Orbital schwannoma: correlation of magnetic resonance imaging and pathologic findings
-
Upload
kaan-guenduez -
Category
Documents
-
view
212 -
download
0
Transcript of Orbital schwannoma: correlation of magnetic resonance imaging and pathologic findings

Received: 23 October 2002Revised: 27 March 2003Accepted: 27 March 2003Published online: 18 June 2003© Springer-Verlag 2003
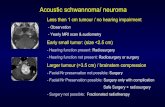
Abstract Purpose: To report thecorrelation between magnetic reso-nance imaging (MRI) findings andhistopathology of orbital schwanno-mas. Methods: This study is a retro-spective noncomparative intervent-ional case series of three consecu-tive patients with orbital schwanno-ma. After preoperative MRI, all patients underwent orbitotomy andtumor removal. Histopathologic andimmunopathologic studies of the excised tumors were performed. Themain outcome measures were MRIfeatures, histopathology, and theirrelationship to the cohesiveness ofthe tumor. Results: The patients’ ages were 56 years (patient 1), 43years (patient 2), and 18 (patient 3)years. MRI demonstrated that the tu-mors were well-circumscribed, in-traconal in patient 1, superior extra-conal in patient 2 and inferotempo-ral extraconal in patient 3. The tu-mor in patient 1 had a partly cavi-tary appearance, while the tumors inpatients 2 and 3 had a solid appear-ance on MRI. The tumor had hetero-geneous signal intensity in patients1 and 2 and homogeneous signal in-tensity in patient 3 on T2-weightedimages. All patients underwent orbi-
totomy and tumor removal. In pa-tients 1 and 2, the tumor was gelati-nous and fragmented during remov-al. The fragments were completelyexcised in patient 1 and an incom-plete piecemeal tumor excision wasmade in patient 2. In patient 3, com-plete excision without fragmentationwas performed. Pathologic examina-tion revealed that the tumor was ofAntoni B pattern in patient 1, mixedAntoni A and B patterns in patient2, and marked Antoni A pattern inpatient 3. At a mean follow-up of23.7 months (range: 22–26 months)after surgery, all patients retainedpreoperative visual acuity. Patient 2developed recurrence at 21 monthsfollow-up and underwent Krönleinorbitotomy for excision of the recur-rent tumor. Conclusions: MRI isuseful in depicting both the anatomiclocation and internal consistency of orbital tumors. Schwannomaswith MRI evidence of cavitarychange or heterogeneous signal in-tensity on T2-weighted images werefound to have marked Antoni B pattern on histopathology, impartinga friable structure and fragmentedexcision.
Graefe’s Arch Clin Exp Ophthalmol(2003) 241:593–597
DOI 10.1007/s00417-003-0681-1
S H O RT C O M M U N I C AT I O N
Kaan GündüzCarol L. ShieldsIlhan GünalpEsra ErdenJerry A. Shields
Orbital schwannoma: correlation of magneticresonance imaging and pathologic findings
Introduction
Schwannoma (neurilemoma) is a peripheral nerve tumorthat can occasionally occur in the orbit [13]. This tumoris composed primarily of Schwann cells; hence, the term
schwannoma has been preferred over neurilemoma.Schwannoma is associated with neurofibromatosis in2–18% of cases [10, 12].
Orbital schwannoma typically presents as a well-cir-cumscribed mass located in an intraconal or extraconal po-
K. Gündüz (✉)G.M.K. Bulvarı 116/3,06570 Maltepe, Turkeye-mail: [email protected]: +90-312-2291812
K. Gündüz · I. GünalpOncology Service, Department of Ophthalmology,Ankara University Faculty of Medicine,Ankara, Turkey
C. L. Shields · J. A. ShieldsOncology Service, Wills Eye Hospital,Thomas Jefferson University,Philadelphia, Pennsylvania, USA
E. ErdenDepartment of Pathology,Ankara University Faculty of Medicine,Ankara, Turkey

sition. Rarely, orbital schwannoma can present as an intra-muscular [2] or epibulbar [7] tumor and demonstrate ex-tension through the superior orbital fissure into the cavern-ous sinus [14]. This neural tumor may induce orbital pain.
Orbital schwannoma generally arises from the sensorybranches of the ophthalmic division of the trigeminalnerve. The supraorbital and supratrochlear nerves are morecommonly affected than the infraorbital nerve [3, 9, 12].Rarely, schwannoma can develop from one of the motornerves such as the oculomotor or ciliary nerves [11].
The purpose of this report is to describe correlationsbetween magnetic resonance imaging (MRI) findingsand histopathologic findings in 3 cases of orbitalschwannoma.
Materials and methods
This study is a retrospective noncomparative interventional caseseries of 3 consecutive patients with orbital schwannoma managedbetween April 2000 and May 2001 by one of us (K.G.). The patients underwent ophthalmic examination including visual acui-ty, pupillary light reactions, Hertel exophthalmometry, intraocularpressure, slit-lamp biomicroscopy, and funduscopy.
After preoperative MRI was obtained, the patients underwentorbitotomy and the tumors were totally excised. The diagnosis ofschwannoma was established histopathologically. Immunohisto-chemical staining with S-100 protein was employed to verify thediagnosis.
The patients returned for follow-up at 10 days for suture removal and again 1 month after the operation. Examinations weremade at 3- to 6-month intervals thereafter.
Results
Patient demographics and preoperative tumor featuresdemonstrated by MRI are shown in Tables 1 and 2. Noneof the patients had neurofibromatosis. MRI showed thetumor as well-circumscribed in all three cases. The shapeof the tumor was oval in patient 1 (Fig. 1a), fusiform in
patient 2 (Fig. 2a), and round in patient 3 (Fig. 3a) (Table 2). In all cases, schwannoma was isointense withrespect to the extraocular muscle and cerebral gray mat-ter on T1-weighted images (Fig. 3a), hyperintense onT2-weighted images (Figs. 1b, 2b, 3b), and showed mod-erate contrast enhancement (Figs. 1a, 2a) (Table 2). Thetumor in patient 1 had a cavitary appearance (Fig. 1a)with thin fibrous septa extending across the cavitation.The tumors in patients 2 and 3 had a solid appearance onMRI. The tumor had heterogeneous signal intensity inpatients 1 and 2 (Figs. 1b, 2b) and homogeneous signalintensity in patient 3 (Fig. 3b) on T2-weighted images.
Table 3 lists the surgical approach, pathology, follow-up, complications, and final status. Patient 2 underwent or-bitotomy with superolateral eyelid crease approach and pa-tients 1 and 3 had orbitotomy with inferotemporal orbitalrim approach. The tumors in patients 1 and 2 were gelati-nous in consistency, discohesive, and fragmented duringremoval. The tumor in patient 1 was nevertheless totallyexcised. In patient 2, an incomplete piecemeal tumor exci-sion was carried out. The tumor in patient 3 was cohesiveand totally excised within its capsule. During surgery, thenerve of origin was identified as the supraorbital nerve inpatient 2. In the other cases, the nerve of origin could notbe identified. There were no intraoperative complications.
Grossly, the schwannomas were well-circumscribedand were yellow–gray. Histopathologic examinationshowed that the encapsulated tumor was composed ofcells with eosinophilic cytoplasm having indistinct cellborders and oval nuclei. The nuclei formed either solidstructures (Antoni A pattern) or were arranged in a loosemyxomatous background (Antoni B pattern). In the Antoni A pattern, the nuclei formed palisading and occa-sional tangles of fibrillary processes called Verocay bod-ies. The schwannoma had slightly more Antoni B por-tions than Antoni A portions in patient 1 (Fig. 1c),equivalent Antoni A and B portions in patient 2 (Fig. 2c)and greater Antoni A than Antoni B portions in patient 3
594
Table 1 Patient demographicsand pertinent clinical featuresin three patients with orbitalschwannoma
Patient Age (years), sex Involved side Proptosis Motility restriction Pain
1 56, female Left 7 mm All positions Absent2 43, female Right 2 mm Upgaze Present3 18, female Right 0 None Present
Table 2 Tumor features on MRI of three patients with orbital schwannoma (+ present, − absent)
Patient Location Shape T1-Wa T2-Wa Contrast Cavitary enhancement change
1 Intraconal Oval Isointense Hyperintense, heterogeneous Moderate +2 Superior extraconal Fusiform Isointense Hyperintense, heterogeneous Moderate −3 Inferotemporal extraconal Round Isointense Hyperintense, homogeneous Moderate −
a Tumor signal intensity with respect to the extraocular muscle and cerebral gray matter on T1-weighted (T1-W) and T2-weighted (T2-W) images

Postoperatively, patient 2 developed 2 mm of blepha-roptosis and transient sensory deficit in the upper eyelidskin area. Tumor recurrence was noted in the same patient at 21 months follow-up after initial surgery. Sheunderwent Krönlein orbitotomy for excision of the recur-rent tumor. After the second operation, she developedcomplete blepharoptosis. At a mean follow-up of23.7 months (range 22–26 months) after surgery, all pa-tients retained preoperative visual acuity.
Discussion
Schwannoma has a predilection for the head, neck, andflexor surfaces of the upper and lower extremities. It fre-quently arises from the peripheral nerves located in theseanatomical sites. Pain and neurological symptoms arerare unless the tumor becomes large [4]. Schwannomagenerally occurs as a solitary lesion but it can be multi-ple and occur in the setting of neurofibromatosis [4].Schwannoma is uncommon in the orbit. In a review of645 histopathologically proven orbital tumors, schwan-noma accounted for <1% [13].
Orbital schwannoma generally develops in young tomiddle-aged adults [2, 3, 7, 9, 12, 14]. The ages of ourpatients ranged from 18 to 56 years. Schwannoma oc-curred as an intraconal orbital tumor in one patient andas an extraconal tumor in two patients in our series. Theclinical presentations of orbital schwannoma were allud-ed to previously in the introduction.
There have been few reports on the MRI findings oforbital schwannoma [1, 3]. In our series, MRI showedthe tumor to be well-circumscribed, isointense with re-spect to the extraocular muscle and cerebral gray matteron T1-weighted images, hyperintense on T2-weightedimages with moderate contrast enhancement. However,other MRI features contributed information regarding theinternal consistency of the mass. The tumors in patients1 and 2 showed a heterogeneous signal intensity on T2-weighted images corresponding to the myxoid changeswithin the tumor, that appeared to correlate with AntoniB pattern. These portions displayed greater water contentand thus demonstrated a higher signal intensity on T2-weighted images than the more cellular (Antoni A pat-tern) regions of the tumor [3].
Schwannomas can undergo central necrosis and devel-op a cavitary appearance on MRI. Rarely, an orbital
595
Fig. 1a–c A 56-year-old woman with left orbital schwannoma.a T1-weighted contrast-enhanced sagittal MRI demonstrating theintraconal schwannoma with central cavitary changes. b T2-weighted coronal MRI demonstrating the intraconal schwannomahyperintense to the extraocular muscle and cerebral gray matter.The central cavitary portion has a higher signal intensity than theperipheral solid portion of the tumor. c Histopathologic examina-tion shows that the tumor is composed predominantly of Antoni Bpattern with some Antoni A areas (hematoxylin–eosin, ×200)
(Fig. 3c) (Table 3). The heterogeneous appearance onT2-weighted images in patients 1 and 2 was found tocorrelate with the myxoid changes and Antoni B patternin the tumor. All patients demonstrated positive immuno-reactivity with S-100 protein.

596
Fig. 2a–c A 43-year-old woman with right orbital schwannoma.a T1-weighted axial MRI demonstrating the superiorly locatedschwannoma with moderate enhancement after contrast injection.b T2-weighted axial MRI showing the schwannoma hyperintenseto the extraocular muscle and cerebral gray matter. Antoni B por-tions demonstrate a higher signal intensity due to increased watercontent. c The tumor is composed of Antoni A and Antoni B pat-terns in roughly equal proportions (Hematoxylin–eosin, ×200)
Fig. 3a–c An 18-year-old woman with right orbital schwannoma.a T1-weighted axial MRI showing the round extraconal schwan-noma isointense to the cerebral gray matter. b T2-weighted coro-nal MRI showing the extraconal schwannoma hyperintense to thecerebral gray matter. c The tumor is composed primarily of AntoniA pattern with palisading of the nuclei (Hematoxylin–eosin, ×40)

schwannoma can undergo complete central cavitation withonly a thin rim of tumor tissue remaining in the periphery[6, 15]. Under these circumstances, the schwannoma maygive the false impression of a cystic orbital mass. The tu-mor in patient 1 had a partially cavitary appearance withfibrous septa extending across the cavitation. It is uncom-mon to see cavitary changes in orbital tumors. Other tumors that may exhibit cavitary change besides schwan-noma include inflammatory lesions, cavernous hemangio-ma, adenoid cystic carcinoma, rhabdomyosarcoma, andlymphangioma [5]. The presence of a cavitary tumor out-side the lacrimal gland fossa in an adult orbit should raisea high index of suspicion for orbital schwannoma.
The tumors in patients 1 and 2 were fragmented dur-ing removal. Based on the MRI and pathologic observa-tions from our series, tumors with cavitary change (patient 1) and extensive Antoni B areas (patient 2) ap-pear to be gelatinous and difficult to excise intact. Fromthis report, it is our impression that preoperative MRI isimportant in predicting the surgical challenge. Those tu-mors with MRI evidence of cavitation or heterogeneoussignal on T2-weighted images should be exposed widely
and gently removed as they tend to be gelatinous with amore friable capsule.
Although orbital schwannoma is benign, total excisionis advised to prevent recurrence and the rare malignanttransformation [8, 9, 12]. In one series, there was no re-currence after incomplete excision of 6 orbital schwanno-mas at a median follow-up of 2.8 years after surgery [9].However, incomplete excision of the tumor in one of ourpatients led to tumor recurrence within 2 years after ini-tial surgery. Although malignant transformation is rare,incomplete excision of orbital schwannoma demonstratedlate recurrence and malignant transformation in one caseof a patient with neurofibromatosis [10].
In summary, MRI is useful in depicting both the ana-tomic location and internal consistency of orbital tumors.Schwannomas with MRI evidence of cavitary change orheterogeneous signal intensity on T2-weighted imageswere found to have marked Antoni B pattern on histopa-thology and a friable structure leading to fragmented ex-cision at surgery. An incomplete piecemeal tumor exci-sion under these circumstances may lead to tumor recur-rence.
597
Table 3 Treatment features, pathology, follow-up, and patient status in three patients with orbital schwannoma (IT orbitotomy with in-ferotemporal orbital rim approach, ST orbitotomy with superotemporal skin crease approach)
Patient Surgery Pathology Postoperative Follow-up Recurrencecomplications
Capsule Antoni pattern Verocay bodies S-100
1 IT Present Antoni B>A Absent + None 23 mos No2 ST Present Antoni B=A Present + 2 mm ptosis 26 mos Yesa
Sensory deficit3 IT Present Antoni A>B Present + None 13 mos No
a The patient developed recurrence at 21 months follow-up and underwent Krönlein orbitotomy for excision of the recurrent tumor
References
1. Abe T, Kawamura N, Homma H,Sasaki K, Izumiyama H, Matsumoto K(2000) MRI of orbital schwannomas.Head Neck Radiol 42:466–468
2. Capps DH, Brodsky MC, Rice CD,Mrak RE, Glasier CM, Brown HH(1990) Orbital intramuscular schwan-noma. Am J Ophthalmol 110:535–539
3. Carroll GS, Haik BG, Fleming JC,Weiss RA, Mafee MF (1999) Peripheral nerve tumors of the orbit.Rad Clin North Am 37:195–202
4. Enzinger FM, Weiss SW (1995) Soft tissue tumors, 3rd edn. Mosby, St Louis
5. Fetkenhour DR, Shields CL, Chao AN,Shields JA, Guterman CB, Eagle RC Jr(2001) Orbital cavitary rhabdomyosar-coma masquerading as lymphangioma.Arch Ophthalmol 119:1208–1210
6. Lam DSC, Ng JSK, To TAF, AbdullahV, Liew CT, Tso MOM (1997) Cysticschwannoma of the orbit. Eye11:798–800
7. Marc’hadour FL, Romanet JP, Fdili A,Peoc’h M, Pinel N (1996) Schwanno-ma of the bulbar conjunctiva. ArchOphthalmol 114:1258–1260
8. Rootman J, Goldberg C, Robertson W(1982) Primary orbital schwannomas.Br J Ophthalmol 66:194–204
9. Rose GE, Wright JE (1991) Isolatedperipheral nerve sheath tumours of theorbit. Eye 5:668–673
10. Schatz H (1971) Benign orbital neuri-lemmoma: sarcomatous transformationin von Recklinghausen’s disease. ArchOphthalmol 86:268–273
11. Shen WC, Yang DY, Ho WL, Ho YJ,Lee SK (1993) Neurilemmoma of theoculomotor nerve presenting as an orbital mass: MR findings. AJNR14:1253–1254
12. Shields JA (1989) Diagnosis and management of orbital tumors. Saunders, Philadelphia
13. Shields JA, Bakewell B, AugsburgerJJ, Flanagan J (1984) Classificationand incidence of space-occupying lesions of the orbit. Arch Ophthalmol102:1606–1611
14. Shields JA, Kapustiak J, Arbizo V,Augsburger JJ, Schnitzer RE (1986)Orbital neurilemoma with extensionthrough the superior orbital fissure.Arch Ophthalmol 104:871–873
15. Tsuzuki N, Katoh H, Ohnuki A, Ishihara S, Miyazawa T, Nawashiro H,Shima K (2000) Cystic schwannoma of the orbit: Case report. Surg Neurol54:385–387