P. Nottingham Chaplin, Ed.D. Good Lite School Health ... · P. Kay Nottingham Chaplin, Ed.D....
Transcript of P. Nottingham Chaplin, Ed.D. Good Lite School Health ... · P. Kay Nottingham Chaplin, Ed.D....
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
1
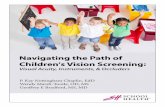
Vision Screening:
Getting to the Nitty-Gritty of How to Screen… What to Use…and What to Avoid
P. Kay Nottingham Chaplin, EdD
• Former Director/Lead Trainer – Vision Initiative for Children – WVU Eye Institute
• Trained >1,600 individuals, 178 workshops (majority on location)
• Current Director – Vision and Eye Health Initiatives at Good-Lite and Vision Screening and Eye Health Consultant for School Health Corporation
• Member – Expert Advisory Committee to the National Center for Children’s Vision and Eye Health at Prevent Blindness
• Member - Questionnaire Work Group, a Children’s Vision Massachusetts coalition project to study screening the birth to 3 population
• National Vision Screening Trainer for Prevent Blindness
• Consultant to Vision Screening Committee of the American Association for Pediatric Ophthalmology and Strabismus
• Will see “great” and “really awful” eye charts manufactured by The Good-Lite Company and marketed through Good-Lite and School Health Corporation, but focus is not to push product from the podium
• Focus is to use power of podium to encourage appropriate and evidence-based vision screening as part of a strong Vision Health System of Care
Introduction and Disclaimer
2
How to Build a Strong Vision Health System of Care
3http://nationalcenter.preventblindness.org/resources-2
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
2
Evaluating Your Vision Health Program
4http://nationalcenter.preventblindness.org/resources-2
3 Vision Screening Approaches
5
• Three approaches to vision screening, depending on child age:
1. Developmental questions
2. Optotype-based (a.k.a. test of visual acuity) beginning at 3 years
3. Instrument-based beginning at 6 months
• Optotype = name of shape, letter, or number to identify
• Optotype-based screening measures visual acuity
• Provides info about presence or absence of refractive error and pathology within the visual pathway
• Instrument-based screening measures for presence of amblyopia risk factors: Significant refractive error
Asymmetry of refractive error
Asymmetry of eye alignment
Presence of cataract
1. Vision milestone at age 8 weeks (by 6 weeks and no later than 8 weeks)
• Eye contact
a. Does the infant have good eye contact with parents?
b. Does the infant already copy facial expressions?
6
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
3
7
Eye contact with parents is essential to developing bonding and communication.
Lack of eye contact can interfere with early emotional and general development.
• Early intervention should begin immediately.• The infant’s parents should receive assistance in
helping the infant to develop communication through all the senses.
• The infant should receive an eye exam from an eye doctor without delay.
8
9
2. Vision milestone at age 12 weeks
• Enjoyable visual interaction
a. Does the infant have a social smile?
b. When the parent smiles at the infant, does the infant respond with a smile?
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
4
10
A social smile means the brain is maturing, the infant can see short distances, and the infant is making sense of an object.
A social smile boosts bonding and is one of the cornerstones of communication between infant and parent.
11
3. Vision milestone at age 3 to 4 months
• Awareness of and exploration of hands
a. Does the infant watch her hands?
b. Does the infant bring his hands to midline and to his mouth?
c. Does the infant hit and grasp toys hanging above her?
12
Awareness of hands leads to exploring the hands with the mouth, which leads to using the hands to explore the infant’s world.
Exploration with hands gives concrete information about abstract objects, including size, form, surface quality, and weight.• This concrete
information will be stored in the infant’s brain to combine with the visual concept of each object.
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
5
13
4. Vision milestone at age 5 to 6 months:
• Watching and copying goal-directed reach and learning to copy motor functions
a. Does the infant watch other children playing?
b. Does the infant reach for objects?
1) Does the infant look at the object when reaching?
c. Are the infant’s eyes straight?
14
Reaching for a desired object leads to goal-directed behavior and shows desire, interest, and curiosity – critical elements for learning.
If the infant is not reaching for objects, maybe the infant cannot see the objects.
If the eyes appear to intermittently turn in or out at age 6 months, recommend that the infant receives an eye exam by eye doctor.
5. Vision milestone at age 7 to 10 months
• Recognition of familiar faces
a. Does the infant recognize family members before hearing their voice or seeing their smile?
b. Does the infant look at or into the parent’s eyes?
15
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
6
16
If the infant does not recognize faces and does not look at, or into the eyes, of the parent, the infant may have “face blindness” and should be referred for a neurological assessment.
A child with “face blindness” may incorrectly be diagnosed with an autism spectrum disorder. (Google “60 Minutes” and face blindness.)
Threshold vs. Critical Line
• Threshold screening
Move down chart until child cannot correctly identify majority of optotypes
• Critical line screening
Use only line child needs to pass according to child’s age
• Research supports using single, LEA Symbols optotypes surrounded with bars for children ages 3 to 5 years at 5 feet
Single, Surrounded LEA Symbols
18
Vision in Preschoolers (VIP) Study Group. (2009). Findings from the Vision in Preschoolers (VIP) Study. Optometry and Vision Science, 86(6), 619-623.
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
7
Importance of Appropriate Tools
• “Visual acuity scores can be significantly affected by the chart design.” (p. 1248)
• Bailey, I.L. (2012). Perspective: Visual acuity – Keeping it clear. Optometry and Vision Science, 89(9), 1247-1248.
• Excluding optotype size, “each visual acuity level on a test chart should present an essentially equivalent task”. (p. 740)
• Bailey, I. L., & Lovie, J. E. (1976). New design principles for visual acuity letter charts. American Journal of Optometry & Physiological Optics, 53(11), 740-745.
20
National and International Distance Visual Acuity Eye Chart Recommendations
• 1980 - National Academy of Sciences-National Research Council (NAS-NRC)
• Recommended Standard Procedures for the Clinical Measurement and Specification of Visual Acuity
• Committee on Vision. (1980). Recommended standard procedures for the clinical measurement and specification of visual acuity. Report of working group 39. Assembly of Behavioral and Social Sciences, National Research Council, National Academy of Sciences, Washington, DC. Advances in Ophthalmology, 41:103–148.
• 1984 - International Council of Ophthalmology (ICO)
• Visual acuity measurement standard. • www.icoph.org/dynamic/attachments/resources/icovisualacuity1984.pdf
• 2003 - World Health Organization Prevention of Blindness & Deafness (WHO)
• Consultation on Development of Standards for Characterization of Vision Loss and Visual Functioning
• Prevention of blindness and deafness. Consultation on development of standards for characterization of vision loss and visual functioning. Geneva: WHO;2003 (WHO/PBL/03.91).
• 2010 – American National Standards Institute, Inc.
• ANSI Z80.21-1992 (R2004) Approved May 27, 2010• Performance standard for the optical design of optotypes used in clinical visual
acuity measurement systems
21
Optotypes approximately equal in legibility
Horizontal between-optotype spacing = 1 optotype width
Vertical between-line spacing = height of next line down
Geometric progression of optotype sizes of 0.1 log units (logMAR, ETDRS)
5 optotypes per line
Optotypes black on white background with luminance between 80 cd/m2 and 160 cd/m2
Similar recommendations across guidelines
Design guidelines = “ETDRS chart”
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
8
22
Tips:• Line outside optotypes• 20/32 vs. 20/30• 10 feet vs. 20 feet
YES
NO
23
Do the following eye charts fit national/international eye chart design guidelines?
Yes or No?
NO
24
GuidelineAllen Sailboat Lighthouse Tumbling
EHOTV LEA
SymbolsSnellen Sloan
Letters
Optotypes should be approximately equal in legibility
X X X
Horizontal between-optotype spacing = 1 optotype width
X X X
Vertical between-line spacing = height of next line down
X X X
0.1 log unit geometric progression of optotype sizes
X X X
5 optotypes per line X X X
Optotypes black on white background X X X X X X X X
Similar mean visual acuity values when compared with the Landolt C international reference (------ = not included in study)
NO ------ NO X NO X ------ ------
Allen Pictures
“Sailboat”
Lighthouse or “House, Apple, Umbrella”
TumblingE HOVT LEA Symbols Snellen Sloan
Letters
Candy, T. R., Mishoulam, S. R., Nosofsky, R. M., & Dobson, V. (2011). Adult discrimination performance for pediatric acuity test optotypes. Investigative Ophthalmology & Visual Science, 52(7), 4307-4313.
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
9
Options for Pediatric Eye Charts
LEA Symbols HOTV
25
• Only pediatric eye chart with optotypes that blur equally at threshold
• Culturally neutral
• Children call optotypes what they want
• i.e., Square may be an iPad
• Circle may be hula-hoop
LEA Symbols
26
Candy, T. R., Mishoulam, S. R., Nosofsky, R. M., & Dobson, V. (2011). Adult discrimination performance for pediatric acuity test optotypes. Investigative Ophthalmology & Visual Science, 52(7), 4307-4313.
Hered, R. W., Murphy, S., & Clancy, M. (1997). Comparison of the HOTV and Lea Symbols charts for preschool vision screening. Journal of Ophthalmic Nursing & Technology, 16(2), 68-73.
• Young children: 10 feet from chart to child’s eyes
• New, standardized charts will be at 10 feet
• 10/xx on left side of chart with 20/xx on right side
Screening Distance
27
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
10
• 100% spacing between optotypes (1 optotype-width)
• Unequal spacing BETWEEN lines – not geometric progression of 0.1 log (logMAR)
• Arbitrary and non-standardized between-line spacing
NO - “Linear-Spaced” Eye Charts
28
• Between-optotype spacing >100%
• Unequal spacing BETWEEN lines – not geometric progression of 0.1 log (logMAR)
• Between-line spacing is arbitrary
• Basically contains lines of single optotypes
NO - “Wide-Spaced” Eye Charts
29
No Single Optotypes or Flashcards Without Surround Bars for Typically Developing Children
30
• Visual acuity results, on average, 3 lines worse on charts with lines vs. single, non-crowded optotypes
• For example, 20/32 with single, isolated optotype and 20/80 with line chart
Youngson, R. M. (1975). Anomaly in visual acuity testing in children. British Journal of Ophthalmology, 59(3), 168-170.
Hilton, A. F., & Stanley, J. C. (1972). Pitfalls in testing children’s vision by the Sheridan Gardiner single optotype method. British Journal of Ophthalmology, 56(2), 135-139.
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
11
• a.k.a. ETDRS chart
• a.k.a. logMAR chart
Want “Proportional” Spacing
31
32
Occluders – Younger Children <10 Years
SunflowersFun Frames –Frosted
33
Instrument-Based Screening
Welch Allyn SureSight
Welch Allyn Spot Vision Screener
Plusoptix S12
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
12
• Instruments
• Require minimal child response or interaction
• Titmus is a machine and not an instrument
Instrument-Based Screening
34
Neely, D. E. (2013). The eyes have it: Advances in vision screening should lead to early diagnosis, treatment of preventable blindness in children. AAP News, 34(5), 14-15.
35
Letters LEA Symbols
Titmus Examples
Current Recommendations
36
Miller, J. M., Lessin, H. R., American Academy of Pediatrics Section on Ophthalmology, Committee on Practice and Ambulatory Medicine, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, & American Association of Certified Orthoptists. (2012). Instrument-based pediatric vision screening policy statement. Pediatrics, 130(5), 983-986. Retrieved from http://pediatrics.aappublications.org/content/130/5/983.full.pdf+html
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
13
Instrument-Based Screening
• Most experts believe cannot convert instrument measurement to visual acuity
• If use instruments, have test of visual acuity as back-up
• Forgot to charge battery
• Device malfunctions
• Cannot achieve a reading
• Head Start children in Vision in Preschoolers Study
• Could “nearly always” participate in instrument-based screening if unable to participate in optotype-based screening, and vice versa
Vision in Preschoolers Study Group. (2007). Children unable to perform screening tests in Vision in Preschoolers Study: Proportion with ocular conditions and impact on measure of test accuracy. Investigative Ophthalmology & Visual Science, 48(1), 83-87. Retrieved from http://www.iovs.org/content/48/1/83.full.pdf+html
• Pointing to each optotype to help children know where they are on the chart is permissible.
True or False?
False• 1.8 “Line-by-line isolation or
pointing may be used, but not letter by letter.”
Pointing from World Health Organization
38
• Can just anyone screen vision?
• World Health Organization recommends “regular training” for screeners
because “ . . . the skill of the testeraffects very significantly the validity and variability of the outcome.” p.6
39
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
14
40
Prevent Blindness Certified Screener
http://www.preventblindness.org/become-vision-screener
Place individual cards on floor in front of child.
Ask child to step on the card that matches your symbol.
Matching Variation
41
World Health Organization (2003) says:
• May be less tedious for children to read 1st optotype on left-side of chart until missing one and then moving up a line and reading entire line
• Camparini et al. found: ETDRS-Fast (reading 1 letter per row until a mistake is made) yields accurate results compared with standard method of reading each optotype on every line.
• Also – significantly reduced test time
No Need to Read Each Optotype on Every Line
42
Camparini, M., Cassinari, P., Ferrigno, L., & Macaluso, C. (2001). ETDRS-Fast: Implementing psychophysical adaptive methods to standardized visual acuity measurement with ETDRS charts. Investigative Ophthalmology & Visual Science, 42(6), 1226-1231.
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
15
• Down Syndrome, prematurity, juvenile idiopathic arthritis, and neurofibromatosis.1
• A family history of amblyopia, strabismus, retinoblastoma, congenital cataracts, or congenital glaucoma.1
• Developmental delays, intellectual disabilities, neuropsychological conditions, and/or behavioral issues that render them untestable.1
• Low birth weight, prolonged supplemental oxygen, or grades III or IV intraventicular hemorrhage.2-3
• Retinopathy of prematurity.2-3
• Whose mothers smoked or used drugs or alcohol during pregnancy.2-3
• Whose mothers had rubella, toxoplasmosis, venereal disease, herpes, cytomegalovirus, or human immunodeficiency virus during pregnancy.2-3
• Whose mothers experienced difficult or assisted labor, which may be associated with fetal distress or low Apgar scores.2-3
• Known or suspected central nervous system dysfunction evidenced by developmental delay, cerebral palsy, dysmorphic features, seizures, or hydrocephalus.2-3
• On the autism spectrum.4
Children Who Should Bypass Vision Screening and Go Directly to Eye Exam
43
44
Children Who Should Bypass Vision Screening and Go Directly to Eye Exam
References:
1American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel. (2012). Preferred Practice Pattern® Guidelines. Amblyopia. San Francisco, CA: American Academy of Ophthalmology. Retrieved from www.aao.org/ppp
2American Optometric Association. (1994; Revised 1998; Reviewed 2004). Optometric clinical practice guideline: Care of the patient with amblyopia. St. Louis, MO: American Optometric Association. Retrieved from www.aoa.org/documents/CPG-4.pdf
3American Optometric Association. (2002). Optometric clinical practice guideline. Pediatric eye and vision examination. St. Louis, MO: American Optometric Association. Retrieved from www.aoa.org/documents/CPG-2.pdf
4Jacobson, L. (2013). Cerebral dysfunction in children: Should this be the central tenet for a new system of classification? Developmental Medicine & Child Neurology. Advance online publication. doi:10.1111/dmcn.12328
• 2003-Policy Statement from:
• American Academy of Pediatrics
• American Association of Certified Orthoptists
• American Association for Pediatric Ophthalmology and Strabismus
• American Academy of Ophthalmology
• Ages 3-5 years:
• Majority of optotypes on 20/40 line
• Or 2-line difference between eyes even if difference is in passing lines (i.e., 20/25 and 20/40)
• Ages 6 years and older
• Majority of optotypes on 20/30 (20/32) line
• Or 2-line difference between eyes even if difference is in passing lines (i.e., 20/20 and 20/32)
Referral Criteria
45
Eye examination in infants, children, and young adults by pediatricians. (2003). Pediatrics, 111(4), 902-907.
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
16
• American Association for Pediatric Ophthalmology and Strabismus
• Ages 3 years:
• Majority of optotypes on 20/50 line
• Ages 4 years:
• Majority of optotypes on 20/40 line
• Ages 5 years and older:
• Majority of optotypes on 20/32 (or 20/30) line
• Or 2-line difference between eyes even if difference is in passing lines (e.g., 20/25 and 20/40)
Referral Criteria
46
http://www.aapos.org/terms/conditions/131
47
Keep track of “untestable” children.
Untestable children were 2x as likely to have vision problems than those who passed vision screening.
If you have reason to believe that the child may perform better on another day, consider rescreening the child within 6 months.
Otherwise, refer untestable children for an eye examwith eye care professional skilled in treating young children and adolescents.
Vision in Preschoolers Study Group. (2007). Children unable to perform screening tests in Vision in Preschoolers Study: Proportion with ocular conditions and impact on measure of test accuracy. Investigative Ophthalmology & Visual Science, 48(1), 83-87.
American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel. (2012). Preferred Practice Pattern® Guidelines. Amblyopia. San Francisco, CA: American Academy of Ophthalmology. Retrieved from http://one.aao.org/preferred-practice-pattern/amblyopia-ppp--september-2012
• Color deficiencies cannot be corrected
• Important for teachers and parents to know
• Early childhood curriculum heavily color-coded
• Johnny may get into trouble for not sitting on the red circle in circle time because he does not see a red circle
Color Vision Deficiency Screening? Why? When?
48
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
17
49
50
Blog on Good-Lite website
https://www.good-lite.com
51
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
18
52
Stereoacuity(Muscle Balance)
PASS 2
Stereo Butterfly
53
Stereoacuity levels:480 sec arc for 3 and 4yo; + 240 sec arc for 5yo and older, blank, demo
Stereoacuity levels:• Wings (upper) = 2,000• Antenna = 1,100• Wings (lower) = 1,000• Abdomen = 600
Why Not Random Dot E?
54
• Did not go to 2nd VIP phase
• Elise Ciner, OD, stereoacuity expert with VIP:
• High untestability rate compared with Stereo Smile (PASS II)
• Concerns with 50 cm vs. 40 cm (16 in.) screening distance
• Unclear whether 550 sec arc stereo level is sensitive enough to detect visual conditions
Personal Communication 1/19/11 and 2/21/11
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
19
• Analysis of VIP Study data found:
• Testability of Stereo Smile II ages 3 to 5 years – 99%
• Preschool children “unable” to complete stereoacuity testing – 5.75 times more likely to have vision disorder –should be referred
• Preschool children who could complete demonstration card only with no measurable stereopsis – 16.2 times more likely to have a vision disorder – should be referred
Stereo Smile II
55
Ciner, E. B., Gi-shuang, Y., Kulp, M. T, Maguire, M. G., Quinn, G. E., Orel-Bixler, D., Cyert, L. A.., Moore, B., & Huang, J. for the Vision in Preschoolers (VIP) Study Group. Stereoacuity of preschool children with and without vision disorders. Optometry and Vision Science, 91(3), 351-358.
• If child strongly resists your covering one eye and does NOT resist your covering the other eye: One eye may be preferred for vision; the other eye may have amblyopia.
What to do?• Test second eye first
• Return to first eye
If this does not work?• Refer to an eye care
professional for comprehensive eye exam
56
Vision Screening Tips and Review
• Instruments = options for detecting amblyopia risk factors
Take-Home Message . . .
57
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
20
Do not fit national/international eye chart design guidelines:
Take-Home Message . . .
58
59
Take-Home Message . . .
• Line outside optotypes• 20/32 vs. 20/30• 10 feet vs. 20 feet
NO
YES
LEA Symbols
Take-Home Message:
60
HOTV
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
21
• Research supports using single, LEA Symbols optotypes surrounded with bars for children ages 3 to 5 years at 5 feet
Take-Home Message . . .
61
Vision in Preschoolers (VIP) Study Group. (2009). Findings from the Vision in Preschoolers (VIP) Study. Optometry and Vision Science, 86(6), 619-623.
62
• No pointing and holding pointer at optotype.
• If you must show child optotype to identify, point to optotype and immediately remove pointer.
63
Year of Children’s Vision
http://nationalcenter.preventblindness.org/year-childrens-vision
Archived vision screening webinars in Resources
National Center for Children’s Vision & Eye Health
http://nationalcenter.preventblindness.org/
RESOURCES:
P. Kay Nottingham Chaplin, Ed.D. kay@good‐lite.comGood‐Lite and School Health Corporation 304‐906‐2204
22
64
Identify 3 mistakes in image:1. Pointing at
optotype
2. Incorrect chart
3. Holding occluder incorrectly
65
Thank You for Your Time and Attention!
P. Kay Nottingham Chaplin, Ed.D. [email protected] 304-906-2204