Netter's Osteoarthritis R Hip
-
Upload
bryan-paul-ramirez -
Category
Documents
-
view
220 -
download
0
Transcript of Netter's Osteoarthritis R Hip
-
8/4/2019 Netter's Osteoarthritis R Hip
1/3
Greene: Netter's Orthopaedics, 1st ed.
Copyright 2006 Saunders, An Imprint of Elsevier
DEGENERATIVE DISEASES AND DISORDERS
Osteoarthritis
Osteoarthritis of the hip may be primary (idiopathic) or secondary to an underlying hip disorder(eg, pediatric hip disease, osteonecrosis, previous infection, or previous trauma). Typical
presenting symptoms are indolent onset of anterior thigh or groin pain that is deep and activity
related. Occasionally, the pain is referred to the buttocks or distal thigh. As degeneration of thearticular cartilage progresses, the duration and the frequency of the pain intensify. Pain at rest or
pain that wakens the patient at night is associated with severe arthritis.
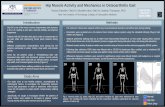
The most sensitive sign of early osteoarthritis of the hip is loss of internal rotation ( Figure 17-12 ). As the disease and joint contractures progress, decreased abduction, flexion, and extensionare observed. A coxalgic limp, with or without Trendelenburg lurch, is often present.
Figure 17-12 Osteoarthritis of the Hip
-
8/4/2019 Netter's Osteoarthritis R Hip
2/3
Anteroposterior (AP) and lateral radiographs show joint space narrowing in the early stages and
osteophytes, cyst formation, and sclerosis as the disease progresses ( Figure 17-13 ).
Osteophytes can occur in the floor of the acetabulum and around the periphery of the femoral
head and may cause lateralization and proximal migration of the femoral head.
The differential diagnosis includes:
Osteonecrosis of the femoral head (evident on radiographs)
Trochanteric bursitis (localized tenderness, normal radiographs)
Lateral femoral nerve entrapment (burning pain, sensory changes, normal
motion)
Lumbar disc herniation or degenerative disc disease (buttock pain, distal
motor and sensory changes, no restriction of hip motion)
Tumors of the lumbar spine, pelvis, or upper thigh (back pain, night pain,
-
8/4/2019 Netter's Osteoarthritis R Hip
3/3
normal motion)
Nonoperative treatment includes education of the patient, activity modification, optimization ofany leg-length discrepancies (often with a small heel lift), and judicious use of nonsteroidal anti-
inflammatory drugs (NSAIDs). Physiotherapy to improve range of motion is often unsuccessfulbecause this type of exercise provokes joint pain. Low-impact exercises, particularly swimming,
may improve muscle strength. As the disease progresses, the patient will benefit from the use ofa cane in the opposite hand.
Adolescents and young adults who have malalignment of the acetabulum, proximal femur, or
both, may benefit from realignment osteotomies of the pelvis, proximal femur, or both.
Arthrodesis should be considered for adolescents or young adults with unilateral end-stagearthritis and no other significant limb dysfunction. In other patients who have severe pain and
joint erosions, a total hip replacement arthroplasty is indicated (see Figure 4-8 ). These
procedures can dramatically reduce pain and improve function, but the decision for surgery
should be made with an understanding of potential complications, including infection (0.5% to1.0%), dislocation (8% to 10%), and deep venous thrombosis (40% to 60% if no prophylaxis is
used).
The long-term concern of total joint arthroplasty is aseptic loosening. When a joint implant isloose and has to be revised, less bone stock is available and the rates of all complications are
higher, particularly the rate of recurrent loosening. The risk of needing to replace a hip
arthroplasty is very low in a patient older than 65 years, who typically places moderate demandson the joint and who has a limited life expectancy, but it is virtually universal in a young adult
who is in good health and places more strenuous demands on the joint. Appropriate preoperative
planning and better implants have improved the results of both primary and revision arthroplasty.
Email to ColleaguePrint Version
Copyright 2008 Elsevier Inc. All rights reserved. - www.mdconsult.com