Outlook 2012
-
Upload
the-institute-for-healthcare-consumerism -
Category
Documents
-
view
214 -
download
0
description
Transcript of Outlook 2012

www.theihcc.com
ISSUE || Annual 2012
The Official Magazine of
The Institute for HealthCare Consumerism
Our 2012 Experts Share Insights
Ronald E. Bachman
Bonnie BrazzellGilbert W. Lowerre
Mike La Penna
Leah Binder
Grace-Marie Turner
Mark Merritt
Melissa Van Dyke
Doug Bulleit
Karen Ignagni
Larry Boress
Dr. Wendy Lynch
Frederick D. Hunt
Jon Comola
William R. Boyles
Kevin McKechnie
Wolf Kirsten
Laura Carabello

Affordablewith a partner who doesn’t just talk lower costs, but guarantees them. Healthstat offers healthcare solutions that drive better employee health while reducing healthcare costs. Our experience, advanced technology, scalability and predictive modeling system can create an environment of wellness that works. As the leading provider of on-site primary care, health risk intervention, chronic care management and occupational medicine, Healthstat is here to change healthcare for the better. Inspire a healthy change today, by visiting healthstatinc.com.
Generated a 2:1 ROI in year 1.
Implemented Healthstat for his company last year.
Used only 2 sick days. Increased her sales by 5%.
Healthcare is
wellness that works. As the leading provider of on-site primary care, healthrisk intervention, chronic care management and occupational medicine,Healthstat is here to change healthcare for the better. Inspire a healthychange today, by visiting healthstatinc.com.
010463.6_CDHCSolutions.indd 1 2/16/12 10:26 AM

I n s I d e
www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 3
(From the publishers of CDHC Solutions, the official magazine of The Institute for HealthCare Consumerism)
The Institute for HealthCare Consumerism www.theihcc.com
8 Health Care ConsumerismThe Journey to Health Care Consumerism: The Fifth Generation Revealed
If you are a policyholder, a covered plan member, a patient, or a stakeholder in any part of the vast “health care industrial complex” you may have had the
opportunity to participate in the growing evolution of consumerism. But, have you been offered, engaged or are you benefiting from it?
By Ronald E. Bachman, Chairman, Editorial Advisory Board, The Institute for Health Care Consumerism
17 Health Care Outlook on Policy & Legislation2012: The Pivotal Year for Consumer-directed Health Care
Businesses are in a quandary. Major deadlines are approaching to comply with the federal health law. At the same time, many businesses are hoping they will be
rescued by the Supreme Court or by Congress to repeal or significantly amend the health care law.
By Grace-Marie Turner, President, Galen Institute
18 Health PlansImproving Health Care Quality and Bringing Costs Down: Encouraging Signs but Clouds on Horizon
Health care costs are crushing the economy, eating up state budgets, frustrating employers and causing consumers to make difficult kitchen table tradeoffs.
By Karen Ignagni, President, CEO, American Health Insurance Plans (AHIP)
22 Health Plans – Self-fundingBright Future for Self-funding Health Plans
After initial concern about the impact of the 2010 health reform law, it is easy to see that the opportunities and market for self-funded plans administered by TPAs is very bright.
By Frederick D. Hunt, Active Past President, Society of Professional Benefit Administrators (SPBA)
26 Account-based PlansMaelstrom: How Markets, Regulation and Litigation Affect the Outlook for HSAs
If you’ve been watching the health care debate closely, you can be forgiven for thinking that the Cold War, and all of its attendant sacrifices, was for nothing..
By Kevin McKechnie, Executive Director, American Bankers Association’s HSA Council
34 Supplemental Health BenefitsAs Employers’ Attitudes Change, Voluntary Benefits Become a Necessity in a Health Plan
The role of voluntary in employers’ benefits programs is changing, and employers’
attitudes toward voluntary have been changing along with it. Voluntary has continued to grow in sales and in account penetration, even during the recent recession.
By Gilbert W. Lowerre, CEBS, CLU, ChFC, President and Bonnie Brazzell, Vice President, Eastbridge Consulting Group
40 Pharmacy Benefit ManagementPBMs in 2012 and Beyond: Fighting for Consumers and Payers
Pharmacy benefit management (PBMs) is the one industry in America to have met the three-fold challenge posed by a generation of policymakers and consumer
advocates: to simultaneously reduce costs, expand access, and improve the quality of health benefits for the 215 million Americans with prescription drug coverage.
By Mark Merritt, President, CEO, Pharmaceutical Care Management Association (PCMA)
42 Population Health ManagementDriving Employee Engagement in Today’s Global Economy
To remain competitive in today’s global marketplace, employers are finding it necessary to invest substantial resources to improve the health—and ultimately
productivity—of their employees by offering a combination of health benefits, workplace health programs and external health management resources.
By Larry Boress, President, CEO, Midwest Business Group on Health (MBGH)
48 Health Care Consumerism Collaborative StrategiesLinking Enterprises With the Community to Enable Health and Well-being
Health is shaped by more than individual choices and medical care. There are two types of risk factors influencing individual health; those under the direct control of the individual and factors beyond the individual’s control.
By Jon Comola, Founder, WRGH.org, GKEN.org and Wolf Kirsten, President, Founder,
International Health Consulting
51 Health Care AccessCDHPs put the Consumer in the Driver’s Seat, but Employers ‘Take the Wheel’ With Workplace On-site Clinics
Employers have always been participants in the health care system as indirect purchasers of health care
benefits for their workforce and as direct beneficiaries of a healthy and productive workforce.
By Mike La Penna, National Worksite Health Center Association
57 Health Rewards & IncentivesEnergizing Workplace Wellness Programs; The Role of Incentives, Rewards and Recognition
The use of worksite wellness programs among large companies have surged in recent years, despite the economic downturn.
By Melissa Van Dyke, President, Incentive Research Foundation

I n s I d e & O n l I n e learn.COnneCt.share.
61 Health Care Consumerism Decision Support Tools
Ready, Willing, but not Quite Able: The Status of Consumer Involvement in Health Care
No longer in its infancy, health care consumerism is emerging into a stand-alone industry. We can see its expanding influence. It has its own advocacy groups
and publications, such as this one; it takes a prominent position at human resources conferences. In a sure sign of its growing presence, the medical establishment also has noticed, prompting a mix of welcoming and concerned responses.
By Dr. Wendy Lynch, Health as Human Capital Foundation
64 Consumer-designed Health TechCDH Tech Vision: Big Waves Will Drive
Health Consumers
As early as 1998 the “consumer-driven” health care movement was about new technology. Early adopters like HealthMarket, Definity and Lumenos knew having
a spending account was only one feature of the new payment and benefits model. Employees with a combined health savings account (HSA) or health reimbursement arrangement (HRA) plus advanced market information and support tools were transformed into the ultimate consumer.
By William R. Boyles, Publisher, Interpro Publications Inc.
67 Medical Tourism2012: The Rise of a Global Health Care System
In the past few years, medical travel has drawn interest from the self-funded employer community and the nation’s health plans, sparking growth and, in the wake of health care reforms, promising to transform
medical travel into a global and integrated health care system. By Laura Carabello, Chief Creative Officer, CPR Strategic
Marketing Communications
70 Health Data AnalyticsThe Importance of Reducing Early Elective Newborn Deliveries
Of the many attention-grabbing topics in health care today, maternity care remains among the most critical issues for employers and employees alike.
By Leah Binder, CEO, The Leapfrog Group
72 Consumerism Care NetworksOn Careful Networks and Support of Long-term Care
Case in point: Care. Some folks take care to provide for their future care, while others couldn’t care less—about how much, or how little, care they’ll eventually need, or who will provide it—until they need it.
By Doug Bulleit, Founder, DCS Health
PROVIDER FORECASTS
12 ConnectYourCarePutting the Consumer Truly in the Driver’s Seat
By Jamie Spriggs
14 FIS Healthcare SolutionsDriving Increased CDHC Adoption in 2012 and Beyond
By Dr. John Reynolds
20 AetnaAetna HealthFund Plans Reduce Costs and Employees Get the Care They Need
By Chris Riedl
24 UMR Healthcare ServicesDeclining Health of Workforce Top Concern for Employers
By Bart Halling
28 U.S. BankWhy the New Health Exchanges Matter: Realizing Greater Value from HDHPs and HSAs.
By Ralph L. Bernstein
30 TSYSPowering the Model: A Deep Dive into TSYS Healthcare’s Interchange Sharing Model
By Trey Jinks
32 DataPathThe Pros and Cons of Consolidation
38 TransitionsSetting Your Sights on the Aging Workforce
By Pat Huot
46 MasterCardIncentive Programs: Key to Promoting Employee Health and Lowering Health Care Costs
By Beth Griffin
54 HealthstatEmployers Hold the Key to Solving the Health Care Crisis
By John Kaegi
69 Medserv GlobalMedical Travel Options Important Addition to Cost-effective Benefit Design
By John Linss
Departments
6 From the Editor & Publisher as Consumerism transforms health Care, so does our annual Outlook Issue
75 Who’s Who Profiles
78 Resource Guide/Ad Index
4 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com


It is hard to believe this is the sixth year we have produced our annual Outlook issue. Six years ago we debuted our “Outlook 2007: A Look at the Year Ahead in Benefits &
Compensation.” The publication was much smaller and only a handful of the articles focused on health care or health care consumerism.
Fast forward to 2012, and the landscape of health and benefit management has changed, and our organization and the publication also has changed with the times.
Formerly known as CDHC Solutions, we, along with many thought leaders in the industry, have discovered health care consumerism, which has gone from a buzzword to a national megatrend, is much more than just about account-based plans.
While flexible spending accounts (FSA)s, health reimbursement arrangements (HRA)s and health savings accounts (HSA)s, paired with a high-deductible health plan (HDHP), is the engine to the health care consumerism locomotive, consumerism is so much more. Like the Nile River, health care consumerism runs wide and deep.
The same can be said for this publication, which is our largest edition to date. This year’s “HealthCare Consumerism Outlook 2012” features new categories and an all-star cast of contributors, who are considered the top thought leaders from eclectic backgrounds. However, they all have one common belief and that is the power of consumerism and empowering individuals to take charge of their health and well-being.
This year we feature 16 articles on topics such as health care consumerism, policy & legislation, health plans, self-funding, account-based plans, supplemental benefits, pharmacy benefit management, population health management, collaborative strategies in consumerism, health care access alternatives, health rewards & incentives; health decision support tools, consumer-design health technology, medical tourism, health data analytics and the emergence of care networks.
In our first year we showcased our contributors on the cover of the magazine. This year we are doing the same.
We hope you enjoy this issue and find it useful as a guide for the upcoming year, as the landscape of health care continues to shift. We also welcome you to become a member of The Institute for HealthCare Consumerism by going to www.theihcc.com. Much like the ever-changing face of health care, The Institute website also changes and is a one-stop shop for education and collaboration between your peers.
We also would like to thank our contributors for this publication. We are honored by your participation not only in this magazine but also for supporting the health care consumerism movement.
Thanks again to: Ron Bachman, Grace-Marie Turner, Karen Ignagni, Fred Hunt, Kevin McKechnie, Bonnie Brazzell, Gil Lowerre, Mark Merritt, Larry Boress, Jon Comola, Wolf Kirsten, Mike La Penna, Melissa Van Dyke, Dr. Wendy Lynch, William R. Boyles, Laura Carabello, Leah Binder and Doug Bulleit.
Sincerely,
As Consumerism Transforms Health Care, so Does our Annual Outlook Issue
todd CallahanEditorial [email protected] Field
l e t t e r eDitor & publisher
6 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
www.theihcc.comVOLUME 9 NO. 3 ANNUAL OUtLOOk 2012
Published by FieldMedia LLC292 South Main Street, Suite 400
Alpharetta, GA 30009 Tel: 404.671.9551 • Fax: 770.663.4409
CEO/ PUbLIShEr/EdItOr-IN-ChIEFDoug Field
404.671.9551 ext. 101 · [email protected]
ASSOCIAtE PUbLIShEr Brent Macy
404.671.9551 ext. 103 · [email protected]
EdItOrIAL dIrECtOrTodd Callahan
404.671.9551 ext. 105 · [email protected]
SENIOr EdItOrMavian Arocha-Rowe
404.671.9551 ext. 104 · [email protected]
ASSOCIAtE EdItOr/SOCIAL MEdIA MANAGErJonathan Field
ASSOCIAtE EdItOrMatt Macy
404.671.9551 • [email protected]
SALES ASSOCIAtESNAtIONAL ACCOUNt MANAGEr
Brent Macy 404.671.9551 ext. 103 · [email protected]
VICE PrESIdENt OF bUSINESS dEVELOPMENt Susan Yakots
404.671.9551 ext. 102 · [email protected]
bUSINESS dEVELOPMENt ASSOCIAtESDavid Cerri
404.671.9551 ext. 106 · [email protected]
ACCOUNt MANAGErJoni Lipson
800.546.3750 · [email protected]
Rogers Beasley 404.671.9551 · [email protected]
Art dIrECtOrKellie Frissell
404.671.9551 ext. 107 · [email protected]
ChAIrMAN OF CdhC SOLUtIONS EdItOrIAL AdVISOry bOArd
Ronald E. Bachman, CEO, Healthcare Visions
EdItOrIAL AdVISOry bOArd
Kim Adler, Allstate; Diana Andersen, Zions Bancorporation;
Bill Bennett; Doug Bulleit, DCS Health; Jon Comola, Wye River
Group; John Hickman, Alston+Bird LLP; Tony Holmes, Mercer
Health & Benefits; Marc Kutter, PilotHSA; Sanders McConnell,
My HSA Rewards; Roy Ramthun, HSA Consulting Services LLC;
John Young, CIGNA
WEBMASTER Kevin Carnegie
COPY WRITER + PRLana Perry
770.298.1959 · [email protected]
rEPrINtSSusan Yakots
404.671.9551 ext. 102 · [email protected]
bUSINESS MANAGErKaren Raudabaugh
404.671.9551 ext. 108 · [email protected]
CDHC Solutions™ Volume 8 Issue 2Copyright ©2012 by FieldMedia LLC. All rights reserved.
CDHC Solutions™ is a trademark of FieldMedia LLC. CDHC Solutions™ is published eight times yearly by FieldMedia LLC., 292 South Main Street, Suite 400, Alpharetta, GA 30009. Periodical postage paid at Alpharetta, GA and additional mailing offices.
TO SUBSCRIBE: Make checks and money orders payable to CDHC Solutions™ magazine 292 S. Main Street, Suite 400, Alpharetta, GA 30009 or visit www.cdhcsolutionsmag.com. Non-qualified persons may subscribe at the following rates: single copy $7.50; $75.00/yr in the U.S., $105/yr in Canada and $170/yr international. Please contact FieldMedia at 404.671.9551 or [email protected] for name/address changes.
PrINtEd IN thE U.S.A.
CDHC Solutions™ is designed to provide both accurate and authoritative information with regard to the understanding that the publisher is not engaged in rendering legal, financial or other professional service. If legal advice is required, the services of a professional adviser should be sought.
The magazine is not responsible for unsolicited manuscripts or photographs. Send letters to the editor and editorial inquiries to the above address or to [email protected]. Permission to reuse content should be sent to, [email protected].

Defined Contributions & Consumer-Driven Health Plans
Attract and Retain Better TalentEmployees are more apt to stay with a company that off ers an extensive selection of benefi ts. Don’t let rising health costs and shrinking budgets keep you from acquiring a quality work force.
Defi ned Contributions Deliver Choice and SavingsYou can determine the amount to contribute to employees’ benefi t accounts. Off er a limited number of benefi t plans for employees to choose from, or release them into the local insurance marketplace. Employees can use their “benefi t allowance” to choose the plans that best meet their needs. The balance is calculated in real time, making it easy for employees to see how their selections aff ect their paycheck.
We’re Committed to Participant EducationOur downloadable guides and online videos help participants understand their options and make the best elections for their situation.
Convenient Online & Mobile ManagementWhether you’re an employer enrolling a new hire or a participant fi ling a claim, our online portal and smartphone apps make it easy.
Call 1-800-946-6342 to get a quote today!
800-946-6342WorkableSolutions.com7120 Lake Ellenor Drive, Orlando, FL 32809
Medical FSADependent Care FSAHealth Reimbursement Arrangement (HRA)Health Savings Account (HSA)Commuter Benefi ts
Health Exchange TechnologyDefi ned ContributionBenefi t Administration OutsourcingWellness ProgramCOBRA Administration
your employee benefi ts package has never looked healthier
With Workable Solutions’
Flexible Solutions to your HR Challenges
YOUR SATISFACTION IS GUARANTEED OR WE’LL GIVE YOU A 100% REFUND.
WorkablePERFORMANCEGUARANTEE
2012 HR GOALS:
Reduce expenses
Provide quality employee benefits
Attract & retain better talent
Spend less time administering benefits

8 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
HealtH Care Consumerism
By Ronald E. Bachman FSa, maaa » Chairman Editorial advisory Board » ThE InSTITuTE oF hEalThcaRE conSumERISmprEsidEnt & CEo » hEalThcaRE vISIonS, Inc.
The fifth generation? Many of you are probably thinking, “Wow, I missed the first four generations.” If you are a policyholder, a covered plan
member, a patient, or a stakeholder in any part of the vast “health care industrial complex” you may have had the opportunity to participate in the growing evolution of consumerism. But, have you been offered, engaged or are you benefiting from it?
The most recognized forms of early generation health care consumerism are account-based plans. These are plans such as health savings accounts (HSA)s and health reimbursement arrangements (HRA)s.
A Kaiser study showed 23 percent of employers offer a plan with an HRA or an HSA. Enrollment of covered workers in account-based plans increased from 13 percent in 2010 to 17 percent in 2011, or about 1 in every 6 plan members.
But health care consumerism is more than account-based plans. Health care consumerism is about engaging employees with information and incentives
to change behaviors and improve health and health care purchasing decisions, regardless of plan design. As plans evolve, the emphasis is less on the plan design and more on how to promote, encourage, incent, and reinforce healthy behaviors and increase healthy lifestyle choices.
Health care consumerism is a market megatrend, evolving with or without government mandated health reforms. Health care consumerism is an extension of individuals taking control of their lives with personal needs and preferences.
It is a part of the same cultural movement of individuals who buy and sell goods on eBay, purchase cars on Craigslist, manage their music on iTunes, manage their stock portfolios on the Internet, pump their own gas, and bank with an ATM.
Overview of the First Four Generations of Health Care Consumerism
1. Plan Design. A high-deductible plan or an account-based plan is an example of first generation health care consumerism that focus mainly on lowering discretionary expenses (e.g. emergency room, prescription drugs).
A recent Rand study found that when people shifted into health insurance plans with deductibles of at least $1,000 per person, their health spending dropped an average of 14 percent. Health care spending also was lower among families enrolled in high-deductible plans that had health savings accounts.
The Journey to Health Care Consumerismthe Fifth Generation revealed
Health care consumerism is about
engaging employees with information and incentives to change
behaviors and improve health and health care purchasing decisions,
regardless of plan design.
BEHAVIORAL CHANGE AND COST MANAGMENT POTENTIALLow Impact High Impact
1st Generation 2nd Generation 3rd Generation 4th Generation Consumerism Consumerism Consumerism Consumerism
Focus on Focus on Integrated Personalized Discretionary Behavior Health & Health &Spending Changes Performance Health Care
Traditional Traditional Plans Plans with Consumer Information
The Evolution of Health CareFuture Generations of Health Care Consumerism

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 9
Account-based plans are a good start. However, if the goal is to change member behaviors and to engage them to make better-informed health and health care decisions, more than a new plan design is needed.
2. Behavioral Change. Many plans have evolved into second generation designs with financial incentives focusing on wellness, disease management, and health literacy. Most employers implementing second generation programs are seeking to produce measurable results of employee engagement and healthy outcomes.
A Quest Diagnostic report showed 60 percent of employees who participate in wellness programs report that the incentive is a deciding factor in their choice to participate. Incentives have been so successful in increasing participation that approximately two-thirds of the employers who invest in employee wellness use an incentive to drive employee participation. Bio-metrics (e.g. blood pressure, cholesterol, body mass index, waist size, and A1(c)) are popular as measuring standards for improved outcomes.
3. Health & Performance. Industry leaders have been promoting third generation plans that recognize healthy employees impact the corporate bottom line. Companies moving to third generation concepts recognize that health plans are the “maintenance contracts” for their human capital—their most valuable asset. These efforts add a focus on workplace health, safety and stress management. Studies show that stress impacts a company in many ways:
1. Health care – 21.5 percent of total health care costs
2. Turnover – 40 percent of the primary reasons that employees leave a company
3. Presenteeism – 50 percent of presenteeism is a function of stress
4. Disability – 33 percent of all disability and workers’ compensation costs
5. Unscheduled Sickness – 50 percent of the primary reasons that employees take unscheduled absence days
4. Personalized Health – Fourth gen-
eration health care consumerism moves from broad-based population manage-ment to very personalized health care based on genomics, predictive model-ing, wireless wellness monitoring, cul-turally sensitive disease management, outcomes, and health status. Fourth generation also expands health literacy to include personalized information therapy that is consistent and compat-ible with provider clinical therapies.
In summary, more and more benefit managers are implementing effective second generation plans. But, many also are including new products and services from third and fourth generation health care consumerism.
Creative vendors are already working with early adopters developing, testing, and imple-menting various aspects of future generation programs. Forward-thinking human resource vice presidents are becoming a more critical part of senior management by taking advantage of these new developments for increasing per-sonalized health programs, improving corpo-rate productivity, growing revenues and profits, supporting strategic workforce initiatives and lowering health care costs.
The “promises” of health care consumerism
are expanding with the continued evolution of new generation products and services. Each new generation builds on the previous ones and produces a new dimension and meaning of health care consumerism. Each evolution can be analyzed by understanding the change produced in the five building blocks. I have previously written about these first four generations. The market has continued to change. We can now begin to see the start of the newest evolution of health care consumerism.
Fifth Generation Health Care Consumerism
The fifth generation of health care consumerism is beginning to reveal itself.
Thought leaders are identifying the concepts, and creative solution providers are developing the newest generation of products and services.
An important insight to the future and fifth generation health care consumerism comes from a book called ”Blue Zones” by Dan Buettner. In “Blue Zones,” he studied cultures around the world where people are living longer (high percentage older than 100) and more productive lives (by 10 or more years). By relating the book’s findings to the evolution of health care consumerism, we can see a fifth
Major Building blocks of Consumerism
Personal Care Accounts
Wellness/Prevention Early Intervention
Disease and Case Management
Information Decision Support
Incentives & Rewards
The Promise of Demand Control & Savings
The Promise of Wellness
The Promise of Health
The Promise of Transparency
The Promise of Shared Savings
The Promises of Consumerism
It is the creative development,
efficient delivery of these elements that
will prove the success or failure of
consumerism.

10 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
HealtH Care Consumerism
Ronald E. Bachman FSa, maaa » ContinuEd from pagE 9
generation that differs from the first four by moving consumerism from:
1. Personalized (self) to Community (others)
2. Health to Productive Longevity 3. Self-help to Helping Others4. Being Served to Sharing5. Taking to Giving6. Secular to Spiritual7. Monetary to Emotional8. Head (logic) to Heart (feelings)
Community Health Care. Fifth gen-eration health care consumerism can be called Community Health Care. It is about socially engaging community, family and friends in a meaningful connected healthy lifestyle.
Social networking is growing as a driving force in many parts of our lives. A PricewaterhouseCoopers study found that near-ly a third (32 percent) of consumers have used some form of social media for health care pur-poses. The self-absorbed “Me” generation is giv-ing way to sharing communities on Facebook, LinkedIn, Plaxo and YouTube.
Personal Care Accounts: A fifth generation world moves us from financial incentives to intrinsic emotional and charitable rewards. Unlike HSAs or HRAs, fifth generation personal care accounts will not be about accumulating money. They will include accumulating credits for charitable giving, “paying it forward” accounts, and volunteer support.
Wellness: The goal of wellness or health management programs will no longer be stated as getting healthy, but to having a long and productive life. For employers, it may mean increasing support for walking compacts, group activities, and worksite yoga and meditation.
Corporate health events will include family and friends, not just employees. To promote teaming, and group support corporate health clubs will be open to dependents, friends, and neighbors. For solution providers, stress measurements will become as critical as biometric testing. Health treatments will
recognize the interaction between mind and body. New brain science discoveries will support psycho-physical initiatives in wellness and disease management programs.
Disease Management: For disease or condition management programs, the emphasis will shift from recovery to functionality. It will no longer be acceptable to simply eliminate symptoms or use traditional medical treatments to deal with chronic conditions. The ultimate measurement will be functionality.
Effective treatments will include genomic testing and interventions, predictive modeling, and proteomics. The goal will be for individuals to return to doing their jobs effectively, adequately perform the activities of daily living, continue social contacts, and participate in desired lifestyle activities.
Plans will encourage the development of disease specific teams and support groups working towards common health goals. Key personal relationships will develop as “friendship pods.”
Information: Information and decision support programs will expand to include concepts such as “sharing circles”, “mentoring groups”, and “wise-men councils.”
“Cyber-health aides” will use push tech-nology to expand and link information thera-
Personal Care Accounts
Wellness/Prevention Early Prevention
Disease and Case Management
Information Decision Support
Incentives & Rewards
The Consumerism
Grid
Initial Account Only
100% Basic Preventive Care
Information, Health Coach
Passive InfoDiscretionary
Expenses
Cash, Tickets, Trinkets
Activity & Compliance Rewards
Web-based behavior change support
programs
Compliance Awards, disease specific
allowances
Personal health mgmt, info with incentives to
access
Zero balance account activity, outcome-based
incentives
Indiv & Group Corporate Metric Rewards
Worksite wellness, clinics, safety, stress/error
reduction
Population Mgmt, Integrated Health Mgmt, Integrated Back-to-Work
Health & performance info, integrated health
work data
Non-health corporate metric driven incentives
Specialized Accts, Matching HRAs, Expanded QME
Genomics, predictive modeling push
technology
Wireless cyber support, cultural DM, Holistic
care
Arrive in time info, information therapy,
social networks
Personal development plan incentives, health
status related
1st Generation 2nd Generation 3rd Generation 4th Generation 5th Generation Consumerism Consumerism Consumerism Consumerism Consumerism
Focus on Focus on Integrated Personalized Community Discretionary Behavior Health & Health & Health &Spending Changes Performance Health Care Health Care
“Volunteer” Vessels, Pay Forward, Charitable
Giving
Natural Resource Flows, Longevity more than
Health
Functionality, Community, Faith &
Spirituality
Friendship Pools, Wisemen Sharing Circles
Psychological rewards, Recognition, Honor,
Respect, Love
In general, the theme of the fifth generation health care consumerism will be “LEARN, CONNECT
and SHARE.”

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 11
pies with clinical therapies. We will learn both from those who have experience and those cre-ative individuals who are experimenting with new ideas.
Clinical and lifestyle information will be shared across generations. Physicians and other care providers will be supplemented with not just paraprofessionals, but with practical lifestyle insights from an informed experienced trusted circle of personal advisors and mentors.
Incentives: Incentives will shift from financial to psychic rewards of recognition, honor, respect and love for others. Faith, hope and spirituality will become an important feature of these recovery, functional improvement programs, incentives and support.
Believing in something bigger than one’s self can have a strong healing and behavioral impact. Regardless of one’s personal health, assisting, helping, or teaching someone less fortunate is a powerful health producing psychic positive.
In general, the theme of the fifth genera-tion health care consumerism will be “LEARN, CONNECT and SHARE.”
It will provide collaboration between others who have ideas and knowledge of ideas,
experiences of what works, what doesn’t work, lifestyle support, along with the industry’s helpful solution providers. It is about serving others, not just helping one’s self.
A fifth generation mindset is less individually competitive and materialistic. Fifth generation participants want to be engaged in meaningful work but enjoy life, family, and contribute to the community. For older individuals it is about moving from career success to community significance. There will be more volunteering, giving, sharing of wisdom and support to others.
The above consumerism grid is the “crystal ball”—a visual framework—for understanding the future generations of health care consumerism and the five major building blocks. The overall goal of health care consumerism is to assist individuals in making more informed health and health care decisions, which will favorably impact clinical outcomes and lower the cost of health care.
Expected SavingsExpected savings will vary based upon the
effectiveness of programs supporting the health care consumerism concepts. Consumerism with
proper plan design, supported by information and incentives, has proven itself over recent years to lower costs and improve the quality of care. The American Academy of Actuaries reports that health care consumerism lowers costs in the first year by 12 to 20 percent and reduces future trend increases by 3 to 5 percent.
Other experience studies and actuarial modeling indicate that a plan can expect to save at least 5 to 8 percent annually over the next five years and enjoy a 2 percent reduction in trend each year. Actual annual savings have topped 10 percent in many cases. Savings of up to 30 percent or more are possible.
At its best, health care consumerism empowers individuals with tools that allow them to know more about their health and health care decisions. Health care consumerism puts the power of access and the selection of quality providers into the hands of individuals.
Health care consumerism may not be the silver bullet for all health care and health care problems facing the country, but it is a darn good start with great promise and with the new evolutions advancing effective solutions.
If you haven’t found your path forward, it’s time to find your place on the road of this dynamic “Journey to Health Care Consumerism.”
The American Academy of Actuaries reports that health care consumerism lowers costs in the first year by 12 to 20 percent and reduces future trend increases by 3 to 5 percent.
EffectivePrograms
Implemented
Basic
Expanded
Complete
Comprehensive(Future)
Passive
2%
3.4%
4%
5%
1st Generation
3%
5.8%
7%
10%
2nd Generation
7%
12-15.0%
17%
20%
3rd Gen & Future
10%
20.0+%
25%
30%
Potential Savings fromFull Implementation of Consumerism
Achievement of savings and improved outcomes is dependent upon both the Type and Effectiveness of
the programs implemented.
Gross* Savings as % of Total Plan Costs(Programs Applicable to All Members)
Traditional PlansConsumerism Plans
*Excludes Carry-over HRAs/HSAs and any added Administrative Costs of Specialized Programs

hEalTh caRE conSumERISm
12 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By JamIE SpRIggS
Founder and PresidentconnEcTyouRcaRE
The app for healthcare.actually there are several apps for healthcare. there
are apps to help you live a healthy life including apps to help you eat better, exercise more and quit smoking. Companies associated with healthy products like nike and Weight Watchers are increasingly providing free apps to enhance the consumer experience with their products and services. there are also apps that help you manage your financial interactions with the healthcare system. increasingly, consumers can look to mobile apps to help them manage their health and their healthcare.
Healthcare consumerism is a quietly growing movement within the us healthcare system. employers recognize that a significant amount of money spent on healthcare in the us is due to preventable behavioral decisions. Healthcare consumerism, or consumer directed healthcare, is based on the premise that if americans have more financial stake in the healthcare system then they will make better healthcare decisions. as a result, more employers and employees are selecting higher deductible health plans paired with a health account—often a Health savings account (Hsa) or a Healthcare reimbursement arrangement (Hra). While the inner workings of the accounts are different the fundamental idea of encouraging healthcare saving and consumerism via a health account is the same.
Consumerism today means mobile and apps. today’s healthcare user is more sophisticated, more
technologically savvy and a better consumer. in order to compete successfully, healthcare organizations need to provide the same level of access and convenience as retailers.
CYC mobile from ConnectYourCare is a five-star rated smartphone app that helps consumers manage their healthcare budgets and helps simplify the healthcare experience. the app enables users to view balances, claim details and upload receipts using the phone’s camera.
receiving five star reviews for this type of app is particularly significant because while most americans are happy with their primary care physician and their medical care in general, they are typically not happy with their interactions with the financial
aspect of healthcare. Filing claims is often cumbersome and frustrating. it is eye opening to see finicky customers download a healthcare app, use it on a regular basis, and report a 5-star experience.
Is this the future of healthcare? many employers and benefits providers think so. advanced
benefits providers have applications that allow customers to refill prescriptions and find pharmacies via their mobile devices. Companies that are able to effectively offer valuable, user
friendly health apps become more desirable as a healthcare partner by creating benefit solutions that fit into a busy lifestyle. the 2012 consumer demands on-the-go access to their benefits from anywhere.
the consumer market has effectively delivered apps that promote healthy living. the nike + GPs app allows users to track their runs, play ‘Power songs’ during critical moments in their workouts and even passes along words of encouragement from their Facebook friends. this popular 4+ star app is one of many apps encouraging healthy lifestyle choices.
many current and future healthcare apps promise conveniences already available in the consumer market. Consumers can already review restaurants and make reservations with apps from urban spoon, Yelp and open table. Healthcare apps promise the ability to compare healthcare providers and make an appointment with the selected provider. similarly, just as current apps help consumers track financial health, there are more and more apps promised to help track physical health.
Government regulation and market forces are driving americans to be better consumers of healthcare. the healthcare market is responding with more consumer tools including increased use of apps. Consumers can take comfort in the early apps and look forward to many innovations to come.
Jamie Spriggs is founder and president of ConnectYourCare. In 2002, Jamie set out to radically change the face of consumer-directed healthcare by providing a CDH platform that empowers businesses and employees to benefit from tax-advantaged health accounts and consumer choice. For more information about ConnectYourCare, see www.connectyourcare.com
Putting the Consumer Truly in the Driver’s Seat
Today’s healthcare user is more sophisticated, more
technologically savvy and a better consumer. In order to compete successfully, healthcare organizations
need to provide the same level of access and convenience as retailers.

ConnectYourCare has the expertise to simplify account administration, drive account enrollment and deliver greater employee satisfaction.
Don’t just wish for better service. Partner with a company that delivers it.
Account Administration Excellence
• HSA, HRA, FSA, VEBA, Retirement and Commuter benefit accounts
• Multi-account healthcare payment card
• Online participant portal and employer dashboard
• Participant communications designed to drive enrollment using proven Consumerology® principles
Service Excellence
• Industry leading customer service performance metrics
• 24x7 customer service center
• Tiered account management structure for optimal account service
• Fast and accurate claims processing
• Award-winning technology
www.connectyourcare.com

hEalTh caRE conSumERISm
patients are not accustomed to feeling empowered—but they should get used to it. the trend toward consumer-driven health care (CDHC) is placing
more information, more choices and more power in the hands of consumers than ever before. Because the benefits of CDHC require greater consumer responsibility and accountability, access to hands-on information is key. Consumers want easy-to-find answers to questions like:
• WhatplanshouldIenrollin?• What’sthedifferencebetweenahealthsavings
account (Hsa) and a health reimbursement account(HRA)?
• Havemyclaimsbeenpaid?• What’smybalance?• Whatservicesdoesmyaccountcover?• WhatincentivesdoIhavethatIshouldbeaware
of?• HowcanIsavemoneyonhealthcare?• Howmuchismyhealthcaregoingtocostme?
tools must be developed to provide answers to these and other customer queries. in response, Fis™ offers a fully integrated WealthCare Portal that gives consumers control over their wealth and health care information using a computer or mobile device.
Consumers can use the portal’s built-in decision engine, complete with worksheets, to determine which type of CDHC account is best for their circumstances. among the variables factored into the decision: the person’s anticipated health care costs, expected annual contributions from the employer and consumer, health status of all covered family members, current income and tax status and other forecasting tools.
the WealthCare Portal also contains the information needed to manage health such as lifestyle tips for managing or avoiding high blood pressure, cholesterol and other chronic conditions, interactive health risk assessments, medical appointment reminders that automatically sync to existing online calendars, prescription refill reminders and more. in addition, there is a section of the WealthCare Portal that displays investment performance for the unused funds currently held in the account.
using the same technology currently in use with financial management programs like Quicken®, the consumer can migrate this data painlessly and automatically, manage investments and pay health care bills using online bill payment.
When government-mandated administrative simplification and unified coding are in place, entering personal health records (PHrs) using the WealthCare Portal could be accomplished as easily as exporting a contact list today. mobile device-based barcode scanners will let consumers pay for and record health care purchases at retailers using CDHC account funds. account details could be displayed prominently on the WealthCare Portal Web site, so each visit to the site alerts the consumer to balance information, recent payments and other financial information.
integrating all this functionality seamlessly and making it easy to use is critically important. that’s why Fis has ensured that the WealthCare Portal is technologically sound and consumer focused. the following components are critical to the solution:
• Technologythatisreal-time,dependableandintegrated
• Respectforthedifferentcommunicationchannelsdemanded by consumers
• Capabilitythatallowsuserstomanagetheircommunication preferences
• Anadministrative and social media engine for driving the CDHC messages
nearly all the elements for a mature CDHC market are in place – including such factors as the necessary technology, regulatory incentives, consumer demand, potential cost savings and efficiencies. all that’s been missing is the ability to pull it all together—until now. With Fis’ WealthCare Portal, a solution finally exists to drive increased CDHC plan adoption and usage.
Driving Increased CDHC Adoption in 2012 and Beyond
By John REynoldS
PresidentFIS hEalThcaRE
14 Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com

The increasingly consumer-directed U.S. healthcare system is marked by rising costs, regulatory changes and chronic ineffi ciencies that plague all parties involved. FIS™ Healthcare Solutions is helping to transform the healthcare industry by facilitating the fl ow of information and funds among patients, payers, providers and fi nancial institutions.
Thanks to deep industry expertise, proven technology and extensive relationships across the fi nancial and healthcare payments spectrum, FIS can deliver a complete healthcare solution suite that seamlessly connects thousands of individuals and organizations.
As a result, healthcare providers get a single interface for streamlining HIPAA and fi nancial transactions. Payers gain a consumer-directed healthcare (CDH) administration platform to improve relationships with members and employee groups. Patients have a more seamless healthcare experience – from saving and paying for care, to making treatment decisions. And fi nancial institutions are well positioned to strengthen and grow their healthcare customer relationships.
To learn more about our complete healthcare solution suite, visit www.fi sglobal.com/healthcare.
We’re forging new connectionsamong patients, payers, providersand fi nancial institutions.
© 2012 FIS and/or its subsidiaries. All rights reserved.
fi sglobal.com
HEALTHCARE
FINANCIAL SOLUTIONS • PAYMENT SOLUTIONS • BUSINESS CONSULTING • TECHNOLOGY SERVICES
Learn more about ourhealthcare payment solutions atwww.fi sglobal.com/healthcare
FIS_Healthcare ad_OP1.indd 1 3/16/12 10:49 AM

Content and Design AHIP—All Rights Reserved: © AHIP 2012
It’s been proven over and over again that healthy employees tend to be happier and more productive. That’s why wellness programs have become so prevalent. And, that’s why we developed two convenient online courses providing you with everything you need to know to create and maintain a culture of wealth in your organization.
Wellness, Part One: Wellness, Prevention, and Value-Based CareThis course takes a practical approach to worksite wellness, guiding you through the stages of program development.
Wellness, Part Two: Combating Chronic Diseases through Workplace Wellness ProgramsThis course offers an in-depth look at chronic diseases along with the unhealthy behaviors that often precipitate illness, positioning the workplace as a venue for combating disease.
Learn. Achieve. Succeed.www.ahip.org/[email protected]
How Much Do You Know About Wellness Programs?
For details, visit www.ahip.org/courses or call the Support Team at 800.509.4422.

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 17
PoliCY & leGislation
By gRacE-maRIE TuRnER » prEsidEnt » galEn InSTITuTE
At a recent conference about the new health overhaul law in the state of Washington, one exasperated business owner asked the speaker, “Will someone please just tell me how much
this is going to cost me?”Unfortunately, like so much about the Affordable Care
Act, that question is just not answerable.Dennis Lockhart, president of the Federal Reserve
Bank of Atlanta, also reports about his conversations with business owners: “We’ve frequently heard strong comments
to the effect of ‘my company won’t hire a single additional worker until we know what health insur-ance costs are going to be.’”
Businesses are in a quandary. Major deadlines are approaching to comply with the federal health law. At the same time, many businesses are hoping they will be rescued by the Supreme Court or by Congress to repeal or significantly amend the health care law.
The U.S. Supreme Court heard an unprecedented 5 1/2 hours of argument about key
provisions of the law in late March and a decision is expected in June. But few court watchers expect the entire law to be struck down. Even if the controversial mandate that individuals must purchase government-sanctioned insurance were to be declared unconstitutional, then 90 percent of the law still would stand, including the mandate that businesses must provide expensive health insurance or pay a fine, and a plethora of new taxes on businesses, individuals and health insurance.
The future and fate of the health overhaul law likely will be a major issue in the 2012 presidential and congressional elections, with virtually every Republican pledging to repeal the law. If President Obama is re-elected, it will be almost impossible for Congress to get enough votes to repeal all or even parts of it.
So businesses wait in uncertainty and frustration. Employers are holding off on hiring new employees because of their uncertainty about the costs of the mandatory insurance or the extent of the federal fines they would have
to pay if they drop or don’t offer health coverage. This is depressing job creation and the economic recovery.
One restaurant owner said that he couldn’t afford to provide the expensive health insurance the health law requires, but even paying the annual fine of $2,000 to $3,000 per worker would consume more than the entire profit margin of his business. His business plans are paralyzed by ObamaCare.
The cost and complexity of the law may very well lead to delay in getting it implemented. The Obama administration’s problems with the law build by the day. For example, a majority of states are resisting the creation of the required health insurance exchanges. The main role of the exchanges will be to allocate federal subsidies for health insurance to eligible individuals and families, and states also must approve and regulate the health plans offering coverage in the exchanges.
If the states aren’t ready by January 2013, the federal government is required to get federal exchanges up and running by the end of next year. But there is no money to do that, and the Republican leadership in the House of Representatives will resist any efforts to provide the funding. So there is, for now, a stalemate on setting up these key agencies tasked with implementing ObamaCare.
Congress will be keeping a close watch on the expected cost of the subsidies. As they soar, Congress will have an even greater incentive to revisit and possibly delay startup of the law.
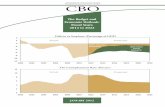
Former Director of the Congressional Budget Office Douglas Holtz-Eakin estimates that as many as 35 million more people than Congress expected will seek taxpayer-subsidized health insurance, adding $1 trillion to the $2.6 trillion 10-year cost.
One of the reasons many in the business community supported passage of the health law was because of promises it would finally get their health costs under control.
Mr. Obama repeatedly promised the American people he would reduce a typical family’s premium $2,500 a year before the end of his first term.
But costs are rising now even faster than before the law was enacted in March 2010. A Kaiser Family Foundation sur-vey found that premiums for a family policy topped $15,000 a year in 2011, increasing an average of $1,300 in the last year—three times faster than the year before. The Kaiser survey
2012: The Pivotal Year for Consumer-directed Health Care
“The cost of [account-based health plan]
coverage is considerably more affordable than either PPO/POS plan
or HMO plan coverage in 2011,” the NBGH
survey found.
continued on page 74

18 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By KaREn IgnagnI » prEsidEnt, CEo » amERIcan hEalTh InSuRancE planS
HealtH Plans
Health care costs are crushing the economy, eating up state budgets, frustrating employers and causing consumers to make difficult kitchen table tradeoffs.
In the past 50 years, health care expenditures have risen five times faster than the economy has grown.
At the federal level, health costs are the major driver of our long-term deficits. At the state level, the rising cost of Medicaid is consuming a greater portion of state budgets and causing funding for K-12 education, higher education and transportation to remain flat or decline.
The story is similar for employers. Health expenditures are driving up the costs of benefits. For employees, they are consuming an ever-larger share of tight family budgets.
The policy question is, “Has the country come to the proverbial fork in the road?” And, to paraphrase Yogi Berra, “Are we prepared to take it?”
Looking back gives us some answers, as well as cause for encouragement and caution. In recent decades, the only interruption in the cost-rising cycle occurred in the
1990s with the development of health maintenance organizations (HMOs). For a short period of time, the health cost curve trended down and purchasers and consumers saw real relief. However, with cost reduction came pushback.
The lesson we should take away from this experience should not be that managed care didn’t succeed. The key takeaway—that also needs to be confronted today—is that consumer and purchaser cost reduction was (and still is) provider revenue reduction.
It’s Not the ’90s AnymoreThe managed care backlash came, in part, from
clinicians that saw a shift in payment to structures that relied on primary care with internists and family physicians directing referrals to specialists. Many clinicians also resisted
having the need for tests and procedures reviewed by managed care plans. In addition, hospitals and physicians opposed the narrowing of networks, with calls for legislation that restricted or prevented their usage whatsoever.
As pushback grew, legislative campaigns were launched. There were accusations that prepayment created incentives to deny care and the review of tests and procedures was characterized as second-guessing. Tools needed to better coordinate care and ensure value were shelved and, predictably, costs exploded.
Skip ahead. Today, there is consensus finally that the rate of increase in health care costs and long-standing gaps in quality and safety cannot be sustained. Purchasers, consumers and government payers are rightfully demanding value for their health care investments and there are promising signs new solutions are working. While the challenges may be similar, the most promising innovations are fundamentally different than they were in years past.
Achieving Value for Consumers and Purchasers
Awareness of the scope of the problem has accelerated efforts to enable the provision of care that is safe, effective and affordable. Across the country, new payment models are being implemented. What’s different from the tools used in the ’90s is that cost and quality goals are being set and health plans, hospitals and clinicians are working together to align incentives to reward the provision of care that is high quality and cost effective.
Health plans are working with primary care physicians to offer a “medical home” to patients. The concept is to support physicians’ efforts to provide preventive care, coordination of care for multiple conditions, and services designed to maintain health and to coordinate care for those with chronic conditions.
New accountable care models span a broad spectrum of care and involve health plans and providers working together to move away from paying for each service rendered toward financial arrangements that reward performance.
A third approach involves health plans partnering with physician groups to pay for episodes of care, identify
Improving Health Care Quality and Bringing Costs Down:encouraging signs but Clouds on Horizon
Purchasers, consumers and government payers are rightfully demanding
value for their health care investments and
there are promising signs new solutions
are working.

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 19
and promote best practices, reduce treatment variation, and provide better results and value to patients.
What is strikingly different from past efforts is that these designs are emerging from partnerships among health plans, hospitals and physicians, who are working together to reform payment systems based on a shared recognition of the urgent need for practice transformation.
Improved measurement tools developed by credible, objective third parties have enabled health plans and providers to agree on best practices and steps that will demonstrate tangible improvements. Goals now relate both to the quality and cost of care; neither are reviewed in isolation. These new models empower purchasers and patients to assess value and make informed choices.
Plan and provider partnerships also are becoming longer term, creating incentives to invest in both health prevention and health improvement.
Putting Technology to WorkThe ability to set performance goals is
supported by an enhanced ability to measure, collect, aggregate and analyze information on provider performance to pinpoint gaps in care and help drive quality improvement.
Increasingly, health plans’ HIT infrastruc-ture is enabling information exchange to support doctor and patient decision-making—in real time—thereby providing access to needed infor-mation at the point of care. Whether through electronic health records, patient registries, or an alternative HIT infrastructure, better use of secure, confidential data helps identify gaps in care, supports case management of chronic conditions and creates more patient awareness.
Spurring Patient EngagementEngagement in treatment choices helps
patients make informed decisions and adhere to treatment plans and wellness programs designed for their specific conditions, such as heart disease, hypertension, obesity, asthma and diabetes.
Incentives can include waiving or reducing cost sharing for high-performing providers, particular settings of care (e.g., centers of
excellence), or certain types of medical treatments, tests or screenings that have been proven to improve health outcomes. Incentives also are available for reaching health goals, such as adherence to prescription drug regimens, completing health risk assessments, or meeting physical activity and healthy eating goals.
Other strategies we are seeing in the mar-ket include: waiving copayments for particular prescription drugs for patients who have had a myocardial infarction or for patients with asthma or diabetes to follow physician-recom-mended prescription therapies; and encourag-ing patients with diabetes to better manage their hemoglobin levels by providing blood glucose monitors.
Challenges on the Policy FrontEvery year, the U.S. Department of Health
and Human Services provides an analysis of the year-to-year drivers of health care costs.
From 2000-2006, about half the growth in health care spending was attributable to increases in the prices being charged for health care services, such as hospital care, nursing home services and prescription drugs - the other half was attributable to utilization of health care services.
Now, according to government analysts, the annual growth in health expenditures is fueled primarily by price increases. Acknowledging the role of medical prices is critically important because there is nothing that clears a crowded Washington conference room faster than a discussion about how much is being charged for medical care. When it comes to health care costs, there is no upside for politicians to even frame this challenge – unless consumers and purchasers demand action.
Indeed, very few observers have connected the dots about the effects of larger hospital systems purchasing lower cost community hospitals, hospitals buying physician practices, which is increasing the cost of procedures previously done in physician offices, and the costly boom in buildings and construction.
The policy discussion has not focused enough on how these trends are baking in revenue expectations that cannot be sustained. But these are issues that will be of growing
concern to consumers and purchasers and the role of regulation should be to ensure that markets can function effectively and that the new tools that are showing promising results are allowed to work.
Transforming our health care system is not going to be easy, but it is necessary. We know what must be done to implement a sustainable, modernized health care system that engages patients and rewards value over volume.
However the challenge for this decade is whether there will be the political will to address structural barriers to progress, fend off poten-
tial legislative campaigns to resist change and maintain the status quo and continued support of consumers and purchasers being empow-ered with great transparency, more choice and more effective care. That’s our mission in the health plan community and that’s what our new suite of products and resources are designed to achieve. As President and Chief Executive Officer of America’s Health Insurance Plans (AHIP), Karen Ignagni is the voice of health insurance plans, representing members that provide health care, long-term care, dental and disability benefits to more than 200 million Americans. Ignagni joined the organization as its chief executive in 1993. From there she led two mergers with other organizations to form AHIP in 2003, making AHIP the leading voice for the health plan community in America.
When it comes to health care costs, there is no upside for politicians to even frame this challenge—unless consumers and purchasers demand action.
Transforming our health care system is not going to be easy, but it is necessary

20 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
hEalTh planS
By chRIS RIEdl
hEad of ConsumErism and produCt innovation
aETna
Many employers are currently performing a “balancing act” as they search for the right health benefits for their organization. While
organizations are looking for health benefits plans that will help them reduce their health care costs, they also want to continue offering plans that allow their employees to access the health care services they need. although these may appear to be opposing needs, aetna HealthFund plans have a proven history of achieving both of these goals.
aetna recently announced results from the eighth annual aetna HealthFund study, which is the longest-running review of consumer-directed health plans in the industry. the results showed employers who completely replaced their traditional health benefits plans with aetna HealthFund consumer-directed plans saved more than $400 per member per year.
employers that completely transitioned to aetna HealthFund plans saw the most dramatic cost savings, but employers who simply offered aetna HealthFund plans as an option still saw significant reductions in their health care costs. the employers offering an aetna HealthFund plan option experienced savings of more than $150 per member per year for members enrolled in all health plan options, even though the other plan options offered had a similar overall plan value.
Aetna HealthFund Members Receiving Recommended Care at the Right Time
in addition to reducing health care costs, the study showed members with aetna HealthFund plans received more preventive care from their primary care physicians than members with traditional Preferred Provider organization (PPo) plans. the study also found aetna HealthFund members:
• receive screenings for cervical cancer, colorectal cancer, and prostate cancer, as well as mammograms and immunizations, at a higher rate compared to members in PPo plans.
• use the prescription drugs necessary to treat chronic conditions such as diabetes, congestive heart failure, high blood pressure and high cholesterol at similar rates as PPo members.
• select generic drugs at a higher rate than members in PPo plans, allowing members to reduce their prescription drug costs and generating up to four percent pharmacy cost savings for employers.
even though aetna HealthFund members access as much or more care than members with traditional PPo plans in many instances, the study found members with aetna HealthFund plans spent seven percent less on overall health care costs. By receiving recommended care earlier, members with aetna HealthFund plans are better able to avoid more significant and costly health care issues in the future.
Online Tools Give Employees the Information They Need
employees with aetna HealthFund plans also were more engaged health care consumers, using online tools more than twice as often as members with PPos. aetna is committed to providing members with the resources they need to better understand the quality and cost of the health care services they receive.
one popular tool is the member Payment estimator, which provides real-time out-of-pocket cost estimates for in-network and out-of-network care for more than 500 commonly used, non-emergency health care services. this level of detail—a first for health plan members—gives members a more complete picture of the costs involved and helps people better plan for and budget for health care.
the member Payment estimator received more than 67,000 hits per month in 2011, and that number jumped to more than 92,000 in January 2012. aetna members are not the only ones taking notice—the u.s. Government accountability office recently recognized the member Payment estimator as the only tool from a private health insurance company that “provides estimates of a consumer’s complete cost.”
With these types of industry-leading tools and the innovative aetna HealthFund plan designs, aetna can partner with employers to maintain their “balancing act” of controlling health care costs and encouraging employees to take a more active role in their health care.
Aetna HealthFund Plans Reduce Costs and Employees Get the Care They Need

Job # Prev. Users
Art Director Copy Writer
Acct Mgr.Proj. Manager
Studio Artist
Filename Last Modified
DeadlineClientBleedTrimLive
Cont
ent
Location Fonts & Placed Graphics
AETCORP1134A_CDHP_PS AETCORP1134A_CDHP_PS.indd 2-3-2012 2:56 PM ffernandez/ffernandez
12/20/11 Sig Gross
Aetna Betsy Guerro
8.625” x 11.125” Caroline Paik
7.875” x 10.5” Eibhin McLoughlin
7” x 9.4375” Frank Fernandez
Family StyleFoco Regular, Bold
Name Color Space Eff. Res.aetna_orange_cmyk_c.eps 42-20967427_RF_r2.psd CMYK 347 ppi PlanSponsorCDHP-orange.tif CMYK 749 ppi
Cyan Magenta Yellow Black
ffernandez (quad core)
Setu
p
110 Fith Avenue New York, N.Y. 10011
No
tes
Per
sonn
el
at
None
212-463-1036
Any questions regarding this material please call Print Production Manager Kristen Walsh
Document Path: NYC-Creative:Volumes:NYC-Creative:Studio:MECHANICALS:AETNA:2012:AETCORP1134:Plan Sponsor:A size:AETCORP1134A_CDHP_PS.indd
Inks
Quality health plans & benefitsHealthier livingFinancial well-beingIntelligent solutions
Smarter is when your employees are 2x more likely to take charge of their health.
More involved employees and savings.
1Aetna HealthFund® Eighth Annual Study Results, released December 2011. © 2012 Aetna Inc. Plans offered by Aetna Life Insurance Company and its affiliates. Health benefits and health insurance plans contain exclusions and limitations. 2012002
See the proof at smarteris.aetna.com/cdhp
• Decrease overall medical costs by 7% and prescription costs by 16%. • Proven savings of more than $400 per member per year.• 9% fewer non-routine physician visits.1
S:7”
S:9.4375”T:7.875”
T:10.5”B:8.625”
B:11.125”

22 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
selF-FunDinG
By FREdERIcK d. hunT » aCtivE past prEsidEnt » SocIETy oF pRoFESSIonal BEnEFIT admInISTRaToRS (SpBa)
I started in employee benefits in the designing discussions of the U. S. Department of Labor’s Employee Retirement Income Security Act (ERISA). Today, ERISA is a hallowed word, but during drafting
and passage, insurers, employers, unions and every one else gave it the nickname Every Ridiculous Idea Since Adam.
ERISA was designed to be, and remains, the ultimate consumer protection law. The level of disclosure and fiduciary duty were considered excessive, and it was considered the sure death of employee benefits. Of course, to the contrary, ERISA sparked phenomenal growth in employee benefit plans and the number of Americans receiving stable coverage.
The largest ERISA growth has been in self-funded health plans, and self-funding is the giant player. It is estimated nearly three-fourths of workers in health employee benefits is self-funded. Even most health coverage business of many health insurance companies and Blues is self-funded plans, with the insurer using the marketing term ASO (Administrative Services Only) to describe their self-funding services. The most important players in self-funding are third
party administrator (TPA) firms.I mention this story for two reasons. First to show
that every major law impacting employee health plans is greeted with moans for health plans. I have heard the premature death announcement dozens of times, but each time employee benefits grow and bloom.
After initial concern about the impact of the 2010 health reform law, it is easy to see that the opportunities and market for self-funded plans administered by TPAs is very bright.
How does it work? Self-funding is when an employer or benefit plan writes a customized plan of coverage, like an insurance policy, and arranges a trust or funding system for paying the claims. The next move is getting stop-loss coverage, which acts like reinsurance to protect the employer/plan from high claims from either one person or
the whole. That is a simplistic description, but it also takes precise administration and intense understanding of the various laws and regulations.
Nearly all self-funded plans use a TPA from the start. The reason is that the processing requirements and government compliance is so complex that, as judges often warn in legal matters, ”Only a fool represents himself.”
TPAs also are known for year-round service and assistance as new laws, regulations and opportunities arise. As noted earlier, some insurance companies call their administration work TPA and some call it ASO. Legally both are subject to the same requirements. (See compliance concern below.)
Why a Bright Future for Self-funding and TPAs?
(1). Insurance companies have become the whipping boy of PPACA, with fines, limitations, restrictions and other disincentives throughout the law. I predicted two years ago that insurers will depart the U.S. fully-insured market, and people thought I was crazy. However, I had the advantage of some inside information, but now, even The New York Times is writing that health insurance companies will soon be “extinct.”
Many of the punitive measures on insurers also will make life unpleasant or uncertain for employers with insured plans. There are already signs of insurers shifting from employer group customers to individual coverage.
So, self-funding is the remaining strong source of employee benefits. Also, most of the factors and new rules, which the insurance companies will find unlivable, have been the law (mostly ERISA) for self-funding for almost 30 years. So TPAs and self-funded clients flourish in the consumer-friendly environment.
(2). Employers are becoming more dedicated than ever to having their own employee benefits health plan. In the old days, employee benefits were just a bothersome “fringe benefit.” However, employers have quickly figured out that sponsoring an employee benefit plan is a business survival tool.
Why? As employers read and hear all the delays and limited
or rationed services that are a problem for all government-overseen health plans around the world, they realize that vital
Bright Future for Self-funded Health Plans
“After initial concern about the impact of the 2010 health reform law,
it is easy to see that the opportunities and
market for self-funded plans administered by
TPAs are very bright.”

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 23
employees could be off work for long periods waiting for diagnosis and care, and maybe not the best care. That is lost productivity. So, just as employers pay for instant-repair and service plans for their vital equipment and computers, they realize they need a good plan which they can customize to serve the needs of their particular workforce. This gives them more bang for the buck, and provides services quickly to get the workers back into productivity.
As employers have streamlined staffing, it makes quickly returning employees to work all the more important. The moral of the story is having a custom-designed employee health plan is a business survival tool.
An employer steering workers to individual coverage does not achieve the new needs for quick care and coverage for things that this particular workforce wants and needs most, and will probably not be reliable as a source of coverage.
(3). The government alternatives are not attractive and are apt to be shaky. There is big question whether state exchanges will function as envisioned. States are skittish and fearful exchanges could become a financial black hole for which they have the actual or political liability. Also, the exchanges depend on having insurance companies willing to offer policies in a market with expected high claims and low premiums and other micro-managing review by the states. So, states may find they have exchanges, but no insurer offering coverage to buy. To add to the problem, Congress is already diverting part of the intended subsidies to make exchanges more affordable for states, to other uses. As a result, the exchanges may be stripped-down or be rationed.
Similarly, Medicare will be going through upheaval for several years, and Medicaid will probably face big cuts in many states, which simply cannot afford such a loss in their budget. So, health reform has painted itself into what is looking like a dead end.
So, for employers, more than ever before, a self-funded health plan and good TPA firm are the best and perhaps only choice.
In the marketplace, we also are seeing first signs, and have been told to brace for a major shift over the next couple of years
as large, previously-insured employers and employers smaller than previously normal—under 100 lives—seek self-funding and solicit TPAs to create custom-designed self-funded benefit plans for them. We’re ready, including coordinating with stop-loss firms to assure that the smaller firms have the security and stability they need.
(4). Government compliance is potentially the biggest “risk” for employers and employee benefit plans, and PPACA simply expands the compliance responsibilities. I am proud to brag that SPBA member TPAs are on the cutting edge.
In fact, we play an active role as a non-partisan, non-political candid resource for government officials who seek advice and ideas from SPBA and our member TPAs about how laws and regulatory issues would work “in the real world.” Also, self-funding TPAs have long lived and are experienced on dealing with fiduciary duty, disclosure and tightly-monitored administrative cost oversight that is choking insurers.
However, there are compliance issues, which self-funding will need to face and solve. Insurance companies who do TPA duties for their self-funded clients under the term ASO, have traditionally been more closely connected to the insurance company, and tend to get their compliance information and policies from the insurance company’s legal department from lawyers trained in insurance law, which is very different from ERISA and other self-funding laws.
Not only is that like getting advice from a lawyer in France for U.S. business, but some things allowed in insurance or general business law can be prosecuted as a federal crime under ERISA, the ultimate consumer protection law. So, ASO will need to merge into the TPA world smoothly and be sure they are up to speed so inaccurate advice does not cause problems that embarrass the whole private employee benefits and health coverage system.
Variables and Probable Outcomes
Does my forecast have any variables, unknowns, or possible bumps in the road? Yes,
but they are not insurmountable, especially considering the many advantages and support the private health benefits system provides for the government and people.
The U.S. Supreme Court will mainly decide if the individual mandate is constitutional, and If the mandate, or any other part of the law, is found to be unconstitutional. Now that brings into question whether the whole law is thus tainted and unconstitutional. Unfortunately the law forgot to include “severability” wording that would say that if any part is shot down, the rest remains.
Another unknown is can Uncle Sam force states to increase their Medicaid load by about 30 percent. State budgets have been seriously dragged down by the current Medicaid drain, and an additional increase will lead to even more desperate financial problems.
The biggest long-range issue is the individual mandate. Unfortunately, it has become a political rallying point. I understand the Constitutional concerns, but if there is no mandate, there is actuarial anti-selection death spiral for all non-employer shared-risk “insurance.”
Why?Who would be crazy enough to pay
insurance premiums when they are healthy when they could simply wait and only sign up, with guaranteed acceptance, on their way to the hospital.
No joke: When this first came up, I got calls from two companies with machines that could go in ambulances or hospitals or medical offices for instant easy signing up for insurance. So “victory” in repealing the mandate would starve to death the individual insurance system, including state exchanges. So, this is a be-careful-what-you-wish-for scenario.
Even if the Supreme Court approves the individual mandate, the penalties are so low that the financial incentive to game the system will still be strong and will have an effect. So, I predict that even if the law remains untouched the total number of uninsured, when implemented, will be about the same as the much-bemoaned level during the prior decades. To read this article in its entirety, please visit www.theihcc.com.

24 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By BaRT hallIng
Vice President, consumer solutionsumR
SElF-FundIng
Bart Halling is vice president of consumer solutions at umr, the nations largest third party administrator (tPa). He and his team focus on creating and implementing
“activation strategies” for the 2.3-plus million members currently participating in self-funded plans across umr’s book of business.
employer clients at umr span a wide range of industries from manufacturing and hospital systems to services firms and public sector entities and range in size from just under 200 members to more than 100,000-plus members. umr offers a broad span of consumerism strategies aimed at creating positive behavior change and using concepts within value-based benefit designs (VBBD) to create momentum shift within an employee population. the following are excerpts from an interview with Halling regarding the direction of the industry as it relates to incentive programs.
Health care has remained at the top of the list for concerns that our country is currently struggling with. As you work with employers, what is one of their most common concerns?Halling: First, i agree health care, and more broadly, the health status of our nation’s workforce is a top concern for employers. many of us in the industry are in active debates about which wellness, disease management, incentive or coaching program might be most effective in addressing these issues. almost all of us agree healthier workers are good for business. so, i think the no. 1 concern we continue to see from clients is a declining aggregate health and the unavoidable impact it has on an organization’s success.
Does this represent a major shift of perspective for employers? For years employers seem to have been most concerned about delivering benefit programs to attract and retain strong candidates and workers. Halling: i wouldn’t call it a radical shift, as employers have always had concern for the health of their workforce, but the undeniable fact that poor and declining health has a negative effect on almost all metrics of cost attached to an employee has forced new perspective. major employers across the country are seeing results from group studies that show even simple biometric markers, like Body mass index (Bmi) as predictors of higher employee costs related to medical claims, short-term disability, workers compensation and absences/presenteeism. employers across the country have had their hands forced to become more directly involved in the health of their team members. that can be uncomfortable and demands a new set of strategies and tactics.
What about the employees? Are they feeling financial heat from the trends in declining health or have they been insulated from the problem by their employer-funded health plans?Halling: Clearly, the recent birth (or rebirth depending on your perspective) of consumerism in health care has created more visibility of the financial impact of poor health. expanding “wallet share” tactics on health care costs for plan participants have created a drive toward more consumeristic behaviors. Households have been forced to deal with an almost three-fold increase in costs in the last 12 years, growing from an average cost for families of $5,791 (1999) to more than $15,073 (2011)*. unfortunately few families have seen a corresponding increase in disposable income to make up the difference.
So, with all of that “positive” news on costs hitting employers straight on, how are they coping? What strategies are most prevalent?Halling: many employers are anxious to identify behaviors to encourage and implement incentive programs to motivate change. one caution: understand the powerful impact of culture on an incentive program’s potential. We continually see evidence the old axiom “culture trumps everything” is true. employers who do not address gaps between their culture and their health strategies, will struggle to reach their program’s potential. that said, many employers are moving aggressively from reward programs, asking only for participation, to requiring action, results and improvement in health metrics. Focus has aligned with driving employee engagement and creating tangible results. many plan sponsors also are raising the bar on health metric targets every year.
How do you see participants reacting now and in the future to these employer incentive programs?Halling: reaction ranges from full engagement to suspicious curiosity as to “why my employer should care what i eat and how much i exercise.” this is a tough spectrum for employers to navigate. those who are able to get buy-in around the value to the participant and become healthier, will be the most successful. We are at the crossroads of a tremendous opportunity to supercharge the nation’s workforce, and employers who understand the health and wealth landscape will gain the greatest advantage and find corporate value they did not realize was within their reach.
*Kaiser/hrEt survey of Employer sponsored health Benefits (1999-2011).
Declining Health of Workforce Top Concern for Employers

(or try to)
Those who can, do. Those who can’t, imitate.
Self-funded benefits administration is not simple and it sure doesn’t seem easy. So enlist the expertise of UMR, a UnitedHealthcare company, to get the flexibility, insight and expertise you expect from a third-party administrator plus the scale and reach of a Fortune 50 company.
Only UMR can give you the significant network discounts of UnitedHealthcare.
Only UMR can give you a totally integrated approach to benefits administration or easily plug and play with your preferred vendors.
Only UMR can easily respond to health care mandates, regulations and market changes.
Making the simple complicated is commonplace. Making the complicated simple…that’s UMR.Find out more at www.umr.com.

26 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By KEvIn mcKEchnIE » ExECutivE dirECtor » amERIcan BanKERS aSSocIaTIon’S hSa councIl
aCCount-BaseD HealtH Plans
If you’ve been watching the health care debate closely, you can be forgiven for thinking the Cold War, and all of its attendant sacrifices, was for nothing.Fighting, as this nation did, to thwart the Soviets—who
would nationalize private property, invalidate the rule of law and destroy individual liberty—can only be considered worthwhile if, in victory, we applied to ourselves the lessons we spent so much blood and treasure teaching others.
In recent testimony before Congress, Health and Human Services (HHS) Secretary Kathleen Sebelius said the “private [health insurance] market is in a death spiral.” Here is evidence that we have failed to learn these lessons.
The Orwellian spectacle of the Administration official most responsible for putting the private market in such jeopardy going before Congress to lament its demise is a chilling message for America.
It’s like watching the victim of a crime being comforted by the perpetrator.
The Affordable Care Act’s (ACA) mandates onerous penalties and the capricious manner in which they are enforced are the reasons health insurance is so expensive.
And, the situation is only going to get worse. The Secretary’s broad powers
allow her to force some groups to comply but to exempt others from the Act’s many requirements. The Secretary doesn’t need to give any reasons for these choices.
Favoritism doesn’t even begin to describe this practice.
To favoritism we add compul-sion; in 2014 when every American must buy health insurance or face a penalty, the liberty to use your own money as you see fit will be eroded, perhaps permanently. In and of itself, reduction in personal liberty
is anathema to Americans but more disturbing is duplicity; the entire debate over health care reform was launched with a promise - “if you like your plan you can keep it”.
It is now abundantly clear this was nothing more than a
bold-faced lie.It also was a lie complete with sticker shock; the
Congressional Budget Office (CBO) has provided a new estimate of the President’s health care law. It is now expected to cost twice the 2009 estimate, more than $1.7 Trillion over 10 years.
All this bad news has been met with a voracious market. Employer adoption of consumer-directed health plans (CDHP)s generally, but health savings accounts (HSA)s, in particular, are not just growing but growing faster than any other product. Choose your metric: account balances, covered lives or plan participants. By every measure, HSAs are the growth opportunity in the employee benefits industry as companies claw back savings through conversion.
We know this because HSA Council members report record growth for the 2011 enrollment season: “Thirty-four percent growth in accounts”; “36 percent growth in HSA balances.” These are the unassailable signs that the switch from traditional plans to HSA plans is in full swing.
But, even with record adoption data in the employer-sponsored segment, the trend hasn’t extended into fully insured plans. To be clear, HSA-qualified plans are on the rise in all market segments but fully insured plans are under assault by the ACA’s major regulations, the medical loss ratio (MLR) and actuarial value (AV) regulations.
This is not unexpected; the majority of the ACA’s painful changes are visited upon fully insured small group and individual plans, the very plans expected to be offered in the ACA’s state exchanges.
The HSA Council is using every weapon at hand to convince HHS to amend its regulations, but as of this writing, the tacit assurances we have received that our suggestions will be adopted have yet to be found in an amended regulation.
Accordingly, the viability of HSA-qualified plans in the exchanges is in question. Consider the conclusions Milliman Consulting reached in its report to the HSA Council on the effects of the MLR regulation on HSAs:
The medical loss ratio formula doesn’t take into account contributions to HSAs. Many high-deductible health plans are accompanied by an HSA, which covers much of the first-dollar costs
Maelstrom: How Markets, Regulation and Litigation Affect the Outlook for HSAs
“The Affordable Care Act’s (ACA) mandates onerous penalties and
the capricious manner in which they are enforced
are the reasons health insurance is so
expensive.”

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 27
before the plan’s deductible is reached. HSA contributions are currently not reflected in the medical loss ratio calculations.
High-deductible health plans may not be able to raise rates fast enough to keep up with rising costs. High-deductible health plans will require larger annual rate increases than typical medical plans because medical inflation will have a greater impact on claim levels than plans with lower deductibles.
High-deductible health plans have fewer premium dollars to cover their fixed expenses. Every plan has fixed expenses that it covers with premiums. Since high-deductible health plans have lower premiums than other plans, a greater percentage of the premium must be used to pay these fixed expenses.
For example, $400 of fixed expenses represents 40 percent of a $1,000 premium, but only 20 percent of a $2,000 premium and just 8 percent of a $5,000 premium. Therefore, it is harder for a lower premium plan to keep its non-claim expenses below 20 percent of its adjusted premiums as the medical loss ratio rule requires.
High-deductible health plans
have less predictable claims experience that could increase the risk of paying rebates. High-deductible insurance plans pay fewer claims than plans with low deductibles. But when high-deductible health plans pay claims, the claim dollar amounts tend to be larger. This lower-frequency/high-payment creates less actuarial predictability, which can result in high claims in one year and low claims in another. If the plan has low claims, it may not meet the 80 percent medical loss ratio and be required to pay rebates.
If you assume HHS sees a role for HSAs in the exchanges, it is curious indeed that they
issued a rule so injurious to them. Perhaps it’s our fault; one strategic flaw in our thinking has always been that the administration would embrace HSAs simply because the order to buy health insurance in 2014 presupposes there are affordable plans in the exchanges in the first place. HSAs are invariably the most affordable plans in the market.
Instead we are seeing a confrontational body of regulation, much more in tune with the ideological objections of congressional democrats than the practical goals of administration lawyers. The ideologues are clearly winning this important policy debate.
More evidence of this dynamic is found in the recently proposed AV regulation. The AV regulation is the methodology HHS will use to determine if a plan is eligible to be sold in the exchanges and at what metal level. Where the MLR is punitive, the AV is nebulous. Supposedly providing guidance as to how HSAs will be treated under their rule, HHS says:
“because generally only a portion of an HSA is used in a year for health services, HSA contributions would be adjusted so that the employer receives the same credit for HSA contributions in the numerator of the AV calculation as it would receive for the same amount of first-dollar insurance coverage.”
Got that?As we parse the meaning of HHS guidance,
it appears the proposed rule penalizes HSA owners by creating perverse incentives to spend more money per medical good or service. If HSA owners spend “only a portion” of their dollars on health services, as HHS assumes, then they only get credit for what is spent, not what is saved.
We will be making HHS aware that HSA owners have lower utilization rates because of the simple fact they are spending their own money, so they spend it more prudently. Accordingly, one conclusion we have reached about this rule is it appears to penalize prudent spending.
More importantly, because the AV rule does not take into account the dollars an individual contributes to their account or all the
dollars an employer contributes, if the employee doesn’t use it all, the plan could have an AV which disqualifies it from being offered in the exchanges.
Alternatively, we are encouraging HHS to adopt the methodology both the CBO and the American Academy of Actuaries (AAA) established in their commentary about how AV should be calculated for high deductible plans.
According to CBO:
“the actuarial value of consumer-directed plans would include the expected value of any contributions that an insurer or employer sponsoring the plan would make to an enrollee’s account—so that contribution could be set to make the overall actuarial value of the consumer-directed plan equal to the value of a conventional health plan.”
CBO’s approach recognizes the entire value of contributions made to the account
The American Academy of Actuaries makes another point:
“If the contributions are automatic, it may be appropriate to simply add the value of the contribution to the actuarial value of the high-deductible health plan.”
Many government-sponsored plans use a “premium pass through” architecture where the monthly premium includes a fixed contribution to the HSA. HHS’ proposed AV rule doesn’t even recognize this architecture—ironic since many HHS employees undoubtedly have HSAs funded in exactly this manner. The proposed rule ignores any automatic contribution to the account made by individuals or small business, which necessarily lowers the AV of the plan.
Of course, those disaffected by these rules also are doubling down on the chances the Supreme Court will declare the ACA unconstitutional. To read this article in its entirety, please visit www.theihcc.com.

28 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By Ralph BERnSTEIn
senior Vice President, emerGinG strateGies & innoVation u.S. BanK, coRpoRaTE paymEnT SySTEmS
January 1, 2014 is right around the corner, one of the key dates in the affordable Care act. this is when the new health insurance exchanges
will launch, giving access and relief to many small business owners and potentially millions of uninsured individuals.
there’s still some uncertainty about what exactly the exchanges will include, but it’s likely high-deductible health plans (HDHPs) will play pivotal roles. one of the big challenges to their success will be perception. Consumer-directed health care terminology scares people. they hear “high-deductible health plan” and think “more cost” instead of “more savings.” the reality is, most people never approach their deductible, even when you factor in prescriptions. so by choosing an HDHP, the “low premium health plan,” they’re trading a higher deductible they’re unlikely to meet anyway for signifi cantly lower premium expenses. that’s great for everyone—employer and employee.
But there’s a “gotcha” among the good news—the gap between what the insurance company will cover and what has to be paid out of pocket. that rabbit hole creates anxiety among potential enrollees and makes a strong case for a health savings account (Hsa). it’s the bridge; the medical safety net. ideally, individuals would open Hsas in their 20s, so when they get to an age when they really need the extra help, a sizable nest egg will be there; but any consumer can benefi t from setting aside tax-advantaged dollars for health care expenses and retirement. this will be especially true for those who choose to enroll in an Hsa as a complement to an HDHP within the new exchanges.
Butthenwhat?WetendtothinkofHSAsassimple bank accounts, but as the exchanges mature, and as we continue to think about how to pay for health care and save money, new applications will emerge that will make benefi t savings and spending accounts even more attractive:
• Asadditionstodefinedcontributionprograms.in these programs, employees are given dollars to go out and buy the health coverage they want. Participants will naturally gravitate to the most affordable, highest-value packages: HDHPs bundled with Hsas.
• Aspartofhealthy-livingincentiveprograms.Join a gym or attend smoking cessation classes?DollarscanbedepositedintoyourHsa as a reward for “good” behavior.
• Assupplementstoanyhealthinsuranceplan.today, Hsas are tied to HDHPs, but that limits participation and keeps consumers from making good choices. if Hsas and HDHPs were decoupled, something that i’ve written about before, everyone could take advantage of the tax benefi ts. this would mean a lesser burden on the health care system overall and lower costs for everyone.
even if you are not a small employer or do not have uninsured employees right now, you need to watch how the exchanges develop. the satellite benefi ts—the greater reliance on CDHC programs, the expanded value of Hsas, and the improved understanding of patient responsibility—will affect you today and how you plan the benefi ts you offer. You’ll see how to protect the health of your employees, and your bottom line.
U.S. BancorpU.S. Bancorp Center, 800 Nicollet MallMinneapolis, MN 55402usbankhealthcare@usbank.com800.334.9207www.healthcare.usbank.com
Why the New Health Exchanges Matter: Realizing Greater Value from HDHPs and HSAs
accounT-BaSEd hEalTh planS

Deposit products offered through U.S. Bank, NA.
Member FDIC (3/12)CDHCS312
Wherever You Go, We’re There.
Simple. Convenient. Always Accessible. When choosing an HSA, FSA or HRA, make sure it offers the convenience, accessibility, and flexibility you expect in today’s fully connected, on-the-go world.
To download U.S. Bank Healthcare Mobile, simply visit the Android™ Market or iTunes™ App Store. To scan the code, download the free QR reader app for your Smartphone.
Our Healthcare Mobile app for both Apple™ and Android™ devices makes it easy for you to check your benefit-spending account balances, view transactions and claim details, and instantly make smart decisions about your healthcare dollars – no matter where you are. And when the app is paired with our best-in-class account-management site, expert customer service, and convenient payment card, you get a great solution that not only supports a healthier workforce but yields real cost benefits. Anywhere. Anytime. Any day.
For more information on adding a spending account to your benefits program, call us at 800-334-9207.
www.healthcare.usbank.com

30 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
accounT-BaSEd hEalTh planS
Health Care Plan Administration — The History of Paper vs. Plastic
For decades, gaining access to a Flexible spending account (Fsa) was laborious and difficult, at best. then in the early 2000s, debit cards were introduced and gave participants an easy-to-use solution for spending their Fsa dollars. the efficiencies gained with the simple swipe of plastic were immeasurable for both cardholders and tPas: fewer paper claims; fewer receipts and eoBs to retain; and fewer calls into the call center. no other enhancement had a single greater impact. adoption was slow in the early years, but as anti-fraud measures were applied to the cards (e.g. iias), adoption has grown significantly in the last five years. even still, less than 40 percentofFSAandHRAtransactionsoccurbyusingacard.Why?
Interchange Sharing and Other Advantages of a TSYS Card-Enabled Plan
Historically, the administrative gains have largely been offset by the cost of the card, or by integration difficulties incorporating the card. these obstacles have generated card ambivalence among tPas and employers and challenge the value proposition of switching from the old faithful paper-claims model. tsYs has responded by bringing together an industry leading, healthcare card-centric payment processing system with an interchange sharing philosophy, providing a clear advantage for every stakeholder.
Third Party AdministrationFor tPas, it is all about increased revenues. tsYs Healthcare’s
offering provides tPas with a share of the interchange revenue from every card swipe. through tsYs’ flexible management of plan options, a tPa is presented with unparalleled card opportunities. tsYs Healthcare offers a variety of multi-purse solutions (Hsa/Fsa/Hra, Dependent Care, transportation, line of Credit) on the same card. advanced authorization logic enables carding of complex Hra designs, and substantiation can be set in a way that balances the tPa’s internal support requirements and card usability. in addition, more transactions are auto-substantiated through iias and flexible plan design options like claims feed integration and recurring transactions functionality.
Historical models in which card middlemen kept all the interchange and tacked on a card administration fee cannot
compete with tsYs Healthcare’s model. With us, more card-based spending means lower administrative costs and higher revenue for tPas through interchange sharing.
EmployersFor employers, it is all about increased adoption. For our
customer’s customers, a tsYs Healthcare card-enabled program means both a cost-effective and highly customizable plan, which facilitates the secure disbursement of funds that is easy to deploy to employees. the short implementation cycle and unequaled, tsYs-owned card delivery minimizes disruptions to the employer and increases employee adoption. no longer just an efficiency and payment enabler, the card can also be used to drive a participant’s healthy behavior through messaging and rewards.
Plan Participant
For plan participants, it is all about convenience. tsYs Healthcare’s “People-Centered Payments” approach makes a participant’s qualified medical transactions easy and secure. information, messaging and statements all enable the participant to proactively manage their tax-advantaged payroll deductions and receive the services that they require. all of this is aimed at driving card utilization by the participant, resulting in increased revenue for the tPa, as well as participant satisfaction and overall convenience with less “pay-and-chase” overhead.
Deployment of a card to an existing Fsa, Hra, Hsa and even transportation plan is easy, and tsYs Healthcare provides end-to-end support along with value-added services like a dispute management call center, statements and on-demand collateral production.
Our Philosophy — People-Centered Payments with TSYS Healthcare
Sowhatdoes“People-CenteredPayments”reallymean?it means that tsYs Healthcare commits to and takes personal responsibility for meeting your needs and the needs of your business. We will leverage our team’s expertise in the healthcare and payments industry and enhance our relationship with you to anticipate your needs, proactively solve problems and create solutions to grow your business. and, our team members will never lose sight of the fact that behind every payment transaction is a person or business depending on us to get it right.
Powering the Model: A Deep Dive into TSYS Healthcare’s Interchange Sharing Model
© 2012 Total System Services, Inc.® All rights reserved worldwide.
TSYS® is a federally registered service mark of Total System Services, Inc.
A winning combinationOur unique experience in both the healthcare and payment services industries means unmatched expertise and reliability. Known for our elite levels of customer service and a long-term commitment to the industry, TSYS Healthcare® is focused on lasting relationships and people-centered paymentsSM.
Integrity | Relationships | Excellence | Innovation | Growth
Learn more at www.tsyshealthcare.com or call us at +1.706.649.5080
Get to know us. [email protected]
By TREy JInKS
GrouP executiVe TSyS hEalThcaRE

© 2012 Total System Services, Inc.® All rights reserved worldwide.
TSYS® is a federally registered service mark of Total System Services, Inc.
A winning combinationOur unique experience in both the healthcare and payment services industries means unmatched expertise and reliability. Known for our elite levels of customer service and a long-term commitment to the industry, TSYS Healthcare® is focused on lasting relationships and people-centered paymentsSM.
Integrity | Relationships | Excellence | Innovation | Growth
Learn more at www.tsyshealthcare.com or call us at +1.706.649.5080
Get to know us. [email protected]

32 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
As the adoption of consumer-driven health has grown, so too has the technology to administer those plans. What was once a relatively small but
diverse group of consumer-driven technology providers has now been inundated by players from every level of the corporate hierarchy.
For the most part, this is a positive trend. large insurance and technology companies have provided the wealth necessary to increase education and awareness of consumer-driven principles. economies of scale have been produced, utilizing integrated administrative platforms, consumer education tools, mobile apps and payment cards, making the implementation of these accounts not only less expensive, but easier to use.
But as is the case when any industry attracts the attention of those who were not in the first wave of innovation, there are secondary consequences, which are not always good for those on the lower end of the corporate food chain.
Is it Really ‘Just Business?’
By definition, efficiency is produced by systematizing the delivery and operation of the functions of an industry in alignment with the evolving best practices of delivering those goods or services. the problem comes when what is “best” is more related to profit than process. the mentality of a huge corporation with widely divergent business units is very different from the small to mid-sized businesses that fuel most of the employment in this country.
speaking specifically to the consumer-driven technology market, the goals of the corporate parent often supersede the needs of subsidiary companies, and those smaller business units often come up short on investment, or are eliminated entirely if the goals of the parent change, without regard to the clients served by that unit. to a huge
corporation, “it’s just business.” to a small business, it’s personal. everything is personal to a small business.
And Then There’s Venture Capitalanother trend growing in the consumer-driven
technology arena is the influx of venture capital. most of the original companies that created systems for administering consumer-driven plans have either been
sold to larger entities, or have been bought by venture capital groups. those bought have broadened their appeal with increased marketing and sales funds, However, the product itself has not necessarily improved, and the internal focus changes from pleasing current clients to one of preparing for a sale.
Before venture capital, there is a true partnership between the founding company and its clients. afterwards, it’s more of a marriage of convenience hinged on the goals of the investors, and when
the company is eventually sold, the well-being of existing clients will not be the focus of the negotiation.
A Word to the Wise
economies of scale produced by those focused solely on the bottom line do not always produce the best product for the end user. Brokers and administrators seeking technology vendors in the current consumer-driven technology market would be wise to fully understand the ownership and long-term goals of potential partners before entering into a relationship.
DataPath, Inc. is a management-owned, privately-held company that has been focused on creating solutions for administering employee benefit plans since 1984 by entering into mutually-beneficial, long-term relationships, and by understanding the needs of our partners. Our full-spectrum product line includes solutions for administering FSAs, HSAs, HRAs, Transit, POPs, COBRA, and Retiree Billing, with 24/7 online access for Administrators, Employers, and Employees, all integrated with the mySourceCard® MasterCard Debit Card. For more information, visit www.dpath.com.
The Pros and Cons of Consolidation
Brokers and administrators seeking technology vendors
in the current consumer-driven technology market
would be wise to fully understand the ownership
and long-term goals of potential partners before
entering into a relationship.
accounT-BaSEd hEalTh planS

800.633.3841 • www.dpath.com • [email protected]
FSA, HSA, HRA, Transit, COBRA, Retiree Billing, and more. Online and fully integrated with the mySourceCard® Debit Card.
You started your own business because you wanted
to be your own boss — to control how you grew,
to develop your own relationships, to do things better.
Now, everything you have is tied up in that business.
Employees count on you. Clients depend on you.
For you, it’s more than business.
It’s personal.DataPath understands.
We’ve been focused on personal relationships
and doing things better for 28 years. We understand your
business is more than a revenue stream — it’s your life’s work.
Creating the best administrative solutions for you is ours.
Call today and let’s work together.

34 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By gIlBERT W. loWERRE, cEBS, clu, chFc » prEsidEnt » EaSTBRIdgE conSulTIng gRoupBy BonnIE BRaZZEll » viCE prEsidEnt » EaSTBRIdgE conSulTIng gRoup
VoluntarY/suPPlemental BeneFits
The role of voluntary in employers’ benefi ts programs is changing, and employers’ attitudes toward voluntary have been changing along with it. Voluntary has continued to grow in sales
and in account penetration, even during the recent recession. Driven by concerns about health care reform and
continued benefi t cost shifting, employers are turning more frequently to voluntary solutions, adding more and more voluntary coverages to their benefi ts portfolio.
Chart 1 shows the number of voluntary coverages offered by employers, broken down by account size.
Voluntary is clearly a popular option among all size accounts. While the largest employers are more likely
to offer voluntary products, a majority of companies in the smallest category have at least one voluntary coverage. And those that offer voluntary appear to value the advantages voluntary products bring. In all size groups, more employers offer three or more voluntary products than offer one
or two products. Voluntary products are clearly satisfying the needs of those that offer them.
Fifty-nine percent of new voluntary sales are new
coverages offered in addition to the core benefi t program. Historically, many employers added voluntary products because employees requested them and since the employees were paying for them, the attitude was often “if they want them, why not?” Employers often didn’t really consider these additional coverages as a part of their benefi t plan. That attitude is disappearing.
The other forty-one percent of new voluntary sales are “Takeovers,” coverages that are replacing prior voluntary or employer-paid products. This escalating trend indicates employers are becoming more discerning about voluntary
program quality and are using voluntary as a tool in shifting benefi t costs. In other words, voluntary has become an important part of the basic benefi t plan the employer offers.
As a result, the selection of voluntary programs has become an integral part of the overall benefi ts strategy, dually responding to employee needs and wants, while also furthering the strategic goals set for the benefi t program. Employers, understandably, are becoming more involved in the selection and implementation of their expanding portfolio of voluntary benefi ts.
The starting point is to select product classes that fi t the strategy and the needs/wants of the employee population. Today, the answer is more likely to include multiple products, as can be seen in Chart 2.
As Employers’ Attitudes Change, Voluntary Benefi ts Become a Necessity in a Health Plan
Voluntary products are clearly satisfying
the needs of those that offer them.
# of Voluntary Benefits Offered
40%35%30%25%20%15%10%
5%0%
40%35%30%25%20%15%10%
5%0%
40%35%30%25%20%15%10%
5%0%
20%15%10%
5%0%
20%15%10%
5%0%
1
11%
4%
25%19%
15%
33%
17%12%
38%
17%15%
8%
2 3-5 6+ 1 2 3-5 6+ 1 2 3-5 6+
Medium Accounts(101-2,000 employees)
Small Accounts(10-100 employees)
Large Accounts(2,000+ employees)
Chart 1:

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 35
Chart 2:
Once employers, usually with the help of their broker or consultant, decide on the basic product strategy, carriers need to be selected. It is not uncommon for programs with multiple products to include multiple carriers.
Most brokers believe that no one company can be best in every product category. The good news is more insurance companies now offer voluntary coverages, and those who have been in the market have been investing to upgrade their voluntary capabilities and offerings.
Selecting a carrier involves comparisons on a variety of criteria, often requiring the expert input of the employer’s benefi t advisor.
Employers reported they examine a variety of important issues when selecting carriers, as shown in Chart 3. While, in the
past, many employers selected carriers based on the enrollment process they would use, today more employers are rightly considering enrollment after selecting the carrier they prefer.
Instead, price (even though employees are paying the premium), reputation, and administrative/technical support, ratings, and “best of breed” product availability are seen as more important. This indicates a growing voluntary maturity and an appreciation for the strategic importance of carrier selection.
Now, employers should turn to the question of enrollment process. In the past, brokers and carriers had proprietary or preferred enrollment processes, and built their sales language to lead their clients to the preferred solution. Again, the world has changed. Selecting a methodology involves consideration of a range of issues.
The makeup of the account,
distribution of employees, number of locations, culture, and employer preferences all are important considerations.
In addition, employers need to consider the types of products that are to be enrolled. Some products require relatively little education and support while others require extensive education and interaction.
Some methods are less expensive than others. And if the account is enrolling products from multiple carriers, an open enrollment system is required. Also, it’s important to consider whether this will be a voluntary-only enrollment or also will be used to enroll core or
Employers often didn’t really consider these additional coverages as a part of their benefi t plan. That attitude is disappearing.
Term Life
STD
All Hospital/Supplemental Medical
Accident
Dental
Cancer
UL/WL
LTD
Vision
Critical Illness
LTC
AD&D
Other
17.8%
14.8%
13.0%
12.4%
9.6%
7.7%
7.6%
5.1%
4.1%
3.8%
2.5%
1.2%
0.4%
Line of BusinessPercent of Sales
Sales by Product
STD: Short Term Disability UL/WL: Universal Life/Whole LifeLTD: Long Term Disability LTC: Long Term Care
AD&D: Accidental Death and Disability
0% 20% 40% 60% 80% 100%
Price
Reputation
Admin/Tech Support
Ratings
Best of breed products
Range of products
Prior experience
Personalizedenrollment materials
Carrier will enroll
Single bill for voluntary
Broker recommendationSiingle bill for EEand ER paid plans
Advertising
87%
77%
73%
67%
63%
60%
54%
47%
52%
41%
48%
42%
14% 2009
Importance in Choosing a CarrierPercent Rating as 4 or 5
(Scale: 1 to 5, with 5 being “Very Important”)
Price 87%
77%Reputation 77%77%
73%
Price
Reputation 77%77%
73%
67%
Admin/Tech Support
Reputation
Admin/Tech Support 73%
67%
63%
Ratings
Admin/Tech Support
Ratings
73%
67%
63%
60%
Best of breed products
Ratings
Best of breed products 63%
60%
54%54%
Range of products
Best of breed products
Range of products
63%
60%
54%
47%
Prior experience
Range of products
Prior experience 54%
47%Personalizedenrollment materials
Prior experience
Personalized 47%47%
52%
41%
Carrier will enrollenrollment materials
Carrier will enroll
47%
Single bill for voluntary 41%
Carrier will enroll
Single bill for voluntary 41%
Siingle bill for EEand ER paid plansSiingle bill for EEand ER paid plansSiingle bill for EE 42%
14%Advertising 14%14%and ER paid plans
Advertising 14%14%
Broker recommendation
41%
48%
42%
Single bill for voluntary
Broker recommendation
41%
Siingle bill for EE 42%
Chart 3:
continued on page 37

@AIGBenefits +AIG Benefit SolutionsAIG Benefit Solutions AIGBenefitSolutions

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 37
VoluntarY/suPPlemental BeneFits
other employer-paid benefi ts. Working trough these issues with their brokers, employers come to a wide range of conclusions, meaning that fl exibility and openness are often key attributes of the selected process.
Most employers have come to recognize this and are open to selecting the best methodology, regardless of how they’ve enrolled in the past or personal preferences.
Employers can choose between third-party systems, broker-owned systems or carrier systems. All have become more fl exible and diverse over the years. For example, Chart 4 shows the enrollment methodologies currently offered by voluntary carriers.
In addition, employers are increasingly interested in value-added, supporting services, which may be offered by the carrier or the broker. The ability to enroll new hires, 24/7/365 enrollment, benefi t administration software, educational tools for employees, online self-service capabilities, and eligibility audits are becoming more common in the marketplace.
At this point, the employer has probably relied heavily on the expertise of their broker or benefi t advisor. And through the process, they have come to appreciate the knowledge and the degree of client-focus the broker brings to these
decisions. In the past, many employers relied on specialty voluntary advisors, often employed by a large voluntary insurance company, for this expertise.
Today, more than 95 percent of all brokers include voluntary in their portfolio and their level of expertise is growing rapidly, as impending health care reform and increasing employer interest have encouraged them to embrace voluntary. If the employer has gotten this far with their broker, they most likely have a partner who is prepared to be their trusted advisor for their voluntary program.
Employers have come to view voluntary as a key part of their benefi ts strategy and an important element in satisfying the needs of their employees, using the same care and effort with their voluntary choices as they do with their employer-paid decisions.
The analysis and selection of voluntary products, carriers, enrollment methodologies and advisors are all a part of that process. The result is better benefi t programs and more satisfi ed employers and employees.
Following his field experience as a producer and field sales manager for a major insurance company in New York State, Lowerre spent 10 years with the Life Insurance Marketing and Research Association
(LIMRA) in Hartford, Conn. In 1989, he left his position as an officer at LIMRA to start Eastbridge Consulting Group Inc. After 21 years, Eastbridge has become the leading U.S. consultancy with a specialty in voluntary product and worksite marketing and is known internationally for its research and consulting skills. Lowerre’s specialties include business strategy design, distribution development, marketing planning, worksite marketing, voluntary insurance, and employee benefits. Lowerre helps design new business models, enhance the performance of existing businesses, and helps companies enter new markets. He was inducted into the International Worksite Marketing Hall of Fame in 2006, Lowerre has an undergraduate degree in psychology and a master’s degree in management. He has three grown children and lives with his wife in Avon, Conn.
Bonnie Brazzell is a leading expert on worksite marketing of fi nancial services products. Prior to Eastbridge, she had 25 years of experience with a major worksite/voluntary carrier. During her carrier career she worked in various positions including underwriting, product development, market development, and customer marketing. Brazzell joined Eastbridge in 1999. She manages consulting projects for both worksite/voluntary and group clients. She focuses on strategic, business, and marketing planning; competitor, product, and market analyses; and business line assessments. Brazzell also oversees a variety of research projects—both consortia and client specifi c—designed to improve the marketing of group and voluntary products. She has helped clients of all types develop and improve their marketing strategies.
Bonnie is a frequent speaker at industry events and has had articles published in numerous publications. She has a degree in mathematics and lives in Columbia, S.C.
GroupMeeting
100%
80%
60%
40%
20%
0%
100%
67%61%
53% 48% 48%
26%
IndividualMeeting
Self-Enrolled
InboundTele
OutboundTele
Web IVRGroup
100%
67%
Individual
61%
Self-
53%
Inbound
48%
Outbound
48%
Web
26%
IVR
Enrollment Methods Offered by Carriers
Group Meetings, Individual Meetings, Self-enrolled, Inbound Telephonic (Call Center-passive), Outbound Telephonic (Call Center-scheduled time to call), Web (Internet enrollment), Interactive Voice Response
Today, more than 95 percent of all brokers include voluntary in their portfolio and their level of expertise is growing rapidly, as impending health care reform and increasing employer interest have encouraged them to embrace voluntary.
Chart 4:
gIlBERT W. loWERRE and BonnIE BRaZZEll » ContinuEd from pagE 35

38 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
volunTaRy/SupplEmEnTaRy BEnEFITS
By paT huoT, dIREcToR
dirECtor, managEd vision CarE
TRanSITIonS opTIcal, Inc.
When it comes to vision benefits, you may be thinking that an aging workforce equals a greater financial burden for you. and you wouldn’t be entirely wrong.
While today’s older americans are staying more active and living longer, they’re still more likely to experience health problems—including vision problems—that can drive up medical costs and reduce productivity.
think about it: as we age, we begin experiencing changes such as trouble seeing up-close, increased eyestrain and fatigue and decreased color recognition. after age 40, some workers may need vision correction for the first time—and not seeking care could spell trouble for employers. Consider that one in four employees, age 45 and older, takes frequent breaks to rest his or her eyes at work because they hurt or feel tired.
age also puts us at higher risk for many eye diseases and vision problems stemming from health issues such as diabetes and high blood pressure. Keep in mind that one in three employees will experience an eye disease by the time they reach 65.
Fortunately, there’s an easy way for employers to save money while increasing employee productivity and satisfaction. While vision benefits are among the least expensive ancillary benefits, arguably they have the highest return-on-investment. You can reap the rewards simply by knowing what to look for in a vision plan and how to position it to your employees.
Selecting a Vision Planthe key is to look for comprehensive plans that cover
regular eye care to check for vision problems and eye health issues, as well as premium eyewear options that can correct, protect and enhance an employee’s vision.
Why Premium Eyewear?it makes sense: if you can’t see well, you can’t work well.
even slightly miscorrected vision can result in a 20 percent decrease in employee productivity. While the right eyeglass prescription can make a big difference, even 20/20 vision doesn’t mean an employee is seeing his or her best.
there are many (fixable) factors that can affect the way we see—especially as we age. For example, sensitivity to light or glare is more common with age. more than eight out of 10 americans 45 and over say glare affects their vision outdoors, while 20 percent of those 55 and over have trouble seeing while driving at night.
By choosing vision plans that include lens options like adaptive transitions® lenses and anti-reflective coatings, employers can help their employees see better, and therefore be more productive. many comprehensive vision plans offer discounts on transitions lenses, which continuously adapt to changing light – reducing glare to diminish eyestrain and fatigue. they also block 100 percent of uV rays, which have been linked to the development of eye diseases like cataract and macular degeneration. Plus, they’re what employees want. nine out of 10 employees 45 and over are interested in vision plans that cover premium lens options like transitions lenses.
Making Sure You See the Benefitalmost all of your employees will agree that vision benefits
are important—becoming even more valuable with age. But despite this, one out of four employees will not enroll in a company vision plan, and a third of those who do enroll won’t use it. as an employer, there are simple steps you can take to make sure your employees—younger and older alike—take advantage of their plan, so you see the benefit as well.
• Educateyouremployeesduringtheenrollmentperiodaboutthevalueofvisionbenefitsfortheiroverallhealthandproductivity. a new tool called the individual Healthy sight Calculator shows employees their risk for various vision problems and health issues based on their age, gender and ethnicity—a real wake-up call for those of us advancing in years. Consider using the Healthy sight Calculator to reinforce their risks as well as their potential savings through their quality vision benefit (HealthySightCalculator.org).
• Stayinfrontofyouremployeesyear-roundtomakesurethosewhoenrolledaretakingadvantageoftheirbenefitsbeforetheendoftheyear.You can download complimentary newsletters, handouts and videos to share with employees at HealthySightWorkingForYou.org.
9251BelcherRd.PinellasPark,Florida33782800.533.2081ext.2262HealthySightWorkingForYou.org Twitter.com/TransitionsMVC Facebook.com/HealthySightWorkingForYou
Setting Your Sights on the Aging Workforce

Regular eye exams and quality eyewear help protect employees’ eyes and overall health – and ensure they’re seeing their best – so they can perform their best.
Transitions Optical is proud to recognize brokers who go above and beyond to promote vision benefi ts.
Learn more about the importance of vision benefi ts and the Transitions Vision Benefi ts Broker of the Year award at www.HealthySightWorkingForYou.org
Congratulationsto the 2011 Transitions Vision Benefi ts
Broker of the Year!
Patrick TibbsFinancial Services Representative
Everence Financial Advisors

40 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
PHarmaCeutiCal BeneFits manaGement
By maRK mERRITT » prEsidEnt & CEo » phaRmacEuTIcal caRE managEmEnT aSSocIaTIon (pcma)
Pharmacy benefit management (PBMs) is the one industry in America to have met the three-fold challenge posed by a generation of policymakers and consumer advocates: to simultaneously
reduce costs, expand access and improve the quality of health benefits for the 215 million Americans with prescription drug coverage.
Although PBMs will save consumers and payers almost $2 trillion in prescription drug costs—a 35 percent savings over the next decade—drugstores and drug manufacturers
are fighting back with new tactics of their own that could increase costs for consumer and payers.
How are Payers Reacting to Higher Drugstore Prices?
With approximately 60,000 pharmacies in America—many in close proximity to one another—payers have demanded discounts from drugstores in exchange for participation in the pharmacy net-works. On average, consumers who patronize independent pharma-cies have access to 21 other nearby chain, supermarket, “big box,” or other independent pharmacies.
One major drugstore chain is demanding a 20 percent pre-mium over its competitors and
has refused to renew network contracts. However, surveys confirm that 61 percent of employers want access to lower cost plans that exclude the most expensive drugstores from their coverage network.
Likewise, more than four-fifths of insured adults are unwilling to pay higher premiums to gain access to more drugstores. Consumers and payers want America’s 60,000 pharmacies to compete for their business and are willing to reward those offering lower prices.
New 2012 Medicare Part D data released by the
Centers for Medicare & Medicaid Services (CMS) show the growing popularity among Medicare Part D beneficiaries of plans with lower cost preferred pharmacy network options. Enrollment in these plans has skyrocketed and is now offered by many of the largest Part D plan sponsors. Almost a third of all beneficiaries are enrolled in a preferred pharmacy network plan.
How are States Looking to Save in Medicaid Pharmacy?
Over the past decade, public programs have increasingly sought to emulate the tactics used in the private sector to reduce prescription drug costs. The drugstore lobby has opposed efforts in Medicaid to transfer pharmacy payment decisions away from government officials. Most recently, retailers have opposed efforts by Governors Andrew Cuomo (D-NY), Chris Christie (R-NJ), Rick Perry (R-TX) and others to replace fee-for-service Medicaid prescription drug benefits with commercial-market approaches in which third party pharmacy benefit experts—not state government officials—determine pharmacy payment rates.
State Medicaid programs typically overpay for pharmacy benefits because the state officials, who set payment rates, are pressured by powerful drugstore lobbies to set payment levels artificially high.
Medicaid also uses fewer generic drugs than other programs. Over the next decade, greater use of PBM tools in Medicaid could save $33 billion—without cutting benefits or payments to doctors and hospitals.
How are Brand Drug Manufacturers Using Copay Coupons to Undermine Formularies?
Copay coupons undermine payers and PBMs’ ability to use different copay amounts to reduce drug costs. Plan costs rise dramatically when enrollees choose expensive brands over more affordable options.
The economics of brand copay coupons are simple: each time a drug company can sell a $150 product by helping cover a $50 copay, it gains $100 in revenue, which is paid by the employer, union, or health plan offering that coverage.
PBMs in 2012 and Beyond: Fighting for Consumers and Payers
“… More than four-fifths of insured adults are
unwilling to pay higher premiums to gain access
to more drugstores. Consumers and payers want America’s 60,000 pharmacies to compete
for their business and are willing to reward
those offering lower prices.”

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 41
Copay coupons encourage patients and prescribers to gravitate toward higher-cost brands that offer copay coupons in each therapeutic class. As one analyst puts it, copay coupons “warp the system,” and “steer prescriptions to higher-priced drugs that would ordinarily be written for generics,” and “lead to higher overall costs.”
One major copay coupon covered all but $4 of the consumer’s copayment, making the consumer cost for a $150 non-preferred prescription the same or less than generic alternatives. Though the consumer paid just $4, the health plan still paid two-thirds of the original price, or approximately $100. If the consumer had used a generic, the total cost to the consumer and plan would have been as low as $4.
By definition, copay promotions target only those who already have prescription drug coverage (i.e., those who pay copays). These programs are not means-tested or designed to help the poor or uninsured. Considered illegal kickbacks in federal health programs, copay coupons are banned in Medicare and Medicaid.
The number of copay coupon programs marketed to the American public has increased by more than 260 percent in the past two years. The number of programs listed on the consumer website www.internetdrugcoupons.com is now more than 340. Brand drug makers now spend $4 billion annually on copay coupon programs, and vendors administering such programs report manufacturers earn a 4:1 to 6:1 ROI.
In 2009, half of the 109 best-selling U.S. brand-name drugs were promoted by coupons, and the number of coupon subsidy programs has skyrocketed since then, from 86 in July 2009 to 362 in November 2011. Coupons are aggressively marketed to consumers by TV, radio, Internet ads, and through physicians and pharmacists.
And consumers are using them up, unaware of the negative impact on their premiums. In 2010 alone, copay coupons were used in one-eighth of all brand-name drug purchases, or 100 million prescriptions.
The increased popularity of coupons have prompted a class action lawsuits in four federal
courts against major drug manufacturers for illegally subsidizing copayments for expensive brand-name prescription drugs such as Lipitor and Nexium through the promotion of copay coupons.
The lawsuit alleges that the payments by eight drug makers—Abbott, Amgen, AstraZeneca, Bristol-Meyers-Squibb, GlaxoSmithKline, Merck, Novartis, and Pfizer—are illegal under a federal statute prohibiting commercial bribery because the undisclosed payments to patients and pharmacies are made through a ‘shadow claims system’ designed to keep information about the presence or amount of these payments from health plans.
Community Catalyst, a national consumer advocacy organization, warns that while prescription drug coupons appear to save consumers money by reducing or eliminating copayments, in reality, they dramatically increase the cost of health care by driving up health insurance premiums and potentially causing consumers to hit benefit caps or lose coverage altogether.
“Pharmaceutical corporations are duping consumers with misleading coupons that are more about increasing corporate profits than actually reducing the cost of drugs for consumers” said Wells Wilkinson, director of the Prescription Access Litigation project at Community Catalyst. “If not stopped, the use of these deceptive coupons will increase costs for consumers’ health plans by billions of dollars, contributing to higher premiums and the increasing loss of coverage and benefits for Americans.”
It is estimated that copay coupons could increase 10-year prescription drug costs by $32 billion for employers, unions and other plans sponsors if current trends continue.
Several other key copay coupon questions remain, including:
• Each year, $4 billion is spent marketing copay coupons, which yield a 6:1 return on investment. Besides payers, who pays this $24 billion to manufacturers?
• If the goal of copay coupons is to remove financial barriers to adherence, why do they only target consumers who already have prescription drug coverage (i.e.
those with copays) instead of the 50 million Americans who don’t?
• If the goal of copay coupons is to help consumers in financial need, why aren’t they means-tested and targeted toward low-income people?
• Do copay coupons encourage newly diagnosed patients to try expensive brands before trying generics?
• Why are copay coupons banned as illegal kickbacks in Medicare and other federal programs?
Mark Merritt is President and CEO of the Pharmaceutical Care Management Association (PCMA), the national association representing America’s pharmacy benefit managers (PBMs), which administer prescription drug plans for more than 216 million Americans with health coverage provided through Fortune 500 employers, health insurance plans, labor unions, and Medicare Part D. Merritt took the helm of PCMA in March 2003 and quickly raised the industry’s profile. He is repeatedly ranked as one of the most effective trade association CEOs in America and has been inducted into the U.S. Chamber of Commerce’s elite “Association Committee of 100,” representing America’s top trade association executives. In recognition of his aggressive advocacy for lower cost prescription medications, the Generic Pharmaceutical Association (GPhA), which represents the world’s leading generic drug manufacturers, honored Merritt with its prestigious “Outstanding Contribution” award. Merritt also serves on the Editorial Advisory Board for Drug Benefit News. Merritt is credited with designing and implementing innovative, campaign-style strategies that go beyond traditional Washington-style lobbying campaigns. He has pioneered strategies that reach beyond the boundaries of Washington politics to communicate more effectively with diverse constituencies from Wall Street to Main Street to Hollywood.
In 2009, half of the 109 best-selling U.S. brand-name drugs were promoted by coupons, and the number of coupon subsidy programs has skyrocketed since then, from 86 in July 2009 to 362 in November 2011.

42 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
PoPulation HealtH manaGement
By laRRy BoRESS » prEsidEnt and CEo » mIdWEST BuSInESS gRoup on hEalTh
To remain competitive in today’s global marketplace, employers are finding it necessary to invest substantial resources to improve the health—and ultimately productivity—of their
employees by offering a combination of health benefits, workplace health programs and external health management resources.
Unfortunately, many employers experience low pro-gram participation and disappointing levels of engagement in employee use and understanding of these health benefits
and wellness programs. In addi-tion, employers have increased the financial responsibility of employ-ees, seeking to better manage health care expenses.
The resulting cost-shifting to employees often results in under-utilization of health care services, reduced adherence and compli-ance with treatment regimens and declining health. Rather than con-taining costs and improving health, the combination of low engage-ment and higher cost-sharing is having the opposite effect, which contributes to driving up employer
health care expenditures. To combat these problems, employers are exploring
alternative approaches to traditional benefit designs and health improvement programs in an effort to change behavior and motivate employees to be more responsible for their health.
To help employers understand and use these new approaches, the Midwest Business Group on Health (MBGH) conducted a series of studies over a four-year period. A non-profit coalition of more than 100 employers, including Abbott Laboratories, Boeing, Kraft Foods and Walgreens, MBGH’s member organizations cover more than 3 million lives and spend in excess of $3 billion on health care. MBGH is one of 60 coalitions in the United States, and is a founding member, of the National Business Group on Health (NBCH).
Each year, the coalition conducts one or more applied research initiatives designed to test innovative health benefit strategies, gauge their impact and identify solutions for barriers to success. Recent studies have focused on the triggers and barriers of engagement in worksite programs. This research revealed that leading-edge employers, who experienced lower costs, were successful due to their ability to both integrate their data and to adopt value-based benefit design offering incentives and disincentives to motivate behavior change.
Despite widespread media about how companies could improve medication adherence by lowering medication copays, the survey found a significant majority of employers did not view copays as barriers to optimal outcomes, apparently finding value in employees having skin in the game.
This article provides an overview of the current climate for employers along with a snapshot of MBGH’s recent research, key findings and recommendations for employers.
Why are Employers’ Still Offering Health and Wellness Benefits?
Employers still see great value in offering health benefits to their employees for several reasons:
• They need to offer health benefits to recruit and retain talent.
• A healthy workforce results in higher productivity.• Their population is not getting healthier and few
patients take responsibility for own health.• The marketplace is not meeting their expectations
for keeping people healthy or treating them in quality, safe, cost-effective ways.
Another key factor often overlooked is that, while individuals see their doctors once or twice a year, for 10-12 minutes on average, employers have an opportunity to educate and motivate their workforce on how to improve their health since they see employees more than a 1,000 hours a year.
What is the State of our Workforce Health and Wellness Programs?
Employers are finding that despite the many benefits
Driving Employee Health Engagement in Today’s Global Economy
Rather than containing costs and improving
health, the combination of low engagement and
higher cost-sharing is having the opposite
effect, which contributes to driving up employer
health care expenditures.

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 43
they offer, their covered populations are not as healthy as they should be. Studies show many people are entering the workforce with early chronic disease, and that employees tend to have an entitlement mentality, which keeps them from being more proactive with their health (i.e. determining clinical or cost options).
Other challenges and realities existing include the fact that compliance with medica-tions and treatment is less than optimal and participation and engagement in wellness activi-ties and preventive screenings are low, wasting millions of dollars annually.
Unfortunately, businesses are finding that, as Saul Levin, MD, said, “Wellness is a chronic, relapseable condition needing constant attention and monitoring.”
Employer Views of Health’s Impact on Productivity
To better understand this situation and to find solutions, MBGH conducted a series of surveys of employers, employees, dependents, physicians and health coaches of health management firms. The research found:
• Ninety-five percent of employers agree there is a link between an employee’s health and their productivity
• Eighty-four percent of employers believe health benefits are a necessary cost of doing business
• Eighty-five percent of employers view health benefits as an investment in human capital with a measurable out-come
• Seventy-eight percent of all employ-ers agree the new law makes it more important than ever to keep workers healthy to keep costs down
Employers recognize the need to address chronic disease. Chronic disease is a significant and costly problem, representing more than 80 percent of health benefit costs. Most problems can be attributed to individuals allowing conditions to get worse, because they don’t stay on their medications, don’t eat correctly and are not being screened regularly by their doctors to identify or address early new risk factors.
Through proper screening, treatment,
monitoring, education and motivation, people could dramatically improve health outcomes and reduce health benefit costs (i.e. avoiding unnecessary emergency room visits and hospitalizations), resulting in improved productivity and keeping people on the job.
Targeting the Message to the Consumer
The public relations firm Edelman has done extensive research in understanding how to communicate with consumers. They found it’s critical to engage people at their level of readiness and identified different types of consumer readiness in their research:
• Health Actionists are highly engaged and interested in health and willing to persuade others to take action.
• Health Traditionalists are very interested in health, particularly as it pertains to sustainability and nutrition, but they tend not to persuade others to take action.
• Health On-demanders think about health when they need to and are the least likely to care about being healthi-er, and most likely to only think about health when they, or a member of their family, becomes sick. This group usual-ly looks to others to form their opinions about health.
• Health Disempowered are indi-viduals whose barriers to better health are attributed to confusion and lack of financial resources. They are the most likely to find health information con-fusing and contradictory and say they don’t have enough money to take good care of their family’s health.
• Health Neophytes tend to be younger, healthy and carefree.
• Health Apathetics are less likely to be motivated to take care of their health and also are less likely to share opinions about health with others.
Value-based Benefit DesignFrom 2006-2010 MBGH conducted a
series of research on value-based benefit design, the use and impact of incentives, the triggers
and barriers to engagement and communication of worksite wellness programs. The research involved surveys and focus groups of employers, employees, dependents, physicians and health coaches of health management firms.
The goals of this research were to:• Understand what prompts (triggers)
or prevents (barriers) employees from participating or maintaining involve-ment in their benefits and wellness programs.
• Realize what motivates employees to take responsibility for managing their health.
• Determine the influencers of employ-ee decisions and actions by collect-ing input from audiences beyond the employee.
• Gain insight on how to motivate and engage employees through communi-cation, culture, programs and activities.
Employee Views on Health and Recommended Approaches to Increase Engagement
MBGH’s research found individuals have an emotional attachment to their health and they take the role of managing their family’s health very seriously. However, individuals need the confidence to take action and the conviction to keep working at improving their health.
They are often motivated by personal stories about others they can relate—people with the same health condition or life stage. When they engage in programs they want to see the results, feel the results and hear the results, so they can make healthy lifestyle change permanent. The vast majority believe the most credible source for health information is their doctor.
As far as managing their health, the vast majority see being healthy as extremely impor-tant. They believe they can keep themselves healthy on their own, which is why they often don’t participate in employer wellness programs. However, they are interested in their company offering access to certain programs and services (i.e. on-site medical clinics).
The research also revealed employees see a bad diagnosis or significant emotional event as a major wake-up call to changing unhealthy

*Enabled by IncentOne®Quest, Quest Diagnostics, Blueprint for Wellness, any associated logos, and all associated Quest Diagnostics registered or unregistered trademarks are the property of Quest Diagnostics. All third party marks - ® and ™ - are the property of their respective owners. © 2011 Quest Diagnostics Incorporated. All rights reserved.
Healthy employees have their rewards Introducing Blueprint for Wellness Rewards™ from Quest Diagnostics. Now, the same company you use to create health insight through wellness screenings can help you use rewards to drive improvement. Blueprint for Wellness Rewards* makes it simple to reward on the outcomes that matter, encouraging employees to be accountable for their health and take action to improve it.
Customize your Rewards:
• Choosethemetricsandthresholdsthat are right for your culture
• Selecttherewardsthatwillmotivateyour employees —insurance premium reductions, health savings contributions, gift cards and others
• Applyyourbrandtooureasy-to-use reporting portal
Request a demo and learn more about Wellness Rewards from the leader in clinical laboratory testing, Quest Diagnostics.
Call us at 1.800.654.7824 or visit BlueprintforWellness.com/rewards
Measures that Matter. Wellness that Works.™

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 45
PoPulation HealtH manaGement
behaviors. Family and loved ones also are strong triggers for making healthy changes – especially spouses and physicians. Co-workers also can serve as major infl uencers to getting employees interested and involved in worksite health programs. Finally, senior management can serve as a strong infl uencer if company morale is high.
Based on the fi ndings in the research, our recommendations to employers include:
• Providing employees with best-in-class tools, resources and support and make it convenient for them to have access to information at all times.
• Ensuring that the organizational cul-ture of health supports not only the work environment, but that senior management is involved in workplace health programs.
• Including family members, especially spouses, in benefi ts and workplace pro-grams.
• Sharing employee testimonials or per-sonal experiences to help employees better relate to specifi c problems or health conditions.
• Encouraging employees to share clini-cal screening results with their physi-cians so that they can walk through the report together.
• Promoting team challenges at the work-place or convene a group of co-workers who want to make similar changes.
• Showing employees the results of their actions so they can make healthy lifestyle changes permanent.
• Giving employees small, achievable goals to help them stay motivated.
• Making sure senior management is visible at workplace programs and that organizational culture is high.
Increasing Employee Engagement and Participation
We found that an employee’s top barriers to engaging and participating in employer-sponsored benefi ts and programs include trust, time, money, convenience and stress.
Trust takes the lead as the biggest barrier—25 percent of employees say they don’t participate in company-sponsored wellness programs because
they aren’t sure what the company is going to do with the information. Time is a major barrier because of other commitments. Money is a major barrier, especially for those who believe they have to choose between basic needs such as buying food or paying for a health class. Convenience is a major factor for those who lead a hectic lifestyle. Finally, stress is a major barrier for those who have too many commitments or who perceive lifestyle change as a burden.
MBGH’s recommendations for addressing barriers to engagement:
• Employers need to better understand how culture has an effect on employee’s health and well-being. Focus on the elements of your organization’s culture that will instill trust.
• Creating a culture highlighting trust encourages employees to better participate in programs. Be transparent and honest when communicating to employees—about benefi ts (i.e. how much health care costs are, including what the employer pays per employee).
• Understand lack of time is a signifi cant barrier to employees participating in activities. In addition to a full time job, many are going to school, have another job, elderly parents or small children. Offer programs through different chan-nels (i.e. online programs or self-study)
• Make participation in workplace well-ness events easy by offering activities during work hours and at convenient times.
• Provide tools and resources helping employees determine their actual cost of health care services. Help employees more effectively navigate their fi nancial health care needs and personal fi nan-cial needs
• Because many employees indicate they are over-committed and often perceive making lifestyle changes a burden, provide information and resources on resiliency/stress management to help them better manage the stress they are feeling. Be sure to communicate the resources that can be offered through an Employee Assistant Programs (EAP).
Impact of FamiliesEmployees state family and loved ones can
serve as positive or negative infl uences to healthy behavior in how the people closest to them either support their effort to be healthy, or act in ways that make it more diffi cult to change to a healthy behavior.
Alternatively, consider adopting a family-based solution to a wellness problem, engaging and informing family members on what can be done to support the worker’s positive behaviors and what incentives may be available for reach-ing certain participation or activity levels.
Key Infl uencers and Motivators for Behavior Change
Employees’ views of incentives vary but most see the value of using them as a motivator. Overall, employees are open to the use of incen-tives and disincentives but perceive incentives as more powerful in changing behavior.
MBGH Research has shown fi nancial incentives and premium reductions are most favored by employees, but, ultimately, the fear of pain and risk aversion serves as greater motivators to changing behavior than incentives or disincentives
MBGH’s recommendations on incentives include:
• Structure incentives as part of the ben-efi t design to encourage participation in activites and programs.
• Connect employees with effective resources as soon as they are motivated to change—make sure they know where to go for information when they need it most.
• Communicate what’s available to them frequently.• Offer an incentive tied to obtain-
ing an annual physical—i.e., developing individualized goals based on the results.
• Employees will see it as an oppor-tunity to work with the physi-cian and the results can lead to healthy behavior changes.
To read this article in its entirety, please visit www.theihcc.com
laRRy BoRESS » ContinuEd from pagE 43

46 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By BETh gRIFFIn
As the average annual premium for employer-sponsored health care has jumped more than 115 percent since 1999,1 u.s. employers continue to
name the cost of providing health care benefits to active employees as their no. 1 benefits priority.2 Key drivers of rising health care costs are obesity—almost three-fourths of american adults are overweight or obese3—and other illnesses that lifestyle changes can prevent.
to help americans live healthy lives—and to contain the cost of health care for consumers, employers, and payers—it is imperative we implement programs that motivate consumers to make healthy lifestyle choices. employer-sponsored wellness programs reward employees for taking care of themselves and encourages healthy behaviors. research commissioned by masterCard, and conducted by Harris interactive, demonstrates that offering rewards or incentives is the most effective way to engage employees in wellness programs.
Incentives More Than Double Participation Rates in Wellness Programs
While 78 percent of employees we surveyed work for companies offering a wellness program, less than half (46 percent) participate. Yet when offered rewards or incentives, employees, working at companies offering such incentives, participate in wellness programs at more than twice the rate than employees not offered incentives—61 percent versus 26 percent. Wellness incentives have strong appeal for employees: seventy percent of those surveyed said they were extremely likely or likely to participate in a wellness program to receive an incentive.
Monetary Rewards are the Top Motivator
to participate in a wellness program, money is the incentive employees said was most appealing, even more than reduced health insurance premiums. We tested
the concept of a wellness-prepaid card, learning that employees see them as equally appealing as getting extra money in their paycheck. Prepaid cards also are easy to administer, since an outside program manager can process the incentives without burdening a company’s Hr department. We also learned what the optimal incentive structure would look like.
even more important, a wellness card would motivate most employees to sign up and stick with a wellness program. more than half of those who currently don’t
participate in wellness programs said they would be likely to do so if a wellness card was offered. the distinctive features
of a branded prepaid card were the factors employees said were most likely to motivate them to participate in a wellness program.
Incentives Cost-effectively Engage Employees in Wellness Programs While Lowering Costs
Wellness programs can attract and retain talented employees, and they also encourage those at risk for disease to change behaviors before they get sick—and reward them for doing so. making lifestyle changes is critical to restraining health care costs, since 75 percent of employers’ medical costs are currently spent on treating chronic conditions. masterCard research demonstrates rewarding employees helps raise participation in wellness programs.
About the Author:Beth Griffin is Global Business Leader, Global Prepaid Products & Services, for MasterCard Worldwide. Griffin leads the MasterCard team that works with employers, payers, and program managers to configure prepaid cards that deliver healthcare benefits more effectively and efficiently.
To learn more about MasterCard healthcare solutions, please visit mastercard.com/healthcaresolutions.
1 Kaiser Family Foundation and the Health Research and Educational Trust, 2008.
2 Deloitte Consulting LLP and the International Society of Certified Employee Benefit Specialists, 2011 Top Five Total Rewards Priorities Survey.
3 U.S. adults aged 20–74. Centers for Disease Control and Prevention, National Health and Nutrition Examination Survey, 2007–2008.
INCENTIVE Programs:Key to Promoting Employee Health and Lowering Health Care Costs
populaTIon hEalTh managEmEnT
70%of employees surveyed said they were extremely likely or likely to participate in a wellness program to receive an incentive.

Simplify employee healthcare payments with MasterCard Healthcare Payment Solutions.®
With unique and flexible solutions, a MasterCard health benefits card lets employees pay for
out-of-pocket healthcare expenses at the doctor’s office or drugstore, just like a debit or prepaid
card. Except in this case, they’re using pretax funds from their healthcare benefits account. Best of
all, they don’t have to submit paper claims or wait for check reimbursement. Add MasterCard to
your healthcare payment program.
Start by visiting mastercard.com/healthcaresolutions.
ADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCEADVANCING CONVENIENCE ADVANCING COMMERCE
©2012 MasterCard.MasterCard, MasterCard Healthcare Payment Solutions, and the MasterCard Brand Mark are trademarks of MasterCard International Incorporated.
Health and WellnessSolutions
Health and WellnessSolutions
Ironically, checks aren’tnearly as flexible as plastic.
C
M
Y
CM
MY
CY
CMY
K
MAE90040_Healthcare_ad_ECFC_X1a.pdf 1 3/8/12 3:22 PM

48 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
CollaBoratiVe strateGies
By Jon comola » foundEr » WhRg.oRg & gKEn.oRg
By WolF KIRSTEn » prEsidEnt & foundEr » InTERnaTIoInal hEalTh conSulTIng
Health is shaped by more than individual choices and medical care. There are two types of risk factors influencing individual
health; those under the direct control of the individual and factors beyond the individual’s control.
Corporate policy and programs to promote healthy lifestyles are an integral part of the overall health of the employee and his or her family. Putting the consumer at the heart of health decisions is a prerequisite to understanding the individual’s role in creating and maintaining health. However, consumerism is a necessary but insufficient condition to fully realize personal health.
The graphic to the right illustrates the connection between employees’ health and the community.
The economic and social policies within the community play a role in creating an environment conducive to promot-
ing healthy lifestyles. One striking example is the nature of the infra-structure within a given commu-nity. The lack of walkways, paths, parks and other green areas makes it extremely difficult for an individ-ual, even with the best intentions, to be physically active.
One only needs to look at most European countries where the amount of walkers and cyclists compared to the United States is impressive because European’s overall physical activity is generally higher than Americans. While Europe also faces serious challenges with regard to obesity, the dimensions are different than
in the U.S. Many other social and political factors also come into
play to create healthier environments, such as safety, crime, clean air, commercial interests, etc., making the pursuit of a healthy lifestyle a complex issue beyond the individual’s drive and motivation. Enhanced cooperation between sectors, government agencies and community leaders is needed to follow a more integrated and effective approach.
Role of the Employer
The employer can play a significant role in creating health-promoting environments. Employers, who provide leadership and participate in the economic revitalization and long-term growth and prosperity of the region, help create and sustain a regional health care environment that is designed to meet the needs of the people in and outside of the workplace.
However, employers face considerable internal and external challenges in creating healthy working environments and encouraging healthier lifestyles among employees:
• Economic – approval for investment resources• Cultural – openness to real change
Collaborative Strategies in Health Care Consumerism:LinkingEnterpriseswiththeCommunity toEnableHealthandWell-being
This partnering approach toward community
health requires broad stakeholder collaboration.
Employers are ideal agents to foster this
collaboration because they are benign, yet
vested stakeholders, in the health care system.
2005USA
Deaths2,447,910
Heart, Cancer,Stroke, Pulmonary,
Diabetes . . .
Actual Causes of Death“Human Behaviors”
Tobacco, Obesity, Diet, Inactivity,Alcohol, Motor Vehicle . . .
Root Causes “Human Conditions”
Stress, Anger, Poverty, Economics, Education Levels, Depression, Unemployment,
Broken Families, Environmental Factors, Emptiness, Hopelessness, Disconnectedness
Adapted from: National Civic League, Healthy Communities Conference 1994 Updated With CDC Data and Best Practices
Provider Response and
Individual Accountability
IndividualAccountability
Individual andCommunity
Accountability
Public Health andOrganizational
Policy
Health Care Policy
Community,Economic,
Education, andSocial Policy

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 49
• Behavioral – employee engagement• Logistical – reaching all covered lives• Community – environmental determi-
nants to health• Service delivery – effective integration
of internal, external, and emerging partners
• Communication – CDHP, HRA, HSA, FSA, 401k, RHSA
• Strategic – turning data to information into knowledge to drive action
Employer strategies, when taken as a whole, support individual health, wealth and well-being and result in better employee performance and productivity, greater employee presenteeism and lower absenteeism. Employers, who partner with communities to create sustainable strategies that create and support healthier, more livable communities, take an approach focusing on:
• population health improvement• economic vitality• community capacity building and• quality of life enhancements
Collaboration is EssentialThis partnering approach toward
community health requires broad stakeholder collaboration. Employers are ideal agents to foster this collaboration because they are benign, yet vested stakeholders, in the health care system. Employers also have a unique ability as a trusted and credible catalyst to be the convener of community resources. The health of the workplace and the health of the community are inextricably linked.
Collaboration among government, private and not-for-profi t sectors is a pre-requisite to enabling a healthy individual and creating healthy communities. However, a word of caution is warranted: “Collaboration is an unnatural human act” as John Seffrin, CEO of the American Cancer Society is fond of saying.
There is tremendous fragmentation in health care, with each interest group moving forward in whatever direction they feel is appro-priate. Despite the fact there is more that unites health, business and government sectors in pro-moting health, each sector tends to bring its own narrow perspective to discussions rather
than advancing what would be in the interest of the community. Therefore, the employer and employer representative organizations need to push for collaborative strategies and be the cata-lyst of a more integrated and united approach.
Employers have an inherent interest, and developing strategies creating healthy communities is worth the investment and yields measurable improvements in improved employee and community health and productivity.
Linking Social Responsibility and Employee Health and Well-being
Next to the employer with a vested inter-est a number of international organizations are advocating for this collaborative and integrat-ed approach. The World Health Organization (WHO) has explicitly designated enterprise-community involvement as a key area of infl u-ence for healthy workplaces (see fi gure 2).
Increasingly, the employer has an obligation to be socially responsible with regard to its
immediate community as well as its own employees. To many, this type of engagement is known as Corporate Social Responsibility (CSR) and has been receiving increasing attention in the business and political world. The World Business Council for Sustainable Development defi nes corporate social responsibility as, “the continuing commitment by business to behave ethically and contribute to economic development while improving the quality of life of the workforce and their families as well as of the local community and society at large.” Responsible business practices are concerned with issues, which not only meet but also go beyond the legal requirements. Examples of relevant standards and codes of conduct include:
• United Nations Global Compact (www.unglobalcompact.org)
• Global Reporting Initiative (www.globalreporting.org)
• OECD Guidelines for Multinational Enterprises (www.oecd.org/daf/investment/guidelines)
Mobilize
Prioritize
Plan
Do
LeadershipEngagement
Ethics & Values
WorkerInvolvement
Physical WorkEnvironment
Enterprise CommunityInvolvement
PsychologicalWork Environment
Personal WorkEnvironment
Assess
Assemble
Psychological Psychological
Evaluate
Improve
Figure 2: The World Health Organization (WHO) Healthy Workplace Model for Action

50 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
CollaBoratiVe strateGies
Jon comola and WolF KIRSTEn » ContinuEd from pagE 49
The benefits of responsible business initiatives include: reductions in cost and risk, strengthened legitimacy and reputation, increased competitive advantage and creation of win–win situations through synergistic value creation. Examples of such initiatives include:
• Providing free or affordable primary health care to workers and family members.
• Implementing gender equity policies within the workplace, even if not legally required.
• Extending advice and assistance to small and medium-sized enterprises (SMEs) with regard to creating healthy workplaces.
• Subsidizing public transportation and bicycles for employees to ride to work (if safe).
• Offering family-centered programs influencing health behaviors of friends and neighbors.
Noteworthy examples of corporate citizenship come out of South Africa where enterprises have long fought the HIV/AIDS epidemic. One such example is Mercedes-Benz South Africa, which has extended its successful workplace HIV/AIDS program to support SMEs and the broader community.
The “Siyakhana Project” (Siyakhana means “to build together” in isi-Xhosa) is designed to simultaneously tackle HIV/AIDS at the workplace, in communities, and at the primary health care level to ensure a holistic response. This involves a broad-based, public-private partnership between the government, the National Union of Metalworkers of South Africa, community-based organizations, the local Chamber of Business, provincial Department of Health, the German development agency and a health care company.
The results are impressive with more than 9,000 employees trained and counseled; 6,980 employees voluntarily tested for HIV; 595 managers trained on HIV/AIDS in the workplace in 55
SMEs, and 850 HIV positive patients referred into the treatment program with 150 people on anti-retroviral treatment.
For too long has the link between CSR and employee health and well-being been ignored, e.g. the above listed codes and conducts do not focus on employee health. The WHO Healthy Workplace model and framework is one of the first global initiatives to link and integrate the two areas. A special effort is being made to encourage SMEs to create healthy workplaces through socially responsible business practices and point them toward opportunities that are not as resource-intensive or require high-level expertise.
This initiative is being supported by the International Association for Worksite Health Promotion (IAWHP) and the recently created Global Health Promotion and Innovation Awards. CSR Europe, the leading European business network for corporate social responsibility with around 80 multinational corporations and 35 national partner organizations, also has made well-being in the workplace a key focus of their initiatives.
In the United States, Partnership for Prevention has published a document highlighting community-based health initiatives sponsored by local and national companies as part of its “Leading by Example” campaign. The publication makes a case for how business leaders have become catalysts for healthy community models in much the same way as they have invested in improving the health and productivity of their employees (e.g. Integris Health, GlaxoSmithKline, American Express,
Live Well Omaha, DTE Energy, Rochester Business Alliance, Rapid Packaging, University of Texas MD Anderson Cancer Center, Johnson & Johnson, State Farm Insurance Companies and Dow Chemical).
ConclusionFragmentation in health care persists as
interest groups continue to pursue their narrow goals. The integration of health improvement initiatives and collaborative community strategies are very much needed in order to improve population health and reduce health care costs. The authors would like to underline this need and point to global opportunities on how to engage in collaboration and overcome fragmentation. Employers are called on to take advantage of the given opportunities and take a leadership role in the collaborative process, as healthy communities are the cornerstone of healthy enterprises and their sustainability. In particular, the increasing interest in corporate social responsibility (CSR) and its link to health provides a unique opportunity not to be missed. Shareholders are now showing an interest in how employers are promoting employee health as well as the health of the community. To this regard, a new Global Health Promotion and Innovation Awards Program has been established by the Global Knowledge Exchange Network on Healthcare. The program represents a unique development, bringing together the best Asian, European, African, and American community and workplace health innovators to exchange ideas and foster improved understanding with health leaders in government, business and non-
governmental organizations. The first awards summit is scheduled for November 2012. Jon Comola is the founder of WRGH.org and GKEN.org both not for profits focused on promoting emerging better practices in health and health care. This catalytic process brings senior level executives together to learn, connect and share. Email: [email protected]
Wolf Kirsten is president and founder of International Health Consulting (www.wolfkirsten.com) based in Tucson, Ariz., and Hamburg, Germany, as well as the president of the International Association for Worksite Health Promotion (www.iawhp.org). Email: [email protected]
Making physical activity easy: Groningen, Netherlands (“Bicycle Capital of the World”)

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 51
HealtH Care aCCess For 2012
By mIKE la pEnna » viCE prEsidEnt » naTIonal WoRKSITE hEalTh cEnTER aSSocIaTIon
Employers have always been participants in the health care system as indirect purchasers of health care benefits for their workforce and as direct beneficiaries of a healthy and productive
workforce. Moreover, there has always been a very active interest
by the self-funded employer since they pay costs directly, and they feel each increase in health care costs without any insurance program to buffer the impact. When their costs go up, it is for their own work force and not for some intangible third party risk pool.
Sometimes there is a partnership of sorts with the employees through consumer cost share programming like consumer-directed health plans (CDHP)s, but there is still a direct impact for the firm for any increases in the cost of health care. At some point in time, the employer comes to the realization their cost trend is dependent upon the ‘consumer as proxy’ to determine value, with the assumption an individual who shares in cost can do some comparison shopping and will, eventually, make a good decision.
However, if the consumer has little or no accurate information and there is limited access to primary care in a community, the CDHP process will fail. This failure is the result of the consumer being overwhelmed by a combination of direct and immediate need for care, coupled with confusion about how to evaluate care options, especially for secondary and tertiary levels of medical care.
As consumers continue to be challenged by access and a drought of information, the firm is being energized at the c-suite level to address all costs in a tough economy. This means looking at each and every direct cost of production.
This strategy is even more intense in the public environment where the tax base limitations are causing basic benefits to be re-examined. Consumers and their employers are at the proverbial ‘learning moment,’ as they reconsider the overall health care options and what they can do to access value for their benefit dollars.
While employers may not yet have specifics about health care reform and what it might mean, they do know their employees will be competing in a marketplace where many more Americans will be eligible to receive health coverage. It will be more difficult to assure employees have access to quality services that assures efficient and effective care.
This has sparked a rise in what has been termed ‘retail medical outlets.’ There is hardly a street with two stoplights that does not have a couple of drugstores vending flu shots and prescriptions that can be conveniently filled at the nearby pharmacy counter. Utilization is reported to be up by some
CDHPs put the Consumer in the Driver’s Seat, but Employers ‘Take the Wheel’ With Workplace On-site Clinicsrole of employer-as-sponsor Changing to ‘employer-provider’
If the consumer has little or no accurate
information and there is limited access to
primary care in a community, the CDHP
process will fail.”

52 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
HealtH Care aCCess For 2012
mIKE la pEnna » ContinuEd from pagE 51
15-percent for retail sites but many realize that patient access, because of pure convenience, may not complement overall health status.
We have come a long way in attempting to integrate care and the access at a pharmacy-sponsored primary care site, even if it is paid out of consumer-directed funds, is not easily coordi-nated with other powerful programs addressing wellness and disease state management.
The firm or employer wanting to be abso-lutely sure of a dependable and high-value access point for their workforce is simply responding by creating one for their employee population. Often, these begin with a clinic and with access right at work. These are generally a fully outfitted primary care access point, a workplace on-site physician clinic, forming the basis for an impres-sive workplace health program.
These programs are way beyond the ‘com-pany doctor’ concept, and the firms implement-ing this strategy are sophisticated thought lead-ers in the Fortune 100 category. They are not replacing or supplementing on-site occupational health programs. They are creating a brand new medical office complex at the workplace complete with dental, vision care, pharmacy, imaging, lab services and rehabilitation support.
These sites are ambulatory medical centers that any community would be proud to have as a resource, and the employee acceptance has been exactly what one would expect from a consumer when they have services tailor-made to their
needs, placed in a location that is convenient, and priced competitively to any other option.
On-site Clinics With Full Services are Becoming the Mainstream
This becomes an obvious choice for the employee, but do these programs make sense for the employer? The answer is the typical consultative response, ‘It all depends.’ Properly done and thoughtfully deployed to a sufficient number of employees in a typical U.S. health care environment, the returns become obvious and are easily quantified.
When the programs are installed on an amateurish basis without clear goals or placed in an environment and offered to a more modestly-sized workforce, there is a chance there will be minimal impact on cost. Worse, these programs are costly to install, and they often serve only a segment of the beneficiary population who can reach the facilities. Careful analysis is generally the best way to make sure the programs will produce the desirable result.
One might assume the on-site clinic move-ment is all about cost and cost controls, but the reality is employers who have installed these programs are conspicuous in their commit-ment to their employees. Early adopters include Toyota, Pitney-Bowes, Miller-Coors, Disney World, Microsoft, Cisco and Cerner.
When a firm considers whether an on-site
clinic is right for them, they can look to some of the most respected and admired firms in the country and see model programs that are com-mitted to, first, the advancement of workforce health status and, secondly, to cost control.
Many firms have contracted with specialty service firms to start their programs and manage them on their behalf. However, some firms just go out and start their own programs.
Perdue, QuadGraphics, Rosen Hotels and Cerner have robust primary care programs that would be the envy of any health care system. They each provide a full range of services to the entire covered population—employees, spouses and dependents.
In the case of Perdue, QuadGraphics and Rosen, they have been doing this for some 20 years. QuadGraphics and Cerner offer services to other employers based on their own successful models. They don’t have to ‘sell’ these programs; they only have to expose employers to what they have already adopted for their own work force. Employers and happy employees become the standard in a community for other employers to emulate.
One of the most recent additions to the on-site community is BP, which opened a multi-discipline site at its corporate headquarters in Houston. After just a few months, the program is already fully subscribed, and the result is that hundreds of physicals have already been provided to employees and beneficiaries on-site.
BP has invested in a personal health record, and has constructed its benefit plan to financially encourage employees and dependents to have annual physicals and engage in the application of the PHR in its own personal health care plan-ning. BP’s entry into the Houston marketplace would be the equivalent of a startup of a new four-doctor medical practice. For its employees, the existence of a full primary care site next to a state-of-the-art child care center in walking distance from covered parking, and many other amenities, is a statement about being a ‘best in class’ employer.
This is not the Traditional Primary Care Office
Modern workplace medical clinics have adopted the principles of the ‘medical home,’ one

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 53
of those great ideas that has been around for 40 years, but has never really been implemented. The idea is that the patient is at the center of the health care delivery process, receiving continuous and comprehensive health care from one physician who serves not only as a direct care provider, but also as a coordinator of the entire care process.
One problem with the medical home has been that it is extremely labor intensive and pri-mary care physicians are wired for productivity. Any time dedicated to ‘coordinating’ is not con-sidered productive by the reimbursement pro-grams physicians depend upon for their bread and butter. Also, the management of patient care requires an electronic medical record and staff dedicated to communication and coordination.
Employers ‘get it’ and can invest in the cap-ital and staff support to achieve the integration that hospitals and doctors could never achieve. An employer directly benefits from every dollar invested in the health and well-being of its work force.
This is the reason every employer-sponsored program has a state-of-the-art electronic medical record system and most program the clinic staffing component to assure appointment times are generous by patient standards and luxurious compared to any private practicing physician. The reason for the visit length is to assure there is a complete engagement between the primary care provider and the patient concerning not only the reason for the visit, but the general health status of the patient. Cold sufferers are given decongestants, but their blood pressure and other health systems are checked, as well.
What does the consumer see in these clinics?
They see immediate access, a full range of service, one-stop shopping, articulation with the benefit plan, longer appointments, upscale sur-roundings, exclusivity and it is all proximal to the workplace. There is no mystery why engagement is so high. It is because they deliver the highest level of consumer sensitive services.
Does It Work For The Employer?Firms with workplace medical clinics and
the programming that support them consistently
report neutral or neg-ative health care-cost inflation and wide employee acceptance. Any vendor providing these services can give anecdotal information about cost savings and ROI that would sug-gest the programs are consistent in the deliv-ery of cost advantage and employee satisfaction.
Credible research can only be done by qualified and objective studies conducted over time, but firms like Toyota and QuadGraphics report statistics that have been verified by outside actuarial firms, and their experiences with cost savings are significant. QuadGraphics can show it has actually ‘bent the curve’ with its home-grown programming, and Toyota reports double-digit cost savings (externally verified) in the first year of clinic operation at its newest plant in San Antonio.
More importantly, perhaps, is the capture rate of employees. Capture seems like a term that is not too consumer sensitive, but it implies there is an engagement process. No one is really ‘captured’ or coerced. Actually, they are enticed and encouraged, and when they visit, they become convinced. Typical first-year capture for initial startup clinics is in the 60-percent range when a quality offering is combined with benefit redesign supporting the clinic choice. Once the employee is engaged, they stay, and we have yet to see a clinic utilization rate drop or reverse. Some clinics serve more than 85 percent of their employees primary care needs.
When one considers an active employee and beneficiary base organized around a primary care site with an EMR and a PHR, the possibilities for continued health status change are endless. With an on-site clinic program and an engaged patient base, disease state management programs can be tailor-made and preventive and intervention processes can have direct and immediate impact. Some employer managed clinics now use benchmarking standard to the HMO industry and regularly beat the managed care companies that their clinics have replaced.
Imitation is the Most Sincere Form of Flattery
As employers follow other employers into this space, it is interesting to note that insurance companies and health care systems also are lining up to enter the fray.
HCA, the largest for-profit health care system in the country, has a unit that deploys on-site services, as do several other large health systems and hospitals. Cigna, Aetna and United can provide on-site clinic services. Of course, one of the nation’s largest—and getting larger—health care providers, Walgreens, is committed to both the employer site-of-service, as well as hundreds of retail locations.
The Future?As these programs continue to become vis-
ible and accepted, and as pressure for primary care access becomes more intense, the employ-ees who have access to a workplace solution will realize not only better access, but better value for their health care benefit dollars. They will be the first in the community to experience a medical home offering and they will have an integrated offering that incorporates wellness programming, high-tech social media support and sophisticated care management and con-cierge services.
Simply put, when thought leaders and industry giants like Toyota, Cisco, Microsoft, Google, BP and Cerner engage in any prod-uct design or development in partnership with knowledgeable health care providers, the result is forward thinking and seldom modeled on the status quo. These programs are setting a stan-dard in value and services that will become the new laboratory for population management and for consumer health care access.

54 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
hEalTh caRE accESS FoR 2012
By John KaEgI
chieF strateGisthEalThSTaT Inc.
In just eight years, america’s health care bill will represent 20 percent of the nation’s economy, doubling what it was just 20 years
ago. some of the reasons for continued high medical inflation include:
• Increasingvisitstoemergencyrooms. in 2009 alone, visits to the er increased 10 percent to an all-time high of 136 million.
• PoorAmericanhealthbehaviors. thirty-two percent of men and 35 percent of women are now considered obese, which over the next 20 years will add:
• Anextra7.8millioncasesofdiabetes;
• 6.9millioncasesofheartdisease and strokes;
• Over500,000morecasesofcancer; and
• Anadditional$66billionperyear to the cost of health care.
• Demandforprimarycaredoctorsexceedssupply. the affordable Care act (aCa) is adding 32 million more insured patients to a system that will lose 160,000 primary care physicians by 2020.
unfortunately, our nation’s current political thinking about health care irrationally assumes that:
• Peoplewillbehaveintheirownbestinterests;
• Competitionamongproviderswillyieldefficient, convenient care; and
• Providersassmallbusinesseswillinvest in technology to enhance outcomes.
these fundamental economic principles may work in our free enterprise system in general, but they do not explain how health care works. it is vital we understand and work within the economics of health care if we hope to correct the root causes for higher health care costs, which are:
1. Poor health behaviors2. misaligned provider incentives; and3. Disconnected health information.
the fact of the matter is employers are america’s only entity with the leverage to influence and motivate people to take better care of their health. unless employers make a commitment to paternalistic health management for their employees, they will never find a solution to controlling costs and quality.
another economic principle leads most to focus their health and wellness programs on the 15 percent of patients with chronic conditions because they are responsible for 80 percent of health care costs. these disease management programs have largely been ineffective in lowering cost because once in the high cost category, there is little that can be done.
if employer-based health management programs are to succeed, this economic misadventure must change. the greatest opportunity to mitigate medical cost inflation is preventing the next wave of patients with expensive chronic conditions. employers and providers must place greater emphasis on the 85 percent of employees who are yet to experience high health costs in an effort to keep them out of the top 15 percent. such strategy will significantly lower downstream health care costs. this hardly means ignoring those with chronic conditions but, rather, stop shorting investment in those without.
this begins by compensating clinicians for health and wellness outcomes rather than the number of procedures they can justify.
utilizing more nurse practitioners is another effective step toward a focus on wellness and will help fill the growing physician access crisis. nurse practitioners are naturally oriented to wellness, patient empathy as well as salary-based compensation rather than fee-for-service reimbursement.
at the same time employers must increase the use of stimuli (incentives and penalties) in employee health benefit plans to motivate
behavioral change. examples include mandatory participation in, or at least cash incentives, to participate in health risk assessment (Hra) and wellness programs.
Due to a principle called “loss aversion,” penalties are more effective than dollar incentives to motivate reluctant employees to refocus on their health. examples of penalties include: requiring Hra participation to qualify for health benefits, increasing deductibles for poor health behaviors like smoking and obesity, and restricting participation in the premium health plans to those who commit to health management. a company today requiring its employees to participate in an Hra and be tobacco-free or participate and complete tobacco cessation programs in order to participate in the health benefits plan has a 93 percent participation rate.
once employees take that first step into the company’s health management program, convenience and accessibility become key to maintaining participation. at this point, upside dollar rewards can be effective as well.
Personal health coaching, providing online emedicine support and after-hours access, and implementing a completely high-tech environment are rapidly becoming the norm. the latter includes use of electronic medical records cross the care spectrum and utilizing online appointment booking and check-out/payment systems, all of which Healthstat has already adopted into its on-site health management programs.
today’s employer-based on-site health centers have enough history to sufficiently tell us the best results accrue to employers committed to a culture of health. By taking a more paternalistic approach and investing in on-site health management programs that incorporate a comprehensive suite of online operational technologies, employers have the very real ability to become tHe solution to the nation’s health care crisis.
Employers Hold the Key to Solving the Health Care Crisis

Reduced his health claims. Saved the company $700.
Healthcare is Predictable
with a partner who identifies and manages health risks early. Healthstat’s unique predictive modeling system promotes early knowledge and treatment of health risks to prevent sudden complications from derailing your business. Our experience, advanced technology and scalability can help you create an environment of wellness that works. As the leading provider of on-site primary care, health risk intervention, chronic care management and occupational medicine, Healthstat is here to make healthcare better. Inspire a healthy change today, by visiting healthstatinc.com.
Implemented Healthstat for his
company last year.
Found out he had diabetes. Learned
to manage it at work.
that works. As the leading provider of on-site primary care, health risk intervention, chronic care management and occupational medicine, Healthstat is here to make healthcare better. Inspire a healthy change today, by visiting healthstatinc.com.
Reduced his health claims. Saved the
Implemented Healthstat for his
company last year.
010463_5_Healthstat_cdhcsolutions_newlogo.indd 1 2/13/12 6:03 PM


www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 57
HealtH reWarDs & inCentiVes
By mElISSa van dyKE » prEsidEnt » IncEnTIvE RESEaRch FoundaTIon
The use of worksite wellness programs among large companies have surged in recent years, despite the economic downturn. A 2008 survey by Hewitt Associates discovered
93 percent of major companies (5000-plus employees) sponsor some form of a worksite wellness program. The primary reasons cited for company sponsorship were:
• to promote health (45 percent); • reduce health care costs (34 percent); • aid retention (32 percent); • improve morale (31 percent); • aid recruitment (28 percent); and • improve productivity (21 percent).
In its 2010 analysis, Population Health Improvement: A Market Research Survey, the Care Continuum Alliance reported 89 percent of surveyed health plans and health systems offer wellness programs. Further, 61 percent of current purchasers [of vendor-supported wellness programs
or services] view wellness programs as a “must have” within their organizations, and 89 percent of purchasers predict a trend toward more wellness programs within their organizations.
While the studies may differ in their assessment of workplace wellness program adoption (likely due to varying definitions), they all point to a trend toward greater implementation of such programs over the past decade or so. The reasons for broader adoption of wellness programs are varied but include the compelling evidence of a strong ROI in wellness programs in terms of reduced medical and
related costs, as well as lower absenteeism rates. This article examines existing research and case studies
to assess the state of workplace wellness incentives and the supporting return-on-investment (ROI) data, and makes
recommendations for determining what rewards are most effectively used in wellness programs.
A Positive Ration Short term (ROI) for corporate wellness programs has
been well documented over the past two decades. Year-round comprehensive corporate wellness initiatives have shown savings-to-cost ratios of more than $3 for each $1 invested in medical costs, absenteeism, worker’s compensation, short-term disability and increased productivity. Some examples:
• Johnson & Johnson, which started its first wellness program in 1979, saves an estimated $9 million per year from reduced medical utilization and lower administrative expenses in its Healthy People program. J&J reports that, “Our focus on health and wellness among our U.S. workforce has helped reduce per-capita health plan costs by $400 per employee per year and significantly improved overall employee health and productivity.”
• Citibank’s comprehensive health management program demonstrates that for every dollar invested in programming activities, $4.56 to $4.73 is saved in reduced health care costs.
• Union Pacific Railroad’s medical self-care program achieved cost savings of $2.78 for every dollar invested by reducing inappropriate emergency room and outpatient visits.
In a meta-analysis of the literature on costs and savings associated with workplace disease prevention and wellness programs, Harvard researchers, led by Katherine Baicker, recently reported in the New England Journal of Medicine that medical costs fall by about $3.27 for every dollar spent on wellness programs and that absenteeism costs fall by about $2.73 for every dollar spent.
Baicker and her colleagues say the most relevant question for organizations today is not whether they should offer wellness programs, but rather “how these programs should be designed, implemented and evaluated in order to achieve the best outcomes.”
Energizing Workplace Wellness Programs; The Role of Incentives, Rewards and Recognition
The reasons for broader adoption of
wellness programs are varied but include the
compelling evidence of a strong ROI in wellness
programs in terms of reduced medical and
related costs, as well as lower absenteeism rates.

LEARN. CONNECT. SHARE.
Members of The Institute join their fellow health and management industry professionals and nationally-recognized leaders in this online community to LEARN, CONNECT and SHARE in a 24/7, global environment as the journey toward health care consumerism continues.
Members of The Institute are:• Employers• Humanresourcesbenefitsmanagers• C-suiteexecutives• Financialmanagementdecisionmakers• Brokers• Advisors• Consultants• TPA’s• Administratorsofregionalhealthplanproviders• Solutionproviders• Thoughtleadersandindustryleaders
Membership is FREE and allows participants unrestricted access to the rich content and networking capabilities within, including latest articles, case studies, white papers, press releases, podcasts, videos and blogs focused on innovative health benefit management. Members also are able to post and share content and contribute to the collaborative environment within The Institute.
Benefits of Your FREE Membership:• Learn,ConnectandSharewithNetworkPeersandIndustry
InnovatorsaswellasFellowMembers• CreateaMemberProfileandJointheConversationby
CreatingBlogs,CommentingandMessaging• ReceivetheOfficialPrintPublicationofTheInstitute,
CDHC Solutions• TheIHCTodayeNewsletterDeliveredBi-monthly• ReadtheLatestBreakingNewsPertainingtoHealthCareLaws• InteractwithFellowMembers,SearchandReadContent
withinaSpecificNetwork• ReadBlogsfromIndustryExperts• ListentoTheInstitute’sWeeklyOnlineRadioShowand
AccessitsArchives• AccesstoTheInstitute’sHealth&WellnessVideoLibrary• UnrestrictedAccesstoFREEWhitePapers,Surveysand
ResearchandAllOtherContent• BecomeaStudentandTakeCoursesatTheInstitute’s
UniversityLaunchingApril2012• ReceiveaMemberDiscountforFORUMEastandWest
ConferenceSeries
BECOME A FREE MEMBERof The Institute for HealthCare Consumerism!
Sign Up Today for your FREE Membership to The Institute for HealthCare Consumerism at: theihcc.com/en/membership/membership
IHC-BecomeMemberAd.indd 1 2/16/12 12:39 AM

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 59
HealtH reWarDs & inCentiVes
A Variety of Methods The question is, how do you insure that
employees participate? Companies have tried a variety of methods to increase employee involvement, some of which have proven more effective than others. Mandatory employee participation, for example, may backfi re.
The results of an Aon Hewitt survey released in June 2011 found that “the inability to motivate and change habits has prompted concern” among employers. The report cited 56 percent of respondents who said “motivating participants to change unhealthy behaviors is the most signifi cant challenge to accomplishing its health-care program goals.”
Some progress has been made: A 2008 Health2 Resources survey of the membership of the National Association of Manufacturers (NAM) and the ERISA Industry Council (ERIC) says the number of employers offering incen-tives for health and wellness or disease man-agement programs rose from 62 to 71 percent in just one year.
Wellness program incentives are most com-monly used to encourage participation in health risk assessments (HRAs) and for actions such as attending fi tness classes, receiving immuniza-tions and reducing or stopping smoking.
Generally, rewards for participation range from cash to gift cards to merchandise. According to a 2007 report from the Kaiser Family Foundation, about 6 percent of fi rms vary premium contributions based on employ-ees’ participation in wellness programs, up from 3 percent in 2005.
Some employers have begun varying the premiums paid by their employees for health insurance based on health outcomes or attainment of goals. This approach has been endorsed, to some degree, by Congress and the White House in the Patient Protection and Affordable Care Act of 2010 (PPACA), which permits employers to offer cash incentives to employees for participating in wellness programs and for reaching certain targets. Current law limits the value of wellness incentives to 20 percent of the total health care premium spent per worker. When new rules under the PPACA go into effect in 2014, limits will rise to between 30 and 50 percent.
Theory and Practice Safeway is perhaps the organization best
known for the use of differential premiums and is reputably the model for the incentives component of the PPACA described above. Safeway has instituted a program with substan-tial differences in premiums, depending on an employee’s healthiness. The plan uses differing premiums, based on various factors such as smoking, weight, blood pressure and choles-terol levels. Employees are screened and they receive a discount off the base level premium for each test they pass or standard they meet.
The attractiveness of Safeway’s approach—and the emphasis on differential premiums in the PPACA—is obvious. In theory, if one requires workers to pay higher premiums if they fail tests for measures such as smoking, weight, blood pressure and cholesterol, they will want to become healthier to reduce their costs. When they do, the employer gets a fi tter and healthier workforce and reduces medical expenses and absenteeism. Employees benefi t in the form of lower deductibles and premiums.
In practice, Safeway’s results are impres-sive in some areas but marginal in others. According to Safeway’s statistics, the proportion of employees classifi ed as obese declined by fi ve percentage points between 2005 and 2009, while the proportion who were overweight declined by one percentage point. Meanwhile, 40 percent of workers and spouses who failed the blood pressure test in 2008, passed in 2009; 30 percent of former smokers registered as tobacco-free, and 17 percent who failed the cholesterol test in 2008 passed in 2009.
In the short-term, Safeway admits its program boosts medical expenses at fi rst because the screenings prompt people to seek treatment for newly detected problems.
Millions in SavingsInternational Truck and Engine
Corporation uses participation and attain-ment incentives to encourage high health risk assessment (HRA) participation and to assign employees to primary, secondary and tertia-ry health promotion/disease prevention pro-grams. International’s smoking policy was a
by-product of this initiative. More than half of the employees who identifi ed themselves as smokers actively participated in the smoking cessation course or quit smoking entirely.
Longitudinal study results at International, consisting of three separate retrospective sur-veys initiated in 2000, 2002 and 2004 indi-cated fi ve-year savings of $13.4 million against an investment of $1.2 million, resulting in a net savings of $12.1 million. The investment costs include staffi ng, handbooks (plus the shipping and handling fees) training, communication materials, incentives (including participation and attainment rewards) and early detection screenings.
Since International funded the cost of the initiative, the ROI for each year was calculated from the “plan paid” perspective. As such, the estimated plan paid ROI for the fi ve-year period was $9.70 for each dollar invested.
A CaveatROI is not the only consideration. Writing
in the January 2010 issue of the New England Journal of Medicine, Harald Schmidt and col-leagues argue that, “[Attainment incentives] might be fundamentally unfair because they might be only technically voluntary, out of reach for the socio-economically disadvantaged, a burden on the doctor-patient relationship and, ultimately, a source of higher out-of-pocket insurance premium costs for the very people who can least afford them”.
Nonetheless, 56 percent of employers plan to hold employees accountable for a larger share of health plan costs according to a 2010 Towers Watson study. With costs escalating, it is likely that employers will pursue attainment related incentives and disincentives aggressively within the bounds of the law. To read this article in its entirety, please visit www.theihcc.com
mElISSa van dyKE » ContinuEd from pagE 57
Preventable medical conditions represent an unsustainable drain on the nation’s fi nances.


www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 61
HealtH DeCision suPPort
By dR. WEndy lynch » hEalTh aS human capITal FoundaTIon
No longer in its infancy, health care consumerism is emerging into a stand-alone industry. We can see its expanding influence. It has its own advocacy groups and publications, such as
this one; it takes a prominent position at human resources conferences. In a sure sign of its growing presence, the medical establishment also has noticed, prompting a mix of welcoming and concerned responses.
The business of consumerism also has spawned a new generation of startups racing to become the leading provider of information consumers need. Besides adding momentum and activity to the field, these new companies are a signal that investors have sufficient confidence to bet hundreds of millions on consumerism’s growth and success. Having ridden in on the backs of high-deductibles and health savings accounts (HSA)s, consumerism has now arrived as a legitimate alternative to the status quo.
Given the major strides it has achieved, those of us witnessing progress on the front lines of consumerism have reason to be encouraged. More than ever before, there are efforts to make information available, to include individuals in health care choices, to expose previously hidden price and quality differences, and to apply market pressure to out-of-control spending. Industry leaders are busy building “it,” on the assumption that when it’s built, consumers will come.
But will they? Away from the front lines of tool-building and information-gathering, removed from policy fights about transpar-ency and portability, does the aver-age consumer want information or know how to use it? What role do they prefer to play in health care decisions?
Based on results of our recent national survey, the Altarum Survey of Consumer Opinions, this article reveals a consumer landscape containing both challenges and opportunities. Overall, there are strong signals of interest, but limited evidence of active participation. Consumers may be willing to play an active role in care, but thus far have had limited experience in doing so.
First, this article will cover the status of consumer involvement in health care both in terms of consumerism behaviors and role preferences. Next, it will describe the underlying factors associated with involvement. Lastly, it will outline some implications for consumerism efforts in the future.
Do Most People Behave as Active Consumers in Health Care?
Being a consumer involves two basic actions: selecting a product and purchasing that product. It implies active involvement in making choices and conducting a business transaction. These are usual behaviors in virtually every other aspect of life, from buying a burger to financing a home mortgage. While we may not make careful comparisons before every purchase, more often than not, we will at least check the price on a menu before we order. Not so in health care.
When asked about the amount of research they do before making a purchase, far fewer people reported doing extensive research before selecting a doctor than before selecting a car or home appliance. Another startling discovery was that only 43 percent of respondents had ever asked about the price of a service before going to the doctor, and only 29 percent had asked about price in the past year. More notably, only 54 percent ever recall a doctor offering them more than one treatment option from which to choose, as opposed to simply hearing a recommendation.
Additionally, despite recent growth in the availability of health-related information, few people report using such sources. For most of us, it seems the information revolution in health care has not yet arrived. The most common source of information people use to select a doctor is the advice of friends and family (77 percent), while only one-in-five have ever sought other sources of information.
Thus, the basic elements of consumer-oriented behavior are largely absent in health care. Most people do not spend time selecting care, take an active role in choosing among options, or ask about price. The subtle distinction is this: Most citizens remain recipients of care rather than participants in care. Once in the system, patients are still more inclined to say “ok, whatever you say,” than “tell me what my options are.”
Ready, Willing, but Not Quite Able: The Status of Consumer Involvement in Health Care
The subtle distinction is this: Most citizens
remain recipients of care rather than
participants in care.

62 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
HealtH DeCision suPPort
dR. WEndy lynch » ContinuEd from pagE 61
Contradictions Between What People Say and What They Do
Given the low frequency with which respondents reported active involvement in the behaviors and actions of consumerism, one might assume they have a correspondingly low interest in being involved. Not so. Their opinions and preferences tell a different story. A majority of respondents want to play the primary role in decisions about their care.
Consistently, the opinions shared by respondents portray a different sentiment than one would expect from the actions they report having taken in the past. Collectively, the results highlight some signifi cant contradictions between behaviors and preferences. Consider these fi ndings:
• While most people want to play an active role in their health care deci-sions, few are confi dent they can fi nd information to select better quality or lower prices. Very few believe they can affect costs by shopping.
• Most say they would be comfortable asking their doctors about the price of care, but only half have actually asked. It suggests that consumers are willing to ask, but have not had suffi cient motivation to do so.
• While about two-thirds agree the quality of care varies across providers, a minority have actually compared quality before selecting a provider. Once again, there is an understanding that quality differs, but little corresponding action to fi nd better quality care.
• When asked if they would switch pro-viders to save money, the vast majority of consumers say they would. Indeed, 60 percent of respondents said they would switch doctors to save $60. However, only 10 percent report hav-ing switched for that reason.
To the extent that one can generalize, these fi ndings describe a population that often has
interest in playing an active role in care and is willing to consider changing providers to save money and get better care. However, few take action to get information or make a choice based on what they learn. It is as though we are poised for a shift toward greater consumer involvement, but have not yet reached the tipping point.
What Factors are Associated With More Consumer-like Behaviors?
Survey results suggest several factors infl uence consumer behaviors. We can categorize them in three areas: role preference, skill or experience and fi nancial incentive.
Role Preference People vary in the degree to which they
prefer the traditional role of patient or a more consumer-oriented partnership. It follows those who feel more comfortable taking direction from doctors may not choose to ask about price or treatment options. Indeed, this seems to be the case.
While few people report wanting the doctor to take total control of decisions, some do not want to be the primary decision maker themselves. Those who preferred a less active role in decisions were less likely to recall being given treatment options by their physician. Also, those who reported feeling uncomfortable asking their doctor about the price of care (being an active consumer) were far less likely to report having ever asked.
Both role preferences and consumer behav-iors were strongly associated with age in the survey; young people prefer a greater level of involvement in decisions and a higher likelihood of information seeking and comparison shop-ping. This implies increased adoption of consum-erism behaviors over time.
Role preferences play an important role in how patients interact with the health care system. What we don’t know is how stable those preferences are. Do these preferences stay relatively consistent, or do experiences and incentives infl uence them over time? These are important questions to address in the future.
14% 17%
29%
39%
56%
43%
That I can reduce cost of health care by shopping
*That I can select better qualified doctors
Consumer confidence applying information Very Confident Somewhat Confident Uncertain/Not Confident
22.1%
39.3%
30.8%
6.6%
0.9%
Completely in charge myself
Mostly myself with input from MD
Equal input from self and MD
Mostly MD with input from myself
MD completely in charge
Desired role in medical decisions

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 63
Awareness and SkillsBecause most people report a willingness to
take action based on information about price or quality, it follows that the lack of actions taken thus far is due to the lack of available infor-mation. In fact, only about one-in-five people reported having ever looked online for official ratings of quality or patient ratings of satisfac-tion. Using such information has not become mainstream. Plus, only 14 percent reported being very confident they could lower the cost of care by shopping, which means they either don’t believe such information is available or they wouldn’t know how to apply the information use-fully. Once again, young people are the exception to this rule. Almost 40 percent of respondents under 35 reported seeking online information from peers.
Promoting awareness of price and quality information, and facilitating easy use of compari-son tools will be critical to moving the industry forward.
Financial IncentiveThe survey offered an opportunity to explore
how health plan cost-sharing corresponds to consumerism behaviors. As one might expect, individuals with greater personal responsibility for the cost of health care services reported being more actively engaged in consumerism behaviors.
For example, those at the highest deductible levels were more than twice as likely to have asked about the price of care as those with a small deductible.
This finding confirms an association between financial responsibility and cost con-sciousness. While it is not possible to conclude which comes first, it does reinforce the widely-held belief that individuals with high deduct-ibles, such as those found in consumer-directed health plans (CDHPs), take a more active role in gathering information about price. Naturally, an individual will pay more attention to price when spending his or her own money.
ImplicationsConsumerism activities are not yet the norm
in health care. Most people are not accustomed to comparing or shopping for health care services. That said, there is a clear preference by most people for greater involvement in decisions and a willingness to make use of price and quality information—if they had it.
The significant gap between what people say they would do and what they actually do indicates the information they need is not readily available at the right time, or they lack the confidence or skill to use it.
More research is needed to understand what types of information, delivered in what ways, would prompt consumers to make active choices based on quality or price. Further, because of the generational differences in both preferences and actions, it will be important to understand how to support specific populations with the right type of information delivered in the most effective way.
Overall, these results provide encouraging news about the general readiness and willingness of consumers to take an active role in health care decisions. At the same time, the findings identify some significant gaps between opinions and active consumerism behaviors.
While those leading consumerism efforts continue to pave the way with new solutions, it also is vital to encourage a greater following of active consumers. This means a better understanding of the factors that trigger action and broader, targeted information delivery at the time and in the format consumers need it. About the survey: In late 2011, Altarum administered the survey via the Internet to a national panel of respondents. It was taken by 3,258 employed people with a median age of 45 years. Fifty-four percent were female, 74 percent were white, 55 percent had at least a college degree, and the median annual income was $50,000–$59,000. Respondents were required to have either PPO or traditional indemnity health insurance, not an HMO or government-sponsored coverage. Respondents had insurance deductible levels ranging from zero to $10,000 or more.
Wendy D. Lynch PhD is co-director for Altarum’s Center for Consumer Choice in Health Care, a research center focused on understanding and promoting active individual involvement in health care decisions. She also consults to large corporations and agencies in the health care industry.
29%
13%
24%
40%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
25-34 35-44 45-54 55-64 65+
Age Group
Completely in charge myself
Mostly myself with input from MD
Equal input from self and MD
Mostly MD with input from myself
MD completely in charge
Differences in desired role in decisions by age group
30%
37%
14% 10%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Online expert ratings of quality (Online patient ratings of bedside manner)
25-34
35-44
45-54
55-64
65+
Use of online sources of information by age goup

64 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
By WIllIam R. BoylES » puBlishEr » InTERpRo puBlIcaTIonS Inc.
As early as 1998 the “consumer-driven” health care movement was about new technology. Early adopters like HealthMarket, Definity and Lumenos knew having a spending account
was only one feature of the new payment and benefits model. Employees, with a combined health savings account (HSA) or health reimbursement arrangement (HRA), plus advanced market information and support tools, were transformed into the ultimate consumer. Consumers need the whole package.
The icing on the cake was clear in those early days: online claims, online accounts and patient access to their health records was a necessity in conusmerism, but none of
those existed. By giving consumers control over their spending accounts and linking it with ‘the Internet,’ the ultimate patient, a true consumer of health care, would be created. The new Bible of consumerism was a 900-page book on the subject by Harvard Business School professor Dr. Regina Herzlinger, considered the guru of consumer-driven health care.
Flash forward to 2012. Hundreds of
new apps are on display at the major health tech conferences, with billions flowing into consumer-level phone and computer products aimed at patients. Employers and employees are tapping into dozens of new account-linked online benefits, tools and prices.
The 2012 HIMSS meeting in Las Vegas attracted 34,000 attendees and more than a thousand exhibitors. A HIMSS survey revealed there is a massive shortage of trained staff in the HIT world because the number of IT innovations has exploded: Most IT companies have less than $10 million in capital invested with little or no return on investment. Almost all are venture capital-funded businesses.
What does this have to do with consumer-
driven health care and employers? It shows how convinced investors are there will be a major change in how medical care is organized and delivered. Most ‘apps’ seen today were first envisioned back in the days of “consumer-driven health care,” such as individual genetic profiles, consumer-designed health benefits and advanced chronic care networks.
Health accounts are not just financial transactions. They mix with mainstream medical reform and delivery advances like “accountable health research” and “mass individual customization.”
Today the growth of the first piece—the accounts—is exploding. Our latest update (chart) shows HSA accounts have grown each year from January-to-January by a rock solid 22 percent a year for the last three years, well over one million accounts per year. HRAs, the original ‘consumer-driven’ health care vision, also are growing fast and reaching millions. Both seem destined to be the mainstream products of the future.
Employer and employee premium increases for HSA and HRA-linked benefits have slowed by at least half on average nationwide. Both are increasingly linked to incentives, wellness program and quality measures. This shows the
CDH Tech Vision: Big Waves Will Drive Health Consumers
We know employers are moving to re-design
benefits and give workers more skin
in the game, and we know the coming health
tech will enhance the progress made so far.
CDH teCH WorDs
598,656
732,069
942,404
21.7% 20.1% 22.7%
Accounts added prior year

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 65
accounts piece is well along the expected path from the early days of consumerism. Each quarter, national economists admit consumerism is at least half the cause of the slowdown in national health spending. With defined contribution and higher deductibles rising, few believe we are going back.
However, what is not as obvious is how much more is coming. There are a billion people on Facebook and hundreds of millions with iPads, but the vast majority of doctors still use paper claims. Most will not open an email from a patient. The idea of linking clinical studies or customized self-designed premiums for HSAs or HRAs is a lost idea in a world where PPOs and claims-based payments have not changed.
In today’s environment claims are uniformly submitted electronically, but many consumers still have little skin in the game. It’s easier to make an appointment for your dog to visit a vet than for your child to visit a pediatrician. Seeing your claims online is available everywhere, but seeing the cost of your next colonoscopy, or how much you should pay for it, is blacked out. It’s a world of half-consumers.
With this in mind, Interpro Publications has been looking down the road for answers. What we found is that huge, little-noticed but critically important structural changes have not yet even happened. Five megatrends we are calling “consumer health technology” or CDH Tech, will define everything, and play in perfectly with the progress made so far in the health care consumerism movement.
The Five Pillars Of ‘Health Tech’ That Will Turbocharge CDH
• Telecomm The new world of e-health consumers is everywhere, but nobody is really connected. The major telecoms worldwide have that connection. What is about to happen is a massive wave of system-wide adoption instead of little pieces. A little-noticed deal struck last month between AT&T and the American Medical Association is a signpost. It lets hundreds of thousands of doctors link medical records.
Verizon’s new wireless network is another example: It lets all emails be HIPAA-compliant automatically—all of them—across all current email systems without changing your password. The impact on patients will be profound.
• Telemed Most people still think of ‘telemedicine’ as something providing advice to rural doctors in India. Think again. The University of Pittsburgh Medical Center now uses iPhones and iPads in 19 medical specialties to do everything from surgery to mental health, and dozens of medical centers are signing on to the ‘telehealth’ movement. Multiple medical schools give free iPads to all students. Doctors across the world are making referrals within their own hospital, doing office visits with at-home patients, and monitoring millions of patients wearing devices. It’s just the beginning of a stunning change that will re-define 20th century medicine.
• Bank Tech Call it the CDH account video game model. Mobile apps on multi-sized devices are becoming the ideal platform for displaying all the good stuff from HSA, HRA and FSA
products, and apps and portals are exploding. But this is just the start. New connectivity standards for payers will allow undreamed of linkages between claims histories, cost predictors and account balances. Employers, consumers and providers will share a world connected to their individual purchasing power, enabling more skin in the game. The growth in consumer accounts and provider e-payments could well merge in an online world.
• Artificial Intelligence In most industries AI is driving consumer marketing. The same is about to happen with connected health consumers. Patients are about to be turbocharged due to the rising connectivity and data warehouse capabilities in the wired health world. Often patients will know more than their doctors about themselves and their medical histories. The days of “looking up” medical information on WebMD-like sites will look quaint by comparison. The really big shift is near: self-monitoring linked to self-treatment for healthy patients.
• Retailization Downstream medical services like retail clinics, at-home
The Perfect Storm
1
Smartphones
Mobile App Users
High SpeedBroadband
Decline inPhysician Numbers
AdvancedAnalytics
RisingCosts

66 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
WIllIam R. BoylES » ContinuEd from pagE 65
online self-care, and use of ‘physician substitutes” are all starting to gain traction. Everything from lab tests to imaging results will move into a consumer’s Google inbox. That means more and more payments for medical care will be made in a retail setting, including and especially at home. The tech gurus see millions of new ‘medical data points’ online paid for like iPad apps -- using cards. In case you guessed it, the telecoms will be the big beneficiaries since ‘the Internet’ traffic will double.
Employers Are Winners In the New CDHT Environment
As fun as it is to look into the future, what about the real-world impact on today’s employers? This question really links directly to the original idea that health accounts are half the equation. We know employers are moving to re-design benefits and give workers more skin in the game, and we know the coming health tech will enhance the progress made so far.
How will they merge?The answer is employers will be major
beneficiaries of the larger trend. The first indications can be seen in a variety of advanced
offerings coming downstream that might be classified as “personalized communication” or web-based health care. These are tied to population health tools like health risk assessments, medical reminders, and social media tools, and employers are an integral piece with a major role to play.
All five of the pillars above will boost the common connection between employers, patients, providers, insurers and financial institutions in ways that are not that different from what is envisioned by the new crop of products on display to enable consumers. In a truly linked world, each of the spokes in the consumer-centric wheel provide supporting roles: Payers and financial institutions have one tab on the menu, employers have another and the medical connection to the patient is another.
Imagine a “personal health record” in this connected future. Employers and employees still split the cost of the premium, and insurers and TPAs are continuously connected and feeding real-time data. Banks and AIs are in the same familiar mix, feeding in account and investment data.
But the “Five Pillars Of Health Tech” underlie the new configuration. Telecoms feed all of the data back and forth between all of the players. Telemed links the individual patient
to the new medical infrastructure. Bank Tech allocates and processes fees and subscription charges at both the wholesale and retail level and feeds summary data to the consumer. Artificial Intelligence uses the data generated by Telemed and Bank Tech on the Telecomm pipeline to customize patient-centered medicine. And all of this feeds new products and services in the new Retailization world, including payments.
Conclusion: Consumer-designed Health Tech
After 10 years, account-based health designs are becoming more and more about adoption strategy than innovation in local health financing markets and employer radar screens. Ten years of solid innovation has created an employer-consumer toolkit years ahead of the curve.
This means adoption speed will depend increasingly on broader system-wide ‘consumer-designed’ technology trends like telecommunications. telemedicine, bank technology, AI and retailization. That is exactly what is about to happen. Current innovations that are best-in-breed will be the biggest beneficiaries of larger and more robust changes in the health IT landscape. Companies, which are able to follow the big picture, will be in the best position to ride the next wave of consumer health technology. William R. Boyles is the founder of a media company that publishes two specialized newsletters: Consumer Driven Market Report and HealthPlanMarkets. The company also performs industry-wide market research. Boyles has worked for more than 40 years as a trained professional journalist and standing member of the U.S. House and Senate Periodical Press Galleries. He started in health care in 1971 as a medical claims review analyst for Blue Shield of Michigan, and worked in 1974 at the national Blue Shield Association (Chicago). He earned an M.A. in specialized communications from the University of Michigan, and began covering the U.S. Congress and health industry in 1976. Interpro published the first specialized newsletter on the HMO product, the first newsletter on PPOs, and in the first newsletter on consumer-driven health care.
Graphics courtesy of UMPG.
CDH teCH WorDs

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 67
meDiCal tourism
By lauRa caRaBEllo » ChiEf CrEativE offiCEr » cpR STRaTEgIc maRKETIng communIcaTIonS
In the past few years, medical travel has drawn interest from the self-funded employer community and the nation’s health plans, sparking growth and, in the wake of health care reforms, promising to transform medical
travel into a global and integrated health care system. A forecast by Deloitte Consulting projects medical
tourism originating in the U.S. could jump tenfold over the next decade, to nearly 16 million Americans a year seeking high quality, cost-effective procedures, from knee and hip replacements to prostate surgery and heart bypasses.
In 2011, Lowe’s Cos. and PepsiCo Inc. generated a great deal of buzz around domestic medical travel when both companies announced employees would have the option of traveling to Centers of Excellence for certain surgeries, fully covered with no copays or deductibles.
The biggest driver behind medical travel’s growing popularity, of course, has been skyrocketing health care costs. The U.S. not only spends much more per capita on health care, but also has had one of the highest spending growth rates, with both public and private health expenditures growing at rates outpacing comparable countries.
In contrast, medical care overseas is significantly less expen-sive—and efficiencies greater—than
in the U.S. because of lower costs of living, real estate values and other factors.
For example: spinal fusion costs $16,000 in Thailand compared to $41,000 in the U.S.; an in vitro fertilization cycle in Turkey costs $9,500 compared to $15,000; and hip replacements in Malaysia cost $12,000 compared to $33,000.
Part of medical travel’s growing appeal for employers is it meshes well with health insurance, including limited benefit plans, preferred provider organizations and high-deductible health plans. Another attractive feature of medical travel is it offers a personal touch, from initial phone call to follow up – at a time when patient-centered, personalized medicine is
coming into its own. This year will bring increased momentum in the
adoption of the medical travel health care benefit in response to increased corporate buy-in, demand for the specialty surgeries readily available overseas, expansion of the health savings accounts (HSA)s affiliate program to allow for travel expenses, and, coming full circle, increased inbound medical travel to the U.S.
Corporate Buy-inThe employer market has begun to embrace medical
travel as a means of controlling health care costs and improving outcomes, particularly domestic medical travel for employees who feel more comfortable and safer traveling within the U.S.
During the past year, Lowe’s paid for employees and dependents to travel to Cleveland Clinic for heart surgery. The procedure was fully covered by health insurance with no copays or deductibles, representing 234,000 employees and many more dependents covered by its self-funded health insurance plan.
Similarly, PepsiCo announced an arrangement allowing its employees to travel to Johns Hopkins Medicine in Baltimore for cardiac and joint-replacement surgeries, representing 250,000 employees and dependents.
To promote the medical travel offering among employees, PepsiCo developed a comprehensive communication program that included HR training, employee meeting presentations, a print enrollment guide mailed to the homes of all employees, and a promotional brochure. PepsiCo is positioning the benefit as one of the “exceptional extras” that PepsiCo provides employees.
Right now, the PepsiCo benefit provides care only at Johns Hopkins’ Baltimore facility, but additional domestic and international care locations are a possibility for the future.
Centers of Excellence attract patients and employers alike by emphasizing quality, as well as by negotiating a single rate, which includes fees for surgeons, anesthesiologists and all medical care up until the patient is discharged. We can expect to see more such arrangements in the coming year.
2012: The Rise of a Global Health Care System medical travel poised to become a standard health care benefit
The biggest driver behind medical travel’s
growing popularity, of course, has been skyrocketing health
care costs

68 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
meDiCal tourism
lauRa caRaBEllo » ContinuEd from pagE 67
As other major companies begin to recognize the cost-saving potential of medical travel, new partnerships will form, new benefit programs will be implemented, and never-before considered models for how to conduct business will take shape across many sectors of the industry. Likewise, more patients will overcome hesitation about traveling for care once they recognize the superior medical outcomes their colleagues are able to receive.
Employers, who send workers to high-quality hospitals, experience a 20-40 percent cost reduction, which is significant given hospital care spending rose nearly six percent last year.
As the dominoes fall, and more major companies begin offering medical travel to its workforce, the country will be in a better position to generate the level of improved outcomes and decreased health care costs that will have a positive impact on the overall economy.
Specialized SurgeriesFor the 81 million Americans who are
under- or uninsured, medical travel offers one of the few ways to receive surgeries and potentially life-saving treatments, with greater choice on a global scale in the form of unrestricted access to specialized care. Some of these procedures are associated with technology not available or a procedure prohibited or illegal in the United States. Additionally, there may be procedures not yet FDA-approved but are available outside U.S. borders, for example stem cell procedures or HIFU (ultrasound treatment for prostate cancer.)
A growing number of American couples are seeking fertility treatments in places like South Africa, Israel, Italy, Germany and Canada, where the costs can be much lower. The National Center for Health Statistics estimates about 10 percent of the childbearing population (or six million couples) suffer from infertility, a number that could increase if women continue to delay childbirth until later ages.
In the U.S., the average cost of a single in vitro effort is $12,400, and insurance usually does not cover the procedure. For many, cutting costs by traveling overseas will become an inevitable solution. Some concierge services, like PlanetHospital.com, search the globe to find the components for reproductive technology
and international adoption on behalf of clients. Prospective parents often use an egg donor from one country, a sperm donor from another, and a surrogate who will deliver in a third country, which bypasses the laws controlling such methods.
Health Savings Accounts As the number of people who have high-
deductible policies paired with HSAs continues to grow, many individuals are becoming more cost-conscious about their health care. The money in an HSA to pay for medical and surgical procedures, including diagnosis, treatment and preventive measures, often qualify as tax-free.
Key expansion of the HSA affiliate program now allows these accounts to be used for travel expenses. This is significant, given that total coverage under HSAs in 2011 was 11.4 million, up 14 percent from 2010 (an 87 percent increase since 2008). In the past few years there has been a growing tie between HSAs and medical travel, opening up significant opportunities for both industries.
As more individuals begin to make this con-nection, and recognize the opportunity, traveling for medical care will become pervasive—and fueled each year by the nation’s shortage of about 160,000 physicians by 2025—leaving too few to keep up with the flood of newly insured patients seeking care for long-neglected health problems.
In terms of accessing affordable care, places like Toronto, Vancouver and Mexico are likely to draw more Americans who will rely on their HSAs to finance the trip. It comes down to convenience and price. For many it will be a preventive care initiative, along the lines of obesity treatments and wellness programs, with the HSA money going for procedures that have not been traditionally covered by the employer program.
Inbound Medical TravelInbound medical tourism, in which
patients travel from other countries to the U.S., is still booming and successful, and competition is heating up. Some U.S. hospitals are tightening their prices to compete against other U.S. hospitals attracting foreign patients, with many expanding their efforts.
In fact, some hospitals, such as NewYork-Presbyterian/Weill Cornell, Johns Hopkins and Cedars-Sinai Medical Center, now offer VIP amenities, featuring luxury surroundings, gourmet meals and even butlers, in a bid to attract wealthy patients from around the world.
Inbound medical tourism is predicted to exceed half a million patient travelers by 2017, according to a Deloitte Center for Health Solutions report. More than one year ago, the highest percentage of those patients (32 percent) were seeking oncology treatments, according to Stackpole & Associates, an independent research company.
Patients are traveling to the U.S. from:• Mexico – 21.18% • Middle East – 14.07%• South America – 12.33%• Central America (excluding Mexico) –
11.25%• Europe – 11.23%
Russian medical tourists traditionally travel to Israel and Germany, accounting for 45 and 20 percent of patients respectively, but other desti-nations, such as Turkey, Singapore, Switzerland, France and Eastern European countries, are experiencing an increase in popularity.
Residents of Ukraine and Russia are choosing foreign clinics for reasons that include the continuing growth of medical costs in their homeland, and also concerns over low qualification of their doctors, which leads to uncertainty in the diagnoses and in the quality of the locally offered services.
The treatments most sought after by Russians include cardio surgery, organ trans-plantation, eye surgery, oncology and other chronic diseases, requiring advanced medical equipment and specialized after-care.
In addition, Russian patients opt for treatment abroad for availability of treatments and language skills. At the moment, medical travel from Russia is considered prestigious, with the overall outbound stream at one percent of the population, but Russia has potential to become a big player in the outbound medical tourism market.

mEdIcal TouRISm
For a number of years, the concept of medical travel or as some call it, medical tourism, has been discussed among thought leaders as an approach to reduce the
chronically rising health care costs for employers and their employees.
initially, the main barrier to such programs was mostly cultural, as some americans could not conceive that they could get as good or better care in another country. However, this barrier is dropping, as more people are educated about the quality available while their costs continue to increase.
the fact is that medical travel in other parts of the world is very mature with some hospitals catering to as many as 500,000 international patient events per year. as an example of this maturity, Frost & sullivan calculated the medical travel industry had reached $78.5 billion at the end of 2010 with projections to grow to $100 billion by 2012. While this staggering number includes investments in new hospitals and infrastructure, it also represents more than three million patients who traveled for medical care during that year.
these patients are traveling to state of the art hospitals for both critical care and aesthetic procedures. many of these facilities have been built from the ground up to cater to international patients and are accredited by the Joint Commission’s international accreditation program. they are equipped with the latest technology and staffed by internationally trained and board certified physicians. these hospitals also are boasting outcomes as good as or better than those found in the u.s.
as costs continue to rise for employers, and more of these costs have had to be shifted to employees, the economic incentive for medical travel is becoming overwhelming. some self-insured companies recently polled indicate the deductibles in their employee benefit plans are reaching $5,000 with out of pocket maximums climbing as high as $20,000.
For the average employee in the u.s. making $45,000 per year, this is not sustainable and translates to financial devastation for them and their family when a major surgical
procedure is needed. the challenge for employers is there are few direct win-win propositions on the market that reduce cost for employers without resulting in increased cost for employees.
However, some companies are finding that medical travel benefit programs, combined with “high touch” personal patient advocates, can be part of their solution. this approach incorporates a 360-degree approach to a patient’s care. some programs also offer both u.s. Centers of excellence as well as international facilities.
in essence, a medical travel benefit option is offered to all employees, supplementing their existing benefits. therefore,
they can choose local facilities or a traveling option. if they choose their local facilities, then their standard benefit features apply with deductible and co-insurance payments. the patient is essentially on his or her own with respect to logistics and making appointments for the surgery and the aftercare.
on the other hand, if the traveling option is chosen, then the employee typically has no
financial cost for either the procedure or the travel. a personal care advocate is assigned to support both the patient and their family during the entire care event, including aftercare and rehab. that advocate also works with on-site Destination ambassadors who support the patient and their family on a daily basis while they are traveling. often other incentives are included as well.
For the employer, they receive a one-stop-shop service that bundles travel, surgical procedures, Destination ambassadors and surgical complications insurance that limit financial risk. this service will typically save the employer between 40 to 80 percent on the actual cost of the claim.
in summary, employers now have effective options available to reduce the cost associated with larger claims together with lower cost for their employees. these options can be tailored to an employer’s specific needs and can incorporate both covered benefit critical care procedures and employee pay options such as cosmetic surgery, dental and fertility treatments.
Medical Travel Options Important Addition to Cost-Effective Benefit Design
By John lInSS
chairman, FoundermEdSERv gloBal
For the employer, they receive a one-stop-shop service
that bundles travel, surgical procedures, Destination
Ambassadors and surgical complications insurance that
limit financial risk.
www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 69

70 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
HealtH Data analYtiCs
By lEah BIndER » CEo » ThE lEapFRog gRoup
Of the many attention-grabbing topics in health care today, maternity care remains among the most critical issues for employers and employees alike.
For employers, maternity is frequently the source of the majority of inpatient health claims, as well as a significant contributor to long- and short-term disability claims.
For prospective parents, seeking high-quality maternity care is one of the most important activities prior to the birth of a child. And now, through studies done by The Leapfrog Group, employers and employees can compare hospitals on maternity care practices and outcomes that can have a critically significant impact on the health of the mother and baby, as well as the cost of care.
The Leapfrog Group is a coalition of public and private purchasers of employee health benefits founded
more than 10 years ago to work for improvements in health care safety, quality and affordability. Leapfrog administers the annual Leapfrog Hospital Survey, the gold standard for measuring and comparing hospitals’ performance on the national standards that are most relevant to consumers and purchasers of care.
Since 2009, the Leapfrog Hospital Survey has included a measure asking hospitals to report on the rate of Early Elective Newborn Deliveries on its hospital survey. An Early Elective Delivery is one performed between 37 and 39 completed weeks gestation without a medical indication, via medical induction or a cesarean section while the woman is not in active labor or experiencing spontaneous rupture of membranes.
When Leapfrog first reported on this measure in 2010, it was the first national organization to bring attention to this alarming practice of babies being delivered too early for no medical reason. Leapfrog continues to be the only organization publicly reporting rates of early elective deliveries by hospital. Because early elective deliveries are dangerous for
both women and babies, anyone seeking maternity care can use Leapfrog’s publicly available data on rates by hospital at www.leapfroggroup.org/TooEarlyDeliveries to elect the best hospitals for maternity care.
Potential Risks of Early Elective Newborn Deliveries
Newborns delivered too early and without a medical indication, such as preeclampsia, are at risk for both short- and long-term health problems. In the Journal of the American College of Obstetricians and Gynecologists, Dr. Alan Fleischman, former vice president and medical director at the March of Dimes, notes that newborns delivered between 37 and 38 6/7 weeks of gestation have increased mortality and neonatal morbidity as compared with newborns born later at term.
Short-term morbidities of an early term infant include respiratory distress, temperature instability, increased bilirubin resulting in in-hospital treatment, and infection, resulting in longer average hospital stays and higher morbidity rates than an infant carried to 40 weeks.
An analysis of U.S. singleton live births at term between 1995 and 2001 found the mortality rate decreased with increasing gestational age from 0.66 per 1,000 live births at 37 weeks to 0.33 per 1,000 live births at 39 weeks and remained stable from 39 to 40 weeks.
Despite a low absolute risk of infant death at term, the risks were more than 50 percent higher at 37 weeks than at 40 weeks. The rates for neonatal infection and later sudden infant death syndrome also decrease with increasing gestational age.
Another study found elective delivery before 39 weeks of gestation—including elective inductions, elective repeat cesarean deliveries, and elective primary cesarean deliveries—is associated with significant neonatal morbidity with 17.8 percent of neonates delivered electively at 37 to 38 weeks and 8 percent of those delivered electively at 38 to 39 weeks requiring admission to a newborn special care unit for an average of 4.5 days compared with 4.6 percent of neonates delivered at 39 weeks or beyond.
Furthermore, recent studies have shown a nearly five-
The Importance of Reducing Early Elective Newborn Deliveries
Leapfrog estimates $1 billion could be saved
annually by reducing the rate of early elective
deliveries to 1.7 percent across all hospitals

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 71
fold increase in brain development in the last five weeks of pregnancy—frequently referred to as an “explosion of brain development.” Failure to allow an infant’s brain to fully develop can lead to developmental and emotional delays later in life.
Neonatal morbidities experienced by these early-term neonates lead to increased admission to neonatal intensive care units, which results in increased medical costs. Because maternity costs are some of the highest health care costs for employers, it is important employers look to work with hospitals with the lowest rates of early elective deliveries.
For employers offering high-deductible health plans, this is of even greater importance. Costs of an elective cesarean can be up to four times as much as an uncomplicated delivery, and NICU stays can cost upwards of $3,000 per day for infants born too early, according to the March of Dimes.
Leapfrog estimates $1 billion could be saved annually by reducing the rate of early elective deliveries to 1.7 percent across all hospitals. It is important for consumers to be proactive in carefully selecting a provider in order to prevent added costs and health challenges to mothers and their newborns.
Leapfrog Results of 2011 Early Elective Newborn Deliveries Measure
On Jan. 25, 2012, The Leapfrog Group presented its findings from the 2011 Leapfrog Hospital Survey on Early Elective Deliveries.
This is Leapfrog’s second year reporting on the early elective deliveries measure.
Data from the 2010 survey showed reporting hospitals had an average of 17 percent elective deliv-eries between 37 and 39 weeks. In 2011, that average dropped to 14 percent. This is prom-ising news. However, hospitals are still
delivering babies before 39 weeks far too often. Leapfrog’s target for early elective deliveries is 5 percent. Many hospitals have achieved this milestone—39 percent of all reporting hospitals.
Unfortunately, rates across the country and even within states vary widely—from less than 5 percent to more than 40 percent within the same community. Leapfrog is encouraged by hospitals having adopted policies preventing early elective deliveries, and further encouraged that 65 per-cent of all hospitals reporting in 2010 and 2011 showed improvement in reducing their rates of early elective deliveries.
The chart above demonstrates the great variation among hospitals. Most promising is how many hospitals are achieving Leapfrog’s target of 5 percent or less—39 percent of all reporting hospitals in 2011, an increase from 30 percent of all hospitals in 2010.
However, this still implies that six of every 10 reporting hospitals are electively delivering babies at a rate higher than Leapfrog’s standard. There also was a large variation on state-by-state average rate of early elective deliveries. Ohio had the lowest rate, at 7.6 percent, while Alabama showed the highest rate, at 22.5 percent of deliveries between 37 and 39 weeks performed electively.
Important Information for Women
Leapfrog is committed to further communication and education for women and providers on the importance of eliminating early
elective deliveries in order to help all hospitals achieve a rate of 5 percent or less.
Despite these great dangers posed to infants for a practice occurring far too often, The Leapfrog Group is the only organization reporting rates of early elective deliveries by hospital and providing women with critical information needed to select a provider for maternity care. Data for all reporting hospitals is available on Leapfrog’s website at www.leapfroggroup.org/TooEarlyDeliveries. CDHC_MD_Outlook Piece.docx Leapfrog is proud to partner with organizations like Childbirth Connection, March of Dimes, and the national health plans (Aetna, Cigna, UnitedHealthcare and WellPoint) to educate women on the importance of the last weeks of pregnancy.
Many women are unaware of the risks and potential complications of an early elective delivery. A study performed by Childbirth Connection found many women who had an early elective delivery were not aware of the risks it carried.
Furthermore, many of these women stated they would not have proceeded with their delivery prior to 39 completed weeks if they had been fully educated on the potential harm to them and their baby. To further assist women, the March of Dimes has developed a checklist of questions for women to ask their provider if he or she suggests that she schedule a cesarean section or induction prior to 39 completed weeks. Those questions to ask include:
• Is there a problem with my health or the health of my baby that may make me need to have my baby early?
• Can I wait to have my baby until I’m closer to 39 weeks?
• Why do you need to induce my labor?• How will you induce my labor?• Will inducing labor increase the chance
that I’ll need to have a c-section?• Why do I need to have a c-section?• What problems can a c-section cause
for me and my baby?• Will I need to have a c-section in future
pregnancies?
Num
ber
of H
ospi
tals
Rate of Early Elective Deliveries
20102011
300
250
200
150
100
50
00-5% 5-10% 10-15% 15-20% 20-25% 25-30% 30-35% 35-40% 40%+

72 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
Care netWorK
By doug BullEIT » foundEr » dcS hEalTh
Have you ever noticed how some of our favorite words—words like strike, spike, hike and… like—often mean different things
in different contexts? Others—like sanction, sanguine, bolt and buckle—can even take on contrasting connotations as their settings change.
Case in point: Care. Some folks take care to provide for their future care, while others couldn’t care less—about how much, or how little, care they’ll eventually need, or who will provide it—until they need it.
There’s an awful lot of talk these days about health care and, perhaps, even more about its mounting costs and reimbursement plans.
Sadly, there’s comparatively little care being given to long-term care (LTC): Where are all of us baby boomers going to go for the in-home care that most of us will need as we, ideally, age-in-place?
Less than 10 percent of us carry private insurance to cover these costs and Medicare/Medicaid will step up only if and when we become demonstrably indigent. Sooner still, how many of us have already been jolted by the unanticipated needs of a loved one?
Forward-looking organizations like The Institute for HealthCare Consumerism (IHC) are taking care to make sure comparatively neglected health care consumerism strategies get the attention they deserve. And, by way of previews of coming attractions, expect to see more care and attention coming to LTC as well.
But, it’s not as if we’re all asleep at the LTC wheel even now. There are any number of exciting new initiatives aiming to bring empowering consumer-driven techniques to seniors: a group that’s, itself, already fi nancially and otherwise moti-
vated to age-in-place for as long as they can. Moreover, some of the same Web 2.0/3.0 technologies
that have shown real gains in health care are now beginning to fi nd similar roles in LTC as well: GrandCare, CareZone, CareVerge and other carefully-crafted patient-centric platforms.
And, as is often the case on any frontier, these early-stage companies are coming at the problem from some-what different directions. However, what they tend to have in common are many of the same continuum of care dynamics that animate other Patient-Centered Medical Home (PCMH) strategies: e.g., more serious social networks aimed to encircle seniors within a different “continuum” comprising care-givers of all sorts.
More than three-fourths of all health care costs stem from various chronic conditions. And of all individuals over 65 years-old, four of fi ve suffer from at least one chronic
On Careful Networks and Support of Long-term Care
More than three-fourths of all health care costs
stem from various chronic conditions.
couldn’t care less—about how much, or how

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 73
affliction; indeed, more than 20 percent of all seniors have five or more. And, these figures don’t even count the bulk of home care and other LTC services.
But all the news here isn’t all that bad. Inasmuch as seniors drive such a disproportionate share of all costs, the clear opportunity to manage LTC better holds enormous promise. And, the power of virtual community ecosystems, as well as the communications technologies needed to bring them all together, is at hand.
Even a cursory overview of the technolo-gies* involved in what might be thought of as Careful Networking would fill more space than available here.
However, suffice it to say, the requirements exacted by LTC—let alone its allied health-care applications—introduce security, systems and user-interface issues that collectively suggest a unique architectural approach.
Also known as Community-as-a-Service, or CaaS) solutions, there are a variety of non-technical reasons for this particular hue of mobile cloud computing as well.
To fully appreciate the LTC opportunity enabled by CaaS, we must begin to think in terms of three-dimensional value propositions: First, of course, is the elder/patient herself (e.g., what set of Internet-enabled applications bring not only help and assistance but new meaning to
her daily life?); as mentioned above, commu-nity/social networking provides surprisingly potent motivators in both directions. (i.e., trusted caregivers can make all the difference in creating a critical audience mass); in turn, this same extended community “mass” cre-ates a more compelling case drawing in the professional caregiver ecosystem as well.
Indeed, in this Careful Network picture, one could envision yet more dimensions of new ecosystem opportunity. Here’s a prime example…
Growing quickly in vigor and number, seniors bring diverse skills and life experiences to their respective communities; moreover, they have the same yearning to matter (albeit with more time on their hands) as the rest of us…maybe more.
In other words, a given senior may, at the same time, be a beneficent actor in any or all three dimensions. He or she can, at different, and/or, perhaps, the same stage of his or her life be a provider as well as a recipient in a carefully designed and managed network; he or she can “time bank” his or her efforts for future credit and/or receive direct compensation and/or merely recognition now.
A good example of the kind of Careful Network innovation that we can expect to see more of in the near future is Family Health Network’s Connected For Life (CFL) platform
now being deployed in the Research Triangle area of North Carolina.
CFL will, in turn, power a countywide “ElderCore” program where each an every senior forms the core of a Careful community comprising, “ElderCorps” of seniors and others all allied against the unsustainable cost of LTC.
The author: Doug Bulleit, a member of The Institute for HealthCare Consumerism’s League of Leaders, founded DCS Health. He now advises Family Health Network and previously served as BellSouth Corporation’s Chief Strategist
* For elaboration on Web 2.0/3.0 dynamics, for example, see unpublished Boyles & Bulleit white paper at http://silverbulleits.typepad.com/dcs/2009/05/the-semifinal-cut-on-web-30.html
Inasmuch as seniors drive such a disproportionate share of all costs, the clear opportunity to manage LTC better holds enormous promise.

also found health insurance is consuming a big-ger share of employer budgets, pre-empting pay raises and pushing higher costs onto employees.
Analysts at the Congressional Budget Office estimate the average policy for those who get health insurance through the workplace will cost $20,000 a year for a family of four by the year 2016. Millions of Americans, who buy insurance on their own, will pay at least $2,100 a year more for their policies than if the law had not passed, CBO says.
One of the tools that many companies have used to help hold down health costs also is threatened by the health law.
Many employers are offering health plans that engage their employees as partners in man-aging health costs, giving them more control over health care and health spending decisions. A 2011 survey conducted by the National Business Group on Health (NBGH) and Towers Watson on Purchasing Value in Health Care found that companies offering account-based health plans, such as health savings accounts or health reim-bursement arrangements, had coverage costs that were $900 lower than average for employee-only coverage and $2,885 lower for preferred provider and point of service (PPO/POS) plans.
The number of people with HSA/HDHP (high-deductible health plan) coverage rose to more than 11.4 million in January 2011, up from 10 million in January 2010, 8 million in January 2009, and 6 million in January 2008. Companies have found these account-based plans valuable in helping them continue to offer affordable coverage.
“The cost of [account-based health plan] coverage is considerably more affordable than either PPO/POS plan or HMO plan coverage in 2011,” the NBGH survey found.
The Obama administration would not have had the audacity to directly kill health savings accounts and other high-deductible plans directly in the health overhaul law. But it has plenty of leeway to do it through regulation. As a result, consumer-directed plans are at risk of being strangled by obscure and complex regulations issued by the Department of Health and Human Services (HHS).
If the new HHS rules remain unchanged, HSAs are likely to wither on the vine.
The specific provision that targets HSAs is the “medical loss ratio” (MLR), which regulates how health insurance carriers must spend the money collected from premiums. The MLR rules require health insurance carriers to spend 85 percent of the money they collect from premiums on direct medical care for large groups and 80 percent for individual and small groups. The remainder can go to administrative expenses, such as negotiating with companies about costs and benefits and due diligence in paying bills to make sure premium dollars are being spent appropriately.
HHS has been very inflexible in listening to the real world impact of its regulations imple-menting this provision. As an example, the final MLR rules released on Dec 2, 2011, rejected insurers’ requests that the health expenditure side of the MLR equation include anti-fraud efforts. That means the new MLR rules constrain the ability of health plans to fight fraud because that spending now must count toward their administrative expenses. It’s a catch-22. Under the new HHS rules, health insurance companies will have a disincentive to fight fraud and protect policyholders’ premium dollars.
The MLR rules discriminate against high-deductible health plans in another important way because the rules only count payments made directly by insurers as medical expenses. Health care costs paid by individuals below the deductible don’t qualify, making it hard for these plans to meet the 80 percent MLR test.
In other words, HHS rules mean that if an individual pays for a health care service to meet the deductible, the expenditure does not count toward the MLR ratio, even though the full amount is actually a payment for medical services. High-deductible policies provide customers protection against large medical expenses, but carriers may not pay out the required percentage every year in medical claims, making it very difficult for them to meet the MLR tests. Only about 5 percent of HSA policies have claims above the deductible.
“If it is too difficult [for HSAs to meet the MLR test], insurance companies won’t offer them,” said Roy Ramthun, who played a major role in writing HSA regulations during the Bush administration. “That would mean the most
affordable policies would go off the market.”A new report by Milliman Inc. finds that
high-deductible health plans, including those with HSAs, are much more likely to be adversely impacted by the medical loss ratio requirements than other types of health plans. The report also showed that consumers who rely on HSAs are likely to experience higher costs and may even be forced to get more expensive replacement coverage.
“HSAs were widely anticipated to be the low-cost bronze plans for consumers under the Patient Protection and Affordable Care Act,” said Kevin McKechnie, executive director of American Bankers Association’s HSA Council, which commissioned the Milliman study. “The medical loss ratio requirements make this very difficult and the requirements with respect to HSAs need to be adjusted, as we have repeatedly advised Health and Human Services. We urge the U.S. Senate and the White House to prevail upon HHS to revise this rule to prevent politically difficult, unintended consequences.”
The bottom line: One of the tools that busi-nesses have found to be most valuable in helping them offer affordable coverage could be strangled by these complex and obscure MLR regulations.
There also will be less competition in the health insurance market. Companies selling poli-cies to individuals and small groups already are threatened by the law. They have higher market-ing costs and higher customer service expenses, and it is especially difficult for them to meet the MLR tests because their administrative costs are necessarily higher. Many health insurance com-panies have slashed the number of employees, cut agent commissions, and taken other harsh steps to reduce overhead, but this also is slashing customer services. To read this article in its entirety, please visit www.theihcc.com
PoliCY & leGislation
“If it is too difficult [for HSAs to meet the MLR test], insurance companies won’t offer them,” said Roy Ramthun.
By gRacE-maRIE TuRnER » ContinuEd from pagE 17
74 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com

HSA/HRA/FSA TecHnology: AdminiSTRATion & mAnAgemenT
TSyS Healthcare® provides end-to-end strategic payment solutions for consumer directed healthcare. We partner with benefits administrators, financial institutions, health plans, and software providers to navigate all aspects of HSAs, HRAs, FSAs, transportation accounts, cash reimbursements, and lines of credit. TSYS Healthcare cards offer participants the security they expect along with the ability to conveniently access funds from multiple accounts and manage their benefits payments with simplified single-card access. Clients and partners benefit from simplified processes, reduced paperwork and cost savings that can contribute to improved return on investment.
“We built the TSyS Healthcare platform to meet the market demand for reliable, configurable and intelligent solutions. Understanding the dynamic U.S. healthcare market, our customers rely on our option-driven system to prepare them for the future.”
— Trey Jinks, Group Executive, TSYS Healthcare
TSyS [email protected]
Access these profiles online at www.TheIHCC.com and www.EmployersWeb.com
www.theihcc.com Who’s Who Profiles
www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 75
HSA / HRA / FSA AdminiSTRATion And FinAnce
evolution1 and its Partners serve more than seven million consumers, making it the nation’s largest electronic payment, on-premise and cloud computing healthcare solution that administers reimbursement accounts, including HSAs, HRAs, FSAs, VeBAs, Wellness and Transit Plans. It is the only solution that meets more than 1,200 unique plan designs, provides innovative auto-substantiation technologies, simplifies user experience, and automates workflow for Partners, employers, and consumers. It does all this on one technology platform comprised of Lighthouse1™, PayDirect®, the Benny® Prepaid Benefits Card, Lighthouse1 OneCard™ and integrated web portals. Evolution1 and its Partners are dedicated to delivering value, reducing costs and simplifying the business of healthcare.
eVolUTion1, [email protected]
“The combination of our innovative products will further our leadership position in a rapidly changing healthcare market. Together with our Partners we are committed to reducing costs and simplifying the business of healthcare.”
— Jeff Young Chairman and CEO, Evolution1
deciSion SUPPoRT & coST-SAVingS ToolS
my HSA Rewards allows individuals to earn cash rewards for purchases made through merchants participating in the program. At launch, the merchant network consists of hundreds of major online retailers representing thousands of brands. The program works like an airline mileage program, but, instead of earning miles, participants earn cash rewards that are directedto a health savings account (HSA). There is no cost to the employer or the employee to join.
“if you want to grow your Health Savings Account faster and with ease, my HSA Rewards is a smart and simple way to put real cash into your HSA from the purchases you make every day.”
— Sanders McConnell, President, My HSA Rewards
my HSA ReWARdS12460 Crabapple RoadSuite 202-254Alpharetta, GA 30009 [email protected]

76 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
Since 1988, Flex has provided comprehensive, benefit reimbursement services to employers throughout the U.S. that are better, faster and more seamless than any in the marketplace. We are advocates of consumer-driven health plans and have fully-dedicated ourselves to the strategic concept of tax-advantaged and account-based programs.
Our core portfolio includes:n COBRA Administrationn Flexible Spending Accounts (FSAs)n Health Reimbursement Arrangements (HRAs)n Health Savings Accounts (HSAs) – Employer & Individual Solutions!n Transit/Parking Reimbursement Accounts (TRAs)n And more!
Our robust, integrated resources provide everything employers need to integrate Flex Plans, including scalable features, simplified transactions/reimbursements, plan design expertise, education/ communication resources and online access.
Just Flex it™ today and discover how simple benefits administration can truly be.
HSA/HRA/FSA TecHnology: AdminiSTRATion & mAnAgemenT
FlexiBle BeneFiT SeRVice coRPoRATion (Flex)10275 W. Higgins Road, Suite 500 Rosemont, IL 60018
www.JustFlexit.com [email protected]
www.theihcc.comWho’s Who Profiles
Solutions to help your innovative health and benefit programs.
PoPUlATion HeAlTH And WellneSS
dataPath, inc., is one of nation’s largest providers of cdH solutions specializing in account-based administration systems.
Since 1984, service providers using DataPath systems have provided administrative solutions for over 1 million participants of FSA, HRA, HSA, and COBRA. DataPath is the only solutions provider to design and deliver a full Suite of systems for handling 125, 105, 132, COBRA, HSAs, Credit and Debit Cards all delivered to account holders through a single Internet portal, myRSC.com.
“With the significant changes in healthcare today, our software solutions allow users to create custom plans for clients that benefit both the employer and employee. not only have we created a single platform for all systems with myRSc.com, with the integration of our mySourcecard® debit card at Wal-mart and other retailers, our clients are able to offer a hassle-free solution with 100% compliance.”
dATAPATH, inc.1601 WestPark Drive, Suite 9Little Rock, AR 72204
501.296.9990www.dpath.com
HSA/HRA/FSA TecHnology: AdminiSTRATion & mAnAgemenT
lifeSynch changes behaviors to improve lives. Our approach integrates care of the mind and body to enhance health, increase productivity and minimize unnecessary medical expenses. Built on a solid foundation of understanding human behavior and how to motivate behavior change, we deliver proven outcomes through:
“Whether it’s lifeSynch’s health coaching, eAP/Work-life, integrated medical-behavioral health or utilization management services, we integrate our behavioral health and behavior change expertise to ensure our members reach their goals and achieve sustainable, long-term improvements toward their health and well-being.”
– Sean Slovenski, President of LifeSynch,
liFeSyncH2101 W. John Carpenter FrwyIrving, Texas 75063800-207-5101www.lifesynch.com
ToTAl PoPUlATion HeAlTH mAnAgemenT
n Proven methods that lead to increased engagement and sustained behavior change.
n Clinicians and coaches who provide personalized attention and form trusted relationships with members.
n Customizable programs that easily incorporate into existing benefits and services.
n Scientifically proven best-practice guidelines to proactively manage care.
n Scalable, user-friendly technology.

www.TheIHCC.com I CDHC Solutions™ I IHC Annual Outlook 2012 77
SUPPlemenTAl HeAlTH
delta dental leads the industry in designing innovative dental coverage programs that keep costs down and deliver quality care. Our diverse client list includes everyone from Fortune 100 companies to public agencies to individuals and families. Our customer’s satisfaction is based on our expansive dentist network, cost-saving mechanisms and superior customer service. We are part of the Delta Dental Plans Association that provides dental coverage to more than 56 million people in the US.
delTA denTAl1130 Sanctuary Pkwy, Suite 600Alpharetta, GA 30009
770-641-5196
Access these profiles online at www.TheIHCC.com and www.EmployersWeb.com
www.theihcc.com Who’s Who Profiles
HSA / HRA / FSA AdminiSTRATion And FinAnce
After 25 years of delivering best of breed products and services in the consumer-directed marketplace, we have embarked on a journey with Aetna to become the nation’s largest, most innovative, consumer-directed health plan solution. Together, we represent a unique solution for employers of all sizes allowing them the ability to consolidate vendors for one-stop shopping and an integrated healthcare experience for their employees. When you combine Aetna, a pioneer in the development and growth of consumer-direct health plans with PayFlex, an innovative, technology-driven provider of account-based plans, you get a dynamic combination of national presence, proven experience and solid performance.
Rob Butler, PayFlex Systems USA, Inc., President
HSA/HRA/FSA TecHnology: AdminiSTRATion & mAnAgemenT
ceridian provides cdHc administration with your business in mind. As a leading provider of human resource, benefits and payment solutions, Ceridian helps organizations control costs, save time, optimize their workforce, grow revenue and minimize financial risk. Ceridian’s CDHC administration services are designed to generate significant, sustainable savings through increased employee engagement. Our solution includes innovative features such as integrated account access, promotional communications, online claims and receipt uploads, and a mobile application coming soon.
“The key to controlling health care costs is also an employer’s most valuable resource – their employees. ceridian goes beyond typical benefits administration to help employers form a phased, multiyear plan for engaging employees in their health and health care, which significantly lowers costs in the long term.”
– Ernie Harris, Senior Product Manager for CDHC, Ceridian
ceRidiAn3201 34th Street SouthSt. Petersburg, FL 33711
727-395-1764 [email protected]

Solutions to help your innovative health and benefit programs.
If you use the services of our solutions providers, please tell them you saw their ad in CDHC Solutions™.Requests for Permissions to reuse content contact Copyright Clearance Center at [email protected].
advertising contacts
Aetna ................................................... 20-21
AhiP .................................................. 16, 78
AiG........................................................... 36
Allstate .................................................... 79
Ceridian .....................................................77
ConnectYourCare ................................. 12-13
DataPath ....................................... 32-33, 76
Delta Dental ...............................................77
Dss research ............................................76
envision Pharmaceutical services ...............78
evolution1 ..................................................75
flexible Benefit service Corporation ...........76
fis healthcare solutions ...................... 14-15
healthstat ............. Inside Front Cover, 54-55
ihC Call for Content....................................60
ihC healthCare Consumerism radio..............5
ihC Membership Benefits ...........................58
lifesynch ...................................................76
MasterCard .......................................... 46-47
Medserv Global ..........................................69
My hsA rewards ........................................75
Payflex ......................................................77
Quest Diagnostics .......................................44
Target ........................................................56
Transitions ........................................... 38-39
TsYs healthcare ............................ 30-31, 75
UnitedhealthCare .........................Back Cover
UMr .................................................... 24-25
Us Bank ............................................... 28-29
Workable solutions ......................................7
advertising index
404.671.9551
CEO/PublIshErDoug Field [email protected] · ext. 101
AssOCIAtE PublIshErBrent Macy [email protected] · ext. 103
VICE PrEsIdEnt Of busInEss dEVElOPmEntSusan Yakots [email protected], ext. 102
busInEss dEVElOPmEnt AssOCIAtEDavid Cerri [email protected], ext. 106
ACCOunt mAnAgErsJoni Lipson [email protected]
Rogers Beasley [email protected]
rEPrIntsSusan Yakots [email protected], ext. 102
R e s o u R c e G u i d e
www.theihcc.comWho’s Who Profiles
78 IHC Annual Outlook 2012 I CDHC Solutions™ I www.TheIHCC.com
PRoFeSSionAl deVeloPmenT
Health Insurance 101: An Orientation is a new, flexible online course offered by AHiP.
It is designed to teach health insurance basics to those new to health care or individuals who wish to review the fundamentals. The course is formatted in short modules; you learn at your own pace and on your own time, moving through the materials as you choose. Plus, AHIP will customize the course to fit your organization’s specific learning requirements.
AmeRicA’S HeAlTH inSURAnce PlAnS 601 Pennsylvania Ave., NWSouth Building, Suite 500Washington, D.C. 20004
Lindsey Miranda Canaley
Tel: 800.509.4422Fax: 202.861.6354 [email protected] www.ahip.org/courses
envision Pharmaceutical Services, inc is a full service pharmacy benefits management company that delivers! We deliver because our business model is based on transparency and full disclosure, guaranteeing 100% pass through pricing of all pharmaceutical manufacturer rebates and administrative fees at the point-of-sale. Additionally, our affiliate, Envision Insurance Company, is a national Prescription Drug Plan which enables us to offer a variety of solutions for your retirees. Envision is truly a “different” PBM!
“envision is pleased to be recognized by its clients surveyed by the Pharmacy Benefits management institute for three consecutive years as the top performer in virtually every category evaluated. This solidifies our leadership position in providing transparency and full disclosure to the PBm marketplace while continuing to find innovative solutions.”
— Kevin M. Nagle, President & CEO, Envision Pharmaceutical Services/Rx Options
PHARmAceUTicAl BeneFiTS mAnAgemenT
enViSion PHARmeceUTicAl SeRViceS, inc.John Ewell, EVP Marketing

LEO BURNETT U.S.A.A DIVISION OF LEO BURNETT COMPANY, INC.
Ad/ID No. AHFP0262 – Job No. 610-ALALFNP1001 – Allstate “Complete” Ad – 4C – (T 7.875" x 10.5") – 2011
101506d_AS_262_Complete_Mag_a01.indd
Printed in the U.S.A.
AD: G. Nobles PSM: B. Dolnick
Allstate • “Complete” Ad • CDHC Solutions • 4C • Ad# AHFP0262
101506d_AS_262_Complete_Mag_a01.indd
LeoBurnett/Allstate/101506
Allstate Financial Benefi ts Print Ads
PM: Barnes
Operator: EZ 06/03/11_9:50am STUDIONEDIGITAL
What’s Missing From Your Benefi ts Program? Allstate Benefi ts. The partner who’ll keep employees covered in today’s
changing benefi ts environment. And, with the #1 critical illness product
in America, it’s no wonder we’re one of the fastest-growing benefi ts
providers in the country. Call an Allstate Benefi ts Representative today
and let the Good Hands go to work for you.
1-866-895-8677
or allstateatwork.com
You’re in Good Hands.
Allstate Benefi ts Internal Data 2010; LIMRA. Allstate Benefi ts is the marketing name used by American Heritage Life Insurance Company (Home Offi ce, Jacksonville, FL), a subsidiary of The Allstate
Corporation. © 2011 Allstate Insurance Company. www.allstate.com or www.allstateatwork.com
Life • Disability • Critical Illness • Accident • Medical Gap
10.5
" Tri
m
7.875" Trim
11.3
33"
Ble
ed
8.833" Bleed
9.5
" Liv
e
6.833" Live
Scale: 1" = 1"

UnitedHealthcare’s industry-leading consumer-driven health (CDH) plans were designed to get employees on the path to good health with improved lifestyle habits and use of the health care system. � at’s why our plans o� er:
• 100% preventive coverage and personalized messaging based on individual health care needs
• Easy-to-use resources for employees, including treatment cost estimators, Quicken HealthSM Expense Tracker, and Health Care LaneSM to help members understand and maximize their health care bene� ts
• Banking through our own OptumHealth Bank, Member of the FDIC, off ering integrated access to account balances and a debit card that makes payments easier
Tools like these help employees become active in their own health care decisions. We also off er the employer ready-to-use tools to implement and successfully maintain its consumer-driven health plans.
For more information on UnitedHealthcare’s CDH plans, visit uhctogether.com/CDH or call 1.866.438.5651.
©2011 United HealthCare Services, Inc. Insurance coverage provided by or through UnitedHealthcare Insurance Company or its affi liates. Administrative services provided by or through UnitedHealthcare Insurance Company, United HealthCare Services, Inc. or their affi liates. Health plan coverage provided by or through a UnitedHealthcare company.
UHCEW506202-001
Grow Healthy.
Engaging consumers to make informed health care decisions