Neonatal Encephalopathy: Case Studies -...
Transcript of Neonatal Encephalopathy: Case Studies -...

10/21/2016
1
N I C O L E J . W I L L I A M S D O O N A N , M D
D I V I S I O N O F P E D I A T R I C N E U R O L O G Y
G I L L E T T E C H I L D R E N ’ S S P E C I A L T Y H E A L T H C A R E
N o v e m b e r 2 , 2 0 1 6
Neonatal Encephalopathy: Case Studies
� Nothing to disclose.
Learning Objectives
� Recognize and evaluate encephalopathy in newborns
� Describe the utility of brain MRI and EEG for diagnosis and prognosis in neonatal encephalopathy
� Identify treatments available for neonatal encephalopathy

10/21/2016
2
Outline
� Define neonatal encephalopathy and hypoxic-ischemic encephalopathy
� Clinical evaluation of encephalopathy
� Therapeutic hypothermia
� Neuromonitoring
� Neonatal seizures
� Neuroimaging
� Perinatal stroke
Background
� Injury to the developing brain is a major cause of death and neurologic disability worldwide
� For survivors� Cerebral Palsy
� Intellectual disability
� Epilepsy
Case 1
� Term male LGA infant
� Uncomplicated pregnancy
� Delivery via stat C/S for prolapsed cord
� Depressed at birth, HR undetectable, apneic
� Apgar 1 at 1 min, 4 at 5 min, 6 at 10 min
� Resuscitation in delivery room
� PPV, intubation, spontaneous respiratory effort at 19 minutes
� Laboratory results� Cord VBG pH 6.9, base deficit 14

10/21/2016
3
Case 1
� Transfer to Children’s Hospital and Clinics- St. Paul NICU
� Initial neurologic exam� Bicycling movements concerning for seizures
� Minimal spontaneous movement, decreased level of consciousness, hyperreflexia
Neonatal Encephalopathy
� Decreased level of consciousness� Seizures� Abnormal muscle tone or strength� Abnormal reflexes� Abnormal cranial nerves� Feeding difficulties� Respiratory insufficiency or apnea� Irritability� Autonomic dysfunction� Encephalopathy
Evaluation of Neonatal Encephalopathy
� Clinical history � Pregnancy, delivery, gestational age, postnatal course, family
history
� Neurologic exam including severity of encephalopathy
� Diagnostic studies

10/21/2016
4
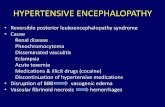
Causes of Encephalopathy in Newborns
� Hypoxic-ischemic insult
� 50-80%
� Intracranial hemorrhage
� Perinatal stroke
� Traumatic brain injury
� Meningitis/encephalitis
� Congenital brain malformation
� Epileptic encephalopathies
� Inborn errors of metabolism
� Hypoglycemia
� Electrolyte imbalance
� Hypocalcemia
� Severe hyperbilirubinemia
� Systemic illness (organ failure, sepsis)
Neonatal Hypoxic-Ischemic Encephalopathy
� Mechanism of injury� Interruption in blood flow or gas exchange to and from fetus
� Hypoxic-ischemic injury
� Most common cause of acute neurologic impairment and seizures in term neonates
� 1-6 per 1000 live births in developed countries
� Cause of 1 in 5 neonatal deaths worldwide
Neonatal Hypoxic-Ischemic Encephalopathy
� Clinical features consistent with acute peripartum or intrapartum event
� Apgar scores <5 at 5 and 10 minutes
� Metabolic acidosis
� Cord arterial pH <7.0 or base deficit ≥12 mmol/L
� Brain MRI/MRS consistent with hypoxia-ischemia
� Multisystem organ failure

10/21/2016
5
Neonatal Hypoxic-Ischemic Encephalopathy
� Sentinel hypoxic or ischemic event immediately before or during labor and delivery
� Ruptured uterus
� Placental abruption
� Umbilical cord prolapse
� Amniotic fluid embolus with severe/prolonged maternal hypotension and hypoxemia
� Maternal cardiovascular collapse
� Maternal fetal hemorrhage
� Fetal hemorrhage secondary to vasa previa
� Specific patterns in fetal heart trace can suggest hypoxic-ischemic event
Clinical Encephalopathy: Mild
� Increased muscle tone
� Deep tendon reflexes brisk
� Transient behavioral abnormalities
� Poor feeding
� Excessive crying, irritability
� Excessive sleeping
� Normalize 3-4 days of life

10/21/2016
6
Clinical Encephalopathy: Moderate
� Lethargic
� Low tone
� Depressed deep tendon reflexes
� Primitive reflexes sluggish or absent
� Apnea
� Seizures
� Possible full recovery 1-2 weeks
� Initially well or mild encephalopathy followed by sudden deterioration
Clinical Encephalopathy: Severe
� Stupor or coma� Low tone� Depressed deep tendon reflexes� Irregular breathing� Absent primitive reflexes� Abnormal eye movements� Pupils dilated, fixed or poorly reactive� Early seizures� Irregular HR and BP� Increased alertness 4-5 days of life� Persistent feeding and tone abnormalities
Modified Sarnat Scale
Severity Stage Stage 1 Stage 2 Stage 3
Level of consciousness
Alert, hyperalert Lethargic, obtunded
Stuporous
Spontaneousactivity
Normal Decreased No activity
Posture Normal Distal flexion, full extension
Decerebration
Tone Normal or hypertonia
Hypotonia Flaccid
Primitive reflexes: SuckMoro
NormalExaggerated
WeakIncomplete
AbsentAbsent
Autonomic function:PupilsHeart Rate
Respirations
NormalNormal
Normal
ConstrictedBradycardia
Periodic breathing
Dilated/non-reactiveVariable HR
Apnea

10/21/2016
7
Case 1
� Intrapartum event: prolapsed cord
� Laboratory evidence of hypoxic-ischemic insult
� Metabolic acidosis
� Clinical syndrome of neonatal encephalopathy
� Does the patient meet criteria for therapeutic hypothermia?
Therapeutic Hypothermia: Inclusion criteria
� ≥36 weeks gestation and birth weight > 1800 grams
� Hypothermia can be initiated <6 hrs of life
� Evidence of HIE or perinatal depression/asphyxia
� Laboratory criteria� Cord or infant blood gas within 1 hr of age
� pH <7.00 OR base deficit ≥16 meq/L
� OR blood gas with pH 7.01-7.15 or base deficit 10-15.9 AND Apgar ≤5 at 10 min or ventilation required for at least 10 min
� Neurologic exam� Moderate or severe encephalopathy based on modified Sarnat
Score (Stage 2 or 3)

10/21/2016
8
Therapeutic Hypothermia: Exclusion criteria
� Major congenital anomalies
� Chromosomal syndromes
� Major head trauma causing intracranial hemorrhage
� Condition not compatible with survival
Cochrane Review 2013: Cooling for newborns with hypoxic-ischemic encephalopathy
� 11 randomized controlled trials through May 2012
� 1505 term and late preterm infants
� Moderate/severe encephalopathy and evidence peripartum asphyxia
� Cooling instituted <6 hours of age
� Outcome at 18 months� Statistically significant and clinically important
� Reduction in death, RR 0.75, NNT 11 (11 studies, 1468 infants)
� Reduction in neurodevelopmental disability of survivors, RR 0.77, NNT 8 (8 studies, 917 infants)
� Adverse effects of cooling minimal
� Benefits of cooling outweigh short-term adverse effects
Jacobs SE et al. 2013 RR=relative risk. NNT=number needed to treat.
Neuroprotective Mechanisms of Hypothermia
� Reduction in cerebral metabolism� Prevents edema and loss of membrane potential
� Reduces accumulation of glutamate, lactate, nitric oxide
� Inhibits platelet activating factor, inflammatory cascade
� Inhibits excito-oxidative cascade leading to secondary energy failure
� Inhibits enzymes responsible for apoptosis
� Reduces extent of brain injury
� Decrease in seizures???
Shankaran 2012, Johnston 2011

10/21/2016
9
Case 1 Follow Up
� Whole body hypothermia for 72 hours
� EEG mild encephalopathy (discontinuous)
� Brain MRI normal
� Home on AED, tapered off outpatient
� Development and neurological exam at 12 months normal
Case 2
� Term AGA female infant delivered via uncomplicated repeat C/S following normal pregnancy
� Events at 7 hrs of life in well baby nursery� Stiffening with apnea followed by limpness and pallor
� Brief, self-resolved
� During feeding and during bath
� Labs: normal electrolytes, CRP, CBC
� Transferred to NICU for further evaluation
Case 2
� Spells recurred
� Clinical encephalopathy emerged
� Feeding difficulties
� Hypotonia
� Decreased level of alertness

10/21/2016
10
Diagnostic Studies for Neonatal Encephalopathy
� Neuromonitoring� aEEG
� Conventional EEG- routine
� Conventional EEG- prolonged video
� Laboratory studies� Blood
� Urine
� CSF
� Neuroimaging� Head Ultrasound
� Head CT
� Brain MRI
Neuromonitoring in the NICU
� Indications� Evaluate seizures
� Differential diagnosis of paroxysmal events
� Electrographic seizures in high risk infants
� Assess risk for seizures
� Monitor anticonvulsant therapy
� Prognosis
� Severity and duration of abnormalities predictive
� Diagnostic evaluation of encephalopathy
Shellhaas et al. 2011
Neuromonitoring in the NICU
� Conventional EEG� Pro: Gold standard
� Con: Limited access to techs, interpretation
� aEEG� Pro: Apply and interpret at bedside, track trends
� Con: Lower sensitivity and specificity for seizures

10/21/2016
11
EEG for Prognosis in HIE
� cEEG� Burst suppression or low voltage poor prognosis >48 hrs
� aEEG
� Normalization of record by 48 hrs good prognosis
Nash et al. 2011, Thoresen et al. 2010
Burst Suppression EEG
Neonatal Seizures
� Neonatal brain predisposed to seizures� Excitation predominates in neuronal networks
� Inhibition relatively underdeveloped
� Incidence seizures 22-64% in mod-severe HIE� Decreased by hypothermia?
� Increasing evidence seizures increase neurologic injury
Volpe 2008, Wusthoff et al. 2011, Scher et al. 1993, Jensen 2006.

10/21/2016
12
Focal Seizure
Rhythmic sharp waves in left hemisphere associated with clonic jerking right arm and leg
Pinto LC and Gilberti P 2001
Case 2
� EEG: seizures confirmed, burst-suppression background
� Extensive neurometabolic and genetic lab evaluations (blood, urine, CSF)
� Brain MRI normal
� Multiple anticonvulsant medications � Phenobarbital, levetiracetam, lorazepam
� Seizures controlled on therapeutic phenytoin
Neonatal Epileptic Encephalopathies
� Inborn errors of metabolism� Nonketotic hypyerglycinemia (glycine encephalopathy) � Sulfite oxidase/molybdenum cofactor deficiency
� Pyridoxine deficiency or dependency� Folinic-acid responsive syndrome� Menke’s disease
� GABA transaminase deficiency� GLUT-1 deficiency syndrome � Peroxisomal disorders� Mitochondrial disorders
� Organic acidemias
� Structural brain malformation� Focal or multifocal cortical dysplasia� Hemimegalencephaly
� Infantile epileptic encephalopathies� Channelopathies� Other gene mutations

10/21/2016
13
Case 2 Follow Up
� Infantile epilepsy gene panel identified a clinically significant gene mutation
� At 18 months, she is seizure free on medication and has mild global developmental delay
Case 3
� Term baby boy, NSVD at home
� Perinatal depression: poor respiratory effort, received bag-mask ventilation, Apgars 4,6,8
� Seizures began at 1 ½ hrs of life (bicycling,
lipsmacking)� sodium 119, loaded phenobarbital
� Subsequent seizures within first 12 hrs of life
� tongue thrusting, lip smacking, rhythmic jerking both
arms and legs, clonic left arm only

10/21/2016
14
Case 3
� Exam: decreased movement and low tone of L arm
� EEG: initially discontinuous but normal by 2nd day of life, no epileptic activity
� Next diagnostic study?
Goals of Neonatal Neuroimaging
� Etiology of brain injury
� Evolution of brain injury
� Monitor effect of intervention
� Prognosis for future neurodevelopment
Imaging Modalities: Pros and Cons
� Head Ultrasound
� Head CT
� Brain MRI

10/21/2016
15
Brain MRI in HIE
• Brain MRI• Signal abnormalities on T1/T2 sequences appear 3-4 days
and best seen >7 days after injury
• Diffusion-weighted imaging
• Sensitive for acute ischemia
• Diffusion abnormalities most prominent 24-96 hrs of life
• Pseudonormalization 6-8 days (>10 days if cooled)
• MR spectroscopy
• High lactate within few hrs, NAA declines in days-week
• Severity of changes correlates with severity of brain injury
Bednarek et al. 2011
MRI for Prognosis
� Presence and severity of brainstem injury strongest predictor of neonatal death
� Abnormal signal posterior limb of internal capsule predicts inability to walk independently by 2 years
� Sensitivity 0.92, specificity 0.77
� MRI after hypothermia remains accurate predictor
Martinez-Biarge et al. 2011, Rutherford et al. 2010
Case 3
� MRI: acute stroke in right MCA territory

10/21/2016
16
Perinatal Stroke
� Focal or multifocal disruption in cerebral blood flow� Arterial or venous� Thrombosis or embolization
� Age between 20 weeks fetal age to 28 days postnatal age
� Confirmed by neuroimaging or neuropathologicalstudies
� Symptoms in neonates� Seizures� Encephalopathy� Abnormal neurologic examination
Perinatal Arterial Stroke
� Incidence:� As high as rates of large-vessel arterial strokes in adults
� >1:2500-4000 live births
� 90% occur within first week of life
� Risk factors for perinatal stroke� Infection, complex congenital heart disease,
preeclampsia, maternal drug use, traumatic delivery, inherited or acquired defect in coagulation, placenta pathology
� Recurrence rate <3%
Lee et al. 2005, Lynch 2009.
Case 3 Follow Up
� Remaining NICU course� Sodium normal by second day of life
� No seizures after 12 hrs of life
� Normal exam, weakness resolved by day 3
� At 19 months, mild left arm weakness and seizure-free

10/21/2016
17
Conclusions
� Causes of neonatal encephalopathy are diverse
� History, clinical examination and special diagnostic studies all contribute to determining the underlying diagnosis
� Effective treatments require recognition of the syndrome of neonatal encephalopathy and specific diagnosis of underlying etiology
� Newborn nurses have a critical role in recognizing encephalopathy in their patients
References-1
� Bednarek et al. Impact of therapeutic hypothermia on MRI diffusion changes in neonatal encephalopathy. Neurology 2011;78:1420-7.
� D’Alton ME et al. Neonatal Encephalopathy and Neurologic Outcome, Second Edition. Obstetrics & Gynecology 2014;123(4):896-901.
� Jacobs SE et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev 2013.
� Jensen FE. Developmental factors regulating susceptibility to perinatal brain injury and seizures. Curr Opin Pediatr. 2006;18:628-33.
� Johnston et al. Treatment advances in neonatal neuroprotection and neurointensive care. Lancet Neurol 2011;10:372-82.
� Lee et al. Predictors of outcome in perinatal arterial stroke: a population-based study. Annals of Neurology 2005;58:303-308.
� Lynch JK. Epidemiology and classification of perinatal stroke. Seminars in Fetal & Neonatal Medicine 2009;14:245–249.
� Martinez-Biarge et al. Predicting motor outcome and death in term hypoxic-ischemic encephalopathy. Neurology 2011;76:2055-61.
� McAdams RM and Juul SE. Neonatal encephalopathy: update on therapeutic hypothermia and other novel therapies. Clin Perinatol 2016;43:485-500.
� Nash et al. Video-EEG monitoring in newborns with hypoxic-ischemic encephalopathy treated with hypothermia Neurology 2011;76(6):556-62.
References-2
� Nelson et al. Antecedents of neonatal encephalopathy in the Vermont Oxford Network encephalopathy registry. Pediatrics 2012;130:878-886.
� Pinto LC and Giliberti P. Neonatal seizures: background EEG activity and the electroclinicalcorrelation in full-term neonates with hypoxic-ischemic encephalopathy. Analysis by computer-synchronized long-term polygraphic video-EEG monitoring. Epileptic Disorders 2001;3(3):125-32.
� Rutherford et al. Assessment of brain tissue injury after moderate hypothermia in neonates with hypoxic-ischemic encephalopathy: a nested substudy of a randomized controlled trial. Lancet Neurol 2010;9:39-45.
� Scher et al. Electrographic seizures in preterm and full-term neonates: clinical correlates, associated brain lesions, and risk for neurologic sequelae. Pediatrics 1993;91(1):128-34.
� Shankaran S. Hypoxic-ischemic encephalopathy and novel strategies for neuroprotection. ClinPerinatol 2012;39:919-929.
� Shankaran S et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 2005;353:1574-84.
� Shellhaas RA et al. The American clinical neurophysiology society’s guideline on continuous EEG monitoring in neonates. J Clin Neurophys 2011;28(6):611-7.
� Thoresen et al. Effect of hypothermia on amplitude-integrated electroencephalogram in infants with asphyxia. Pediatrics 2010;126(1):e131-9.
� Volpe JJ. Neurology of the newborn, 5th Ed. 2008.� Wusthoff et al. Electrographic seizures during therapeutic hypothermia for neonatal hypoxic-
ischemic encephalopathy. J Child Neurol 2011;26(6):724-8.