Neoplasia Ppt
-
Upload
elstella-eguavoen-ehicheoya -
Category
Documents
-
view
408 -
download
3
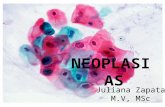
Transcript of Neoplasia Ppt

Neoplasia Patho
Patho 2Fall 2011

Cancer“It has been estimated that approximately 35
billion cells divide each day in a healthy adult, and any of these divisions could produce a rogue cell population that continues to grow without constraint. Uncontrolled cell growth is called “cancer”. We make about 100 cancer cells per day but fortunately our immune system recognizes these cancer cells as foreign and immediately destroys the cells before they have the chance to develop into a malignant tumor.”
Bancroft

CancerRefers to all malignant neoplasmsMay arise from most organsMorbidity and mortality vary by type of CAMany are curable or treatableRanks 2nd to CV disease as leading cause of death in USAffects all age groupsCauses more deaths in children age 3 – 15 than any other disease

Cancer1 out of 3 Americans will develop cancer in their lifetime; 1 in 4 deaths in US is due to cancerMost common in all: Skin CA
Men: prostate, lung, colorectalWomen: Breast, lung, colorectal
Lung cancer is leading cause of CA death in US. Is resistant to treatment

PathoCancer cells first develop from mutation in a single cell. This cell grows without the control that characterizes normal cell growth. At a certain stage of development, the cancer cell fails to mature into the type of normal cell from which it originated .Cancer cells are capable of spreading from site of origin (metastasis)

Altered Cell GrowthNeoplasia = new growth of cells; disorder of altered cell differentiation and growthNeoplasm = abnormal tissue which results

Cell ProliferationOrderly process that provides body with means for replacing cells as neededUsually a balance between # cells dying and # cells proliferatingUnlike normal cells, cancer cells undergo unrestrained growth and division. Without intervention, they continue to grow until they produce death. Some neoplasia’s grow fast and other grow slowly.

Cell DifferentiationProcess by which proliferating cells are transformed into specialized cell types, which determines cell functionThe more highly specialized a cell, the more likely it will lose it’s ability to reproduce and divide Stem cells remain incompletely differentiated throughout life

Cell Differentiation Groups of Cell types:
Undifferentiated Stem cells: can be triggered to divide & reproduce several progenitor cells—> several cell lines Parent or progenitor: blood, skin, liver cell--are partly differentiated—produce specialized cells (cell lines) when stimulated Well or fully-differentiated: neural, striated & cardiac muscle: cannot divide —have the structural and functional characteristics of a specific cell line
Under genetic & environmental control

Cell Cycle
Nondividing permanent cells, like neurons, cardiac muscle
G0—resting phase; can be stimulated to divide

Cell CycleCell cycle is sequence of events cell goes thru from one mitotic division to next. Has 4 major phases:
G1 (Gap 1): cell prepares to make DNAS phase: DNA synthesis actually takes placeG2: prepares for mitosis (cell division)M phase: mitosis occursG0: resting phase (becomes mitotically dormant)
http://www.cellsalive.com/cell_cycle.htm

Cell CycleEntry into and progression thru stages are controlled by proteins called cyclins and their inhibitors. There are checkpoints in cell cycle which determine accuracy with which DNA is duplicated.Defects in either of these can contribute to development of cancer (may cause genetic instability of cancer cells)

Neoplasms Do not obey normal tissue growth laws: --Do not occur in response to appropriate stimulus --Continue to grow after the stimulus has ceased --Function independently of body’s needs: -faster growth rate -increase in size at expense of rest of body’s
needs -great variation in cell size, shape, arrangement Neoplasms have 2 tissue types: --Parenchymal (organ cells) --Stromal (supporting tissue—connective, vascular)

Benign NeoplasmsComposed of well-differentiated cells that resemble cells of tissues of originSlow growth rateRemain localized to site of origin without capacity to infiltrate, invade, or metastasizeMay become encapsulatedLess blood supply than malignant neoplasmUsually do not cause death unless interfere with vital functions because of their location Can cause alterations in body function thru abnormal alteration of hormones

Benign tumors--Fibroids

Benign Uterine Tumor with Clearly Defined Edges
Benign Uterine Tumor with Clearly Defined Edges

Malignant Neoplasms = Cancer
Atypical cell structure; abnormal nucleus & chromosomes Lose differentiation or resemblance to origin cell--more anaplastic Not cohesive, irregular growth pattern, no capsule formed, not distinct from surrounding tissue Invade adjacent cells rather than pushing aside Varying growth rates and do not die within normal timeframeMore blood supply than normal tissue Hallmark Sign of malignancy: ability to metastasize or spread to distant sites See Porth Table for comparison of benign vs. malignant

Naming Tumors
Benign tumors: tissue name + “-oma”Eg: osteoma = benign bone tumor
Malignant tumors (cancers)Epithelial tissue: tissue name + “carcinoma”Mesenchymal tissue: tissue name + “sarcoma”“Malignant _____oma”Eg: Adenocarcinoma = Cancer of glandular tissue

Spread of CancerDirect invasion & extension – local spread, mechanical, lysis with enzymesSeeding of CA cells in body cavitiesMetastasis

MetastasisAbility of CA cells to spread to distant sitesClumps of malignant cells break off & travel thru blood (hematogenic spread) or lymph (lymphatic spread) to new site – most are killed by body’s defense mechanismsIn lymph nodes, CA may die, grow into mass, or remain dormant

MetastasisMetastasisCells in a primary tumor develop the ability to escape and travel in the bloodImagine you were a cancer cell. What abilities would you need to survive in the tumor? What abilities would you need to metastasize?

Cancer Progression

Metastasis
Surviving CA cells leave lymph nodes & enter venous blood & are carried to major organs: bone, liver, lungs, brainOriginal tumor = primary neoplasmMetastatic site = secondary neoplasm (retains characteristics of primary tumor)

Tumor GrowthGrowth Fraction (GF) = ratio of dividing cells / G0 cells A tissue with a large percentage of proliferating cells and few cells in G0 has a high growth fraction. So, chemotherapeutic drugs are much more toxic to tissues that have a high growth fraction than to tissues that have a low growth fraction. Why?Doubling time (TD) = time to double total mass of CA cells
GF and TD are very fast until tumor outgrows blood supply, then slowsMay be influenced by hormones

Etiology of CancerGenes that cancer cells contain – encode for cancer causing proteinsProto-oncogenes = Normal genes that regulate cell growth & differentiation & are active for only a short time in cell cycleOncogenes = gene mutations which become cancer-causing genes; are active continuously & promote unregulated, abnormal & disordered growth. Selected oncogenes have been associated with numerous cancer types
Mutations in p53 gene have been implicated in development of lung, breast, and colon cancer

Oncogenesis: Mechanism by which a normal cell is transformed into cancer cell by random genetic mutation or mutation induced by exposure to physical (radiation), chemical (many environmental and manmade substances) or biological (oncogenic viruses, immunodeficiency) carcinogensIs a monoclonal origin because a single cell is transformed into a cancer cell

Tumor Supressor GenesTumor Supressor genes =anti-oncogenes
normally inhibit inappropriate cell growth--start senescence and crisis or cell death
senescence = when cells stop dividing -- in response to growth inhibiting proteins like P53 crisis = when cells die
Abnormal tumor suppressor genes are inherited or mutant genes Fail to inhibit inappropriate cell growth Mutation of TP53 gene is found in 50% of human cancers, codes for p53 protein which functions as a suppressor of tumor growthFHIT (fragile histidine triad protein) gene: tobacco smoke causes it to mutate – seen in small cell lung cancer




Stages of Cancer GrowthInitiation: exposure of cells (especially those actively synthesizing DNA) to enough carcinogens that alter cell's genome-irreversible mutation Promotion: induction of unregulated accelerated growth by some agent, chemical, or endogenous hormoneProgression: process whereby tumor cells get malignant characteristics Metastasis: spread


Mrs. T Has Liver Cancer …Mrs. T Has Liver Cancer …Her doctor did an initial molecular diagnosis and put her on targeted therapy; the tumor shrank by almost 75%Two years later the tumor was growing again, and this time it did not respond to the drugLast year she was diagnosed with metastases in her femur that has not responded to the drug eitherMrs. T wants to know why the cancer cells stopped responding. Are they not all the same cells?

Cervical Cancer

In Review…
Cancer is error in DNA creates abnormal clonal cells which multiply and function inappropriately, leading to:
Unchecked increase in # of cellsAbility to invade body structuresAbility to metastasize to distant locationsInappropriate cell life span

Risk Factors Heredity : < 5 % of all CA--MOST cancers are due to spontaneous genetic mutations
Oncogenes: specific genes that CA cells contain-- may be inherited by autosomal dominant or autosomal recessive patterns
Oncogenic viruses: viruses that may cause CA--alter genome of infected cell & cells it divides into
Includes DNA and RNA virusesCause CA by inserting viral genes into host's DNA which then replicates
Herpesvirus cervical CA, Epstein-Barr virus -> Burkitt’s lymphoma, human papillomavirus (HPV) skin & cervical CA, Hepatitis B & C liver cancer, HTLV-1 leukemia Oncogenic bacteria--H. Pylori--linked to gastric CA and lymphoma

Risk FactorsChemical carcinogenesis: cause mutations
Polycyclic aromatic hydrocarbons• tobacco smoke CA of head & neck, lungs, pancreas,
bladder– Food and drugs
• Plants: aflatoxin (mold) & betel nut liver CA• Food preparation: smoked and charbroiled meats• Alcohol: carcinogen promotor; carcinogenic effect of
cigarette smoke is enhanced in presence of alcohol• Nitrosamines: develop from nitrites (a food additive) in
presence of amines & nicotine gastric CA
Industrial Agentsasbestos, cadmium, chromium, nickel, benzene -> Lung & other CAs
• Nitrogen mustard & mustard gas leukemias & lymphomas

Risk Factors • Immune deficiency
– Immune surveillance hypothesis -- says immune system plays key role in detecting mutant / cancer cells and killing them
– Immunodeficiency states are associated with increased CA rates
– All immune cells can kill CA cells—NK (natural killer), T & B lymphocytes, macrophages
– Tumor cells can evade immunosurveillance

Risk Factors• Hormones
– Role is unclear and controversial– Excessive hormone use, especially
estrogen, may contribute to certain form of cancer while reducing risk of other forms
– Link may be due to ability of hormones to drive cell division of malignant phenotype

Risk Factors
• Radiation– Ionizing radiation (from atomic bomb,
diagnostic or work exposure): skin cancer and leukemias, etc.
– Ultraviolet radiation • Effects are usually additive and usually
long delay between time of exposure and time of cancer detection

7 Warning Signs of Cancer
C: Change in bowel / bladder habits A: A sore that doesn’t heal U: Unusual bleeding / discharge T: Thickening / lumps in breast, etc. I: Indigestion / difficulty swallowing O: Obvious change in mole or wart N: Nagging cough or hoarseness

Clinical Manifestations
• Most body functions affected Initial S&S at primary site, then systemic– S/S due to disrupted tissue
integrity: Pain, bleeding, wounds, effusions or edema
– Cachexia: wt. loss and muscle wasting; weakness, anorexia, & anemia
• Cause is multifactorial

Clinical Manifestations– Paraneoplastic syndromes:
• Cancer cells can have effect on hormones
– Increased ADH SIADH – Increased ACTH Cushing
Syndrome – Increased PTH Hypercalcemia

Staging and Grading• Grading = looking at cell histology
& comparing to normal– Stage I – IV– Stage I – small localized cancers – Stage II and III – locally advanced
and/or with local lymph node involvement
– State IV – inoperable or metastatic– Prognosis depends on type of cancer

Staging and Grading
• Staging = based on clinical picture & spread of disease– T = tumor size– N = lymph nodes involved– M = metastasis– Lung cancer example– Breast Cancer example

Staging and Grading
• T = Tumor– T0 – T4 (4 being most severe)
• N = Lymph nodes– N0 – no lymph node involvement– N3 – extensive node involvement
• M = Metastasis– M0 – no metastasis– M1 – metastases present

Diagnostic tests• Link to Web Path• History and Physical• Blood Tests (tumor antigens)• Cytology (eg: Pap)• Biopsy

Diagnostic Test• Tumor Markers – antigens expressed
on surface of tumor cells or substances released from normal cells in response to presence of tumor– Used for screening, dx, establishing
prognosis, monitoring treatment, detecting recurrent disease
– Eg: PSA – prostate cancer screening

Hepatic Adenoma

Breast Cancer

Liver metastases