New Jersey Division of Medical Assistance and Health...
Transcript of New Jersey Division of Medical Assistance and Health...
-
Electronic Data Interchange
July 2003 Version
New Jersey Division of Medical Assistance and
Health Services (DMAHS)
PHARMACY
NCPDP-HIPAA COMPANION GUIDE
November 2011 Version
POS, NCPDP Version 5.1 Batch, NCPDP Version 1.1
-
Electronic Data Interchange
July 2003 Version
DMAHS NCPDP-HIPAA Companion Guide
Table of Contents November 2011 Version
Page i
SECTION 1 – INTRODUCTION
1.1 NEW JERSEY DMAHS INTRODUCTION Page 1-1 1.2 HIPAA BACKGROUND Page 1-3 1.3 HIPAA INTERNET LINKS Page 1-5 1.4 COMPANION GUIDE ORGANIZATION Page 1-7 1.5 CHANGES COMPARED TO PRIOR VERSION Page 1-8
SECTION 2 – ELECTRONIC DATA INTERCHANGE
2.1 HIPAA TESTING Page 2-1 2.2 TELECOMMUNICATION SPECIFICATIONS Page 2-1 2.3 ELECTRONIC MEDIA SPECIFICATIONS Page 2-4 2.4 INTERCHANGE NAMING CONVENTION Page 2-6
SECTION 3 – NCPDP SPECIFICATIONS
3.1 NCPDP V5.1 CLAIM TRANSACTION FORMAT Page 3-1 3.2 NCPDP 1.1 BATCH TRANSACTION STANDARD Page 3-21
SECTION 4 – ERROR RESPONSE SPECIFICATIONS
4.1 ERROR RESPONSE SPECIFICATIONS Page 4-1 4.2 PHARMACY EMC PROOF REPORTS Page 4-2
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-1 Section 1 NCPDP v5.1
Introduction November 2011 Version
SECTION 1.1 – NEW JERSEY DMAHS INTRODUCTION
New Jersey Division of Medical Assistance and Health Services (DMAHS) and Molina Medicaid Solutions are very pleased to make available this November 2011 Version of the NCPDP-Health Insurance Portability and Accountability Act (HIPAA) Companion Guide. This document represents our ongoing effort to adhere to the HIPAA transaction set requirements. HIPAA provides all healthcare entities a tremendous opportunity to realize many administrative and systemic benefits because it provides a national standard of transaction and code sets for the electronic exchange of healthcare information. New Jersey DMAHS and Molina Medicaid Solutions are committed to the implementation of all HIPAA transaction sets as the sole format for all state and federal programs processed through the New Jersey Medicaid Management Information System (NJMMIS) at Molina Medicaid Solutions. The purpose of this manual is to provide information necessary to electronically submit Point of Sale (POS) claims and Pharmacy Electronic Data Interchange (EDI) claims to Molina Medicaid Solutions, our fiscal agent. HIPAA requirements apply to all State Pharmacy benefit claims including Medicaid and NJ FamilyCare Fee-For-Service (FFS) pharmacy claims, Pharmaceutical Assistance to the Aged and Disabled (PAAD), Senior Gold Prescription Discount Program, AIDS Drug Distribution Program (ADDP), and Cystic Fibrosis (CF) program. This manual is to be used in conjunction with the National Electronic Data Interchange Transaction Set Implementation Guides. The Implementation Guides can be obtained exclusively from NCPDP for members by calling 1-480-477-1000 or are available for download on their web site at www.ncpdp.org. The Implementation Guides provide the National HIPAA transaction and code set requirements, compared to the New Jersey DMAHS Companion Guide, which only provides the supplemental requirements specific to New Jersey DMAHS, as permitted within the structure of the NCPDP-HIPAA transaction sets. All providers who submit claims electronically to New Jersey DMAHS must adhere to the NCPDP-HIPAA Implementation Guide and the New Jersey DMAHS Companion Guide requirements. This Companion Guide addresses the NCPDP Version 5.1 and 1.1 Batch Version transaction sets. HIPAA does not mandate the use of these transaction sets for the exchange of healthcare data. Any provider may continue to submit paper claims, except for compound drugs, and receive a paper remittance advice. However, if a provider elects to submit claims electronically and/or receive an electronic remittance advice, HIPAA does require the use of standard transaction and code sets. Please note that there is a level of interpretation required when reviewing the Implementation Guides. Additional changes may be required to bring our Companion Guide in line with the intent of the Implementation Guides. Therefore, this document is subject to change. All comments, suggestions, and/or questions regarding this Companion Guide should be directed to the New Jersey DMAHS NCPDP Coordinator:
http://www.ncpdp.org/
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-2 Section 1 NCPDP v5.1
Introduction November 2011 Version
Lorraine Harris, NCPDP Coordinator New Jersey Medicaid P.O. Box 712 Trenton, NJ 08625-0712 Phone: 609-631-6616 Email: [email protected] Submitters are requested to refrain from contacting Molina Medicaid Solutions Provider Services regarding related HIPAA issues and questions.
mailto:[email protected]
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-3 Section 1 NCPDP v5.1
Introduction November 2011 Version
SECTION 1.2 – HIPAA BACKGROUND In the early 1990s, the Bush Administration assembled an advisory group of health care industry leaders to discuss ways to reduce health care administrative costs across the nation. This group, which is now recognized as the Workgroup for Electronic Data Interchange (WEDI), recommended that Federal legislation be passed to implement a nationwide standard of transaction and code sets to be used by the healthcare industry. This law was entitled “The Health Insurance Portability and Accountability Act” (HIPAA) and was enacted on August 21, 1996 under the Clinton Administration. HIPAA requires several provisions. One such provision dealt with the portability of health insurance coverage during a change in employment, and primarily affected employers and health insurers. This provision has already gone into effect. Another provision often referred to “Administrative Simplification”, deals with the implementation of healthcare standards, of which transaction and code sets are but one part. Although this Companion Guide deals with electronic pharmacy (NCPDP) claims transaction sets, there are several others that will be required by the mandatory implementation date of October 16, 2003:
Eligibility Inquiry and Response: HIPAA mandates the use of Version 4010 of the X12 270/271 Eligibility & Benefit Inquiry & Response EDI Transactions for this purpose.
Claim Transaction Sets: HIPAA mandates the use of 837 Professional, Institutional, and Dental transaction sets. (Please see the New Jersey HIPAA 837 Companion Guide at www.njmmis.com for specific New Jersey implementation dates.)
Claim Status Inquiry and Response: HIPAA mandates the use of Version 4010 of the X12 276/277 Claim Status Inquiry & Response EDI Transaction for this purpose.
Referral Certification & Authorization: HIPAA mandates the use of Version 4010 of the X12 278 Health Care Service Review EDI Transaction for this purpose.
Enrollment & Disenrollment: HIPAA mandates the use of Version 4010 of the X12 834 Benefit Enrollment & Maintenance EDI Transaction for this purpose.
Premium Payment & Remittance Advice: HIPAA mandates the use of Version 4010 of the X12 820 Group Premium Payment EDI Transaction for this purpose.
HIPAA also requires the standardization of code sets. Any coded field or data element contained in a HIPAA transaction must adhere to a national set of code set values, including medical services and diagnoses. As such, New Jersey DMAHS is required to discontinue the use of local codes, including pharmacy edit codes.
http://www.njmmis.com/
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-4 Section 1 NCPDP v5.1
Introduction November 2011 Version
In addition to the transaction and code set aspects, there are other requirements of the “Administrative Simplification” provision of HIPAA:
Privacy: Standards must be adopted by all health plans, clearinghouses, and providers that ensure the protection and appropriate disclosure of individually identifiable health information. A final rule has been published by the Department of Health and Human Services and requires mandatory implementation by April 2003.
Security: Standards must be adopted by all health plans, clearinghouses, and providers that ensure the integrity and confidentiality of the healthcare information. Whereas the transactions rule dealt specifically with electronic records, the security rule addresses healthcare information in all types of media. The Department of Health and Human Services has not yet published the final rule.
National Identifier Codes: Standards must be adopted by all health plans, clearinghouses, and providers regarding unique identifiers for providers, plans, employers, and individuals (beneficiaries). Presently, a final rule has been issued for the Employer ID. The Department of Health and Human Services for all other remaining identifiers has not yet published final rules.
Enforcement: The Office of Civil Rights has been appointed to administer enforcement efforts related to the privacy rule and has been given the authority to invoke penalties for compliance failures.
Although this Companion Guide deals with only one aspect of the entire “Administrative Simplification” provision, it is worth noting that all covered entities (health plans, clearinghouses, and providers) and their business partners are required to adhere to all aspects of the provision.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-5 Section 1 NCPDP v5.1
Introduction November 2011 Version
SECTION 1.3 – HIPAA INTERNET LINKS The following is a list of government agencies, industry leaders, and transaction and code set standards organizations associated with HIPAA. Although this is not an exhaustive list, each entity plays an integral role in the success of HIPAA and collectively, represents a wealth of information that could not otherwise be included in our Companion Guide.
Accredited Standards Committee (ASC X12)
ASC X12 develops and maintains standards for inter-industry electronic interchange of business transactions. http://www.x12.org/
American Medical Association (AMA)
This site is a resource for the Current Procedural Terminology 4th Edition codes (CPT-4). The AMA copyrights the CPT codes. http://www.ama-assn.org/
Association for Electronic Health Care Transactions (AFEHCT)
A healthcare association dedicated to promoting the interchange of electronic healthcare information. http://www.afehct.org/
Centers for Medicare and Medicaid Services (CMS)
Formerly known as HCFA, this site provides the Electronic Health Care Transactions and Code Sets Model Compliance Plan. http://www.cms.gov/hipaa/hipaa2/ This site is the resource for information related to the Healthcare Common Procedure Coding System (HCPCS). http://cms.hhs.gov/medicare/hcpcs/ This site is the resource Medicaid HIPAA information related to the Administrative Simplification provision. http://www.cms.gov/medicaid/hipaa/adminsim/
Designated Standard Maintenance Organizations (DSMO)
This site is a resource for information about the standard setting organizations, and transaction change request system. http://www.hipaa-dsmo.org/
http://www.x12.org/http://www.ama-assn.org/http://www.afehct.org/http://www.cms.gov/hipaa/hipaa2/http://cms.hhs.gov/medicare/hcpcs/http://www.cms.gov/medicaid/hipaa/adminsim/http://www.hipaa-dsmo.org/
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-6 Section 1 NCPDP v5.1
Introduction November 2011 Version
Health Level Seven (HL7)
HL7 is one of several ANSI accredited Standards Development Organizations (SDO), and is responsible for clinical and administrative data standards. http://www.hl7.org/
Medicaid HIPAA Compliant Concept Model (MHCCM)
This site presents the Medicaid HIPAA Compliance Concept Model, information and a toolkit. http://www.mhccm.org/
National Council of Prescription Drug Programs (NCPDP)
The NCPDP is the standards and codes development organization for pharmacy. http://www.ncpdp.org/
Office for Civil Rights (OCR)
OCR is the Health and Human Services Office responsible for enforcing the Privacy Rule under HIPAA. http://www.hhs.gov/ocr/hipaa/
United States Department of Health and Human Services (DHHS)
This site is a resource for the Notice of Proposed Rule Making, rules and other information regarding HIPAA. http://aspe.hhs.gov/admnsimp/
Washington Publishing Company (WPC)
WPC is a resource for HIPAA required transaction implementation guides and code sets. http://www.wpc-edit.com/hipaa/
Workgroup for Electronic Data Interchange (WEDI)
A workgroup dedicated to improving healthcare through electronic commerce, which includes the Strategic National Implementation Process (SNIP) for complying with the administrative simplification provisions of HIPAA. http://www.wedi.org
http://www.hl7.org/http://www.mhccm.org/http://www.ncpdp.org/http://www.hhs.gov/ocr/hipaa/http://aspe.hhs.gov/admnsimp/http://www.wpc-edit.com/hipaa/http://www.wedi.org/
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-7 Section 1 NCPDP v5.1
Introduction November 2011 Version
SECTION 1.4 – COMPANION GUIDE ORGANIZATION The New Jersey DMAHS NCPDP-HIPAA Companion Guide is organized into the following sections to provide the necessary information, policies, processes, and requirements to submit pharmacy claims electronically: Section 2 – Electronic Data Interchange The section contains instructions and processes for becoming approved as an electronic submitter for HIPAA transactions, the process for testing HIPAA transactions, and telecommunication and media specifications. Section 3 – NCPDP Specifications This section details the supplemental requirements to the NCPDP Telecommunication Standard Implementation Guide Version 5 Release 1 and the NCPDP Batch Standard Version 1.1 Implementation Guide that are required by New Jersey DMAHS. Both formats require the same transaction set when submitting pharmacy claims. Section 4 – Error Response Specifications This section details the error response requirements that are used by New Jersey DMAHS when NCPDP Version 1.1 batch transactions are received and the system finds an error in the integrity of the batch file.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-8 Section 1 NCPDP v5.1
Introduction November 2011 Version
SECTION 1.5 – CHANGES COMPARED TO PRIOR VERSION
This section lists additional changes made to this November 2011 Version of the NCPDP-HIPAA Companion Guide compared to the previous version. Changes with an asterisk * in the Page# column indicate changes made for the mandatory submission of NPIs on all HIPAA electronic claims, and will become effective on May 23, 2008. All existing payer-specific requirements will remain in effect after May 23, 2008.
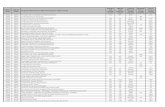
Page# Change November 2011 Version 3-4 Changed requirement for field 335-2C.
Page# Change July 2010 Version Multiple Changed Unisys to Molina Medicaid Solutions throughout the document.
2-3 Removed HMO Encounters specific requirements.
2-5 Added attention line for mailing address.
3-1 Removed HMO Encounters specific requirements.
3-3 Removed HMO Encounters specific requirements from fields 104-A4, 202-B2 and 110-AK.
3-4 Removed HMO Encounters specific requirements from fields 332-CY, 305-C5, 307-C7 and 335-2C.
3-5 Removed HMO Encounters specific requirements from field 466-EZ,
3-6 Removed HMO Encounters specific requirements from comments for COB/Other Payments Segment.
3-7 Removed HMO Encounters specific requirements from comments for COB/Other Payments Segment.
3-9 Removed HMO Encounters specific requirements from fields 443-E8, 431-DV and 472-6E.
3-10 Removed HMO Encounters specific requirements from fields 455-EM, 436-E1, 407-D7, 458-SE, 459-ER and 408-D8.
3-11 Removed HMO Encounters specific requirements from fields 308-C8, 600-28, 461-EU and 462-EV.
3-13 Removed HMO Encounters specific requirements from comments for Compound Segment and fields 409-D9, 412-DC and 433-DX.
3-14 Removed HMO Encounters specific requirements from field 426-DQ.
3-16 Removed HMO Encounters specific requirements from fields 104-A4, 202-B2, 110-AK, 111-AM and 332-CY.
3-17 Removed HMO Encounters specific requirements from fields 455-EM, 436-E1 and 407-D7.
4-1 Removed HMO Encounters specific requirements from comments for Error Response Specifications.
Page# Change February 2009 Version 3-6 Changed requirements for field 301-C1 GROUP ID.
Page# Change May 23, 2008 Version 1-8 Added all changes from prior versions of the NJ Medicaid NCPDP-HIPAA Companion Guide to be
included in this section.
3-3* Added 01 qualifier and comment to enter National Provider Identifier for fields 202-B2 SERVICE PROVIDER ID QUALIFIER and 201-B1 SERVICE PROVIDER ID. Also removed requirement to enter qualifier 05 and entry of Medicaid Provider ID and changed HMO-specific requirements for these fields.
3-5* Added 08 qualifier and comments for entry of State License Number for non-covered entities for fields 466-EZ PRESCRIBER ID QUALIFIER and 411-DB PRESCRIBER ID.
3-9 Added new Medicare Part D Plan ID DFX, Fox Insurance Company and MED, Part D Other for entry in field 340-7C Other Payer ID.
3-11 Added Plan B ® requirements for entry in field 402-D2 PRESCRIPTION/SERVICE REFERENCE NUMBER.
3-15 Added comments clarifying requirements for field 433-DX PATIENT PAID AMOUNT SUBMITTED.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-9 Section 1 NCPDP v5.1
Introduction November 2011 Version
Page# Change May 23, 2008 Version – (continued) 3-16 Changed requirements in the Clinical Segment for fields 111-AM SEGMENT IDENTIFICATION, 491-VE
DIAGNOSIS CODE COUNT, 492-WE DIAGNOSIS CODE QUALIFIER and 424-DO DIAGNOSIS CODE.
3-17* Added 01 qualifier and comment to enter National Provider Identifier for fields 202-B2 SERVICE PROVIDER ID QUALIFIER and 201-B1 SERVICE PROVIDER ID for Reversal Transactions. Also removed requirement to enter qualifier 05 and entry of Medicaid Provider ID and changed HMO-specific requirements for these fields.
3-18 Added Plan B ® requirements for entry in field 402-D2 PRESCRIPTION/SERVICE REFERENCE NUMBER for Reversals.
Page# Change January 2007 Version 3-8 Added new Medicare Part D Plan ID‟s for 2007 for entry in field 340-7C - Other Payer ID. (AmeriHealth
65, Bravo by Elder Care, Envision Rx Plus, HealthSpring Prescription Plan, NMHC Group Solutions, SAMAscript, SierraRx)
Page# Change October 2006 Version 1-2 Changed phone number for Lorraine Harris, DMAHS NCPDP Coordinator.
3-4 Added comments to clarify HMO required entry for field 332-CY - PATIENT ID.
3-5 Removed the comments (to be issued) from field 302-C2 CARDHOLDER ID.
3-9 Added HMO requirements for field 443-E8 - OTHER PAYER DATE.
3-16 Added comments to clarify HMO required entry for field 332-CY - PATIENT ID.
Page# Change April 2006 Version 2-3 Changed reference of monthly remittance advice to weekly 835 remittance advice.
3-1 Changed comment of HMO Encounter claims submitted monthly to weekly.
3-6 & 3-7 Revised comments for COB/Other Payments Segment to identify specific FFS and HMO related requirements.
3-7 Removed previous comment of HMO – not required for field 339-6C.
3-8 Added HMO requirement for field 340-7C when reporting third party payments.
3-9 Added HMO requirement for field 431-DV when reporting third party payments.
4-1 Changed reference of monthly remittance advice to weekly 835 remittance advice.
Page# Change January 2006 Version 1-1 Removed paragraph referencing continued support of version 3C through September 2004 and
requirement of adherence to HIPAA transaction sets for claims with dates of service on or after January 2004.
1-7 Changed section name from Section 4 – 997 Acknowledgement Specifications to Error Response Specifications and renumbered section due to the removal of the previous 835 Specifications section. The information previously contained in the 835 Specifications section can be found in the New Jersey Medicaid HIPAA Companion Guide Version 4010 Addenda.
1-8 New section; Section 1.5 – Changes Compared To Prior Version, added to document changes compared to the prior version.
2-1 Revised NCPDP 1.1 testing process under Section 2.1 - HIPAA Testing.
2-1 to 2-3 Revised Section 2.2 – Telecommunication Specifications to now include Internet Specifications, Submitter Registration - Obtaining a Username and Password and Logging In To Web Site.
2-4 to 2-5 Added Section 2.3 – Electronic Media Specifications that includes CD-ROM Specifications and Tape Cartridge Specifications, Mailing Address For CD-ROM And Tape Cartridge Submissions.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 1-10 Section 1 NCPDP v5.1
Introduction November 2011 Version
Page# Change January 2006 Version – (continued) 2-6 Added Section 2.4 - Interchange Naming Convention.
3-1 to 3-17 Made revisions to Section 3.1 – NCPDP V5.1 Claim Transaction Format to include requirements for HMO encounters and Medicare Part D special requirements.
3-2 Added B3 Transaction Code for return-to-stock of unit dose medications for LTC Pharmacies.
3-2 to 3-3 Added Medicare Part D special requirements for field 104-A4 Processor Control Number.
3-3 Added Medicare Part D special requirements for field 110-AK Software Vendor/Certification ID.
3-5 to 3-6 Added Medicare Part D special requirements for COB/Other Payments Segment.
3-7 to 3-8 Added Medicare Part D special requirements for field 340-7C Other Payer ID.
3-8 Added Medicare Part D special requirements for field 342-HC Other Payer Amount Paid Qualifier and field 431-DV Other Payer Amount Paid.
3-13 Revised comments regarding Prior Authorization Segment.
3-14 Added Medicare Part D special requirements for field 104-A4 Processor Control Number for Reversal Transactions.
3-15 Added Medicare Part D special requirements for field 110-AK Software Vendor/Certification ID for Reversal Transactions.
3-19 Made revisions to Section 3.2 – NCPDP 1.1 Batch Transaction Standard to include requirements for HMO encounters. Also added column for 'Positions' to the NCPDP 1.1 batch record layout tables to identify the positional relationship for each field since these are fixed position fields.
4-1 Changed section name from Section 4 – 997 Acknowledgement Specifications to Error Response Specifications and renumbered section due to the removal of the previous 835 Specifications section. The information previously contained in the 835 Specifications section can be found in the New Jersey Medicaid HIPAA Companion Guide Version 4010 Addenda.
4-2 Added Section 4.2 - Pharmacy EMC Proof Reports.
September 15, 2003 Version – Original Version of the NCPDP- HIPAA Companion Guide
-
DMAHS NCPDP-HIPAA Companion Guide
Page 2-1 Section 2 NCPDP v5.1
Electronic Data Interchange November 2011 Version
SECTION 2.1 – HIPAA TESTING NCPDP 1.1 batch submitters wishing to test their file formats are to contact the Molina Medicaid Solutions EDI Unit at 609-588-6051 prior to sending a NCPDP 1.1 batch test file into Molina Medicaid Solutions for processing. New Jersey Medicaid does NOT offer full production testing, including the creation of an 835 transaction, as part of internal testing. However, New Jersey Medicaid has obtained a third-party certification of our capability to produce a compliant 835 transaction. LTC B3 Rebill testing must be coordinated with Lorraine Harris at (609) 631-6616. SECTION 2.2 – TELECOMMUNICATION SPECIFICATIONS Internet Specifications (NCPDP 1.1 Batch Submissions Only)
New Jersey Medicaid and Molina Medicaid Solutions have deployed an Internet-based solution that will allow the electronic exchange of NCPDP 1.1 batch transactions through the HIPAA Claims link (www2.njmmis.com) on the NJMMIS Web site www.njmmis.com. NCPDP 1.1 batch transactions can be sent seven days a week, Sunday thru Saturday, with the following exceptions, which have been scheduled as maintenance windows.
Wednesdays, 10 p.m. thru Thursdays 2 a.m. and
Saturdays, 8 p.m. thru Sundays 4 a.m., Eastern time. NCPDP 1.1 batch submitters using the Web site will drop-off NCPDP 1.1 batch files and pick-up Response files through a secure area of the New Jersey Medicaid Web site. A valid username and password is required before access is granted for drop-off and pick-up. Only electronic data interchanges in the 837 4010A1 addenda and NCPDP 1.1 batch formats will be accepted for processing on the Web site. Electronic data in the proprietary EMC formats will NOT be accepted on the Web site. Submitter Registration - Obtaining a Username and Password EDI Submitters will be registered on the submitter database upon processing of their New Jersey Medicaid HIPAA EDI Agreement and will receive their Username and Password via the United States Postal Service mail. The New Jersey Medicaid HIPAA EDI Agreements and instructions are found in the Trading Partner Agreement Section (Section 2.7) of the New Jersey Medicaid HIPAA Companion Guide Version 4010 Addenda located on the www.njmmis.com New Jersey Medicaid Web site. These documents can also be found on the New Jersey Medicaid Web site using the Forms & Documents link, then Choose a Type: All and Choose a Topic: HIPAA, press the Submit Request button.
http://www.njmmis.com/http://www.njmmis.com/
-
DMAHS NCPDP-HIPAA Companion Guide
Page 2-2 Section 2 NCPDP v5.1
Electronic Data Interchange November 2011 Version
Submitters are expected to maintain their own passwords and will be able to change their password thru a link on the HIPAA Claims Web site. Within 5 business days, your username and password will be sent to the submitter information listed on the NJMMIS Molina Medicaid Solutions Submitter database, via the United States Postal Service mail. Logging In To Web Site
1. After receiving your username and password, access the Web site (www.njmmis.com) and select the HIPAA Claims link (www2.njmmis.com) from the menu options on left side of screen.
2. Enter your username and password and click on Submit.
3. On the Welcome to the New Jersey Medical Assistance Program Transaction Services Home screen click on the upload link at the upload or download HIPAA files prompt to upload files for processing.
Only files in the approved HIPAA formats may be uploaded.
You can upload up to five files at a time. All files being submitted must be of the same type as indicated in the file type selection area. (i.e. Up to five NCPDP 1.1 batch files can be submitted at one time. If you wish to also submit 837 – 4010X098A1 Professional files these must be sent after the previous file type has been submitted.
Users should allow 30 seconds or more before submitting additional files allowing for file processing between upload attempts.
The combined file size must not exceed 20 MB for NCPDP 1.1 batch files. (i.e. If multiple files are being submitted at one time the combined file sizes must not exceed 20 MB.
While a combined file size of up to a maximum size of 20 MB for NCPDP 1.1 may be submitted, Molina Medicaid Solutions will not perform detailed analysis on files in excess of 5 MB when assisting submitters in resolving errors resulting in the full or partial rejection of a submission. Submitters requiring the technical assistance of Molina Medicaid Solutions EDI staff will be requested to resubmit the claims in question with one or more files where the file size does not exceed 5 MB.
Files can be in ZIP or DAT format only. Please refer to the section on Interchange Naming Convention discussed later in this section for additional information regarding compressed files and naming conventions.
4. Click on the download link at the upload or download HIPAA files prompt to download (pick-
up) your 835 remittance files.
835 remittance files are available for downloading the Wednesday following the weekend processing cycle.
5. Click on the Recent Uploads link of the View a list of Recent Uploads prompt to view the
status of the NCPDP 1.1 batch file and to pick-up the Response file.
http://www.njmmis.com/
-
DMAHS NCPDP-HIPAA Companion Guide
Page 2-3 Section 2 NCPDP v5.1
Electronic Data Interchange November 2011 Version
The TA1/Error column will report if there were any initial errors found in the file or 'No Error' is reported upon initial processing of the file.
The 997/Response column will report if the Response file is available. The Response file will be available on the morning following the running of the NCPDP 1.1 batch file thru the NJMMIS POS system if no initial errors are reported in the TA1/Error column.
The Response file available for downloading will follow the following naming convention.
Submitter ID#_MM_DD_YY_HH_MM_SS_Batch #_Pharm.txt
-
DMAHS NCPDP-HIPAA Companion Guide
Page 2-4 Section 2 NCPDP v5.1
Electronic Data Interchange November 2011 Version
SECTION 2.3 – ELECTRONIC MEDIA SPECIFICATIONS
In addition to the Internet and the Point-of-Sale system, New Jersey Medicaid will permit the submission of NCPDP 1.1 batch transactions on Compact Disc (CD-ROM). New Jersey Medicaid intends to discontinue the use of other media, such as tape and diskette. However, tape cartridge will remain available for those entities whose monthly claim volume exceeds 1,000.
CD-ROM Specifications
Please be advised that CD-ROM submissions will NOT be returned to the EDI Submitter and their receipt and processing status acknowledgements will have to be retrieved from the Web site. These will NOT be sent to the submitter. NJ Medicaid will accept NCPDP 1.1 batch transaction sets submitted on the following types of CD-ROM discs. CD-RW (Rewritable) or CD-R (Recordable)
74 min. 650MB
80 min. 700MB Tape Cartridge Specifications New Jersey Medicaid has discontinued the use of other media, such as round reel tape, and diskette. In lieu of the discountenance of round reel tapes, New Jersey Medicaid will allow the exchange of NCPDP 1.1 batch transactions on tape cartridge media. Tape cartridges will be returned to the submitter‟s address listed on the Molina Medicaid Solutions NJMMIS Submitter file following the weekly adjudication cycle. Please be advised that receipt and processing status acknowledgements will have to be retrieved from the Web site. These will NOT be sent to the submitter. New Jersey Medicaid will accept NCPDP 1.1 batch transaction files submitted on the following types of tape cartridge media.
18-Track 3480 (IBM 3480 compatible)
18-Track 3490 (IBM 3490 compatible)
36-Track 3490E (IBM 3490E compatible)
All tape cartridge interchanges must be recorded in Extended Binary Coded Decimal Interchange Code (EBCDIC) and have an internal label in the standard IBM tape label format. The external label of the CD-ROM or Tape Cartridge submission must appear as follows:
-
DMAHS NCPDP-HIPAA Companion Guide
Page 2-5 Section 2 NCPDP v5.1
Electronic Data Interchange November 2011 Version
NJMMIS NCPDP 1.1 BATCH – CD-ROM or CART TAPE SUBMISSION
Creation Date: (a) Submitter ID #: (g)
Cart/CD #: (b) Submitter Name: (h)
Record Count: (c)
$ Amount: (d)
Trans Type: (e) Phone #: (i)
Density: (f)
(a) Creation Date: The creation date of the submission as it appears on the encoded
claims and as it appears in the Transaction Header Section.
(b) Cart/CD#: An external identifying number.
(c) Record Count: The number of records included in the interchange.
(d) $ Amount: The total dollar amount of all the transactions billed in the interchange.
(e) Trans Type: The type of transaction set encoded on the tape: NCPDP 1.1.
(f) Density: Specify on the outside of the label the recording density used when creating the tape cartridge.
(g) Submitter ID #: The Submitter‟s ID number assigned by Molina Medicaid Solutions.
(h) Submitter Name: The name of the Submitter submitting the interchange.
(i) Phone Number: This is not required, just helpful.
Mailing Address For CD-ROM And Tape Cartridge Submissions CD-ROMs and tape cartridges must be properly packaged for mailing. New Jersey Medicaid is not responsible for damage occurring to interchanges in the mailing process. All CD-ROM and tape cartridge submissions are to be mailed to:
Via U.S. Mail Other Carriers Computer Operations Computer Operations Attn: EDI Attn: EDI Molina Medicaid Solutions Molina Medicaid Solutions P.O. Box 4814 3705 Quakerbridge Road Trenton, New Jersey 08650- 4814 Suite 101 Trenton, New Jersey 08619
-
DMAHS NCPDP-HIPAA Companion Guide
Page 2-6 Section 2 NCPDP v5.1
Electronic Data Interchange November 2011 Version
SECTION 2.4 - INTERCHANGE NAMING CONVENTION Regardless of the media CD-ROM, Cartridge Tape or Web site, for the submission of NCPDP 1.1 batch transactions, New Jersey Medicaid will support the DOS file-naming convention of 8-characters followed by a 3-character extension. The naming convention for batch files is as follows: The file name format MUST be one alphabetic (A thru Z) character ('A' for the first transmission of the day, 'B' for the second, etc. up to 'Z') followed by the 7-digit EDI Submitter ID Number (as assigned by Molina Medicaid Solutions) with the REQUIRED 3-character file extension of .DAT. Example: A1234567.DAT Any interchanges that do not follow this naming convention will NOT be processed. The EDI Submitter number in the interchange name MUST match the EDI Submitter number in the Transaction Header Segment. NCPDP 1.1 batch submissions may include any number of claims as long as the size of the interchange being submitted does NOT exceed 20 megabytes. There is no minimum or maximum number of claims required for an EDI submission, regardless of the media or method of submission, except that the size of the interchange being submitted does NOT exceed 20 MB. EDI submissions with file properties set to “READ ONLY” will NOT be accepted. Multiple interchanges may be sent daily however an EDI Submitter is NOT to exceed more than 999 interchanges in a day (from the period of midnight to midnight). Only one Transaction Header and Trailer Record must be contained within a file. Multiple files may be submitted in a compressed format with a .zip file extension. (i.e. multiple files within one .zip file, all files containing only one Transaction Header and Trailer Record.)
A1234567.zip – Compressed file
A1234567.dat – 1st file in compressed file
B1234567.dat – 2nd file in compressed file
C1234567.dat – 3rd file in compressed file. If multiple files are being submitted at one time the combined file sizes must not exceed 20 MB.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-1 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
SECTION 3.1 – NCPDP V5.1 CLAIM TRANSACTION FORMAT
General Information: All numeric fields are to be right justified by the software vendor. All alpha-numeric fields are to be left justified by the software vendor. Billing and Reversal transactions will be accepted. The following transactions will not be accepted:
Eligibility, Prior Authorization, Information Reporting, or Controlled Substance transactions.
The Rebill transaction is only accepted from LTC pharmacies. Special Requirements: The following is a detail of our submission requirements. Medicare Part D Special Requirements: The remarks section for each field will reference “PART-D” when listing specifications for claims being submitted to New Jersey for Medicare Part D coverage claims. Field 101-A1 BIN Number You are to continue to use the existing BIN Number of 610515 on all transactions submitted to Molina Medicaid Solutions for processing. Field 104-A4 Processor Control Number You are currently required to enter a value of NJP followed by the seven digit EDI Submitter ID that has been assigned to you by Molina Medicaid Solutions. Effective for all transactions submitted as of January 1, 2006 you are be required to populate this field with new Processor Control Number values when submitting claims that were submitted to and approved by the Medicare PDP and the claim is now being submitted to New Jersey for consideration of the outstanding Medicare Part D patient deductible and/or coinsurance/co-payment responsibility. These PCN values are required by Medicare Part D to enable tracking of out-of-pocket payments made on behalf of the Medicare Part D beneficiary.
When submitting a claim for a beneficiary enrolled in either the State‟s Prescription Drug Program for the Aged and Disabled (PAAD) or the State‟s Senior Gold prescription drug program, you are to submit the claim with a Processor Control Number of PAAD.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-2 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
When submitting a claim for a beneficiary enrolled in the State‟s AIDS Drug Distribution Program (ADDP), you are to submit the claim with a Processor Control Number of ADDP.
When submitting a claim for a beneficiary enrolled in other than the State‟s Prescription Drug Program for the Aged and Disabled (PAAD), the State‟s Senior Gold prescription drug program, or the State‟s AIDS Drug Distribution Program (ADDP), you are to submit the claim with a Processor Control Number of SUPPNJ.
Claims for beneficiaries that are not enrolled in Medicare Part D and claims where New Jersey is being billed as the primary payer because Medicare Part D has denied coverage on the claim should be submitted with a Processor Control Number that is equal to ten (10) spaces. Field 110-AK Software Vendor/Certification ID Effective for all transactions submitted as of January 1, 2006 you are be required to populate this field with the data that you were previously reporting in the Processor Control Number field. Specifically, the first three positions of this field must contain the value of NJP. Starting in position four of this field, you are to report the seven digit EDI Submitter ID that has been assigned to you by Molina Medicaid Solutions. This EDI Submitter ID is the certification id that Molina Medicaid Solutions uses to confirm that you have been certified for the submission of electronic claims.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-3 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
Transaction Header Segment Required Field Field Name Mandatory
or Optional Remarks
101-A1 BIN NUMBER M Must be 610515
102-A2 VERSION/RELEASE NUMBER M Must be 51
103-A3 TRANSACTION CODE M B1 = Billing B3 = Rebill (valid only for return-to-stock of unit dose medications for LTC Pharmacies) Note - B2 see page 3-16
104-A4 PROCESSOR CONTROL NUMBER M See pages 3.1 – 3.2 Ten Spaces = Beneficiaries not enrolled in
Medicare Part D and claims where New Jersey is being billed as the primary payer because Medicare Part D has denied coverage on the claim.
PAAD = Beneficiaries enrolled in New Jersey‟s Prescription Drug Program for the Aged and Disabled (PAAD) Program or New Jersey‟s Senior Gold Program
ADDP = Beneficiaries enrolled in New Jersey‟s AIDS Drug Distribution (ADDP) Program
SUPPNJ = Beneficiaries enrolled in other than New Jersey‟s (PAAD), Senior Gold or (ADDP) Prescription Drug Programs
109-A9 TRANSACTION COUNT M
202-B2 SERVICE PROVIDER ID QUALIFIER M Must be 01 = National Provider Identifier (NPI)
201-B1 SERVICE PROVIDER ID M Enter 10-digit National Provider Identifier (NPI)
401-D1 DATE OF SERVICE M YYYYMMDD
110-AK SOFTWARE VENDOR/CERTIFICATION ID M NJP+7 digit submitter number e.g. NJP1234567
Patient Segment Required Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 01
331-CX PATIENT ID QUALIFIER O
332-CY PATIENT ID O
304-C4 DATE OF BIRTH M YYYYMMDD
305-C5 PATIENT GENDER CODE M 1 digit 1 = Male 2 = Female
310-CA PATIENT FIRST NAME M Enter full first name of beneficiary
311-CB PATIENT LAST NAME M Enter full last name of beneficiary
322-CM PATIENT STREET ADDRESS O
323-CN PATIENT CITY ADDRESS O
324-CO PATIENT STATE / PROVINCE ADDRESS O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-4 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Patient Segment Required Field Field Name Mandatory
or Optional Remarks
325-CP PATIENT ZIP/POSTAL ZONE O
326-CQ PATIENT PHONE NUMBER O
307-C7 PATIENT LOCATION M Up to 2 digits 0 = Not Specified 1 = Home 2 = Inter-Care i.e., Intermediate Care Facility 3 = Nursing Home i.e., Nursing Facility 4 = Long Term/Extended Care 5 = Rest Home 6 = Boarding Home 7 = Skilled Care Facility i.e., SNF 8 = Sub-Acute Care Facility i.e., ALRs /CPCHs 9 = Acute Care Facility 10 = Outpatient 11 = Hospice
333-CZ EMPLOYER ID O
334-1C SMOKER / NON-SMOKER CODE O 1 digit 1 = Non-Smoker 2 = Smoker
335-2C PREGNANCY INDICATOR O 1 digit 1 = Non Pregnant 2 = Pregnant
Pharmacy Provider Segment Optional Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O 02
465-EY PROVIDER ID QUALIFIER O
444-E9 PROVIDER ID O
Prescriber Segment Required
Field Field Name Mandatory or Optional
Remarks
111-AM SEGMENT IDENTIFICATION M 03
466-EZ PRESCRIBER ID QUALIFIER M 01 = National Provider Identifier (NPI) 08 = State License Number
411-DB PRESCRIBER ID M If EZ = 01 – Enter 10-digit National Provider Identifier (NPI)
HIPAA NON-COVERED ENTITIES ONLY: If EZ = 08 – Enter State License Number, at your
option, proceed with 2-character state code. (e.g.NJMA123456)
Omit entry of spaces and special characters in this field.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-5 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Prescriber Segment Required Field Field Name Mandatory
or Optional Remarks
467-1E PRESCRIBER LOCATION CODE O
427-DR PRESCRIBER LAST NAME O
498-PM PRESCRIBER PHONE NUMBER O
468-2E PRIMARY CARE PROVIDER ID QUALIFIER
O
421-DL PRIMARY CARE PROVIDER ID O
469-H5 PRIMARY CARE PROVIDER LOCATION CODE
O
470-4E PRIMARY CARE PROVIDER LAST NAME O
Insurance Segment Required Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 04
302-C2 CARDHOLDER ID M First 10 digits of Beneficiary ID (see 303-C3) or the 16 digit number on the Health Benefits ID card
312-CC CARDHOLDER FIRST NAME O
313-CD CARDHOLDER LAST NAME O
314-CE HOME PLAN O
524-FO PLAN ID O
309-C9 ELIGIBILITY CLARIFICATION CODE O
336-8C FACILITY ID O/M Mandatory for LTC Rebill – report the LTC facility Medicaid provider number – 7 digits
301-C1 GROUP ID O Omit or leave blank
303-C3 PERSON CODE M Last 2 digits of Beneficiary ID; when using the card control number from the Health Benefits ID card, leave blank
306-C6 PATIENT RELATIONSHIP CODE O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-6 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
COB/Other Payments Segment Fee For Service - Only required if beneficiary is covered by another payer. New Jersey, as a government agency, will continue to require the submission of a COB/Other Payments Segment for each insurer to whom the claim has been submitted prior to the submission of the claim to the State of New Jersey without exception. If we have knowledge of insurance resources that include drug coverage and a COB segment is not present on the incoming claim for each of the known insurance resources, then payment on your claim will be denied. When the insurance coverage is Medicare Part D, we expect the COB segment reflecting the adjudication by the Medicare Part D processor. Failure to include the COB segment on any claim for a Medicare Part D enrolled beneficiary for a drug product that is Medicare Part D covered by statute will result in the denial of your claim. Field 340-7C Other Payer ID New Jersey will continue to use a New Jersey specific code set to identify other third party resources. New values have been defined by the State of New Jersey for the specific Medicare approved PDPs. You will continue to use a value of 99 in the Other Payer ID Qualifier field (339-6C). The new Other Payer ID values that have been established in support of the Medicare Modernization Act (MMA) are listed below. Please be advised that the value of OTH cannot be used to identify Medicare Part D as the insurer. If the value of OTH is used to identify the COB segment as reflecting Medicare Part D rather than the appropriate value, the claim will be denied. Field 342-HC Other Payer Amount Paid Qualifier and Field 431-DV Other Payer Amount Paid The NCPDP standard allows for the reporting of up to six occurrences of Other Payer Amount Paid Qualifier and Other Payer Amount Paid. When reporting the actual amount of the payment made by the third party health plan, the Other Payer Amount Paid Qualifier is to be coded with a value of 08 (Sum of all reimbursement) and the amount reported in the Other Payer Amount Paid is to be the amount of the actual payment that you are scheduled to receive from the health plan. In the event that the health plan has approved the service but will make no payment on the claim because the payment due has been applied to either the patient‟s deductible liability and/or coinsurance/co-payment liability, an Other Payer Amount Paid Qualifier of 08 is not required. The amount to be reported to us as the patient deductible amount should be returned to you by the payer in the Amount Applied to Periodic Deductible field (Field 517-FH) on the Response Pricing Segment.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-7 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
The amount to be reported to us as the patient coinsurance/co-payment amount should be returned to you by the payer in the Amount of Copay/Co-Insurance field (Field 518-FI) on the Response Pricing Segment. An Other Payer Amount Paid Qualifier of 99 is to be used to report both the patient deductible liability as well as the patient coinsurance/co-payment liability. The first entry is to be used to report the patient deductible amount and the second entry is to be used to report the patient coinsurance/co-payment amount. When the claim involves only a coinsurance/co-payment amount, you still must code two entries with an Other Payer Amount Paid Qualifier of 99. The first entry must be coded with an Other Payer Amount Paid Qualifier of 99 and an Other Payer Amount Paid of zeros to indicate that there is no deductible amount on the claim and the second entry must be coded with an Other Payer Amount Paid Qualifier of 99 and an Other Payer Amount Paid that is equal to the patient coinsurance/co-payment amount. Do NOT submit two repetitions, each with zero dollars, unless the Part D payer provides zero dollars in both 517-FH and 518 –FI. Field 472-6E Other Payer Reject Code When the COB segment being provided reflects Medicare Part D, it is essential that you include on the transaction all reject codes returned to you by the Medicare Part D PDP. These codes will be used to determine if New Jersey will accept primary payer responsibility on a claim for a Medicare Part D enrolled beneficiary for a drug product that is deemed to be a Medicare Part D covered benefit by statute. The only codes that you are to report in this field are the reject codes that are returned to you by the health plan/insurer. You are not to augment this list of reject codes with any reject codes that are not present on the response transaction received from the health plan. (COB/Other Payments Segment Fee For Service - Only required if beneficiary is covered by another payer. Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 05
337-4C COORDINATION OF BENEFITS/OTHER PAYMENTS COUNT
O 1, 2, 3 A maximum of 4 occurrences is supported
338-5C OTHER PAYER COVERAGE TYPE O
339-6C OTHER PAYER ID QUALIFIER M Must be 99
340-7C OTHER PAYER ID M Values Provided by the State of New Jersey. Required for claims with other insurance; 3-character code identifies the other insurance Pharmacy Benefit Manager (PBM): Private TPL (Not Part D) ADV = Advance PCS AET = Aetna/USHC CAR = CareMark CIG = Cigna Continued on next page
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-8 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
Field Field Name Mandatory or Optional
Remarks
340-7C OTHER PAYER ID (continued) M EXP = Express Scripts FIR = FirstHealth NPA = NPA OTH = Other PAI = PAID PCS = PCS PRO = ProServ RES = Restat TRI = TriCareI UHS = United Health WEL = Well Point PART-D: Medicare C Plans CAE = Aetna US Healthcare CAP = Aetna US Healthcare PPO CAM = Americhoice CAH = Amerihealth 65 CEC = Evercare Choice CHO = Horizon Healthcare NJ COX = Oxford Health Plans NJ CUH = United Healthcare Medicare D Plans DAE = Aetna Life Insurance DAH = AmeriHealth 65 DAP = American Progressive Life and Health DBR = Bravo by Elder Care DCA = Coventry Advantra RX DCG = CIGNA DER = Envision Rx Plus DFH = First Health Premier DFX = Fox Insurance Company DHN = Health Net DHO = Horizon Healthcare DHS = HealthSpring Prescription Plan DHU = Humana DME = Medco Health Solutions DMH = Memberhealth DNM = NMHC Group Solutions DPA = Pacificare Life DPL = Pennsylvania Life DRX = RXAmerica DSA = SAMAscript DSI = SierraRx DSS = Silverscript DST = Sterling Plus RX DUA = United American Continued on next page
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-9 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
Field Field Name Mandatory or Optional
Remarks
340-7C OTHER PAYER ID (continued) M DUH = United Healthcare DUN = Unicare DWE = Wellcare MED = Part D Other
443-E8 OTHER PAYER DATE O
341-HB OTHER PAYER AMOUNT PAID COUNT O
342-HC OTHER PAYER AMOUNT PAID QUALIFIER
O/M Private TPL (Not Part D): Mandatory when applicable. PART-D: 08 = When reporting the actual amount of the
payment made by the third party health plan when applicable
99 = 1st occurrence of qualifier value of 99 to
report both the patient deductible liability 99 = 2
nd occurrence of qualifier value of 99 to
report the patient coinsurance/co-payment liability
431-DV OTHER PAYER AMOUNT PAID O/M Private TPL (Not Part D): Mandatory when applicable. PART-D: For 08 above, the amount of the actual payment
that you are scheduled to receive from the health plan
For the 1st 99 above enter the patient deductible
liability For the 2
nd 99 above report the patient
coinsurance/co-payment liability LTC Rebill: required when applicable
471-5E OTHER PAYER REJECT COUNT O
472-6E OTHER PAYER REJECT CODE M
Workers’ Compensation Segment Optional Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O 06
434-DY DATE OF INJURY O
315-CF EMPLOYER NAME O
316-CG EMPLOYER STREET ADDRESS O
317-CH EMPLOYER CITY ADDRESS O
318-CI EMPLOYER STATE/PROVINCE ADDRESS
O
319-CJ EMPLOYER ZIP/POSTAL ZONE O
320-CK EMPLOYER PHONE NUMBER O
321-CL EMPLOYER CONTACT NAME O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-10 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Workers’ Compensation Segment Optional Field Field Name Mandatory
or Optional Remarks
327-CR CARRIER ID O
435-DZ CLAIM/REFERENCE ID O
Claim Segment Required Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 07
455-EM PRESCRIPTION/SERVICE REFERENCE NUMBER QUALIFIER
M Must be 1 = RX
402-D2 PRESCRIPTION/SERVICE REFERENCE NUMBER
M 7 digit prescription number (left zero fill prescription numbers less than 7 positions) Plan B ® OTC claims enter a Service Reference Number up to 7 digits, omit spaces and special characters
436-E1 PRODUCT/SERVICE ID QUALIFIER M Must be 03
407-D7 PRODUCT/SERVICE ID M 11 digit NDC (compounds 11 zeros or 1 zero)
456-EN ASSOCIATED PRESCRIPTION/SERVICE REFERENCE #
O Partial fill not supported.
457-EP ASSOCIATED PRESCRIPTION/SERVICE DATE
O Partial fill not supported.
458-SE PROCEDURE MODIFIER CODE COUNT M 1, 2, 3, 4 A maximum of 4 occurrences is supported
459-ER PROCEDURE MODIFIER CODE M Used only when a procedure modifier code applies. Up to four modifiers can be sent.
442-E7 QUANTITY DISPENSED M 9(7)V999 LTC Rebill - Report actual metric quantity of service units administered. If all units are being recycled report „0‟ (zero).
403-D3 FILL NUMBER M Up to 2 digits
405-D5 DAYS SUPPLY M Up to 3 digits
406-D6 COMPOUND CODE M 1 digit
408-D8 DISPENSE AS WRITTEN (DAW)/PRODUCT SELECTION CODE
M 1 digit Blank = not dispensed as written 1 = dispense as written 2 to 99 = Not Applicable
414-DE DATE PRESCRIPTION WRITTEN M YYYYMMDD
415-DF NUMBER OF REFILLS AUTHORIZED M 2 digits - Enter up to 2 digits in 2 digit field reflecting number of refills authorized by prescriber
419-DJ PRESCRIPTION ORIGIN CODE O
420-DK SUBMISSION CLARIFICATION CODE O/M 8 is acceptable for compound claims as applicable
460-ET QUANTITY PRESCRIBED O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-11 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Claim Segment Required Field Field Name Mandatory
or Optional Remarks
308-C8 OTHER COVERAGE CODE M 00 = Not specified; pharmacist unaware of insurance coverage
01 = No other coverage; Pharmacist unaware of insurance coverage
02 = Other coverage exists – payment collected, TPL payment reported on claim
03 = Other coverage exists – claim not covered; drug product not covered by carrier
04 = Other coverage exists – payment not collected i.e., other insurance claim can not be processed electronically
05 = Managed care plan denial 06 = Other coverage denied – not participating
provider 07 = Other coverage exists, not in effect on DOS 08 = Claim is billing for copay; payment reflects
100% copayment
429-DT UNIT DOSE INDICATOR O
453-EJ ORIG PRESCRIBED PRODUCT/SERVICE ID QUALIFIER
O
445-EA ORIGINALLY PRESCRIBED PRODUCT/SERVICE CODE
O
330-CW ALTERNATE ID O
454-EK SCHEDULED PRESCRIPTION ID NUMBER
O
600-28 UNIT OF MEASURE M EA = each, GM = grams, and ML = Milliliters
418-DI LEVEL OF SERVICE O
461-EU PRIOR AUTHORIZATION TYPE CODE M 0 = No PA number 1 = PA number entered 5 = Exemption from Rx (i.e. Nonparticipating
pharmacy in other insurance provider network)
462-EV PRIOR AUTHORIZATION NUMBER SUBMITTED
O Enter 10-digit PA number in 11 digit field Enter „0‟ in first field position
463-EW INTERMEDIARY AUTHORIZATION TYPE ID
O
464-EX INTERMEDIARY AUTHORIZATION ID O
343-HD DISPENSING STATUS O Partial fill not supported. This field must be blank.
344-HF QUANTITY INTENDED TO BE DISPENSED
O Partial fill not supported.
345-HG DAYS SUPPLY INTENDED TO BE DISPENSED
O Partial fill not supported.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-12 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
DUR/PPS Segment Optional Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 08
473-7E DUR/PPS CODE COUNTER O 1, 2, 3…9 A maximum of 9 is supported
439-E4 REASON FOR SERVICE CODE O
440-E5 PROFESSIONAL SERVICE CODE O
441-E6 RESULT OF SERVICE CODE O 00 = Not specified 1A = Filled as is, false positive 1B = Filled prescription as Is 1C = Filled with different dose 1D = Filled with different directions 1E = Filled with different drug 1F = Filled with different quantity 1G = Filled with prescriber approval 1H = brand-to-generic change 1J = Rx-to-OTC change 1K = Filled with different dosage form 2A = Prescription not filled 2B = Not filled, directions clarified 3A = Recommendation accepted 3B = Recommendation not accepted 3C = Discontinued drug 3D = Regimen changed 3E = Therapy changed 3F = Therapy changed-cost increase
acknowledged 3G = Drug therapy unchanged 3H = Follow-up/report 3J = Patient referral 3K = Instructions understood 3M = Compliance aid provided 3N = Medication administered
474-8E DUR/PPS LEVEL OF EFFORT O
475-J9 DUR CO-AGENT ID QUALIFIER O
476-H6 DUR CO-AGENT ID O
Coupon Segment Optional Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O 09
485-KE COUPON TYPE O
486-ME COUPON NUMBER O
487-NE COUPON VALUE AMOUNT O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-13 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
Compound Segment Required on claims for compound drugs. Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 10
450-EF COMPOUND DOSAGE FORM DESCRIPTION CODE
O
451-EG COMPOUND DISPENSING UNIT FORM INDICATOR
M 1 = Each 2 = Gram 3 = Milliliter
452-EH COMPOUND ROUTE OF ADMINISTRATION
O
447-EC COMPOUND INGREDIENT COMPONENT COUNT
M Up to 2 digits 1, 2, …24, 25 A maximum of 25 ingredients will be accepted. Identifies the ingredient within a compound (i.e. Ingredient Number 12)
488-RE COMPOUND PRODUCT ID QUALIFIER M Must be 03
489-TE COMPOUND PRODUCT ID M Enter 11 digit NDC
448-ED COMPOUND INGREDIENT QUANTITY M 9(7)V999
449-EE COMPOUND INGREDIENT DRUG COST M S9(6)V99
490-UE COMPOUND INGREDIENT BASIS OF COST DETERMINATION
O
Pricing Segment Required Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 11
409-D9 INGREDIENT COST SUBMITTED M S9(6)V99
412-DC DISPENSING FEE SUBMITTED M S9(6)V99
477-BE PROFESSIONAL SERVICE FEE SUBMITTED
O
433-DX PATIENT PAID AMOUNT SUBMITTED O/M Required when applicable/including Part D COB claims
438-E3 INCENTIVE AMOUNT SUBMITTED O
478-H7 OTHER AMOUNT CLAIMED SUBMITTED COUNT
O
479-H8 OTHER AMOUNT CLAIMED SUBMITTED QUALIFIER
O
480-H9 OTHER AMOUNT CLAIMED SUBMITTED O
481-HA FLAT SALES TAX AMOUNT SUBMITTED O
482-GE PERCENTAGE SALES TAX AMOUNT SUBMITTED
O
483-HE PERCENTAGE SALES TAX RATE SUBMITTED
O
484-JE PERCENTAGE SALES TAX BASIS SUBMITTED
O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-14 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Pricing Segment Required Field Field Name Mandatory
or Optional Remarks
426-DQ USUAL AND CUSTOMARY CHARGE M S9(6)V99 Provider usual and customary charge. For compounds, report usual and customary charge for entire compound.
430-DU GROSS AMOUNT DUE O
423-DN BASIS OF COST DETERMINATION O
Prior Authorization Segment Not Accepted. Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O 12
498-PA REQUEST TYPE O
498-PB REQUEST PERIOD DATE-BEGIN O
498-PC REQUEST PERIOD DATE-END O
498-PD BASIS OF REQUEST O
498-PE AUTHORIZED REPRESENTATIVE FIRST NAME
O
498-PF AUTHORIZED REPRESENTATIVE LAST NAME
O
498-PG AUTHORIZED REPRESENTATIVE STREET ADDRESS
O
498-PH AUTHORIZED REPRESENTATIVE CITY ADDRESS
O
498-PJ AUTHORIZED REPRESENTATIVE STATE/PROVINCE ADDRESS
O
498-PK AUTHORIZED REPRESENTATIVE ZIP/POSTAL ZONE
O
498-PY PRIOR AUTHORIZATION NUMBER--ASSIGNED
O
503-F3 AUTHORIZATION NUMBER O
498-PP PRIOR AUTHORIZATION SUPPORTING DOCUMENTATION
O
Clinical Segment Optional Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O 13
491-VE DIAGNOSIS CODE COUNT O 1, 2, 3, 4, or 5. A maximum of 5 Diagnosis Codes will be accepted
492-WE DIAGNOSIS CODE QUALIFIER O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-15 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Clinical Segment Optional Field Field Name Mandatory
or Optional Remarks
424-DO DIAGNOSIS CODE O Enter the five character ICD-9 diagnosis code in 15-digit field
493-XE CLINICAL INFORMATION COUNTER O
494-ZE MEASUREMENT DATE O
495-H1 MEASUREMENT TIME O
496-H2 MEASUREMENT DIMENSION O
497-H3 MEASUREMENT UNIT O
499-H4 MEASUREMENT VALUE O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-16 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
The following are Reversal Transaction Segments Transaction Header Segment Required (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
101-A1 BIN NUMBER M Must be 610515
102-A2 VERSION/RELEASE NUMBER M Must be 51
103-A3 TRANSACTION CODE M B2
104-A4 PROCESSOR CONTROL NUMBER M See pages 3.1 – 3.2 Ten Spaces = Beneficiaries not enrolled in
Medicare Part D and claims where New Jersey is being billed as the primary payer because Medicare Part D has denied coverage on the claim.
PAAD = Beneficiaries enrolled in New Jersey‟s Prescription Drug Program for the Aged and Disabled (PAAD) Program or New Jersey‟s Senior Gold Program
ADDP = Beneficiaries enrolled in New Jersey‟s AIDS Drug Distribution (ADDP) Program
SUPPNJ = Beneficiaries enrolled in other than New Jersey‟s (PAAD), Senior Gold or (ADDP) Prescription Drug Programs
109-A9 TRANSACTION COUNT M
202-B2 SERVICE PROVIDER ID QUALIFIER M 01 = National Provider Identifier (NPI)
201-B1 SERVICE PROVIDER ID M Enter 10-digit National Provider Identifier (NPI)
401-D1 DATE OF SERVICE M YYYYMMDD
110-AK SOFTWARE VENDOR/CERTIFICATION ID M NJP+7 digit submitter number e.g. NJP1234567
Patient Segment Optional (Reversal Transaction). Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O 01
331-CX PATIENT ID QUALIFIER O
332-CY PATIENT ID O
304-C4 DATE OF BIRTH O
305-C5 PATIENT GENDER CODE O
310-CA PATIENT FIRST NAME O
311-CB PATIENT LAST NAME O
322-CM PATIENT STREET ADDRESS O
323-CN PATIENT CITY ADDRESS O
324-CO PATIENT STATE / PROVINCE ADDRESS O
325-CP PATIENT ZIP/POSTAL ZONE O
326-CQ PATIENT PHONE NUMBER O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-17 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Patient Segment Optional (Reversal Transaction). Field Field Name Mandatory
or Optional Remarks
307-C7 PATIENT LOCATION O
333-CZ EMPLOYER ID O
334-1C SMOKER / NON-SMOKER CODE O
335-2C PREGNANCY INDICATOR O
Claim Segment Required (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION M 07
455-EM PRESCRIPTION/SERVICE REFERENCE NUMBER QUALIFIER
M Must be 1 = RX
402-D2 PRESCRIPTION/SERVICE REFERENCE NUMBER
M 7 digit prescription number (left zero fill prescription numbers less than 7 positions) Plan B ® OTC claims enter a Service Reference Number up to 7 digits, omit spaces and special characters
436-E1 PRODUCT/SERVICE ID QUALIFIER M Must be 03
407-D7 PRODUCT/SERVICE ID M 11 digit NDC (compounds 11 zeros or 1 zero)
456-EN ASSOCIATED PRESCRIPTION/SERVICE REFERENCE #
O
457-EP ASSOCIATED PRESCRIPTION/SERVICE DATE
O
458-SE PROCEDURE MODIFIER CODE COUNT O
459-ER PROCEDURE MODIFIER CODE O
442-E7 QUANTITY DISPENSED O
403-D3 FILL NUMBER O
405-D5 DAYS SUPPLY O
406-D6 COMPOUND CODE O
408-D8 DISPENSE AS WRITTEN (DAW)/PRODUCT SELECTION CODE
O
414-DE DATE PRESCRIPTION WRITTEN O
415-DF NUMBER OF REFILLS AUTHORIZED O
419-DJ PRESCRIPTION ORIGIN CODE O
420-DK SUBMISSION CLARIFICATION CODE O
460-ET QUANTITY PRESCRIBED O
308-C8 OTHER COVERAGE CODE O
429-DT UNIT DOSE INDICATOR O
453-EJ ORIG PRESCRIBED PRODUCT/SERVICE ID QUALIFIER
O
445-EA ORIGINALLY PRESCRIBED PRODUCT/SERVICE CODE
O
330-CW ALTERNATE ID O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-18 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) Claim Segment Required (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
454-EK SCHEDULED PRESCRIPTION ID NUMBER
O
600-28 UNIT OF MEASURE O
418-DI LEVEL OF SERVICE O
461-EU PRIOR AUTHORIZATION TYPE CODE O
462-EV PRIOR AUTHORIZATION NUMBER SUBMITTED
O
463-EW INTERMEDIARY AUTHORIZATION TYPE ID
O
464-EX INTERMEDIARY AUTHORIZATION ID O
343-HD DISPENSING STATUS O
344-HF QUANTITY INTENDED TO BE DISPENSED
O
345-HG DAYS SUPPLY INTENDED TO BE DISPENSED
O
Insurance Segment Optional (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O
302-C2 CARDHOLDER ID O
312-CC CARDHOLDER FIRST NAME O
313-CD CARDHOLDER LAST NAME O
314-CE HOME PLAN O
524-FO PLAN ID O
309-C9 ELIGIBILITY CLARIFICATION CODE O
336-8C FACILITY ID O
301-C1 GROUP ID O
303-C3 PERSON CODE O
306-C6 PATIENT RELATIONSHIP CODE O
DUR/PPS Segment Optional (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O
473-7E DUR/PPS CODE COUNTER O
439-E4 REASON FOR SERVICE CODE O
440-E5 PROFESSIONAL SERVICE CODE O
441-E6 RESULT OF SERVICE CODE O
474-8E DUR/PPS LEVEL OF EFFORT O
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-19 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
(cont.) DUR/PPS Segment Optional (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
475-J9 DUR CO-AGENT ID QUALIFIER O
476-H6 DUR CO-AGENT ID O
Pricing Segment Optional (Reversal Transaction) Field Field Name Mandatory
or Optional Remarks
111-AM SEGMENT IDENTIFICATION O
409-D9 INGREDIENT COST SUBMITTED O
412-DC DISPENSING FEE SUBMITTED O
477-BE PROFESSIONAL SERVICE FEE SUBMITTED
O
433-DX PATIENT PAID AMOUNT SUBMITTED O
438-E3 INCENTIVE AMOUNT SUBMITTED O
478-H7 OTHER AMOUNT CLAIMED SUBMITTED COUNT
O
479-H8 OTHER AMOUNT CLAIMED SUBMITTED QUALIFIER
O
480-H9 OTHER AMOUNT CLAIMED SUBMITTED O
481-HA FLAT SALES TAX AMOUNT SUBMITTED O
482-GE PERCENTAGE SALES TAX AMOUNT SUBMITTED
O
483-HE PERCENTAGE SALES TAX RATE SUBMITTED
O
484-JE PERCENTAGE SALES TAX BASIS SUBMITTED
O
426-DQ USUAL AND CUSTOMARY CHARGE O
430-DU GROSS AMOUNT DUE O
423-DN BASIS OF COST DETERMINATION O
RESPONSE TRANSACTIONS Please refer to the response matrices in the Implementation Guide for specific usage.
-
DMAHS NCPDP-HIPAA Companion Guide
Page 3-20 Section 3 NCPDP v5.1 NCPDP Specifications
November 2011 Version
SECTION 3.2 – NCPDP 1.1 BATCH TRANSACTION STANDARD Requirements in the Batch Transaction Standard that are specific to New Jersey DMAHS are indicated below. Transaction Header Section Required
Field Field Name Mandatory
or Optional Positions Remarks
880-K4 Text Indicator M 1 Hex 02 (Stx)
701 Segment Identifier M 2-3 00
880-K6 Transmission Type M 4 T = Transaction
880-K1 Sender ID M 5-28 7 digit Submitter number
806-5C Batch Number M 29-35 Unique number assigned by sender, matches trailer (must be 7 digit number)
880-K2 Creation Date M 36-43 CCYYMMDD
880-K3 Creation Time O 44-47 HHMM
702 File Type M 48 P = Production, T = Test
102-A2 Version /Release Number M 49-50 11
880-K7 Receiver ID M 51-74 610515
880-K4 Text Indicator M 75 Hex 03 (Etx)
Detail Data Record Required
Field Field Name Mandatory
or Optional Positions Remarks
880-K4 Text Indicator M 1 Hex 02 (Stx)
701 Segment Identifier M 2-3 G1
880-K5 Transaction Reference Number
M 4-13
NCPDP Data Record M 14 Varies Must be version 5.1
880-K4 Text Indicator M Varies Hex 03 (Etx)
Trailer Record Required
Field Field Name Mandatory
or Optional Positions Remarks
880-K4 Text Indicator M 1 Hex 02 (Stx)
701 Segment Identifier M 2-3 99
806-5C Batch Number M 4-10 Should match Header
751 Record Count M 11-20 File record count including header and trailer
504-F4 Message O 21-55
880-K4 Text Indicator M 56 Hex 03 (Etx)
-
DMAHS NCPDP-HIPAA Companion Guide
Page 4-1 Section 4 NCPDP v5.1
Error Response Specifications November 2011 Version
SECTION 4.1 – ERROR RESPONSE SPECIFICATIONS The NCPDP standards only allows for a reject or error response at the file level. When the file fails an edit at the header or trailer record levels the entire batch file is rejected and an error response file is created and made available for the submitter to download. The error response consists of a Transaction header section and a Trailer record. The trailer record will contain an explanation for the rejection of the file. Transaction Header Section Required Field Field Name Mandatory
or Optional Positions Remarks
880-K4 Text Indicator M 1 Hex 02 (Stx)
701 Segment Identifier M 2-3 00
880-K6 Transmission Type M 4 E = Error
880-K1 Sender ID M 5-28 7 digit Submitter number
806-5C Batch Number M 29-35 Unique number assigned by sender, matches trailer
880-K2 Creation Date M 36-43 CCYYMMDD
880-K3 Creation Time O 44-47 HHMM
702 File Type M 48 P = production, T = test
102-A2 Version /Release Number M 49-50 11
880-K7 Receiver ID M 51-74 610515
880-K4 Text Indicator M 75 Hex 03 (Etx)
Trailer Record Required Field Field Name Mandatory
or Optional Positions Remarks
880-K4 Text Indicator M 1 Hex 02 (Stx)
701 Segment Identifier M 2-3 99
806-5C Batch Number M 4-10 Should match Header
751 Record Count M 11-20 File record count including header and trailer
504-F4 Message O 21-55 Explanation for rejection of file
880-K4 Text Indicator M 56 Hex 03 (Etx)
-
DMAHS NCPDP-HIPAA Companion Guide
Page 4-2 Section 4 NCPDP v5.1
Error Response Specifications November 2011 Version
SECTION 4.2 - PHARMACY EMC PROOF REPORTS Pharmacy EMC Proof Reports are error reports that are mailed to the NCPDP 1.1 batch submitters to report an error(s) found for a particular transaction(s) within the NCPDP 1.1 batch file processed by the NJMMIS System. The error message, “Parsing error for segment(s)” will be reported in the response file for the transaction(s) that contained an error in the format structure for a particular transaction(s) disallowing the transaction to adjudicate. The transaction containing the error will be reported in the Record Number column of the error report.
REPORT ID: XC151R03 STATE OF NEW JERSEY PAGE: 1
RUN DATE: 03/01/2005 DEPARTMENT OF HUMAN SERVICES
DIVISION OF MEDICAL ASSISTANCE AND HEALTH SERVICES
PHARMACY EMC PROOF REPORT
FILE NAME : 8800000_0001234.dat SUBMITTER ID : 8800000 DATE PROCESSED : 03/01/2005
RECORD NUMBER SEGMENT NUMBER FIELD NAME
--------------- -------------- ----------
91 HD
RECORDS RECEIVED - 753 RECORDS ON TRAILER - 753 CLAIMS ADJUDICATED - 750
NUMBER OF FORMAT ERRORS - 1 FORMAT ERRORS FOUND ON THIS FILE
Transactions containing errors should be corrected and resubmitted in the next batch for processing.