MRD backgrounder_3 pager 191115_A4
Transcript of MRD backgrounder_3 pager 191115_A4

The importance of minimal residual disease (MRD) in blood cancer
Key take-aways
Blood cancers: incurable diseases of the blood and bone marrow
Blood cancers are the fifth most common cause of cancer death worldwide and lymphoma, leukaemia and myeloma are the main types.1
Minimal residual disease (MRD) is a term used in blood cancer, meaning that small number of cancer cells remain in the patients’ blood or bone marrow following treatment. MRD is a major cause of relapse for patients with blood cancer.2
Assessing MRD is important as it allows physicians to assess the extent to which a treatment is working, whether a patient is likely to relapse or if they have achieved a deep remission.
MRD is also significant as it is a novel, innovative endpoint which promises to predict longer-term outcomes in people with blood cancers, such as overall survival.2
Blood cancer is an umbrella term for cancers that affect the blood, bone marrow and lymphatic system. Approximately one person is diagnosed with blood cancer every 35 seconds and one person dies of blood cancer every minute worldwide.1
There are three main categories of blood cancer, and some types are more common than others:
Blood cancer treatment and Minimal Residual Disease (MRD)By reducing the number of cancer cells in a patient’s blood, bone marrow or lymph nodes to the lowest attainable level, patients can live as normal a life as possible and without symptoms. This is called remission.6
Patients can appear to respond well to treatment, so achieving ‘complete remission’, meaning there is no evidence of cancer in the body using standard tests and the patient shows no signs or symptoms of disease. However, patients may be left with a tiny number of cancer cells within the blood or bone marrow which can regrow and after a few weeks or months, may cause them to relapse. This tiny population of remaining or residual cancerous cells in the body are termed ‘Minimal Residual Disease’ (MRD) and are a major cause of relapse in patients with CLL, MM and follicular lymphoma (FL, a subtype of NHL).2
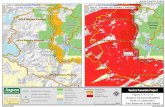
Bone marrow with cancerous
B-lymphocytes in an untreated CLL patient
Few cancer cells left in the bone marrow
(MRD) in a CLL patient
No cancer cells left in the bone marrow
(negative MRD)
Lymphoma – e.g. Non Hodgkin's lymphoma (NHL), which is the tenth most common cancer worldwide3
Leukaemia – e.g. Chronic lymphocytic leukaemia (CLL), which is the most prevalent type of leukaemia4
Myeloma – e.g. Multiple myeloma (MM), a less common type of blood cancer
While blood cancer can affect anyone at any stage of life, the risk of developing blood cancers such as NHL and CLL increases with age, meaning they predominantly affect the elderly.5,6
Although blood cancers can develop slowly and treatments can keep the disease under control for many years, many are incurable.7

An analogy of MRD testing: Leaves in a swimming pool9
How do we detect residual cancer cells?8
A minute proportion of cancerous cells still present in a patient can cause them to relapse in the future – so measuring MRD is crucial for physicians to assess how well a patient is responding to treatment.
Testing for these cancerous cells previously relied upon microscopes and small numbers of remaining cancer cells after treatment could not always be detected. In these patients, these cells were given the opportunity to regrow and so may have caused the patient to relapse.
Recent advances in scientific knowledge and medical technology have enabled us to detect these residual cells after treatment with greater accuracy. A patient is said to be ‘MRD-negative’ when even these highly sensitive tests are not able to detect remaining cancer cells.
This means they have achieved a ‘deep’ remission and are also more likely to sustain a longer-term disease control compared to patients with residual cancer (MRD) after treatment. Importantly, deep remissions are associated with prolonged progression free survival (PFS) and overall survival (OS).2
How are the cancer cells sampled for testing? Samples of blood or tissue from the bone marrow can be taken and the very low levels of residual cancer cells measured. Although a more invasive sampling method, MRD levels are usually higher in the bone marrow compared to blood, as the bone marrow is harder to clear of the cancer cells.
A standard bone marrow test is like taking a sample from a swimming pool. If leaves are found in the bucket, it suggests there are likely to be leaves floating elsewhere in the pool – or with blood cancer, a notable number of cancer cells remaining in the body.
MRD testing is like examining the sample of water in the bucket for tiny fragments of substances that exist only in leaves. These tiny fragments represent MRD, or the tiny number of blood cancer cells remaining in the body after treatment, which are only detectable with highly sensitive tests.
Thus, a negative finding with MRD testing provides much greater confidence that the blood or bone marrow is clear of the abnormal cells.
Using a microscope, it can be possible to find roughly
one harmful cell in 100 healthy cells, which is a very
high level of disease.
New technology is able to increase the level of detection to one in
10,000.8
Blood sample Bone marrow sample

Relapse
Critically, accurate detection of MRD enables physicians to:8
Reduce the risk of relapse, as the likelihood of relapse can be assessed and follow-up treatment given, as needed.
Identify patients who achieve a deep or MRD-negative remission and require no further treatment, so avoiding unnecessary side effects and time on treatment.
Indicate how effectively a treatment is working and predict whether continued treatment is likely to improve a patient’s longer term outcomes.
Roche is leading the way in novel clinical trial design, using MRD as both a primary and secondary endpoint to show superiority of one treatment over another. Importantly, the European Medicines Agency (EMA) has recently published guidelines on the use of MRD in clinical trials as an indicator of the likelihood of a patient achieving longer endpoints such as progression free survival (PFS) or overall survival (OS).2
Meanwhile, the U.S. Food and Drug Administration (FDA) is also considering MRD as a meaningful endpoint, using which the effectiveness of a treatment can be assessed earlier, helping to decrease lengthy development timelines and reduce delay in patient access to more effective treatment options.
1.
2.
3.
Dep
th o
f rem
issi
on
Why is testing for MRD in CLL, MM and FL important for patients in both the short- and long-term?
What is MRD?
People with blood cancer can respond to treatment to varying degrees, ranging
from no response, to some reduction in the level of disease, to achieving
“complete remission” and showing no signs of the disease.
MRD is a condition where a small, or minimal, number of cancer cells remain in the patients’ blood or bone marrow following treatment, and is the main
cause of relapse in blood cancer.
Achieving ‘MRD negativity’ means a patient is in a deep remission and has no
detectable cancer cells, even using modern, more sensitive tests.
Time
No relapse
Patient 1Non responder with disease progression
Patient 4Complete responder to treatment
Patient 5Complete responder with MRD negative disease
Patient 2Stable disease
Complete MRD
Patient 3Partial responder to treatment
Treatment
Key:

NP/GAZY/1511/0038a
References
1. Globocan (2012) Estimated incidence, mortality and 5-year prevalence: both sexes. Available at: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx (Last accessed November 2015).2. European Medicines Agency (2014) Guideline on the use of minimal residue disease as an endpoint in chronic lymphocytic leukaemia studies. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/12/WC500179047.pdf (Last accessed November 2015).3. Cancer Research UK. Non-Hodgkin lymphoma incidence statistics. Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/non-hodgkin-lymphoma/incidence# heading-Five (Last accessed November 2015).4. Byrd JC et al. Introduction to a series of reviews on chronic lymphocytic leukemia. Blood 2015: 126 (4); 427.5. Cancer.net. Leukemia - Chronic Lymphocytic - CLL: Risk Factors. Available at: http://www.cancer.net/cancer-types/leukemia-chronic-lymphocytic-cll/risk-factors (Last accessed November 2015).6. Cancer.net. Lymphoma - Non-Hodgkin: Risk Factors. Available at: http://www.cancer.net/cancer-types/lymphoma-non-hodgkin/risk-factors (Last accessed November 2015).7. Liu Q et al. Improvement of Overall and Failure-Free Survival in Stage IV Follicular Lymphoma: 25 Years of Treatment Experience at The University of Texas M.D. Anderson Cancer Center. J Clin Oncol 2006: 24 (10); 1582-9.8. Boldeanu F et al. Minimal Residual Disease - Generalities and Perspectives. TMJ 2011: 61; 3 – 4.9. Lymphomation.org. Minimum Residual Disease (MRD) with PCR ("molecular photocopying") of blood or marrow samples. Available at: http://www.lymphomation.org/MRD.htm (Last accessed November 2015).