North Dakota Medicine Fall 2008
-
Upload
university-of-north-dakota-school-of-medicine -
Category
Documents
-
view
226 -
download
0
description
Transcript of North Dakota Medicine Fall 2008

UND athletics, medical school team up for Division I
Improving the quality of hospital care in North Dakota
Life in the lab: There’s no substitute for experience
Fall 2008VOLUME 33, NUMBER 4www.ndmedicine.org

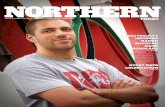
THE UNIVERSITY OF NORTH DAKOTA SCHOOL OF MEDICINE AND HEALTH SCIENCES ISplaying an integral part in UND’s five-year transition to Division I sports.
“You bet, a top sports medicine and athletic training program is an essential ingredientin successful Division I athletics,” says UND athletic director Brian Faison. “And my
experience around the country tells me that at UND, we have one of the very bestand truly unique sports medicine-athletic training programs.”
For Division of Sports Medicine Director Steve Westering, MA, ATC (BSAT ‘94),that’s welcome reassurance but not really a surprise.
“Since the inception of the current program in 1991, we have tried to providequality education and service,” says Westereng, who also is the principal athletic
trainer for UND football. He notes that the mission of the Division of SportsMedicine—which is part of School of Medicine’s Department of Family and
Community Medicine—is to serve the region through provision of education,research and service in sports medicine.
“We recognize that sports medicine is a multidisciplinary field involving many facets ofthe health care community,” Westereng says. The Division provides direction for the
Bachelor of Science in Athletic Training degree program, a fourth-year medical elective insports medicine, and residency training in sports medicine. Service components of the
Division are handled through the athletic training services provided for UND athletics and theCenter for Sports Medicine, a clinical practice in sports medicine for student-athletes as well as the
general public. Research and continuing education are vital aspects of the Division to improve thequality of care for athletes regionwide.
UND athletics, medical school
DIVISION IDepartment of Family and Community Medicine’s
Division of Sports Medicine scores big with athletes, coaches
team up for
NORTH DAKOTA MEDICINE Fall 2008 5
Pictured from left: Division of Sports Medicine Director Steve Westering,MA, ATC (BSAT ‘94), and UND Athletic Director Brian Faison

47
1015
16
POSTMASTER: Send address corrections to:ND Medicine Address Correction UND School of Medicine and Health SciencesOffice of Administration and Finance Attn: Kitty Monley501 North Columbia Rd. Stop 9037,Grand Forks, ND 58202-9037 e-mail: [email protected] phone: 701-777-2431
NORTH DAKOTA MEDICINE and past issues of THE REVIEW are available at www.ndmedicine.org
FEATURESUND Athletics and Medical School Team Up for Division I 4
Sports medicine program plays a key role in UND’s strategy to move to Division 1
Life in the Lab 7Students gain practical research experience working withaccomplished biomedical investigators
Improving the Quality of Hospital Care in North Dakota 10Network leverages valuable resources to strengthen North Dakota’s 34 rural hospitals
Life on the Cutting Edge 15Successful alum shares what makes him tick in thefast-paced world of reconstructive and plastic surgery
Match Day: Moving on for Residency 16Family medicine is the most popular choice of Doctor of Medicine (MD) ‘08 grads
DEPARTMENTSStudent Profile 12Guest Columnist 14News Briefs 20Alumni Notes 27In Memoriam 29Planning Ahead 30Parting Shots 31
NORTH DAKOTA MEDICINE
UNIVERSITY OF NORTH DAKOTA SCHOOL OF MEDICINE AND HEALTH SCIENCES
ROBERT O. KELLEY, President, University of North Dakota
H. DAVID WILSON, Vice President for Health Affairs Dean, School of Medicine and Health Sciences
EDITOR Juan PedrazaWRITERS Andrea Herbst, Pamela Knudson,
Pat Miller, Gary Niemeier, Wendy Opsahl, Juan Pedraza
CONTRIBUTORS Shelley PohlmanGRAPHIC DESIGN Laura Cory, John Lee, Victoria Swift PHOTOGRAPHY Laura Cory, Pat MIller, Wanda WeberCOVER ART Wanda Weber
www.ndmedicine.orgDESIGN Eric Walter
Laura Cory
NORTH DAKOTA MEDICINE (ISSN 0888-1456; USPS077-680) is published five times a year (April, July,September, December, February) by the University ofNorth Dakota School of Medicine and Health Sciences,Room 1000, 501 N. Columbia Road Stop 9037, GrandForks, ND 58202-9037. Periodical postage paid at Grand Forks, ND.
Printed at Fine Print Inc., Grand Forks, ND.
All articles published in NORTH DAKOTA MEDICINE,excluding photographs and copy concerning patients, canbe reproduced without prior permission from the editor.
Want more NORTH DAKOTA MEDICINE?Look for this symbol, and check out our WEB EXCLUSIVES site:www.ndmedicine.org
In the Summer ‘08 issue of ND MEDICINE (page 27), information about John Eickman,MD ‘04, and R.J. Moen, MD ‘00, was incorrect. Please see Alumni Notes in this issuefor the correct text.
NORTH DAKOTA MEDICINE Fall 2008 3

4 NORTH DAKOTA MEDICINE Fall 2008

THE UNIVERSITY OF NORTH DAKOTA SCHOOL OF MEDICINE AND HEALTH SCIENCES ISplaying an integral part in UND’s five-year transition to Division I sports.
“You bet, a top sports medicine and athletic training program is an essential ingredientin successful Division I athletics,” says UND athletic director Brian Faison. “And my
experience around the country tells me that at UND, we have one of the very bestand truly unique sports medicine-athletic training programs.”
For Division of Sports Medicine Director Steve Westering, MA, ATC (BSAT ‘94),that’s welcome reassurance but not really a surprise.
“Since the inception of the current program in 1991, we have tried to providequality education and service,” says Westereng, who also is the principal athletic
trainer for UND football. He notes that the mission of the Division of SportsMedicine—which is part of School of Medicine’s Department of Family and
Community Medicine—is to serve the region through provision of education,research and service in sports medicine.
“We recognize that sports medicine is a multidisciplinary field involving many facets ofthe health care community,” Westereng says. The Division provides direction for the
Bachelor of Science in Athletic Training degree program, a fourth-year medical elective insports medicine, and residency training in sports medicine. Service components of the
Division are handled through the athletic training services provided for UND athletics and theCenter for Sports Medicine, a clinical practice in sports medicine for student-athletes as well as the
general public. Research and continuing education are vital aspects of the Division to improve thequality of care for athletes regionwide.
UND athletics, medical school
DIVISION IDepartment of Family and Community Medicine’s
Division of Sports Medicine scores big with athletes, coaches
team up for
NORTH DAKOTA MEDICINE Fall 2008 5
Pictured from left: Division of Sports Medicine Director Steve Westering,MA, ATC (BSAT ‘94), and UND Athletic Director Brian Faison

The UND Athletic Training Program, apart of the Division of Sports Medicine, “was the first undergraduate athletictraining program in the country to belocated in a medical school,” Westerengnotes. “We’re also actively involved inthe education of family practiceresidents in the area of sports medicine.”
As the University’s athletics enter thenew era of Division I across the board(UND men’s and women’s hockey arealready Division I programs), the medicalschool’s sports medicine program islikewise preparing for some changes.
“We’ve already started recruiting andhiring additional staff to tackle our newDivision I-related needs,” Westerengsays. That’s basically building on asports medicine and athletic trainingprogram with a well-grounded reputation.The Task Force report on the Division Imove indicated that UND alreadymatched up well with Division Iinstitutions in various key measures,such as the number of sports UNDoffers, the quality of facilities availableto UND athletes, and the supportsystems—including sports medicine—that UND already has in place.
UND has highly successful athleticprograms. In addition to seven nationalchampionship titles in men’s hockey(only one other institution has more),UND has won national championshipsin football and women's basketball andhas a nationally recognized reputationin other sports, as well. UND’s student-athletes have earned a combined 3.0 orhigher grade point average in 16 of thelast 17 semesters.
“The move to Division I means a muchhigher level of commitment, forexample, more scholarships forathletes,” he notes. “It’s going to take usfive years to get through this process.”
Westereng says the sports medicineprogram is fully ready for the transitionto Division I.
“With regard to football, for example,in Division I, every workout, everygame, needs be covered (by an athletictrainer),” he says. “Our program aims toprovide the best, most comprehensivecoverage that we can—we aim to takecare of our student-athletes at a range ofpractice sessions and games. We haveto prepare ourselves to meet thisDivision I transition and its higherexpectations.”
“I have been a football trainer for nineyears, and I oversee all the trainers inthe other sports,” Westereng says.“Right now we have nine faculty, andtogether we teach 41 credits throughoutthe year; seven of us are service-oriented, and five of us are with athleticteams. We’re going to expand that.We’re unique in that we’re all in onehouse, in the medical school.”
Faison says a top-notch sports medicineprogram is essential to drawing high-caliber student-athletes to the school.
“The availability of a program like thisis an integral part of the recruitmentpackage,” he explains. “And we’veabsolutely got one of the best sportsmedicine programs going. Student-athletes and their parents want to besure that you’ve got the kind ofacademic support and athletic trainingsupport that you need to have. Wehope that nobody ever gets hurt, butthe reality is that injuries happen, andfolks want to know that they’re going toget the best care and treatment that’sout there—and that’s what we offerhere at UND.”
Faison says coaches also look to thesports medicine program on campus.
“Because of our highly specializedsports medicine program, we’re goingto get our athletes back as soon as it’ssafe and reasonable to have themback,” Faison says.
—Juan Pedraza
“We’re uniquein that we’re allin one house, in
the medicalschool.”
6 NORTH DAKOTA MEDICINE Fall 2008

PPORTUNITIES FOR UNDERGRADUATES TO GAIN RESEARCH EXPERIENCE AT THE SCHOOL OF MEDICINEand Health Sciences have never been better. This past summer, the addition of three new programs for
undergraduates enabled more than 40 students to work in the lab with researchers. Studies included those focusedon more effective drugs to treat epilepsy, potential breakthroughs in preventing Parkinson’s and Alzheimer’s diseases, thehealth effects of heavy metals in the environment, and the use of biomarkers to diagnose different types of cancer.
There’s no substitutefor experience
Undergraduate students and their mentors in the Department of Pathology are from left: Tom Botsford, Grand Forks; Kathryn Carlson,Brookings, SD; Assistant Professor Seema Somji; Assistant Professor Scott Garrett; Caitlin Johnson, Grand Island, NE; Ryan Zahn,Bottineau, ND; and Robin Johnson, Bismarck.
Life inthelab
NORTH DAKOTA MEDICINE Fall 2008 7
O

The undergraduate research programsnot only provide a valuable source ofpaid labor for researchers, but they alsogive students insights that help themplan their careers.
“Part of the reason I wanted to go intomedicine is because I like the sciencebehind it,” said Jenna Wald, fromDickinson, ND, a senior biology majorwho spent her summer working in aDepartment of Pharmacology,Physiology and Therapeutics lab.
“There are physicians who do researchin addition to practicing medicine,” sheexplained. “I'm looking at incorporatingresearch into my career as an option formy future.”
While some students decide that life inthe lab isn’t for them, others decide thatit’s exactly what they want.
“Students, when they’re going to schooland taking science classes, interpretwhat the field is like based on whatthey’re getting in the classroom,” notedScott Garrett, PhD, an assistantprofessor of pathology who serves as amentor to the undergrads.
“The lab is what the environment isreally like. You’re giving themopportunities to test the water,” he said.Megan Fettig, Bismarck, ND, a seniormajoring in biology, chemistry andsecondary education, thought shewould go into teaching after graduating.But participating in a research projectchanged her mind.
“Part of my reason for not wanting togo to graduate school was that in thefuture, I wanted enough time for familyand kids,” she said. “Doing researchand being exposed to women rolemodels – seeing how they handledthings and how it can be done – wasreally valuable.”
An undergraduate might start out byperforming such menial tasks aswashing glassware or restockingsupplies, but there can be great rewardsfor those who stick with it.
“Students can significantly contribute toa lab and an experiment,” said SeemaSomji, PhD, an assistant professor ofpathology and an undergraduatementor. “They’ve learned the basics.They know how an experiment goes.
“All these students can go back into alab and really work on a project,” shesaid. “They have a head start comparedto other students.”
That can lead to having their names ona published paper, which helps buildan impressive curriculum vitae, Somjinoted.
Ryan Zahn, Bottineau, ND, a seniormajoring in biology, chemistry andmusic, hasn’t decided whether hewants to go to medical school orgraduate school. The opportunity toconduct research is what attracted himto an undergraduate program.
“We each have our own specificproject that we work on,” he said. “Weget actual lab experience. We doeverything ourselves. We runexperiments. We analyze the data. It’sbeen great and it’s helped me a lot.” Whether Zahn ends up in a doctor’scoat or a lab coat, he’ll have the benefitof firsthand experience to help him decide on a career path.
—Patrick Miller
8 NORTH DAKOTA MEDICINE Fall 2008
“The lab is what the environment is really like. You’re giving them opportunities to test the water.”

NORTH DAKOTA MEDICINE Fall 2008 9
Jenna Wald, a senior biology major from Dickinson, ND, hopes to combine careers by practicing medicine and conducting research.

OVER THE PAST FEW YEARS, Acouple of major studies have shown,and the Institute of Medicine hasemphasized, that the quality of healthcare in America is not even close tothe level that we should expect fromthe world's most expensive healthcare system. Problems with quality arepervasive throughout both outpatientand inpatient settings and may beresponsible for thousands of deathseach year.
Small rural hospitals are no exceptionin the continual reach toward a better,safer system, but they are at timesforgotten both in terms of theircontribution to health care andfunding needed in order to maintainaccess to care for the country’s 59million rural residents. Small ruralfacilities are faced with manysignificant challenges, the mostpressing today related to finance andworkforce issues. Despite these
challenges, North Dakota’s small ruralhospitals are committed to providingquality care and have worked togetherto develop something innovative, notto mention smart. Seeing strength innumbers, they banded together toform a single network committed tosharing the effort to improve qualitythroughout the state.
The new Critical Access Hospital(CAH) Quality Improvement Network
Hospital Care
10 NORTH DAKOTA MEDICINE Fall 2008
Improving the Quality of
in North Dakota

(QIN) is a long and official way ofsaying the hospitals partnered togetherfor a stronger voice. Supported by theNorth Dakota Medicare Rural HospitalFlexibility (Flex) Program and the NorthDakota Small Hospital ImprovementProgram (SHIP), the Network isadministered through the Center forRural Health at the University of NorthDakota School of Medicine and HealthSciences.
North Dakota’s 34 small rural hospitalshave been working toward thenetwork’s development over the pastyear, under direction from an executivecommittee. A full-time coordinator,Jody Ward, Minot, ND, acts as aclearinghouse for information,regulations and requirements for thesehospitals, effectively saving theindividual facilities a notable amount oftime. She provides technical assistancethroughout the state and serves as aliaison to stakeholders.
“The network is a valuable platform tomake new connections with each otherand maintain continuity among ruralhospitals in North Dakota,” said Ward.Representatives on the network areusually risk managers, quality expertsand nurses. The goal of the group is notto discuss specific cases but largerthemes and issues.
“We want to use best practices aroundthe country to compare to internal datagathered by our facilities, and thenexceed national standards,” Ward said.
The hospitals are using the newnetwork to ensure they are providingthe highest quality of care for ruralresidents while leveraging limitedresources across communities.Hospitals have access to a variety ofstate and federal experts in a number offields, as well as education and trainingfor staff. New employees will be pairedwith mentors to help with theacclimation process. The network actsas a collective voice for small hospitalsthroughout the state.
What’s driving the quality movement?According to David Pate, MD, CEO ofSt. Luke’s Episcopal Hospital inHouston, TX, the Institute of Medicine(IOM) and Institute for HealthcareImprovement have increased bothpatient and hospital awareness of the
importance of ensuring quality. St.Luke’s is considered a leader inpromoting clinical excellence.
“When IOM tried to quantify thenumber of patients who die each yearin hospitals due to the consequences oftheir care, I think that really hit home,”said Pate. “The field had to face up tothe fact that care is not as safe as itcould be and that our outcomes are notas good as they could be. The publicand policymakers want to know whywe spend so much money on healthcare and don’t have the qualityoutcomes that other countries have.What we pay and what we receive inreturn are driving forces.”
Closer to home, an advisory committeedrives the quality movement for thenetwork. The committee includesrepresentatives from the Center forRural Health, North Dakota HealthcareReview, Inc., North Dakota HospitalAssociation, and North DakotaDepartment of Health, along with largerhospitals which work collaborativelywith small hospitals in their region.
“The new network will bridgeknowledge and expertise across healthsystems,” said Marlene Miller, MSW,director of the Flex and SHIP programsat the Center for Rural Health at theUND School of Medicine and HealthSciences. “We are leveraging eachother as resources to strengthenhealth care in North Dakota.”
- Wendy Opsahl
WEB EXCLUSIVE:To learn more about the new qualitynetwork, visit :www.ndmedicine.org
“We are leveraging each other as resources to strengthen health care
in North Dakota.”
NORTH DAKOTA MEDICINE Fall 2008 11

STUDENT PROFILE
12 NORTH DAKOTA MEDICINE Fall 2008

Firefighter to PhysicianTAKING TIME OFF BETWEENundergraduate and medical schoolturned out to be one of the bestdecisions for 31-year-old, Montana-bornKevin Sullivan, a fourth-year medicalstudent at the UND School of Medicineand Health Sciences. For six years aftergraduating from the University ofMontana, Sullivan continued a job hestarted in college: fighting wildfires.
Those years were anything but a waste,he says. They proved to beindispensable. Hand-in-hand with theblazes were lessons giving him leadershipand teamwork skills he knows arecrucial in the medical world. He had tointeract constantly not only with hiscrew and the public, but also with fire,for him a comparably living organism.His experiences with the unpredictabilityof wildfire gave him valuable insights.
“It breathes, it eats, it moves, and it’sunpredictable a lot of the time, muchlike patients. You can’t always predictwhat it’s going to do, and you have toalways be on your toes for any kind ofchange,” he says.
Although facing fires is unnerving, itgave Sullivan the ability to handle high-stress situations and to deal withdifficult people in those stressfulsituations. It all boils down to beingmentally mature.
“I thank fire big time for that, and forbeing able to step back from a processand being able to analyze it when thingsaren’t exactly the best situations as faras danger and complexity goes,” he says.
And when situations aren’t out ofcontrol? Sullivan also believes his timeoff from school will help him to betterconnect with his patients. Heunderstands going out and working
hard and sees this as a way of relatingto, and gain confidence from, patients.
He’ll never regret his choice tocontinue firefighting for those six years,but has always known medicine wasthe career for him. The WesternInterstate Commission for HigherEducation (WICHE) program gave himthe chance to achieve it. Like otherstudents from states without medicalschools, Sullivan hoped for one of thefew non-resident spots available inother states’ medical programs.
He wasn’t let down. The UND medicalschool accepted him through WICHE,and he was glad, because the patient-centered learning program at UNDturned out to be more beneficial thanwhat many of his friends experienced atlecture-based medical schools.
Although originally intending tobecome an orthopedic surgeon, Sullivannow plans to pursue anesthesiology.Why? It will allow him to interact withpeople while still being hands-on byperforming procedures, two thingshe loves most.
- Andrea Herbst
from
“It breathes, it eats,
it moves, it’s unpredictable”
and
NORTH DAKOTA MEDICINE Fall 2008 13
KEVIN SULLIVANMD CLASS OF 2009HOMETOWN: Superior, MTHIGH SCHOOL: Superior
High School PARENTS: K.C. and Carol Sullivan

14 NORTH DAKOTA MEDICINE Fall 2008
GUEST COLUMNIST
Dear Friends:
When I got the call last fall asking if I would be interested in being nominated as acandidate for the presidency of the University of North Dakota, it was easy to answer“Yes.” It was easy because I already knew something about one of the jewels in theUND crown: the School of Medicine and Health Sciences. I had visited UND in thepast, thanks to my good friend Dr. Ed Carlson of UND’s Department of Anatomy andCell Biology. He had brought me to UND as the guest speaker in an anatomy seminar.
Let me share some of the impressive things that I have learned about North Dakota’smedical school:
◆ Hundreds of physicians around the state volunteer their valuable time toteach our students. That’s a unique partnership that significantly enhances thequality of our medical education. I have been impressed by our patient-centered approach to medical education.
◆ Family medicine is the single most popular choice of members of the UNDDoctor of Medicine Class of 2008. Sixteen graduates, about 27 percent of the59-member class, have elected to pursue training in family medicine, mostlyin North Dakota and other Midwestern states. That's why the School ofMedicine and Health Sciences has consistently ranked among the topmedical schools nationally for producing family physicians.
◆ I was particularly pleased to learn that the medical school produces orsponsors numerous community outreach activities in North Dakota, such asthe annual Medical School for the Public; the North Dakota Women’s HealthConnection; and Science Day, an annual event put on by first- and second-year medical students for fifth- and sixth-graders that is designed to stimulatechildren's interest in science and features a hands-on approach to learning.
◆ INMED -- Indians Into Medicine -- has a national reputation. About 20 percentof the American Indian doctors working in the United States today wereeducated through the INMED program at UND, which reserves seven spotsin each medical school class for Native Americans from around the country.
◆ Another gem in the School of Medicine and Health Sciences crown is theCenter for Rural Health, home of the Rural Assistance Center, the country'sonly national health information clearinghouse for health care professionalsand administrators.
◆ UND is becoming nationally recognized for what Sen. Byron Dorgan likes tocall “deep brain research.” The School of Medicine and Health Sciences hasattracted millions of dollars for research in such critical areas as Alzheimer'sand Parkinson's diseases.
These are just a few of the impressive and important aspects of the UND School ofMedicine and Health Sciences. The research components will continue to beimportant as we move ahead. Working together with the faculty and other partners,we will look for synergies, for ways of interconnecting our current strengths. We willbe creative, innovative, and entrepreneurial as we continue to build the bestpossible medical school for the citizens of North Dakota.
Robert O. KelleyPresident
Dr. Robert Kelley began serving asUND’s 11th president July 1, 2008
UND School of Medicine and Health Sciences:
A Jewel in the UND Crown

ALUMNI PROFILE
Allen Van Beek, MD (BS Med '66),knows that plastic surgery is a growingobsession in our image-consciousculture. But rather than performingBotox on bridesmaids, Van Beekdevoted his career to the delicate art ofreconstructive surgery.
An adjunct professor at the Universityof Minnesota with a practice in Edina,the Westfield, ND, native is a pioneerin the field of microsurgery: the use ofmicroscopes to fix nerves and bloodvessels. It's a highly-specialized skillthat helps him reconstruct the limbs —and lives — of his patients.
Although he envisioned life as a laid-back family doctor in Montana, hisexperience patching up combatants inVietnam as a flight surgeon took him ina unexpected direction. After the war,Van Beek credits friend Dennis Trzpuc,MD (BS Med '66), with leading him tothe Indiana University School ofMedicine, where he completed asurgical residency.
A New FocusThe ready supply of injured veteransspurred his interest in an emergingspecialty: microsurgery. He traveled toSan Antonio, TX, to research nerveswith expert Sidney Ochs, PhD, anddeveloped a passion for the microscope:“I loved it, and have never stoppedoperating with the microscope.”
At the time few centers formicrosurgery existed, but the nearbyUniversity of Louisville was one ofthem. Van Beek jumped at the chance,and learned a new idea: “free-flap,”whereby tissue is moved to new areasof the body. This was squarely theprovince of plastic surgery, and VanBeek’s mentor, Harold Kleinert, MD,suggested he address it. Slyly, Kleinertalready had a position in mind for hisprotégé. “I was sort of auctioned off.”
After residency training at SouthernUniversity School of Medicine inSpringfield, IL, Van Beek settled inMinneapolis, realizing his goal ofestablishing a microsurgery program. “Itwas as close to home as I could get.”
North Dakota was a formativeinfluence. As a youth, Van Beekexperienced a ‘limb trauma’ first-handwhen he fell from a tractor and brokehis leg. The most colorful aspect, hesays, was his transfer to a Bismarckhospital: “It took place in a hearse.”
His father, Lester, an auctioneer,sometimes dealt with farm animals. VanBeek decided to become a veterinarian,until a real one advised him otherwise:“Son, become a doctor.” The adviceresonated.
High ProfilesVan Beek's highest profile reattachmentcase was that of John Thompson. In1992 the Hurdsfield, ND, farm boy losthis arms to a spinning power take offshaft. Thompson eventually regainedlimited use of his hands and fingers andtoday does motivational speaking.
Even more daunting was a newbornwith missing fingers, severed during acesarean procedure. The case of KristenMeckle, of Crosby, ND, remains theyoungest successful finger replant ever.Lower-profile, but also important is hismission work through Grace Church inEden Prairie. During trips to Centraland South America, he treats defects ofthe hand and face. “These are kids whootherwise wouldn't be taken care of.”
Van Beek knows that his pioneeringand multifaceted work as a surgeon isn'tjust about limbs and faces: “We'rereally dealing with quality of life.”
- Gary Niemeier
Life on the Cutting Edge
Allen Van Beek, MD (BS Med ‘66),receives the Sioux Award, the highesthonor bestowed by the UND AlumniAssociation during Homecomingactivities in October.
NORTH DAKOTA MEDICINE Fall 2008 15

MATCH DAY
One in Four MD '08 Grads Choose Family MedicineFamily medicine is the single most popular choice of members of the UND Doctor of Medicine (MD) Class of 2008. Sixteengraduates, 27 percent of the 59-member class, have elected to pursue training in family medicine, mostly in North Dakotaand other Midwestern states. Emergency medicine, attracting eight graduates, is the second-most popular specialty, followedclosely by general surgery, with seven. Six grads chose internal medicine and another six chose pediatrics. “We are veryproud of our outstanding medical students, and very pleased that so many of them have elected to pursue medical specialtiesthat are most needed in North Dakota,” said H. David Wilson, MD, vice president for health affairs and dean of the UNDmedical school. Medical school graduates, who began training this past summer, generally pursue three to five years ofresidency training to become eligible for certification in the medical specialty of their choice. Other specialties selected byUND medical graduates of '08 are: obstetrics-gynecology (four); diagnostic radiology (three); anesthesiology (two);neurosurgery (two), and one each in dermatology, neurosurgery, plastic surgery, psychiatry and urology.
MD Class of 2008 Residency SitesNAME LOCATION PROGRAM
Anderson, Christopher Mayo School of Graduate EMERGENCYMedical Education Program MEDICINERochester, MN
Barker, Kyle UNDSMHS GENERAL Grand Forks, ND SURGERY
Batcheller, April William Beaumont Hospital OBSTETRICS/Royal Oak, MI GYNECOLOGY
Beals, Bryan Creighton-Nebraska Health PSYCHIATRYFoundation – Omaha, NE
Bolander, Nevin Kalamazoo Center for Medical EMERGENCYStudies/Michigan State Univ. MEDICINEProgram – Lansing, MI
Brantl, Rylan University of Missouri SURGERYColumbia Program (PRELIMINARY)Columbia, MO
University of Missouri NEUROSURGERYColumbia Program – Columbia, MO
Brickner, Derek Lincoln Medical Education FAMILY Partnership Program MEDICINELincoln, NE
Cawley, John Fort Collins Family Medicine FAMILY Program – Fort Collins, CO MEDICINE
Clapp, Allison UNDSMHS TRANSITIONALFargo, ND (Year 01)
Mayo School of Graduate RADIOLOGY-Medical Education Program DIAGNOSTICRochester, MN
Clauson, Ryan University of Nebraska Medical SURGERYCenter, College of Medicine Program (PRELIMINARY)Omaha, NE
University of Nebraska Medical UROLOGYCenter College of Medicine ProgramOmaha, NE
16 NORTH DAKOTA MEDICINE Fall 2008

NAME LOCATION PROGRAM
Cook-Shimanek, Margaret University of Colorado School PEDIATRICSof Medicine Children’s HospitalDenver, CO
Dahl, Brian St. Joseph Hospital Program SURGERYChicago, IL (PRELIMINARY)
Delgado, Jamael Banner Good Samaritan Medical FAMILYCenter Program - Phoenix, AZ MEDICINE
Duty, Laura University of Utah Program PEDIATRICSSalt Lake City, UT
Eckardt, Gerald Medical College of Wisconsin NEUROLOGICALAffiliated Hospital Program SURGERYMilwaukee, WI
Fenstad, Eric Mayo School of Graduate INTERNAL Medical Education Program MEDICINERochester, MN
Froelich, Joy UNDSMHS FAMILYBismarck, ND MEDICINE
Gelderloos, Irminne UNDSMHS GENERALGrand Forks, ND SURGERY
Gullickson, Nicole Siouxland Medical Education FAMILYFoundation Program MEDICINESioux City, IA
Hatlestad, Preston University of Minnesota/St. John’s FAMILYHospital Program – St. Paul, MN MEDICINE
Hegge, Ryan Southern Illinois University DIAGNOSTICProgram – Springfield, IL RADIOLOGY
Hegge, Theresa Southern Illinois University PLASTICProgram – Springfield, IL SURGERY
Hoovestol, Ryan University of Nebraska Medical INTERNAL Center, College of Medicine MEDICINEProgram - Omaha, NE
Hope, Brian University of Minnesota Medical PEDIATRICSSchool - Minneapolis, MN
Keene, David University of Illinois College of FAMILYMedicine Program/Methodist MEDICINEMedical Center – Chicago, IL
Keup, Christine University Hospital/University of OBSTETRICS/Cincinnati College of Medicine GYNECOLOGYProgram – Cincinnati, OH
Knoll, Katherine University of Missouri PEDIATRICSChildren’s Mercy HospitalKansas City, MO
Knudson, Joshua TriHealth (Good Samaritan GENERAL Hospital) Program – Cincinnati, OH SURGERY
Knudson, Richelle UNDSMHS TRANSITIONALFargo, ND (Year 01)
Mayo School of Graduate Medical DERMATOLOGYEducation Program – Rochester, MN
NORTH DAKOTA MEDICINE Fall 2008 17

NAME LOCATION PROGRAM
Knutson Bueling, Robyn University of Minnesota/ FAMILYMethodist Hospital Program MEDICINESt. Louis Park, MN
Kvamme, Corrine Synergy Medical Education EMERGENCYAlliance/Michigan State University MEDICINEProgram – Saginaw, MI
Lindgren, Christopher University of Nebraska Medical EMERGENCYCenter Program – Omaha, NE MEDICINE
Longfors, Nancy Eastern Virginia Medical School GENERAL Program – Norfolk, VA SURGERY
Longhurst, Claire Phoenix Children’s Hospital/ PEDIATRICSMaricopa Medical Center ProgramPhoenix, AZ
Magura, Lindsay Duke University Hospital Program INTERNALDurham, NC MEDICINE
McCann, Michelle Grand Rapids Medical Education OBSTETRICS/and Research Center/Michigan GYNECOLOGYState University Program Grand Rapids, MI
Miller, Jessica UNDSMHS FAMILY Bismarck, ND MEDICINE
Narloch, Jennifer University of Nebraska Medical INTERNAL Center College of Medicine Program MEDICINEOmaha, NE
Nybakken, Mary UNDSMHS FAMILYBismarck, ND MEDICINE
Ostlie, Jane Altru Health System FAMILYGrand Forks, ND MEDICINE
Pedersen, Chad Gunderson Lutheran Medical INTERNALFoundation Program MEDICINELa Crosse, WI
Peters, Shannon UNDSMHS TRANSITIONALFargo, ND (Year 01)
Mayo School of Graduate Medical ANESTHESIOLOGYEducation Program – Rochester, MN
Price, Tyler University of Nebraska School EMERGENCYof Medicine Program – Omaha, NE MEDICINE
Ranum, Joshua Altru Health System FAMILYGrand Forks, ND MEDICINE
Reisenauer, Justin Kalamazoo Center for Medical EMERGENCYStudies/Michigan State University MEDICINEProgram – Kalamazoo, MI
Roers, Stacy Altru Health System FAMILYGrand Forks, ND MEDICINE
Samaraweera, Ravinda University Hospital/University of NEUROLOGYCincinnati College of Medicine Program - Cincinnati, OH
18 NORTH DAKOTA MEDICINE Fall 2008

NAME LOCATION PROGRAM
Scherber, Holly Mayo School of Graduate Medical INTERNALEducation Program MEDICINEScottsdale, AZ
Shaffer, Andrew William Beaumont Hospital SURGERYProgram - Royal Oak, MI (PRELIMINARY)
(Year 01)
Splichal, Katherine Case Western Reserve University PEDIATRICSUniversity Hospitals of ClevelandProgram – Cleveland, OH
St. Germain, Chad Hennepin County Medical Center TRANSITIONALMinneapolis, MN (Year 01)
Creighton University Program RADIOLOGY Omaha, NE DIAGNOSTIC
Steinle, Jill University of Wisconsin Hospital OBSTETRICS/and Clinics Program GYNECOLOGYMadison, WI
Stoy, Sean University of Colorado Program SURGERYDenver, CO (PRELIMINARY)
Voigt, Matthew Medical College of Wisconsin ANESTHESIOLOGYAffiliated Hospitals ProgramMilwaukee, WI
Wagner, Todd Case Western Reserve University FAMILY University Hospitals of Cleveland MEDICINEProgram – Cleveland, OH
Welsh, Megan UNDSMHS FAMILYBismarck, ND MEDICINE
Wiest, Eric Grand Rapids Medical Education EMERGENCYand Research Center/Michigan MEDICINEState University Program Grand Rapids, MI
Wilson, Winter Altru Health System FAMILYGrand Forks, ND MEDICINE
Zimny, Matthew William Beaumont Hospital EMERGENCYProgram - Royal Oak, MI MEDICINE
NORTH DAKOTA MEDICINE Fall 2008 19
Medical students anxiously open their Match Day envelopes to discover their residency placements.

NEWS BRIEFS
UND Center for Rural Health, Fargo VAMedical Center Share $10 Million RuralHealth Resource Center ProjectThe Fargo VA Medical Center and the Center for RuralHealth at the University of North Dakota (UND) medicalschool were awarded federal funding from the U.SDepartment of Veterans Affairs to enhance health caredelivery to rural veterans and close gaps in quality andaccess to care that result from geographic isolation. Thefive-year, $10 million grant supports a new network of VAhealth care facilities and academic institutions that willwork together to develop and disseminate strategies thatoptimize care for rural veterans. The partnership includesVA hospitals and community-based clinics located in Iowa,Illinois, Nebraska, Minnesota, North Dakota and SouthDakota, as well as university partners at the UND Centerfor Rural Health, the University of Iowa, University ofMinnesota, and University of Nebraska. In addition todeveloping and disseminating strategies to optimize carefor rural veterans, the new multi-state Rural HealthResource Center will also assist the VA Office of RuralHealth in Washington, DC, in creating policies to eliminatepotential disparities in care faced by rural veterans.
The Rural Health Resource Centerdirector is Peter Kaboli, MD, MS, VAstaff physician and associateprofessor of general internalmedicine, University of Iowa; thedeputy director is Alana Knudson,PhD, associate director for researchat the UND Center for Rural Health,Grand Forks. Knudson is anaccomplished investigator andprogram leader whose researchincludes population health, quality and safety, andfinancial access for rural and frontier populations. “Whatwe discover through this Center’s projects will influencehow veteran health care is delivered across rural America,”said Knudson.
The Rural Health Resource Center will focus on identifyinggaps in rural health care and unique barriers to care facedby rural veterans and then use this knowledge to developand test innovative strategies to improve access and qualityand eliminate disparities. The funding allows the VA anduniversity research team to bring together experts in healthservices research, public health, health care policy andfinancing, and dissemination and implementation of bestpractices.
Senator Dorgan Talks Diabetes Fundingfor Native American Programs Senator Byron Dorgan (D-ND) visited with staff andstudents from the UND Center for Rural Health recently inGrand Forks regarding the importance of continued federalfunding of diabetes research, prevention, treatment andeducation. Twyla Baker-Demaray, MS, Mandan, Hidatsaand Arikara Nation; Jacque Gray, PhD, Choctaw andCherokee; Sierra Abe, Mandan, Hidatsa and ArikaraNation; Erin Martin, Turtle Mountain Band of Chippewa,and Alana Knudson, PhD, thanked Dorgan for his supportof diabetes-related funding and expressed the importanceof funding to several of the Center’s projects affiliated withNative American health. Dorgan was in Grand Forks toreceive the 2008 Congressional Leadership Award for hisleadership on extending the Special Diabetes Program(SDP) in Congress from the Juvenile Diabetes ResearchFoundation International, the American DiabetesAssociation and the National Indian Health Board (NIHB).
The SDP includes two programs – the Special StatutoryFunding Program for Type 1 Diabetes Research whichfunds type 1 diabetes research through the NIH, and theSpecial Diabetes Program for Indians (SDPI) which fundsprevention, treatment and education programs for NativeAmericans with type 2 diabetes through the Indian HealthService. Both programs have demonstrated a significantreturn on the federal investment and are transforming thelives of people with diabetes, Dorgan said.
“Diabetes is a serious problem for our tribal communities,”said Gray, assistant professor at the Center for Rural Health.“Funding is essential for continued improvement of NativeAmerican health. The federal diabetes programs are makinga positive impact, as are the Center’s.”
Dorgan has authored legislation to extend the SDP for anadditional five years, and the bill currently has 48 co-sponsors in the Senate. As chairman of the Senate IndianAffairs Committee, he has also worked to raise awarenessabout the significant progress that has been made in tribalcommunities struggling with diabetes.
“I plan to keep pushing for policies that will supportinnovative ways to deal with this disease,” Dorgan said.
“Diabetes is a serious problem that hits our AmericanIndian communities particularly hard. It’s important that wefind ways to educate the public about how to preventdiabetes and how to treat it effectively once they havebeen diagnosed.” Last year, Congress renewed the SpecialDiabetes Program for an additional year as part of theMedicare bill, and this year Dorgan is working to ensurethat Congress renews the program for an additional twoyears as part of the Medicare bill.
20 NORTH DAKOTA MEDICINE Fall 2008
Alana Knudson, PhD

NEWS BRIEFS
Medical school scientist earns major international award for pace-setting research in thebiochemistry of free-radical damageMatthew Picklo, PhD, a scientist at the University of North Dakota School ofMedicine and Health Sciences neuroscience lab, has been awarded the prestigiousinternational Esterbauer Award for 2008 for his research into the damage caused byfree radicals in the body. The award, given to one researcher worldwide every twoyears, will be presented to Picklo at an international meeting in Nagano, Japan, thisfall. “I was very surprised that I got this award, but also very pleased,” says Picklo,associate professor in the medical school’s Department of Pharmacology,Physiology and Therapeutics and adjunct professor in the UND Department ofChemistry. Picklo has been invited to present his work at the fall meeting in Japan.He studies oxidative damage to lipids, caused by what commonly are known as“free radicals,” products of normal, everyday living that accumulate with age.Usually, the body disposes of these free radicals, but this requires the presence ofantioxidants (found in popular nutritional supplements, such as vitamins E and Cand omega-three fish oil).
“Oxidative (or free radical) damage is a toxic hallmark of multiple diseasesincluding Alzheimer's disease, Parkinson's disease, diabetes, and atherosclerosis,”notes Picklo. “My laboratory studies how the brain gets rid of these toxins”produced by the action of free radicals in the body. By understanding thesepathways, we can develop potential therapeutic strategies.”
The Esterbauer Award is given by the Vienna, Austria-based International HNE-Club, an informal group of researcherswith wide interests spanning all aspects of lipid oxidation and other types of oxidation. The International HNE-Club is aGroup of Interest within the International Society for Free Radical Research.
NORTH DAKOTA MEDICINE Fall 2008 21
North Dakota Team Advises National Summit on Nursing Faculty ShortagesA team of nursing experts from North Dakota shared theirexpertise at the first Nursing Education Capacity Summit inJune at Washington, DC. Sponsored by the AARP, theRobert Wood Johnson Foundation (RWJF) and the U.S.Department of Labor (DOL), the Summit was created toidentify solutions to the nurse faculty shortage that is forcingnursing schools to turn away thousands of qualified nursingcandidates each year. Summit participants developedapproaches to improving nursing education capacity, withthe ultimate goal of reversing the persistent nursing shortagethat could leave the United States without enough nurses.North Dakota’s delegation included Jacqueline Mangnall,PhD, RN, Jamestown (ND) College; Chandice Covington,PhD, and Julie Anderson, PhD, UND College of Nursing,Grand Forks; Evelyn Orth, MSN, MMGT, RN, United TribesTechnical College, Bismarck; Jan Kamphuis, PhD,Medcenter One, Bismarck; Larry Anderson, North DakotaDepartment of Commerce, Bismarck; Jane Roggensack, MS,RN, MeritCare Health System, Fargo; Patricia Moulton,PhD, UND Center for Rural Health (CRH), Grand Forks;Constance Kalanek, RN, North Dakota Board of Nursing,Bismarck, and Linda Wurtz, AARP, Bismarck.
North Dakota is uniquely positioned to contribute to thesummit because of its commitment to team work,demonstrated best practices related to increasing the
nursing workforce, and excellent capacity to build evenmore effective partnerships for solutions in the future,according to Moulton, assistant professor at the CRH. “Thisteam comprises a well-connected, representative body ofnurses, workforce development representatives, andconsumer advocates who are fully committed toimplementing initiatives geared toward assuring that nursingeducation in North Dakota will be able to meet the growingdemand for nurses now and in the future,” said Mangnall,leader of the state’s team.
The Summit comes at a critical time for nursing, she said.Latest surveys project that the United States could fall shortby close to half a million registered nurses by 2025 withoutaggressive action. The supply of new nurses is failing tokeep pace with rising patient demand, in part because asignificant number of interested and qualified nursingschool applicants have been turned away in recent yearsdue to a growing shortage of nursing faculty.
For more information on the Nursing Education Capacity Summit, visit: http://www.ndmedicine.org

NEWS BRIEFS
Researcher Nets $1.52 Million RO1 toProbe Anxiety SecretsUND School of Medicine andHealth Sciences neuroscientistSaobo Lei, MD, PhD, has beenawarded a prestigious and highlycompetitive R01 five-year granttotaling $1.52 million by theNational Institutes of Health (NIH)National Institute of Mental Healthto study, at the cellular level, themechanisms that trigger anxiety.“Anxiety is among the most commonpsychiatric disorders and affects about 20 million Americanpeople,” says Lei, assistant professor of pharmacology,physiology and therapeutics. “Everyone at some time oranother feels anxious, sometimes enough to warrantmedical treatment. But even though there are drugs whichcan be used to treat anxiety, we are still achieving onlymodest success in treating and curing this disorder.
“It is of significant interest to further explore these anxiety-producing mechanisms in the brain,” says Lei, who grew upin central China and obtained his medical degree there. “Ofcourse, we expect our research to lead to novel and muchmore effective therapeutic strategies to deal with anxiety.”Lei’s five-year NIH RO1 grant will support severalresearchers. The Research Project Grant (R01), the originaland historically oldest grant mechanism used by NIH,provides support for health-related research anddevelopment based on the mission of the NIH.
CRH Funds Scholarships for HealthQuality Conference ParticipantsThe Center for Rural Health at the University of NorthDakota (UND) School of Medicine and Health Sciencesfunded scholarships through its SHIP program for threeNorth Dakota health professionals to attend nationalconferences on providing quality health care in ruralcommunities. Charlene Hansen, nursing services directorand quality improvement (QI) director/manager at SouthwestHealthcare Services, Bowman; Paula Brown, ADON, QI,RM, at McKenzie County Healthcare Systems, Watford City,and Jody Ward, North Dakota Critical Access HospitalQuality Improvement Network coordinator, Minot, attendedthe National Rural Health Association’s Annual Quality andClinical Conferences in July at San Diego, CA. Participationin the conferences is funded by the Small HospitalImprovement Program (SHIP) at the UND School of Medicineand Health Sciences’ Center for Rural Health in GrandForks. A goal of SHIP, a federally funded initiative sponsoredby the Office of Rural Health Policy, Health Resources andServices Administration, is to help hospitals reduce medicalerrors and support quality improvement initiatives.
Amundson Testifies on Sustainability ofRural Community Access to PhysiciansIf not for the Conrad J-1 Visa Program,a federal program which provides allstates with visa waivers forinternational physicians, “more of ourrural health care facilities all acrossthe country would be closed today,”said UND Center for Rural HealthAssistant Professor Mary Amundson,MA, in testimony recently to the U.S.House Subcommittee on Immigration,Citizenship, Refugees, Border Securityand International Law.
In her invited testimony, Amundson explained the currentstate of access to rural health care, citing statistics ondeclining rates of medical students choosing familymedicine and warnings of physician shortages. Althoughthere is a call from the Association of American MedicalColleges to increase medical school class size, “this willtake time which our fragile rural health care systems don’thave; our health care systems simply won’t survive.Immediate policy solutions to the physician shortageproblem are needed today.”
Amundson explained the importance of the Conrad State 30Improvement Act, which would address necessary changesdue to a decrease in the number of physicians enteringtraining on the J-1 Visa. It includes such reform measures asmaking the program permanent, providing increasedflexibility for states to manage the program, and creating amechanism that allows the 30-doctor-per-state cap toincrease under certain conditions.
“This is a very successful program and it is helping toaddress our needs as a nation to improve access to careamong the nation’s most vulnerable populations,”Amundson testified. “The amendments in the Conrad State30 Improvement Act are important to further improve theprogram and ensure that physicians are available to servethe nation’s underserved.”
This legislation, sponsored by Senator Kent Conrad (D-ND)in 1994, temporarily amended the Immigration andNaturalization Act to authorize state or equivalentdepartments of health to directly act as IGAs (InterestedGovernment Agencies) in support of waiver requests ofpetitioning facilities located in the state.
22 NORTH DAKOTA MEDICINE Fall 2008
Saobo Lei, MD, PhD Mary Amundson, MA

NEWS BRIEFS
Hospitals Form Network to Enhance CareThe Critical Access Hospital (CAH) Quality ImprovementNetwork (QIN) is supported by the North Dakota MedicareRural Hospital Flexibility (Flex) Program and the NorthDakota Small Hospital Improvement Program (SHIP),administered through the Center for Rural Health. NorthDakota’s 34 small rural hospitals have been working towardthe network’s development over the past year, underdirection from an executive committee. A full-timecoordinator, Jody Ward, Minot, will act as a clearinghousefor information, regulations and requirements for thesehospitals, effectively saving the individual facilities a notableamount of time. She will provide technical assistancethroughout the state and serve as a liaison to stakeholders.A registered nurse, she has experience providing support tocritical access hospitals throughout the state.
“The network will be a valuable platform to make newconnections with each other and maintain continuity amongrural hospitals in North Dakota,” said Ward. The hospitalswill use the new network to ensure they are providing thehighest quality of care for rural residents while leveraginglimited resources across communities. Hospitals will haveaccess to a variety of state and federal experts in a numberof fields, as well as education and training for staff. Newemployees will be paired with mentors to help with theacclimation process. The network will act as a collectivevoice for small hospitals throughout the state.
Executive committee members include: Cathy Swenson,chief executive officer, Nelson County Health System,McVille; Doris Vigen, director of nursing, Union Hospital,Mayville; Louise Dryburgh, chief executive officer, FirstCare Health Center, Park River; Candy Thompson, directorof nursing, St. Aloisius Medical Center, Harvey; BertSpeidel, quality improvement (QI) coordinator, SakakaweaMedical Center, Hazen; Charlene Hansen, QI coordinator,Southwest Healthcare Services, Bowman, and ShawnSmothers, chief executive officer, Trinity KenmareCommunity Hospital, Kenmare.
Assisting the network with its efforts is an advisorycommittee which includes representatives from the Centerfor Rural Health, North Dakota Healthcare Review, Inc.,North Dakota Hospital Association and North DakotaDepartment of Health, along with larger hospitals that workcollaboratively with small hospitals in their region.
“The new network will bridge knowledge and expertiseacross health systems,” said Marlene Miller, MSW, directorof the Flex and SHIP programs at the Center for RuralHealth at the UND School of Medicine and HealthSciences, Grand Forks. “We can leverage each other asresources to strengthen health care in North Dakota.”
Center for Rural Health StrengthensServices for People with Head InjuriesThe federal Health Resources and Services Administration(HRSA) has awarded the North Dakota Department ofHuman Services (DHS) a grant to strengthen thecoordination of services for individuals with traumatic braininjuries (TBI). The $118,000 award is for year 2 of a three-year project designed to help North Dakota better addressthe needs of military veterans, American Indians, and otherswith traumatic brain injuries.
DHS has partnered with the Center for Rural Health at theUND of Medicine and Health Sciences to administer theproject. The Center managed the state's original planninggrant for traumatic brain injury. Additional funding partnersinclude the Dakota Medical Foundation—which recentlyprovided $20,000 to support the North Dakota TBIPartnership the North Dakota—the Head Injury Association,and the Anne Carlsen Center.
Nationally, the Centers for Disease Control estimates abouttwo percent of the population is affected by traumatic braininjuries that disrupt the normal function of the brain. Usingthis estimate, about 12,800 North Dakotans have braininjury-related disabilities. The main causes of such injuriesinclude falls, traffic accidents and assaults.
In North Dakota, tribal injury prevention experts havehelped focus attention on brain injuries and the need toaddress the leading causes of TBI hospitalizations amongAmerican Indians. The North Dakota AdministrativeCommittee on Veterans Affairs says more soldiers aresurviving traumatic brain injuries, and understanding theirconcerns and enhancing services is important.
Grant funds will be used to improve screening and referralsfor needed services and service coordination. Other goalsinclude strengthening cultural awareness, implementing apeer mentoring pilot program involving American Indians,promoting education and awareness through a statewidesummit this fall, targeted medical education, anddeveloping a resource library. Resources may also be usedto explore ways to track the incidence of traumatic braininjuries in North Dakota.
“The Center for Rural Health has a 28-year history ofconnecting resources and knowledge to strengthen thehealth of people in rural communities,” said RebeccaQuinn, TBI program coordinator at the Center for RuralHealth. “We look forward to enhancing the delivery ofservices to individuals and their families affected bytraumatic brain injury.”
NORTH DAKOTA MEDICINE Fall 2008 23

NEWS BRIEFS
MD Class of 2012 Begins StudiesSixty-two new freshman medical students, members of theDoctor of Medicine (MD) Class of 2012, started theirjourney to become physicians in August at the UND Schoolof Medicine and Health Sciences. The students, 26 men and36 women, range in age from 21 to 37 years, with theaverage age of 24. They come to medical school with workexperience in an array of fields and academic degrees inbiology, chemistry, psychology, nutrition and dietetics,psychology, nursing, and engineering. Two students holdthe PhD degree, one has earned a law degree, and othershold master’s degrees.
“We always look forward with great anticipation towelcoming a new class,” says Judy DeMers, MEd, associatedean for student affairs and admissions. “The Class of 2012is a group of exceptional students, reflecting the highacademic standards of the UND medical school. They entermedical school with a variety of impressive health care andhumanistic activities to their credit. “It should be awonderful year.” Medical students’ first week is dedicatedto orientation, including introduction to the four-year,“patient-centered” curriculum. Special emphasis is placedon the students’ new roles and expectations of them ashealth care professionals.
Orientation concludes with the White Coat Ceremonyduring which students receive their first white coats, thephysician’s traditional garment, donated by the NorthDakota Medical Association. They recite the Oath ofHippocrates, an ancient vow to uphold basic professionalprinciples. Nicholas Neumann, MD, associate dean for theschool’s Southwest Campus, Bismarck, presented thekeynote address, “Set Your Expectations High, Serve thePeople, and Change the World.”
Dammen Scholarship Presented toOutstanding Third-year StudentMegan Miller, a third-year medicalstudent from Dickinson, ND, is thefirst recipient of the GertrudeDammen Scholarship. The scholarshipis funded by the GertrudeDammen/Allison Gentle MedicalEducation Endowment established lastyear with a $100,000 gift to the UNDFoundation from Allison and Milton“Bud” Gentle, San Antonio, TX,daughter and son-in-law of GertrudeDammen. Miller, who earned an undergraduate degree inbiochemistry and chemistry from the University ofColorado, Boulder, served as treasurer of the student sectionof the local chapter of the American Medical Associationand chair of the Pediatric Interest Group. She represents herclass on the state medical association’s Commission onMedical Services and is a member of the class’s SocialCommittee. In 2002, she received the ASCP Book Award.
The Dammen scholarship is intended for a medical studentwho has a proven record of academic achievement, thestrong potential to succeed in the future, and financial need.The scholarship will be renewed if the recipient continuesto meet scholarship criteria. Preference is given to a studentwho graduated from a North Dakota high school.
Mrs. Dammen, a native of Wisconsin, earned a degree inmusic from Augsburg College in Minneapolis and venturedto North Dakota where she taught all subjects througheighth grade in rural schools including those near Blanchardand Mayville. She and her husband, George, also a teacher,started farming in 1939 and bought a farm near Mayville in1940; the farm remains in the family.
24 NORTH DAKOTA MEDICINE Fall 2008
Foundation Grants $170,000 for Surgical Simulation LabThe Dakota Medical Foundation recently announced a grant of $170,000 to the University ofNorth Dakota School of Medicine and Health Sciences’ Department of Surgery to support thedevelopment of a simulation skills center. The center will be based at Altru Hospital in GrandForks and at the medical school’s education building in Fargo.
“The Dakota Medical Foundation is honored to partner with the UND medical school and Altruas they work together to ensure the region has a sufficient number of well-trained medicalprofessionals,” says J. Patrick Traynor, JD ‘91, president of the Foundation. The new center willprovide simulation-based training for physicians in the school’s general surgery residencyprogram.
“We are really excited about this grant,” says David Antonenko, MD, PhD, professor of surgery and director of the Surgical Simulation Center. “The center will meet the Accreditation Council for Graduate Medical Education’s requirements for simulation training of general surgery residents.” Family practice and internal medicine residents, medical students, and some allied health professionals will also have access to the center.
Megan Miller
David Antonenko,MD, PhD
http://www.dakmed.org/

NEWS BRIEFS
PA Professors Receive AAPA RecognitionMary Ann Laxen, PA-C (FNP ’91), director and associateprofessor, and Annette Larson, PA-C (FNP ’79), assistantprofessor, Physician Assistant Studies Program, Grand Forks,have been recognized as Distinguished Fellows of theAmerican Academy of Physician Assistants. They have joineda select number of outstanding physician assistants whohave distinguished themselves among their colleagues, aswell as in their communities, by their service to the PAprofession, their commitment to advancing health care forall people, and by their exemplary personal and professionaldevelopment, according to Cynthia Lord, MHA, PA-C,AAPA president. Laxen, associate professor of communityand family medicine, has directed the PA program since1999. Larson, assistant professor of family and communitymedicine, has been a faculty member with the program since1991. The PA Program offers a Master of Physician AssistantStudies degree for experienced health care professionals.Physician assistants are licensed health professionals whopractice medicine as members of a team with their supervisingphysicians. PAs deliver a broad range of medical andsurgical services to diverse populations in rural and urbansettings. AAPA, the only national organization representingphysician assistants in all medical and surgical specialties, isone of the largest medical societies in the United States.
PA Faculty Member Earns a ‘Best-of-Show’Award for Poster PresentationJeanie McHugo, PA-C, MS, assistantprofessor in the UND School ofMedicine and Health Sciences’Physician Assistant program, earneda “best-of-show” award for a posterpresentation titled “Inter-RaterReliability in Clinical Testing” at theAmerican Academy of PhysicianAssistants annual conference in Mayat San Antonio, TX. McHugo holds aBachelor of Science (BS) degree inhuman biology from Mankato (MN)State University and a BS degree in physician assistantstudies from the University of South Dakota. She earned anonline transitional master’s degree in physician assistantstudies from the University of Nebraska, Omaha, and ispursuing a PhD degree in education at UND. Her clinicalbackground is in family medicine and orthopedics. She hasbeen a faculty member of the UND Physician AssistantProgram for four years. She acknowledges Richard Landry,PhD, UND College of Education and Human Development,and Charles (Clint) Hosford, PhD, assistant professor, Officeof Medical Education at the UND medical school, for theirassistance in statistical analysis for this project. McHugojoined the UND medical school in 2004.
Majority of Buckingham Award RecipientsPractice and Teach in North DakotaFifteen of the 18 recipients of the William M. BuckinghamOutstanding Resident of the Year Award are MD graduatesof the UND medical school, practice in North Dakota andserve on the faculty of the school’s Department of Familyand Community Medicine.
The Buckingham Award, presented by the North DakotaAcademy of Family Physicians (NDAFP) since 1991, isnamed for one of the physicians who established the UNDFamily Medicine Residency Program in Bismarck in theearly-1970s. William Buckingham, MD (BS Med ‘49), andRalph Dunnigan, MD (BS Med ‘53), were the first directorsof the program. Among award-winners who took familymedicine residency training in North Dakota and haveestablished their practices in-state are:
Biron Baker, MD ‘95 (Bismarck Residency ‘98), Bismarck;Eric Bakke, MD ‘88 (Grand Forks Residency ‘91), GrandForks; Heidi Bittner, MD ‘91 (Minot Residency ‘94), DevilsLake; Chuck Breen, MD ‘90 (Bismarck Residency ‘93),Hillsboro; Joseph Burns, MD ‘93 (Fargo Residency ‘96),Fargo; Mark Christenson, MD ‘94 (Grand Forks Residency‘97), Grand Forks; Jeff Hostetter, MD (Bismarck Residency‘03), Bismarck; Scott Knutson, MD (Minot Residency ‘04),Minot; Kimberly Krohn, MD ‘96 (Minot Residency ‘99),Minot; Candelaria Martin, MD ‘04 (Minot Residency ‘07),Fort Totten; Kristi Midgarden, MD ‘97 (Grand ForksResidency ‘00), Grand Forks; Ben Muscha, MD ‘92(Bismarck Residency ‘95), Bismarck; Heidi Philpot, MD ‘03(Grand Forks Residency ‘06), Grand Forks; Todd Schaffer,MD ’02 (Grand Forks Residency ‘05), Carrington, and RobertWells, MD (Bismarck Residency ‘01), Jamestown. Theremaining award recipients, who are not UND MD graduates,are practicing in South Dakota, Wisconsin and Florida.Tomasz Jarzembowski, MD (Grand Forks Residency ‘08), isthe most recent recipient of the William M. BuckinghamOutstanding Resident Award.
The purpose of the William M. Buckingham OutstandingResident of the Year Award is to encourage family medicineresidents in the practice of family medicine and in theactivities of the North Dakota Academy of FamilyPhysicians. It was also created to encourage better rolemodeling among family practice residents and to recognizepositive attributes in future practicing family physicians.
Award recipients have demonstrated an exceptional interestand commitment to family medicine, and exemplify thequalities of a family physician including providing caringand compassionate patient care, scholarly inquiry, communityand social awareness, and a maturity in all phases ofpractice. They also exhibit a balance between personal andprofessional activities and involvement in the NDAFP.
NORTH DAKOTA MEDICINE Fall 2008 25
Jeanie McHugo, PA-C, MS

NEWS BRIEFS
Manuchair “Mike” Ebadi, PhD, retired associate dean for research and program development andprofessor emeritus of pharmacology, physiology and therapeutics, is preparing a second, expandededition of the award-winning book, Parkinson’s Disease, which he edited with Ronald Pfeiffer, MD,professor and vice-chair of neurology at the University of Tennessee Health Science Center. Anothereditor, with the Mayo Clinic--Jacksonville, FL, will also participate in the project.
“Parkinson’s disease has a genetic component that opens up a whole new area of importance toneurologists,” he said. Ebadi, who retired from the UND medical school June 30, 2007, resides withhis wife, Pari, in Laguna Niguel, CA.
26 NORTH DAKOTA MEDICINE Fall 2008
Manuchair Ebadi,PhD
Retired Associate Dean Plans Second Edition of Pharmacology Text
PA Program Aims to Improve Health Care for Rural and Underserved PeopleThe needs of the most medically underserved and vulnerable people are at the center of a project launched by thePhysician Assistant (PA) Program at the UND School of Medicine and Health Sciences. The three-year, $463,000 grantfrom the federal Health Resources and Services Administration aims to enhance the education of PA students to deliverprimary care which meets the special needs of five segments of the population:
- Families with children with disabilities, including blindness and physical disabilities - Elderly living alone in rural areas - Farm and ranch families without health care insurance - American Indian youth who, as a group, have a high rate of suicide - Veterans returning from military duty with physical or mental disabilities
Focus groups representing each of the targeted populations will be conducted statewide in North Dakota and inMinnesota, Iowa, Arkansas and Oklahoma, according to Mary Ann Laxen, PA-C (FNP ‘91), director of the PA programand the grant’s principle investigator. “What we learn from the focus groups will be used to identify and prioritize thespecial needs of these populations,” Laxen says, “and to help us to develop learning tools, such as case studies, to betterprepare them to provide effective health care.” Sixty-five students will participate in the enhanced training. The projectaddresses “so many pressing issues in health care today,” Laxen says. “We have young veterans returning from the war,many of them right here in North Dakota, and, as people livelonger and want to remain in their homes, more elderly livingalone in rural areas.”
“The suicide rate on our state’s Native American reservations istragic,” she adds. “Because of our current economic situation, somany people have dropped or lost their health insurance. Theseissues are on the forefront of our health care system today.”
The grant is titled “Educational Training Modules for PhysicianAssistant Students Serving High Risk Populations in Rural andUnderserved Regions of the United States.” PA program facultymembers plan to share new knowledge gained from the projectwith colleagues throughout the country.
The PA program prepares clinically competent physicianassistants, working with and under the supervision of physicians,to provide primary health care for the people in North Dakotaand other rural and underserved areas of the United States. Itsgoals are to alleviate the shortages of primary care providers and toprovide access to comprehensive and affordable health careservices to rural and underserved populations. Most PA studentswho come from rural and underserved areas, after graduation, havegone on to establish their practices in primary care in such areas.
Audrey Bercier, PA ‘07, Turtle Mountain Chippewau,is a physician assistant at the Quentin N. BurdickMemorial Indian Health Facility in Belcourt, ND.

ALUMNI NOTES
Sara Sailer, DPT ’08, has joined Altru Clinic-Lake Region,Devils Lake, ND. She provides physical therapy at Altru’soutreach site in Devils Lake.
Angel Overvold, DO (Family Medicine Residency ’05),practices family medicine at the Innovis Health clinic inWahpeton, ND. She completed family medicine residencytraining at the UND program in Bismarck.
John Eickman, MD ’04, Winston-Salem, NC, recentlypassed the American Board of Neurological Surgery writtenboard exam and earned the distinction of scoring above the99th percentile for the nation. Originally from Grand Forks,he completed his undergraduate education at ConcordiaCollege, Moorhead, MN. He is completing his residency inneurological surgery at Wake Forest University BaptistMedical Center. His wife, Kara (Looysen) Eickman, MD ’04,has recently completed her residency in neurology at WakeForest University and was selected as chief resident for thepast academic year.
Andrea Howick, MD ’04, has joinedthe Altru Health System’s obstetricsand gynecology department in GrandForks. She completed her training atLoyola University Medical Center inChicago, where she received awardsas Outstanding Junior Resident of theYear and Outstanding ResidentEducator. She completed a sub-internship in obstetrics and gynecologyat Southern Illinois University, as well as a medicaleducation elective at James Cook University School ofMedicine in Queensland, Australia.
Cathy Urlaub, PA ’04, practices urology with InnovisHealth in Fargo.
Amanda Diamond, MD ’03, a neurologist, has joinedMeritCare Health System in Fargo, where she practices atthe Neuroscience Center. Originally from Devils Lake, ND,she completed residency training in neurology and afellowship in neurophysiology at Brown University/RhodeIsland Hospital in Providence, RI. Her fellowship studiesincluded training in electroencephalogram andelectromyography studies. She has a special interest in thecare of patients with epilepsy.
Wesley Papenfuss, MD ’03, has joined MeritCare HealthSystem’s surgery department in Bemidji, MN. A generalsurgeon, he specializes in the surgical treatment of a wide rangeof diseases and conditions which involve the breast, stomach,esophagus, pancreas, gallbladder, lower intestines, herniaand abdomen. Papenfuss completed his residency in generalsurgery at Iowa Methodist Medical Center in Des Moines.
Brandon Helbling, MD ’03, has joined the surgerydepartment of Mid Dakota Clinic in Bismarck. He providesgeneral surgical services and performs weight-loss surgery.A native of Mandan, ND, he completed general surgeryresidency training at Michigan State University/Kalamazoo(MI) Center for Medical Studies, where he was honoredwith the Robert H. Hume Excellence in Research Award.He is a member of several professional associationsincluding the Society of American GastrointestinalEndoscopic Surgeons. He is certified in basic life support,advanced trauma life support and advanced cardiac lifesupport.
Rachel Miller, MD ’02, began practicing as a pediatricsurgical child and adolescent gynecologist Sept. 1 atChildren’s Hospital of Minnesota. She recently completedtwo years as a faculty member and a fellow in thepediatrics-gynecology program at Cincinnati Children’sHospital. There are very few -- only about four -- suchfellowship programs in the country, says her father, RonMiller, MD, clinical associate professor of pediatrics, Fargo,and “only about 100 people in the country” who practice inthis field. She completed four years of obstetrics-gynecologytraining at the Oregon Health Sciences University in Portland.
Talitha Sannes-Venhuizen, MD ’02, practices familymedicine at Innovis Health clinics in Detroit Lakes andFrazee, MN. Originally from Frazee, Sannes-Venhuizenearned a bachelor’s degree from the University ofMinnesota-Morris. She completed family medicineresidency training at the Mayo School of Graduate MedicalEducation program in St. Cloud, MN.
R.J. Moen, MD ’00, an emergency room physician,practices at Medcenter One in Bismarck.
Matthew Stayman, MD ’98 (Family Medicine Residency’01), is a family physician with MeritCare Health System inEast Grand Forks, MN.
Erik Dickson, MD ’97, practices family medicine atMarshfield (WI) Clinic-Cornell Center. He married DeborahWeiss on March 20, 2008 in Tampa, FL. She is a flightnurse with Mayo Clinic Medical Transport, based in EauClaire, WI. They live in Chippewau Falls, WI. Dicksoncompleted residency training in family medicine with theEau Claire Regional Education Consortium.
’00s
’90s
NORTH DAKOTA MEDICINE Fall 2008 27

ALUMNI NOTES
Denise Mortenson, PA ’94, has joined the practice ofJeffrey Smith, MD ’85 (Family Medicine Residency ’88), inBismarck. She is certified with the National Commission onCertification of Physician Assistants with special recognitionin primary care and surgery. She also holds certifications inadvanced and basic cardiac life support and advancedtrauma life support. With an extensive background in ruralhealth care, she has worked in Hazen, ND, since 1995.
Marcia Bahl, BSOT ’93, a licensed occupational therapist,has joined Altru Health System’s outreach therapydepartment in Grand Forks. She has experience in providinginpatient and outpatient services, and has worked in mentalhealth, home health, rehabilitation and hand therapy, andin a sub-acute care facility and several nursing homes. Bahlhas an advanced certificate in lymphedema.
Cynthia Kortum, MD (Family Medicine Residency ’91), iswith the Urgent Care department at Innovis Health in Fargo.
Scott Fillmore, MD ‘87, has joined MeritCare HealthSystem’s Broadway Health Center, Fargo, and Thief RiverFalls (MN) Southeast Clinic. A board-certified specialist inphysical medicine and rehabilitation, he completedresidency training at Baylor College of Medicine in 1991 atHouston. He has special interest in sports injuries andspine, musculoskeletal, electrodiagnosis (electromyography)and work-related injuries. Before joining MeritCare, he wasin private practice in Houston.
Jerry Obritsch, MD ’87, of the Mid Dakota Clinic Centerfor Women, Bismarck, was recently awarded the 2008-09ACOG Community Service Award for District VI. TheAmerican College of Obstetricians and Gynecologists(ACOG) established the Community Service Award torecognize a fellow or fellows who are or were recentlyactively involved in a community program that is designedto help underserved or poorly served patient populationswithin the district. The award was presented at the group’sannual clinical meeting in May at New Orleans. Since1991, when he finished residency training at the Universityof Missouri-Columbia, Obritsch has traveled to StandingRock Indian Reservation, south of Bismarck, to provideprenatal and ambulatory gynecological services.
Jeffrey Smith, MD ’85 (Family Medicine Residency ‘88),practices family medicine at Healthways clinic in Bismarck.A native of McHenry, ND, he is board-certified in familymedicine with added qualifications in sports medicine andgeriatrics. He graduated magna cum laude from Valley City(ND) State University and, after earning the MD degree atUND, went on to complete residency training at the UNDfamily medicine program in Bismarck, where he receivedthe Resident Teacher of the Year Award.
Kimberly Kelly, MD ’84, practices dermatology at InnovisHealth in Fargo.
Lori McDonald, PhD (BSMT ’82), King of Prussia, PA, isvice president for quality and compliance with MDSPharma Services. She will lead the company's ongoingprogram to build and manage quality and regulatorycompliance systems across its global business platforms.MDS Pharma Services is a leading provider of innovativedrug discovery and development solutions for thepharmaceutical and biotechnology industries. McDonaldholds a Master of Science degree and a doctorate inpharmaceutics from the University of Michigan.
Robert Grossman, MD (BS Med ’71),has retired after 34 years of practice atWest River Health Services inHettinger, ND. He has dedicated hisprofessional career to advancing thequality and availability of rural healthcare in the state and region, and hasserved as president of the NorthDakota Medical Association, amember of the Blue Cross Blue Shieldboard of directors for the past 10 years (currently serving aschairman), and board member for the North DakotaHealthCare Review. He has been a very active teacher forthe UND medical school. Grossman received his medicaldegree from the University of Colorado.
C. Milton Smith, MD (BS Med ’69), Minot, has joined St.Alexius Medical Center and PrimeCare Health Group inMinot. The board-certified family physician is a former directorof the UND family medicine residency program in Minot.
Delbert Nelson, MD (MS Pharmacology ‘61, BS Med ’61),board-certified family physician, practices part-time at theSoutheast Medical Center in Ellendale, ND; the Oakes (ND)clinic, and emergency room at Oakes Hospital. He recentlyretired from HealthEast Health Care System in St. Paul, MN.With 42 years’ experience in family medicine, he isproviding locum tenens services for physicians who taketime off, including those at the Nelson County Health System,Carrington, Hazen and Wishek, ND.
He earned the MD degree at Baylor College of Medicine inHouston in 1963. He took his internship at BethesdaLutheran Hospital in St. Paul, and served two years as adoctor in the U.S. Air Force. After his discharge from themilitary, he and his family settled in St. Paul where heworked until his retirement.
’80s
’70s
’60s
28 NORTH DAKOTA MEDICINE Fall 2008

IN MEMORIAM
C. Keith Barnes, MD (BS Med ’33), Austin, TX, passed awayMay 17, 2006. After graduating from UND, he completedthe MD degree at the University of Illinois Chicago HealthSciences Center. He was an ophthalmologist.
Edward “Bud” Hagan, MD (BS Med’40), Williston, ND, died June 1, 2008at his home. He was 91.Born to Joan and E.J. Hagan, MD, apioneer surgeon and physician inWilliston, he earned a Bachelor ofArts degree in 1939 and Bachelor ofScience in Medicine degree in 1940,both from UND. He earned the MDdegree at Rush Medical College, anadjunct of the University of Chicago, and took internshiptraining at Ancker Hospital in St. Paul, MN. During hisservice in the U.S. Navy in World War II, he received thePurple Heart, Silver Star, two Bronze Stars and twoPresidential Unit Citations, along with many otherdecorations. He married Kathleen O’Connor in 1949 atCulbertson, MT. In Williston he founded, along with JohnCraven, MD, the Craven-Hagan Clinic where he practicedgeneral medicine until his retirement in 1984. He was veryactive in numerous organizations and committees dedicatedto community development, including the Friends of FortUnion, leading a group of visionaries who devoted timeand effort to re-creating a national historical site thatflourishes today.
Wesley Levi, MD (BS Med ’43), Boise, ID, died Aug. 4,2008. He was 90. A native of South Dakota, he earned theMD degree from Temple University School of Medicine inPhiladelphia. After military service during World War II ona naval hospital ship in the Pacific near Guam, he moved toOmaha, NE, and later practiced in Beulah, ND, from 1949to 1950. He went on to complete a three-year residencytraining program in radiology at Bismarck and becameboard-certified in radiology. In 1960, he established hispractice in Boise. He was preceded in death by his wife,Rosemary.
Newell Braatelien, MD (BS Med ‘45), Moline, IL, apathologist with the Quad City Pathology group for 41years, died May 22, 2008 at Arkansas Hospice. He was 84.He grew up in Crosby, ND, attended the University ofNorth Dakota, and earned the MD degree from theUniversity of Illinois Medical School at Chicago HealthSciences Center. Dr. Braatelien was board-certified inanatomic and clinical pathology.
Anthony “Jim” Lund, MD (BS Med ’48), passed away July7, 2008 in Los Gatos, CA. He was 85. A native of Leeds,ND, he earned a Bachelor of Arts degree in chemistry in1946 and a Bachelor of Science in Medicine degree in1948, both from UND. He received the MD degree fromthe University of Illinois Chicago Health Sciences Center. Aboard-certified obstetrician-gynecologist, he practiced inSanta Clara County, CA, for 30 years. He was preceded indeath by his wife of 52 years, Junieve Lund.
James O’Toole, MD (BS Med ’52), St. Cloud, MN, died July21, 2008 after a battle with multiple myeloma. A native ofGrafton, ND, he earned the MD degree from Stritch Schoolof Medicine of Loyola University in Chicago and tookinternship and residency training at St. Luke’s Hospital inFargo. He was in private practice in Park River, ND, from1956 to 1962 and then continued his medical training atMenninger School of Psychiatry in Topeka, KS, where hewas also employed by the Topeka State Hospital. He alsotook a fellowship in community psychiatry at the MenningerFoundation from 1965 to 1966. Dr. O’Toole served as apsychiatric consultant to the North Dakota Board of PublicWelfare and director and medical director of MemorialMental Health and Retardation Center of Bismarck-Mandanfrom 1969 to 1975. He was associate medical director ofPrairie View Mental Health Center in Newton, KS, from1975 to 1984 and clinical associate professor with KansasUniversity School of Medicine in Wichita from 1976 to1984. Dr. O’Toole is survived by his wife, Georgine.
Marcia Anderson (BSMT ’57), Bismarck, died May 30, 2008after a year-long battle with cancer. She was 72. A native ofGlendale, CA, she grew up in Grand Forks and, afterearning her degree, moved to Bismarck where she worked asa medical technologist at the Bismarck Hospital. She issurvived by her husband, Gary.
Robert Cox (MEDEX ‘75), Kalispell, MT, died June 25, 2008.
Bonnie Bata-Jones (FNP ’78), Excelsior, MN, former facultymember of the Physician Assistant (PA) Program at the UNDmedical school, died July 24, 2008 after a battle with cancer.She was 61. A native of Grafton, ND, she attended St. FrancisSchool of Nursing in Minot where she completed the RNprogram in 1968 and earned a bachelor’s degree at WesternMichigan University in 1977. In 1980 and 1981, she servedas an instructor in UND’s PA program. In 1989, she earneda master’s degree in education at UND and later taught inthe family nurse practitioner program at the University ofMinnesota. A lieutenant colonel in the U.S. Army Reserves,she retired in May 2007 after 24 years of service that tookher around the world. She was a veteran of the Gulf War,serving in Abu Dhabi in 1991. She is survived by herhusband, Darrel Jones.
NORTH DAKOTA MEDICINE Fall 2008 29

PLANNING AHEAD
Celebrate UND’s past
by helping its future.
Every gift, small or big, impacts UND students today, tomorrow, forever.
The UND Foundation, an independent non-profit organization, raises and manages funds that secure a strong future for UND and its students, faculty and alumni. Gifts to UND through the Foundation may be directed to the program or fund you choose.
Give online at www.undfoundation.org or call
$1.25 $12.50 $125 $1,250 $12,500 $125,000
30 NORTH DAKOTA MEDICINE Fall 2008
Today’s medical students must always wear their white coats when working with patients.Second-year medical students Kassi Roselius and Kyle Marthaller listen to the lungs of Annika Opsahl
under the watchful eye of Year 2 Clinical Science Director Jon Allen, MD ‘84

At the American Medical Student Association(AMSA) national convention, this past spring atHouston, medical students raised awareness ofUND’s medical education program and encouragedundergraduates to apply. Tyler Brolin (from left),Michael Greenwood, Morgan Skalsky, KyleMarthaller and (not pictured) Nicole Saur, who waselected Region 8 co-director, gathered with otherstudents from throughout the country to take a lookat their future as physicians. UND received an awardfor recruiting to AMSA (more than 70 percent).
The MD Class of ‘11 hosted freshman medicalstudents at a picnic in August at University Park inGrand Forks. The annual event gives students andtheir families, as well as faculty and staff, a greatopportunity to have some fun and get acquaintedinformally before the rigor of school begins.
Members of the Doctor of Medicine (MD) Classof 2012 received their first white coats during aceremony ending the first week of classes in Augustat the UND medical school. The first-year students,26 men and 36 women, recited the modern versionof the Oath of Hippocrates, an ancient vow touphold basic professional principles.
Calling it “the mostexhilarating experience I’veever had,” Mary AnnLaxen, MAL, PA-C, MAB(FNP ’91), recalls her firstparachute jump this summeras part of a nationwideproject to raise money for programs aimed at fighting violence againstwomen and for scholarships for underprivileged women. Her flighttook off June 21 from West Fargo (ND) Airport. Throughsponsorships, she raised more than $1200 for SOAR (Speaking OutAgainst Rape) and local anti-sexual violence organizations. Laxen isdirector of the Physician Assistant Program and associate professor offamily and community medicine at the UND medical school.
NORTH DAKOTA MEDICINE Fall 2008 31

University of North Dakota School of Medicine and Health SciencesA National Leader in Rural Health - Serving North Dakota since 1905501 North Columbia Road Stop 9037 ● Grand Forks ND ● 58202-9037 701-777-2516 www.med.und.edu
ADDRESS SERVICE REQUESTED
Periodical POSTAGE PAID
UND President Robert Kelley, PhD, (left) chats with Roger Gilbertson, MD, president and chief executive officer of MeritCare HealthSystem, Fargo, during the first stop on the recent UND New Faculty Bus Tour, an annual three-day excursion that showcases the state’sdiverse geography and culture. Kelley, newly installed as UND’s 11th president, was paying a visit to the state’s largest hospital and the mostcomprehensive health care system between Minneapolis and Seattle. MeritCare works closely with UND to train resident-physicians andmedical and other health sciences students; it is one of many health systems with which UND partners to provide health professions educationthroughout the state and region. Gilbertson welcomed the tour group with a presentation about health care in North Dakota and how medicaleducation is provided in a rural state. For more about the bus tour, go to www.ndmedicine.org.