shock
• Airway / Breathing – Oxygen and ventilation (high concentration mask (non-rebreather; self-inflating bag & mask)
• Circulation – fluid bolus, insertion of intraosseous, CPR, paediatric cardiac arrest algorithm
2.Crisis resource management principles: Call for help early, effective leadership, teamwork, role delineation, communication and handover in a crisis situation.
Scenario synopsis:
5 year old admitted to ward with gastroenteritis. Scenario commences with staff responding to oximeter alarm. Child
shows signs of circulatory compromise and shock, with rapid decompensation and loss of output. Scenario concludes
following management of cardiac arrest (non-shockable pathway).
Equipment Required:
• Megacode Kid / SimJunior
• Emergency Bedside equipment - oxygen & suction
• Mock ward medical emergency trolley / scenario equipment on table
Sim Facilitator –instructions: 15 min scenario – 15 min debrief
• First rotation only, inform that there will be 3 rotations in this session - 2 scenarios and 1 PLS / defibrillation assessment.
• Remind participants that this scenario is a chance to consolidate what they have learnt in their e-Learning and face to face course, it is not new information and it is not a test
o Essential premise – “everyone attending is committed to improving their own practice, we bring together knowledge and experience and share those experiences to improve the care we provide to the children we care for.”
Orientate to mannequin and equipment and process:
Refer to OPTIMUS CORE Scenario PreBrief sheet in your course resource pack.
We know that this manikin is plastic, lets work together to paint a picture of what the child is like clinically.
This manikin can have a Guedel airway can be inserted, oxygen can be applied, it can be ventilated using a bag and
mask, fluids and drugs can be administered, and compressions can be done.
I will provide you with handover information for this child then I’d like you to assess the child, intervene where
necessary and evaluate interventions, I will give you additional information about the progress of the child condition on
request. If you need further clinical support please call for help.
We will have a discussion at the end of the scenario about how it unfolded.
1-2 participants commence scenario, the remaining participants are removed from the room and are fed into the scenario as staff on the floor responding to initial call for assistance and then as emergency respondents. If no critical care / advanced or medical staff participating facilitator takes on role of emergency responder leader.
Facilitation Notes:
• Provide specific information about the case as it progresses.
• Discuss core learning objectives during debrief, refer to previous section on Debriefing (p 24).
• A debrief sheet is provided in your resource pack.

Page 32 of 41
Handover provided to initial participants (remaining participants are outside the room):
Samuel, 5 years old admitted to the ward from DEM with gastroenteritis. He initially presented to ED with a three
day history of fevers, vomiting and profuse diarrhoea with minimal oral intake. He had difficult but successful IV
access in ED. Assessed as moderate dehydration requiring IV fluid rehydration. Wt 20kg. Most recent observations:
A. patent B. RR 28, sats 96 C. pale, HR 138, CRT 2-3 sec, BP 90/55, 1x PIVC in situ D. irritable
Oximeter alarms – please assess Samuel.
Time States Patient Status Expected Actions Teaching Points
Recognition of
deterioration in
condition
A. Patent B. RR 35, shallow; SaO2 86% C. HR 150; BP 90/40; CRT
5s; mottled, cool. IV tissued (oedematous hand)
D. Responds to painful stimuli by groaning
E. T39.3
Assess ABCD • Early recognition of deterioration + call for help
• MET activation criteria
• Ward Role allocation
Airway positioning
High flow O2 - face mask +
reservoir
Call for local assistance
Activate MET –Local emergency
number
Allocate Ward Roles – team leader
Circulatory
compromise
A. Patent B. RR 42, SaO2 76% C. HR 170; BP 80/40; CRT
7s; dusky D. Unresponsive E. Large bowel motion noted
Ventilatory support – PEEP - adv • Supportive ventilation
• Anticipatory planning
Prep IV/ IO access & fluid boluses
Cardiac arrest
(PEA)
A: Apnoeic, nil obstruction
B: RR 0; SaO2 not trace
detected
C: (HR70) Pulseless; BP
undetectable; CRT 7s
D: unresponsive. BGL
8.8mmol/l.
Effective CPR • Indications for CPR
• CPR Prep adrenaline
Prep intubation
MET arrival
End scenario
following 2
non-shockable
cycles
A: Nil obstruction
B: RR 0; SaO2 not trace
detected
C: PEA rate 70; BP
undetectable; CRT 7s
ROSC – following adrenaline 10mcg/kg D: BGL 8.8mmol/l
Handover to MET – SBAR • SBAR handover
• Leadership
• Role delineation, Team coordination
• Communication
• Shockable / non-shockable pathway
Apply defib pads, Rhythm
recognition, Safe charging for
defibrillation 4j/kg (dumped)
Adrenaline 10mcg/kg, Fluid
bolus(es)
Consideration of 4 H’s & 4 T’s

Page 33 of 41
The Testing Station
Aim:
• The testing station provides an opportunity for participants to demonstrate learning and meet annual paediatric life
support competency requirements
• The assessment can be divided into CPR and defibrillation to facilitate targeted assessment for core and
advanced participants i.e. core participants complete CPR assessment and advanced participants complete CPR
and defibrillation assessments
• It will be at the discretion of local faculty to decide the assessment requirements of the participants
Equipment required :
• BLS mannequin e.g. Baby Anne™ or Little Junior™
• Self-inflating resuscitation bag to suit mannequin
• Mask sizes 0/1, 2, 3-4
• Paediatric and adult defib pads – laminates provided in resource pack if none available
• Paediatric resuscitation table
• CPR and defibrillation assessment sheets
• Paediatric CPR assessors reference sheet
• Cardiopulmonary arrest algorithm (for defib assessment)
• Defibrillator and rhythm simulator or photo laminates of defibrillator and 4 arrest rhythms (for defib assessment)
Layout :

Page 34 of 41
Structure :
The assessment may be performed as a 1:1 session or as a group. Running the assessment as a group provides the
opportunity for observation of those being assessed on their leadership skills. Creation of psychological safety is
paramount, place emphasis that discussion around others performance outside the assessment space is not
condoned.
Please note this assessment is not an attempt to ‘catch out’ or fail participants who are clearly capable of providing
Basic Life Support. As with the simulations the manikin is not real and some small amounts of prompting may be
required to trigger appropriate responses to some assessment questions. Small errors may be addressed by marking
as ‘Requires further development’ and used as an opportunity for brief discussion at the end of the assessment.
Begin the session by orientating the participants to the environment, equipment available and process – similar to
Prebreifing a simulated scenario.
Below is a guide to running the session as a group and will need modification of roles based on the number of
participants . We would suggest 4 – 5 participants per assessment group.
• Participant 1 is the first responder and is provided with a clinical scenario relevant to their practice. (Please
see next page for Scenario options). They are to proceed through the standard DRSABCD algorithm as per
their assessment sheet and then take on the leadership role (advanced).
• Participant 2 & 3 arrives to help on request for “send for help’ and takes over CPR
• Participant 4 places on defibrillation pads and runs the defibrillator
• Participant 5 gives fluid bolus and adrenalin
‘Core’ participants are expected to successfully perform DRSABCD – up to application of defib pads & respond
appropriately to directions for safety. They can give fluid bolus and adrenaline as directed.
‘Advanced’ participants are expected to successfully proceed through the standard DRSABCD algorithm and then to
continue on through attaching a defibrillator and successfully treating the rhythms provided. Leadership component
includes allocating roles and direction to the team in managing the scenario.
Resources :
On the following pages, please find an assessor’s resource guide including :
• Scenario options for assessments
• Detailed performance criteria for passing/failing participants
• Information on expected knowledge for advanced participants being assessed on defibrillation
• Participant assessment sheets

Page 35 of 41
Assessor’s Guide : Assessment Station Scenario Options
Scenario A
You are caring for James who is two (2) hours post bronchoscopy.
➢ Age: 6 months OR 6 yrs ➢ Weight: 7Kg OR 20Kg ➢ Post theatre James has been vomiting and is very irritable. ➢ Resp rate normal ➢ Tachycardic, CRT < 2 sec, pale.
You enter the room to perform a set of observations and notice that James is lying in the cot/bed is grey looking and appears to be not breathing.
What action do you take?
Scenario B
One of your colleagues asks you to attend a patient’s respiratory observations on while they are at morning tea. The nurse hands over Brian, who was admitted during the night with febrile neutropaenia:
➢ Age: 8months OR 4 years ➢ Weight: 8Kg OR 16kg ➢ Tachypnoea. Increasing respiratory effort; Oxygen via nasal prongs @ 2Lpm maintaining saturations at
95%. ➢ Tachycardic. ➢ Lethargic this morning. ➢ Peripheral IVT @ 52mL/hr N/saline & 5% Dextrose. ➢ First dose of an antibiotic completed 15 minutes ago.
15 minutes later you enter the room to perform a set of observations. On visual assessment Brian is lying in bed and not moving and profoundly pale. No one else is present. What action do you take?
Scenario C
You are working a night shift in a paediatric ward/adolescent mental health. You are observing the children and find Angela a 13 year old, 32Kg with anorexia nervosa, lying on the floor, face down next to her bed. What action do you take?
Other Scenario example: (please use if assessor is not familiar with the assessee’s work area)
You are walking along the 3rd floor medical building hall way and an adult who is carrying an infant/child calls out
“please help my baby/child, she’s not breathing”.
On visual assessment the child is not breathing, cyanosed and is limp in mothers’ arms.
Note: To assist in the flow of scenario, medical emergency equipment can be obtained from a neighboring ward

Page 36 of 41
Assessor’s Guide : Expected Standards of Achievement
PERFORMANCE CRITERIA EVIDENCE OF ACHIEVEMENT
Danger
Checks for and addresses danger to self, patient and others
• Articulates the various types of danger to self and other health professionals.
Example : electrical hazards, water/spills, cytotoxics, body fluids
• Identifies how to correct / mitigate potential risk: ie using PPE, ergonomic
safety
• Discusses the potential danger to the patient
Response
Checks response by using verbal and tactile stimuli
• Demonstrates tactile and verbal behaviour to elicit a response from the
patient. Example “Are you alright?” and firm central stimulation.
Shout / Send for Help
If patient is unresponsive calls for help
• Identifies the appropriate method for gaining the necessary assistance
according to their work area and the situation. Ie. Press emergency buzzer
and initiate local medical emergency response
• Recognises that if there is no local assistance, proceeds with CPR for one
minute prior to seeking help
Airway
Clears and Opens the Airway
• Checks the mouth for any foreign material
• If no foreign material in the mouth, places patient supine
• If vomit/foreign material in the mouth, turns the patient if able and clears the mouth using suction if available
• Opens the airway using the appropriate technique for age group.
➢ Head tilt chin lift into the neutral position for infants under 1 year
➢ Head tilt chin lift into the sniffing position for children over 1 year of age.
• Utilise jaw thrust if suspected C-Spine injury in all ages.
• Considers use of airway adjunct once CPR is in progress - oropharyngeal airway – to facilitate airway opening and effective bag-mask ventilation
Breathing
Assess for normal breathing (look, listen and feel)
Demonstrates effective delivery of breaths to the patient
• Looks for chest wall movement
• Listen for expelled air
• Feel for escape of air from nose and mouth
• If patient not breathing and self-inflating bag is available provide rescue breaths.
• If self-inflating bag is not readily available, assess circulation and commence chest compressions (ie no delay in commencing CPR) whilst equipment is being obtained
• Deliver 2 breaths using self-inflating bag and appropriate size mask to achieve an effective seal.
• Observe for chest wall movement
CPR
Assess for signs of life for up to 10 seconds
Commence CPR – Demonstrates compressions at correct depth, rate and ratio to breaths
• Assess response to resuscitation breaths, ie cough and spontaneous movement, normal breathing
• Assess central pulse in appropriate location
• Infant <1 yr – brachial/femoral
o Child >1 yr – carotid / femoral
• Start chest compressions if:
o You can’t feel a pulse
o Pulse rate is <60 bpm with associated poor perfusion
o There are no “signs of circulation/signs of life”
• If in doubt, commence compressions
• Ensures patient is on a firm surface Ie. Deflate any mattresses, utilise CPR backboards
• Demonstrates appropriate hand position according to age
o Infant <1 yr – 2 fingers or 2 thumbs
o Child > 1 yr – 1 or 2 hands
• Demonstrates the use of the correct compression technique
o Lower half of the sternum all ages
o 1/3 depth of the chest all ages
• Compression to breath ratio single & dual rescuer 15:2

Page 37 of 41
• Ensure chest wall fully recoils between compressions
• Shoulder vertically over the sternum, compressing arm remains straight, equal
time for compression and relaxation
• Compresses at a rate of 100 – 120 per minute
• Pauses compressions to give 2 breaths
• Communicates with second rescuer to avoid any unnecessary interruptions to
compressions
• Coordinates rotation of rescuers every 2 mins.
• Advanced participants aware of continuous compressions once patient intubated, ie no need to pause for breaths
Defibrillation – core & advanced
For advanced participants undergoing Defibrillation assessment refer to additional information below.
• Demonstrates appropriate placement of defibrillation pads o One over apex of mid axillary line and the other immediately below the
clavicle to the right of the sternum o OR anterior / posterior – between shoulder blades on the back and to
the left of the sternum
• Discuss safety aspects of defibrillation o Ensure implanted devices (i.e. pacemaker), GTN patch, ECG dots and
leads are not under the defibrillation electrodes o Look for danger – water, oxygen other flammable substances
• Advanced participants o The operator is responsible for the safety of the patient and members
of the team – “all stand clear” and perform a visual sweep o Shockable rhythm = Ventricular tachycardia and ventricular fibrillation o Non-shockable rhythm = PEA / Asystole o Paediatric joules = 4J/kg
Fluids and medications • Adrenaline
o Can locate on resuscitation trolley
o Dose = 10micrograms / kg
o Utilises resources available – ie Resuscitation Table
o Action – increases myocardial and cerebral blood flow
o Increases heart rate, conduction and contractility
o Increases systemic vascular resistance
• Fluid Bolus
o 0.9% Sodium Chloride 10 - 20mL/kg
o Intraosseous route if in arrest
Communication, documentation and
management
• Demonstrate use of Resuscitation Table
• Awareness of documentation requirements
• Discusses resources available for carers and staff
• Discuss ongoing patient observation post resuscitation (ABCD assessment)
• Familiar with replacement of medical emergency equipment
Advanced:
• Demonstrate use of Paediatric Cardiac Arrest Algorithm – shockable & non-shockable pathways
• Directs team members in providing fluid bolus & adrenalin according to Algorithm
• Consideration of 4H’s & 4 T’s

Page 38 of 41
Assessor’s Guide : Expected Defibrillation Knowledge
Defibrillation
Shockable rhythms 4 joules/kilogram
Ventricular Tachycardia (VT) Ventricular Fibrillation (VF)
Adhesive Pad placement
• Effective defibrillation depends on an adequate current traversing the myocardium. Therefore electrodes should be placed in positions that maximize current flow through the heart.
Defibrillation Safety Factors
• Ensure good contact (no air bubbles) with pads.
• Dry patient’s chest, and there is no water/fluid between personnel and the patient
• Ensure patient is not touching metal surfaces – may result in burns
• Do not place pads over ECG electrodes, monitoring leads, medication patches (ie Glyceryl Trinitrate - GTN), IV tubing/fluid filled tubes, implantable devices
• Pre-charge energy to minimise hands off chest
• Remove flowing oxygen devices one meter away from patients chest
o Leave bag-valve resuscitator attached to ETT/LMA in intubated patients, or detach from ETT/LMA and remove 1m away from patients chest
• Ensure all personnel are standing clear prior to discharge of shock – CPR continues during charge of shock, discontinues during delivery of shock and recommences immediately following delivery of shock.
o the defibrillator team member states ‘stand clear’, and observes that all personnel are not touching the patient, then delivers the shock whilst stating “defibrillating / or shock”

Page 39 of 41
REFERENCES:
Advanced Life Support Group (2015) Advanced Paediatric Life Support- The Practical Approach 5th Edition BMJ Publishing Group
ILCOR guidelines (2015)
Australian & New Zealand Council on Resuscitation, 2015, Guidelines Australian Resuscitation Council, Melbourne

Page 40 of 41
CPR Assessment Sheet (Core and Advanced Participants)
Element Performance Criteria Achieved Needs Further
Development
Danger Checks for and addresses danger to self, patient and others
Response Checks response by using verbal and if required firm central
stimulus
Shout / Send
for help
If patient is unresponsive calls for help
Initiates local emergency response
Airway Clears and Opens the Airway using appropriate position for
age
Breathing
Assesses for normal breathing (look, listen and feel)
Demonstrates effective delivery of breaths (2)
CPR
Assesses for Pulse – no longer than 10 seconds
Commence CPR – Demonstrates compressions at
correct depth, rate and ratio to breaths – 15: 2
Able to verbalise adult ratio 30:2
Continues to call
for help
Ensures continuous CPR whilst calling again for help
after 1 minute if no immediate help arrives
Defibrillation
Demonstrates appropriate placement of defibrillation pads
• 2nd intercostal space on the right side of the chest & 5th
intercostal space on the left side of the chest
• OR anterior / posterior – between shoulder blades on the
back and to the left of the sternum
Has an understanding of safety aspects of defibrillation
• Water, oxygen, flammable substances
• Do not place electrodes over GTN patch, ECG electrodes,
port
Fluids &
medications
Knowledge of fluid resuscitation (fluid type and volume for 10
Kg infant & 20 Kg child)
Knowledge of adrenaline dose (10kg infant & 20Kg child)
– utilises resources as appropriate.
Communication Provides handover of situation using SBAR framework
Paediatric Cardiopulmonary Resuscitation
Assessment Achieved: Not Achieved:
Comments / Recommendations:
Date:
Assessor: (Print Full Name)
Signature: Designation:
Assessee: (Print Full Name)
Signature:
Designation:
Personal Assignment No/s:
Work Location:
Line Manager: (Print Full Name)

Page 41 of 41
Defibrillation Assessment Sheet (Advanced Participants)
Scenario: You’ve arrived at a resuscitation situation, your colleagues are performing effective CPR on a 10 / 25 Kg
child. The defibrillator has arrived and you are asked to place defib pads, assess rhythm and manage according to the
cardiac arrest pathway.
Element Performance Criteria Achieved Needs Further
Development
Rhythm
recognition
Assess rhythm to determine the need for defibrillation
(Ventricular Fibrillation / pulseless Ventricular Tachycardia)
Efficacy of
Shock
delivery
• Maintains CPR prior to assessing rhythm
• Recommences CPR immediately post shock
• Continues CPR for 2 minutes in between shocks before reassessing rhythm and presence of pulse
Selects appropriate sized self adhesive pads
Demonstrates appropriate placement of defibrillation pads
Selects appropriate energy requirements 4j /kg (40j rounds up
to 50j / 100j)
Charges defibrillator (CPR maintained)
• 2nd shock - charges defibrillator prior to end of 2 minute cycle
Considers timing to minimise interruption to chest
compressions, prepares adrenaline 10 micrograms / Kg
for administration following 2nd shock
Safety &
Communicati
on
Ensures electrical safety throughout procedure
Has an understanding of safety aspects of defibrillation:
• Water
• Oxygen, flammable substances • Metal - Do not place electrodes over GTN patch, ECG
electrodes, port Disarms defibrillator (non-shockable pathway)
Operates defibrillator correctly
Delivers shock safely – clearly articulates and ensures “all stand
clear”
Utilises
Resources
Utilises Cardiopulmonary Arrest pathway
Assessment rhythms – VF, VF, Sinus rhythm
Communicatio
n
Records procedure correctly
Paediatric Defibrillation Assessment Achieved: Not Achieved:
Comments / Recommendations:
Date:
Assessor: (Print Full Name)
Signature: Designation:
Assessee: (Print Full Name)
Signature: Designation:
Personal Assignment No/s: Work Location:
Line Manager: (Print Full Name)