Neoplasia & Carcinogenesis
-
Upload
muhammad-helmi -
Category
Health & Medicine
-
view
540 -
download
2
Transcript of Neoplasia & Carcinogenesis

NEOPLASIA

DEFINITION• Neo = New ; Plasia= growth
• Abnormal mass of tissue as a result of abnormal growth or multiplication of cell.
• Growth of neoplastic cell persist in excessive manner even after the stimulus that evoked the changes stop.

CLASSIFICATION OF NEOPLASIA
2 types :
BENIGN MALIGNANT- Suffix = –oma to cell type which the tumor arise
- Eg: fibrous tissue – fibromaBone tissue – Osteoma etc.
- Suffix: –Sarcoma = Malignant tumor (Cancer) that arises from
transformed cells of mesenchymal originEg: Chondrosarcoma
–Carcinoma= Malignant tumor from epithelial originEg: Adenocarcinoma
- Microscopic and gross characteristic relatively inoncent - Invade and destroyed adjacent structure and spread to distant site.(metastasize).
- Remain localized • Will invade other neighbouring tissues & m etastasize (Lymph & BV)
- Amendable to local surgical removal • Lower prognosis than benign tumors

DIFFERENCE BETWEEN MALIGNANT AND BENIGN

TYPE BENIGN MALIGNANT
DIFFERENTIATION @ ANAPLASIA
- Well differentiated - Closely resemble their normal
counterpart.- Mitosis usually rare- Nuclei remain at basal layer
but usually enlarged.
- Poor differentiate@anaplastic- Loss of structure and function- Plemorphism, hyperchromatic,
increase nuclear-cytoplasmic ration, giant cell.
- Mitosis often numerous.- Loss of polarity

LOCAL INVASION
- Remain localized at site of origin
- Does not have the capacity to infiltrate,invade or metastasize.
- Encapsulated.
- Grow by progressive infiltration,invasion, destraction and penetration of surrounding tissue.
- Do not develop well of define capsule.
- Hemmorhage and necrosis.- Ulceration.

METASTASIS - Absent - Metastasize- Factor increase of metastasis • Larger of tumor• Older of tumor• Poorly differentiated- Disseminate by 3 pathways• Seeding body cavity• Lymphatic spread• Hematogenous spread

METHOD OF DIAGNOSIS

Method Explanation
History and physical examination
What the health care worker learns from talking to the patient and through direct examination may give clues to the presence of a neoplasm. Signs and symptoms such as weight loss, fatigue, and pain may be present. A mass may be palpable or visible.
Radiographic technique
The use of plain films (x-rays), computed tomography (CT), magnetic resonance imaging (MRI), mammography, and ultrasonography (US) may be very helpful to detect the presence and location of mass lesions. The findings from these methods may aid in staging and determination of therapy.
Genetic Testing
Genetic markers include chromosomal alterations (translocations, deletions, duplication, etc.); specific gene defects; single nucleotide polymorphisms, and gene rearrangements. Detection of specific genes (such as BRCA-1 for breast cancer) may suggest an increased risk for some malignancies.

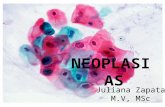
Cytology Methods that sample cells can be simple and cost-effective and minimally invasive. A good example is the Pap smear for diagnosis of cervical dysplasias and neoplasms. Cells exfoliated into body fluids may also be examined. Fine needle aspiration (FNA) can be used to sample a variety of mass lesions.
Tissue biopsy and surgery
Methods that sample small pieces of tissue (biopsy) from a particular site, often via endoscopic techniques (such as colonoscopy, upper endoscopy, or bronchoscopy) can often yield a specific diagnosis of malignancy. At surgery, portions of an organ or tissue can be sampled, or the diseased tissue(s) removed and examined in surgical pathology to determine the stage and grade of the neoplasm.
Autopsy Sometimes neoplasms are not detected or completely diagnosed during life. The autopsy serves as a means of quality assurance for clinical diagnostic methods, as a way of confirming diagnoses helpful in establishing risks for family members, as a means for gathering statistics for decision making about how to approach diagnosis and treatment of neoplasms, and to provide material for future research.

Laboratory analyses
General findings such as anemia, enzyme abnormalities (such as an increased alkaline phosphatase), and hematuria or positive stool occult blood are helpful to suggest further workup. Tumor markers in serum such as carcinoembryonic antigen (CEA), alpha-fetoprotein (AFP), or human chorionic gonadotropin (HCG) can be performed. Unfortunately, they are not all that specific or sensitive, particularly when applied as screening tests to a general population. More specific testing, such as measurement of prostate specific antigen (PSA) levels, may help to determine the presence of specific neoplasms, but such tests are not perfect screening tools in a general population.

Spread of tumour:Direct spread Distant spread
-means tumour spreading and involving the tissues around the tumour.- As example,if the primary tumours arises from the bronchus,this tumour can spread to the lung tissue.
-means the tumour from one site (primary) is now transferred to a distant site (secondary).-This process called metastasis.-There are three ways on how tumour can metastasise to distant sites. (refer table in next slide)

Distant spreadBy Invasion of lymphatic
-Lymphatic are channels lined by endothelium-drain lymph from tissues to lymph nodes (regional lymphnodes) -Ex : Breast carcinoma-enlarged axillary lymph nodes -Usually cancers that spread via lymphatic are *CARCINOMAS.

Hematogenous spread
-Spread via blood channels. -VEINS are more frequently invaded than arteries because: a-thinner walls b-lower pressure c-slower blood flow -Neoplasm that spread via blood channels usually *SARCOMAS

Through body cavity It can either spread via: 1-coelomic cavity-tumours seeding over surfaces in peritoneal,pleural and pericardial spaces. -Ex:Carcinoma in ovary of one side spreading to the other ovary or to other organs in peritoneum 2-Cerebral spinal fluid-occurs for cancers in the brain and spinal cord.


Grading (Differentiation)
• Made by Pathologist• Microscopic appearance • Assesment depends on :
Mitotic activity Nuclear size &
pleomorphism The differentition
• Degree of diff. indicates : Prognosis Appropiate treatment
Grading of Malignant Neoplasms
Grade Definition
I Well differentiated
IIModerately differentiated
III Poorly differentiated
IV Nearly anaplastic
Eg : Adenocarcinoma

Staging(Spreading)
• Made by Surgeon• Gross anatomical appearance
Eg : lung carcinoma
Staging of Malignant Neoplasms
Tis In situ, non-invasive
T Refers to Primary tumors
T1 Small, minimally invasive within primary organ site
T2 Larger, more invasive within the primary organ site
T3 Larger and/or invasive beyond margins of primary organ site
T4 Very large and/or very invasive, spread to adjacent organs
N Refers to Lymph Nodes
N0 No lymph node involvement
N1 Nearby lymph node involvement
N2 Regional lymph node involvement
N3 More distant lymph node involvement
M Refers to anatomical distance metastases
M0 No distant metastases
M1 Distant metastases present

Although benign tumours are confined to their site of origin, they may cause clinical problems due to:
Pressure on adjacent tissues (e.g. benign meningeal tumours causing epilepsy)
Obstruction to the flow of fluid (e.g. benign epithelial tumour blocking a duct)
Production of a hormone (e.g. benign thyroid tumour causing thyrotoxicosis)
Transformation into a malignant neoplasm (e.g. adenormatous polyp progressing to an adenocarcinoma)
anxiety


Morbidity and mortality associated with malignant tumours:
Pressure on and destruction of adjacent tissue
Formation of secondary tumours (metastases)
Blood loss from ulcerated surfaces Obstruction of flow (e.g. malignant
tumour of the colon causing intestinal obstruction)
Production of a hormone (e.g. ACTH and ADH from some lung tumours)
Other paraneoplastic effects causing weight loss and debility

Cachexia (wasting syndrome) • Progressive loss of body fat and lean body mass
accompanied by profound weakness, anorexia, and anemia.
• The origins of cancer cachexia are obscure.• Cachexia is not caused by the nutritional demands of the
tumor. • Results from the action of soluble factors such as
cytokines produced by the tumor or host• Cachexia- the loss of
1.skeletal muscle,
2.adipose tissue
3.immunological competence.

Paraneoplastic Syndrome
• Symptoms complexes in cancer-bearing patients that cannot be explained by :-• local or metastatic spread• elaboration of hormones indigenous to tissue • May represent early manifestations of tumor• May represent significant clinical problems• May even be fatal
• Occurs in about. in 10% of patients with cancer• They are syndromes involving nonmetastatic systemic effects that accompany malignant disease.

Paraneoplastic syndromes
Syndrome Mechanism Example
Cushing Syndrome
Secretion of ACTH-like substance
Lung small cell anaplastic (oat cell) carcinoma
HypercalcemiaParathyroid hormone-
like substanceLung (squamous cell)
carcinoma
HyponatremiaInappropriate ADH
secretionLung small cell anaplastic
(oat cell) carcinoma
PolycythemiaErythropoietin-like
substanceRenal cell carcinoma
Trousseau Syndrome
Hypercoagulable state Various carcinomas
Hypoglycemia Insulin-like substanceVarious carcinomas and
sarcomas
Carcinoid Syndrome
5-hydroxy-indoleacetic acid (5-
HIAA)
Metastatic malignant carcinoid tumors

• From team Omega
CARCINOGENESIS
It is a process by which normal cells are transformed into cancer cells

Carcinogenesis
GENES INVOLVED
ONCOGENES- Genes that induce a
transformed phenotype
- Dominant – single allele mutated
cellular transformation- Protooncogenes :
normal cellular genes that affect growth
& differentiation
- Protooncogenes oncogenes
by : i. Transduction into retroviruses over
expressed ii. Point of mutations
iii.Chromosomal rearrangments
iv.Gene amplification
TUMOR SUPRESSOR GENES
- Prevent uncontrolled growth
- Lost single / both normal alleles allow the
transformation - 2 general group :
‘governors’ & ‘guardians’
- Governor – RB gene ; mutation
cause its function as brake on
cellular proliferation removed
- Guardian : (normal) sensing
genomic damage stop the
proliferation / apoptosis (eg.
TP53) ; mutation of this gene
accelerates mutations in oncogenes & tumor
supressor genes cancer
GENES INVOLVED IN DNA REPAIRmay act like :
Protooncogenes (loss of one copy)
orTumor supressor genes
(loss of both copies)
Malfunction Of MYC Gene

Carcinogenesis: A multiple step process • Carcinogenesis= A multistep process resulting from the accumulation of
multiple genetic alteration , give rise to transform phenotype .
MUTATION
• Mutation provide cells of precursor lesion with a selective advantage (Darwinin Selection) . Once initiate, cancer continue undergoes darwinian selection.
• Over period of time, tumors become more aggressive and acquire greater malignant potential (Tumor Progression, not represent simply by an increase in tumor size) .
Non neoplastic precursor
lesionCancer

• Some mutation may lethal. Others may spur cell growth by affecting proto-oncogenes or cancer suppressor genes.

Hallmarks of cancer
• Self sufficiency in growth signals • Insensitivity to growth inhibitory signals• Evasion (Immortalization) of cell death • Limitless replicative potential • Development of sustained angiogenesis • Ability to invade and metastasize


SELF SUFFICIENCY IN GROWTH FACTORS
1.Growth factors:Normal cells require growth stimulation by growth factors to undergo proliferation.
•Many cancer cells acquire growth self-sufficiency by acquiring ability to synthesize the same growth factors which they are responsive.
•Another mechanism by which cancer cells acquire growth self-sufficiency is by interaction with stroma. In some cases, tumor cells send signals to activate normal cells in the supporting stroma which in turn produce growth factors that promote tumor growth .
2. Growth factor receptors and non-Receptor Tyrosine Kinases
•Mutant receptor proteins deliver continuous mitogenic signals to cells even in the absent of growth factor in the environment .
•Mutation is overexpression of growth factor to level which growth factor receptor which render cancer cells hyperresponsive to level of the growth factor that would not normally trigger proliferation.

*** RAS •Most commonly mutated proto-oncogene in human tumor.
•Normal RAS protein flip back and forth between an excited signal-transmitting state and not active state.
•Activated RAS stimulates downstream regulators of proliferation by two distinct pathway that converge on the nucleus and flood it with signal for cell proliferation.
•Mutational activation of these massengers to the nucleus can mimic growth promoting effect of activation RAS .
•Activating mutation RAS as well as it downstream signaling molecules are very common in wide variety of tumor .
•Also mutation in RAS mimicked by loss-of—function mutations in the GTPase-activating proteins with a failure to stimulate GTP hydrolysis and thereby restrain normal RAS protein.


INSENSITIVITY TO GROWTH INHIBITORY SIGNALS • Products of tumor suppresor genes apply brakes to cell proliferation. Disruption of such
genes renders cells refractory to growth inhibition and mimics the growth-promoting effect on oncogenes .
RB GENES: Governor of the cell cycle
o RB gene product is a DNA-binding protein that expressed in every cell type examined , exists in active hypophosphorylated state and an inactive hyperphosphorylated stated.
o RB exerts antiproliferative effect by controlling regulations of G1/S checkpoint (mitosis cycle) , the portal through which cell must pass before DNA replication commences .

o RB in active form, hypophosphorylation bind to E2F transcription factors. This interaction prevents transcription of genes like cyclin E that are needed for DNA replication, and so the cell arrested in G1.
o Growth factor signaling leads to cyclin D expression, activation of the cyclin D-CDK4/6 complexes, inactivation of RB by phosphorylation , and thus release E2F .
o Loss of cell cycle control is fundamental to malignant transformation. o All cancers have disabled G1 checkpoint due to mutation either RB or genes that affect
RB function such as cyclin D, CDK4, and CDKIs

TP53 GENE: Guardian of the genome
• The p53-encoding tumor suppressor gene, TP53 , one of the most commonly mutated genes in human cancers.
• The p53 proteins prevents neoplastic transformation by three interlocking mechanisms : • Activation of temporary cell cycle arrest (quiescence ) when DNA damage and assist DNA repair
genes.• Induction of permanent cell cycle arrest (Senescence) when DNA damage genes cannot be
repaired• Or triggering of programmed death (apoptosis)
• Rb sense external signal, p53 is central monitor of internal stress, directing stress to one of the three mechanism .
• Example of stresses that trigger the p53 responses pathway including anoxia, inappropriate oncoprotein activity and damage to integrity of DNA .



= The condition or process of deterioration with age.

LIMITLESS REPLICATIVE POTENTIAL:
Telomerase Shortening


NORMAL
TUMOR

Ability to Invade and Metastasize• Metastatic cascade subdivided into :
Invasion of ECMVascular dissemination and homing of tumor
cell
• 2 types of ECM : basement membrane both are composed Interstitial connective tissue of collagen, glycoprotein
and proteoglycans


INVASION OF ECMLoosening of intracellular junctions occurred becauseof E-cadherin lost its function (keep cells together & transmit antigrowth signal) by :
• mutational inactivation of E-cadherin gene
• activation of β-catenin gene (regulating the coordination of cell–cell adhesion and gene
transcription.)
• inappropriate expression of SNAIL & TWIST transcription factors (Give Metastatic Ability)
Degradation of basement membrane & interstitial connective tissue Tumor cells secrete proteolytic enzymes / induce stromalcells elaborate proteases (cathepsin D, urokinase plasminogen activator, MMPs) tumor cell invasion
remodel insoluble components of basement membrane & interstitial matrix + release ECM-sequestered GF

Invasion of ECMChanges in attachment of tumor cells to ECM
Loss in adhesion in normal cells apoptosis ; but
tumor cells are resistant to apoptosis, instead caused
matrix modification by cleaving of basement membrane
proteins (collagen IV, laminin) by MMP generates
novel sites (bind to tumor cells’ receptors) migration
Migration is directed by tumor cell-derived cytokines
(autocrine motility factors) + cleaved products (collagen &
laminin) + some growth factors + stormal cells (HGF/SCF)

Vascular Dissemination & Homing of Tumor Cells
• In circulation, tumor cells vulnerable to destruction by host immune cells – it will form emboli & adhere to
the circulating leukocytes = protection
• Site of extravasation & the organ distribution of metastases based on location of primary tumor and its
vascular or lymphatic drainage. This tropism influences by :
i. Expression of adhesion molecules by tumor cells are preferential to the ligand on endothelium of
target organ
ii. Expression of chemokines (participate in chemotaxis of leukocytes) & their receptors – tumor cells
use similar tricks to home in on tissue
iii. When reach the target colonize the site (tumor cells dependent on a receptive stroma for growth)
• Tumor cells are inefficient in colonizing of distant organs and concept of dormancy refer to prolonged
survival of micrometastases w/o progression

Etiology of cancer: carcinogenic events
• Chemical carcinogens- direct-acting - Indirect-acting
• Radiation carcinogens
• Viral and microbial oncogenesis

CHEMICAL Direct-acting agents Indirect-acting agents
• Does not require metabolic conversion to become carcinogenic
• Require metabolic conversion to become active carcinogenic
• Weak carcinogens • E.g: polycyclic hydrocarbons, aromatic amines, azo dyes
• E.g: alkylating agents

Chemical carcinogens and the tumours with which they are associated:
Chemical Tumor Comments
Polycyclic hydrocarbon Lung cancer Present on fossil fuels
Aromatic amines Skin cancerBladder cancer
Rubber and dye workers
Nitrosamines Gut cancer Proven in animals
Azo dyes Bladder n liver cancer Proven in animals
Alkylating agentse.g: cyclophosphamide
Leukemia Small risk in human
Other organic chemicalse.g: vinyl chloride
Liver angiosarcoma PVC manufactures
Arsenic compounds Skin cancer No longer a common event

RADIATION UV light, x rays, nuclear fission
• Ionizing radiation- cause chromosome breakage, translocation, less
frequency, point mutation- Lead to genetic damage n carcinogenesis- E.g: chronic lymphocytic leukemia , Thyroid carcinoma
(children)
• UV radiation- Damage DNA by forming pyrimidine dimer- Cause skin cancer (melanoma, SCC, BCC)- Risk factor: fair-skinned people

• Initiation - May cause the mutational activation of an oncogen (RAS)
•Promoter - non-mutagenic, non-tumorigenic- Induces cell proliferation- E.g: phorbol esters, hormones, phenols, certain drugs


Cancer Progression Due To Constant Irritation

Normal

Metaplasia

Dysplasia

Carcinogenesis

Xeroderma Pigmentosum• Autosomal recessive• Defects in NER genes = (DNA repair mechanism )• Due to inability to repair DNA damage induced by UV• 200 X increase risk of skin cancer

VIRAL and MICROBIAL
RNA virus:•Cause by Retrovirus: Human T Cell Lymphotropic Virus-1 (HTLV-1)•a/w T cell leukemia/lymphoma•Has tropism for CD4 Tcells target for neoplastic transformation•Transmission: sexual intercourse, blood products or breastfeedin

DNA viruses:
• Human papilloma virus• Epstein-Barr virus• Hepatitis B virus• Kaposi Sarcoma herpes virus