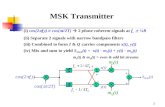
MSK & Burns Rehabilitation Nursingswostroke.ca/wp-content/uploads/2015/12/J-CNA-MSK... ·...
Transcript of MSK & Burns Rehabilitation Nursingswostroke.ca/wp-content/uploads/2015/12/J-CNA-MSK... ·...
www.capitalhealth.ca
MSK & BurnsRehabilitation Nursing
Glenrose Rehabilitation
Hospital
January 11, 2006
Page 22010/08/30
Edmonton and Areawww.capitalhealth.ca
Learning ObjectivesMSK Rehabilitation Nursing
At the conclusion of the presentation the Rehabilitation Nurse will be able to explain:
The anatomy of the MSK system
The pathophysiology of MSK impairment
Clinical signs & symptoms related to MSK impairment
Lab results related to MSK impairment
Rehabilitation nursing interventions to provide care & education for clients with MSK impairment
Page 32010/08/30
Edmonton and Areawww.capitalhealth.ca
Anatomy and Physiology
Skeleton “dried-up body”: bones lying buried within muscles and other soft tissues, providing a rigid framework and support structure of the whole body
Axial: bones that form the longitudinal axis of the body
Appendicular: bones of the limbs and girdles
Page 42010/08/30
Edmonton and Areawww.capitalhealth.ca
Functions
Interdependent with other body systems
Provides protection for vital organs
Provides sturdy framework to support body structures
Stores calcium, phosphorus, magnesium, fluoride
Produces red and white blood cells (hematopoiesis)
Joints and muscles together allow body movement and assist in maintaining body temperature
Page 52010/08/30
Edmonton and Areawww.capitalhealth.ca
Structure and Function
206 bones in human body (350 in infants)
Two basic types of osseous (bone tissue):
• Compact bone (cortical)…dense, smooth and homogeneous
• Spongy bone (cancellous)…a branching network of trabeculae arranged to resist stresses and strains
Page 62010/08/30
Edmonton and Areawww.capitalhealth.ca
Classification
Regionally or according to shape
• Long
• Short
• Flat
• Irregular
• Sesamoid
Page 72010/08/30
Edmonton and Areawww.capitalhealth.ca
Classification
Long bone: • found in limbs (e.g. humerus, femur)• length is greater than width• tubular shaft (diaphysis) and usually a epiphysis at
each end• shaft has a central marrow cavity (yellow for adults;
red for infants)• outer part of shaft is composed of compact bone
covered by connective tissue sheath (periosteum)• ends are composed of spongy bone surrounded by
thin layer of compact bone (articular surfaces covered by hyaline cartilage)
Page 82010/08/30
Edmonton and Areawww.capitalhealth.ca
Classification
Short bone:
• found in hand and foot (e.g. scaphoid, calcaneous)
• cuboidal in shape
• composed of cancellous bone (spongy) surrounded by thin layer of compact bone
• covered with periosteum and articular surfaces covered by hyaline cartilage
Page 92010/08/30
Edmonton and Areawww.capitalhealth.ca
Classification
Flat bone:
• found in vault in skull (e.g. frontal and parietal bones)
• composed of thin inner and outer layers of compact bone
Page 102010/08/30
Edmonton and Areawww.capitalhealth.ca
Classification
Irregular bone:
• include the vertebrae and pelvic bones
• composed of thin shell of compact bone
• interior composed of cancellous bone
Page 112010/08/30
Edmonton and Areawww.capitalhealth.ca
Classification
Sesamoid bone:
• small nodules of bone found in certain tendons where they rub over bony surfaces
• greater [part of sesamoid bone is buried in the tendon and the free surface is covered with cartilage
• largest is the patella (located in the quadriceps femoris)
• function is to reduce friction on the tendon; may also alter the direction of a pull tendon
Page 122010/08/30
Edmonton and Areawww.capitalhealth.ca
Bone Anatomy
spongy bone: needle-like threads surround a network of spaces (trabeculae)
compact bone: no network of open spaces; instead have numerous structural units (osteon or haversian system)
bones are not lifeless; many living bone cells called osteocytes
Page 132010/08/30
Edmonton and Areawww.capitalhealth.ca
Bone Development
Developed by two methods:
• Membranous: bone developed directly from a connective tissue membrane
• Endocondral: a cartilaginous model is first laid down and later replaced by bone
Page 142010/08/30
Edmonton and Areawww.capitalhealth.ca
Bone Development
Osteoblasts: bone building cells; secrete collagen
Osteoclasts: cells that break bone down (bone resorption)
Osteoblasts and osteoclasts work side by side to shape bones
Page 152010/08/30
Edmonton and Areawww.capitalhealth.ca
Bone Healing
Hematoma and inflammation Angiogenesis and cartilage formation Cartilage calcification Cartilage removal Bone formation Remodeling• Serial x-ray films are used to monitor the progress
of bone healing• Type of bone fractured, adequacy of blood supply,
surface contact of fragments and general health of the person influence the rate of fracture healing.
Page 162010/08/30
Edmonton and Areawww.capitalhealth.ca
Structure
Junction of two or more bones is called a joint (articulation)
3 types of joints:
Synarthrosis
Amphiarthrosis
Diarthrosis
Page 172010/08/30
Edmonton and Areawww.capitalhealth.ca
Joints
Synarthrosis: immovable (skull sutures)
Amphiarthrosis: limited motion (vertebral joints and symphysis); bones are joined by fibrous cartilage
Diarthrosis: freely movable
Page 182010/08/30
Edmonton and Areawww.capitalhealth.ca
Types of diarthrosis joints
Ball-and-socket: permit full freedom of movement (hip and shoulder)
Hinge: permit bending in one direction (elbow and knee)
Saddle: allow movement in two planes at right angles to each other (base of the thumb)
Pivot: characterized by the articulation between radius and ulna
Gliding: limited movement in all directions (wrist)
Page 192010/08/30
Edmonton and Areawww.capitalhealth.ca
Page 202010/08/30
Edmonton and Areawww.capitalhealth.ca
Page 212010/08/30
Edmonton and Areawww.capitalhealth.ca
Muscle Contractions
Isometric: muscle length remains constant but force generated by muscles is increased
Isotonic: muscle shortening with no increase in tension within the muscle
Page 222010/08/30
Edmonton and Areawww.capitalhealth.ca
Muscle Tone
Tone: relaxed muscles demonstrate a state of readiness to respond to contraction stimuli
• A muscle that is limp and without tone is flaccid
• A muscle with greater-than-normal tone is spastic
• In conditions characterized by lower motor neuron destruction, denervated muscle becomes atonic (soft and flabby) and atrophies
Page 232010/08/30
Edmonton and Areawww.capitalhealth.ca
Exercise, Disuse and Repair
Hypertrophy: when muscle repeatedly develops maximum tension over time, the cross-sectional area of muscle increases; persists only if the exercise continues
Atrophy: decrease in the size of the muscle because of disuse over a long period of time
Bedrest and immobility cause loss of muscle mass and strength.
Page 242010/08/30
Edmonton and Areawww.capitalhealth.ca
Gerontologic Considerations
Bone mass peaks at about 35 years of age Loss of height due to osteoporosis, kyphosis,
thinned intervertebral discs, and flexion of the knees and hips.
Osteoporosis due to metabolic changes (withdrawal of estrogen and decreased activity)
Bones change in shape and have reduced strength
Page 252010/08/30
Edmonton and Areawww.capitalhealth.ca
Gerontologic Considerations
Fractures are commonCollagen structures are less able to absorb
energy Ligaments become weakOsteoarthritis: joints enlarge and ROM is
diminished Increased inactivity, diminished neuron
stimulation, and nutritional deficiencies contribute to loss of muscle strength
Page 262010/08/30
Edmonton and Areawww.capitalhealth.ca
Fractures
A break in the continuity of the bone and is defined according to its type and extent
Bone is subjected to stress greater than it can absorb
Caused by direct blows, crushing forces, sudden twisting motions, and extreme muscle contractions
Page 272010/08/30
Edmonton and Areawww.capitalhealth.ca
Types of Fractures
Complete: across the entire cross-section of the bone and frequently displaced
Incomplete: through only part of the cross-section of the bone
Comminuted: produces several bone fragments
Closed (simple): does not cause break in skin
Open (compound): skin or mucous membrane wound extends to the fractured bone
Page 282010/08/30
Edmonton and Areawww.capitalhealth.ca
Fractures: Clinical Manifestations
Pain
Loss of function
Deformity
Shortening
Crepitus
Swelling and discoloration
Page 292010/08/30
Edmonton and Areawww.capitalhealth.ca
MSK Modalities
Pelvis: fused, stable, bony ring including sacrum, pubis, and ischium bones
• Stable
• Unstable
Page 302010/08/30
Edmonton and Areawww.capitalhealth.ca
MSK Modalities
Joint Replacement:
• Patients with severe joint pain and disability
• Conditions include osteoarthritis, rheumatoid arthritis, trauma, and congenital deformity
• Joints frequently replaced include hip, knee and finger joints
• “Simple” replacements not usually seen in rehab settings
• Complicated hips (Co-morbidities) and subsequent replacements seen
Page 312010/08/30
Edmonton and Areawww.capitalhealth.ca
Page 322010/08/30
Edmonton and Areawww.capitalhealth.ca
Total Hip Replacement
Indications include: arthritis, femoral neck fractures, failure of previous reconstructive surgeries and problems with congenital hip disease
Usually 60 years or older, however, younger patients with severely damaged and painful hip joints are having surgery
Page 332010/08/30
Edmonton and Areawww.capitalhealth.ca
Total Hip Replacement
Nursing Implications:
• Awareness of potential complications including: dislocation of hip prosthesis, excessive wound drainage, thromboembolism, infection, heel pressure ulcer, heterotrophic ossification, avascular necrosis, and loosening of the prosthesis
Page 342010/08/30
Edmonton and Areawww.capitalhealth.ca
Total Hip Replacement: Patient Teaching
Daily exercise
Use of assistive devices (crutches, walker, cane)
Position legs in abduction and do not flex the hip more than 90 degrees
Avoid certain activities
Page 352010/08/30
Edmonton and Areawww.capitalhealth.ca
Knee Replacement
Indications: severe pain and functional disabilities related to joint surfaces destroyed by arthritis or bleeding into the joint (hemophilia)
• If a patient’s ligaments have weakened, a fully constrained (hinged) or semiconstrained prosthesis may be used to provide joint stability. A nonconstrained prosthesis depends on the patient’s ligaments for joint stability
Page 362010/08/30
Edmonton and Areawww.capitalhealth.ca
Knee Replacement
Efforts are directed at preventing complications (thromboembolism, peroneal palsy, infection, limited ROM)
Frequently, a CPM device is used
Knee is protected with a knee immobilizer (splint, cast or brace) and is elevated when sitting in a chair
Weight-bearing limits are prescribed
Page 372010/08/30
Edmonton and Areawww.capitalhealth.ca
Tibia and Fibula
Most common fracture below the knee resulting from a direct blow, falls with the foot in the flexed position, or a violent twisting motion
Often occur in association with each otherFractures are often open and involve severe
soft tissue damage because of little subcutaneous tissue in the area
Assess for complications
Page 382010/08/30
Edmonton and Areawww.capitalhealth.ca
Managing an External Fixator
Provide support for severe comminuted fractures while permitting active treatment of damaged soft tissue
Fracture is reduced, aligned, and immobilized by a series of pins inserted in the bone
Pin position is maintained through attachment to a portable frame
Provides patient comfort, early mobility, and active exercise of adjacent uninvolved joints
Complications related to disuse and immobility are minimized
Page 392010/08/30
Edmonton and Areawww.capitalhealth.ca
Page 402010/08/30
Edmonton and Areawww.capitalhealth.ca
External Fixator: Nursing Implications
Prepare the patient psychologically Assess for complications Pin care Never adjust the clamps on the frame Teach and encourage isometric and active exercises Assist with weight bearing (as prescribed by the
physician) Fixator is removed after the soft tissue heals; may
require additional stabilization (cast or molded orthosis) while healing
Page 412010/08/30
Edmonton and Areawww.capitalhealth.ca
Ilizarov External Fixator
Device used to correct angulation and rotational defects, to treat non-union, and to lengthen limbs
Tension wires attached to fixator rings; joined by telescoping rods
Bone formation stimulated by prescribed daily adjustments of the telescoping rods
Generally encourage weight bearing
Correction achieved, no adjustments made, fix
Page 422010/08/30
Edmonton and Areawww.capitalhealth.ca
Casting
Indications: applied for purposes of immobilization
Plaster, synthetic fiberglass and synthetic non-fiberglass
Upper extremities, lower extremities, trunk, hip or shoulder areas (spica)
Page 432010/08/30
Edmonton and Areawww.capitalhealth.ca
Casting: Nursing Implications and Complications
Casting process can cause burning
Constrictive edema
Decubitus ulcer
Drop foot
Page 442010/08/30
Edmonton and Areawww.capitalhealth.ca
Page 452010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction
• The application of a pulling force to a part of the body
Page 462010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction Guidelines
Purpose:
• To prevent or reduce muscle spasm
• To immobilize a joint or part of the body
• To reduce a fracture or dislocation
• To treat joint pathology(s)
Page 472010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction Guidelines
The traction setup must:
• Align the distal fragment to the proximal fragment
• Remain constant
• Allow for adequate exercise and diversion
• Allow for optimum nursing care
Page 482010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction Guidelines
Counter traction: the resistance of the body to move in a direction of the forces exerted by a traction device.
• Utilizes the patients body weight; may be increased by elevation of the foot of the bed
Page 492010/08/30
Edmonton and Areawww.capitalhealth.ca
Types of Traction
3 basic types:
Manual: hands are used to exert a pulling force on the bone which is to be realigned.
Skin: strips of tape, moleskin, or some type of commercial skin traction strips applied directly to the skin e.g. traction boots.
Skeletal: tractive force applied directly to the bone using pins, wires and screws.
Page 502010/08/30
Edmonton and Areawww.capitalhealth.ca
Skeletal Traction
Requires the use of Steinmann pins or Kirschner wires for long bone fractures.
Differences are in diameter (Steinmann are larger).
Both comes in a variety of lengths.
Choices based on physician preference, density of bone pin or wire to be inserted through, and the forces to be applied.
Page 512010/08/30
Edmonton and Areawww.capitalhealth.ca
Skeletal Traction
Can also be divided based on the direction of force:
• Straight-line traction e.g. Buck’s traction
• Block and tackle (suspensory)
Page 522010/08/30
Edmonton and Areawww.capitalhealth.ca
Application of Traction
Skin traction cannot be applied over an open wound
Check with patient for possible adhesive allergies
Do not reuse traction cord
Avoid pressure on bony prominences
Never add/remove weights without a written physicians order
Allow weights to hang freely
Never add anything to traction unless ordered by a physician
Page 532010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction: Nursing Implications
Regular visual inspection and documentation includes:
• Weights are hanging freely
• Rope condition and placement
• Knots are free from pulley’s
• Bed linens etc. not interfering with traction
Page 542010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction: Nursing Implications
Maintain proper positioning
Maintain continuous traction
Maintain correct line of pull
Neurovascular checks
Skin examination
Maintain patient independence
Traction systems can vary
NEVER IGNORE A PATIENT’S COMPLAINT
Page 552010/08/30
Edmonton and Areawww.capitalhealth.ca
Traction: Complications
Allergy to adhesive
Skin excoriation and pressure sore development
Peroneal palsy
Bone infection
Depressed scars
Page 562010/08/30
Edmonton and Areawww.capitalhealth.ca
Arthritis
One of the most prevalent chronic health conditions in Canada
A major cause of morbidity, disability, & HC utilization
2000 Affected 16% of population > 15 yrs Includes a large variety of diseases &
conditions
Page 572010/08/30
Edmonton and Areawww.capitalhealth.ca
Osteoarthritis
Affects both sexes, more women then men
Age – single most important factor
2x as common with obesity
Primary with unknown etiology
2nd due to joint injury & long term mechanical stressors
Often affects weight bearing joints first
Degenerative; caused by loss of cartilage
Page 582010/08/30
Edmonton and Areawww.capitalhealth.ca
Osteoarthritis
Pain is often localized
Unilateral joint involvement
Slow course of disease with flare-ups
Crepitus, audible grating, swelling, pain, decreased mobility
Treatment: PT, Stress Reduction, Pain management, Osteotomy, Joint Replacement
Page 592010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory DisordersRheumatoid Arthritis
Chronic, systemic, inflammatory disease affecting the synovia of the joints
Affects all racial/ethnic groups Affects women 2-3 x as often as men Onset at any age (commonly 20 – 40 yrs) Etiology unknown - Theories:
- Autoimmune process- Genetic predisposition- Immune response to unknown antigen- Environmental Factors
Page 602010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory Disorders Rheumatoid Arthritis
Hands affected early; then wrists, ankles, knees
Advanced: hips, shoulders, all joints
May affect all connective tissue
Remissions & exacerbations
Lab results: ↑ erythrocyte sed rates; + rheumatoid factor
Page 612010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory DisordersRheumatoid Arthritis
Treatment goals:– Preservation of function
– Reduction of pain & inflammation
– Prevention of deformities (or correction)
Treatment begins conservatively: rest, salisylates & PT
Patient education program – link to resources (Arthritis Society)
Page 622010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory DisordersRheumatoid Arthritis
Medications: salicylates, NSAIDs, indoles,, antimalarials, penicillinase, with Enbrel, Corticosteroids
Treatments: Immobilization of joints in acute flare-ups; applications of hot & cold, splints to maintain function
Page 632010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory Disorders Juvenile Arthritis
5th most common chronic illness
Cause: Environmental Theories (Microbial, etc.)
S&S of sepsis (fever) ; arthralgias
Serology results
Growth & developmental delay as a result of
↓ physiological function
Progressive systemic sclerosis or scleroderma
Page 642010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory DisordersSystemic Lupus Erythematosus (SLE)
Multisystem, autoimmune, inflammatory disorder
Unknown etiology
Initial manifestation of transient arthritis
Multisystem: Remissions & Exacerbations
Manifestations: Facial butterfly rash, skin rashes, fever, weakness/fatigue, anemia, mouth ulcers, photosensitivity, alopecia, kidney disease,
peri/myocarditis, pleurisy, depression
Page 652010/08/30
Edmonton and Areawww.capitalhealth.ca
Systemic Lupus Erythematosus (SLE)
Management:
Prevention of exacerbations
Nutrition – weight loss or gain
Caution with OTC meds, immunizations
Medications: NSAIDS
Antimalarials- highly effective but slow acting in controlling lupus arthritis, rashes, fatigue
Page 662010/08/30
Edmonton and Areawww.capitalhealth.ca
Systemic Lupus Erythematosus (SLE)
Meds cont’d:
Corticosteroids –reduce inflammation; many side effects
Azathioprine- transplant medication,
immunosuppressant
Cyclophosphamide- for severe infections Used when many organs have been affected
Page 672010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory DisordersSpondylarthropathies
“Spinal arthritis”: group of inflammatory arthropathies with unknown etiology
Common S&S: Inflammatory arthritis of the back (tendon- ligament
insertion points)
Skin lesions may also occur
↑ specific HLA
Absent Rheumatoid Factor
Page 682010/08/30
Edmonton and Areawww.capitalhealth.ca
Inflammatory DisordersAnkylosing Spondylitis
Onset of mild pain in adolescence
Progression: increasing pain & restricted movement d/t development of postural abnormalities
Diagnosis based on S&S
Lab tests
Page 692010/08/30
Edmonton and Areawww.capitalhealth.ca
Metabolic Disorders
Gout – uric acid crystalizes & is deposited in the synovial fluid, joints or articular cartilage
Majority are men > 30
S&S – severe pain, swelling
Diagnosis – History, Lab, Physical Exam
Treatment: Diet, NSAIDS, prednisone colchicine
Page 702010/08/30
Edmonton and Areawww.capitalhealth.ca
Osteoporosis “The Silent Thief”
Bone loss results when bone resorption exceeds bone formation-resulting in decreased bone density increased fragility & risk of fractures (hip, wrist & spine)
Types of osteoporosis include:
- Postmenopausal ( 55 – 70 )
- Senile (over age 70)
- Disease/disuse
Page 712010/08/30
Edmonton and Areawww.capitalhealth.ca
Osteoporosis
Prevalence 1.4 million Canadians (5:1 women to men)
Risk Factors: Genetic, Nutritional, Lifestyle, Ethnic, Endocrine, Medications
Management:- Medications: Oral calcium 800 – 1200 mg/day
- Vitamin D, Estrogen replacement therapy,
- Calcitonin injections (SC or IM)
- Other: Exposure to sunlight, weight bearing exercises
Page 722010/08/30
Edmonton and Areawww.capitalhealth.ca
Osteoporosis
Lab results usually normal
Xray: >30% bone loss
Bone mineral density test
Prevention – strategies to develop peak bone mass & reduce risk factors begin with the young
Page 732010/08/30
Edmonton and Areawww.capitalhealth.ca
Fibromyalgia Syndrome FMS
Associated with RA, SLE
Unknown etiology: theory of normal aging, genetics or environmental factors
High incidence rate in females (85%)
Chronic pain, tenderness, stiffness, fatigue & sleep disturbances
Symmetrical pressure points painful to touch
Page 742010/08/30
Edmonton and Areawww.capitalhealth.ca
Osteogenesis imperfecta
Genetic disorder characterized by bones that break easily with little or no cause
Genetic
Characteristic features vary greatly
Skin biopsy – determine amount of collagen
Surgery – rods placed in long bones to stabilize
Nursing care involves caution with all care
Page 752010/08/30
Edmonton and Areawww.capitalhealth.ca
Traditional Nonpharmacological Interventions
Application of heat & cold
Cold decreases pain & swelling
Heat relaxes the joint & increases ROM
FES (Functional Electrical Stimulation)
Biofeedback techniques – reduce stress
Page 762010/08/30
Edmonton and Areawww.capitalhealth.ca
Alternative Management
Acupuncture
Magnetic therapy
Glucosamine
Herbal preparations
T’ai Chi
Page 772010/08/30
Edmonton and Areawww.capitalhealth.ca
Exercise
OA – daily exercise, progression, general fitness
RA – based on disease progression, patient fatigue level, etc.
Fibromyalgia – slowly increasing exercise relieves S&S
Page 782010/08/30
Edmonton and Areawww.capitalhealth.ca
Complications
Anticoagulation – heparin, warfarin
DVT - common post hip/knee replacement
PE – common complication of DVT, orthopedic surgery
Page 792010/08/30
Edmonton and Areawww.capitalhealth.ca
Complications
HITT - Heparin Induced Thrombocytopenia
Hemophilia - a hereditary coagulation disorder
Anemia – 2nd to blood loss (acute or chronic) nutritional, chronic disease
Page 802010/08/30
Edmonton and Areawww.capitalhealth.ca
MSK Complications
Infections – acute, chronic require prevention! Osteomyelitis, tetanus, gas gangrene
Neuropathic Pain – injury/ aberrant stimulation of the efferent nervous system
Compartment syndrome – high pressure within a closed fascial space reduces the capillary perfusion required
Page 812010/08/30
Edmonton and Areawww.capitalhealth.ca
Nursing
Comprehensive history
Physical examination
Pain assessment
Limitations in performing ADLs
Psychological assessment (changes in body image)
Role change, job retraining
Page 822010/08/30
Edmonton and Areawww.capitalhealth.ca
Mobility
Maintain mobility with therapeutic exercise
Safety considerations
ROM exercises
Therapeutic positioning & positioning aids
Ambulation & gait training
Page 832010/08/30
Edmonton and Areawww.capitalhealth.ca
Mobility
Assessment of movement– Physical: ROM, Muscle strength, balance/coordination,
Weight bearing status (full, partial, non)
– Cognitive
– Psychological
– Environmental
– ROM
Page 842010/08/30
Edmonton and Areawww.capitalhealth.ca
Immobility
Prevent impairment from immobilityMSK – weakness, muscle atrophy,↓ ROM, contractures, osteopenia, HOCV – deconditioning, thromboembolism, postural responsesIntegument - breakdownRespiratory - PneumoniaGU – UTIsGI – constipationCNS – depression, irritability, confusion, social isolation
Page 852010/08/30
Edmonton and Areawww.capitalhealth.ca
Mobility with Aids
Ambulation Aids:• Canes: correct length; Various types. Hold on
• unaffected side, advance cane then affected leg
• Walkers: Various types. Advance walker, affected leg, unaffected leg
• Crutches: correct length. 2, 3, 4 point gait
• Wheelchairs: individualized
Page 862010/08/30
Edmonton and Areawww.capitalhealth.ca
Client Wheelchair Education
Education should include:• Transfers to and from the chair
• Position changes and weight shifts required
• Basic wheelchair maintenance. Modifications increase maintenance & costs
• Operating the wheelchair safely indoors & out
Page 872010/08/30
Edmonton and Areawww.capitalhealth.ca
Orthotics, Splints & Braces
AFOs – prevents ankle pronation; used with the shoe
Corrective shoes routinely used with orthotics
KAFOs – stability at knee, ankle & foot
Page 882010/08/30
Edmonton and Areawww.capitalhealth.ca
Self-CarePersonal Hygiene
Many devices available• Hair – built up handle, universal cuff, loops strapped to
handle
• Oral Hygiene
• Grooming: fixed containers
• Dressing: modification in design & assistive devices • Stretchable clothes, adaptations with velcro, large buttons, loops
on zippers
• Shoes with velcro or elastic closures
• Reachers, long handled shoehorsn, sock pull-ups
Page 892010/08/30
Edmonton and Areawww.capitalhealth.ca
Home Assessment
Home Assessment • Stairs – indoors & out
• Location of all rooms, accessibility
• Thresholds, floor obstructions & coverings
• Furniture arrangement & ability to use
• Telephone location, ability to use
• Bathroom size, safety equipment, toilet height,
• Bedroom height of bed
• Other safety considerations: Ability to control water temperature, access to phone, TV while in bed
Page 902010/08/30
Edmonton and Areawww.capitalhealth.ca
Self-CareBathing & Toileting
Access
Safety bars on the tub & toilet
Benches or tub seats
Hand held shower hoses
Non-slip bath mats & other surfaces
Transfer board
Raised toilet seat
Page 912010/08/30
Edmonton and Areawww.capitalhealth.ca
Altered Body Image
Altered gait, use of assistive devices, deformities, rheumatoid nodules, bruising
Directly related to functional ability
Requires ongoing assessment of the client based on developmental stage
Timing of interventions is essential
Peer support groups are often helpful
Individual counseling may be preferable
Page 922010/08/30
Edmonton and Areawww.capitalhealth.ca
Rehab Nursing Interventions
Prevent complications
Promote quality of life
Promote positive self concept
Advocate through client education & health promotion
Page 932010/08/30
Edmonton and Areawww.capitalhealth.ca
References
Carlos, A. (2005). A Practical Illustrated Guide to Modern Orthopaedics. Mediscript Communications Inc.; Canada.
Homan, S. (2002). Rehabilitation Nursing: Process, Application & Outcomes. 3rd Ed., Mosby; St. Louis.
Schoen, D. (2000). Adult Orthopedic Nursing
Lippincott, Williams & Wilkens; Philadelphia.
Page 942010/08/30
Edmonton and Areawww.capitalhealth.ca
References
Smeltzer, S., Bare, B. (2004). Brunner & Suddarth’s Textbook of Medical – Surgical Nursing. 10th Ed., Lippincott Williams & Wilkens; Philadelphia.
Phipps, W., Monahan, F., Sands, J., Marek, J ., Neighbors, M. (2003). Medical-Surgical Nursing: Health & Perspectives. 7th Ed., Mosby; St. Louis.
www.capitalhealth.ca
Nursing the Rehabilitation Client with Burns
January 11, 2006
Glenrose Rehabilitation Hospital
Edmonton, Alberta
Page 962010/08/30
Edmonton and Areawww.capitalhealth.ca
Objectives
1. Review of the anatomy of skin in relation to burns
2. Discussion of the pathophysiology of burns
3. Examination of the potential complications of burns
4. Rehabilitation nursing interventions for the patient with burns
Page 972010/08/30
Edmonton and Areawww.capitalhealth.ca
Survivability
• The chances of surviving a severe burn has increased dramatically in the past 20 years - a person with 70% burns now has a 50% chance of surviving.
Factors associated with survivability include:1. Age - the very old or very young have increased
mortality2. Total body surface area burned (TBSA) Time +
Intensity = Damage3. Inhalation injury - increases mortality by 30% and
lengthens stay4. Pneumonia and sepsis leading cause of death
Page 982010/08/30
Edmonton and Areawww.capitalhealth.ca
Pathophysiology of Burns/Anatomy of the Skin
Page 992010/08/30
Edmonton and Areawww.capitalhealth.ca
Burn Assessment
• Mechanism of injury/causative agent
• Depth
• Extent
• Patient age
• Location of injury
• Comorbid factors
Page 1002010/08/30
Edmonton and Areawww.capitalhealth.ca
Types of Burns
• Thermal
• Electrical
• Chemical
• Inhalation
• Radiation
Page 1012010/08/30
Edmonton and Areawww.capitalhealth.ca
Thermal Burns
– Most common type, includes exposure to steam, flash, scald, contact and flame
– Caused by exposure or contact with flame, hot liquids, steam, tar or hot objects
– Use cool water initially to decrease skin temperature
– S/S: pain, redness, swelling and drainage of pus
– dressings: AgNO3, polysporin
Page 1022010/08/30
Edmonton and Areawww.capitalhealth.ca
Electrical or Lightning Burns
– Severity of damage is determined by: Type and voltage of the circuit, the pathway through the body, the duration & the resistance of the body
– Least resistance - Nerve tissue; vascular, muscle, skin, fat, bone most resistance
– Entry wound – localized, deep, depressed, dry, charred
– Exit wound – may have multiple exit sites, injury resulting from an explosion
– Visible trauma contradicts underlying trauma
Page 1032010/08/30
Edmonton and Areawww.capitalhealth.ca
Chemical Burns
• Caused by acids and alkalis
• The concentration of the chemical agent and the length of exposure to it are the key factors that determine the extent and depth of damage
Page 1042010/08/30
Edmonton and Areawww.capitalhealth.ca
Inhalation Burns
• Composed of three distinct problems
1. Carbon monoxide intoxication
2. Upper airway obstruction
3. A chemical injury to the lower airway
Page 1052010/08/30
Edmonton and Areawww.capitalhealth.ca
Radiation
• Least common type of burn injury
• Caused by exposure to radioactive source
Page 1062010/08/30
Edmonton and Areawww.capitalhealth.ca
Depth of InjuryFirst Degree – Superficial
• Skin depth – epidermis
• Mechanism of injury – sunburn (UV light), flash flame
• Color/Pain – erythematous, pink, dry & tender no blisters, painful
• Healing time – 5-10 days with no residual scarring
Page 1072010/08/30
Edmonton and Areawww.capitalhealth.ca
Second Degree or Partial Thickness(Superficial & Deep)
• Skin depth – complete epidermis & partial dermis
• Mechanism of injury – hot liquids or solids, direct flame, chemicals, clothing flame, UV light
• Color – moist & blister to white & dry• Pain - very painful• Healing time – 5-21 days with no grafting,
longer if grafting required
Page 1082010/08/30
Edmonton and Areawww.capitalhealth.ca
Superficial Partial Thickness
• Epidermis and upper 1/3 dermis involved
• Dark pink/red, blistered, wet
• Severe pain (exposed nerves)
• Takes longer to heal: 7-14 days
Page 1092010/08/30
Edmonton and Areawww.capitalhealth.ca
Deep Partial Thickness
• Involves injury to deeper skin layers
• Burns are dry and white with red areas that don’t blanch, skin may appear spotted
• Sensation is decreased
• Infection is a concern
• Healing takes longer than 2 weeks, with scarring and possible need for debriding and grafting
Page 1102010/08/30
Edmonton and Areawww.capitalhealth.ca
Third Degree – Full Thickness
• Skin depth – epidermis & dermis
• Mechanism of injury – hot liquid or solids, flame, chemicals, electrical injury
• Color – eschar, charred vessels and dry
• Pain - limited/no pain
• Healing time – grafting required
• Usually have permanent impairments
Page 1112010/08/30
Edmonton and Areawww.capitalhealth.ca
Fourth Degree – Full Thickness Plus
• Skin depth – epidermis & dermis – complete - affects fat, bone fascia, muscle
• Mechanism of injury – hot liquids/solids, flame, chemicals, electrical injury
• Color– eschar, charred vessels and dry
- also affects fat, bone, fascia and muscle
• Pain - limited/no pain
• Healing time – reconstructive surgery usually indicated; severe disfigurement
Page 1122010/08/30
Edmonton and Areawww.capitalhealth.ca
Determining Extent of Injury
• Rule of nines – total body surface areas
• Pediatric assessment
• Estimation of burn size using palm
Page 1132010/08/30
Edmonton and Areawww.capitalhealth.ca
Adult Burns – The Rule of Nines
Page 1142010/08/30
Edmonton and Areawww.capitalhealth.ca
Pediatric Burns Lund & Browder Method
Page 1152010/08/30
Edmonton and Areawww.capitalhealth.ca
Triage Criteria for Burn Patients
• Minor burn injury: can be treated on outpatient basis
• Moderate uncomplicated burn injury: usually requires hospitalization in a institute with experience in burn care or specialized burn treatment facility
• Major burn injury: requires hospitalization in a specialized burn treatment facility
Page 1162010/08/30
Edmonton and Areawww.capitalhealth.ca
Age/Location/Comorbidities
• Children ages 2-4 and young adults ages 15 – 25 years old are the age groups with the greatest numbers of injuries from burns
• Elderly people experience high mortality and morbidity from burns
• Locations of highest risk are the face, neck, hands, feet and perineum
Page 1172010/08/30
Edmonton and Areawww.capitalhealth.ca
Systemic Response
1. Hypovolemia
2. Edema to non burned areas
3. Burn shock
4. Cardiovascular
5. Pulmonary
Page 1182010/08/30
Edmonton and Areawww.capitalhealth.ca
Systemic Response cont’d
6. Gastrointestinal
7. Renal
8. Cellular
9. Metabolic
10. Immunologic
Page 1192010/08/30
Edmonton and Areawww.capitalhealth.ca
3 Phases of Burn Care
1. Emergent/resuscitative phase
2. Acute phase
3. Rehabilitative phase
Page 1202010/08/30
Edmonton and Areawww.capitalhealth.ca
Priorities of Burn Management
• Wound care and closure• Pain management• Prevention or treatment of complications,
including infection• Nutritional support• Maintenance of respiratory and circulatory
status• Fluid and electrolyte balance• GI function
Page 1212010/08/30
Edmonton and Areawww.capitalhealth.ca
Goals of Wound Care
1. Prevent infection
2. Provide comfort
3. Debridement
4. Reduce scarring/contractures
Goal: To promote physical and psychological healing to the fullest extent possible
Page 1222010/08/30
Edmonton and Areawww.capitalhealth.ca
Burn Wound Healing
Burn wound healing occurs in primarily two forms:
- epithelialization
- contraction
Page 1232010/08/30
Edmonton and Areawww.capitalhealth.ca
Factors affecting wound healing
1. Age
2. Infection
3. Nutrition
4. Vitamins
Page 1242010/08/30
Edmonton and Areawww.capitalhealth.ca
Factors affecting wound healing cont’d
5. Trace elements
6. Oxygen
7. Diseases that impair healing
8. Medications
Page 1252010/08/30
Edmonton and Areawww.capitalhealth.ca
Topical Antibacterial Therapy
• Decrease the colonization of bacteria so control of the body’s host defense mechanisms can be maintained
• Promotes healing and closure of a clean wound bed
• Most common agents are polysporin, silver nitrate, ActicoatTM, and SulfamylonTM
Page 1262010/08/30
Edmonton and Areawww.capitalhealth.ca
Wound Dressing Product
• Adaptic
• Telfa
• Sofratulle
• Xeroform
Page 1272010/08/30
Edmonton and Areawww.capitalhealth.ca
Cleansing Solutions
• Clorhexidine (4%)
• Sterile normal saline
• Tap water
Page 1282010/08/30
Edmonton and Areawww.capitalhealth.ca
Special Care Areas
• Eyes– cleanse with NS– lacrilube ungt or tear drops
• Ears– prone to chondritis– sulfamylon ungt BID– avoid pressure
• Face– shave daily– polysporin ungt BID (wash between applications)– NS soaks continuous, change Q4H, rewet prn
• Fingers & toes– wrap separately to prevent webbing
Page 1292010/08/30
Edmonton and Areawww.capitalhealth.ca
Grafts(in order of preference)
• Homograft– allograft
• cadaver
• skin bank
• Xenograft– heterograft
• pig
• cow
Page 1302010/08/30
Edmonton and Areawww.capitalhealth.ca
Graft Care
• Apply appropriate dressing– AgNO3 to clean up graft
– PolysporinTM/AdapticTM to small open areas
• Once healed (red and itchy)– Apply lotion
• Donor Sites– Xeroform placed on in the OR
– Leave xeroform until it falls off (trimming the edges as it dries)
Page 1312010/08/30
Edmonton and Areawww.capitalhealth.ca
Common Problems/Complications
• Altered sensation
• Heterotropic ossification (HO)
• Scarring
• Pain
Page 1322010/08/30
Edmonton and Areawww.capitalhealth.ca
Altered Sensation
• Sensory nerves or sensory receptors in the injured skin may be affected, causing decreased sensation
• Includes – Itchiness
– Skin alterations –Blisters
– Thermoregulation
– Edema
Page 1332010/08/30
Edmonton and Areawww.capitalhealth.ca
Heterotrophic Ossification (HO)
• Accumulation of excess bone across joints
• Occurs in 13-23 % of clients with burns
• Most common in patients with greater than 20% full thickness burns
Page 1342010/08/30
Edmonton and Areawww.capitalhealth.ca
Types of Scars
• There are a number of different scars that can occur in the burn patient and that play an important role in the rehabilitation and treatment of the burned patient.– Normal scars
– Contractures
– Hypertropic scars
– Keloids
Page 1352010/08/30
Edmonton and Areawww.capitalhealth.ca
Factors Affecting Scar Formation
1. Race
2. Age
3. Location
4. Depth
5. Tension
6. Other
Page 1362010/08/30
Edmonton and Areawww.capitalhealth.ca
Pain Management
• Pain is more severe in partial thickness burns due to exposed nerve endings
• Full thickness burns – nerve endings are destroyed
• Pain in full thickness burns is associated with deep pain/pain in the surrounding areas
• Fear & anxiety can increase perception of pain
Page 1372010/08/30
Edmonton and Areawww.capitalhealth.ca
Two Types of Pain Commonto the Burn Client
1. Background pain• Associated with AADL and at rest
• Pain that never goes away
2. Associated pain• Associated with wound care, therapy and
treatments
Page 1382010/08/30
Edmonton and Areawww.capitalhealth.ca
Important nursing actions when caring for a patient with excessive burns
1. Monitor VS
2. Monitor intake and output
3. Assess for pain and administer pain medication as ordered, especially before dressing changes
4. Assess for distal neurovascular changes and monitor for development of limited movements and numbness of affected areas
Page 1392010/08/30
Edmonton and Areawww.capitalhealth.ca
Important nursing actions when caring for a patient with excessive burns
5. Provide dressing changes using sterile technique at least daily and more frequently for excessive drainage
6. Avoid chilling the patient
7. Monitor for development of complications, such as hydration, hypovolemia, infection, and renal failure
Page 1402010/08/30
Edmonton and Areawww.capitalhealth.ca
Nursing Interventions related to Impaired Skin Integrity
• Dryness
• Photosensitivity
• Pruritius
Page 1412010/08/30
Edmonton and Areawww.capitalhealth.ca
Nursing Interventions related to Impaired Physical Mobility
• Positioning
• Splinting
• Exercise
• Compression
Page 1422010/08/30
Edmonton and Areawww.capitalhealth.ca
Nursing Interventions related to Altered Health Maintenance
• Lifestyle
• Self care
Page 1432010/08/30
Edmonton and Areawww.capitalhealth.ca
Emotional Support
• The psychological implications for a client with burns
• Clients may exhibit a variety of responses depending on their phase of recovery
Page 1442010/08/30
Edmonton and Areawww.capitalhealth.ca
Expected Outcomes of Rehab
• Optimal function
• Endurance
• Self direction of care
• Comfort
• Psychosocial adjustment
• Social support
• Family coping, family functioning
• Coping, body image acceptance
Page 1452010/08/30
Edmonton and Areawww.capitalhealth.ca
Discharge Education
• Blister care – NEVER BREAK OPEN
• Exposure to temperature extremes
• Skin care
• Face care
Page 1462010/08/30
Edmonton and Areawww.capitalhealth.ca
Discharge education cont’d
• Pressure garments
• Itching
• Nutrition
• Exercise
Page 1472010/08/30
Edmonton and Areawww.capitalhealth.ca
Health Promotion/Prevention
• Education:– 80% of fires are due to carelessness
– 35% involve children playing with matches
– Smoke detectors are present in 13/14 homes (require regular battery checks/changes)
– Seasonal causes for burns
– Focus on high risk groups
Page 1482010/08/30
Edmonton and Areawww.capitalhealth.ca
Discharge
• Support services are necessary throughout Rehabilitation
• Education begins with onset of treatment• Earlier discharge means that education continues
post discharge• All team members provide to client/family at every
level of treatment• Community support groups assist with
resocialization & coping for years post-discharge• Complications can include PTSD/psychological
problems at any time
Page 1492010/08/30
Edmonton and Areawww.capitalhealth.ca
References
• Bickston, T.H. (2004). Medical-Surgical Nursing Recall. Lippincott Williams & Wilkins:Philadelphia
• Firefighter’s Burn Treatment Unit – University of Alberta, 2005
• Hoeman, S.P. (2002). Rehabilitation Nursing; Process, Application, & Outcomes, 3rd edition. Mosby:Toronto
• http://www.med.ualberta.ca/acicr/pages/ protocols/burns.htm
• Thelan, L., Davie, J., Urden, L., and Lough, M. (1994). Critical Care Nursing:Diagnosis and Management. Mosby:Toronto
Page 1502010/08/30
Edmonton and Areawww.capitalhealth.ca
Musculoskeletal Disorders in Rehabilitation Nursing
Presented by:
Chris Wright RN, BScN, CRRN
Evelyn Myles RN, BScN
Glenrose Rehabilitation Hospital