Monocarboxylic Acid Transport - University of Bristol · the kidney and this requires their...
Transcript of Monocarboxylic Acid Transport - University of Bristol · the kidney and this requires their...

Monocarboxylic Acid TransportAndrew P. Halestrap*1
ABSTRACTMonocarboxylates such as lactate, pyruvate, and the ketone bodies play major roles inmetabolism and must be transported across both the plasma membrane and mitochondrial innermembrane. A family of five proton-linked MonoCarboxylate Transporters (MCTs) is involved inthe former and the mitochondrial pyruvate carrier (MPC) mediates the latter. In the intestine andkidney, two Sodium-coupled MonoCarboxylate Transporters (SMCTs) provide active transport ofmonocarboxylates across the apical membrane of the epithelial cells with MCTs on the basolat-eral membrane transporting the accumulated monocarboxylate into the blood. The kinetics andsubstrate and inhibitor specificities of MCTs, SMCTs, and the MPC have been well characterizedand the molecular identity of the MCTs and SMCTs defined unequivocally. The identity of theMPC is less certain. The MCTs have been extensively studied and the three-dimensional struc-ture of MCT1 has been modeled and a likely catalytic mechanism proposed. MCTs require thebinding of a single transmembrane glycoprotein (either embigin or basigin) for activity. Regula-tion of MCT activity involves both transcriptional and posttranscriptional mechanisms, examplesbeing upregulation of MCT1 by chronic exercise in red muscle (which oxidizes lactate) and inT-lymphocytes upon stimulation. MCT4 has properties that make it especially suited for lacticacid export by glycolytic cells and is upregulated by hypoxia. Some disease states are associatedwith modulation of plasma membrane and mitochondrial monocarboxylate transport and MCTsare promising drug targets for cancer chemotherapy. They may also be involved in drug uptakefrom the intestine and subsequent transport across the blood brain barrier. C© 2013 AmericanPhysiological Society. Compr Physiol 3:1611-1643, 2013.
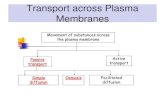
IntroductionMetabolism utilizes and produces many monocarboxylicacids, which are almost totally dissociated at physiologicalpH to their monocarboxylate anions. In quantitative terms byfar the most important are pyruvate and L-lactate that playkey roles in carbohydrate, fat, and amino acid metabolism(65). Other important monocarboxylates include the ketonebodies, acetoacetate, and β-hydroxybutyrate, the short chainfatty acids such as acetate, propionate, and butyrate, and arange of α-keto monocarboxylates produced by transamina-tion of amino acids such as phenylpyruvate (from phenylala-nine), α-ketoisocaproate (from leucine), α-ketoisovalerate(from valine) and α-keto-β-methylvalerate (from isoleucine)(122, 245). Metabolism of monocarboxylates often requirestheir entry into the mitochondria or across the plasma mem-brane. This is illustrated schematically in Figure 1, whileTable 1 shows the role of plasma membrane monocarboxy-late transport in some key tissues. Monocarboxylates mustalso be absorbed from the gut and the glomerular filtrate ofthe kidney and this requires their transport across the plasmamembrane of the relevant epithelial cells (90).
In the great majority of cases monocarboxylate trans-port across cellular membranes is a carrier-mediated process,although short chain fatty acids such as butyrate and acetatemay be exceptions. This is a consequence of their pKa val-ues being about 4.8 which provides sufficient of the lipid-soluble undissociated monocarboxylic acid at physiological
pH for appreciable rates of free diffusion across phospholipidsbilayers (245). However, even in the case of these mono-carboxylates solute carriers may significantly enhance theirrate of transport (196). For their metabolism, the majorityof monocarboxylate transport across the plasma membraneis mediated by proton-linked MonoCarboxylate Transporters(MCTs) which catalyze the net transport of a monocarboxy-late anion with a proton (112, 118, 245). This is appropriatesince it is usually the monocarboxylic acid that is the netproduct or substrate of a metabolic pathway (245). For mono-carboxylate uptake from the gut or kidney, Sodium-coupledMonocarboxylate Transporters (SMCTs) play an importantrole since the sodium gradient provides a driving force toenable uptake against a concentration gradient (90). Table 2presents the gene names and chromosomal locations of the dif-ferent MCT and SMCT isoforms as well any alternative namesand the sequence identifiers of the reference mRNA. Transportof pyruvate and other monocarboxylates into the mitochon-dria is mediated by a distinct proton-linked carrier knownas the Mitochondrial Pyruvate Carrier (MPC) (72, 118, 120).Between them MCTs, SMCTs, and the MPC can account for
*Correspondence to [email protected] School of Biochemistry and The Bristol Heart Institute, University ofBristol, Bristol, United KingdomPublished online, October 2013 (comprehensivephysiology.com)DOI: 10.1002/cphy.c130008Copyright C© American Physiological Society.
Volume 3, October 2013 1611

Monocarboxylic Acid Transport Comprehensive Physiology
Gluconeogenesis and amino acid metabolism
Glucose GlucoseLactate Alanine serine cysteine
Carbohydrate oxidation and lipogenesis
GlucoseGlucose Alanine serine cysteine
Mitochondrion
LactatePyruvate
Gluc-6-PGluc-6-P
Pyruvate Pyruvate
Oxaloacetate
Phosphoenol-
Acetyl-CoAMalate
Pyruvate
Fatty acyl-CoA
KeyMitochondrial pyruvate
AcAc+βHB Citrate pyruvateCO2
carrier (MPC)
Other mitochondrial metabolite carriers
Plasma membrane mono-ran rter
AcAc+βHB
OxaloacetateCitrate
Acetyl-CoA
Fatty acyl-CoA
Fatty acids Triglycerides
carboxylate tespot
Other plasma membrane transporters
AcAc Acetoacetate
Cytosol
AcAc+ββHB Fatty acids body metabolismFatty acid and ketone
βHB β-hydroxybutyrate
Figure 1 Key metabolic pathways requiring monocarboxylate transport across the plasma and inner mitochon-drial membranes. Note that the particular metabolic pathways operating within any cell will depend on the tissue.This Figure does not include monocarboxylate absorption from the lumen of the intestine or reabsorption from thekidney which are illustrated in Figure 10.
the transport of all the major monocarboxylic acids acrosscellular membrane membranes, but it remains possible thatthere are orphan members of other transporter families yet tobe identified that can also transport monocarboxylates.
Techniques for MeasuringMonocarboxylate TransportMeasuring monocarboxylate transport into cells and mito-chondria presents some major challenges that are not alwaysappreciated. These relate to the rapid rates of transport, theconcurrent carrier-independent rates of transport mediatedby free diffusion of the undissociated monocarboxylic acid,and the metabolism of the substrate. These have been wellreviewed elsewhere (245) but will be summarized brieflybelow.
Use of radiolabeled substratesThe most common method for measuring monocarboxylatetransport involves the use of radiolabeled substrates whereuptake into cells or vesicles is rapidly terminated at discretetime points by centrifugation or by vacuum filtration with or
without prior addition of inhibitor (inhibitor stop). Determi-nation of intracellular labeled substrate requires correctionfor extracellular contamination. Although this can be doneby washing rapidly with ice-cold buffer in the presence oftransport inhibitors, loss of accumulated substrate by diffu-sion, or metabolism during the washing procedure may betoo rapid to avoid substantial errors. Rather, it is preferable tocorrect for extracellular contamination by using membrane-impermeable markers such as [14C] or [3H] sucrose or inulin(245). Another major problem with the use of radioactivemonocarboxylates is their rapid metabolism which results inthe majority of the radiolabel accumulated within the cellbeing distributed within a large pool of intracellular metabo-lites. When analyzed carefully, it is found that in most cellstransport is extremely fast but is followed by a slower accu-mulation of the label that corresponds to this metabolism.This is often mistakenly analyzed as the rate of transport.There are no entirely satisfactory inhibitors of metabolismthat do not interfere in some way with the measurement oftransport, and the most reliable way to avoid the problemis to ensure initial rates of transport are measured by usinglow temperatures and short times of uptake (10 s to 1 min).These considerations impose major constraints on the typesof kinetic experiment that can be performed using radioactivemonocarboxylates.
1612 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
Table 1 The expression of plasma membrane monocarboxylate transporters in different tissues and their normal physiological roles. Manytissues express more than one transporter and these may be in different locations in the tissues or differ between the basolateral and apical surfacesof polarized epithelial cells. There are also significant species differences in which MCT isoforms are expressed in each tissue, especially for MCT2.These points are discussed more fully the text. Note that all cells become glycolytic under hypoxic/anoxic conditions and export lactic acid.
TissueMajor monocarboxylatetransporters expressed Major roles of plasma membrane monocarboxylic acid transport
Liver MCT1, MCT2, MCT7 Entry of lactic acid for gluconeogenesis and lipogenesis. Export ofketone bodies
Heart MCT1 Entry of lactic acid and ketone bodies for oxidation as respiratory fuels
Red skeletal muscle MCT1 Entry of lactic acid and ketone bodies for oxidation as respiratory fuels
White skeletal muscle MCT4 Export of lactic acid produced by glycolysis
Kidney cortex MCT1, MCT2 Lactic acid uptake for gluconeogenesis
Kidney tubule epithelialcells
SMCT1, SMCT2, MCT1, MCT2 Reabsorption of lactate, pyruvate, and ketone bodies
Intestinal epithelial cells SMCT1, SMCT2, MCT1, MCT2 Absorption of lactate, pyruvate, and ketone bodies
Adipose tissue MCT1 Efflux of lactic acid produced by glycolysis
Blood brain barrier MCT1 Transport of lactic acid and ketone bodies into the brain centralnervous system
Neurons MCT1, MCT2 Uptake of lactic acid and ketone bodies as respiratory fuels
Glial cells and astrocytes MCT1, MCT4 Efflux of lactic acid produced by glycolysis for subsequent use as arespiratory fuel by neurons
Retina MCT1, MCT3, MCT4 Rapid export of lactic acid produced by glycolysis is important tomaintain osmotic balance in the retina
Insulin-secreting β cells No MCTs expressed All glycolytic pyruvate is oxidized and uptake of pyruvate from theblood is prevented avoiding inappropriate insulin secretion duringexercise
Red blood cells MCT1 Efflux of lactic acid produced by glycolysis
T-lymphocytes MCT1 Efflux of lactic acid produced by glycolysis by glycolysis especiallyduring activation and proliferation
Tumor cells MCT1, MCT4 Efflux of lactic acid produced by glycolysis in most tumor cells althoughsome on the periphery of a solid tumor oxidize lactic acid
Testis MCT1, MCT2, MCT4 Essential for spermatogenesis. Spermatid cells oxidize lactic acidproduced by Sertoli cells
Sperm MCT2, MCT4 Energy metabolism of sperm is mainly glycolytic
Table 2 Members of the SLC16A family that act as proton-linked monocarboxylate transporters (MCTs)
Protein name Human gene name Aliases Human gene locus mRNA reference sequence ID
MCT1 SLC16A1 MOT1 1p12 NM_003051
MCT2 SLC16A7 MOT2 12q13 NM_004731
MCT3 SLC16A8 MOT3 REMP 22q112.3-q13.2 NM_013356
MCT4 SLC16A3 MOT4 MCT3 17q25.3 NM_004207
MCT7 SLC16A6 MOT7 MCT6 17q24.2 NM_004694
SMCT1 SLC5A8 AIT 12q23.1 NM_145913
SMCT2 SLC5A12 — 11p14.2 NM_178498
Volume 3, October 2013 1613

Monocarboxylic Acid Transport Comprehensive Physiology
Real-time measurement of transportFortunately, for MCTs many of these constraints can be over-come by measuring the associated proton transport. This hasthe added advantage of allowing transport to be monitoredin real time by following changes in either the intracellularor extracellular pH using either intracellular or extracellularpH electrodes (37,168,181,265,276) or the intracellular pH-sensitive fluorescent dyes such as 2′-7′-bis-(carboxyethyl)-5-6-carboxy-fluorescein (BCECF) (43,176,291,303,305,310).The same approach can be used for measuring monocar-boxylate transport into isolated mitochondria but because ofthe small matrix volume of mitochondria the pH changesare smaller and more difficult to determine with accuracy(108,133). For sodium-linked transport of monocarboxylatesvia SMCTs transport can be monitored in real time usingelectrophysiological techniques since in this case monocar-boxylate uptake involves the translocation of a net positivecharge across the membrane that is detected as a flow of cur-rent (90, 277).
Other techniquesA promising new technique for measuring monocarboxylatetransport into tissues is nuclear magnetic resonance spec-troscopy coupled with the use of hyperpolarized [13C]-labeledsubstrates (125). However, this highly sophisticated techniqueis unlikely to become available to most laboratories.
Correcting uptake rates for transport mediatedby free diffusionWhen rates of transport are determined by using isotopicallylabeled substrates or pH measurements, it is essential thatcorrection is made for carrier-independent transport of theundissociated monocarboxylic acid which can diffuse throughthe lipid phase of biological membranes (304). This is espe-cially true for short chain monocarboxylates such as acetateand butyrate with high pKa values, but becomes increas-ingly important for all monocarboxylates at lower pH andhigher concentrations since the rate of diffusion is linearlyrelated to the concentration of undissociated acid (245). Dif-fusion rates are best determined following the addition of highconcentrations of a potent inhibitor of the transporter suchas α-cyano-4-hydroxycinnamate (CHC) for the MPC andp-chloromercuribenzenesulfonate (pCMBS) for MCTs. ForSMCTs, the difference between the rate of transport observedin the presence and absence of Na+ can be used to assesscarrier-mediated transport (90, 245).
The Proton-linked MonocarboxylateTransporter FamilyHistorical perspectiveFor many years, transport of acetate, L-lactate and pyruvateacross the plasma membrane was thought to occur solelyby diffusion of the undissociated monocarboxylic acids, but
the demonstration in 1974 that proton-linked transport ofL-lactate and pyruvate into human red blood cells couldbe specifically inhibited by CHC revealed that a specifictransporter was involved (110, 116). Subsequently, the sub-strate and inhibitor specificity and detailed kinetics of thistransporter were extensively characterized by the laborato-ries of both Halestrap and Deuticke (see 67, 245). Studies ofthe kinetics and substrate and inhibitor specificity of mono-carboxylate transport into hepatocytes (76) and heart cells(241, 248) suggested that there might be several MCT iso-forms which was later confirmed as outlined below. Themolecular identity of the MCT present in erythrocytes wasfirst established in Halestrap’s laboratory by specific labelingof the protein with its inhibitor 4,4′-di-isothiocyanostilbene-2,2′-disulfonate (DIDS) (244) followed by purification andN-terminal sequencing (246). Parallel studies in the labo-ratory of Goldstein and Brown led to the sequencing of acDNA encoding for a protein predicted to contain 12 trans-membrane helices (TMs), a characteristic of members of theMajor Facilitator Superfamily (MFS) of solute transporters(157). Although the function of the wild-type transporter wasnot identified at this stage, it was established that a phenylala-nine to cysteine mutation in the protein enhanced uptake ofmevalonate, a monocarboxylate required for cholesterol syn-thesis, into Chinese Hamster Ovary cells. These authors wenton to demonstrate that the protein was widely expressed inthe plasma membrane of mammalian tissues and that heterol-ogous expression of the wild-type protein in a human cancercell line that lacked the endogenous protein facilitated theiruptake of L-lactate and pyruvate (159). They named the pro-tein MCT1. The N-terminal sequence of the MCT purifiedfrom rabbit erythrocytes by Poole and Halestrap (246) con-firmed that it was the same protein as the MCT1 identified inGoldstein and Brown’s laboratory. The prediction that theremight be a family of MCTs was confirmed first by Garcia etal. (91) who demonstrated the presence of a novel MCT iso-form, named MCT2, in tissues such as liver and kidney thatexpressed little MCT1, and then by Price et al. who revealedthe existence of another six proteins with shared sequencemotifs which they named MCTs3-8 (250).
Defining features of MCT family membersWith the complete sequencing of the mouse and humangenome it is now known that in mammals there are 14 relatedtransporters with shared sequence motifs which constitutea family of proteins known as the SoLute Carrier family16 (SLC16) or MCT family (118). Related proteins can befound in all eukaryotic organisms whose genomes have beensequenced, including Caenorhabditis elegans and Saccha-romyces cerevisiae (119). The MCT (SLC16) family is amember of the MFS according to the transporter classifica-tion system of Milton Saier (see http://www.tcdb.org/) and isalso known as the MonoCarboxylate Porter family (2.A.1.13)(114). Family members are defined by the presence of twohighly conserved sequences—[D/E]G[G/S][W/F][G/A]W
1614 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
C
RPR
RD
K
Highly conserved motifs
characteristic of the MCT family
K in TM1 and R and D in TM8 are involved in proton
and monocarboxylatebinding during the translocation cycle
N
Extracellular
Intracellular
Figure 2 Conserved sequence motifs that define membership of the SLCA16 (MCT)family. Family members are defined by the presence of two highly conserved sequences,[D/E]G[G/S][W/F][G/A]W and YFxK[R/K][R/L]xLAx[G/A]xAxAG, which traverse the leadinto TM1 and TM5 respectively as well as a conserved R and RP in the lead in to TMs 3and 6. Sequence variation between different SLC16A family members is greatest in loopsbetween helices and in the N- and C-termini; the TM segments are more conserved.Members of the family known to transport monocarboxylates all contain a lysine (K) onthe cytosolic side of TM1 and an aspartate (D but glutamate in MCT7) and arginine (R) inthe centre of TM 8. These groups are believed to play a critical role in binding the protonand monocarboxylate anion during the translocation cycle.
and YFxK[R/K][R/L]xLAx[G/A]xAxAG which traverse thelead into TM1 and TM5 respectively (119). As illustratedin Figure 2, they are predicted to contain 12 transmembranehelices with intracellular C- and N-termini and a large cytoso-lic loop between TM6 and TM7. This prediction is supportedby the pattern of chemical labeling and protease digestion ofendogenous MCT1 in rat erythrocytes (249). The TM regions
are better conserved than the loops and C-terminus which isa characteristic of other MFS members (118). The mobilityof the MCTs on SDS-PAGE together with theoretical pre-dictions suggest that family members are not glycosylated(119) and for MCT1 this has been confirmed experimentally(247, 249). The phylogenetic relationship of members of themammalian SLC16 (MCT) family is presented in Figure 3
Aromatic aminoacid transporter
Thyroid hormonetransporter
OrphanOrphan
SLC16A14/MCT14
SLC16A2/MCT8
SLC16A11/MCT11
Carnitinetransporter
Orphan
SLC16A9/MCT9SLC16A13/MCT13
Orphan Ketone bodytransporter
SLC16A6/MCT7SLC16A4/MCT5
OrphanOrphan
SLC16A5/MCT6SLC16A12/MCT12
0.1SLC16A1/MCT1
SLC16A7/MCT2SLC16A8/MCT3
SLC16A3/MCT4
Confirmed proton-linked monocarboxylate transporters
SLC16A10/TAT1
Figure 3 Phylogenetic tree of members of the SLC16A family. Both the SLC and MCT nomenclatureare given. Only four members are confirmed as proton-linked monocarboxylate transporters withSCL16A6 (MCT7) the only other member likely to be so. Seven members of the family are currentlyof unknown function (orphan transporters).
Volume 3, October 2013 1615

Monocarboxylic Acid Transport Comprehensive Physiology
which illustrates the unfortunate mismatch between the MCTand SLC16 nomenclature. This arose primarily because theMCTs were named in order of their characterization at thefunctional level, while the SLC16 numbers were generatedas the cDNA sequences became available (118). A correc-tion was also made when it was recognized that the MCTidentified in white skeletal muscle and named MCT3 (310)was subsequently renamed as MCT4 when it was recognizedto be a different but closely related isoform to the MCT3identified in retinal pigment epithelium (RPE) (119, 231).This also required renumbering of the MCTs original namedMCT4, MCT5, and MCT6 (250) to MCT5, MCT6 andMCT7 (119).
Only four members of the human MCT family havebeen shown unequivocally to transport monocarboxylates;these are SLC16A1 (MCT1), SLC16A3 (MCT4), SLC16A7(MCT2), and SLC16A8 (MCT3) (112, 114, 118) althoughmore recent data have implicated SLC16A6 (MCT7) inthe transport of ketone bodies such as β-hydroxybutyrateacross the liver plasma membrane in Zebra fish (137). Othermembers of the SLC16 family whose transport propertieshave been well characterized are SLC16A2 (MCT8), whichis a high affinity thyroid hormone transporter (84), andSLC16A10 (TAT1 or MCT10) which is an aromatic aminoacid transporter (158). The properties and roles of these trans-porters are reviewed elsewhere (301). SLC16A5 (MCT6)has been reported to facilitate the proton-linked transport ofbumetanide, but its natural substrate remains unknown (197).MCT9 (SLC16A9) was suggested to be a carnitine trans-porter on the basis of changes in serum carnitine levels asso-ciated with a genetic polymorphism and subsequent expres-sion in Xenopus oocytes confirmed this (280a). The other 5members of the SLC16 human family are currently referredto as “orphan” transporters because their substrates remainunknown. Table 1 summarizes the major tissue distributionand metabolic functions of the MCTs known to transportmonocarboxylates (MCTs1-4).
General features of monocarboxylate transportby MCT family membersExtensive studies were performed on the kinetics of monocar-boxylate transport into human and rat erythrocytes (67-69,75,110,168) and Ehrlich-Lettre tumor cells (15,43,149,276,291)which are now known to express only MCT1 (246,310). Thesedata provided evidence for the likely mechanism of MCT1 thatis assumed to be shared by MCT2, MCT3, and MCT4. MCT1facilitates net cotransport of a monocarboxylate anion with asingle proton or exchange of an intracellular monocarboxy-late with an extracellular monocarboxylate; monocarboxy-late exchange was found to be significantly faster than nextproton-linked transport (43, 67, 245, 276). A more detailedkinetic analysis of L-lactate uptake into erythrocytes revealedthat transport follows an ordered mechanism (62,63) as illus-trated in Figure 4. A proton binds to the carrier first with a
Extracellular Intracellular
C
CH+
H+
H+
H+
CH+
Lac– Lac–
Lac–
Lac–H+
Lac–
Lac–
CH+
CH+
Ck2
k1
k1 > k2
X
Net reaction
Figure 4 MCTs follow an ordered kinetic mechanism. Transport isshow for the lactate anion moving with a proton from the extracellu-lar to the intracellular compartment, but all steps are freely reversible.The conformational change of the protein that translocates the lac-tate and proton occurs faster for the substrate bound carrier (k1) thanthe unbound carrier (k2) which accounts for why monocarboxylateexchange is faster than net movement of monocarboxylic acid.
Km of 0.2 μmol/L (equivalent to a pKa of 6.7 for the accept-ing group) followed by the monocarboxylate anion. There isthen a conformational change that translocates the monocar-boxylate and proton across the membrane, followed by theirrelease, monocarboxylate first and then the proton. The ratelimiting step is the return of the MCT to the original conforma-tion, which explains why the transporter mediates monocar-boxylate exchange faster than net transport. MCTs catalyzefacilitated diffusion of the monocarboxylic acid rather than“active transport” since there is no energy input other thanthat provided by the concentration gradients of the mono-carboxylate and proton across the membrane. However, thisdoes mean that a proton gradient can drive the uptake ofthe monocarboxylate anion. MCT1 operates equally wellin either direction with the relationship between the influxand efflux kinetics being defined by the Haldane equation{(Vmax/Km)influx = (Vmax/Km)efflux} (119, 305). The net rateof transport of any monocarboxylate will be determined bythe difference between the rates of influx and efflux and atthermodynamic equilibrium the concentration ratio of mono-carboxylate inside the cell to outside the cell is equal to theratio of [H+]out to [H+]in (245). Transport can be stimulatedby decreasing the pH from 8 to 6 on the cis-side, primar-ily through a decrease in the Km for the monocarboxylate,or by raising the pH on the opposite side of the membranevia an increase in the Vmax of transport by stimulating therate which the unloaded carrier reorientates in the membrane(67, 245).
1616 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
BCECF-AM
BCECF
LactateLactate
H+ H+
pHi
Oocytes loadedwith AM ester of
BCECF
Monocarboxylatetransport measured as
a decrease in pHi
BCECF-AM
MCT cRNA
MCT cRNA
MCT protein
MicroinjectXenopus oocyteswith mRNA
Translation to MCT protein
Translocation to membrane
Immunofluorescence microscopyconfirms expression of MCT at plasma membrane
Express MCT in oocytes ofXenopus laevis by microinjectionof cRNA
(A)
(B)
(C) Measure transport activity with [14C] substrate of by measuring changesin intracellular pH with a fluorescentpH indicator BCECF
10 min
2.5 mmol/L 5 mmol/L 7.5 mmol/L 10 mmol/L 15 mmol/L 20 mmol/L
[L-lactate]
ΔF 440/4900.1
Figure 5 Characterization of the properties of MCTs by expression in Xenopus laevis oocytes.
Determining substrate and inhibitor specificitiesof individual MCT isoformsTo characterize the other MCT isoforms it was necessaryto find a suitable expression system that lacks significantendogenous MCT activity. Although some mammalian celllines such as MIN6 and Ins-1 have very low endogenousMCT activity (324), the most amenable system proved to bethe Xenopus laevis oocyte which possesses almost no endoge-nous MCT activity. cRNA for the required MCT isoform ismicroinjected into the oocytes and then transport measured2 to 3 days later using radiolabeled substrates or changesin intracellular pH monitored with intracellular electrodes orBCECF. This expression system is illustrated in Figure 5, andhas been used successfully to characterize MCT1 (36, 37),MCT2 (35) and MCT4 (71,176) but not MCT3. For the latteronly a very limited characterization has been reported usinga yeast expression system (101). Table 3 and Table 4 summa-rize the substrate and inhibitor specificities of MCTs 1 to 4,respectively, which are described briefly below.
MCT1MCT1 is expressed in most tissues and is the best character-ized MCT isoform.
Substrate specificity
MCT1 exhibits a broad specificity for short chain monocar-boxylates including those substituted on the 2- (α-) and 3-(β-)positions with small groups such as halides, hydroxyland carbonyl groups. Major naturally occurring substratesinclude L-lactate, pyruvate, D-β-hydroxybutyrate, acetoac-etate, acetate, and butyrate, although the latter two can betransported at relatively fast rates by free diffusion of theundissociated monocarboxylic acid (37, 43, 67, 245). Km val-ues for the major physiological substrates together with therange of concentrations found in vivo are summarized inTable 3. Because of its major role in metabolism, L-lactate isquantitatively by far the most important substrate for MCT1and the transporter is stereoselective for L-lactate over D-lactate. However, for β-hydroxybutyrate, whose D-isomeris the normal metabolite, MCT1 shows no sterospecificity.The ketoacids derived by transamination of the branchedchain amino acids (α-ketoisocaproate, α-ketoisovalerate, andα-keto-β-methylvalerate) and phenylalanine (phenylpyru-vate) may be also be transported by MCT1 but their hydropho-bic side-chains leads to a very slow release of the boundmonocarboxylate following translocation across the mem-brane, and thus net transport rates are also slow (43). Indeed,these ketoacids act as potent competitive inhibitors of the
Volume 3, October 2013 1617

Monocarboxylic Acid Transport Comprehensive Physiology
Table 3 The affinity of MCT family members for monocarboxylates of physiological importance. Km values (mmol/L) are shown for MCT1(37), MCT2 (35), and MCT4 (71, 176) expressed in Xenopus laevis oocytes except for those in parentheses which are derived from endogenousMCT1 present in a mouse cancer cell line (43) or, for propionate and acetate, erythrocytes (241). For MCT3 the only published Km value is forL-lactate (6 mmol/L) and this was obtained following MCT3 expression in Yeast (101). Where available, plasma concentrations (mmol/L) of themonocarboxylates in normal human subjects are from (114). Km values for nonphysiological monocarboxylates can be found in (112, 245).Where data are not available this is indicated by NA.
Monocarboxylate MCT1 MCT2 MCT4 Plasma concentration
Acetate (3.73)[3.5] NA NA 0.030
Propionate [1.5] NA NA NA
L-lactate 3.5 (4.5) 0.74 28 1.51
D-lactate (27.5) NA 519 NA
Pyruvate 1.0 (0.7) 0.08 153 0.064
D-β-hydroxybutyrate (10.1) 1.2∗ 130 0.060
γ-hydroxybutyrate (7.7) NA >500# NA
Acetoacetate (5.5) 0.8 216 0.041
α-Ketobutyrate (0.2) NA 57 NA
α-ketoisocaproate† 0.7 0.1 95 NA
α-ketoisovalerate† 1.3 0.3 113 NA
∗D,L racemic mix used in these studies.#Uptake too low to measure accurately.†These substrates are transported slowly and acted better as inhibitors.
transport of L-lactate and pyruvate which may play a role inthe pathology of Maple Syrup Urine Disease and Phenylke-tonuria (43, 115).
Inhibitors
A number of nonphysiological competitive inhibitors ofMCT1 have been described including analogues of CHCthat played a major role in the discovery of the MCTs(110, 116, 245). CHC has a Ki value of 250 to 500 μmol/Lunder physiological conditions (43,276) and it has been usedto study the role of MCT1 in metabolism by some workers.However, it is important to recognize that CHC cannot beused in this way because it also inhibits the MPC and does sowith a potency at least 2 orders of magnitude greater than itinhibits MCT1 (108,116). Stilbene disulfonates such as DIDSand 4, 4′-dibenzamidostilbene-2, 2′-disulfonate (DBDS) alsoinhibit MCT1 with Ki values of 2-500 μmol/L with greaterinhibition being observed for the more hydrophobic stil-bene disulfonates such as DBDS (43, 242, 243). Even themost potent of these inhibitors, N,N,N′,N′-tetrabenzyl-4,4′-diaminostilbene-2,2′-disulfonate (K0.5 2.5 μmol/L) showeda much lower affinity for MCT1 than for the chloride/bicarbonate exchanger AE1 (also known as Band 3) (242,243)making them also unsuitable for specific inhibition of MCT1.Inhibition of MCT1 by stilbene disulfonates is usuallyreversible, but in rat erythrocytes DIDS was shown to producea rapid reversible inhibition of transport followed by a slowerirreversible phase caused by one of the two isothiocyano groupcovalently modifying a lysine on MCT1 (243, 244, 313). It
should be noted that the Ki values for CHC and stilbenedisulfonate analogs are highly dependent on the pH gradi-ent across the plasma membrane and much lower values areobtained when the cytosolic pH is higher than the extra-cellular pH (43). Other nonspecific, reversible inhibitors ofMCT1 include phloretin (43, 306) and bioflavenoids such asquercetin (15) while irreversible inhibition can be induced byN-hydroxysulfosuccinimides (74), organomercurial reagentssuch as mersalyl and pCMBS (69, 276) and isobutylcarbonyllactayl anhydride (73, 149).
More recently a new class of highly specific MCT1inhibitors have been developed by AstraZeneca that exhibitvery high affinity (Ki values in the nmol/L range) (104, 200).Measurements of L-lactate transport into Xenopus laevisoocytes confirmed that these inhibitors (exemplified by AR-C155858) exhibit a low nmol/L Ki value against MCT1 butare inactive against MCT4 (212). The use of chimeric trans-porters that contained combinations of domains derived fromMCT1 and MCT4 revealed that the AR-C155858 bindingsite is contained within the C-terminal half of MCT1 andinvolves TM domains 7 to 10 (213). Subsequent studiesrevealed that AR-C155858 can also inhibit MCT2 but onlywhen it is associated with the ancillary protein basigin and notwhen associated with embigin (see under ancillary proteinsbelow). By contrast, MCT1 is inhibited equally well by AR-C155858 whether associated with basigin or embigin (213).The potent inhibition of MCT1 by AR-C155858 was con-firmed for endogenous MCT1 in rat erythrocytes where it waspossible to determine both an accurate Ki value (2 nmol/L) andthe number of molecules of MCT1 per erythrocyte (80,000).
1618 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
Table 4 Inhibitor sensitivity of the major MCT isoforms. Data are presented as K0.5 values under conditions approximating to physiological, butthe values given can only be indicative since the measured K0.5 can depend on many factors including substrate concentration, pH gradient acrossthe plasma membrane and the ancillary protein with which the MCT is associated. Unless otherwise stated (a reference in parentheses) the datapresented for MCT1 are for the endogenous protein present in a mouse breast tumor cell line (43) and for MCT2 (35) and MCT4 (176) expressedin Xenopus oocytes. For MCT2, some agents were tested at only a single concentration (0.1 mmol/L) and data are presented as percentageinhibition. Note that inhibition will also be caused by competing monocarboxylates with Ki values the same as their Km values for transport as asubstrate. ND—not determined. NI—no inhibition.
Inhibitor MCT1 MCT2 MCT4
α-cyanocinnamate analogs
α-cyanocinnamate 1.7 mmol/L ND ND
α-cyano-4-hydroxycinnamate 166 μmol/L 24 μmol/L 990 μmol/L
α-fluorocinnamate 724 μmol/L ND ND
Phenylcinnamate 61 μmol/L ND ND
UK5099 8.1 μmol/L ND ND
Stilbene disulphonates
DIDS 434 μmol/L ND NI
SITS 1.18 mmol/L ND ND
DBDS 215 μmol/L 44% ND
DNDS > 5 mmol/L NI ND
TBenzDS 6.7 μmol/L ND ND
NBDS 397 μmol/L ND ND
AstraZeneca inhibitors
AR-C155858 2 nmol/L (212) <10 nmol/L∗ (213) > 10 μmol/L
AR-C117977 2 nmol/L (200) 21 nmol/L (200) > 1 μmol/L (200)
Other inhibitors
Phloretin 5.1 μmol/L 14 μmol/L 41 μmol/L
Quercetin 2 μmol/L (245) 5 μmol/L ND
5-nitro-2-(3-phenylpropyl-amino)benzoate 9.3 μmol/L 25% 240 μmol/L
Niflumic acid 6.1 μmol/L 14% ND
3-isobutyl-1-methylxanthine 288 μmol/L ND 970 μmol/L
Mersalyl† 50 μmol/L ND ND
p-mercuribenzene sulfonate† μmol/L NA 21 μmol/L
∗Inhibition of MCT2 by AR-C155858 is only observed when MCT1 is associated with basigin and not embigin (212,213).†Inhibition by organomercurials is only observed when MCT1 associates with basigin and not embigin (311).
From the latter value, the turnover number (kcat) of MCT1 at6◦C was calculated to be 12/s (212) and using the activationenergy of MCT1 determined in tumor cells (43) enabled thevalue at 37◦C to be estimated as about 400/s. The time depen-dence of MCT1 inhibition in oocytes following extracellularapplication or intracellular injection of AR-C155858 suggeststhat it binds to MCT1 from the cytosolic side (212).
MCT2When Garcia et al. discovered hamster MCT2 they showedby immunofluorescence microscopy that it was expressed inliver, kidney, brain, sperm tails, skeletal muscle, and heartof the hamster (91). However, unlike MCT1, MCT3, and
MCT4, there appears to be a considerable species differ-ences in the tissue expression profile of MCT2 and this isassociated with much less conservation of the sequence ofMCT2 across species than the other isoforms (145,174). BothNorthern blot analysis and inspection of the human ExpressedSequence Tags (EST) database suggests relatively low expres-sion levels of MCT2 in human tissues with the exception oftestis (174, 250). However, in mouse and rat, Northern andWestern blot analysis show the protein to be expressed inliver, kidney, brain, and testis, but not in heart or skeletal mus-cle (145). Hamster MCT2 was first functionally expressed ininsect Sf9 cells and reported to transport lactate and pyru-vate with a higher affinity than MCT1 (91). This was subse-quently confirmed when rat MCT2 was expressed in Xenopus
Volume 3, October 2013 1619

Monocarboxylic Acid Transport Comprehensive Physiology
laevis oocytes and characterized more fully (35, 174). MCT2exhibits a substrate specificity that is similar to MCT1 butwith a 5- to 10-fold higher affinity for most substrates. Thus,Km values (mmol/L) for pyruvate, L-lactate, acetoacetate, andD,L-β-hydroxybutryate and are about 0.1, 0.74, 0.8, and 1.2,respectively, compared to values of about 1, 3.5, 5.5, and12.5 for MCT1. MCT2 is also more sensitive than MCT1 toinhibition by a range of inhibitors including CHC, DBDS, andDIDS. It was reported to be insensitive to the organomercurialreagent pCMBS (35, 91) but this was subsequently shown tobe because pCMBS inhibits MCT1 by binding to its ancillaryprotein, basigin (see below) whereas MCT2 usually associateswith embigin which is insensitive to pCMBS (311).
MCT3 and MCT4Philp and colleagues originally identified MCT3 as a devel-opmentally expressed protein in the chick RPE (229) andsubsequently identified it as a member of the MCT familywhich they named MCT3 (319). It was functionally expressedin Saccharomyces cerevisiae (yeast) and shown to transportL-lactate with a Km of about 6 mM but to be insensitive toCHC, phloretin and pCMBS (101). No detailed characteriza-tion of MCT3 expressed in Xenopus laevis oocytes has beenreported but its high sequence identity with MCT4 suggeststhat it is likely to exhibit similar properties. Indeed MCT4 wasoriginally thought to be the mammalian homologue of chickMCT3 (310) until a distinct mammalian MCT3 was found tobe expressed in the human and mouse RPE (232, 318).
MCT4 was identified during a search of the EST databasefor novel members of the MCT family (250). Northernand Western blotting as well as EST database analysisshowed MCT4 to be quite widely expressed but espe-cially so in tissues that rely on glycolysis for their energymetabolism such as white skeletal muscle fibres, astrocytes,white blood cells, chondrocytes, and some mammalian celllines (71, 154, 191, 250, 310). In the rat, MCT4 is expressedin the neonatal heart, which is more glycolytic in its energymetabolism than the adult heart where MCT4 is absent butMCT1 abundant (128, 310). When expressed in Xenopuslaevis oocytes MCT4 exhibits a much lower affinity for mostsubstrates and inhibitors than MCT1, with Km and Ki valuessome 5- to 10-fold higher (71, 176). Thus Km values for L-lactate and D-β-hydroxybutyrate were measured as 28 and130 mmol/L, respectively, but, in marked contrast to MCT1and MCT2, the affinity for keto acids is considerably lowerthan the corresponding hydroxy acids with values for pyru-vate and acetoacetate of about 150 and 210 mmol/L respec-tively (176). Ki values for DIDS, CHC, and phloretin arealso much higher with little inhibition observed at concentra-tions giving >50% inhibition of MCT1 (71,176). By contrast,the organomercurial reagent pCMBS is at least as potent aninhibitor of MCT4 as MCT1, most probably because it doesnot interact directly with MCT but inhibits by binding to theancillary protein, basigin, that is common to both isoforms(311).
N
ss
Two or threeextracellular
immunoglobulindomains
depending onsplice variant
Multipleglycosylation
sitesss
MembraneTransmembraneand intracellular
domains essentialfor interaction with
MCT1Conserved glutamateresidue in TM helix
CFigure 6 Schematic diagram showing key structural features of basi-gin and embigin which are essential ancillary proteins for MCT activity.
MCTs require the ancillary proteins embigin orbasigin for correct membrane expressionAs noted above, inhibition of MCT1 in rat erythrocytes byDIDS exhibits a slower phase of irreversible inhibition thatis caused by one of the two isothiocyano group covalentlymodifying a lysine on MCT1 (243, 244, 313). Western blot-ting with antibodies against MCT1 revealed that this irre-versible inhibition is accompanied by the formation of a formof MCT that runs at about 120 kDa on SDS-PAGE, higherthan either monomeric or dimeric MCT1 that run at 45 and90 kDa, respectively. This larger MCT1 band was shownto be a cross-linked product formed by the second isothio-cyano group of DIDS cross-linking MCT1 to another proteinof about 70 kDa. This was subsequently identified as embi-gen which is also known as gp-70 (247). Embigin is notexpressed in many tissues but a closely related protein calledbasigin (also known as CD147, OX-47, EMMPRIN, or HT7)is widely expressed. As illustrated in Figure 6, both basiginand embigin have a single transmembrane domain (TMD)containing a conserved glutamate residue, a short intracellu-lar C-terminus, and a large glycosylated extracellular domainwith two or three immunoglobulin domains depending on thesplice variant (103, 141, 198, 201).
MCT1 and MCT4 were shown by immunofluorescencemicroscopy to colocalize with basigin in a variety of differ-ent cells and tissues (66, 160, 230, 324) as illustrated for thecardiac myocyte and islet of Langerhan in Figure 7. Further-more, when a cross-linking antibody against basigin was usedto aggregate basigin into a cap at one end of a cell, MCT1 wasfound to move with the basigin implying that the two proteinsbind strongly to each other (160). This was confirmed by theircoimmunoprecipitation from solubilized plasma membranes(160). In addition, when attempts were made to overexpressMCT1 or MCT4 in a variety of cell lines both proteins were
1620 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
BasiginMCT1 Overlay
Rat islet oflangerhan
β cells
50 μm
50 μm
Exocrinecells
Rat cardiacmyocyte
Figure 7 Basigin colocalizes with MCT1 in the heart and Islets of Langherhan.Data were obtained using confocal microscopy as described references 160 and 324,respectively.
retained in the Golgi apparatus/endoplasmic reticulum andfailed to reach the plasma membrane. However, both MCT1and MCT4 were correctly targeted to the plasma membranewhen coexpressed with basigin, suggesting that basigin actsas an essential chaperone for both MCTs (160). When suchexpression studies were performed using constructs of MCT1and basigin tagged with either the cyan or yellow variantsof green fluorescent protein (CFP and YFP) at the C- orN-terminus, fluorescence resonance energy transfer (FRET)between the CFP and YFP was observed, confirming thatthe two proteins are <100 Å apart (312). FRET was alsodemonstrated between basigin tagged with CFP on its C-terminus with basigin tagged with YFP on its C-terminus.Taken together with the antibody capping studies, these datasuggest that MCT1 is likely to exist as an MCT1-basigindimer. Through the use of CD2/basigin chimeras, the bindingof basigin to MCT1 was shown to involve its TM domainand/or intracellular tail rather than the extracellular domain(160). Subsequent experiments using site-directed mutagene-sis and molecular modeling suggested that the TM domain ofbasigin lies adjacent to TMs 3 and 6 of MCT (178,311,313).
Although basigin is the preferred binding partner forMCT1, in its absence MCT1 can express with embigin as itdoes in rat red blood cells (213, 247). Basigin is also the pre-ferred binding partner for MCT4, whereas embigin is stronglypreferred by MCT2 which is not well expressed with basigin(213,311). Indeed, when the C-terminus of MCT2 is removed,basigin is unable to support any MCT2 expression which nowbecomes totally dependent on the presence of embigin (213).By contrast, the C-terminus of MCT1 has no effect on itsinteraction with either embigin or basigin. Taken together,these data demonstrate that, although the choice of ancillaryprotein is not absolute, MCT1 and MCT4 prefer basigin andMCT2, embigin.
Basigin and embigin may influence the propertiesand membrane targeting of MCTs
Characterization of lactate transport in rat and rabbit ery-throcytes suggests that the choice of ancillary protein doesnot influence the kinetic properties of MCT1 (213). How-ever, the ancillary protein can influence the sensitivity ofMCTs to inhibitors. Thus, inhibition of MCT1 activity bypCMBS occurs when MCT1 is expressed with basigin butnot with embigin. This was shown to be because organomer-curial reagents attack a labile disulfide bridge in the distalimmunoglobulin fold of basigin that is unreactive in embi-gin (213, 311). The choice of ancillary protein has also beenshown to influence the sensitivity of MCT2 to inhibition byAR-C155858 which was greatly reduced when MCT2 wasexpressed with embigin rather than basigin. This is not thecase for MCT1 where the choice of ancillary protein is with-out effect (213). Studies using MCT1 and MCT2 with theirC-terminal tails removed as well as those using MCT1/MCT2chimeric transporters suggested that the modulation of MCT2sensitivity to AR-C155858 by embigin involves interactionswith both the intracellular C-terminus and TMs 3 and 6 ofMCT2 (213).
An additional role that the ancillary protein can play is intargeting MCT expression to different cell surfaces in polar-ized cells. In the case of MCT1, basigin targets the transporterto the basolateral membrane of most polarized cells, includ-ing epithelial cells in the kidney, liver, gut, and thyroid, buta single L252A mutation of basigin redirects MCT1 to theapical surface (66). However, in the RPE, basigin-mediatedtargeting of MCT1 is ignored and MCT1 is expressed withbasigin at the apical membrane. MCT3 and MCT4 possessdominant sorting signals in their C-terminal cytoplasmic tailsthat ensure their basolateral expression independently of basi-gin (44).
Volume 3, October 2013 1621

Monocarboxylic Acid Transport Comprehensive Physiology
Outside openInside open
152
4
8
63
9
7
10
11
12
3
1 524
8
6
9
7
1011
12
1 524
8
63
9
7
10
11
12
Z
Y
X
20°
–20°
Z
Y
X
K38
–3 angstrom in Y–4 angstrom in Z
K38
F360F360
K45K45 K282K282 K413
K413
20°–20°
Straightenhelix 11
Figure 8 The structure of MCT1 derived from molecular modeling is shown in the two conformations representingthe two forms, “inside open” and “outside open,” with substrate binding sites on opposite sides of the membrane. TheN-terminal domain is colored red and the C-terminal domain colored blue, while the intracellular loop connectingthe two is not modeled and shown as a connecting line. Cross-sections of the transporter are rendered with a solvent-accessible surface. The position of K38 (green) and F360 (yellow) are shown as these are critical residues for thetranslocation cycle and substrate specificity, respectively. D302 and R306, which are also essential for activity, are notshown for clarity, but line the channel next to F360. Lysine residues (K45, K282, and K413) involved in DIDS bindingare rendered magenta. The axis system used for the C-terminal domain rotations to generate the open model isshown in the centre of the figure. The schematic diagram below the model structures illustrates how individual helicesare proposed to move during the transformation between inward and outward facing conformations of MCT1. TheFigure is based on the structure reported in Ref. 313.
The Structure and Molecular Mechanismof MCTsAlthough no three-dimensional crystal structure of any mem-ber of the MCT family has been reported, other members ofthe MFS have now been crystallized and structures obtainedin a variety of conformations (1, 60, 136, 203, 281, 317). Inagreement with topology predictions they all share a similaroverall structure with intracellular C- and N-termini and 12transmembrane helices organized into two distinct N- and C-domains, each containing 6 TM helices that are connectedby a large intracellular loop between TM helices 6 and 7.Extensive site-directed mutagenesis combined with molecu-lar modeling has allowed prediction of the likely structure
of MCT1 in both the “inside-open” conformation (with sub-strate binding site facing the cytosol) and an “outside-open”conformation with DIDS bound to the extracellular substratebinding site (178, 313). These are illustrated in Figure 8. Ini-tially, the “inside-open” conformation was modeled based onan alignment of the predicted TM sequences with those ofthe Escherichia Coli glycerol phosphate transporter whosestructure (1PW4) has been solved (136). This modeled struc-ture was found to be consistent with results of extensivesite-directed mutagenesis studies of MCT1 that had identi-fied residues essential for expression of active MCT1 in theplasma membrane (87, 178, 258, 313).
1622 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
K38
K306 D302
+
K38
K306 D302 –
–
–
–
–
– –+
K38
K306 D302
+
L K38
K306 DH302
+
L
L Lactate
LactateH+
+
+
+ L
Substratebinding
Domainrearrangement
Substraterelease
H+
Figure 9 Cartoon illustrating the proposed mechanism of lactic acid transport by MCT1. Lactic acidprotonates K38 causing the channel to open. Lactate then moves into the open extracellular side of thepore and forms an ion pair with K38. In the next step, the proton on K38 is transferred to aspartate302 (D-) neutralizing the aspatate side chain (DH). This is followed by migration of lactate through thepore where it forms an ion pair with R306 (R+). Once K38 is deprotonated and lactate is occupyingthe specificity filter, the transporter relaxes back toward the closed state and releases lactic acid intothe intracellular space. The cartoon is based on the mechanism reported in Ref. 313.
Subsequent studies employed site-directed mutagenesis toidentify four extracellular lysines residues (K38, K45, K282,and K413) that are involved in the binding of DIDS. Usinga combination of feasible domain translocations and helixrotations, combined with energy minimizations and liganddocking software a second structure was predicted repre-senting MCT1 with DIDS bound in an “outside-open” con-formation (313). Similar domain rearrangements were pre-dicted for the E. Coli Lac-Permease during its catalytic cycle(1, 102, 273, 325) and are entirely consistent with a subse-quently published crystal structures of the E. Coli fucosetransporter (FucP2) in an “outside-open” conformation (60)and the E. Coli xylose transporter in a ligand-bound, outward-facing, partly occluded conformation (281). The two mod-eled structures suggest a likely translocation cycle, illustratedin Figure 9, that can account for the critical roles of keyresidues identified by site-directed mutagenesis (313). In theproposed “outside-open” conformation of MCT1, a lysineresidue (K38) identified as being essential for MCT1 activ-ity is located in a hydrophobic pocket at the bottom of asubstrate-binding channel. Even conservative changes of thislysine to arginine or glutamine cause MCT1 to be inactivedespite being properly expressed at the plasma membrane(313). The hydrophobic environment will favor this lysineremaining uncharged (i.e., unprotonated) but upon accept-ing a proton it will provide a binding site for the monocar-boxylate anion. It is proposed that MCT1 then undergoesa domain rearrangement, as originally suggested by Broerand colleagues (87), involving a modest reorganization of theinterface between the 6-helix N-terminal domain and the sim-ilar 6-helix C-terminal domain that are linked by a 30 residueloop of unknown structure (313). Similar domain rearrange-ments have been proposed for the catalytic cycle of the E. ColiLac-Permease (272). During the domain rearrangement, thelactate and proton are proposed to pass through the channelto an intracellular substrate binding site involving aspartate
and arginine residues (D302/R306). These are known to beessential for activity from site-directed mutagenesis and arethought to form an ion pair in the channel (87, 178). As themonocarboxylate and proton bound to K38 are transferred toD302/R306, the MCT1 will relax back to the “inside-open”state with the deprotonation of K38 and exposure of the D302and R306 to the intracellular medium. The monocarboxy-late and proton can then be released and the transport cyclerepeated.
Interestingly the three critical residues (K38, D302, andR306) required for the proposed translocation cycle are alsopresent in MCT2, MCT3, and MCT4. However, they arenot conserved in either SLC16A2 (MCT8) or SLC16A10(MCT10), neither of which mediates proton-linked transport.Nor are all three present in any of the orphan members of theSLC16 family except SLC16A6 (MCT7) where there is a con-servative substitution of D302 by a glutamate. These consid-erations lead to the conclusion that MCT7 is the only orphanmember of the MCT family that is likely to be a true proton-linked MCT. Consistent with this, it has recently been reportedthat zebra fish with a mutation in SLC16A6 exhibit hepaticsteatosis that is associated with accumulation of ketone bodiesin the liver. These data suggested that MCT7 may transportketone bodies such as β-hydroxybutyrate out of the liver andexpression of the protein in Xenopus laevis oocytes confirmedthis transport activity. The presence of MCT7 in the oocyteplasma membrane enabled a β-hydroxybutyrate induced cur-rent across the membrane to be detected that was absent inuninjected eggs (137). Although this might seem to imply anelectrogenic rather than protogenic transport of the monocar-boxylate into the oocyte, this may not be the case since thecharge transfer was small and not dissimilar to that observedfor transport mediated by MCT1 expressed in oocytes (37).
The molecular model and proposed translocation cycledescribed above can explain other published data on thestructure and function of MCTs. For example, mutation of
Volume 3, October 2013 1623

Monocarboxylic Acid Transport Comprehensive Physiology
phenylalanine 360 to cysteine enables MCT1 to transportmevalonate, a larger monocarboxylate which is not a sub-strate for wild-type MCT1 (157, 159). In the modeled struc-tures of MCT1, Y306 is close to the D302/R306 ion pair in thesubstrate binding channel and thus the smaller side chain ofcysteine compared with phenylalanine will allow the internalcavity of the channel to accommodate a larger monocarboxy-late (313). The model also predicts that residues in both halvesof MCT1 play essential roles involved in the translocationcycle; K38 (TM1) is in the N-terminal domain while D302and R306 (TM8) and F360 (TM10) are in the C-terminaldomain. Determination of the Km values and inhibitor sensi-tivity of transporter chimaeras in which the C- and N-terminaldomains of MCT1, MCT2, and MCT4 are interchanged haveconfirmed this and suggest that the TM domains, and espe-cially TM7-TM12, are the major determinants of L-lactateaffinity while the C-terminus and intracellular loop betweenTMs 6 and 7 have little influence (212, 213).
Sodium-Coupled MonocarboxylateTransportersHistorical perspectiveIt has been known from many years that epithelia of thekidney and endothelium possess sodium-linked transportsystems for the active absorption of nutrients and reab-sorption of valuable metabolites including monocarboxylates(199, 314). Thus in brush-border membrane vesicles fromkidney transport of L-lactate and pyruvate was found to bestimulated in the presence of an inwardly directed sodiumgradient leading to their accumulation (8,150,188,190,204).Transport was also shown to exhibit strict specificity for Na+
over other cations with an Na+ to lactate stoichiometry of 1(11) or 2 (8, 150, 188, 190). Transport of lactate into intesti-nal brush-border membrane vesicles was also found to besodium-dependent and electroneutral implying a 1:1 sodiumlactate stoichiometry (132,278). In kidney brush-border mem-brane vesicles, Km values for L-lactate were found to be inthe range 0.5 to 4.3 mmol/L (9, 189, 190, 205) with a Km forNa+ of about 50 mmol/L (189, 190). Kinetic data obtainedusing brush-border membrane vesicles supported an orderedbinding process, with Na+ binding and being released beforethe lactate (189). The substrate specificity was found to besimilar to that of the erythrocyte proton-linked transporter(MCT1) with all the important monocarboxylate metabo-lites such a pyruvate, β-hydroxybutyrate, and acetoacetatebeing transported but with little stereoselectivity for D- overL-lactate (8-10, 150, 151, 204, 294, 294). Similar data wereobtained using intestinal brush-border membrane vesicles(132). Like MCT1, the sodium-linked transport was foundto be inhibited by the thiol reagent mercuric acetate (151)and by a number of aromatic and heterocyclic monocarboxy-lates, although in kidney vesicles α-cyanocinnamate deriva-tives were found to be much less effective (Ki = 10 mmol/L)than for MCT1 (270, 295). However, greater sensitivity to
mercurials was reported in intestinal vesicles (278). Conflict-ing results were reported for 4-acetamido-4′-isothiocyanato-stilbene-2,2′-disulfonic acid (SITS) and phloretin (10, 294).One explanation for these data might be the presence of dif-ferent isoforms of a sodium-linked MCT and kinetic evidencefor the presence of distinct sodium-linked monocarboxylatecarriers with different affinities for lactate has been reportedfor the pars convoluta and pars recta of the rabbit kidneyproximal tubule (150, 151). Pyruvate was also found to bea substrate for the Na+-dependent system that transports di-and tricarboxylic acids (151, 187, 204).
Identification of SLC5A8 and SLC5A12as SMCTsThe molecular identity of the first SMCT (SMCT1) wasrevealed when a tumor suppressor found in the human colonwas identified as a member of the SLC5 sodium-coupledtransporter gene family (SLC5A8) (171). When expressedin Xenopus laevis oocytes SLC5A8 was shown to transportmonocarboxylates in a sodium dependent manner (53, 194).Members of the SLC5 family are predicted to have 14 trans-membrane helices with extracellular N- and C-termini (315).A second member of the SLC5 gene family (SCL5A12) waslater shown to act as a lower affinity SMCT and called SMCT2(277). The tissue expression of SMCT1 and SMCT2 is consis-tent with their predicted role in the active absorption and reab-sorption of monocarboxylates from the lumen of the kidneytubules and intestine. Thus both are present in the apical mem-brane of epithelial cells lining the intestinal tract and proximaltubule (96,98,143,284,316). SMCT1 is also expressed in thebrain and retina where it has been suggested to mediate highaffinity uptake of lactate and ketone bodies to act as fuels forthe neuron in much the same manner as has been suggestedfor MCT2 (179, 180).
Functional characterization of SMCT1and SMCT2The properties of SMCT1 and SMCT2 were characterized byexpressing them in Xenopus laevis oocytes (53,96,194,224).Both proteins were confirmed to catalyze the sodium-coupledtransport of monocarboxylates with SMCT1 having a K0.5 forNa+ of about 30 mmol/L and exhibiting slight cooperativ-ity (Hill Coefficient ∼ 1.7). Transport is electrogenic with aNa+: monocarboxylate stoichiometry of 2 to 3. By contrast,SMCT2 was reported to be electroneutral suggesting a stoi-chiometry of 1:1, but the affinity for [Na+] and cooperativitywere found to be similar to SMCT1 (K0.5 ∼ 30 mmol/L; Hillcoefficient 1.4) (98,277). This may account for the discrepan-cies in stoichiometry reported for sodium coupled monocar-boxylate transport into kidney brush border membrane vesi-cles described above. SMCT1 can transport a broad range ofaliphatic monocarboxylates as summarized in Table 5. Theseinclude short chain fatty acids such as acetate, propionate,and butyrate (Km values of about 2.5, 0.12, and 0.08 mmol/L,
1624 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
Table 5 The substrate specificity of SMCT1. Km values are takenfrom (90) which cites the original sources, and where more than onevalue is available the mean value is presented.
Monocarboxylate Km
Acetate 2.46 mmol/L
Propionate 130 μmol/L
Butyrate 77 μmol/L
L-lactate 190 μmol/L
D-lactate 910 μmol/L
Pyruvate 390 μmol/L
Nicotinate 310 μmol/L
Acetoacetate 210 μmol/L
β-D-hydroxybutyrate 1.44 mmol/L
β-L-hydroxybutyrate 2.33 mmol/L
γ-hydroxybutyrate 1.62 mmol/L
α-ketoisocaproate 210 μmol/L
Benzoate 1.1 mmol/L
Salicylate 1.5 mmol/L
5-aminosalicylate 6.5 mmol/L
respectively), metabolically important ketoacids includingpyruvate, acetoacetate, and α-ketoisocaproate (Km valuesof about 0.39, 0.21, and 0.21 mmol/L, respectively) andhydroxyl acids such as L-lactate, β-D-hydroxybutyrate, andγ-hydroxybutyrate (Km values of about 0.19, 1.4, and 1.6mmol/L, respectively). There is some stereospecificity for L-over D-lactate but little for D- over L- β-hydroxybutyrate asshown in Table 5. Aromatic monocarboxylates such as ben-zoate and salicylate are also substrates for SMCT1 as is nicoti-nate (Km values of about 1.1, 1.5, and 0.3 mmol/L, respec-tively). Inhibitor studies of SMCT1 expressed in oocytes haveconfirmed the expected competitive inhibition between differ-ent monocarboxylates and allowed a range of other inhibitorsto be identified. With 0.1 mmol/L propionate as substrateprobenecid and ibrobrufen at 1 mmol/L gave 75% and 95%inhibition, respectively, 0.1 mmol/L XHX and phloretin gaveabout 25% inhibition while neither 0.5 mmol/L SITS nor 0.1mmol/L phlorizin were inhibitory (53).
SMCT2 has been less extensively studied than SMCT1,but comparison of the ability of monocarboxylates to inhibitnicotinate uptake into Xenopus laevis oocytes suggested thatits affinity is an order of magnitude lower than SMCT1 withKm values determined for butyrate, nicotinate and L-lactateof 2.6, 3.7, and 16.9 mmol/L, respectively (277).
Tissue distribution of SMCT1 and SMCT2Unlike the members of the MCT family, SMCT1 and SMCT2are not widely expressed and are primarily found in the api-cal membrane of epithelial cells lining the intestinal tract and
proximal tubule, although they are also found in the thyroid,brain, and retina (90). In the intestine, SMCT1 is predomi-nantly expressed in the large bowel and terminal ileum whileSMCT2 is strongly expressed in the jejunum with little or noexpression in the duodenum, terminal ileum, or large intes-tine (298). This distribution is consistent with their proposedrole in the absorption of short-chain fatty acids from the gut.Uptake will be initiated in the ileum with the lower affinitytransporter (SMCT2) while the presence of the higher affin-ity transporter (SMCT1) in the colon will ensure completeabsorption and also allow the uptake of butyrate, acetate, andformate produced by the intestinal microflora into the colono-cytes where they act as essential energy substrates. In the kid-ney, the major role of the SMCTs is thought to be reabsorptionof lactate and pyruvate and mice deficient in either SMCT1alone (83) or both SMCT1 and SMCT2 (285) show greatlyelevated lactate concentrations in the urine. The expressionof SMCT2 is evident throughout the whole length of theproximal tubule (S1/S2/S3 segments) whereas the expressionof SMCT1 is mostly restricted to the straight portions ofthe proximal tubule (S3 segment) (98, 267). This distributionimplies that the lower affinity transporter, SMCT2, initiatesmonocarboxylate absorption in the early parts of the prox-imal tubule whereas the higher affinity transporter SMCT1operates in the latter parts of the proximal tubule where mono-carboxylate concentrations will be lower. This confirms ear-lier data suggesting the presence of an SMCT with a loweraffinity for lactate and pyruvate in the pars convoluta (S1/S2)than the pars recta (S2/S3) of the proximal tubule (150, 151).In the brain, expression of SMCT1 is restricted to neuronswhere, in conjunction with MCT2, it may be involved in theactive uptake of lactate and ketone bodies to be used as res-piratory fuels (90, 180), while the lower affinity SMCT2 isfound in astrocytes (179). Similarly, in the retina SMCT1 isexpressed primarily in the neurons but also on the basalateralsurface of the RPE while SMCT2 expression is restricted tothe Muller cells which are the glial cells of the retina (179).
Physiological Roles ofMonocarboxylate TransportersThe primary metabolic role of MCTs 1 to 4 is the transport ofL-lactate, pyruvate, and ketone bodies (D-β-hydroxybutyrateand acetoacetate) produced or utilized in metabolism acrossthe plasma membrane of cells with L-lactate being quantita-tively the most important. It is actually the monocarboxylicacid that is metabolized, and thus the proton-linked monocar-boxylate transport facilitated by the MCTs is ideally suited totheir metabolic roles. All MCT isoforms can facilitate boththe influx and the efflux of monocarboxylates, with the netdirection of transport depending on the concentration gra-dients of protons and mononocarboxylate across the plasmamembrane. By contrast, the primary role of the SMCTs isthe active absorption of or reabsorption of monocarboxylatesfrom the lumen of the intestine and kidney tubule driven by the
Volume 3, October 2013 1625

Monocarboxylic Acid Transport Comprehensive Physiology
sodium gradient across the plasma membrane. These differentroles will be considered in turn.
Lactic acid efflux from cellsLactic acid is the product of anaerobic glycolysis and in mostcells and tissues this only occurs at appreciable rates whenoxygen supply is compromised and glycolysis stimulated.MCT1 is usually responsible for efflux of this lactic acid.However, some cells, including red blood cells, lymphocytes,astrocytes, tumor cells, and white muscle fibers rely on glycol-ysis for their energy supply even when oxygen is present (aer-obic glycolysis). Consequently, they routinely produce largeamounts of lactic acid that must be exported from the cell(118, 122, 192). Of these “specialist” glycolytic cells, quan-titatively the most important lactic acid producers are whiteskeletal muscle fibers that rely on glycolysis for their ATPproduction. Such fibers predominate in muscles responsiblefor short-term, high-intensity exercise (26,122,152,154) andexpress large amounts of MCT4 (28, 310). As noted above,characterization of the properties of MCT4 in Xenopus laevisoocytes (71, 191) revealed it to possess a very high Km forpyruvate (@150 mmol/L compared to 1 mmol/L for MCT1)effectively preventing it from transporting pyruvate out of thecell. This makes good physiological sense since glycolysisrequires lactate dehydrogenase (LDH)-meditated conversionof pyruvate to L-lactate to regenerate cytosolic NADH fromNAD+, and so it is important that pyruvate is not lost from thecell. If it were, glycolysis would stall and the muscle wouldbecome energetically compromised (118,122). Another char-acteristic of MCT4 is its high Km for L-lactate (@20 mmol/L)which might not be expected for an MCT isoform that isinvolved with exporting lactic acid from muscle. However,this high Km does provide an explanation as to why prolongedhigh intensity exercise leads to muscle fatigue since restrict-ing the rate of lactic acid export leads to its accumulationwith a consequent drop in intracellular pH, inhibiting glycol-ysis and ATP production (154). The resulting fatigue limitsfurther exercise and so prevents excessive lactic acid accumu-lation in the blood that might otherwise lead to a dangerousdrop in blood pH (26, 122, 152, 154).
Tumor cells also exhibit very high rates of lactic acidefflux since they are highly dependent on glycolysis fortheir ATP synthesis (the Warburg effect). Some tumor cellsuse MCT1 for this purpose, whilst others, especially moreinvasive tumors have upregulated MCT4 activity probablyinduced by overexpression of hypoxia inducible factor 1 α
(HIF-1α) (49,70,223). Lactic acid efflux is also important dur-ing the activation and proliferation of resting T-lymphocytes,which is accompanied by a switch from aerobic to gly-colytic metabolism and a massive increase in lactate pro-duction (16, 100, 105). Efflux of this lactic acid is medi-ated primarily by MCT1 whose specific inhibition with thepotent AstraZeneca inhibitors such as AR-C155858 block T-lymphocyte proliferation and act as potent immunosuppres-sant drugs (77, 104, 200, 214).
Lactic acid uptake into cellsSome tissues can be net users of lactic acid; for example,it is a good substrate for gluconeogenesis in the liver andthe kidney proximal convoluted tubules, and for lipogenesisin adipose tissue and liver (65, 122). These tissues expresseither or both MCT1 and MCT2 depending on the species(119, 145, 227, 250). MCT2 exhibits a lower Km for L-lactatethan MCT1 (35) and thus is relatively more active at lowerblood lactate concentrations. However, any advantage thismay provide is unlikely to be of great significance since the tis-sue expression of MCT2 is highly species dependent and canbe very low compared with expression of MCT1 in the sametissue (119,145,174,250). Lactic acid is also a very importantrespiratory substrate for heart and red skeletal muscle whereuptake is mediated primarily by MCT1 (26,121,154). Indeed,in skeletal muscle there is a strong correlation between theamount of MCT1 expressed in muscle fibers and their oxida-tive capacity (mitochondrial content) (310). MCT1 also facili-tates the transport of lactate across the blood brain barrier to beoxidized by neurons for which it can act as an important respi-ratory fuel (20,169). Transport of the lactate into the neuronsthemselves is mediated by either MCT1 or MCT2 dependingon the species (20,92,122,234). In both muscle and the brain,there is cooperation between MCT isoforms involved in lacticacid efflux and influx by different cell types within the sametissue, and this will be discussed further below.
Ketone body metabolismThe ketone bodies, acetoacetate and D-β-hydroxybutyrate areproduced by the liver under conditions of high fatty acidoxidation such as during endurance exercise and starvationand are then taken up by tissues such as heart, red skeletalmuscle, and brain and used as efficient respiratory substrates(262,298). Export of the ketone bodies from the liver involvesMCTs (144) and is thought to be mediated by either MCT1or MCT2 depending on the species (91, 145, 174), althoughrecent data suggests that MCT7 may also play an importantrole (137).
Monocarboxylate absorption in the intestineand kidneyShort-chain fatty acids such as acetate, propionate, andbutyrate are produced in large amounts by bacterialfermentation in the intestine where they may play an impor-tant role in maintaining the homeostasis of the gut epithe-lium (59, 271). The presence of MCT1 in the gut epithelium(59, 94, 159, 210, 260, 267, 283, 308) is consistent with theirplaying a key role in short chain fatty acid uptake. Net absorp-tion of these and other monocarboxylates such as lactate fromthe lumen of the gut to the blood requires their transportacross both the apical and basolateral plasma membrane ofthe epithelial cells. As shown in Figure 10, this is thoughtto involve MCT1 at the basolateral membrane operating inconjunction with SMCT1 or SMCT2 (SLC5A8 or SLC5A12)
1626 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
LumenMonocarboxylate
Apical
SMCT
Monocarboxylate
Na+
Na+
Na+H+
K+ H+
BasolateralMCT
Monocarboxylate
Blood
Figure 10 Monocarboxylate uptake from the intestinal and kidneytubules involves cooperation of SMCTs and MCTs on the apical andbasolateral surfaces of epithelial cells. Note that as shown the processwould cause the pH of the cell to rise as protons are move with themonocarboxylate across the basolateral membrane and this must becompensated for by pH regulatory mechanisms.
at the apical membrane (90,143). Consistent with this, MCT1is strongly expressed on the basolateral surface of gut epithe-lial cells in the stomach and intestine (91) whereas membersof the SMCT family are expressed primarily on the apicalsurface (143). Clearly, this proposal requires an additional pHregulatory mechanism to compensate for the proton that is
transported out of the cell with the monocarboxylate usingMCT1 but is not taken up with the monocarboxylate via theSMCT. A similar situation is found in the kidney where MCT1is strongly expressed on the basolateral surface of epithelialcells in the proximal tubules of kidney with MCT2 beingrestricted to the collecting ducts, while the SMCT SLC5A8is expressed at the apical membrane (91, 316). Here it wouldseem likely that the two carriers cooperate in the reabsorptionof monocarboxylates such as lactate and the ketone bodiesfrom the glomerular filtrate, although the relative distributionof the MCTs and SMCT is not the same in different regionsof the kidney tubule suggesting a more complex picture(316).
In addition to their role in the mediating uptake of mono-carboxylate metabolites from the gut and kidney, MCT1 andSMCT1 may also be important in facilitating the absorptionof various drugs such as salicylate, valproic acid, nateglin-ide, atorvastatin, gamma-hydroxybutyrate and nicotinic acid,and also transporting them across the blood brain barrier(90, 97, 122). This is discussed in more detail elsewhere(4, 192, 299).
MCTs are involved in shuttling lactate betweencell types within a tissueThere is increasing evidence that within a tissue lactic acidproduced by glycolysis in one cell type can be exported foruse in other cells as a respiratory fuel (20, 38). The best doc-umented examples of such “lactate shuttles” are in brain andskeletal muscle which are illustrated in Figure 11.
Skeletal muscle
Skeletal muscles generally contain a mixture primarily gly-colytic (white) fibers and primarily oxidative (red) fibers with
Blood
NeuronsRed muscle fibres
Glucose Glucose Glucose
Oxidation
ATP
PyruvateLactic acid
Interstitial fluid
Endothelium
MCT1
MCT1
Astrocytes
White muscle fibres
Glucose
Lactic acid Lactic acid
Pyruvate
MCT1/2MCT4
Ketonebodies
MCT1/2Ketonebodies
Lactic acid
Ketonebodies
Lactic acid
Lactic acid
Figure 11 In the brain and muscle MCTs are used to transport lactic and ketonebodies from the blood into the tissue as to shuttle lactic acid between the glycolyticastrocytes and white muscle fibers to the neurons and red fibers that oxidize it. A similarlactic acid shuttle may operate in some tumors where the hypoxic centre of the tumorproduces lactic acid that is oxidized by the normoxic peripheral cells.
Volume 3, October 2013 1627

Monocarboxylic Acid Transport Comprehensive Physiology
each muscle having a different balance depending on whetherit is used primarily for rapid high intensity exercise (gly-colytic) or endurance exercise (oxidative) (26, 38, 154). Theglycolytic white fibers produce lactic acid that leaves the fibervia MCT4 whose properties are well suited for exclusivelyglycolytic cells as noted above. This lactic acid is then takenup and oxidized by the red fibers which express primarilyMCT1, together with MCT2 in some species (82, 91, 145),whose Km values for L-lactate make them well suited forlactic acid uptake (26, 154).
Brain
A lactate shuttle is also thought to operate in the brain whereastrocytes export lactic acid to be oxidized by neurons as agood respiratory fuel (20, 234). The distribution of MCT iso-forms is consistent with this since astrocytes contain MCT1and MCT4 that are suitable for lactic acid efflux, while neu-rons express MCT1 and the higher affinity MCT2 that iswell suited for lactic acid uptake (50, 51, 226, 234, 257). Infact, MCT2 expression in the brain is largely confined to thepostsynaptic density (PSD) of the neurons, a region rich inmitochondria and thought to oxidize lactate as a preferredrespiratory fuel (19,50,234). Targeting of MCT2 specificallyto the PSD is mediated by a PDZ binding motif on the C-terminus of MCT2 (19) that allows it to bind to PSD95, ascaffolding protein found in the PSD (226) whose role isto bind proteins containing a suitable binding motif whichMCT2 contains in its extreme C-terminus (19). The lactateshuttle between astrocytes and neurons has been shown to beimportant for long-term potentiation in the hippocampus ofrats (282). Thus, loss of memory of learned tasks was observedfollowing microinjection of antisense oligodeoxynucleotidesto knockdown either MCT4 or MCT1 expression in astro-cytes or MCT2 expression in neurons. When either MCT1 orMCT4 was knocked down, memory was rescued by localizedinfusion of L-lactate to replace that normally produced by theastrocytes. However, this was not the case when MCT2 wasknocked down since the added lactate was unable to enter theneurons (282).
The retina
There is also evidence that lactate metabolism in the retinainvolves lactate shuttles, with a complex interplay betweenthe RPE, photoreceptor cells, and other neurons (which oxi-dize lactate) and glial cells (Muller cells) which export lac-tate through MCT4 (2). As noted above, MCT3 is exclu-sively located on the basolateral surface of the RPE and isresponsible for lactate efflux into the choroidal blood sup-ply, whereas MCT1, unusually, is exclusively located on theapical surface of the RPE (93,229,231,232). This apical loca-tion of MCT1 is dependent on targeting signals in the basiginrather than the MCT1 (66) whereas MCT3 and MCT4 pos-sess dominant sorting signals in their C-terminal cytoplasmictails that ensure their basolateral expression independently of
basigin (44). Interestingly, mice in which MCT3 was genet-ically deleted were healthy with no significant abnormalitiesin retinal histology, although electrophysiological studies ofretinal function did reveal modest changes in behavior. Thiswould be consistent with a decrease in the pH of the sub-retinal space leading to a reduction in the magnitude of thelight suppressible photoreceptor current (61). However, lossof basigin prevents proper expression of MCT1, MCT3, andMCT4 (230) which may account for the impaired maturationand function of the retina that leads to blindness in basiginknockout mice (113). In this context, an additional role ofMCT1 and MCT3 in the eye may be regulating the volumeof the subretinal space by transporting water with the lacticacid. An accumulation of lactate within the subretinal spacewould cause osmotic swelling, resulting in the retina becom-ing detached from the RPE, but this is prevented by the rapidtransport of lactic acid across the RPE and into the blood (2).Indeed, there is evidence that MCT1 may directly transportwater with lactate (123, 323).
Tumors
Evidence has also been presented for lactate shuttling withinsome tumors where the hypoxic centre of the tumor is gly-colytic and produces lactic acid that is exported by MCT4.This is then taken up by peripheral tumor cells expressingMCT1 that oxidize it as a respiratory fuel (70, 275).
pH regulationIntracellular pH is tightly controlled by regulating the activityof a range of acid extruding and acid loading mechanismssuch as Na+/H+ exchange and bicarbonate/CO2 transport(223, 300). However, in glycolytic cells the efflux of lacticacid via MCT1 or MCT4 is quantitatively the greatest pro-ton extrusion mechanism. This ensures that there is not anaccumulation of lactic acid within the cell that would causeintracellular acidification during conditions of high glycolyticflux. Indeed, in tumor cells, which exhibit especially high ratesof glycolysis, inhibition of MCT activity either pharmaco-logically or genetically causes intracellular acidification andinhibition of tumor growth (15,49,149,165,223). Lactic acidefflux on MCT1 also plays an important role in the restora-tion of intracellular pH during reperfusion or reoxygenationfollowing a period of ischemia or hypoxia, and its inhibitionslows the return of the pH to normoxic values (121,122,296).Interestingly, it has been shown that intracellular carbonicanhydrase II can interact with MCT1 and MCT4 to enhancetheir transport activity (13, 14, 279) while MCT2 is stimu-lated by an interaction with extracellular carbonic anhydraseIV (161). These effects occur independently of the catalyticactivity of carbonic anhydrase, perhaps by enhancing the rateof proton movement to and from the carrier. There may alsobe some interaction between the sodium bicarbonate cotrans-porter (NBC) and MCT1 since coexpression of NBC with
1628 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
MCT1 in Xenopus oocytes gives faster rates of lactate trans-port than with MCT1 alone (12).
Redox communication between cellsMonocarboxylate transport also allows for the redox stateof NADH/NAD+ in one tissue to influence that of anotherthrough the blood concentrations of L-lactate, pyruvate, D-β-hydroxybutyrate and acetoacetate (122, 245). This occursbecause LDH is exclusively cytosolic and uses cytosolicNADH/NAD+ to interconvert pyruvate and L-lactate whileβ-hydroxybutyrate dehydrogenase is exclusively intramito-chondrial and uses mitochondrial NADH/NAD+ to inter-convert acetoacetate and D-β-hydroxybutyrate. Because thereactions catalyzed by both enzymes are close to equi-librium in most cells, cytosolic NADH/NAD+ is in equi-librium with the cytosolic L-lactate/pyruvate ratio and themitochondrial NADH/NAD+ is in equilibrium with mito-chondrial D-β-hydroxybutyrate/acetoacetate. This means thatshifts in the cytosolic NADH/NAD+ ratio cause changes inthe [lactate]/[pyruvate] ratio and vice-versa. Similarly, shiftsin the mitochondrial NADH/NAD+ ratio cause changes inthe [β-hydroxybutyrate]/[acetoacetate] ratio and vice-versa.Because D-β-hydroxybutyrate and acetoacetate can crossthe inner mitochondrial membrane (IMM) on the mitochon-drial pyruvate transporter and all four monocarboxylates aregood substrates for MCTs, the L-lactate/pyruvate and D-β-hydroxybutyrate/acetoacetate ratios in the blood matchthose in the cytosol and mitochondrial matrix and reflectthe NADH/NAD+ redox state of these compartments. Thismeans that a major change in redox state in one tissue will becommunicated to others thus providing a means of communi-cating the redox status of one tissue with that of another withpotential implications for their metabolism. (118, 122, 245).
Regulation of MCT ActivityRegulation of protein expressionThere is increasing evidence for long-term regulation ofthe expression of MCT isoforms in response to changingmetabolic demands and this may occur by both transcriptionaland posttranscriptional mechanisms.
MCT1
Numerous studies have shown upregulation of skeletal mus-cle MCT1 expression in response to chronic stimulation orexercise in rats and humans (7, 21, 27, 29, 55, 79, 99, 153-155, 184, 235, 289, 290, 320). Conversely, down-regulationof lactate transport activity in skeletal muscle in responseto denervation of muscle or spinal injury has been reportedand is thought to involve a decrease in MCT1 expression(183, 236, 237). During aerobic exercise, there are increasesin intracellular [Ca2+] and AMP that play important roles in
stimulating oxidative energy metabolism (166, 207). It is hasbeen proposed that these changes in [Ca2+] and AMP may alsomediate the upregulation of MCT1 expression by activatingthe calcium-dependent protein phosphatase, calcineurin, andAMP-activated protein kinase (AMPK) (122). Calcineurin isthought to play a central role in muscle gene expression andthe calcineurin inhibitors cyclosporine A (CsA) and FK506can remodel skeletal muscle in favor of fast oxidative fibers(209). These fibers express less MCT1 than slow oxidativefibers that express more MCT1 and less MCT4 (310). CsAalso inhibits cardiac hypertrophy (209), a process that is alsoassociated with upregulation of MCT1 expression (148). Cal-cineurin is thought to act by dephosphorylation and activationof the transcription factor NFAT (nuclear factor of activated Tcells) (22) and the MCT1 promoter contains several consen-sus NFAT binding sequences ((T/A)GGAAA(A/N)(ATC)N)(122). The upregulation of MCT1 expression in response toincreased muscle activity may also involve the transcriptionalcoactivator PGC1α (18). PGC1α expression is increased inresponse to increased calcium concentrations and activationof AMPK (166, 207) and is capable of driving the formationof slow-twitch oxidative muscle fibers (173) which primarilyexpress MCT1 rather than MCT4 (310). Furthermore, usingan MCT1 promoter luciferase construct, it was demonstratedthat 5-aminoimidazole-4-carboxamide-1-β-d-ribonucleoside(AICAR), an activator of AMPK, can stimulate the activity ofthe MCT1 promoter twofold in both L6 myoblasts and HepG2hepatoma cells (122). However, in rat Sertoli cells othershave reported that AICAR downregulates MCT1 expressionalthough no direct measurements of promoter activity weremade (86). Thyroid hormone (T3) has also been reported toupregulate MCT1 and MCT4 expression in skeletal muscleat the mRNA level although only MCT4 protein levels werefound to be increased (307). Hypoxia was reported to upreg-ulate MCT1 expression in human adipocytes and this couldbe mimicked by cobalt (227) implying the involvement ofhypoxia inducible factor 1-α (HIF-1α), a transcription factorthat is well known to coordinate the metabolic response ofcells to hypoxia (54). However, in other cell types no upreg-ulation of MCT1 expression by hypoxia was reported underconditions that MCT4 expression was greatly increased (293).Furthermore, unlike the MCT4 promoter, neither the MCT1nor the MCT2 promoter contains hypoxia response elements(HREs) and using luciferase promoter constructs no directactivation by hypoxia of either promoter could be observed(293).
Activation and proliferation of T-lymphocytes is associ-ated with a large stimulation of the rate of glycolysis (16) andthis is accompanied by increased MCT1 expression (200)which is likely to involve a similar calcineurin-dependentmechanism to that described above for skeletal muscle (122).By contrast MCT1 expression in adipose tissue, heart andskeletal muscle was found to be reduced in streptozotocin-induced diabetes (78,107), although others have not observedthis effect in skeletal muscle despite a decrease in measuredrates of lactate transport (255, 256). A decrease in MCT1
Volume 3, October 2013 1629

Monocarboxylic Acid Transport Comprehensive Physiology
expression has also been described in skeletal muscle ofobese rats (256) while an increase in expression was reportedin the brain of obese mice or mice subject to ketosis andchronic hyperglycemia (42, 170, 233). There is also evidencefor changes in MCT isoform expression patterns during devel-opment in the heart (128), inner ear (208), and brain (169) aswell as during the development of the preimplantation embryo(147). In heart, more MCT4 and less MCT1 is expressed inthe neonate than the adult, consistent with the transition fromglycolytic metabolism of glucose in the neonate to oxidativemetabolism in the adult (128).
In addition to the regulation of MCT1 gene transcrip-tion, there is also evidence for posttranscriptional regulationof MCT1 expression. In the heart, MCT1 protein expressionincreases in left ventricle hypertrophy following surgical lig-ation of a major branch of the left coronary artery, yet thereis little change in mRNA (148). Similarly, in cultured HeLacells MCT1 protein expression is increased several fold dur-ing the postmitotic and G1 phases of the cell cycle in theabsence of a change in MCT1 mRNA while MCT4 showedno significant change in expression at either the protein ormRNA levels suggesting that translation of MCT1 mRNAregulation is regulated (122). Such control of translation usu-ally involves specific sequences and secondary structure inthe 5′ or, frequently, the 3′ untranslated regions with whichinitiation factors including eIF4E and other regulatory factorssuch as Maskin or Cup are thought to interact to enhance orrepress translation (95, 175, 186, 251). Since the 3′ untrans-lated region (3′-UTR) of MCT1 is very long (some 1.2 kblonger than either MCT4 or MCT2 in rats), it could well beinvolved in such translational control of MCT1 expression(119). Indeed, the 3′-UTR of MCT1 mRNA contains a poten-tial cytosolic polyadenylation element and hexanucleotideelements, sequences thought to be critical in the regulationof polyadenylation at the exit from the mitotic phase in thecell cycle, that in turn may relieve Maskin or Cup inhibitionof eIF4E (175). Furthermore, changes in the phosphorylationstate of the initiation factor eIF4E and its inhibitor 4E-BP1during the cell cycle are known to regulate the expressionof several proteins at the translational level, and the time ofmaximal 4E-BP1 phosphorylation (129) corresponds with thepeak of MCT1 expression (122).
Posttranscriptional regulation of MCT1 expression mayalso play an important role in preventing MCT1 expression inthe insulin secreting β cells of the Islets of Langerhans whichlack expression of any MCT isoform (324). This is importantto prevent insulin secretion in response to elevated blood lac-tate and pyruvate levels occurring during exercise. Althoughthe promoter of MCT1 contains a CpG island that could be thesite of specific DNA methylation typical of many genes thatexhibit tissue-specific expression patterns (58), no evidencefor this mechanism was obtained (252). Rather, translationalregulation of MCT1 expression involving micro RNA hasbeen implicated. The three isoforms of miR-29 are highlyexpressed and enriched in mouse islets and these selectivelytarget the 3′ untranslated regions of both human and mouse
MCT1 mRNA preventing their translation. Mutation of thecognate miR-29 binding site on the MCT1 mRNA was shownto prevent this effect. Furthermore, inhibition of miR-29aexpression in primary mouse islets was shown to increaselevels of MCT1 mRNA expression, strongly supporting a rolefor miR-29 the β-cell-specific silencing of MCT1 expression(252).
MCT2
Evidence for transcriptional control of MCT2 expression ismore limited. Increased expression of MCT2 mRNA hasbeen described in the brainstem of female rats in responseto food deprivation (48 h), consistent with enhanced utiliza-tion of ketone bodies as a respiratory fuel under these condi-tions (182). However, other studies have reported that obesityalso increases expression of MCT2 (and that of MCT1 andMCT4) in the brain, most prominently in the cortex and inthe hippocampus (233). An increase in MCT1 and MCT2expression in the brain has also been described during recov-ery from a focal ischemic insult (195), whereas in humanadipocytes hypoxia was reported to decrease expression ofMCT2 mRNA while increasing that of MCT1 and MCT4(227). Early comparison of the expression levels of MCT2mRNA and protein imply that MCT2 may also be subjectto posttranscriptional control (145), and further evidence forthis was provided in the brain where increased expressionof MCT2 in response to noradrenalin (46) and insulin orIGF-1 (47) was described. The mechanism was proposed toinvolve activation of translation mediated by stimulation ofthe phosphoinositide 3-kinase—Akt—mammalian target ofrapamycin pathway. Subsequent studies from the same labo-ratory reported that brain-derived neurotrophic factor (BDNF)enhances MCT2 expression in mouse cultured cortical neu-rons by a similar mechanism and suggested that changes inMCT2 expression could participate in the process of synapticplasticity induced by BDNF (261).
MCT3 and MCT4
How MCT3 expression is restricted to the RPE and choroidplexus is not known, but wounding of the RPE resulted in lossof MCT3 and the upregulation of MCT4 expression in migrat-ing cells at the edge of the wound (88). MCT4 expression isgreatly increased by hypoxia, consistent with its proposed rolein exporting lactic acid produced by glycolysis and this effectcan be mimicked by treatment of cells with cobalt (227, 293)suggesting a role for hypoxia inducible factor 1-α (HIF-1α).This is a transcription factor that is well known to coordinatethe metabolic response of cells to hypoxia (54). Indeed, upreg-ulation of MCT4 by hypoxia is lost in cells lacking HIF-1α,and the MCT4 promoter of both human and mouse containsfour potential HIF-1α response elements (HREs). Deletionanalysis using luciferase promoter constructs revealed thatonly the 2 HREs just upstream from the transcription startsite are essential for the hypoxia response (293). Thus MCT4
1630 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
joins a large family of proteins, including several other keyglycolytic enzymes, whose expression is regulated by HIF-1α
(54). MCT4 is also upregulated in the neonatal heart whichis more glycolytic in its energy metabolism than the adultheart where MCT4 is low or absent but MCT1 is abundant(128,310). It is not known whether HIF-1α is responsible forthis increased MCT4 expression although it has been reportedthat increased L-lactate concentrations can increase HIF-1α
levels in cells (64). This might provide a link between thehigh rates of glycolysis in white muscle fibers and MCT4expression. This effect of L-lactate is thought to be medi-ated indirectly by pyruvate derived from lactate inhibitingprolylhydroxylase 2, an enzyme involved in the degradationof HIF-1α when oxygen is abundant (64). Increased expres-sion of MCT4 expression in skeletal muscle has also beendescribed in response to stimulation of AMPK with AICAR(85) but this conflicts with studies using an MCT4 promoterluciferase construct which showed AICAR to inhibit the activ-ity of the MCT4 promoter by more than 50% (122). Further-more, upregulation of MCT4 expression under conditions ofhigh energy demand has only been reported in one study fol-lowing high-intensity treadmill training of rats, and it wasonly modest compared with that of MCT1 (289).
Regulation of MCT activity independentof expressionThere is little evidence for short-term regulation of MCTactivity. Smith & Drewes reported a rapid stimulation ofMCT1 activity in rat brain endothelial cells in response toelevated cyclic AMP and suggested that it might be regulatedby phosphorylation (274), but this was not confirmed by others(122). In Drosophila melanogaster the trafficking of Silnoon,a homolog of MCT1, to the apical membrane is induced bythe kinase activity of LKB1, but it is not known whether thisis mediated by phosphorylation of Silnoon (146), nor whetheran equivalent pathway is present in mammals. Another poten-tial mechanism for the regulation of MCT activity could beby translocation of the transporters from an intracellular storeto the plasma membrane such as occurs for the glucose trans-porter GLUT4 (24). Some evidence for this was obtainedin the heart following ischemia where the resulting hyper-trophy of the left ventricles was accompanied by increasedexpression of MCT1 at the plasma membrane without anincrease in MCT1 mRNA (148). In addition to a possible rolefor translational regulation of MCT1 expression under theseconditions, it was noted that increased expression was asso-ciated with the appearance of a novel intracellular pool ofMCT1 associated with cisternae close to the t-tubules (148).It is possible that expression of MCT1 at the sarcolemmamay occur via a regulated translocation of MCT1 from thisintracellular pool. Interestingly, MCT1 possesses two acidicclusters and an LL motif in the C-terminus; these motifs arebelieved to be important in endosomal-lysosomal targeting ofGLUT4 (269). A further potential mechanism for the rapidregulation of MCT activity could be through the binding of
ligands to the associated ancillary protein, embigin or basi-gin. Although such ligands have yet to be identified, someantibodies against extracellular epitopes of basigin have beenreported to inhibit lactate transport leading to intracellularacidosis and cell death in basigin-expressing cancer cell lines(5). There is evidence for homotropic interaction betweenbasigin expressed on adjacent cells (124) and an intriguingpossibility is that this might play a role in contact inhibitionby reducing glycolytic lactic acid efflux and hence cell pro-liferation much as occurs in T-lymphocytes when MCT1 isinhibited pharmacologically (200).
The Role of Plasma MembraneMonocarboxylate Transport inDisease and Its TreatmentImpaired monocarboxylate transportGenetic knockout of MCT1 is embryonically lethal, confirm-ing the essential role of MCT1 in normal development. How-ever, heterozygous MCT1+/− mice exhibit no gross pheno-typic abnormalities despite a reduction in MCT1 levels byabout 50%. However, they do develop an axonopathy in thebrain and spinal cord by 8 months of age (167). In this con-text it is interesting that oligodendroglial MCT1 expression isreduced in patients with amyotrophic lateral sclerosis, a fatalneurological disease characterized clinically by progressiveweakness and pathologically by cortical and spinal motoneu-ron degeneration (167). These data suggest a role for MCT1in the pathogenesis of this disease and would be consistentwith an essential role for oligodendroglia in providing lactateto act as a fuel to support axon function and neuron survivalmuch as proposed for the lactate shuttle between astrocytesand neurons in the brain (20, 234).
Perturbing MCT1 activity pharmacologically by treat-ment of rats with AR-C117977 has been reported to be withoutmajor adverse effects; no weight loss was detected and littleovert toxicity observed (200). The exception was a markedatrophy of the testes which might be explained by inhibitionof MCT2 rather than MCT1 (32, 212, 213). Indeed, mice inwhich the MCT1 ancillary protein, basigin, has been knockedout are also sterile (142) and MCT2 has been shown to interactwith basigin and not embigin in mouse spermatozoa (177).The basigin knockout mice also show various neurologicalabnormalities and exhibit retinal dysfunction, consistent withdisruption of correct MCT expression in brain and retina(198, 230).
Muscle Fatigue
Accumulation of lactic acid in skeletal muscle is widely heldto cause fatigue, although more recent data has suggested thatthis hypothesis is oversimplistic since lactic acid is also a goodrespiratory fuel for the oxidative fibers (41, 228). Neverthe-less, it is tempting to speculate that some conditions associatedwith muscle fatigue may be associated with impairment of
Volume 3, October 2013 1631

Monocarboxylic Acid Transport Comprehensive Physiology
lactate transport. One such example is cryptic exercise intol-erance in which otherwise healthy individuals suffer severechest pain and muscle cramping on vigorous exercise. Indeed,rates of lactate uptake by the erythrocytes of such patientswere reported to be slower than controls which was attributedto an MCT defect (81), and RT-PCR of MCT1 from musclebiopsies from these patients identified a number of amino aciddifferences that were not attributable to polymorphisms (193).Of these, only a lysine to glutamate mutation in the large cyto-plasmic loop between TMDs 6 and 7 was considered a likelycandidate to affect transporter activity, but when expressed inXenopus oocytes this mutant MCT1 showed normal transportkinetics (118). Thus it remains unclear whether mutations inMCT1 are responsible cryptic exercise intolerance or whetherother factors (such as mutations in embigin or basigin) mightbe involved. It is also intriguing to speculate that autoantibodyinteractions with basigin may underlie some chronic fatiguesyndromes that are known to be associated with autoanti-body production. For example, patients with primary biliarycirrhosis who experience chronic muscle fatigue also haveabnormalities in muscle pH regulation (135) consistent withimpaired lactate transport mediated by autoantibodies againstbasigin (5).
Inappropriate expression of MCTsAs noted above, the insulin-secreting β cell of the Islets ofLangerhans is unusual in expressing no MCTs. It is thoughtthat this is important to prevent inappropriate insulin secretionduring exercise when blood levels of lactate and pyruvate areincreased (324). Consistent with this hypothesis, mutationsthat enhance MCT1 promoter activity have been identifiedin individuals of three separate pedigrees, each displayinghyperinsulinaemia (EIHI) with hypoglycaemia in responseto exercise or pyruvate injection (211). It was proposed thatthis enhanced promoter activity led to expression of MCT1in the β cells enabling them to oxidize pyruvate during exer-cise. This would increase ATP levels sufficiently to stimulatethe inappropriate insulin secretion that leads to the observedhypoglycaemia. Confirmation of this hypothesis was subse-quently provided by the generation of a transgenic mousecapable of doxycycline-induced, β-cell-specific overexpres-sion of MCT1. In vivo induction of MCT1 expression in thesemice was shown to mimic the metabolic responses seen inpatients with EIHI (253).
The importance of MCTs and SMCTs for tumorcells and chemotherapyMCTs
As has already been noted, tumor cells depend on glycoly-sis for their energy metabolism (30, 163, 309). They expresshigh levels of MCT1 or MCT4 to export the large quanti-ties of lactic acid they produce and to maintain an appro-priate pH environment for tumor growth (30, 49, 223, 309).
However, there is considerable variation in the MCT iso-forms and ancillary proteins expressed in different tumors(48,223,238,239). Metastatic tumors frequently show upreg-ulation of HIF-1α and this is associated with increasedMCT4 expression together with its ancillary protein, basigin(48,49,89,223,238). This may be significant because anotherfunction of basigin is to activate extracellular metallopro-teinases (198) that play a key role in tumor cell proliferation,migration, and invasiveness (141,201). Indeed knockdown ofbasigin inhibits the proliferation, invasiveness, and metastaticactivity of malignant melanoma (45, 201, 280).
The increasing awareness of the importance of lacticacid efflux for tumor cell survival and proliferation hasled to its recognition as an important drug target in can-cer (156, 266, 297) and knockdown of MCTs and or basiginhas been shown to impair the growth of tumor cells (165).Inhibiting tumor cell proliferation and inducing death bytreatment with an MCT inhibitor has also been described(80, 275), although the inhibitor used (CHC) is not iso-form specific and is actually much more potent at inhibit-ing the MPC than any MCT (108, 110, 116). Clearly, drugsthat are specific and potent inhibitors of MCT isoformsare required if they are to be used as potential therapeu-tic agents, and the discovery of a class of specific MCT1inhibitors by AstraZeneca will provide a springboard for thisapproach. Indeed, AR-C155858 has already been demon-strated to impair the growth of tumor cells expressing MCT1(165). Encouragingly, rats dosed with the specific MCT1inhibitor AR-C117977 did not show any weight loss or overttoxicity except for a marked atrophy of the testes (200). Thislatter effect is consistent with the proposed role for MCT-1-mediated lactate transport in spermatogenesis (32). This hasallowed one of these drugs (AZD-3965) to enter clinical trialsfor treating cancer (http://www.cancerresearchuk.org/cancer-help/trials/a-trial-azd3965-for-advanced-cancer). A specificMCT4 inhibitor would have particular merit for targetingmetastatic tumor cell lines in which MCT4 is especially highlyas a result of HIF-1α overexpression (30, 49, 89, 223, 309).However, both MCTs and SMCTs may also play a role inthe uptake of other drugs that target metabolism such as 3-bromopyruvate and dichloroacetate (6,23) which might miti-gate against combination therapies.
SMCTs
While MCTs are essential for tumor cells, SLC5A8 was firstdiscovered as a tumor suppressor (171). Its expression issilenced in tumors of colon, thyroid, stomach, kidney, andbrain (90, 130, 172, 206, 221, 222). The tumor-suppressivefunction was originally thought to reflect its role in medi-ating accumulation of butyrate, propionate, and pyruvate, allof which are inhibitors of histone deacetylases (106,286,287).However, it was later shown that tumor suppression wasexhibited by a transport-inactive form of SLC5A8 and thatthis effect is actually mediated by depletion of survivin (56).
1632 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
Other roles of MCTs and basigin in diseaseAn unexpected role of MCT4 is that it acts as West Nile viralreplication resistance factor that delays the temporal transi-tion into the replication phase of endocytosed viral particles(162) while basigin is a receptor essential for erythrocyteinvasion by Plasmodium falciparum (57). Basigin has alsobeen implicated in signaling pathways in inflammation, andas a receptor for viruses, including HIV, but it is not knownwhether these interactions involve changes in MCT1 activity(3, 141, 254, 322).
Monocarboxylate Transport intoMitochondriaRoleSeveral major metabolic pathways require monocarboxylatesto be transported into or out of the mitochondrial matrix(Fig. 1). Thus, oxidation of glucose involves glycolytic pro-duction of pyruvate and its oxidation in the mitochondria bypyruvate dehydrogenase and the citric acid cycle. Fatty acidsynthesis from glucose follows the same pathway with theaddition of pyruvate carboxylation to oxaloacetate within themitochondrial matrix by pyruvate carboxylase. Pyruvate car-boxylation is also required for the de novo synthesis of glucose(gluconeogenesis) and here too transport of pyruvate into themitochondria will be required when L-lactate and some aminoacids are substrates (65, 120, 262, 298). The ketone bodies,acetoacetate and β-hydroxybutyrate must also be transportedout the liver mitochondria where they produced under condi-tions of high fatty acid oxidation and into the mitochondria oftissues that oxidize them such as skeletal and cardiac muscleand neurons (262, 298).
Discovery and characterization of themitochondrial pyruvate carrierThe first study to suggest the presence of a specific carrier formonocarboxylate transport across the IMM was published in1974 (216) and its existence definitively established in thesame year by the demonstration that CHC specifically inhib-ited pyruvate transport into rat liver mitochondria with a Ki
of 2 to 5 μmol/L (116). Because of its key role in trans-porting pyruvate into the mitochondria this MCT is moreusually known at the MPC. CHC was subsequently usedto confirm the importance of the MPC in gluconeogenesisfrom L-lactate and serine but not alanine in liver and kidney,lipogenesis from glucose but not acetate in adipose tissueand pyruvate (glucose) oxidation in the heart and diaphragm(117,185). The kinetics and substrate and inhibitor specificityof the MPC were characterized in isolated liver mitochondria(108,111,218,219) and the substrate specificity is summarizedin Table 6. It was found to have a Km for the 2 and 3 oxoacidspyruvate and acetoacetate of about 0.15 and 0.60 mmol/L,respectively, with very low affinity for the corresponding
Table 6 The substrate specificity of the mitochondrial pyruvate car-rier. Km values are for transport into isolated rat liver mitochondriaand are taken from Ref. 120 which cites the original sources.
Monocarboxylate Km mmol/L
Pyruvate 0.12
Glyoxylate 20
α-ketobutyrate 0.17
α-ketovalerate 0.29
α-ketoisovalerate† 1.4
α-ketocaproate† 1.0
α-ketoisocaproate† 3.9
Phenylpyruvate 2.9
3-hydroxypyruvate 1.6
3-fluoropyruvate 0.22
3-bromopyruvate 1.0
Acetoacetate 0.61
L-lactate 12
D,L-β-hydroxybutyrate 5.6
Oxamate 3.6
Fluoroacetate 0.36
Chloroacetate 0.40
Dichloroacetate 1.1
2-chloropropionate 0.6
3-chloropropionate 2.2
2,2-dichloropropionate 5.6
†These substrates are transported slowly and acted better as inhibitors.
hydroxyl acids, L-lactate and D-β-hydroxybutyrate (Km val-ues of 12 and 6 mmol/L, respectively). Other 2-oxoacids arealso good substrates such as 2-oxobutyrate and 2-oxovalerate(Km values of 0.17 and 0.29 mmol/L, respectively) but largeraliphatic or aromatic 2-oxoacids such as those producedby transamination of phenylalanine (phenylpyruvate) andthe branch chain aliphatic amino acids such as leucine (α-ketoisocaproate), isoleucine (α-keto-β-methylvalerate), andvaline (α-ketoisovalerate) are poorly transported and act asinhibitors of pyruvate transport (108, 111, 115). An addi-tional carrier mechanism has been described for the branchchain keto acids, which is less sensitive to α-cyanocinnamateanalogs (138-140). The MPC will also transport the pyruvateanalogue oxamate and 2 and 3 halogenated monocarboxy-lates such as monochloroacetate and dichloroacetate with highaffinity (Km values of 0.21, 0.25, and 0.46 mmol/L, respec-tively) (108, 111, 218, 219).
Inhibition of the MPC by α-fluorocinnamate is at leasttwo orders of magnitude less effective than α-cyanocinnamateand this was shown to reflect the activation of the double bondby the cyano group making it sensitive to Michael addition
Volume 3, October 2013 1633

Monocarboxylic Acid Transport Comprehensive Physiology
by thiol groups (108, 109). This enables α-cyanocinnamateand its analogs to bind covalently, but reversibly, to a cys-teine on the MPC causing its inhibition. Inhibition of theMPC by α-cyanocinnamate analogues was also shown torequire their transport into the matrix of the mitochondriawhere they bind to a matrix facing site, trapping the carrierin its inward facing conformation (111). The affinity of theanalogs was found to increase with increasing hydrophobic-ity implying the presence of a hydrophobic pocket to whichthe inhibitor bound (111, 116). The most potent of these α-cyanocinnamate analogues is a Pfizer compound, UK5099(α-cyano-5-(1-phenylindol-3-yl)-acrylate) with a Ki of 5 to10 nmol/L (109, 268) and titrations of the MPC activity withthis inhibitor suggested that the concentration of the MPCwithin mitochondria was about 100 pmoles per mg protein.Subsequently, these data were refined using a novel seriesof thiazolidine compounds synthesized by GlaxoSmithKline(e.g., GW604714X and GW450863X) which inhibit the MPCwith Ki values <1 nmol/L (133). Although these inhibitorsare structurally distinct from the α-cyanocinnamate analogs,they also possess an activated double bond that attacks acysteine on the MPC. Using a radioactively labeled analogallowed more accurate determination of the amount of theMPC present in heart, kidney, liver, and brain mitochondriaof 56, 40, 26, and 20 pmoles per mg protein, respectively(133). This was in good agreement with the 45 to 50 pmol permg binding sites for [14C]-α-cyanocinnamate in heart mito-chondria determined by Paradies (217, 220).
The molecular identity of the MPCThe MPC is not a member of the MCT family
It was apparent from the first recognition that specific mono-carboxylate carriers are present in mitochondria and theplasma membrane that they were different molecular enti-ties because of their distinct substrate and inhibitor speci-ficities (116). For example, as noted above, the MPC has ahigh affinity for oxamate but very low affinity for L-lactatewhereas MCT1 has a high affinity for L-lactate but no affinityfor oxamate. This was further confirmed by the discovery ofnovel inhibitors of MCT1 with Ki values of about 1 nmol/Lthat have little effect on the MPC (200, 212) and those thatinhibit the MPC with Ki values <1 nmol/L without affect-ing MCT1 (133). Nevertheless, there are several reports thatMCT1 is present in mitochondria of the heart, skeletal mus-cle, and the brain and it has been suggested that this providesa mechanism for these tissues to oxidize lactate as a res-piratory fuel (17, 39, 40, 126, 321) (38, 127). It is proposedthat lactate rather than pyruvate is transported directly intothe mitochondria where an intramitochondrial LDH may oxi-dize it to pyruvate prior to complete oxidation around thecitric acid cycle. While this might appear to have the advan-tage of avoiding the requirement for mitochondrial NADHshuttles to oxidize cytosolic NADH produced by LDH, there
are strong theoretical arguments against this hypothesis. Oxi-dation of lactate by LDH within the mitochondrial matrixis both energetically unfavorable and incompatible with theknown NADH redox compartmentation within the cell whichmaintains a higher NADH/NAD+ ratio in the mitochondriathan the cytosol (122,264). Furthermore, several workers haveshown that careful density gradient centrifugation removes allsignificant MCT1 and LDH from the mitochondrial fraction(52, 118, 133, 245, 264).
Evidence that the MPC is a member of themitochondrial carrier family
The initial strategy used to identify the MPC utilized its irre-versible inhibition by hydrophobic thiol reagents such as N-phenylmaleimide (NPM). It was shown that α-cyanocinnmatecould protect the MPC from inhibition by NPM and that thiswas associated with less labeling of a 15 kDa inner mito-chondrial membrane protein by [3H]-NPM (288). However,no further purification or sequencing was performed to con-firm the identity of this 15 kDa protein. Subsequent stud-ies in pea mitochondria identified a 19 kDa protein whoseinteraction with a monoclonal antibody inhibited pyruvatetransport into mitochondria (302). However, the majority ofmitochondrial metabolite carriers are members of a 50-strong(in humans) family known as Mitochondrial Carrier Family(MCF) or SLC25 family (215). These carriers share commonsequence motifs within three tandemly repeated sequence ofabout 100 amino acids and are all predicted to have six TMDswith the C- and N-termini facing the intermembrane spaceand a large matrix facing loop between TMDs 3 and 4 (215).This proposed topology has been confirmed for the adeninenucleotide translocase whose three-dimensional (3D) crystalstructure has been solved (225). Other members of the samefamily, most of which are 30 to 36 kDa in size, have beenmodeled on the same structure and features associated withtheir substrate recognition identified (215,263). Partial purifi-cation of the MPC on hydroxyapatite columns with recon-stitution of activity in proteoliposomes were consistent withthe MPC being a member of the MCF (31, 202) and subse-quent affinity purification on a CHC affinity column isolated atransport active protein of 34 kDa but this was not sequenced(25). It was proposed that the 15 kDa labeled protein pre-viously identified as the MPC might result from proteolyticcleavage between TMs 3 and 4, but when purification andsequencing of the 15 kDa protein was performed more than20 years later, it was found to be subunit 4 of cytochromeoxidase (134). An alternative strategy was thus required toidentify the MPC and the availability of the full genomesequence of the yeast Saccharomyces cerevisiae, togetherwith the amenability of this organism for genetic manipu-lation, provided the means. Genetic knockout of each mem-ber of the MPC without an ascribed function was performedand only in the case of YIL006w was inhibitor-sensitive-pyruvate transport into isolated yeast mitochondria isolatedtotally abolished. Thus, YIL006w was proposed to encode
1634 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
the MPC in yeast and homologues, now named SLC25A32,SLC25A33, and SLC25A36, were identified in mouse andhumans (134). However, overexpression of the YIL006w pro-tein in E. Coli and its reconstitution into proteoliposomes byPalmieri’s group suggested that it transported NAD+ and notpyruvate (292). This would be more consistent with its greatersequence similarities to other members of the MCF that trans-port nucleotides rather carboxylates (292), although it shouldbe noted that α-cyanocinnamate binds to the nucleotide bind-ing site of aldehyde dehydrogenase (240).
Identification of a novel protein family involved inmitochondrial pyruvate transport
Since no data have been published confirming or otherwisethat any member the MCF acts as the mammalian MPC it ispossible that non-MCF members are involved in mitochon-drial pyruvate transport. Two very recent papers have indepen-dently identified members of a novel family (pfam UPF0041)of IMM proteins in yeast (Yg1080w, Yhr162w, and Ygr243w)without any previously known function as strong candidatesfor the MPC. Their knockout was reported to abolish UK5099-sensitive mitochondrial pyruvate transport into mitochondriaand impair mitochondrial pyruvate metabolism (33,131). Theyeast proteins were renamed Mpc1, Mpc2, and Mpc3 andit was shown that the mouse and human genomes contain 2orthologs, Brp44L (Mpc1) and Brp44 (Mpc2) whose expres-sion in knockout yeast strains could reestablish pyruvate trans-port. Mouse Mpc1 could directly replace yeast Mpc1 althoughit required both mouse Mpc1 and mouse Mpc2 to reverse theeffects of yeast Mpc3 deletion. Furthermore, coexpression ofmouse Mpc1 and Mpc2 in the plasma membrane of Lactococ-cus lactis induced UK5099-sensitive pyruvate transport intothe cells which was not supported when either was expressedon its own (131). Interestingly, members of this new Mpcfamily contain only two or three TMDs and are thus unlikelyto be transporters in their own right. However, Mpc1 andMpc2 were found to coimmunoprecipitate and blue native-polyacrylamide gel electrophoresis showed them to run atabout 150 kDa suggesting they may form an oligomeric com-plex (33). The published data provide strong evidence for arole for Mpc1 and Mpc2 in mammalian mitochondrial pyru-vate transport and metabolism, and their 15kDa size is consis-tent with the labeling studies that identified the MPC as a 15kDa protein (288). Furthermore, in three unrelated familieschildren presenting with lactic acidosis and hyperpyruvatemiashowed mutations in a conserved region of Mpc1 and theirfibroblasts showed reduced rates of pyruvate-dependent res-piration that could be restored by expression of wild-typeMpc1 (33). However, concerns have been raised about thevalidity of the transport assays used to confirm the role ofMpc1 and Mpc2 in pyruvate transport as opposed to pyru-vate metabolism (113). It is also surprising that pyruvate isunique amongst the metabolically important carboxylic acidssuch as citrate, malate, succinate, and 2-oxoglutarate in notbeing transported by a member of the MCF. An intriguing
possibility is that there is a member of the MCF family stillto be identified that is actually responsible for mitochondrialpyruvate transport but that this requires an interaction withMpc1 and Mpc2 to be active. This would similar to the role ofembigin and basigin as ancillary proteins for MCTs and couldexplain the α-cyanocinnamate sensitive labeling of the 15 kDaprotein identified previously as the MPC (288). Indeed, thereis a conserved cysteine in TM3 of Mpc1 that could act as thethiol group with which the inhibitor interacts (113).
The role of mitochondrial monocarboxylatetransport in diseaseIn view of its central role in metabolism, a molecular defectin the MPC might be expected to be embryonically lethalunless there are other isoforms of the carrier that can com-pensate. This could be why individuals with mutations in aconserved region of Mpc1 but a normal Mpc2 do survive birthbut exhibit sever lactic acidosis and hyperpyruvatemia (33).Genetic impairment of mitochondrial pyruvate metabolism iswell documented (259) and one such case had previously beenproposed to reflect an impairment of mitochondrial pyruvatetransport (34). It is likely that the identification of the MPCwill allow more individuals who exhibit disturbances in theirpyruvate metabolism to be diagnosed with mutations in theMPC gene. Two metabolic diseases where there is good evi-dence for an involvement of the MPC are Phenylketoneuriaand Maple Syrup Urine Disease where there is accumulationof phenylpyruvate and the branch chain ketoacids respec-tively. The ability of these to inhibit the MPC is thought toinhibit pyruvate and ketone body entry into brain mitochon-dria, thus perturbing energy metabolism and resulting in theimpairment of brain development that is characteristic of thesediseases (115, 164).
ConclusionThe importance of monocarboxylic acid transport across theplasma membrane by MCTs in the metabolism of carbo-hydrate, fat, and amino acids is well established and themolecular identity of the carrier proteins involved is known.Their transport properties have been extensively character-ized and there are an increasing number of studies focusedon the regulation of their expression in different tissues and(patho)physiological conditions. Progress is being made onelucidating the 3D structure of MCTs by molecular modelingand site directed mutagenesis which should assist in the devel-opment of isoform specific inhibitors, but the field would begreatly helped by the elucidation of the crystal structure ofan MCT isoform, preferably in association with its ancillaryprotein. Endeavors to achieve this should be stimulated bythe increasing awareness of the significance of MCTs in arange of physiological processes that have clinical implica-tions. These include the energy metabolism of the brain andskeletal muscle and its perturbation in disease, the immune
Volume 3, October 2013 1635

Monocarboxylic Acid Transport Comprehensive Physiology
response that leads to proliferation of T-lymphocytes and theadaption of tissues to hypoxia including the regulation of theirpH in response to enhanced lactic acid production. The roleof MCTs in the proliferation of tumor cells is a particularexample of the latter and is developing into a promising areaof chemotherapy, especially following the development ofpotent and specific MCT1 inhibitors. These agents will alsoprovide a valuable tool for investigating the metabolic roles ofMCT1 in different tissues. An example of this is the use ofan MCT1 inhibitor in mouse studies revealing the importanceof MCT1 for oligodendroglial provision of metabolical sup-port for peripheral axons (167). The development of drugs thatare specific and potent inhibitors of the other MCT isoformsis eagerly anticipated since they would have great potentialfor probing the roles of different MCT isoforms in normalmetabolism and possibly as therapeutic agents. An MCT4specific inhibitor is especially needed since this might beeffective against metastatic tumor cells in which MCT4 oftenpredominate over MCT1 as a result of HIF-1α overexpres-sion (30,49,223). Disease states in which there is perturbationof MCT expression or activity have already been described(e.g., exercise induced hyperinsulimemia) but it is likely thatmore will emerge including associations between susceptibil-ity to known pathologies and polymorphisms in a particularMCT.
The role of SMCTs in the absorption on monocarboxy-lates from the gut and kidney tubules is also well establishedbut, although their molecular identity is established, muchless is known about their structure, mechanism, and regula-tion than is the case for MCTs. Nor is a specific and potentinhibitor available to probe their role in different tissues. Therecognition of SMCT1 as a tumor suppressor (171) may stim-ulate further research in this area as would the recognitionof any disease state that is associated with changes in SMCTexpression or activity.
The transport of monocarboxylates, especially pyruvateand the ketone bodies, across the inner mitochondrial mem-brane is well established as being essential for carbohydrate,fat, and amino acid metabolism and a specific inhibitor ofthe MPC to probe its role in metabolism available. However,although the mechanism and substrate and inhibitor speci-ficity of the MPC have been extensively studied, its molecu-lar identity remains less certain. The discovery of two novelproteins, Mpc1 and Mpc2, that are involved in the trans-port process and whose mutation can lead to impairmentof mitochondrial pyruvate metabolism is a major advancethat should stimulate the field (33, 131). Of particular inter-est will be whether these proteins alone can mediate trans-port or whether a member of the MCF is required. Thereare also important new avenues to explore in relation to theregulation of MPC expression and activity especially in sit-uations known to be associated with changes in mitochon-drial pyruvate metabolism. An obvious example is whetherMPC expression is downregulated in cells that do not oxidizepyruvate but exhibit aerobic glycolysis such as tumor cellsand white muscle fibers.
AcknowledgementsThe author wishes to thank the many students, postdoctoralworkers, and collaborators who have contributed to the stud-ies on plasma membrane and mitochondrial monocarboxylatetransport that have played their part in our increasing under-standing of these important processes and the many fundingbodies who have supported his research.
References1. Abramson J, Smirnova I, Kasho V, Verner G, Kaback HR, Iwata S.
Structure and mechanism of the lactose permease of Escherichia coli.Science 301: 610-615, 2003.
2. Adijanto J and Philp NJ. The SLC16A family of monocarboxylatetransporters (MCTs)-physiology and function in cellular metabolism,pH homeostasis, fluid transport. Curr Top Membr 70: 275-312, 2012.
3. Agrawal SM and Yong VW. The many faces of EMMPRIN - roles inneuroinflammation. Biochim Biophys Acta 1812: 213-219, 2011.
4. Anderson CM and Thwaites DT. Hijacking solute carriers for proton-coupled drug transport. Physiology (Bethesda) 25: 364-377, 2010.
5. Baba M, Inoue M, Itoh K, Nishizawa Y. Blocking CD147 inducescell death in cancer cells through impairment of glycolytic energymetabolism. Biochem Biophys Res Commun 374: 111-116, 2008.
6. Babu E, Ramachandran S, CoothanKandaswamy V, Elangovan S,Prasad PD, Ganapathy V, Thangaraju M. Role of SLC5A8, a plasmamembrane transporter and a tumor suppressor, in the antitumor activityof dichloroacetate. Oncogene 30: 4026-4037, 2011.
7. Baker SK, McCullagh KJA, Bonen A. Training intensity-dependentand tissue-specific increases in lactate uptake and MCT-1 in heart andmuscle. J Appl Physiol 84: 987-994, 1998.
8. Barac-Nieto M. D(−) 3-Hydroxybutyrate cotranport with Na in ratrenal brush-border membrane vesicles. Pflugers Arch 408: 321-327,1987.
9. Barac-Nieto M, Murer H, Kinne R. Lactate-sodium cotransport in ratrenal brush border membrane vesicles. Am J Physiol 239: F496-F506,1980.
10. Barac-Nieto M, Murer H, Kinne R. Asymetry in the transport of lac-tate by basolateral and brush border membranes of rat kidney cortex.Pflugers Arch 392: 366-371, 1982.
11. Barbara B, Podevin R-A. Stoichiometry of the renal sodium L-lactatecotransporter. J Biol Chem 263: 12190-12193, 1988.
12. Becker HM, Broer S, Deitmer JW. Facilitated lactate transport byMCT1 when coexpressed with the sodium bicarbonate cotransporter(NBC) in Xenopus oocytes. Biophys J 86: 235-247, 2004.
13. Becker HM, Hirnet D, FecherTrost C, Sultemeyer D, Deitmer JW.Transport activity of MCT1 expressed in Xenopus oocytes is increasedby interaction with carbonic anhydrase. J Biol Chem 280: 39882-39889,2005.
14. Becker HM, Klier M, Deitmer JW. Nonenzymatic augmentation oflactate transport via monocarboxylate transporter isoform 4 by carbonicanhydrase II. J Membr Biol 234: 125-135, 2010.
15. Belt JA, Thomas JA, Buchsbaum RN, Racker E. Inhibition of lactatetransport and glycolysis in Ehrlich ascites tumor cells by bioflavonoids.Biochemistry 19: 3506-3511, 1979.
16. Bental M, Deutsch C. Metabolic changes in activated T cells: An NMRstudy of human peripheral blood lymphocytes. Magn Reson Med 29:317-326, 1993.
17. Benton CR, Campbell SE, Tonouchi M, Hatta H, Bonen A. Mono-carboxylate transporters in subsarcolemmal and intermyofibrillar mito-chondria. Biochem Biophys Res Commun 323: 249-253, 2004.
18. Benton CR, Yoshida Y, Lally J, Han XX, Hatta H, Bonen A. PGC-1alpha increases skeletal muscle lactate uptake by increasing the expres-sion of MCT1 but not MCT2 or MCT4. Physiol Genomics 35: 45-54,2008.
19. Bergersen L, Waerhaug O, Helm J, Thomas M, Laake P, Davies AJ,Wilson MC, Halestrap AP, Ottersen OP. A novel postsynaptic densityprotein: The monocarboxylate transporter MCT2 is co-localized withdelta-glutamate receptors in postsynaptic densities of parallel fiber-Purkinje cell synapses. Exp Brain Res 136: 523-534, 2001.
20. Bergersen LH. Is lactate food for neurons? Comparison of monocar-boxylate transporter subtypes in brain and muscle. Neuroscience 145:11-19, 2007.
21. Bickham DC, Bentley DJ, LeRossignol PF, CameronSmith D. Theeffects of short-term sprint training on MCT expression in moderatelyendurance-trained runners. Eur J Appl Physiol 96: 636-643, 2006.
1636 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
22. Bigard X, Sanchez H, Zoll J, Mateo P, Rousseau V, Veksler V, Ventu-raClapier R. Calcineurin co-regulates contractile and metabolic com-ponents of slow muscle phenotype. J Biol Chem 275: 19653-19660,2000.
23. Birsoy K, Wang T, Possemato R, Yilmaz OH, Koch CE, Chen WW,Hutchins AW, Gultekin Y, Peterson TR, Carette JE, Brummelkamp TR,Clish CB, Sabatini DM. MCT1-mediated transport of a toxic moleculeis an effective strategy for targeting glycolytic tumors. Nat Genet 45:104-108, 2012.
24. Bogan JS. Regulation of glucose transporter translocation in health anddiabetes. Annu Rev Biochem 81: 507-532, 2012.
25. Bolli R, Nalecz KA, Azzi A. Monocarboxylate and alpha-ketoglutaratecarriers from bovine heart mitochondria - purification by affinitychromatography on immobilized 2-cyano-4-hydroxycinnamate. J BiolChem 264: 18024-18030, 1989.
26. Bonen A. The expression of lactate transporters (MCT1 and MCT4) inheart and muscle. Eur J Appl Physiol 86: 6-11, 2001.
27. Bonen A, McCullagh KJA, Putman CT, Hultman E, Jones NL, Heigen-hauser GJF. Short-term training increases human muscle MCT1 andfemoral venous lactate in relation to muscle lactate. Am J Physiol 274:E102-E107, 1998.
28. Bonen A, Miskovic D, Tonouchi M, Lemieux K, Wilson MC, MaretteA, Halestrap AP. Abundance and subcellular distribution of MCT1 andMCT4 in heart and fast-twitch skeletal muscles. Am J Physiol 278:E1067-E1077, 2000.
29. Bonen A, Tonouchi M, Miskovic D, Heddle C, Heikkila JJ, HalestrapAP. Isoform-specific regulation of the lactate transporters MCT1 andMCT4 by contractile activity. Am J Physiol 279: E1131-E1138, 2000.
30. Brahimi-Horn MC, Bellot G, Pouyssegur J. Hypoxia and energetictumor metabolism. Curr Opin Genet Dev 29: 2570-2578, 2011.
31. Brailsford MA, Thompson AG, Kaderbhai N, Beechey RB. The extrac-tion and reconstitution of the alpha-cyanocinnamate-sensitive pyruvatetransporter from castor bean mitochondria. Biochem Biophys Res Com-mun 140: 1036-1042, 1986.
32. Brauchi S, Rauch MC, Alfaro IE, Cea C, Concha II, Benos DJ, ReyesJG. Kinetics, molecular basis, differentiation of L-lactate transport inspermatogenic cells. Am J Physiol 288: C523-C534, 2005.
33. Bricker DK, Taylor EB, Schell JC, Orsak T, Boutron A, Chen YC, CoxJE, Cardon CM, Van Vranken JG, Dephoure N, Redin C, Boudina S,Gygi SP, Brivet M, Thummel CS, Rutter J. A mitochondrial pyruvatecarrier required for pyruvate uptake in yeast, Drosophila and humans.Science 337: 96-100, 2012.
34. Brivet M, GarciaCazorla A, Lyonnet S, Dumez Y, Nassogne MC, SlamaA, Boutron A, Touati G, Legrand A, Saudubray JM. Impaired mitochon-drial pyruvate importation in a patient and a fetus at risk. Mol GenetMetab 78: 186-192, 2003.
35. Broer S, Broer A, Schneider HP, Stegen C, Halestrap AP, DeitmerJW. Characterization of the high-affinity monocarboxylate transporterMCT2 in Xenopus laevis oocytes. Biochem J 341: 529-535, 1999.
36. Broer S, Rahman B, Pellegri G, Pellerin L, Martin JL, VerleysdonkS, Hamprecht B, Magistretti PJ. Comparison of lactate transport inastroglial cells and monocarboxylate transporter 1 (MCT 1) expressingXenopus laevis oocytes - expression of two different monocarboxylatetransporters in astroglial cells and neurons. J Biol Chem 272: 30096-30102, 1997.
37. Broer S, Schneider HP, Broer A, Rahman B, Hamprecht B, DeitmerJW. Characterization of the monocarboxylate transporter 1 expressedin Xenopus laevis oocytes by changes in cytosolic pH. Biochem J 333:167-174, 1998.
38. Brooks GA. Cell-cell and intracellular lactate shuttles. J Physiol 587:5591-600, 2009.
39. Brooks GA, Brown MA, Butz CE, Sicurello JP, Dubouchaud H. Cardiacand skeletal muscle mitochondria have a monocarboxylate transporterMCT1. J Appl Physiol 87: 1713-1718, 1999.
40. Butz CE, McClelland GB, Brooks GA. MCT1 confirmed in rat striatedmuscle mitochondria. J Appl Physiol 97: 1059-1066, 2004.
41. Cairns SP. Lactic acid and exercise performance : Culprit or friend?Sports Med 36: 279-91, 2006.
42. Canis M, Maurer MH, Kuschinsky W, Duembgen L, Duelli R. Increaseddensities of monocarboxylate transporter MCT1 after chronic hyper-glycemia in rat brain. Brain Res 1257: 32-39, 2009.
43. Carpenter L, Halestrap AP. The kinetics, substrate and inhibitor speci-ficity of the lactate transporter of Ehrlich-Lettre tumor cells studiedwith the intracellular pH indicator BCECF. Biochem J 304: 751-760,1994.
44. Castorino JJ, Deborde S, Deora A, Schreiner R, Gallagher-ColomboSM, Rodriguez-Boulan E, Philp NJ. Basolateral sorting signalsregulating tissue-specific polarity of heteromeric monocarboxylatetransporters in epithelia. Traffic 12: 483-498, 2011.
45. Chen X, Lin J, Kanekura T, Su J, Lin W, Xie H, Wu Y, Li J, ChenM, Chang J. A small interfering CD147-targeting RNA inhibited theproliferation, invasiveness, metastatic activity of malignant melanoma.Cancer Res 66: 11323-11330, 2006.
46. Chenal J, Pellerin L. Noradrenaline enhances the expression of the neu-ronal monocarboxylate transporter MCT2 by translational activation viastimulation of PI3K/Akt and the mTOR/S6K pathway. J Neurochem102: 389-397, 2007.
47. Chenal J, Pierre K, Pellerin L. Insulin and IGF-1 enhance the expres-sion of the neuronal monocarboxylate transporter MCT2 by transla-tional activation via stimulation of the phosphoinositide 3-kinase-Akt-mammalian target of rapamycin pathway. Eur J Neurosci 27: 53-65,2008.
48. Cheng C, Edin NF, Lauritzen KH, Aspmodal I, Christoffersen S, JianL, Rasmussen LJ, Pettersen EO, Xiaoqun G, Bergersen LH. Alterationsof monocarboxylate transporter densities during hypoxia in brain andbreast tumor cells. Cell Oncol (Dordr) 35: 217-227, 2012.
49. Chiche J, Lefur Y, Vilmen C, Frassineti F, Daniel L, Halestrap AP,Cozzone PJ, Pouyssegur J, Lutz NW. In vivo pH in metabolic-defectiveRas-transformed fibroblast tumors. Key role of the monocarboxylatetransporter, MCT4, for inducing an alkaline intracellular pH. Int JCancer 130: 1511-1520, 2011.
50. Chiry O, Fishbein WN, Merezhinskaya N, Clarke S, Galuske R, Mag-istretti PJ, Pellerin L. Distribution of the monocarboxylate transporterMCT2 in human cerebral cortex: An immunohistochemical study.Brain Res 1226: 61-69, 2008.
51. Chiry O, Pellerin L, MonnetTschudi F, Fishbein WN, MerezhinskayaN, Magistretti PJ, Clarke S. Expression of the monocarboxylate trans-porter MCT1 in the adult human brain cortex. Brain Res 1070: 65-70,2006.
52. Clarke SJ, Khaliulin I, Das M, Parker JE, Heesom KJ, Halestrap AP.Inhibition of mitochondrial permeability transition pore opening byischemic preconditioning is probably mediated by reduction of oxida-tive stress rather than mitochondrial protein phosphorylation. Circ Res102: 1082-1090, 2008.
53. Coady MJ, Chang MH, Charron FM, Plata C, Wallendorff B, Sah JF,Markowitz SD, Romero MF, Lapointe JY. The human tumor suppres-sor gene SLC5A8 expresses a Na+-monocarboxylate cotransporter.J Physiol 557: 719-731, 2004.
54. Coleman ML, Ratcliffe PJ. Oxygen sensing and hypoxia-inducedresponses. Essays Biochem 43: 1-15, 2007.
55. Coles L, Litt J, Hatta H, Bonen A. Exercise rapidly increases expressionof the monocarboxylate transporters MCT1 and MCT4 in rat muscle.J Physiol 561: 253-261, 2004.
56. Coothankandaswamy V, Elangovan S, Singh N, Prasad PD, ThangarajuM, Ganapathy V. The plasma membrane transporter SLC5A8 sup-presses tumor progression through depletion of survivin without involv-ing its transport function. Biochem J 450: 169-178, 2013.
57. Crosnier C, Bustamante LY, Bartholdson SJ, Bei AK, Theron M,Uchikawa M, Mboup S, Ndir O, Kwiatkowski DP, Duraisingh MT,Rayner JC, Wright GJ. Basigin is a receptor essential for erythrocyteinvasion by Plasmodium falciparum. Nature 480: 534-537, 2011.
58. Cross SH, Bird AP. CpG islands and genes. Curr Opin Genet Dev 5:309-314, 1995.
59. Cuff M, Dyer J, Jones M, ShirazBeechey S. The human colonic mono-carboxylate transporter isoform 1: Its potential importance to colonictissue Homeostasis. Gastroenterology 128: 676-686, 2005.
60. Dang S, Sun L, Huang Y, Lu F, Liu Y, Gong H, Wang J, Yan N.Structure of a fucose transporter in an outward-open conformation.Nature 467: 734-738, 2010.
61. Daniele LL, Sauer B, Gallagher SM, Pugh ENJr, Philp NJ. Alteredvisual function in monocarboxylate transporter 3 (Slc16a8) knockoutmice. Am J Physiol 295: C451-7, 2008.
62. De Bruijne AW, Vreeberg H, Van Steveninck J. Kinetic analysis ofL-lactate transport in human erythrocytes via the monocarboxylate-specific carrier system. Biochim Biophys Acta 732: 562-568, 1983.
63. De Bruijne AW, Vreeberg H, Van Steveninck J. Alternative substrateinhibition of L-lactate transport via the monocarboxylate-specific car-rier system in human erythrocytes. Biochim Biophys Acta 812: 841-844,1985.
64. De Saedeleer CJ, Copetti T, Porporato PE, Verrax J, Feron O, SonveauxP. Lactate activates HIF-1 in oxidative but not in Warburg-phenotypehuman tumor cells. PLoS One 7: e46571, 2012.
65. Denton RM, Halestrap AP. Regulation of pyruvate metabolism in mam-malian tissues. Essays Biochem 15: 37-47, 1979.
66. Deora AA, Philp N, Hu J, Bok D, Rodriguez-Boulan E. Mechanismsregulating tissue-specific polarity of monocarboxylate transporters andtheir chaperone CD147 in kidney and retinal epithelia. Proc Natl AcadSci U S A 102(45): 16245-16250, 2005.
67. Deuticke B. Monocarboxylate transport in erythrocytes. J Membr Biol70: 89-103, 1982.
68. Deuticke B, Beyer E, Forst B. Discrimination of three parallel pathwaysof L-lactate transport in the human erythrocyte membrane by inhibitorsand kinetic properties. Biochim Biophys Acta 684: 96-110, 1982.
69. Deuticke B, Rickert I, Beyer E. Stereoselective, SH-dependent transferof lactate in human erythrocytes. Biochim Biophys Acta 507: 137-155,1978.
Volume 3, October 2013 1637

Monocarboxylic Acid Transport Comprehensive Physiology
70. Dhup S, Dadhich RK, Porporato PE, Sonveaux P. Multiple biologicalactivities of lactic acid in cancer: Influences on tumor growth, angio-genesis and metastasis. Curr Pharm Des 18: 1319-1330, 2012.
71. Dimmer KS, Friedrich B, Lang F, Deitmer JW, Broer S. The low-affinity monocarboxylate transporter MCT4 is adapted to the export oflactate in highly glycolytic cells. Biochem J 350: 219-227, 2000.
72. Divakaruni AS, Murphy AN. Cell biology. A mitochondrial mystery,solved. Science 337: 41-43, 2012.
73. Donovan JA, Jennings ML. Membrane polypeptide in rabbit erythro-cytes associated with the inhibition of L-lactate transport by a syntheticanhydride of lactic acid. Biochemistry 24: 561-564, 1985.
74. Donovan JA, Jennings ML. N-Hydroxysulphosuccinimido active estersand the L-(+)-lactate transport protein in rabbit erythrocytes. Biochem-istry 25: 1538-1545, 1986.
75. Dubinsky WP, Racker E. The mechanism of lactate transport in humanerythrocytes. J Membr Biol 44: 25-36, 1978.
76. Edlund GL, Halestrap AP. The kinetics of transport of lactate andpyruvate into rat hepatocytes. Evidence for the presence of a spe-cific carrier similar to that in erythrocytes. Biochem J 249: 117-126,1988.
77. Ekberg H, Qi Z, Pahlman C, Veress B, Bundick RV, Craggs RI, HolnessE, Edwards S, Murray CM, Ferguson D, Kerry PJ, Wilson E, DonaldDK. The specific monocarboxylate transporter-1 (MCT-1) inhibitor,AR-C117977, induces donor-specific suppression, reducing acute andchronic allograft rejection in the rat. Transplantation 84: 1191-1199,2007.
78. Enoki T, Yoshida Y, Hatta H, Bonen A. Exercise training alleviatesMCT1 and 4 reductions in heart and skeletal muscles of STZ-induceddiabetic rats. J Appl Physiol 94: 2433-2438, 2003.
79. Evertsen F, Medbo JI, Bonen A. Effect of training intensity on musclelactate transporters and lactate threshold of cross-country skiers. ActaPhysiol Scand 173: 195-205, 2001.
80. Fang J, Quinones QJ, Holman TL, Morowitz MJ, Wang Q, Zhao H,Sivo F, Maris JM, Wahl ML. The H+-linked monocarboxylate trans-porter (MCT1/SLC16A1): A potential therapeutic target for high-riskneuroblastoma. Mol Pharmacol 70: 2108-2115, 2006.
81. Fishbein WN. Lactate transporter defect: A new disease of muscle.Science 234: 1254-1256, 1986.
82. Fishbein WN, Merezhinskaya N, Foellmer JW. Relative distributionof three major lactate transporters in frozen human tissues and theirlocalization in unfixed skeletal muscle. Muscle Nerve 26: 101-112,2002.
83. Frank H, Groger N, Diener M, Becker C, Braun T, Boettger T. Lac-taturia and loss of sodium-dependent lactate uptake in the colon ofSLC5A8-deficient mice. J Biol Chem 283: 24729-24737, 2008.
84. Friesema ECH, Ganguly S, Abdalla A, Fox JEM, Halestrap AP, VisserTJ. Identification of monocarboxylate transporter 8 as a specific thyroidhormone transporter. J Biol Chem 278: 40128-40135, 2003.
85. Furugen A, Kobayashi M, Narumi K, Watanabe M, Otake S, ItagakiS, Iseki K. AMP-activated protein kinase regulates the expression ofmonocarboxylate transporter 4 in skeletal muscle. Life Sci 88: 163-168,2011.
86. Galardo MN, Riera MF, Pellizzari EH, Cigorraga SB, Meroni SB.The AMP-activated protein kinase activator, 5-aminoimidazole-4-carboxamide-1-b-D-ribonucleoside, regulates lactate production in ratSertoli cells. J Mol Endocrinol 39: 279-288, 2007.
87. Galic S, Schneider HP, Broer A, Deitmer JW, Broer S. The loopbetween helix 4 and helix 5 in the monocarboxylate transporter MCT1is important for substrate selection and protein stability. Biochem J 376:413-422, 2003.
88. Gallagher-Colombo S, Maminishkis A, Tate S, Grunwald GB, PhilpNJ. Modulation of MCT3 expression during wound healing of theretinal pigment epithelium. Invest Ophthalmol Vis Sci 51: 5343-5350,2010.
89. Gallagher SM, Castorino JJ, Wang D, Philp NJ. Monocarboxylate trans-porter 4 regulates maturation and trafficking of CD147 to the plasmamembrane in the metastatic breast cancer cell line MDA-MB-231. Can-cer Res 67: 4182-9, 2007.
90. Ganapathy V, Thangaraju M, Gopal E, Martin P, Itagaki S, MiyauchiS, Prasad P. Sodium-coupled monocarboxylate transporters in normaltissues and in cancer. AAPS J. 10: 193-199, 2008.
91. Garcia CK, Brown MS, Pathak RK, Goldstein JL. cDNA cloning ofMCT2, a second monocarboxylate transporter expressed in differentcells than MCT1. J Biol Chem 270: 1843-1849, 1995.
92. Gerhart DZ, Enerson BE, Zhdankina OY, Leino RL, Drewes LR.Expression of monocarboxylate transporter MCT1 by brain endothe-lium and glia in adult and suckling rats. Am J Physiol 273: E207-E213,1997.
93. Gerhart DZ, Leino RL, Drewes LR. Distribution of monocarboxylatetransporters MCT1 and MCT2 in rat retina. Neuroscience 92: 367-375,1999.
94. Gill RK, Saksena S, Alrefai WA, Sarwar Z, Goldstein JL, Carroll RE,Ramaswamy K, Dudeja PK. Expression and membrane localization of
MCT isoforms along the length of the human intestine. Am J Physiol289: C846-C852, 2005.
95. Gingras A-C, Raught B, Sonenberg N. eIF4 initiation factors: Effectorsof mRNA recruitment to ribosomes and regulators of translation. AnnuRev Biochem 68: 913-963, 1999.
96. Gopal E, Fei YJ, Sugawara M, Miyauchi S, Zhuang L, Martin P, SmithSB, Prasad PD, Ganapathy V. Expression of slc5a8 in kidney and its rolein Na(+)-coupled transport of lactate. J Biol Chem 279: 44522-44532,2004.
97. Gopal E, Miyauchi S, Martin PM, Ananth S, Roon P, Smith SB, Gana-pathy V. Transport of nicotinate and structurally related compounds byhuman SMCT1 (SLC5A8) and its relevance to drug transport in themammalian intestinal tract. Pharm Res 24: 575-584, 2007.
98. Gopal E, Umapathy NS, Martin PM, Ananth S, Gnana-Prakasam JP,Becker H, Wagner CA, Ganapathy V, Prasad PD. Cloning and func-tional characterization of human SMCT2 (SLC5A12) and expressionpattern of the transporter in kidney. Biochim Biophys Acta 1768: 2690-2697, 2007.
99. Green H, Halestrap A, Mockett C, OToole D, Grant S, Ouyang J.Increases in muscle MCT are associated with reductions in musclelactate after a single exercise session in humans. Am J Physiol 282:E154-E160, 2002.
100. Greiner EF, Guppy M, Brand K. Glucose is essential for prolifera-tion and the glycolytic enzyme induction that provokes a transition toglycolytic energy production. J Biol Chem 269: 31484-31490, 1994.
101. Grollman EF, Philp NJ, McPhie P, Ward RD, Sauer B. Determinationof transport kinetics of chick MCT3 monocarboxylate transporter fromretinal pigment epithelium by expression in genetically modified yeast.Biochemistry 39: 9351-9357, 2000.
102. Guan L, Mirza O, Verner G, Iwata S, Kaback HR. Structural determi-nation of wild-type lactose permease. Proc Natl Acad Sci U S A 104:15294-15298, 2007.
103. Guenette RS, Sridhar S, Herley M, Mooibroek M, Wong P, TenniswoodM. Embigin, a developmentally expressed member of the immunoglob-ulin super family is also expressed during regression of prostate andmammary gland. Dev Genet 21: 268-278, 1997.
104. Guile SD, Banticka JR, Cheshire DR, Cooper ME, Davis AM, Don-ald DK, Evans R, Eyssade C, Ferguson DD, Hill S, Hutchinson R,Ingall AH, Kingston LP, Martin I, Martin BP, Mohammed RT, MurrayC, Perry MWD, Reynolds RH, Thorne PV, Wilkinson DJ, WithnallJ. Potent blockers of the monocarboxylate transporter MCT1: Novelimmunomodulatory compounds. Bioorg Medl Chem Lett 16: 2260-2265, 2006.
105. Guppy M, Greiner E, Brand K. The role of the Crabtree effect and anendogenous fuel in the energy metabolism of resting and proliferatingthymocytes. Eur J Biochem 212: 95-99, 1993.
106. Gupta N, Martin PM, Prasad PD, Ganapathy V. SLC5A8 (SMCT1)-mediated transport of butyrate forms the basis for the tumor suppressivefunction of the transporter. Life Sci 78: 2419-2425, 2006.
107. Hajduch E, Heyes RR, Watt PW, Hundal HS. Lactate transport in ratadipocytes: Identification of monocarboxylate transporter 1 (MCT1)and its modulation during streptozotocin-induced diabetes. FEBS Lett479: 89-92, 2000.
108. Halestrap AP. The mitochondrial pyruvate carrier - kinetics and speci-ficity for substrates and inhibitors. Biochem J 148: 85-96, 1975.
109. Halestrap AP. The mechanism of the inhibition of the mitochondrialpyruvate transporter by α-cyanocinnamate derivatives. Biochem J 156:181-183, 1976.
110. Halestrap AP. Pyruvate and lactate transport into human erythrocytes.Evidence for the involvement of the chloride carrier and a chlorideindependent carrier. Biochem J 156: 193-207, 1976.
111. Halestrap AP. Pyruvate and ketone-body transport across the mitochon-drial membrane: Exchange properties, pH-dependence and mechanismof the carrier. Biochem J 172: 377-387, 1978.
112. Halestrap AP. The monocarboxylate transporter family-structure andfunctional characterization. IUBMB Life 64: 1-9, 2012.
113. Halestrap AP. The mitochondrial pyruvate carrier: Has it beenunearthed at last? Cell Metab 16: 141-143, 2012.
114. Halestrap AP. The SLC16 gene family structure, role and regulation inhealth and disease. Mol Aspects Med 34: 337-349, 2013.
115. Halestrap AP, Brand MD, Denton RM. Inhibition of mitochondrialpyruvate transport by phenylpyruvate and α-keto-isocaproate. BiochimBiophys Acta 367: 102-108, 1974.
116. Halestrap AP, Denton RM. Specific inhibition of pyruvate trans-port in rat liver mitochondria and human erythrocytes by α-cyano-4-hydroxycinnamate. Biochem J 138: 313-316, 1974.
117. Halestrap AP, Denton RM. The specificity and metabolic implicationsof the inhibition of pyruvate transport in isolated mitochondria andintact preparations by α-cyano-4-hydroxycinnamate and related com-pounds. Biochem J 148: 97-106, 1975.
118. Halestrap AP, Meredith D. The SLC16 gene family - from monocar-boxylate transporters (MCTs) to aromatic amino acid transporters andbeyond. Pflugers Arch 447: 619-628, 2004.
1638 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
119. Halestrap AP, Price NT. The proton-linked monocarboxylate trans-porter (MCT) family: Structure, function and regulation. Biochem J343: 281-299, 1999.
120. Halestrap AP, Scott RD, Thomas AP. Mitochondrial pyruvate transportand its hormonal regulation. Int J Biochem 11: 97-105, 1980.
121. Halestrap AP, Wang XM, Poole RC, Jackson VN, Price NT. Lactatetransport in heart in relation to myocardial ischemia. Am J Cardiol 80:A17-A25, 1997.
122. Halestrap AP, Wilson MC. The monocarboxylate transporter family-role and regulation. IUBMB Life 64: 109-119, 2012.
123. Hamann S, Kiilgaard JF, laCour M, Prause JU, Zeuthen T. Cotransportof H+, lactate, H2O in porcine retinal pigment epithelial cells. Exp EyeRes 76: 493-504, 2003.
124. Hanna SM, Kirk P, Holt OJ, Puklavec MJ, Brown MH, Barclay AN. Anovel form of the membrane protein CD147 that contains an extraIg-like domain and interacts homophilically. BMC Biochem 4: 17,2003.
125. Harris T, Eliyahu G, Frydman L, Degani H. Kinetics of hyperpolarized13C1-pyruvate transport and metabolism in living human breast cancercells. Proc Natl Acad Sci USA 106: 18131-18136, 2009.
126. Hashimoto T, Hussien R, Brooks GA. Colocalization of MCT1, CD147,LDH in mitochondrial inner membrane of L6 muscle cells: Evidence ofa mitochondrial lactate oxidation complex. Am J Physiol 290: E1237-E1244, 2006.
127. Hashimoto T, Hussien R, Cho HS, Kaufer D, Brooks GA. Evidence forthe mitochondrial lactate oxidation complex in rat neurons: Demon-stration of an essential component of brain lactate shuttles. PLoS ONE3: e2915, 2008.
128. Hatta H, Tonouchi M, Miskovic D, Wang YX, Heikkila JJ, BonenA. Tissue-specific and isoform-specific changes in MCT1 and MCT4in heart and soleus muscle during a 1-yr period. Am J Physiol 281:E749-E756, 2001.
129. Heesom KJ, Gampel A, Mellor H, Denton RM. Cell cycle-dependentphosphorylation of the translational repressor eIF-4E binding protein-1(4E-BP1). Curr Biol 11: 1374-1379, 2001.
130. Helm J, Coppola D, Ganapathy V, Lloyd M, Centeno BA, Chen DT,Malafa MP, Park JY. SLC5A8 nuclear translocation and loss of expres-sion are associated with poor outcome in pancreatic ductal adenocarci-noma. Pancreas 41: 904-909, 2012.
131. Herzig S, Raemy E, Montessuit S, Veuthey JL, Zamboni N, West-ermann B, Kunji ER, Martinou JC. Identification and functionalexpression of the mitochondrial pyruvate carrier. Science 337: 93-96,2012.
132. Hildmann B, Storelli C, Haase W, Barac-Nieto M, Murer H. Sodiumion/L-lactate co-transport in rabbit small intestine brush border mem-brane vesicles. Biochem J 186: 169-176, 1980.
133. Hildyard JCW, Ammala C, Dukes ID, Thomson SA, Halestrap AP.Identification and characterisation of a new class of highly specificand potent inhibitors of the mitochondrial pyruvate carrier. BiochimBiophys Acta 1707: 221-230, 2005.
134. Hildyard JCW, Halestrap AP. Identification of the mitochondrial pyru-vate carrier in Saccharomyces cerevisiae. Biochem J 374: 607-611,2003.
135. Hollingsworth KG, Newton JL, Robinson L, Taylor R, Blamire AM,Jones DE. Loss of capacity to recover from acidosis in repeat exercise isstrongly associated with fatigue in primary biliary cirrhosis. J Hepatol53: 155-161, 2010.
136. Huang YF, Lemieux MJ, Song JM, Auer M, Wang DN. Structure andmechanism of the glycerol-3-phosphate transporter from Escherichiacoli. Science 301: 616-620, 2003.
137. Hugo SE, Cruz-Garcia L, Karanth S, erson RM, Stainier DY, SchlegelA. A monocarboxylate transporter required for hepatocyte secretion ofketone bodies during fasting. Genes Dev 26: 282-293, 2012.
138. Hutson SM, Hall TR. Identification of the mitochondrial branched chainaminotransferase as a branched chain alpha-keto acid transport protein.J Biol Chem 268: 3084-3091, 1993.
139. Hutson SM, Rannels SL. Characterisation of a mitochondrial transportsystem for branched chain α-keto acids. J Biol Chem 260: 14189-14193, 1985.
140. Hutson SM, Roten S, Kaplan RS. solubilization and functional reconsti-tution of the branched-chain alpha-keto acid transporter from rat heartmitochondria. Proc Natl Acad Sci U S A 87: 1028-1031, 1990.
141. Iacono KT, Brown AL, Greene MI, Saouaf SJ. CD147 immunoglobulinsuperfamily receptor function and role in pathology. Exp Mol Pathol83: 283-295, 2007.
142. Igakura T, Kadomatsu K, Kaname T, Muramatsu H, Fan Q-WF,Miyauchi T, Toyama Y, Kuno N, Yuasa S, Takahashi M, Takao S,Taguchi O, Yamamura K, Arimura K, Muramatsu T. A Null muta-tion in basigin, an immunoglobulin superfamily member, indicates itsimportant roles in peri-implantation development and spermatogenesis.Dev Biol 194: 152-165, 1998.
143. Iwanaga T, Takebe K, Kato I, Karaki S, Kuwahara A. Cellular expres-sion of monocarboxylate transporters (MCT) in the digestive tract of
the mouse, rat, humans, with special reference to slc5a8. Biomed Res27: 243-254, 2006.
144. Jackson VN, Halestrap AP. The kinetics, substrate, inhibitor specificityof the monocarboxylate (lactate) transporter of rat liver cells determinedusing the fluorescent intracellular pH indicator, 2′,7′-bis(carboxyethyl)-5(6)-carboxyfluorescein. J Biol Chem 271: 861-868, 1996.
145. Jackson VN, Price NT, Carpenter L, Halestrap AP. Cloning of themonocarboxylate transporter isoform MCT2 from rat testis providesevidence that expression in tissues is species-specific and may involvepost-transcriptional regulation. Biochem J 324: 447-453, 1997.
146. Jang C, Lee G, Chung J. LKB1 induces apical trafficking of Silnoon, amonocarboxylate transporter, in Drosophila melanogaster. J Cell Biol183: 11-17, 2008.
147. Jansen S, Esmaeilpour T, Pantaleon M, Kaye PL. Glucose affects mono-carboxylate cotransporter (MCT) 1 expression during mouse preim-plantation development. Reproduction 131: 469-479, 2006.
148. Johannsson E, Lunde PK, Heddle C, Sjaastad I, Thomas MJ, BergersenL, Halestrap AP, Blackstad TW, Ottersen OP, Sejersted OM. Upregu-lation of the cardiac monocarboxylate transporter MCT1 in a rat modelof congestive heart failure. Circulation 104: 729-734, 2001.
149. Johnson JH, Belt JA, Dubinsky WP, Zimniak A, Racker E. Inhibition oflactate transport in Ehrlich ascites tumor cells and human erythrocytesby a synthetic anhydride of lactic acid. Biochemistry 19: 3836-3840,1980.
150. Jorgensen KE, Sheikh MI. Renal transport of monocarboxylic acids:Heterogeneity of lactate transport systems along the proximal tubule.Biochem 223: 803-807, 1984.
151. Jorgensen KE, Sheikh MI. Transport of pyruvate by luminal membranevesicles from pars convoluta and pars recta of rabbit proximal tubule.Biochim Biophys Acta 938: 345-352, 1988.
152. Juel C. Current aspects of lactate exchange: Lactate/H+ transport inhuman skeletal muscle. Eur J App Physiol 86: 12-16, 2001.
153. Juel C. Training-induced changes in membrane transport proteins ofhuman skeletal muscle. Eur J App Physiol 96: 627-635, 2006.
154. Juel C, Halestrap AP. Lactate transport in skeletal muscle - role andregulation of the monocarboxylate transporter. J Physiol 517: 633-642,1999.
155. Juel C, Klarskov C, Nielsen JJ, Krustrup P, Mohr M, Bangsbo J. Effectof high-intensity intermittent training on lactate and H+ release fromhuman skeletal muscle. Am J Physiol 286: E245-E251, 2004.
156. Kaelin WGJr, Thompson CB. Q&A: Cancer: Clues from cellmetabolism. Nature 465: 562-564, 2010.
157. Kim CM, Goldstein JL, Brown MS. cDNA cloning of MEV, a mutantprotein that facilitates cellular uptake of mevalonate, identification ofa point mutation responsible for its gain in function. J Biol Chem 267:23113-23121, 1992.
158. Kim DK, Kanai Y, Matsuo H, Kim JY, Chairoungdua A, KobayashiY, Enomoto A, Cha SH, Goya T, Endou H. The human T-type aminoacid transporter-1: Characterization, gene organization, chromosomallocation. Genomics 79: 95-103, 2002.
159. Kim-Garcia C, Goldstein JL, Pathak RK, erson RGW, Brown MS.Molecular characterization of a membrane transporter for lactate, pyru-vate, other monocarboxylates - implications for the Cori cycle. Cell 76:865-873, 1994.
160. Kirk P, Wilson MC, Heddle C, Brown MH, Barclay AN, Halestrap AP.CD147 is tightly associated with lactate transporters MCT1 and MCT4and facilitates their cell surface expression. EMBO J 19: 3896-3904,2000.
161. Klier M, Schuler C, Halestrap AP, Sly WS, Deitmer JW, BeckerHM. Transport activity of the high-affinity monocarboxylate transporterMCT2 is enhanced by extracellular carbonic anhydrase IV but not byintracellular carbonic anhydrase II. J Biol Chem 286: 27781-27791,2011.
162. Krishnan MN, Ng A, Sukumaran B, Gilfoy FD, Uchil PD, SultanaH, Brass AL, Adametz R, Tsui M, Qian F, Montgomery RR, Lev S,Mason PW, Koski RA, Elledge SJ, Xavier RJ, Agaisse H, Fikrig E.RNA interference screen for human genes associated with West Nilevirus infection. Nature 455: 242-245, 2008.
163. Kroemer G, Pouyssegur J. Tumor cell metabolism: Cancer’s achilles’heel. Cancer Cell 13: 472-482, 2008.
164. Land JM, Clark JB. Inhibition of pyruvate and beta-hydroxybutyrateoxidation in rat brain mitochondria by phenylpyruvate and alpha-ketoisocaproate. FEBS Lett 44, 348-351, 1974.
165. Le Floch R, Chiche J, Marchiq I, Naiken T, Ilk K, Murray CM,Critchlow SE, Roux D, Simon MP, Pouyssegur J. CD147 subunit oflactate/H+ symporters MCT1 and hypoxia-inducible MCT4 is criticalfor energetics and growth of glycolytic tumors. Proc Natl Acad Sci US A 108: 16663-16668, 2011.
166. Lee WJ, Kim M, Park HS, Kim HS, Jeon MJ, Oh KS, Koh EH, WonJC, Kim MS, Oh GT, Yoon M, Lee KU, Park JY. AMPK activationincreases fatty acid oxidation in skeletal muscle by activating PPA-Ralpha and PGC-1. Biochem Biophys Res Commun 340: 291-295,2006.
Volume 3, October 2013 1639

Monocarboxylic Acid Transport Comprehensive Physiology
167. Lee Y, Morrison BM, Li Y, Lengacher S, Farah MH, Hoffman PN,Liu Y, Tsingalia A, Jin L, Zhang PW, Pellerin L, Magistretti PJ, Roth-stein JD. Oligodendroglia metabolically support axons and contributeto neurodegeneration. Nature 487: 443-448, 2012.
168. Leeks DR, Halestrap AP. Chloride-independent transport of pyruvateand lactate across the erythrocyte membrane. Biochem Soc Trans 6:1363-1366, 1978.
169. Leino RL, Gerhart DZ, Drewes LR. Monocarboxylate transporter(MCT1) abundance in brains of suckling and adult rats: A quanti-tative electron microscopic immunogold study. Developmental BrainResearch 113: 47-54, 1999.
170. Leino RL, Gerhart DZ, Duelli R, Enerson BE, Drewes LR. Diet-inducedketosis increases monocarboxylate transporter (MCT1) levels in ratbrain. Neurochem Int 38: 519-527, 2001.
171. Li H, Myeroff L, Smiraglia D, Romero MF, Pretlow TP, Kasturi L,Lutterbaugh J, Rerko RM, Casey G, Issa JP, Willis J, Willson JK, PlassC, Markowitz SD. SLC5A8, a sodium transporter, is a tumor suppressorgene silenced by methylation in human colon aberrant crypt foci andcancers. Proc Natl Acad Sci U S A 100: 8412-8417, 2003.
172. Lin HY, Park HY, Radlein S, Mahajan NP, Sellers TA, Zachariah B,Pow-Sang J, Coppola D, Ganapathy V, Park JY. Protein expressionsand genetic variations of SLC5A8 in prostate cancer risk and aggres-siveness. Urology 78: 971.e1-9, 2011.
173. Lin J, Wu H, Tarr PT, Zhang CY, Wu Z, Boss O, Michael LF, PuigserverP, Isotani E, Olson EN, Lowell BB, Bassel-Duby R, Spiegelman BM.Transcriptional co-activator PGC-1 alpha drives the formation of slow-twitch muscle fibres. Nature 418: 797-801, 2002.
174. Lin RY, Vera JC, Chaganti RSK, Golde DW. Human monocarboxylatetransporter 2 (MCT2) is a high affinity pyruvate transporter. J BiolChem 273: 28959-28965, 1998.
175. MacDonald PM. Translational control: A cup half full. Curr Biol 14:R282-R283, 2004.
176. Manning Fox JE, Meredith D, Halestrap AP. Characterisation of humanmonocarboxylate transporter 4 substantiates its role in lactic acid effluxfrom skeletal muscle. J Physiol 529: 285-293, 2000.
177. Mannowetz N, Wandernoth P, Wennemuth G. Basigin interacts withboth MCT1 and MCT2 in murine spermatozoa. J Cell Physiol 227:2154-2162, 2012.
178. Manoharan C, Wilson MC, Sessions RB, Halestrap AP. The role ofcharged residues in the transmembrane helices of monocarboxylatetransporter 1 and its ancillary protein basigin in determining plasmamembrane expression and catalytic activity. Mol Membr Biol 23: 486-498, 2006.
179. Martin PM, Dun Y, Mysona B, Ananth S, Roon P, Smith SB, Ganapa-thy V. Expression of the sodium-coupled monocarboxylate transportersSMCT1 (SLC5A8) and SMCT2 (SLC5A12) in retina. Invest Ophthal-mol Vis Sci 48: 3356-3363, 2007.
180. Martin PM, Gopal E, Ananth S, Zhuang L, Itagaki S, Prasad BM,Smith SB, Prasad PD, Ganapathy V. Identity of SMCT1 (SLC5A8)as a neuron-specific Na+-coupled transporter for active uptake ofL-lactate and ketone bodies in the brain. J Neurochem 98: 279-288,2006.
181. Mason MJ, Thomas RC. A microelectrode study of the mechanisms ofL-lactate entry into and release from frog sartorius muscle. J Physiol400: 459-479, 1988.
182. Matsuyama S, Ohkura S, Iwata K, Uenoyama Y, Tsukamura H, MaedaK, Kimura K. Food deprivation induces monocarboxylate transporter 2expression in the brainstem of female rat. J Reprod Dev 55: 256-261,2009.
183. Mccullagh KJA, Bonen A. Reduced lactate transport in denervated ratskeletal muscle. Am J Physiol 268: R884-R888, 1995.
184. McCullagh KJA, Poole RC, Halestrap AP, Tipton KF, OBrien M, BonenA. Chronic electrical stimulation increases MCT1 and lactate uptake inred and white skeletal muscle. Am J Physiol 273: E239-E246, 1997.
185. Mendes-Mourao J, Halestrap AP, Crisp DM, Pogson CI. The involve-ment of mitochondrial pyruvate transport in the pathways of gluconeo-genesis from serine and alanine in isolated rat and mouse liver cells.FEBS Lett 53: 29-32, 1975.
186. Mendez R, Richter JD. Translational control by CPEB: A means to theend. Nat Rev Mol Cell Biol 2: 521-529, 2001.
187. Mengual R, Claudeschlageter MH, Poiree JC, Yagello M, Sudaka P.Characterization of sodium and pyruvate interactions of the 2 carriersystems specific of monocarboxylic and dicarboxylic or tricarboxylicacids by renal brush-border membrane vesicles. J Membr Biol 108:197-205, 1989.
188. Mengual R, Leblanc G, Sudaka P. The mechanism of Na-L-lactatecotransport by brush border membrane vesicles from horse kidney:Analysis by isotopic exchange kinetics of a sequential model and stoi-chiometry. J Biol Chem 258: 15071-15078, 1983.
189. Mengual R, Schlageter MH, Sudaka P. Kinetic asymmetry of renalNa+-L-lactate cotransport - characteristic parameters and evidence fora ping pong mechanism of the trans-stimulating exchange by pyruvate.J Biol Chem 265: 292-299, 1990.
190. Mengual R, Sudaka P. The mechanism of Na-lactate co-transport bybrush border membrane vesicles from horse kidney; analysis of rapidequilibrium kinetics in absence of membrane potential. J Membr Biol71: 163-171, 1983.
191. Meredith D, Bell P, McClure B, Wilkins R. Functional and molecularcharacterisation of lactic acid transport in bovine articular chondro-cytes. Cell Physiol Biochem 12: 227-234, 2002.
192. Meredith D, Christian HC. The SLC16 monocaboxylate transporterfamily. Xenobiotica 38: 1072-1106, 2008.
193. Merezhinskaya N, Fishbein WN, Davis JI, Foellmer JW. Mutationsin MCT1 cDNA in patients with symptomatic deficiency in lactatetransport. Muscle & Nerve 23: 90-97, 2000.
194. Miyauchi S, Gopal E, Fei YJ, Ganapathy V. Functional identificationof SLC5A8, a tumor suppressor down-regulated in colon cancer, as aNa(+)-coupled transporter for short-chain fatty acids. J Biol Chem 279:13293-6, 2004.
195. Moreira TJ, Pierre K, Maekawa F, Repond C, Cebere A, Liljequist S,Pellerin L. Enhanced cerebral expression of MCT1 and MCT2 in arat ischemia model occurs in activated microglial cells. J Cereb BloodFlow Metab 29: 1273-1283, 2009.
196. Moschen I, Broer A, Galic S, Lang F, Broer S. Significance of shortchain fatty acid transport by members of the Monocarboxylate Trans-porter Family (MCT). Neurochem Res 37: 2562-2568, 2012.
197. Murakami Y, Kohyama N, Kobayashi Y, Ohbayashi M, Ohtani H,Sawada Y, Yamamoto T. Functional characterization of human mono-carboxylate transporter 6 (SLC16A5). Drug Metab Dispos 33: 1845-1851, 2005.
198. Muramatsu T, Miyauchi T. Basigin (CD147): A multifunctionaltransmembrane protein involved in reproduction, neural function,inflammation and tumor invasion. Histol Histopathol 18: 981-987,2003.
199. Murer H, Berckhardt G. Membrane transport of anions across epithe-lia of mammalian intestine and kidney proximal tubules. Rev PhysiolBiochem Pharmacol 96: 1-51, 1983.
200. Murray CM, Hutchinson R, Bantick JR, Belfield GP, Benjamin AD,Brazma D, Bundick RV, Cook ID, Craggs RI, Edwards S, Evans LR,Harrison R, Holness E, Jackson AP, Jackson CG, Kingston LP, PerryMWD, Ross ARJ, Rugman PA, Sidhu SS, Sullivan M, TaylorFishwickDA, Walker PC, Whitehead YM, Wilkinson DJ, Wright A, Donald DK.Monocarboxylate transporter MCT1 is a target for immunosuppression.Nat Chem Biol 1: 371-376, 2005.
201. Nabeshima K, Iwasaki H, Koga K, Hojo H, Suzumiya J, Kikuchi M.Emmprin (Basigin/CD147): Matrix metalloproteinase modulator andmultifunctional cell recognition molecule that plays a critical role incancer progression. Pathol Int 56: 359-367, 2006.
202. Nalecz KA, Bolli R, Wojtczak L, Azzi A. The monocarboxylate carrierfrom bovine heart mitochondria: Partial purification and its substrate-transporting properties in a reconstituted system. Biochim Biophys Acta851: 29-37, 1986.
203. Newstead S, Drew D, Cameron AD, Postis VL, Xia X, Fowler PW,Ingram JC, Carpenter EP, Sansom MS, McPherson MJ, Baldwin SA,Iwata S. Crystal structure of a prokaryotic homologue of the mammalianoligopeptide-proton symporters, PepT1 and PepT2. EMBO J 30: 417-426, 2011.
204. Nord E, Wright SH, Kippen I, Wright EM. Pathways for monocar-boxylic acid transport by rabbit renal brush border membrane vesicles.Am J Physiol 243: F456-F462, 1982.
205. Nord EP, Wright SH, Kippen I, Wright EM. Specificity of the Na-dependent momcarboxylic acid transport pathway in rabbit renal brushborder membranes. J Membr Biol 72: 213-221, 1983.
206. Ochrietor JD, Linser PJ. 5A11/Basigin gene products are necessary forproper maturation and function of the retina. Dev Neurosci 26: 380-387,2004.
207. Ojuka EO. Role of calcium and AMP kinase in the regulation of mito-chondrial biogenesis and GLUT4 levels in muscle. Proc Nutr Soc 63:275-278, 2004.
208. Okamura H, Spicer SS, Schulte BA. Developmental expression ofmonocarboxylate transporter in the gerbil inner ear. Neuroscience 107:499-505, 2001.
209. Olson EN, Williams RS. Calcineurin signaling and muscle remodeling.Cell 101: 689-692, 2000.
210. Orsenigo MN, Tosco M, Bazzini C, Laforenza U, Faelli A. A mono-carboxylate transporter MCT1 is located at the basolateral pole of ratjejunum. Exp Physiol 84: 1033-1042, 1999.
211. Otonkoski T, Jiao H, Kaminen-Ahola N, Tapia-Paez I, Ullah MS, PartonLE, Schuit F, Quintens R, Sipila I, Mayatepek E, Meissner T, HalestrapAP, Rutter GA, Kere J. Physical exercise-induced hypoglycemia causedby failed silencing of monocarboxylate transporter 1 in pancreatic betacells. Am J Hum Genet 81: 467-474, 2007.
212. Ovens MJ, Davies AJ, Wilson MC, Murray CM, Halestrap AP. AR-C155858 is a potent inhibitor of monocarboxylate transporters MCT1and MCT2 that binds to an intracellular site involving transmembranehelices 7-10. Biochem J 425: 523-530, 2010.
1640 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
213. Ovens MJ, Manoharan C, Wilson MC, Murray CM, Halestrap AP. Theinhibition of monocarboxylate transporter 2 (MCT2) by AR-C155858is modulated by the associated ancillary protein. Biochem J 431: 217-225, 2010.
214. Pahlman C, Qi Z, Murray CM, Ferguson D, Bundick RV, Donald DK,Ekberg H. Immunosuppressive properties of a series of novel inhibitorsof the monocarboxylate transporter MCT-1. Transpl Int 26: 22-29,2013.
215. Palmieri F. The mitochondrial transporter family (SLC25): Physio-logical and pathological implications. Pflugers Arch 447: 689-709,2004.
216. Papa S, Paradies G. On the mechanism of translocation of pyruvate andother monocarboxylic acids in rat-liver mitochondria. Eur J Biochem49: 265-274, 1974.
217. Paradies G. Interaction of alpha-cyano-[14C]cinnamate with the mito-chondrial pyruvate translocator. Biochim Biophys Acta 766: 446-450,1984.
218. Paradies G, Papa S. The transport of monocarboxylic oxoacids in ratliver mitochondria. FEBS Lett 52: 149-152, 1975.
219. Paradies G, Papa S. On the kinetics and substrate specificity of thepyruvate translocator in rat liver mitochondria. Biochim Biophys Acta462: 333-346, 1977.
220. Paradies G, Ruggiero FM. Characterization of the alpha-cyanocinnamate binding site in rat heart mitochondria and in submito-chondrial particles. Biochim Biophys Acta 850: 249-255, 1986.
221. Park JY, Helm JF, Zheng W, Ly QP, Hodul PJ, Centeno BA, MalafaMP. Silencing of the candidate tumor suppressor gene solute carrierfamily 5 member 8 (SLC5A8) in human pancreatic cancer. Pancreas36: e32-39, 2008.
222. Park JY, Zheng W, Kim D, Cheng JQ, Kumar N, Ahmad N, Pow-Sang J. Candidate tumor suppressor gene SLC5A8 is frequently down-regulated by promoter hypermethylation in prostate tumor. CancerDetect Prev 31: 359-365, 2007.
223. Parks SK, Chiche J, Pouyssegur J. pH control mechanisms of tumorsurvival and growth. J Cell Physiol 226: 299-308, 2011.
224. Paroder V, Spencer SR, Paroder M, Arango D, Schwartz S, MariadasonJM, Augenlicht LH, Eskandari S, Carrasco N. Na+/monocarboxylatetransport (SMCT) protein expression correlates with survival in coloncancer: Molecular characterization of SMCT. Proc Natl Acad Sci USA103: 7270-7275, 2006.
225. PebayPeyroula E, DahoutGonzalez C, Kahn R, Trezeguet V, LauquinGJM, Brandolin R. Structure of mitochondrial ADP/ATP carrier incomplex with carboxyatractyloside. Nature 426: 39-44, 2003.
226. Pellerin L, Bergersen LH, Halestrap AP, Pierre K. Cellular and sub-cellular distribution of monocarboxylate transporters in cultured braincells and in the adult brain. J Neurosci Res 79: 55-64, 2005.
227. Perez de Heredia F, Wood IS, Trayhurn P. Hypoxia stimulates lactaterelease and modulates monocarboxylate transporter (MCT1, MCT2,MCT4) expression in human adipocytes. Pflugers Arch 459: 509-518,2010.
228. Philp A, Macdonald AL, Watt PW. Lactate - a signal coordinating celland systemic function. J Exp Biol 208: 4561-4575, 2005.
229. Philp N, Chu P, Pan TC, Zhang RZ, Chu ML, Stark K, Boettiger D,Yoon H, Emmons T. Developmental expression and molecular cloningof REMP, a novel retinal epithelial membrane protein. Exp Cell Res219: 64-73, 1995.
230. Philp NJ, Ochrietor JD, Rudoy C, Muramatsu T, Linser PJ. Loss ofMCT1, MCT3, MCT4 expression in the retinal pigment epithelium andneural retina of the 5A11/basigin-null mouse. Invest Ophth Vis Sci 44:1305-1311, 2003.
231. Philp NJ, Yoon H, Grollman EF. Monocarboxylate transporter MCT1is located in the apical membrane and MCT3 in the basal membraneof rat RPE - Rapid Communication. Am J Physiol 274: R1824-R1828,1998.
232. Philp NJ, Yoon HY, Lombardi L. Mouse MCT3 gene is expressedpreferentially in retinal pigment and choroid plexus epithelia. Am JPhysiol 280: C1319-C1326, 2001.
233. Pierre K, Parent A, Jayet PY, Halestrap AP, Scherrer U, Pellerin L.Enhanced expression of three monocarboxylate transporter isoforms inthe brain of obese mice. J Physiol 583: 469-486, 2007.
234. Pierre K, Pellerin L. Monocarboxylate transporters in the central ner-vous system: Distribution, regulation and function. J Neurochem 94:1-14, 2005.
235. Pilegaard H, Domino K, Noland T, Juel C, Hellsten Y, Halestrap AP,Bangsbo J. Effect of high-intensity exercise training on lactate/H+transport capacity in human skeletal muscle. Am J Physiol 276: E255-E261, 1999.
236. Pilegaard H, Juel C. Lactate transport studied in sarcolemmal giantvesicles from rat skeletal muscles: Effect of denervation. Am J Physiol269: E679-E682, 1995.
237. Pilegaard H, Mohr T, Kjaer M, Juel C. Lactate/H+ transport in skeletalmuscle from spinal-cord-injured patients. Scand J Med Sci Sports 8:98-101, 1998.
238. Pinheiro C, Longatto-Filho A, Azevedo-Silva J, Casal M, Schmitt FC,Baltazar F. Role of monocarboxylate transporters in human cancers:State of the art. J Bioenerg Biomembr 44: 127-139, 2012.
239. Pinheiro C, Reis RM, Ricardo S, Longatto-Filho A, Schmitt F, BaltazarF. Expression of monocarboxylate transporters 1, 2, 4 in human tumorsand their association with CD147 and CD44. J Biomed Biotechnol2010:427694. doi: 10.1155/2010/427694, 2010.
240. Poole RC, Bowden NJ, Halestrap AP. Derivatives of cinnamic acidinteract with the nucleotide binding site of mitochondrial aldehydedehydrogenase - effects on the dehydrogenase reaction and stimulationof esterase activity by nucleotides. Biochem Pharmacol 45: 1621-1630,1993.
241. Poole RC, Cranmer SL, Halestrap AP, Levi AJ. substrate and inhibitorspecificity of monocarboxylate transport into heart cells and erythro-cytes - further evidence for the existence of 2 distinct carriers. BiochemJ 269: 827-829, 1990.
242. Poole RC, Cranmer SL, Holdup DW, Halestrap AP. Inhibition ofL-lactate transport and band-3-mediated anion transport in erythro-cytes by the novel stilbenedisulphonate N,N,N′,N′-tetrabenzyl-4,4′-diaminostilbene-2,2′-disulphonate (TBenzDS). Biochim Biophys Acta1070: 69-76, 1991.
243. Poole RC, Halestrap AP. Reversible and irreversible inhibition, bystilbenedisulphonates, of lactate transport into rat erythrocytes - identi-fication of some new high-affinity inhibitors. Biochem J 275: 307-312,1991.
244. Poole RC, Halestrap AP. Identification and partial purificationof the erythrocyte lactate transporter. Biochem J 283: 855-862,1992.
245. Poole RC, Halestrap AP. Transport of lactate and other monocarboxy-lates across mammalian plasma membranes. Am J Physiol 264: C761-C782, 1993.
246. Poole RC, Halestrap AP. N-Terminal protein sequence analysis of therabbit erythrocyte lactate transporter suggests identity with the clonedmonocarboxylate transport protein MCT1. Biochem J 303: 755-759,1994.
247. Poole RC, Halestrap AP. Interaction of the erythrocyte lactate trans-porter (monocarboxylate transporter 1) with an integral 70-kDa mem-brane glycoprotein of the immunoglobulin superfamily. J Biol Chem272: 14624-14628, 1997.
248. Poole RC, Halestrap AP, Price SJ, Levi AJ. The kinetics of transportof lactate and pyruvate into isolated cardiac myocytes from guinea pig- kinetic evidence for the presence of a carrier distinct from that inerythrocytes and hepatocytes. Biochem J 264: 409-418, 1989.
249. Poole RC, Sansom CE, Halestrap AP. Studies of the membrane topol-ogy of the rat erythrocyte H+/lactate cotransporter (MCT1). BiochemJ 320: 817-824, 1996.
250. Price NT, Jackson VN, Halestrap AP. Cloning and sequencing of fournew mammalian monocarboxylate transporter (MCT) homologues con-firms the existence of a transporter family with an ancient past. BiochemJ 329: 321-328, 1998.
251. Proud CG. Regulation of mRNA translation. Essays Biochem 37: 97-108, 2001.
252. Pullen TJ, da Silva Xavier G, Kelsey G, Rutter GA. miR-29a andmiR-29b contribute to pancreatic beta-cell-specific silencing of mono-carboxylate transporter 1 (Mct1). Mol Cell Biol 31: 3182-3194,2011.
253. Pullen TJ, Sylow L, Sun G, Halestrap AP, Richter EA, Rutter GA. Over-expression of monocarboxylate transporter-1 (SLC16A1) in mousepancreatic beta-cells leads to relative hyperinsulinism during exercise.Diabetes 61: 1719-1725, 2012.
254. Pushkarsky T, Zybarth G, Dubrovsky L, Yurchenko V, Tang H, GuoHM, Toole B, Sherry B, Bukrinsky M. CD147 facilitates HIV-1 infec-tion by interacting with virus-associated cyclophilin A. Proc Natl AcadSci U S A 98: 6360-6365, 2001.
255. Py G, Lambert K, Milhavet O, Eydoux N, Prefaut C, Mercier J.Effects of streptozotocin-induced diabetes on markers of skeletal mus-cle metabolism and monocarboxylate transporter 1 to monocarboxylatetransporter 4 transporters. Metabolism 51: 807-813, 2002.
256. Py G, Lambert K, PerezMartin A, Raynaud E, Prefaut C, Mercier J.Impaired sarcolemmal vesicle lactate uptake and skeletal muscle MCT1and MCT4 expression in obese Zucker rats. Am J Physiol 281: E1308-E1315, 2001.
257. Rafiki A, Boulland JL, Halestrap AP, Ottersen OP, Bergersen L. Highlydifferential expression of the monocarboxylate transporters MCT2and MCT4 in the developing rat brain. Neuroscience 122: 677-688,2003.
258. Rahman B, Schneider HP, Broer A, Deitmer JW, Broer S. Helix 8 andhelix 10 are involved in substrate recognition in the rat monocarboxylatetransporter MCT1. Biochemistry 38: 11577-11584, 1999.
259. Riazi R, Khairallah M, Cameron JM, Pencharz PB, Des Rosiers C,Robinson BH. Probing pyruvate metabolism in normal and mutantfibroblast cell lines using 13C-labeled mass isotopomer analysis andmass spectrometry. Mol Genet Metab 98: 349-355, 2009.
Volume 3, October 2013 1641

Monocarboxylic Acid Transport Comprehensive Physiology
260. Ritzhaupt A, Wood IS, Ellis A, Hosie KB, ShiraziBeechey SP. Identifi-cation and characterization of a monocarboxylate transporter (MCT1)in pig and human colon: Its potential to transport L-lactate as well asbutyrate. J Physiol 513: 719-732, 1998.
261. Robinet C, Pellerin L. Brain-derived neurotrophic factor enhances theexpression of the monocarboxylate transporter 2 through translationalactivation in mouse cultured cortical neurons. J Cereb Blood FlowMetab 30: 286-298, 2010.
262. Robinson AM, Williamson DH. Physiological roles of ketone bodies assubstrates and signals in mammalian tissues. Physiol Rev 60: 143-180,1980.
263. Robinson AJ, Overy C, Kunji ERS. The mechanism of transport bymitochondrial carriers based on analysis of symmetry. Proc Natl AcadSci U S A 105: 17766-17771, 2008.
264. Sahlin K, Fernstrom M, Svensson M, Tonkonogi M. No evidence ofan intracellular lactate shuttle in rat skeletal muscle. J Physiol 541:569-574, 2002.
265. Schneider U, Poole RC, Halestrap AP, Grafe P. Lactate-proton co-transport and its contribution to interstitial acidification during hypoxiain isolated rat spinal roots. Neuroscience 53: 1153-1162, 1993.
266. Schulze A, Harris AL. How cancer metabolism is tuned for proliferationand vulnerable to disruption. Nature 491: 364-373, 2012.
267. Sepponen K, Ruusunen M, Pakkanen JA, Poso AR. Expression ofCD147 and monocarboxylate transporters MCT1, MCT2 and MCT4 inporcine small intestine and colon. Vet J 174: 122-128, 2007.
268. Shearman MS, Halestrap AP. The concentration of the mitochondrialpyruvate carrier in rat liver and heart mitochondria determined with α-cyano-β-(1-phenylindol-3-yl)acrylate. Biochem J 223: 673-676, 1984.
269. Shewan AM, Marsh BJ, Melvin DR, Martin S, Gould GW, James DE.The cytosolic C-terminus of the glucose transporter GLUT4 contains anacidic cluster endosomal targeting motif distal to the dileucine signal.Biochem J 350: 99-107, 2000.
270. Siebens AW, Boron WF. Effect of electroneutral luminal and basolaterallactate transport om intracellular pH in salamander proximal tubules.J Gen Physiol 90: 799-831, 1987.
271. Singh B, Halestrap AP, Paraskeva C. Butyrate can act as a stimulatorof growth or inducer of apoptosis in human colonic epithelial cell linesdepending on the presence of alternative energy sources. Carcinogene-sis 18: 1265-1270, 1997.
272. Smirnova I, Kasho V, Kaback HR. Lactose permease and the alternatingaccess mechanism. Biochemistry 50: 9684-9693, 2011.
273. Smirnova I, Kasho V, Choe J-Y, Altenbach C, Hubbell WL, KabackHR. Sugar binding induces an outward facing conformation of LacY.Proc Natl Acad Sci U S A 104: 16504-16509, 2007.
274. Smith JP, Drewes LR. Modulation of monocarboxylic acid transporter-1 kinetic function by the cAMP signaling pathway in rat brain endothe-lial cells. J Biol Chem 281: 2053-2060, 2006.
275. Sonveaux P, Vegran F, Schroeder T, Wergin MC, Verrax J, RabbaniZN, De Saedeleer CJ, Kennedy KM, Diepart C, Jordan BF, Kelley MJ,Gallez B, Wahl ML, Feron O, Dewhirst MW. Targeting lactate-fueledrespiration selectively kills hypoxic tumor cells in mice. J Clin Invest118: 3930-3942, 2008.
276. Spencer TL, Lehninger AL. L-lactate transport in Ehrlich ascites tumorcells. Biochem J 154: 405-414, 1976.
277. Srinivas SR, Gopal E, Zhuang L, Itagaki S, Martin PM, Fei YJ, Ganap-athy V, Prasad PD. Cloning and functional identification of slc5a12as a sodium-coupled low-affinity transporter for monocarboxylates(SMCT2). Biochem J 392: 655-664, 2005.
278. Storelli C, Corcelli A, Cassano G, Hildmann B, Murer H, Lippe C. Polardistribution of sodium-dependent and sodium-independent transportsystems for L-lactate in rat enterocytes. Pflugers Arch 388: 11-16, 1980.
279. Stridh MH, Alt MD, Wittmann S, Heidtmann H, Aggarwal M, RiedererB, Seidler U, Wennemuth G, McKenna R, Deitmer JW, Becker HM.Lactate flux in astrocytes is enhanced by a non-catalytic action ofcarbonic anhydrase II. J Physiol 590: 2333-2351, 2012.
280. Su J, Chen X, Kanekura T. A CD147-targeting siRNA inhibits theproliferation, invasiveness, VEGF production of human malignantmelanoma cells by down-regulating glycolysis. Cancer Lett 273: 140-147, 2009.
280a.Suhre K, Shin SY, Petersen AK, Mohney RP, Meredith D, WageleB, Altmaier E, Deloukas P, Erdmann J, Grundberg E, Hammond CJ,de Angelis MH, Kastenmuller G, Kottgen A, Kronenberg F, ManginoM, Meisinger C, Meitinger T, Mewes HW, Milburn MV, Prehn C,Raffler J, Ried JS, Romisch-Margl W, Samani NJ, Small KS, Wich-mann HE, Zhai G, Illig T, Spector TD, Adamski J, Soranzo N, GiegerC. Human metabolic individuality in biomedical and pharmaceuticalresearch. Nature 477: 54-60, 2011.
281. Sun L, Zeng X, Yan C, Sun X, Gong X, Rao Y, Yan N. Crystal structureof a bacterial homologue of glucose transporters GLUT1-4. Nature 490:361-366, 2012.
282. Suzuki A, Stern SA, Bozdagi O, Huntley GW, Walker RH, MagistrettiPJ, Alberini CM. Astrocyte-neuron lactate transport is required forlong-term memory formation. Cell 144: 810-23, 2011.
283. Tamai I, Takanaga H, Ogihara T, Higashida H, Maeda H, Sai Y, Tsuji A.Participation of a proton-cotransporter, MCT1, in the intestinal trans-port of monocarboxylic acids. Biochem Biophys Res Commun 214:482-489, 1995.
284. Teramae H, Yoshikawa T, Inoue R, Ushida K, Takebe K, Nio-KobayashiJ, Iwanaga T. The cellular expression of SMCT2 and its comparisonwith other transporters for monocarboxylates in the mouse digestivetract. Biomed Res 31: 239-249, 2010.
285. Thangaraju M, Ananth S, Martin PM, Roon P, Smith SB, Sterneck E,Prasad PD, Ganapathy V. c/ebpdelta Null mouse as a model for thedouble knock-out of slc5a8 and slc5a12 in kidney. J Biol Chem 281:26769-26773, 2006.
286. Thangaraju M, Carswell KN, Prasad PD, Ganapathy V. Colon cancercells maintain low levels of pyruvate to avoid cell death caused byinhibition of HDAC1/HDAC3. Biochem J 417: 379-389, 2009.
287. Thangaraju M, Karunakaran SK, Itagaki S, Gopal E, Elangovan S,Prasad PD, Ganapathy V. Transport by SLC5A8 with subsequentinhibition of histone deacetylase 1 (HDAC1) and HDAC3 underliesthe antitumor activity of 3-bromopyruvate. Cancer 115: 4655-4666,2009.
288. Thomas AP, Halestrap AP. Identification of the protein responsiblefor pyruvate transport into rat liver and heart mitochondria by spe-cific labelling with N-phenylmaleimide. Biochem J 196: 471-479,1981.
289. Thomas C, Bishop D, Moore-Morris T, Mercier J. Effects of high-intensity training on MCT1, MCT4, NBC expressions in rat skeletalmuscles: Influence of chronic metabolic alkalosis. Am J Physiol 293:E916-22, 2007.
290. Thomas C, Perrey S, Lambert K, Hugon G, Mornet D, Mercier J.Monocarboxylate transporters, blood lactate removal after supramaxi-mal exercise, fatigue indexes in humans. J Appl Physiol 98: 804-809,2005.
291. Thomas JA, Buchsbaum RN, Zimniak A, Racker E. Intracellular pHmeasurements in Ehrlich ascites tumor cells utilising spectroscopicprobes generated in situ. Biochemistry 18: 2210-2218, 1979.
292. Todisco S, Agrimi G, Castegna A, Palmieri F. Identification of themitochondrial NAD+ transporter in Saccharomyces cerevisiae. J BiolChem 281: 1524-1531, 2006.
293. Ullah MS, Davies AJ, Halestrap AP. The plasma membrane lactatetransporter MCT4, but not MCT1, is up-regulated by hypoxia througha HIF-1 alpha-dependent mechanism. J Biol Chem 281: 9030-9037,2006.
294. Ullrich KJ, Rumrich G, Kloss S. Reabsorption of monocarboxylic acidsin the proximal tubule of the rat kidney I. Transport kinetics of D-lactate,Na-dependence, pH dependence and effect of inhibitors. Pflugers Arch395: 212-219, 1982.
295. Ullrich KJ, Rumrich G, Loss S, Fasold H. Reabsorption of monocar-boxylic acids in the proximal tubule of the rat kidney III. Specificityfor aromatic compounds. Pflugers Arch 395: 227-231, 1982.
296. Vandenberg JI, Metcalfe JC, Grace AA. Mechanisms of intracellular pHrecovery following global ischaemia in the perfused heart. CirculationRes 72: 993-1003, 1993.
297. Vander Heiden MG. Targeting cancer metabolism: A therapeutic win-dow opens. Nat Rev Drug Discov 10: 671-684, 2011.
298. VanItallie TB, Nufert TH. Ketones: Metabolism’s ugly duckling. NutrRev 61: 327-341, 2003.
299. Varma MV, Ambler CM, Ullah M, Rotter CJ, Sun H, Litchfield J, Fen-ner KS, El-Kattan AF. Targeting intestinal transporters for optimizingoral drug absorption. Curr Drug Metab 11: 730-742, 2010.
300. Vaughan-Jones RD, Spitzer KW, Swietach P. Intracellular pH regula-tion in heart. J Mol Cell Cardiol 46: 318-31, 2009.
301. Visser WE, Friesema EC, Visser TJ. Minireview: Thyroid hormonetransporters: The knowns and the unknowns. Mol Endocrinol 25: 1-14,2011.
302. Vivekananda J, Oliver DJ. Detection of the monocarboxylate transporterfrom pea mitochondria by means of a specific monoclonal antibody.FEBS Lett 260: 217-219, 1990.
303. Von Grumbckow L, Elsner P, Hellsten Y, Quistorff B, Juel C. Kineticsof lactate and pyruvate transport in cultured rat myotubes. BiochimBiophys Acta 1417: 267-275, 1999.
304. Walter A, Gutknecht J. Monocarboxylic acid permeation through lipidbilayer membranes. J Membr Biol 77: 255-264, 1984.
305. Wang XM, Levi AJ, Halestrap AP. Kinetics of the sarcolemmal lactatecarrier in single heart cells using BCECF to measure pH(i). Am J Physiol267: H1759-H1769, 1994.
306. Wang XM, Poole RC, Halestrap AP, Levi AJ. Characterization of theinhibition by stilbene disulphonates and phloretin of lactate and pyru-vate transport into rat and guinea-pig cardiac myocytes suggests thepresence of 2 kinetically distinct carriers in heart cells. Biochem J 290:249-258, 1993.
307. Wang YX, Tonouchi M, Miskovic D, Hatta H, Bonen A. T-3 increaseslactate transport and the expression of MCT4, but not MCT1, in ratskeletal muscle. Am J Physiol 285: E622-E628, 2003.
1642 Volume 3, October 2013

Comprehensive Physiology Monocarboxylic Acid Transport
308. Welter H, Claus R. Expression of the monocarboxylate transporter 1(MCT1) in cells of the porcine intestine. Cell Biol Int 32: 638-645,2008.
309. Wiederkehr A, Wollheim CB. Impact of mitochondrial calcium on thecoupling of metabolism to insulin secretion in the pancreatic beta-cell.Cell Calcium 44: 64-76, 2008.
310. Wilson MC, Jackson VN, Heddle C, Price NT, Pilegaard H, Juel C,Bonen A, Montgomery I, Hutter OF, Halestrap AP. Lactic acid effluxfrom white skeletal muscle is catalyzed by the monocarboxylate trans-porter isoform MCT3. J Biol Chem 273: 15920-15926, 1998.
311. Wilson MC, Meredith D, Fox JEM, Manoharan C, Davies AJ, HalestrapAP. Basigin (CD147) is the target for organomercurial inhibition ofmonocarboxylate transporter isoforms 1 and 4 - the ancillary proteinfor the insensitive MCT2 is embigin (Gp70). J Biol Chem 280: 27213-27221, 2005.
312. Wilson MC, Meredith D, Halestrap AP. Fluorescence resonance energytransfer studies on the interaction between the lactate transporter MCT1and CD147 provide information on the topology and stoichiometry ofthe complex in situ. J Biol Chem 277: 3666-3672, 2002.
313. Wilson MC, Meredith D, Bunnun C, Sessions RB, Halestrap AP. Stud-ies on the DIDS binding site of monocarboxylate transporter 1 suggest ahomology model of the open conformation and a plausible translocationcycle. J. Biol Chem 284: 20011-20021, 2009.
314. Wright EM. Transport of carboxylic acids by renal membrane vesicles.Ann Rev Physiol 47: 127-141, 1985.
315. Wright EM, Turk E. The sodium/glucose cotransport family SLC5.Pflugers Arch 447: 510-518, 2004.
316. Yanase H, Takebe K, Nio-Kobayashi J, Takahashi-Iwanaga H, IwanagaT. Cellular expression of a sodium-dependent monocarboxylate trans-porter (Slc5a8) and the MCT family in the mouse kidney. HistochemCell Biol 130: 957-966, 2008.
317. Yin Y, He X, Szewczyk P, Nguyen T, Chang G. Structure of themultidrug transporter EmrD from Escherichia coli. Science 312: 741-744, 2006.
318. Yoon H, Donoso LA, Philp NJ. Cloning of the human monocarboxylatetransporter MCT3 gene: Localization to chromosome 22q12.3-q13.2.Genomics 60: 366-370, 1999.
319. Yoon HY, Fanelli A, Grollman EF, Philp NJ. Identification of a uniquemonocarboxylate transporter (MCT3) in retinal pigment epithelium.Biochem Biophys Res Commun 234: 90-94, 1997.
320. Yoshida Y, Hatta H, Kato M, Enoki T, Kato H, Bonen A. Relation-ship between skeletal muscle MCT1 and accumulated exercise duringvoluntary wheel running. J Appl Physiol 97: 527-534, 2004.
321. Yoshida Y, Holloway GP, Ljubicic V, Hatta H, Spriet LL, Hood DA,Bonen A. Negligible direct lactate oxidation in subsarcolemmal andintermyofibrillar mitochondria obtained from red and white rat skeletalmuscle. J Physiol 582: 1317-1335, 2007.
322. Yurchenko V, Constant S, Eisenmesser E, Bukrinsky M. Cyclophilin-CD147 interactions: A new target for anti-inflammatory therapeutics.Clin Exp Immunol 160: 305-317, 2010.
323. Zeuthen T, Hamann S, laCour M. Cotransport of H+, lactate and H2Oby membrane proteins in retinal pigment epithelium of bullfrog. J Phys-iol 497: 3-17, 1996.
324. Zhao C, Wilson MC, Schuit F, Halestrap AP, Rutter GA. Expres-sion and distribution of lactate/monocarboxylate transporter isoformsin pancreatic islets and the exocrine pancreas. Diabetes 50: 361-366,2001.
325. Zhou Y, Guan L, Freites JA, Kaback HR. Opening and closing of theperiplasmic gate in lactose permease. Proc Natl Acad Sci U S A 105:3774-3778, 2008.
Volume 3, October 2013 1643