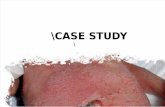
Neonatal Case Study
description
Transcript of Neonatal Case Study

Neonatal Case StudyPresented by: Mikaela Hew MS CN
June 11, 2013UCSD Dietetic Internship 2012-2013

Outline and Objectives
Neonatal patient populationNormal digestive tract/abdominal wall developmentWhat is Gastroschisis?Case study patient, medical course, complications, labs, growth
charts, medications, summary of feedingCholestasis of parenteral nutritionCase study nutrition care process (estimated needs, diagnosis,
monitoring and evaluation)Prognosis/Conclusion

Introduction
Gestational age• Preterm <37 weeks gestation• Term 37-42 weeks gestation• Post Term >42 weeks gestation
Birth weight• Low birth weight (LBW) <2,500g• Very low birth weight (VLBW) <1,500g• Extremely low birth weight (ELBW) <1,000g
Gastrointestinal and abdominal wall development

Gastroschisis: DefinitionStructural defect, or “hole” in the abdominal wall in which abdominal organs go out of the abdomen to the exterior of the body.

Gastroschisis: Pathophysiology and diagnosis
PATHOPHYSIOLOGY• Defective development of mesenchyme in abdominal wall• Involution of the umbilical vein causing weakness or rupture
DIAGNOSIS• Prenatal ultrasound 14 weeks after conception• Maternal Serum Alpha Fetoprotein (MSAFP)

Gastroschisis: Complications and Treatment
COMPLICATIONS• Amniotic fluid exposure interferes with normal development• Atresia• Hypothermia, dehydration, sepsis, hypoglycemia• Prolonged feeding problems, slow weight gain• Need for parenteral nutrition
TREATMENT• Surgery: necrotic segments, reduction of the bowel, gastrostomy,ileostomy, jejunostomy• SILO placement: protective covering for organs until the bowel is slowly reduced (by hand) back into the abdominal cavity.

Gastroschisis: Patient Outcomes
• Normal development, slow growth (Minnesota Neonatologists Study)• Need for prolonged parenteral nutrition• Depending on how much bowel is left, possible short gut/bowel
syndrome• Intestinal dysmotility• Malabsorption from mucosal injury• Gastroesophageal reflux
DIETARY MANAGEMENT

Case Study Patient
“BB” is a baby boy, born at 34 weeks, 4 days• Weight: 2064g (37th%) Length: 45cm (56th%) Head Circumference:31cm (50th%)
Mother 20 y/o G2P0111• G2: pregnant twice• P0: did not carry any to full-term• P01: had one pre-term• P011: had one abortion (or spontaneous abortion/miscarriage)• P0111: one is living
BB with no spontaneous cry, floppy. Radiant warmer, plastic bag, positive pressure ventilation, intubation and transfer to Neonatal Intensive Care Unit at 17 minutes of life. Born w/ Congenital Gastroschisis: necrosis, ischemia and perforation

APGAR Scores
Quick test performed at 1 and 5 minutes after birth.
• 1 minute: how well the baby tolerated the birthing process
• 5 minutes: how well the baby is doing outside the mother’s womb
Score out of 10
BB’s APGAR Scores:• 1 minute: 2• 5 minutes: 8 (-1 color, -1 respiratory
effort)

Medical Course: Digestive SystemDate Procedure Indication/Findings1/18/2013 Primary closure versus SILO placement attempt to close the abdomen, with gastrointestinal contents in place. BB required silo
placement in the operating room to temporarily house the intestines
1/24/2013 SILO Fascial Closure reduction of the bowel2/4/2013 Bowel Ultrasound found non-perfused tissue masses in the center of the abdomen, minimal peristalsis, care
team with guarded prognosis of bowel survival
2/12/2013 Upper Gastrointestinal Series series of x-rays found mid-bowel distension and stoppage of flow probably a result of atresia2/17/2013 Bowel ultrasound loop of bowel without perfusion, bowel improving3/6/2013 Barium enema found massive distension of proximal and mid-jejunal loops in the right side of the abdomen,
indicating obstruction by probable adhesions or stenosis. The findings are consistent with the history of small obstruction and relatively unused colon
3/12/2013 Exploratory laparotomy, segmental bowel resection, jejunostomy and mucous fistula
commonly referred to as “Loop ostomy”, an ostomy was created and mucous fistula which was used for re-feeding.
4/6/2013 Bloody output from proximal ostomy BB made NPO4/17/2013 Kidney, Ureter, Bladder (KUB) negative for obstruction4/17/2013 Distal ostomy contrast study caliber of colon appeared normal, no colonic stricture found5/6/2013 Herniation of proximal stoma required pressure, small blood loss5/13/2013 Small bowel follow-through no obstruction5/16/2013 Stoma closure/anastamosis attachment of bowel, stoma closure, required NPO


Medical Course: Additional Complications
DATE Medical Complication1/17/2013 Prematurity
1/19/2013 Anemia
1/28/2013 Elevated triglycerides
2/4/2013 Candidal dermatitis
2/11/2013 Cholestasis of parenteral nutrition/direct hyperbilirubinemia
2/23/2013 Peripheral pulmonic stenosis
2/23/2013 Neonatal thrombocytopenia
3/7/2013 Hypochloremia w/ metabolic alkalosis
3/28/2013 Neonatal abstinence syndrome-suspected-resolved
4/3/2013 Elevated GIR, Dbili
4/6/2013 Left Hydrocele
Ongoing High ostomy output with episode of dumping

Laboratory Values: Direct Bilirubin

Laboratory Values: Alkaline Phosphatase

Infant Growth: Weight
Normal for a preterm infant to lose weight after birth (≤15%)
Birth weight should be regained by two weeks of life
BB trends upward between the 10th-50th
%tile

Infant Growth: Length
Desired length of a preterm infant is about 0.8-1.1cm/week. For BB, now about 0.6-0.8cm/week at term.
Length more accurately reflects lean body mass and is not influenced by fluid status.
BB’s length experienced a few distinct drops in measurement, but is now trending back up along the 50th%tile.

Infant Growth: Head Circumference
Normal for an infant to lose head circumference during the first postnatal week by approximately 0.5cm.
Catch-up growth: 0.5cm/wk between birth and 3months.
BB’s head circumference has grown steady from March to date >50th%tile.

Vitamin Supplementation
FAT SOLUBLE VITAMINS: • Vitamin A: If premature, lower liver stores, lower serum retinol values• Vitamin E: If preterm, low body stores. Supplementation varies depending on
formula feeders, receiving therapeutic iron• Vitamin D: If preterm, limited reserves. If on PN, may have adequate serum
levels(most often supplied adequately in parenteral nutrition)
OTHER VITAMINS:• Vitamin K: endogenous production impaired by long term parenteral nutrition or antibiotic usage• Multivitamin may be warranted in low volume feedings

Mineral Supplementation
ELECTROLYTES• Sodium and potassium: excreted quickly during first 10-14 days in preterm
infants. • Magnesium, calcium, phosphorus are all accrued during the last trimester of
pregnancy. IRON
• Lower in preterm infant than term infant• Supplementation not indicated during first 2 weeks of life
TRACE MINERALS• Zinc for breastfed infants• Copper affected by dietary zinc

Nutritionally related medications/supplements
• At birth: Plasmalyte A IV bolus 21mL and 1,000mL infusion (water, electrolytes and 21kcal/L)NaCl 26mL, Vitamin K 1mg, Dextrose 10% • AQUADEKS 0.5mL 4/24-5/15 (likely supplemented in suspicion of malabsorption)• Cholecalciferol 400units 4/8-4/26 and 4/28-5/15 and 5/26-5/30 and 6/4-6/6• Epoetin Alfa 300units/kg 4/14-4/23• Pepcid 4/7-4/7• Prevacid 4/19-5/11 and 5/25-5/30 and 6/4 to current• Ferrous Sulfate 6.9 mg 4/14-4/25 (increased while on epoetin alfa)• Ferrous Sulfate 4.65mg 4/25-4/26 and 4/28-5/11 (decreased once patient started on small enteral feeds)• Ferrous Sulfate 5.4mg 5/11-5/15• Ferrous Sulfate 11.5mg 5/29-5/30• Fish Oil/DHA 100mg/mL 4/14-4/26• Actigall 15mg/kg 4/17-5/15• NaCl infusions since birth• Na Acetate in TPN since birth• Trace elements in TPN since birth• Pediatric multivitamin in TPN since birth

Summary of Feeding (See Handout)
• Bowel unable to be utilized due to Gastroschisis, areas of necrosis and ischemiaTotal Parenteral Nutrition
• Glucose infusion rate range: 8.8-15.6mg/kg/min• MBM used for 3 monthsPregestimilNeocate via Nipple and Gavage• Persistently elevated direct bilirubin
• IL lowered 1/18 from 2.5 to 2g/kg• IL lowered 4/27 from 3 to 2.5g/kg• IL lowered 5/21 from 2.5 to 1g/kg
• History of high output to ostomy with distal re-feeds. • Late March: 26-49.6mL/kg/d• 4/29-5/4: 23-62/mL/kg/d• Fish oil stopped 4/26
• Frequent NPO for procedures/tests, ostomy output• TPN has been providing 100% of estimated nutrition needs up until 2 weeks ago

Cholestasis of Parenteral Nutrition
• Diagnosed 2/11, approximately 1 month after birth• Common problem in the NICU
• Causes:• Long term dependence on TPN• Prematurity• Spontaneous ileal perforation• Gastroschisis• Multiple gastrointestinal surgical procedures

Cholestasis of Parenteral Nutrition
• Pathophysiology for elevated Direct Bilirubin:• Impaired hepatic bile flow• Immature organ development including adynamic gallbladder (bowel
disuse)• Upsurge in release of direct bilirubin as infant matures• Direct liver damage resulting from TPN
• Pathophysiology for high Alkaline Phosphatase• Damaged liver which regurgitates hepatic alkaline phosphatase back into
the serum• Impaired biliary excretion of the enzyme

Cholestasis of Parenteral Nutrition
Medical Nutrition Therapy
• Discontinuation of TPN with advancements of enteral feeding
• Cyclic TPN• Decreased doses of lipid infusion• Fish oil based IV fat emulsions, or oral
supplementation (Texas Children’s Hospital)

Estimated Nutrition Needs
Total Fluids: 150-200mL/kg/d110-120 kcal/kg/d3-4 g/kg Protein
Re-estimated nutrition needs (3/26)Total Fluids 150-200mL/kg/d120-130 kcal/kg/d3-4 g/kg Protein

Diagnosis/Monitoring and Evaluation
Nutrition Diagnosis (PES): Patient w/ altered GI function r/t Gastroschisis AEB Parenteral Nutrition
Monitoring/Evaluation:Continue gaining weight at approximately 30g/dAdvance from TPN to enteral feeding as medically ableMonitor GIR and trend direct bilirubinMonitor weight changes, GI status/availability for enteral feeding,
feeding progression, pertinent lab values.

Conclusion
• BB is now 145 days old • Prognosis for Gastroschisis promising and the neonatologists have
noted overall improvements in BB’s bowel health/healing.• BB continues to have difficulty with po feeding requiring TPN
• Recently large bilious residuals and emesis (indicative of intolerance)• Oral aversion w/ NG placement for enteral feeding
• Long term TPN in setting of poor po can continue to compromise organ function and increase the risk of metabolic bone disease.

References• Groh-Wargo S, Thompson M, Cox JH. Nutritional care for high-risk newborns. Bonus Books; 2000• Gastroschisis. University of Michigan Health System website. http://www.med.umich.edu/fdtc/diagnoses/fetal_diagnoses/abdominal/gastroschisis.shtml. Accessed May 31, 2013.• Pediatric Omphalocele and Gastroschisis. Medscape. http://emedicine.medscape.com/article/975583-overview#a0104. Accessed May 19, 2013.• Gastroschisis, what to expect. Minnesota Neonatal Physicians, P.A. website. http://www.minnesotaneonatalphysicians.org/info_gastroschisis.php?thisPage=parents. Accessed
May 31, 2013.
• Gastroschisis treatments. UCSF Medical Center.org. http://fetus.ucsfmedicalcenter.org/gastroschisis/treatment.asp. Accessed May 27th, 2013. • Durfee SM, Benson CB, Adams SR, et al. Postnatal outcome of fetuses with the prenatal diagnosis of gastroschisis. J Ultrasound Med. 2013;32(3):407-12.• Birth Defects: Gastroschisis. CDC.gov. http://www.cdc.gov/ncbddd/birthdefects/gastroschisis.html. Accessed June 8th, 2013.• Holland AJ, Walker K, Badawi N. Gastroschisis: an update. Pediatr Surg Int. 2010;26(9):871-8.• Santiago-Munoz PC, McIntire DD, Barber RG, Megison SM, Twickler DM, Dashe JS. Outcomes of pregnancies with fetal gastroschisis. Obstet Gynecol 2007:110 (3); 663–8.• Apgar Scores. Medline Plus Website. http://www.nlm.nih.gov/medlineplus/ency/article/003402.htm. Updated December 2, 2011. Accessed March 12, 2013.• Hydrocele. Mayo Clinic website. http://www.mayoclinic.com/health/hydrocele/DS00617. Accessed May 28, 2013.• M.D. RE. Pediatric Nutrition Handbook. American Academy of Pediatrics; 2009.• Nehra D, Carlson SJ, Fallon EM, et al. A.S.P.E.N. Clinical Guidelines: Nutrition Support of Neonatal Patients at Risk for Metabolic Bone Disease. J Parenter Enteral Nutr. 2013;1-29• Beaston, L. Preterm Infant Nutrition Guide. Rady’s Children’s Hospital 2013;1-3.• Wong KK, Lan LC, Lin SC, Chan AW, Tam PK. Mucous fistula refeeding in premature neonates with enterostomies. J Pediatr Gastroenterol Nutr. 2004;39(1):43-5.• Klein CJ, Revenis M, Ravenis M, Kusenda C, Scavo L. Parenteral nutrition-associated conjugated hyperbilirubinemia in hospitalized infants. J Am Diet Assoc. 2010;110(11):1684-
95.• Causes of Neonatal Cholestasis. UpToDate. http://www.uptodate.com/contents/causes-of-neonatal-cholestasis. Accessed June 4th, 2013.• Enzymatic Measures of Cholestasis. UpToDate. http://www.uptodate.com/contents/causes-of-neonatal-cholestasis. Accessed June 4th, 2013.• Rees C. Management of PN-induced Cholestasis. Practical gastroenterology 2005: (24);62-68 • Klein CJ, Havranek TG, Revenis ME, Hassanali Z, Scavo LM. Plasma fatty acids in premature infants with hyperbilirubinemia: before-and-after nutrition support with fish oil
emulsion. Nutr Clin Pract. 2013;28(1):87-94.
• Rangel S, Calkins C, Cowles R, Barnhart D, Huang E, Abdullah F, Arca M, Teitelbaum D. Parenteral nutrition-associated cholestasis: an American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J of Pediatric Surgery 2012: 47(1); 225-240.
• Premkumar MH, Carter BA, Hawthorne KM, King K, Abrams SA. High rates of resolution of cholestasis in parenteral nutrition-associated liver disease with fish oil-based lipid emulsion monotherapy. J Pediatr. 2013;162(4):793-798.e1.
• Cholestasis. Evidence Analysis Library of Academy of Nutrition and Dietetics. http://andevidencelibrary.com/search.cfm?keywords=cholestasis&x=0&y=0. Accessed June 3, 2013.• Evidence Analysis Library. Academy of Nutrition and Dietetics. http://andevidencelibrary.com/default.cfm. Accessed June 4th, 2013.• Hagadorn, James I; Wolkoff, Leslie; Esposito, Patricia; Brumberg, Heather L; Emerick, Karan; Gerace, James R. Alterations in parenteral nutrition management for the treatment of
parenteral nutrition‐associated cholestasis in term and preterm infants. Cochran Library 2009: 2
• Hagadorn, James I; Wolkoff, Leslie; Esposito, Patricia; Brumberg, Heather L; Emerick, Karan; Gerace, James R. Medical therapies for parenteral nutrition‐associated cholestasis in term and preterm infants. Cochran Library 2009: 2
• Feldman D, Pike JW, Adams JS. Vitamin D. Academic Press; 2011.• Mutlu M, Cayir A, Cayir Y, Ozkan B, Aslan Y. Vitamin D and Hyperbilirubinaemia in Neonates. HK J Paediatr 2013;18:77-81• Burstyne M, Jensen GL. Abnormal liver functions as a result of total parenteral nutrition in a patient with short-bowel syndrome. Nutrition. 2000;16(11-12):1090-2.• Brumbaugh D, Mack C. Conjugated hyperbilirubinemia in children. Pediatr Rev. 2012;33(7):291-302.• Mehta NM, Compher C. A.S.P.E.N. Clinical Guidelines: nutrition support of the critically ill child. J Parenter Enteral Nutr. 2009;33(3):260-76.