NEW PAGE-CAMPBELL MERGER» Abdominal Aortic Aneurysms ABDOMINAL AORTIC ANEURSMS: UPD ATE ON...
Transcript of NEW PAGE-CAMPBELL MERGER» Abdominal Aortic Aneurysms ABDOMINAL AORTIC ANEURSMS: UPD ATE ON...

Non-Profit Org.U.S. Postage
PAIDNashville, TN
Permit No. 3432
Please contact us at Vanderbilt Heart and Vascular Institute1215 21st Avenue South • Medical Center East, Suite 5200Nashville, TN 37232-8802 • Phone: (615) 322-2318
for more information:
Vanderbilt UniversityMarketing Department3401 West End AvenueSuite 470WNashville, TN 37203
On July 1, 2006, Vanderbilt Heart and Vascular Institute and Page-Campbell Cardiology Group officially joined forces to provide the most comprehensive cardiology services in Middle Tennessee. Please join us in welcoming:
» Andre L. Churchwell, MD » Keith B. Churchwell, MD » Walter K. Clair, MD » Marshall H. Crenshaw, MD
» Rand T. Frederiksen, MD » G. Christian Friesinger, MD » Clifford L. Garrard, Jr., MD » Mark D. Glazer, MD
» Rob R. Hood, MD » Adam J. Prudoff, MD » Thomas R. Richardson, MD » Mark A. Stankewicz, MD
new page-campbell merger:

Fall 2006 Volume 1 Issue 2 www.vanderbiltheart.com
Vanderbilt Heart and Vascular Institute Quarterly Publication
Jayant Bagai, MDGeneral Clinical Cardiolog y ProgramVA Hospital
Jeffrey Boord, MDPreventive Cardiolog y Program
John Kimbrough, MDCardiovascular Medicine
James Muldowney, MDGeneral Clinical Cardiolog y ProgramVA Hospital
Allen Naftilan, MDAssistant Professor, Cardiovascular Surgery
Michael Petracek, MDProfessor, Cardiac Surgery
Charles B. Ross, MDAssistant Professor, Vascular Surgery
Douglas Sawyer, MDHeart Failure Program
Mark Wigger, MDHeart Transplantation Program
new physicians:
Abdominal Aortic Aneurysms:Update on Guidelines for Screening & Treatment Recommendations
» Marc A. Passman, MD » Thomas Naslund, MD
Advances in Cardiac SurgicalApproaches to Heart Failure& Transplantation
» Frank G. Scholl, MD
Contemporary Approach to Ablationof Atrial Fibrillation
» Dawood Darbar, MD, PhD
in this issue: from the editor:Robert N. Piana, MDAssociate Professor of MedicineDirector, Vanderbilt Cardiovascular NetworkAssociate Chief, Division of Cardiovascular Medicine Director, Interventional Cardiolog y Fellowship Training ProgramEditor, Vanderbilt Heart
ThesecondissueofVanderbilt Heartmarksseveralmilestones forourprogram. In July2006,clinicalgrowthsurgedaheadwith fullintegration of the Page-Campbell Cardiology practice into the Vanderbilt HeartInstitute.Thismergeristheculminationofaclose,6-yearaffiliation,withpotentialtoexpandVanderbiltHeart’spracticevolumeby20,000patients.Inparallel,Dr.JohnByrnehascontinuedexpansionofthecardiacsurgicalprogram’sscopeanddepthwiththerecruitmentofDr.MichaelPetracek,aleadingNashvilleheartsurgeonformorethan20years.Dr.Petracekbringsexpertiseinstentlessaorticvalvesurgeryandminimallyinvasivemitralvalvesurgery. VanderbiltHearthascarefullycoupledclinicalgrowthwithafocusonquality.The June2006accreditation ofVanderbiltHeart as aChest PainCenter by theSocietyofChestPainCentersrecognizesthis“qualityfirst”approach.Dr.WaleedIrani of Vanderbilt Heart and Dr. Marc Mickiewicz of Emergency Medicine areChestPainCenterjointmedicaldirectors;CardiologyCaseManager,JeannieByrdprovidesnursingguidance.ThisnationalrecognitionplacesVanderbiltHeartamongprovidersofferingoptimaldiagnosisandmanagementofacutecoronarysyndromesandheartfailure. VanderbiltHeartalsocontinuestogarnernationalrecognitionthroughacademicaccomplishments.ChiefofCardiovascularMedicine,Dr.DougVaughanisalongtimeleader invascularbiologyand thrombosis research. In June2006, theNationalHeart,Lung,andBloodInstituteawardedDr.Vaughana5-year,$16-millionSCCOR(Specialized Center of Clinically Oriented Research) grant to study thrombosis.Dr.Vaughan’smultidisciplinaryteamwillfocusonincreasedthromboembolicriskleadingtomyocardialinfarctionandstrokefoundinpatientswithdiabetes,insulinresistance,andobesity. Readonforanin-depthlookatourprogramsinaorticaneurysmrepair,cardiactransplant,andatrialfibrillationmanagement.

» Abdominal Aortic Aneurysms
AbdominAl Aortic Aneurysms: updAte on Guidelines for screeninG And treAtment recommendAtions
Marc A. Passman, MDAssistant Professor of SurgeryDivision of Vascular SurgeryVanderbilt University Medical Center
Aorticaneurysmsoccurwhen theaorta expands toadiameter1.5 times thenormaladjacentaorta.Aorticaneurysmsaccountfor15,000deathsannuallyandarethe15thleadingcauseofdeathintheUnitedStates.Ofthese,9,000deathsareduetoabdominalaorticaneurysms(AAA),withtheremainderlocatedinthethoracicaorta.AAAsarefoundin4%to8%ofmenand0.5%to1.5%ofwomen.Increasingage,smoking,gender,andfamilyhistoryrepresentthemostsignificantriskfactorsforAAA. The impetus to screen for AAA is motivated by itsprevalenceandnaturalhistory.AlthoughAAAsmaybeasymptomaticforyears,upto40%willeventuallyruptureifundiagnosedor leftuntreated.Whenruptureoccurs,prognosisispoor,withmostdeathsoccurringoutofthehospital.Forpatientswhosurvivetohospitaladmission,emergentAAArepairisassociatedwithhighmortality;only10% to25%of individualswith rupturedAAAssurviveuntildischarge.
AAA SCREENING RECOMMENDATIONS
EvidencesupportingscreeningforAAAshasbeenslow to evolve. In 1996, the US Preventive ServicesTask Force (USPSTF) found insufficient evidence torecommend for or against routine AAA screening ofasymptomaticadults,citingtheneedformoredatafrompopulation-based screening trials. Since then, resultsfromseveralpopulation-based,randomizedcontrolledtrialsofAAAscreeninghavebeenpublished.Onthebasisof thisnewevidence,USPSTF recentlyupdateditsrecommendationforAAAscreeningtoinclude:
❤ One-timescreeningforAAAbyultrasonographyinmenaged65to75yearswhohaveeversmoked.(ThisisaGradeBrecommendation-atleastfairevidencetheserviceimprovesimportanthealthoutcomes,andbenefitsoutweighharms.) ❤ NorecommendationfororagainstscreeningforAAAinmenaged65to75whohaveneversmoked.(ThisisaGradeCrecommendation-atleastfairevidencetheservicecan improvehealthoutcomes,but thebalanceofbenefitsandharms is too close to justifyageneralrecommendation.) ❤ RecommendsagainstroutinescreeningforAAAinwomen.(ThisisaGradeDrecommendation-atleastfairevidencetheserviceisineffectiveorharmoutweighsbenefits.) Although updated recommendations are a step inthe right direction, they are not without controversy.USPSTF found evidence that screening and electivesurgical repair of AAAs in men aged 65 to 75 yearswhoarecurrentor former smokers leads todecreasedAAA-specificmortality.However,USPSTFdeferredanyrecommendation for men in this age group who haveneversmokedasthelowerprevalenceofAAAsoffsetsanybenefitofscreening,deferringanyrecommendationsinthis group at this time. Also USPSTF recommended noscreeninginwomen,citinglowAAAprevalence.Accordingtotheserecommendations,womenandnonsmokingmen,even thosewith a family history ofAAA,do notmeritscreening,despitewell-documentedhighprevalenceofAAAsinthesesubgroups.Inaddition,USPSTFconcluded
2
Thomas Naslund, MDAssistant Professor of SurgeryDivision of Vascular SurgeryVanderbilt University Medical Center

thatinwomenandnonsmokingmen,“screeningandearlytreatmentresultinimportantharms,”butdonotspecificallydefine “harms” precluding elective AAA repair.Because of these criticisms, the Society for VascularSurgery and the Society for Vascular Medicine andBiologycontinuetorecommendscreeningforAAAinallmenaged60to85years;womenaged60to85yearswithcardiovascularriskfactors;andmenandwomen50yearsandolderwithafamilyhistoryofAAA.Afterinitialscreening,USPSTFalsorecommendsnofurthertesting if aortic diameter is <3 cm; ultrasonographyannuallyifaorticdiameterisbetween3cmand4cm;ultrasonographyeverysixmonthsifaorticdiameterisbetween4cmand4.5cm;andreferraltoavascularspecialistifaorticdiameteris>4.5cm. WiththestrengthofUSPSTFrecommendationsandtheworkof theNationalAneurysmAlliance,effortsto provide a one-time AAA screening benefit underMedicarePartBreachedamilestoneonFebruary8,2006,withthesigningoftheDeficitReductionActof2005,alsoknownastheBudgetReconciliationBill.ItincludestheScreeningAbdominalAorticAneurysmsVery Efficiently Act, a provision that will implementAAA screening as a Medicare benefit for at-riskbeneficiaries65yearsandolder.ThelegislationtakeseffectJanuary1,2007.Althoughtherearelimitationstothisbenefit,itisanimportantsteptowardplacingAAAsattheforefrontofpublicawareness.
AAA TREATMENT RECOMMENDATIONS ThegoalofelectiveAAArepairispreventingruptureandprolonginglife,andshouldbeperformedwhenruptureriskishighcomparedwithoperativeriskandinpatientswhoselifeexpectancyislongenoughtorealizebenefit.SelectionofpatientsforAAArepairis determined by balancing estimates of aneurysmrupture risk, elective operative mortality risk, lifeexpectancy,andpatientpreference. ThestrongestriskfactorforAAAruptureismaximalaorticdiameter.ThenaturalhistoryofclinicallyapparentAAAsisdifficulttodetermine,butbybestestimates,the1-yearriskofrupturewhentheAAAis<4cmis0%;4cmto5cm,0.5%to5%;5cmto6cm,3%to15%;6cmto7cm,10%to20%;7cmto8cm,20%to40%;and>8cm,30%to50%.RupturerisksubstantiallyincreasesasAAAdiameterincreasesfrom5cmto6cm.LevelIevidencefortreatmentofsmallAAAsfromtworandomizedprospectiveclinicaltrialsconductedintheUnitedKingdomandtheUnitedStatessupportsthisnotion.BothtrialsconcludedsurveillanceofAAAof4cmto5.5cmissafe,andsurgerydidnotresult inany long-term survivaladvantage, therebyreinforcing the 5.5 cm threshold. A rapid rate ofaneurysmexpansion(>1.0cm/y)alsoisusedasanindication for repair independent of absolute size;however, the value of expansion as a predictor ofruptureriskislessclear.
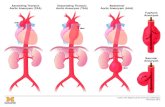
Figure 1: Computed tomography angiogram three-dimensional reconstruction
showing abdominal aortic aneurysm before (A) and after (B) endovascular
stent graft repair.
3
A B

» Abdominal Aortic Aneurysms continued
If you are a patIent and you would lIke to fInd out more about aaa screenIng and
treatment optIons, contact the VanderbIlt Vascular clInIc at (615) 343-2887 for an appoIntment.
If you are a health care proVIder and would lIke to dIscuss a patIent referral wIth a
Vascular surgeon, contact the dIVIsIon of Vascular surgery offIce at (615) 322-2343.
Aswithrupturerisk,reportedoperativemortalityofconventionalo p e n A A A r e p a i r v a r i e sconsiderably in the l i terature.Manyreferral-basedseriesfromindividualcentersofexcellencedescribe 30-day perioperativemortalityof1%to5%followingelectiveconventionalopenAAArepair.Conversely,manyrecentpopulation-basedseriesemployingstatewideornationaldatabasesindicatehighermortality,inthe4%to8%range.Suchvariationsupportstheexcellentresultsandlowmortalityratesoftenachievedbyselectedreferralcenterswithveryexperiencedsurgeons. Endovascularaneurysmrepair(EVAR)emergedintheearly1990sas an alternative treatment forAAAandhashadanexpandingroleinrecentyears.Manystudieshave demonstrated equivalentsa fe ty and e f f i cacy o f EVARcompared wi th conven t iona lopenrepair.Short-termbenefitsofEVARincludereducedintensivecare unit and hospital lengths
o f s tay, reduced b lood loss ,fewermajorcomplications,andmore rapid recovery.However,studieswithlongerfollowupareinconsistent with some reportssuggestingequivalentoutcomes,whi le others raised concernsaboutEVARdurability,includingproblemsofendoleak,needforlatereinterventions,conversiontoopenrepair,orboth,andalowincidenceofdelayedrupture.Onlyrecentlyhaspublishedrandomizeddatasupportedaperioperativesu r v iva l advan tage, bu t th i swas not sustained beyond thefirst postoperative year. Sincecontinuedriskforcomplicationsare recognized over the longterm after EVAR, managements t r a t eg ie s f o r endovascu la rrepairofaneurysmmusttakeintoaccounttheneedforpermanentlong-termfollowup.Eventssuchasendovascularleak,migration,andaneurysmenlargementarewel l -descr ibed poten t ia l la teeventsthatcanbeeasilymonitoredthrough specialty care. When
complications fol lowing EVARareidentified,simple,minimallyinvasive procedures can resultin sat is factor y resolut ion andpreventionofneedforconversiontoopenoperationoraneurysmrupture. Patients who are notavailable for careful long-termfollowuphaverisksofunforeseenlateEVAR-relatedcomplicationsand may be bet ter ser ved byconventionalopenrepair.Withuncertainlong-termdurabilityandeffectiveness,aswellastheneedforongoingsurveillance,basedoncurrentevidence,EVARismostapp rop r ia t e f o r pa t i en t s a tincreasedriskforconventionalopen AAA repa i r. As moreprospect ive randomized databe come a va i l ab l e , and a stechnologyevolves,theroleofEVAR may evolve to support alowerthresholdforAAArepairand may shif t the r isk -benefi tra t io o f sc reen ing to jus t i f ymore w idesp read sc reen ingthan cur ren t ly recommendedbyUSPSTF.
4

» Advances in Cardiac Surgical Approaches to Heart Failure and Transplantation
AdvAnces in cArdiAc surgicAl ApproAches to heArt fAilure And trAnsplAntAtion
Frank G. Scholl, MDAssociate Professor Cardiac Surgery DepartmentVanderbilt Transplant Center
Animportantcomponentofoursurgicaltreatmentofend-stageheartfailureisourbridgetothetransplantassistdevice(VAD)program.WehavereinvigoratedthisaspectoftheprogramwiththeadditionoftheThoratecVAD toourbridgeprogram.Usinga combinationoftheNovacorLeftVentricularAssistSystem(LVAS)andthe Thoratec Percutaneous Assist Device (PVAD), wesuccessfullybridgedfivepatientstohearttransplantationin2005andhaveonepatientcurrentlyawaitingtransplantonaNovacordevice.ThistremendousachievementwasaccomplishedthroughthecommitmentofourVADteamandadedicatedVADcoordinator. Newdevelopmentsintheprogramincludeashifttowardnewer,smallerimplantabledevicesandashifttowardout-of-hospitalcareforourVADpatientsawaitingheart transplant. The addition of new and improvedtechnologieswillimprovequalityoflifeofVADpatients,while insuring the continued successof theprogram.WeplantoincorporatetheThoratecIVAD(ImplantableVentricularAssistDevice)forpatientsinneedofsingleorbiventricularsupport. Ourhistoryofsuccesswithventricularassistdevicesandourrecentexcellentresultsinourbridgetotransplantpatientshaveledtoopportunitiestoparticipateinclinicaltrials. We will soon be participating in an excitingmulticenter,pivotaltrialoftheJarvik2000axillaryflowventricular assist device. This will bring cutting edgetechnologytooureligiblebridgetotransplantpatients. Insummary,theVanderbilthearttransplantteamisdevotedtoprovidingworld-classcaretoourend-stageheartfailurepatients.Theseexcitingnewdevelopmentsinhearttransplantandventricularassistprogramswillhelpensureourpatientsreceivethebestpossiblecarethroughallphases,frominitialevaluationtoposttransplantmanagement.Welookforwardtothefutureandhopeyouandyourpatientswillbeapartofit.
At Vanderbilt University Medical Center, 2005was a year of milestones for heart transplantation.In2004-2005,we transplantedourprogram’s500thadultpatientandour100thpediatricpatient.Lastyearwetransplantedoneoftheyoungestsetoftwinsintheworld. Fittingly, July 2005 marked the 20th year ofourprogram,givingnewheartsandnewlives toourpatients. Whilewecelebratethesepastaccomplishments,wecontinuetoenhancethetransplantprogram.Wehaveadded new leadership in both medical and surgicalaspectsoftheprogram,hiringthreetransplantcoordinatorsandadedicatedtransplantpharmacist.Wealsohaveaddedadedicateddonorcoordinatortoimprovedonoravailabilityandquality,inordertomaximizesuccessfultransplantoutcomes. Underthisnewleadership,clinicaloutcomeshaveexceededthenationalbenchmarkfor1-yearsurvival.Theactualsurvivalfor2005was100%.Thesestatisticsdemonstrate the best early survival outcomes in the20-yearhistoryofahearttransplantprogramthathastraditionallyachievedexcellentclinicaloutcomes. Clinicaltrialsofnewmedicationstoimprovelong-term outcomes in our heart transplant patients willcontinue.Werecentlyhavebeeninvitedtoparticipateinaposttransplantevaluationofsirolimusformaintenanceimmunosuppression.Thisnewermedicationmayhavefewer side effects and help decrease incidence ofallograftvasculopathy.
5

Contemporary approaCh to ablation of atrial fibrillation
OvERvIEw
AtrialFibrillation(AF)isthemostcommon arrhythmia encounteredin clinical practice, accountingfor approximately one third ofhospitalizationsforcardiacrhythmicdisturbance. An estimated 2.2millionAmericanshaveparoxysmalor pers is tent AF; prevalenceincreases with age to more than6%inoctogenarians.Moreover,AFconfersanaverageannualstrokeriskof5%,uptoseventimestherateinthegeneralpopulation.ConventionalAF management has focused onrestorationandmaintenanceofsinusrhythmwithelectricalcardiovascularand an t ia r rhy thm ic agen t s ,controllingtheventricularresponsetochronicAFwithagentsthatslowheart rate and anticoagulation toreducestrokerisk.Nevertheless,theefficacyofthesemodalitiesislimited,and the morbidity and mortalityattributabletoAFremainsignificant. Recen t advances in ourunderstanding of AF have led todevelopment of catheter ablationtechniquesthatcouldfeasiblyachieveacureforAF.Thisreviewdiscusses
new insights into mechanismsinitiating and perpetuating AFand how they impact catheterablation of AF. It also highlightstheevolutionofdifferentstrategiesandtechniquesforAFablationandpresentsVanderbiltUniversity‘sAFAblation Program results with theleft atrial circumferential ablationapproach. Catheter ablation forAFwasfirstreportedmorethanadecadeago.Duringthisrelativelyshorttime,ourstrategiesandtechniqueshavedramatically evolved in parallelwi th improved unders tandingof mechanisms ini t iat ing andmaintainingAF.
MEChANISMS Of Af
Based on experimental andclinical studies using a varietyof catheter and surgical ablationtechniques,itispossibletopostulatetwo mechanisms for AF initiationandperpetuation. 1. Primary drivers: Some typesofAF,particularlyparoxysmalAF,may be primarily dependent ontachycardiasthatinitiateanddriveAF.Althoughoftenlocatedinthe
pulmonaryveins(PVs),driversalsomayoriginatefromthesuperiorvenacava,veinofMarshall(asmallveinfromtheleftatrium,openingintothecoronarysinusincloseproximitytotheleftsuperiorPV),orcoronarysinus, or within the left or rightatrium. Furthermore, secondarytachycardias resul t ing from aprimarydriveralsomayfunctionasAF drivers.Once the primarydriverinducessecondarydrivers,AFperpetuationismorelikely.Thisoccurseveniftheprimarydriveris extinguished, as other driverscontinue to function. AF also isperpetuated by microreentrantcircuits, or “rotors,” exhibitinghigh-frequency periodic activityfromwhichspiralwave frontsofactivationradiateintosurroundingatrialtissue.Theserotorsactivateatriaatexceedinglyhighfrequenciesandresultinfibrillatoryconduction.Importantly, dominant rotors inAFareprimarilylocalizedinthejunctionbetweentheleftatrium(LA)andPVs.Basedonthismechanism,successful ablation of AF shouldtargeteliminationofprimaryandsecondarydriverswithstrategies
Dawood Darbar, MD, PhDDirector Cardiac Electrophysiolog y LaboratoryVanderbilt University
» Contemporary Approach to Ablation
6

such as electrically “disconnecting” PVs from theLAbyablatingaroundveinorigins. 2. Multiple wavelet reentry: In 1959, Moe andAbildskovadvancedthemultiplewavelethypothesis.Inthisconcept,AFismaintainedbymultipleindependentwaveletsmovingaroundfunctionallyrefractorytissue.AFmaintenancedependson theprobability that,atanypointintime,asufficientnumberofactivewaveletscansustainelectricalactivity.Wavelengthisanimportantdeterminantofwaveletnumber.Factorsshortening refractoriness or slowing conductionwill shorten wavelength and facilitate attainmentof the critical number of wavelets. Based on thismechanism, AF ablation requires modification ofthe atrial substrate to prevent attainment of thecriticalnumberofcirculatingwavelets.
ClINICAl RElEvANCE TO CAThETER AblATION Of Af
Basedon thesemechanistic insights, catheterablationofAFcouldtargeteitherdriversoriginatingfromthePVs,LA,orelsewhere,ortheLAsubstratesuchthatAFcannolongeroccureveninthepresenceofadriver.Ahybridapproachalsocouldbeused.A careful literature review, however, reveals PVablationremainsexperimental,andismostsuitableforpatientswhoserecurringsymptomaticepisodesofAFhavenotbeensuppressedbyantiarrhythmicdrugsorwhodonotwishtotakelong-termantiarrhythmicmedications.Further,radiofrequency(RF)ablationseemsmosteffectivewhenapplyingablationenergyat the LA-PV junction.Discrete RFapplications torapidlyfiringPVarrhythmogenicfocihavepotentialofcuringparoxysmalAF.However, the techniquehasproven inadequate inmanypatientsbecauseof prolonged procedure times, frequent need forrepeat interventions, and an unacceptable rateof PV stenosis. Understanding and overcominglimitationsofthefocalPVablativeapproachhave
incitedelectrophysiologiststoproposetwoalternativeapproaches,theso-called“segmentalPVisolation”and“circumferentialPVablation.” Segmental PV Isolation: Ha i s saguer re e t a l
describedresultsofPVsegmentalisolationguidedbycircumferentialmappingdataobtainedwithasteerablecircularcatheter(Figure1).ActivationwasnevercircumferentiallysynchronouswithinPVduringsinusrhythm,indicatingpreferentialbreakthroughsinto thevein from theatrium.Thehypothesiswasthat,althoughPVmusclecoversalargeportionofthePVostialperimeter,specificbreakthroughsitesofconductancewiththeLAallowostialPVdisconnectionwith minimal ablation. LA-PV breakthrough wasdeterminedbymappingtheperimetricdistributionand activation sequence of PV potentials, thusguidingostialablationtosegmentsshowingearliestFigure 1: Schematic representation of the ‘segmental PV isolation’ approach. A mapping catheter (Lasso) is positioned at the os of the left superior pulmonary vein (LSPV). As activation is never circumferentially synchronous within the PVs, specific breakthrough sites of conductance within the left atrium (LA) allow ostial PV disconnection. Since the breakthrough is at pole # 3, ablation (abl) at this site may electrically disconnect the vein from the rest of the atrium.
7

activationwiththeendpointofPVdisconnection(Figure2).Theextentofperimetricablationwasconfined,minimizingriskofPVstenosis. The main limitation of this approach is properalignmentofthemappingcatheterwiththenotoriouslyirregulargeometryofPVs,making interpretationofrecorded electrograms challenging. Furthermore,catheter drift may mislead the operator regardingostialposition.Finally,thistechniqueisnotapplicabletoRFablationoutsidePVostia,whichmay requirecomplete circumferential lesions to produce distaldisconnection.
ClinicalstudieshavedemonstratedcompleteelectricalisolationofPVswithasegmentalapproachpreventsrecurrentAFinabout70%ofpatientswithparoxysmalAFandabout25%ofpatientswithpersistentAF.Lessfavorable results inpatientswithpersistentAF likelyreflect the minor role played by PVs in this patientpopulation. In addition, isolation of PVs addressesonlyonepossiblemechanismforAF;manyothersarenottargetedbythisapproach.Furthermore,eveniftheprimarydriver iseliminatedbyPVablation,patientswithpersistentAF likelyhave secondarydrivers thatmayperpetuateAF.
» Contemporary Approach to Ablation continued
8
Figure 2: Elimination of pulmonary vein (PV) potentials by segmental ostial ablation. Shown are leads I and V5, distal bipole of an ablation catheter (Abld), bipolar electrograms recorded with a decapolar ring catheter (Lasso) positioned at ostium of left superior PV (L1–2 and L9–10), and proximal and distal bipoles of a quadripolar catheter positioned within coronary sinus (CSp and CSd). Before ablation (A), several PV potentials were recorded at ostium (arrows). After segmental ostial ablation (B), PV potentials were no longer present. Reproduced from Oral et al, with permission.

Circumferent ia l PV Ablat ion: To c i r cumven tthese l imitations, Pappone proposed a purelyanatomicapproach:CircumferentialRFlesionsarecreated using three-dimensional electroanatomicguidance around ostia of each PV, with the aimof disconnecting these veins from the LA, whilereducingriskofPVstenosis(Figure3).Animportantdistinction between these approaches is that anapproach aimed at eliminating arrhythmogenictriggersor critical connectionsbetween substrateandtrigger,irrespectiveofongoingtriggeractivity,appearstoyieldgreatersuccess.Ananatomicallybasedprocedureeliminatestheneedformappingspontaneous or induced arrhythmias and would,therefore,effectivelypreventrecurrentAFcausedbymultiplefoci,evenifnewfocieventuallyemerge. Anadditionaladvantageis the lesioncanbetailored tovaryingPV-LAjunction features,unlikecircumferentialablationcatheterswithaprefixedsizeanddesign,whicharedifficulttoaccommodateinostiawithlargerdiameters,eccentricshape,ora complex proximal PV branching pattern. Thisapproach also appears more feasible than leftatrialcompartmentalizationthroughasinglelongline encircling PVs and connecting to the mitralannulus.TheoverallsuccessrateofcircumferentialPV ablation is about 85%. Interestingly, patients
with paroxysmal (86%) or permanent AF (83%),had similar success rates, raising thequestionofreversibilityofAF-inducedelectrophysiologicatrialchanges.ArecentrandomizedstudydemonstratedamodificationofcircumferentialPVablation(encirclingleftandright-sidedPVswithanablationlinealongtheposteriorLA)isabout20%moreeffectivethansegmental PV isolation in preventing paroxysmalAFrecurrences.
vANDERbIlT UNIvERSITy Af AblATION PROGRAM
Vanderbi l t Univers i ty ’s e lec t rophysio logylaboratory,establishedin1984,offerscomprehensiveevaluationandtreatmentofallcardiacarrhythmias.InterestinAFablationtherapyatVanderbiltUniversitybeganinthemid-1990s,withthefirstAFablationperformed in 1998. The AF program has grownrapidly,andin2004,weperformed60AFablations;55in2005. AF Clinical Outcomes: Improved understandingofmechanismsinitiatingandmaintainingAFhasledtomodificationofourablativeapproach.Currently,our approach is a modification of the left atrialcircumferentialapproach,withencirclementoftheleftandrightPVsandlinearlesionsattheroofoftheposteriorLAandbetweencircumferentiallesions
9
Figure 3:Ablation lines created during left atrial ablation. A 3D representation of left atrium and PVs was
constructed with an electroanatomic mapping system. Red tags represent sites at
which radiofrequency energy was delivered. Left- and right-sided PVs are encircled. Also
shown are ablation lines in mitral isthmus and posterior left atrium. A, left posterior oblique projection; B, posteroanterior projection. LS
indicates left superior; LI, left inferior; RS, right superior; RI, right inferior; and LA, left atrium.
Reproduced from Oral et al, with permission.

» Contemporary Approach to Ablation continued
andthemitralvalveannulus.AblationisguidedbytheEnsiteNavX(EndocardialSolutions,St.Paul,MN)three-dimensionaladvancedmappingsystem,whichisintegratedwithitsnovelthree-dimensionalCT/MRI(computedtomography/magneticresonanceimaging) image-importing function. This systempermits three-dimensional modeling of the leftatrium and PVs, with real-time visualization ofanystandardelectrophysiologycathetertoassistablation.Figure4showsaviewofleftatrialthree-dimensionalanatomyconstructedwiththeEnSiteNavXsystemandanimportedMRIimage.ItalsoshowsthetwocircumferentiallesionscreatedbyRFenergytoencircletheipsilateralPVsasapair,andlinearlesionsbetweenthetwocircumferentiallesionsattheroofoftheLAandbetweenthelesionsandthemitralvalveannulus.
Thecharacteristicsof58consecutivepatientswithparoxysmal/persistentAFwhohaveundergonetheleftatrialcircumferentialapproachatVanderbiltUniversityareshowninTable1.ResponsetoAFablation is defined in terms of complete absence of AF by Holter monitoring (on no antiarrhythmicdrugs); partial response if >75% reduction in frequency and duration of symptoms, with or withoutpreviouslyineffectiveantiarrhythmicdrugs;orrecurrenceifnochangeinfrequencyanddurationofAF.Duringaveragefollowupof14±3months,73%ofpatientswithparoxysmalAFhadnosymptomaticrecurrenceofAF(Figure5).ThesuccessratewaslowerinpatientswithpersistentAF.Table2delineatescomplicationsassociatedwiththeseprocedures.
Table 1: Characteristics of patients who have undergone the left atrial circumferential ablation approach at Vanderbilt University.
Characteristic No. of patients (n = 58)
Age 56 ± 10 Male/Female 44/14 Paroxysmal/Persistent AF 46/12 Duration of AF (yr) 5 ± 2 Frequency of symptoms (episodes/month) 20 ± 17 Ejection fraction 0.56 ± 0.02 Left atrial diameter (cm) 42 ± 3.4 Structural heart disease 7 (12%) No. of failed AADs 2.4 ± 1.3 Follow-up (months) 14 ± 3 AF, atrial fibrillation; AADs, antiarrhythmic drugs.
10
Figure 4: A left lateral view of the left atrial 3D anatomy constructed by the EnSite NavX (left panel) and imported MRI (right panel). Two circumferential lesions were created by RF energy to encircle the ipsilateral PVs as a pair and linear lesions were generated between the roof of the circumferential lesions at the roof of the left atrium and between circumferential lesions and the mitral valve annulus on the left side.

Table 2: Complications associated with left atrial circumferential ablation approach.
Complication No. of patients (n = 58)
Pericardial tamponade 1/58 (1.7%) Transient ischemic attack 1/58 (1.7%) PV narrowing (<50%) 2/58 (3.4%) Symptomatic PV stenosis 0 Left atrial flutter 4 (6.9%)
PV, pulmonary vein
CONClUSION
ThelastdecadehasseenremarkableadvancesinourunderstandingofAFandhasledtocatheterablation techniques demonstrating the feasibility of achieving cure. However, given the mechanisticheterogeneityofAF,itseemsunlikelythatoneminimumsetofablationlesionswilleverbeeffectiveforallpatients.Nonetheless,futureadvancesintechniquesandtechnologyanddemonstrationofablationoutcomesinprospectiverandomizedtrialswilllikelyexpanduseofablationinbroadAFpopulations.
Figure 5:Outcomes in patients with paroxysmal and persistent atrial fibrillation (AF) who underwent the left atrial ablation approach at Vanderbilt University.
paroxysmal afpersistent af
11
new staff member:Kimberly Vernier, BSN, MSN, APRN-BC, Chest Pain and Stroke Coordinator, Emergency Services