MODULATION OF T CELL FUNCTION BY COAGULATION FACTOR Xa · ii ‘Modulation of T Cell Function by...
Transcript of MODULATION OF T CELL FUNCTION BY COAGULATION FACTOR Xa · ii ‘Modulation of T Cell Function by...

MODULATION OF T CELL FUNCTION BY COAGULATION FACTOR Xa
by
Kaustav Chatterjee
A thesis submitted in conformity with the requirements for the degree of Master of Science
Graduate Department of Medical Biophysics University of Toronto
© Copyright by Kaustav Chatterjee 2011

ii
‘Modulation of T Cell Function by Coagulation Factor Xa’ Master of Science, 2011 Kaustav Chatterjee Department of Medical Biophysics, The University of Toronto
ABSTRACT
The serine protease factor Xa (FXa) plays an integral role in the coagulation cascade and has
recently been implicated in a variety of proinflammatory roles, establishing it as a link between
coagulation and inflammatory processes. In this thesis, I elaborate on previous literature by
characterizing further the response of primary human T lymphocytes to FXa. Building on
previous literature that describes the effect of FXa on whole T cell populations, I describe here
the effect of FXa on both antigen-independent and antigen-dependent proliferation and
costimulation of primary CD4+ and CD8+ T cells, thereby establishing an immunological role for
FXa. Further, I show that FXa elicits an immediate and direct effect on T cells demonstrated by
the rapid upregulation of the signalling cascade kinases, ERK1 and ERK2. Lastly, I demonstrate
that the protease activated receptor 2 (PAR2) is involved in the mediation of this direct FXa
effect.

iii
ACKNOWLEDGEMENTS
This thesis is the culmination of years of work and it would not have been possible without the
help and support of many individuals.
Firstly, I would like to thank my supervisor, André Schuh, for giving me the opportunity to work
on such an interesting project and for all the support and guidance throughout the years,
including the critical reading and editing of my thesis. I wish you good luck in the future!
To Wendy, Joe, and Xiang-Fu, thank you for all of the support, guidance, and camaraderie, not
to mention your numerous and generous donations of blood, without which the project would
have come to a grinding halt. You made working in a confined space day in and day out
enjoyable. I wish you every success!
To all of my close friends, I thank you for being there for me all of these years through the good
times and especially the bad.
Lastly, to my family (my father, Probir, my mother, Chandra, and my sister, Kisha), to whom I
dedicate this thesis, thank you for your undying and unconditional love and support through
the years, and for your continued faith in me. This thesis truly would not have been possible
without you.

iv
TABLE OF CONTENTS
Abstract ............................................................................................................................................... ii
Acknowledgements ............................................................................................................................ iii
Table of Contents ................................................................................................................................ iv
List of Figures ..................................................................................................................................... vii
List of Abbreviations ......................................................................................................................... viii
Introduction ......................................................................................................................................... 1
Hemostasis and the coagulation cascade ................................................................................................. 1
Extrinsic pathway ...................................................................................................................................... 2
Intrinsic Pathway ....................................................................................................................................... 4
Regulation of procoagulant activity .......................................................................................................... 5
Fibrinolytic pathway .................................................................................................................................. 6
Summary of process .................................................................................................................................. 7
Factor Xa ................................................................................................................................................... 8
Inflammation, immunity and coagulation .............................................................................................. 10
Immunomodulatory roles of FXa ............................................................................................................ 14
Protease activated receptors (PARs) ...................................................................................................... 16
T cell activation and function .................................................................................................................. 18
Relevance of work ................................................................................................................................... 21
Materials and Methods ...................................................................................................................... 23
Cell culture .............................................................................................................................................. 23
Peripheral Blood Mononuclear Cell (PBMC) purification ................................................................... 23
Primary T cell culture for ERK-Phosphorylation assays ...................................................................... 24
Flow Cytometry ....................................................................................................................................... 24
T cell purity .......................................................................................................................................... 24
HLA-A2 typing ..................................................................................................................................... 24
Influenza A MP58-66 response ........................................................................................................... 25

v
PAR1 and PAR2 expression ................................................................................................................. 25
Antigen-Dependent Stimulation ............................................................................................................. 26
Tetanus Toxoid Assays ........................................................................................................................ 26
Influenza A Matrix Peptide Assay ....................................................................................................... 27
Antigen-Independent Stimulation .......................................................................................................... 27
Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) ................................................................. 28
ERK Phosphorylation Assays ................................................................................................................... 29
SDS-PAGE ................................................................................................................................................ 30
Western Blotting ..................................................................................................................................... 31
Data Analysis ........................................................................................................................................... 32
Results ............................................................................................................................................... 33
FXa enhances the antigen-independent proliferation of both human primary CD4+ and CD8+ T cells .. 33
FXa enhances the antigen-dependent proliferation of human primary CD8+ T cells ............................. 34
FXa enhances the antigen-dependent proliferation of human primary CD4+ T cells ............................. 39
PAR1 and PAR2 are expressed by T cells ................................................................................................ 41
PAR1 and PAR2 mRNA expression is activation-independent ................................................................ 42
FXa enhances ERK1/2 phosphorylation in T cells .................................................................................... 45
PAR2 likely mediates FXa signalling in T cells ......................................................................................... 49
Discussion .......................................................................................................................................... 54
FXa enhances the proliferation of both CD4+ and CD8+ T cells ............................................................... 54
FXa provides a costimulatory signal to T cells ......................................................................................... 56
PAR2 is involved in FXa signalling in T cells ............................................................................................. 59
Role of FXa in Innate/ Adaptive Immunity .............................................................................................. 63
Conclusions ............................................................................................................................................. 71
Future Work ............................................................................................................................................ 72
References ......................................................................................................................................... 75

vi
LIST OF FIGURES
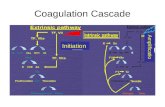
Figure 1: The Coagulation Cascade ............................................................................................................... 3
Figure 2: Structure, synthesis and activation of FX to FXa. .......................................................................... 9
Figure 3: Structure and mechanism of activation of PARs. ........................................................................ 17
Figure 4: The T cell synapse. ....................................................................................................................... 19
Figure 5: FXa enhances the proliferation of CD4+ primary human T cells, in vitro. ................................... 35
Figure 6: FXa enhances the proliferation of CD8+ primary human T cells, in vitro. ................................... 35
Figure 7: FXa enhances a primary human CD8+ T cell response to Flu MP58-66 antigen, in vitro. ........... 38
Figure 8: FXa enhances the proliferation of primary human CD4+ T cells in response to DTT. ................. 40
Figure 9: PAR1 and PAR2 are expressed on the surface of human primary T cells and JE6.1 cells. ........... 43
Figure 10: Activation of JE6.1 cells does not modify PAR2 surface expression. ......................................... 44
Figure 11: PAR1 mRNA expression in primary human T cells and JE6.1 cells is not activation-dependent,
in vitro. ........................................................................................................................................................ 46
Figure 12: PAR2 mRNA expression in primary human T cells and JE6.1 cells is not activation-dependent,
in vitro. ........................................................................................................................................................ 47
Figure 13: 18s rRNA and ABL mRNA expression in primary human T cells and JE6.1, in vitro. .................. 48
Figure 14: FXa induces ERK1/2 phosphorylation in human primary T cells and JE6.1 cells, in vitro. ......... 50
Figure 15: PAR2 mediates FXa signal in T cells and JE6.1 cells. .................................................................. 51
Figure 16: PAR1 transactivation of PAR2. ................................................................................................... 64

vii
LIST OF ABBREVIATIONS
2-ME 2-β-mercaptoethanol AA Amino acid Ab Antibody ABL Abelson murine leukemia viral oncogene homolog AICD Activation induced cell death AP Activation peptide APC Antigen presenting cell AT-III Anti-thrombin III BSA Bovine serum Albumin Ca2+ Calcium ions CD Cluster of differentiation cDNA Complementary deoxyribonucleic acid CPM Counts per minute DNA Deoxyribonucleic acid DTT Diptheria/ Tetanus toxoid EBV Epstein Barr virus EDTA Ethylenediaminetetraacetic acid EGF Epidermal growth factor EPCR Endothelial cell Protein C receptor EPR-1 Effector cell protease receptor 1 ER Endoplasmic reticulum ERK Extracellular signal-regulated kinase FACS Fluorescence-activated cell sorting FBS Fetal bovine serum FITC Fluorescein isothiocyanate FII/ FIIa Factor II (prothrombin)/ Factor IIa (thrombin) FV/ FVa Factor V/ Factor Va FVII/ FVIIa Factor VII/ Factor VIIa FVIII/ FVIIIa Factor VIII/ Factor VIIIa FIX/ FIXa Factor IX/ Factor IXa FX/ FXa Factor X/ Factor Xa FXI/ FXIa Factor XI/ Factor XIa FXII/ FXIIa Factor XII/ Factor XIIa FXIII/ FXIIIa Factor XIII/ Factor XIIIa Gla Glutamic Acid domain GC Germinal centre

viii
GPCR G-protein coupled receptor h Hour HCEC Human conjunctival epithelial cell HK High molecular weight kininogen HLA Human leukocyte antigen HRP Horseradish peroxidase HUVEC Human umbilical vein endothelial cell ICAM-1 Intracellular adhesion molecule 1 IFN-γ Interferon-γ IgG Immunoglobulin-G IL Interleukin IU International units JE6.1 Cells Jurkat E6.1 cells kDA Kilodalton L Litre LFA-1 Lymphocyte function-associated antigen 1 M Molar mAb Monoclonal antibody MAC-1 Macrophage 1 antigen MAPK Mitogen-activated protein kinase MCP-1 Monocytic chemoattractant protein 1 mg Milligram MHC Major histocompatibility complex min Minute mL Millilitre mM Millimolar MP58-66 Matrix protein peptide, residues 58-66 mRNA Messenger ribonucleic acid NFκB Nuclear factor κB NK Cells Natural killer cells nM Nanomolar PAF Platelet activating factor PAI Plasminogen activator inhibitor PAR Protease Activated Receptor PBMC Peripheral blood mononuclear cell PC/ PCa Protein C/ Protein Ca PDGF Platelet-derived growth factor PE Phycoerythrin pERK Phosphorylated extracellular signal-regulated kinase PHA Phytohemagglutinin

ix
PK Prekallikrein PL Phospholipid PP Pro-peptide PS Protein S PVDF Polyvinylidene fluoride RNA Ribonucleic acid rRNA Ribosomal ribonucleic acid RT-PCR Reverse transcriptase polymerase chain reaction SD Standard deviation SDS-PAGE Sodium dodecyl sulphate – polyacrylamide gel electrophoresis SE Standard error siRNA Short interfering ribonucleic acid SMC Smooth muscle cell SP Signal peptide TCR T cell receptor TBS Tris buffered saline TBST TBS with Tween 20 TET Tetracycline TF Tissue Factor TFPI Tissue factor pathway inhibitor Th1/Th2 T helper cell 1/2 TM Thrombomodulin TNF-α Tumor necrosis factor α t-PA Tissue-type plasminogen activator Tris tris(hydroxymethyl)aminomethane μg Microgram μL Microlitre μM Micromolar u-PA Urokinase-type plasminogen activator vWF von Willebrand Factor

1 | I n t r o d u c t i o n
INTRODUCTION
In this thesis, I elaborate on recent literature by further characterizing the response of enriched
human T lymphocytes to the serine protease coagulation factor Xa (FXa). Building on previous
literature, I describe here the effect of FXa on both antigen-independent and antigen-
dependent proliferation and costimulation of enriched CD4+ and CD8+ T cells, thereby
establishing a more physiologically significant immunological role for FXa. Further, I
demonstrate that this effect is immediate and direct, and that the protease activated receptor
2 (PAR2) is involved. I will begin by describing the coagulation system and components of the
immune system, and how the two are intimately linked, focusing on the significance of FXa. In
subsequent sections, I will detail my methods, the results of my experiments that establish a
clearer immunomodulatory role for FXa, and the significance of the work.
Literature suggests that the coagulation system is intimately linked with immune and
inflammatory responses. For example, it is now known that the initiation of coagulation is not
only a hemostatic response, but also a key event in the local and systemic response to
inflammatory stimuli [1-4]. I will later discuss several molecular links and evidence of crosstalk
between the coagulation and inflammation systems that have also been described recently.
HEMOSTASIS AND THE COAGULATION CASCADE
Hemostasis involves the maintenance of the balance between procoagulant responses to
prevent excessive bleeding at sites of vascular injury and the maintenance of circulation, by
keeping blood in a fluid state. This process involves the regulation of the pro-coagulant

2 | I n t r o d u c t i o n
cascades and their anti-coagulant counterparts, as well as of the fibrinolytic pathway and its
regulatory elements, which are all linked via complex feedback loops and parallel pathways.
The coagulation system can be viewed as a cascade of proteolytic reactions in which zymogens
are cleaved to produce active proteins [5-7]. Historically, coagulation was thought to proceed
via two distinct pathways; the extrinsic pathway, following damage to the blood vessel resulting
in the exposure of tissue factor (TF), and the intrinsic pathway, initiated by the activation of
platelets and the release of platelet granules. We now understand that the two are part of a
single cascade with multiple feedback loops (Figure 1).
EXTRINSIC PATHWAY
Typically upon vascular injury, TF, a subendothelial/endothelial membrane glycoprotein, which
is normally present in the circulation at very low levels [8], is exposed to the circulation, and
initiates blood coagulation [10]. The vitamin-K dependent proenzyme, FVII, binds to the
extracellular portion of TF via γ-carboxyglutamic acid residues and calcium bridges, which in
turn converts it into an active serine protease (FVIIa). The TF-VIIa complex activates FIX, and
subsequently FX into their active serine-protease counterparts, FXa and FIXa, respectively. FXa,
along with its cofactor FVa, in the presence of calcium and phospholipids, form a ‘prothrombin-
ase’ complex that converts prothrombin (FII) to its active serine protease counterpart thrombin
(FIIa). Thrombin activates platelets, and converts circulating fibrinogen monomers into
insoluble fibrin polymers, both of which serve as the foundation for a blood clot. Furthermore,
the generation of thrombin leads to amplification of the system, as thrombin feedback
activates factor V.


3 | I n t r o d u c t i o n
Figure 1: The Coagulation Cascade
The intrinsic cascade is initiated when contact is made between blood and exposed negatively
charged endothelial cell surfaces. The extrinsic cascade is initiate upon vascular injury, which
leads to the exposure of TF and the activation of FVII to FVIIa. The two pathways converge at
the activation of FX to FXa. The activation of FVII by FXa (red arrow), and of FIX by TF-VIIa
(orange arrow), further links the two pathways. FXa hydrolyzes and activates prothrombin to
thrombin, which then converts fibrinogen to fibrin and activates FXIII to FXIIIa. In a positive
feedback loop (green arrows), thrombin also activates FXI, FVIII and FV, thereby amplifying the
coagulation cascade. Finally, FXIIIa crosslinks fibrin polymers, thereby solidifying the clot. Ca,
Calcium ions, HK, high molecular weight kininogen; PK, prekallikrein; PL, phospholipid.

4 | I n t r o d u c t i o n
INTRINSIC PATHWAY
Thrombin can also be generated through the initiation of the intrinsic pathway [reviewed in 5-
7]. Upon vascular damage, FVIII-von Willebrand factor (vWF) multimer complexes, and
collagen-containing subepithelial structures, are exposed to the circulation. This allows
circulating platelets to bind to the collagen and FVIII-vWF multimer complexes, undergo a
morphological change, release the contents of their granules, and aggregate at the site.
Simultaneously, the exposure of negatively charged phospholipids and subendothelial
structures leads to the adsorption of FXII and kininogen (with bound prekallikrein and FXI).
Upon binding, FXII is activated partially to its protease counterpart, FXIIa. FXIIa then cleaves and
activates prekallikrein and FXI into kallekrein and FXIa, respectively. This process is amplified by
the conversion of partially activated FXIIa by kallekrein into an even more kinetically potent
protease.
FIX, which binds to the surface of aggregated platelets via γ-carboxyglutamic acid residues that
interact with calcium bridges, is activated by FXIa and remains bound to the platelets. Here, it
interacts with FVIII, which in turn is activated by thrombin (which exists in trace amounts in the
circulation) or by FXa (via feedback amplification). Using FVIIIa as a cofactor, in the presence of
calcium and phospholipids, FIXa forms a ‘ten-ase’ complex that activates circulating FX, which
also binds to the surface of platelets via γ-carboxyglutamic acid residues. FXa remains bounds
to the surface where it attaches to its cofactor FVa. FV is either adsorbed from plasma and
cleaved by thrombin into FVa, or is released as FVa from platelet α-granules. The FXa-FVa
complex then binds to, cleaves and activates circulating prothrombin into thrombin, which is

5 | I n t r o d u c t i o n
released into the circulation. The generation of thrombin once again leads to amplification of
the system as thrombin feedback activates factors V, VIII and XI.
Downstream of both pathways, thrombin induces local platelet aggregation and produces fibrin
monomers from plasma fibrinogen molecules. Further, it cleaves and activates FXIII to FXIIIa,
which covalently links fibrin monomers into fibrin polymers that form a mesh over the
adherent, aggregated platelets. Platelet contractile activity draws the polymerized fibrin mesh
tightly over the injured vascular surface and away from the luminal flow of blood. Once
unwanted blood flow is stopped, the fibrin polymers are gradually lysed to dissolve the clot.
Both FXa and thrombin are multi-directional in their reactions between the coagulation
complexes, and it is now recognized that both the extrinsic and the intrinsic pathways are
complementary and are both essential for the formation of FXa and thrombin. However, the
VII-TF complex is able to directly convert FIX to FIXa, and subsequently, FX to FXa, allowing the
extrinsic pathway to bypass the early initiating events of the intrinsic cascade. This, and the fact
that all events downstream of both pathways beginning with the formation of FXa are common
to both pathways, highlights a central and critical role for FXa in the process.
REGULATION OF PROCOAGULANT ACTIVITY
The regulatory mechanisms, which keep procoagulant activity under tight control, serve two
main functions: to limit the size of the fibrin clot thereby protecting the nearby tissue from
ischemia, and to localize clot formation to the site of injury, thereby preventing systemic
thrombosis. Tissue factor pathway inhibitor (TFPI) in plasma, becomes active when trace
amounts of FXa are produced during the initiating events of the extrinsic pathway. When active,

6 | I n t r o d u c t i o n
it binds directly to the TF-VIIa complex mentioned above, and slows down the activation of FIX
and FX [10-13]. Another inhibitor, anti-thrombin III (AT-III), directly inactivates thrombin and
several other serine proteases (factors IXa, Xa, XIa, XIIa, and TF-VIIa) [14,15]. The actions of
both TFPI and AT-III are greatly enhanced in the presence of heparin and similar
glycosaminoglycans [11, 16]. Normal endothelial cells express heparin sulphate (a sulphated
glycosaminoglycan), which binds to and increases the activity of AT-III, thereby preventing clot
formation in undamaged areas. Two other vitamin K-dependent inhibitors, Protein C (PC) and
Protein S (PS), work together to inactivate FVa and FVIIIa [17, 18]. PC is converted to its active
serine protease form, PCa, upon the binding of thrombin to thrombomodulin (TM) [19]. TM-
bound thrombin then undergoes a conformational change, loses its potent procoagulant
activity, and activates PC readily. Furthermore, the activation of PC by thrombin-TM is
enhanced dramatically when it is bound to the endothelial cell protein C receptor (EPCR)[20],
and its activity is enhanced in the presence of PS [18]. The thrombin to thrombin-TM switch is
important in the normal physiological state, as normal endothelial cells express TM that bind
any circulating thrombin, thereby preventing clot formation in undamaged areas.
FIBRINOLYTIC PATHWAY
Following coagulation, once excessive bleeding at the site of injury has stopped, vascular repair
ensues. Platelet derived growth factor (PDGF), which is released from platelet α-granules,
induces proliferation of vascular smooth muscle cells and fibroblasts. The fibrin mesh then
undergoes lysis under the action of plasmin, to prevent blood vessel obstruction. The zymogen,
plasminogen, which circulates in the blood bound to fibrinogen, is proteolysed partially into its

7 | I n t r o d u c t i o n
active form, plasmin, by the serine proteases, tissue-type plasminogen activator (t-PA) and
urokinase-type plasminogen activator (u-PA) [21,22]. Activated plasmin remains bound to fibrin
and degrades it into large soluble fragments that are released into the circulation. In addition,
kallikrein generated during the initiation of the intrinsic pathway, may also convert some
plasminogen to plasmin. As well, proteases released by neutrophils also degrade the fibrin
polymers which are then removed by phagocytosis [23].
Since plasmin can inactivate fibrinogen, FVIII and FV (which are needed for coagulation), the
plasmin inhibitor α2-Antiplasmin, and to a lesser degree, the non-specific protease α2-
Macroglobulin, function to inactivate circulating free plasmin [17]. Plasminogen activator
inhibitors (PAIs) in the plasma, such as PAI-1 also regulate plasminogen activation by forming
complexes with unbound t-PA, and removing it rapidly from circulation. The balance of t-PA and
PAI-1 is essential for the modulation of fibrinolytic activity [24,25].
SUMMARY OF PROCESS
The key events of coagulation and fibrinolysis can be summarized as follows. The binding of
FVIIa to TF converts FX to FXa, which using factor FVa as a cofactor, converts prothrombin to
thrombin. Thrombin induces fibrin polymerization and platelet activation, and in trace amounts
(in areas that are undamaged) can bind to TM ensuring proper blood flow. Once blood loss
ceases, the fibrin mesh is gradually dissolved, and vascular repair ensues under the activity of
PDGF.

8 | I n t r o d u c t i o n
FACTOR XA
The vitamin K-dependent serine protease FXa plays a central role in coagulation since
components of the coagulation downstream of it are common to both coagulation pathways
[5]. The inactive form of FXa, FX, is synthesized in the liver and requires several post-
translational modifications during biosynthesis before it can be released into the plasma as a
two-chain polypeptide (Figure 2). Following synthesis of the protein and transport to the
endoplasmic reticulum (ER), the signal peptide and adjoining propeptide are removed. This
targets a vitamin K-dependent carboxylase to the amino terminus where it carboxylates the γ-
carbons of glutamic acid residues in a glutamic acid rich domain (Gla domain). This process
occurs, as well, with other vitamin-K dependent proteases such as thrombin, FVII,FIX, PC and PS
[17]. Following γ-carboxylation, the single chain precursor is converted into a two-chain
molecule consisting of a 17kDa light chain and a 45kDa heavy chain held together by a
disulphide bridge. This γ -carboxylation is essential for procoagulant activity as it allows the
protein to bind calcium, which then mediates binding to a phospholipid surface. Furthermore,
the protein is glycosylated before being released into the bloodstream as the zymogen, FX.
The light chain of FX contains two epidermal growth factor (EGF) homology domains, the first of
which contains a Ca2+ binding site that acts as a hinge to fold the EGF and Gla domains together.
This allows FX to recognize and bind to cellular membranes. The heavy chain contains the
activation peptide, which is cleaved during coagulation to induce a conformational change in
the molecule that renders the adjacent latent serine protease catalytic domain active.
Activation of FX is mediated by the TF-FVIIa and FVIIIa-FIXa complexes during coagulation, as


9 | I n t r o d u c t i o n
Figure 2: Structure, synthesis and activation of FX to FXa.
The mature FX molecule is a two-chain polypeptide consisting of a 17-kDa light chain joined to a
45-kDa heavy chain by a disulfide bond (-S-S-). The light chain contains a cluster of glutamic acid
residues (EE) in its amino terminus (Gla domain) and two epidermal growth factor (EGF)
domains (inter-EGF domain). The first EGF homology domain contains a Ca2+ binding site that
acts as a hinge to fold the EGF and Gla domains toward one another, thereby forming a region
involved in the recognition of cellular membrane binding epitopes. The carboxy-terminal heavy
chain contains most of the carbohydrate moieties, as well as the latent serine protease catalytic
domain and the activation peptide. The synthesis of FX involves several post-translational
processing events (green arrow heads). Following synthesis of the protein and transport into
the endoplasmic reticulum, the signal peptide (SP) is removed. Subsequent endopeptidase
cleavage releases the adjoining propeptide (PP), thereby targeting the Gla domain for γ-
carboxylation (+) by a vitamin K-dependent carboxylase, and converts the single-chain
precursor into a two-chain molecule. The protein is also glycosylated prior to being secreted
into the bloodstream as a mature, inactive zymogen. During blood coagulation, activation of FX
by the FVIIa-TF or FIXa-FVIIIa complexes results in a proteolytic cleavage at Arg42-Ile53 (red
arrow head) of the heavy chain, thereby releasing a 52 aa activation glycopeptides from its
amino terminus, and yielding the proteolytically active molecule, FXa.

10 | I n t r o d u c t i o n
well as by Cathepsin G or CD11b while bound to the CD11b/CD18 complex (Mac-1) on
monocytes [28]. Activation by the extrinsic and intrinsic complexes proceeds via proteolytic
cleavage at Arg52-Ile53 of the heavy chain [5], resulting in the release of a 52aa activation
glycopeptide and the formation of an active two-chain peptide. FXa can now associate with its
cofactor, FVa, in the presence of Ca2+ and phospholipids, and can rapidly convert prothrombin
to thrombin. Since thrombin can mediate a variety of procoagulant activities, the generation of
thrombin is a key step, and hence FXa plays a pivotal role in blood coagulation. As I will discuss
below, however, FXa has also been shown to have an effect on a variety of cells that are not a
part of normal hemostasis, alluding to a potential immunomodulatory role.
INFLAMMATION, IMMUNITY AND COAGULATION
Inflammation is the first reaction the body has to foreign pathogens or irritants. The response is
largely dominated by components of the innate immune response that act quickly, in a
relatively non-specific fashion, to neutralize infection. If the infection persists, a more specific
adaptive immune response ensues that specifically targets the infectious agent, eventually
resulting in immunity. Inflammation consists of both humoral and cellular components.
Humoral elements include complement proteins, interferons, platelet activating factor (PAF),
histamine, serotonin, vasoactive amines and products of the kinin system, arachadonic acid
derivatives (prostaglandins and leukotrienes), and cytokines. Cellular elements include
neutrophils, eosinophils, mast cells, monocytes/macrophages, natural killer (NK) cells, platelets,
and endothelial cells [29-36]. An inflammatory stimulus triggers the release and involvement of
these elements, which act together or in sequence, to amplify the inflammatory response and

11 | I n t r o d u c t i o n
to modify and regulate it, until the inflammatory agent is removed, whereby the inflammatory
mediators dissipate, and are catabolyzed or are inhibited.
There is a growing body of evidence suggesting interaction at multiple levels among the various
elements of coagulation and innate immune processes. These include interactions at the
cellular and humoral levels. The simultaneous activation of these two processes is a highly
preserved survival strategy tracing back to early eukaryotic evolution before the separation of
plants and invertebrate animals [37]. Structural homology between various components of the
two processes provides evidence that there exists tight evolutionary linkage between
coagulation and immunity [reviewed in 4]. For example, TF has structural homology to cytokine
receptors [38], the lectin domain of TM has homology to selectins involved in leukocyte
adhesion [39], and the structure of EPCR is very similar to the major histocompatibility complex
(MHC1)/CD1 family of molecules [40]. Therefore, it is likely that components of the two
processes evolved from common ancestors in eukaryotic development, and furthermore, that
these two systems have maintained a high level of integration to protect the host following
tissue injury and microbial invasion. Examples of this integration are discussed below.
First, there exists a third alternative pathway of coagulation initiation that involves cellular
components of the immune system. Monocytes can mediate an alternative procoagulant
response after the binding of FX to the integrin Mac-1 on the monocyte surface [28]. This
process is independent of the initiating events of both the extrinsic and intrinsic pathways, and
instead is triggered by the proteolytic cleavage of monocyte-bound FX [41,42]. This occurs in a
three step process; inflammatory stimuli or ligand binding to Mac-1 induce the release of

12 | I n t r o d u c t i o n
granule proteases [43], released Cathepsin G subsequently cleaves and activates membrane-
bound FX at Leu177-Leu178 in the zymogen’s activation peptide, and the newly generated FXa
remains bound to the monocyte surface and promotes procoagulant activity and thrombin
formation [28]. Since TF, the main initiator of coagulation, is undetectable on normal
monocytes and undisturbed endothelium [44], the assembly of procoagulant components on
the surface of monocytes may be important as an initiating event for coagulation [45] and
anticoagulation [6] in protected membrane microenvironments, and protease-dependent
mechanisms of vascular cell activation and signal transduction.
The endothelium is also a very important link between coagulation and inflammation as
damaged endothelium serves as an interface for both procoagulant and proinflammatory
events. For example, following vascular injury, cytokines such as interleukin-1 (IL-1), IL-6 and
tumor necrosis factor α (TNF- α) , three of the most important initiators of inflammation,
induce the expression of TF on endothelial surfaces [46], that in turn initiates the extrinsic
pathway of coagulation.
Platelets also serve as an important link between the two processes. Following vascular injury
and binding to subendothelial structures, activated platelets release from their granules a
number of elements that modify tissue integrity [47,48]. For example, platelets secrete the
cytokine IL-1, which activates leukocytes and induces neutrophil and monocyte adherence (a
precursor for diapedesis, a key step in targeting immune cells to extravascular sites of infection)
[49]. They are also a major source of soluble CD40 ligand [50], which upregulates cytokine and

13 | I n t r o d u c t i o n
chemokine expression on vascular smooth muscle cells, and upregulates TF synthesis on
macrophages [51].
Upon the onset the inflammation, neutrophils and monocytes rapidly migrate to the target site,
where among other proinflammatory events, the expression of TF on monocytes is greatly
enhanced [9, 52]. These TF-expressing monocytes can generate thrombin locally, which can
then bind to TM on endothelial surface, providing another link between inflammation and
coagulation [53].
There exists interaction between the two processes at the humoral level as well, whereby
biochemical mediators of one process enhance, modify, or regulate the function of the other
process. For example, complement activation can facilitate the assembly and release of
procoagulant enzyme complexes on the surface of platelet microparticles [54]. An increase in
the level of the C4 binding protein (a component of complement activation), as well as
proteolytic cleavage by proteases release by neutrophils, can downregulate the activity of PS
[55]. The inflammatory cytokines TNF-α and IL-1 can downregulate EPCR and TM gene
transcription, that in turn downregulates the PC/PS pathway of anticoagulant activity [56], and
IL-6 can enhance the responsiveness of platelets to thrombin [57]. Acute phase proteins can
inhibit anticoagulant function and increase TF production [55]. As well, inflammation promotes
fibrinogen synthesis [58].
Similarly, components of pro- and anticoagulant processes affect inflammatory and immune
responses. For example, the TF-VIIa complex can directly activate endothelial cells, platelets
and leukocytes and induce the production of proinflammatory cytokines IL-6 and IL-8 via PAR2

14 | I n t r o d u c t i o n
[37, 59]. The PARs are also another important link between coagulation and inflammation (as
discussed below, see Protease Activated Receptors). Activated protein C (PCa) can
downregulate NFκB signalling and mRNA synthesis in monocytes [60-63] and endothelial cells
[64], respectively, leading to the downregulation in the expression of cell surface molecules and
cytokine formation. Thrombin has a multitude of effects on inflammatory processes. It is a
potent chemoattractant for neutrophils [65,66] and monocytes [67], induces mast cell
degranulation [68], and activates the endothelium and enhances the expression of platelet
activating factor (PAF) that stimulates neutrophils [69]. Activation of platelets by thrombin also
increases the expression of CD40 [70,71] ligand that in turn increases the expression of TF and
subsequently the expression of IL-6 and IL-8 [50,72]. Thrombin can also induce the mitogenesis
of a variety of cell types including T cells [73-77].
IMMUNOMODULATORY ROLES OF FXA
Of importance to this thesis, is the observation that FXa has been implicated in a variety of
immunomodulatory roles as well. For example, in addition to causing mast cell degranulation
[78], it can induce the production of the proinflammatory cytokines monocytic chemoattract
protein 1 (MCP-1), IL-6 and IL-8 by endothelial cells and dermal fibroblasts [79,80], as well as of
IL-1 by macrophages [81]. Furthermore, when injected into the paw of rats, it induces an acute
inflammatory response [78], and has also been implicated in a human mesangioproliferative
glomerulonephritis model [82]. These data, together with the observation that FXa directly
stimulates PBMCs and lymphocytes in vitro [83], and has a significant proinflammatory effect in
vivo [78], have implicated FXa as a key link between coagulation and inflammation.

15 | I n t r o d u c t i o n
Although membrane association of FXa occurs during coagulation and is essential for its
procoagulant activity [84, 85], several lines of evidence suggest, however, that this is
insufficient for its proinflammatory action, and that rather, a specific FXa receptor(s) must
mediate these effects [86,87]. The discovery of a putative lymphocyte FXa receptor, deemed
effector cell protease 1 (EPR-1), seemed to resolve this question [88,89]. Reports suggested
that FXa binds to EPR-1 via the FXa inter-EGF repeat domain, and mediates a proinflammatory
effect independent of its serine protease activity [79, 83, 90 - 92]. However, recent studies have
brought the nature and very existence of EPR-1 under suspicion [80, 93,94]. As well, previous
work done in our lab and by others, demonstrates that the serine protease activity of FXa is
necessary for its cellular effects, and that the inter-EGF repeat domain was likely not involved in
FXa membrane/receptor association [80, 87, 93, 94]. Since thrombin, another serine protease,
has been shown to mediate its proinflammatory effects via the protease activated receptors
(PARs), and especially via PAR1, in a protease dependent manner [75, 77, 95-98], it was
speculated that FXa might mediate its cellular effects through these receptors as well [84, 87,
93, 94, 99-101]. Consistent with this notion are recent studies that demonstrate that FXa
induces Ca2+ release and induces ERK1/2 phosphorylation via PAR1 and/or PAR2 in several non-
lymphoid cells such as human umbilical vein endothelial cells (HUVECs), smooth muscle cells
(SMCs), fibroblasts, human mesangial cells, osteoblasts, keratinocytes and kidney epithelial
cells [82, 97, 100, 102-104].

16 | I n t r o d u c t i o n
PROTEASE ACTIVATED RECEPTORS (PARS)
The PARs are a family of homologous seven transmembrane, G-protein coupled receptors. To
date, four members have been described in mouse and in human - PAR1, PAR2, PAR3 and
PAR4. Unlike most G-protein coupled receptors, activation occurs via proteolytic cleavage of
the extracellular N-terminus, rather than via ligand binding (Figure 3) [105-107]. This cleavage
results in the production of a novel N-terminus that acts as a tethered ligand for the receptor,
with the extracellular portions of the receptor forming the ligand binding site. Upon ligand
binding, a conformation change in the receptor occurs that leads to guanine nucleotide
exchange on associated G proteins and initiates intracellular signalling, the downstream
components of which include Ca2+ release from the ER, and extracellular response kinase 1 and
2 (ERK1/2) phosphorylation. PARs are disposable, single-use receptors that are rarely recycled
to the surface. As such, PAR-activated cells become unresponsive to further proteolytic
signalling, until protein synthesis occurs to replenish the cell membrane [106-108].
Of the four PARs, three are activated by thrombin (PAR1, PAR3 and PAR4) [96-98, 109],
whereas PAR2 can be activated by trypsin [110] and mast cell tryptase [111], and to a lesser
degree by the FVIIA/TF complex [84] and FXa [84, 86, 99-101], but importantly, not by
thrombin. Trypsin can also activate PAR4 [112, 113]. This indicates protease selectivity within
the family.
PARs also comprise an important link between coagulation and inflammation, as they serve as
cellular sensors for serine proteases involved in coagulation and anticoagulation. For instance,
the TF-VIIa bound FXa generated during initiating events of the extrinsic pathway activates


17 | I n t r o d u c t i o n
Figure 3: Structure and mechanism of activation of PARs.
A. Proteolytic cleavage of the extended N-terminus by a protease such as thrombin or FXa
results in a neo-N-terminus that serves as a tethered ligand for the receptor. B. Binding of this
ligand to its binding site (formed by the extracellular domains of the protein) is believed to
trigger a conformational change in the receptor that in turn leads to guanine nucleotide
exchange on associated G proteins (Gαβγ), C, and initiates intracellular signalling.

18 | I n t r o d u c t i o n
endothelial cells via PAR1 or PAR2 [7]. In the anticoagulant PC pathway, thrombin-TM activates
PC bound to EPCR, which functions as a required coreceptor for PCa-mediated signalling
through endothelial cell PAR1 [40].
PARs are expressed in a variety of tissue and cell types, including skeletal muscle vascular and
non-vascular smooth muscle, fibroblasts, endothelial cells, epithelial cells, exocrine glands,
keratinocytes, osteoblasts, astrocytes, neurons, platelets, monocytes, and mast cells [114].
T CELL ACTIVATION AND FUNCTION
In order to appreciate the potential contribution of FXa mediated signalling in T cells to the
overall understanding of immune processes, it is necessary to understand T cell activation.
Armed effector T cells are crucial to almost all adaptive immune responses. Adaptive immune
responses are initiated when naive T cells encounter foreign peptides or antigens, through the T
cell antigen receptor (TCR). These antigens are presented by a cell surface protein of the major
histocompatibility complex (MHC) on the surface of an antigen-presenting cell (APC) [115], that
also expresses the co-stimulatory molecules CD80 and CD86 (B7.1 and B7.2, respectively; Figure
4) [116, 117]. This engagement initiates a series of biochemical events that can induce the naive
T cell to 1) enter into a pathway leading to generation of effector T cells, with the rapid onset of
proliferation and production of effector cytokines (which have a variety of immunological roles)
2) enter into an antigenically non-responsive state known as anergy, or 3) undergo apoptosis by
a process known as activation induced cell death (AICD). In most cases, these first encounters
with antigen are thought to occur with a dendritic cell that has taken up antigen at a site of
infection, migrated to local lymphoid tissue and matured to become a potent activator of naive


19 | I n t r o d u c t i o n
Figure 4: The T cell synapse.
Molecules on the surface of a T cell and counterstructures on an APC involved in T cell
activation form the T cell synapse. The characteristic distribution of cell surface molecules,
which form a supramolecular activation complex (SMAC) is shown. The TCR occupies a central
region known as the cSMAC; a peripheral region, known as the pSMAC, contains adhesion
molecules. Upon adhesion of the T cell to APCs, antigenic remnants are presented to the TCR
via either an MHC Class I molecules or an MHC Class II molecule, that interact with either the
CD8 costimulatory molecule (shown in the diagram) or with the CD4 costimulatory molecule
(not shown), respectively. CTLA4, cytotoxic T lymphocyte antigen 4; ICAM1, intercellular
adhesion molecule 1; LFA, lymphocyte-function associated antigen 1; MHC, major
hsitocompatibility complex; PI(3)K, phosphatidylinositol-3-OH kinase; SHP2, SH2-domain
containing protein tyrosine phosphatase; ZAP70, ζ-chain (TCR)-associated protein kinase, 70
kDa; lck, lymphocyte protein tyrosine kinase; CD, cluster of differentiation.

20 | I n t r o d u c t i o n
T cells. The type of response mounted depends on a variety of factors such as the affinity and
duration of the interaction, and notably the presence or absence of costimulation deriving from
interactions between the CD28 costimulatory receptor on T cells and the B7 molecules on APCs,
as well as between the CD8 or CD4 costimulatory receptors on T cells and MHC Class I or Class II
molecules, respectively, on the APCs. The absence of costimulation renders the naive T cells
anergic. CD28 costimulation, in particular, is recognized as a major T cell costimulatory
pathway. It has been implicated in a variety of T cell responses including T cell proliferation, IL-2
(T cell growth factor) production, prevention of anergy, and the induction of anti-apoptotic
factors [116, 117]. It also plays an important role in B cell differentiation and antibody
production by controlling T cell help provided to B cells and germinal center formation. Finally,
CD28 also directs T cells to sites of infection and inflammation by the production of certain
cytokines and the regulation of cytokine receptors.
All T cell effector functions involve cell-cell interactions. When armed effector T cells recognise
specific antigen on target cells, they release mediators that act directly on the target cell,
altering its behaviour. The triggering of properly activated effector T cells by peptide:MHC
complexes is independent of co-stimulation, so that any infected target cell can be activated or
destroyed by an armed effector T cell. CD8+ cytotoxic T cells kill target cells infected with
cytosolic pathogens, thereby neutralizing pathogen replication. CD4+ T helper 1 cells (Th1)
activate macrophages to kill intracellular parasites. CD4+ Th2 cells are essential in the activation
of B cells to secrete the antibodies that mediate humoral immune responses directed against
extracellular pathogens. Thus, effector T cells control virtually all known effector mechanisms of
the adaptive immune response.

21 | I n t r o d u c t i o n
While costimulation is essential to T cell activation and function, the signalling mechanisms
critical for costimulation remain unclear. Current understanding of the process falls short of
describing exactly how signals delivered by the TCR integrate with signals from coreceptors,
such as CD28. The possibility exists then, for the discovery of missing signalling pathways
comprised of unique components, such as FXa, and highlight the potential contribution of this
thesis to the overall understanding of the process.
RELEVANCE OF WORK
FXa plays a pivotal role in blood coagulation as it serves to amplify the production of thrombin,
which in turn facilitates the formation of a fibrin mesh that contributes to clot formation. In
addition to its procoagulant activity, FXa has also recently been implicated in a variety of
immunomodulatory roles such as inducing inflammatory cytokine expression by and
proliferation of a variety of cells involved in inflammation and the immune response. Consistent
with these observations, recent work done in our lab demonstrated that FXa enhances the
proliferation and cytokine release (IL-2, IL-4 and IFN-γ) of antigen-independently sub-maximally
activated enriched human T cells in vitro, and does so in the absence of added anti-CD28
costimulation, alluding to a potential costimulatory role. These effects were reportedly not due
to thrombin, FX, or FIXa. In addition, through desensitization studies, PAR1 and PAR2 were
implicated as potential FXa-signal mediators. Several questions remained unanswered however.
The individual contributions of CD4+ and CD8+ T cells to the overall effect of FXa on enriched
human T cells remained unclear. Furthermore, as discussed before, in normal physiology, T cells
are activated by APCs in an antigen-dependent fashion. Hence, whether FXa enhanced the

22 | I n t r o d u c t i o n
proliferation of T cells activated in a more physiologically relevant scenario was yet to be
determined. Finally, although receptor-agonist desensitization assays were suggestive of PAR1
and PAR2 involvement in the mediation of the FXa signal, the individual contributions of PAR1
and PAR2 were not clear. A better understanding of the aforementioned will help define a
clearer immunomodulatory role for FXa, and hence, serves as a rationale for the work done in
this thesis.

23 | M a t e r i a l s a n d M e t h o d s
MATERIALS AND METHODS
CELL CULTURE
Jurkat E6.1 (Jurkat T lymphoblast, Clone E6.1, ATCC Cat. No. TIB-152) cultures were maintained
in complete RPMI 1640 [RPMI 1640 (Sigma-Aldrich, R8758) supplemented with sodium
pyruvate (GIBCO, 11360-070), minimal essential amino acids (GIBCO, 11140), L-glutamine
(Wisent Biocenter, 609-065-EL), HEPES buffer (Wisent Biocenter, #330-050-EL), 2-beta-
mercaptoethanol (Sigma-Aldrich,3M-3158), penicillin/streptomycin (Wisent Biocenter, 450-
201-EL), and amphotericin B (Sigma-Aldrich, A2942)] and 10% fetal bovine serum (Wisent
Biocenter, 080150). Medium was changed every 2-4 days depending on cell density (guidelines
followed were as described by ATCC).
Peripheral Blood Mononuclear Cell (PBMC) purification Blood was drawn from suitable donors
into vacuum collection tubes containing sodium-heparin (Vacutainer, BD 366480). The blood
was mixed 1:1 with phosphate buffered saline (PBS; Sigma-Aldrich, D8537) and underwent ficoll
density centrifugation as per manufacturer’s protocol (Ficoll-Paque, GE Amersham, 17-1440-
03). Following centrifugation at 400xg for 30min at 18°C, the buffy coat layer residing between
the plasma/PBS and the ficoll interface was removed and washed extensively with PBS. This
population of cells represents the PBMC population. For T cell purification, the PBMCs were
further subjected to magnetic purification to yield enriched total T cells, or enriched CD4+ or
CD8+ T cell populations (Human T Cell Enrichment Kit (19051), Human CD4+ T Cell Enrichment
Kit (19052), and Human CD8+ T Cell Enrichment Kit (19053), StemCell Technologies).

24 | M a t e r i a l s a n d M e t h o d s
Primary T cell culture for ERK-Phosphorylation assays Enriched T cells were cultured in
complete RPMI 1640 supplemented with 10% fetal bovine serum. In addition, between 10-
50IU/mL Interleukin-2 (IL-2, Peprotech Inc., 200-02) and 2.5ug/mL phytohemagglutinin (PHA-P,
Sigma, L8902) were added. Cells were allowed to grow for 2 days, following another 2 days in
culture without PHA-P, prior to the ERK phosphorylation assay.
FLOW CYTOMETRY
T cell purity Enriched primary T cells were either stained with antibodies against the CD3, CD4,
and CD8 epitopes [Phycoerythrin (PE)-conjugated anti-CD3 mouse IgG1 monoclonal antibody
(mAb, eBioscience, Clone UCHT1, 12-0038-73); Fluorescein Isothiocyanate (FITC)-conjugated
anti-CD4 mouse mAb (BD Bioscience Pharmingen, 555346); and PE-conjugated anti-CD8 mouse
IgG1 mAb (eBioscience, Clone HIT8a, 12-0089-73). Briefly, cells were resuspended in ice-cold
FACS buffer [PBS + 2mM EDTA (Bioshop Canada Inc, EDT 001.500) + 5% FBS) at a concentration
of 1x106 cells/mL. Anti-human CD3-PE, anti-human CD4-FITC or anti-human CD8-PE antibodies
were added to 100uL volumes at 1/50 (v/v) dilution followed by incubation on ice for 30 min
and further washing before analysis.
HLA-A2 typing PBMCs from suitable donors, purified according to the Ficoll-Paque protocol (as
described above), were resuspended in ice-cold FACS buffer at 1x106 cells/mL. A FITC-
conjugated anti-human HLA-A2 Ab (a kind gift of Dr. David Spaner, University of Toronto) was
added to 100uL sample volumes at a dilution of 1/50 (v/v). Following incubation on ice for 30
minutes, the cells were washed with ice cold FACS buffer twice before analysis.

25 | M a t e r i a l s a n d M e t h o d s
Influenza A MP58-66 response Cultured PBMCs were either stained with antibodies against
CD8 epitopes (described above) and/or against the Vβ17 segment of the T Cell Receptor (FITC-
conjugated anti-Vβ17 mouse mAb, Clone E17-5F3, BioDesign International, P91234F), in 100uL
volumes. Briefly, anti-human CD8-PE mAb or anti-human Vβ17-FITC mAb was added at 1/50
(v/v) concentration followed by incubation on ice for 30 minutes, followed by two washes with
FACS buffer. In the case of dual staining, the procedure was repeated with the second antibody.
PAR1 and PAR2 expression Enriched primary T cells were resuspended in ice-cold FACS buffer
at concentration of 1x106 cells/mL. Anti-human PAR1 mAbs, ATAP2-PE (PE-conjugated anti-
human-PAR1 mouse IgG1 mAb, Clone ATAP2, Santa Cruz Biotechnology, SC13503-PE) or
WEDE15 (anti-human-PAR1 mouse IgG1 mAb, Clone WEDE15, Immunotech, Beckman Coulter,
PNIM2085), or an anti-human PAR2 mAb 344222-PE (mouse IgG2a mAb, R&D Systems,
FAB3949P) were added to 100uL samples at a concentration of 1/50 (v/v). Following incubation
on ice for 30 minutes, cells were washed twice with FACS buffer prior to analysis. In the case of
staining with WEDE15 mAbs, cells were stained further with a secondary goat-anti-mouse Ab
(PE-conjugated goat-anti-mouse mAb, BD Biosciences Pharmingen, 550589) for 30 min on ice,
and washed twice with FACS buffer prior to analysis. Appropriate isotype controls pertaining to
all Abs listed above were used as controls (mouse IgG1; Santa Cruz Biotechnology SC3877,
mouse IgG1-PE; Santa Cruz Biotechnology SC2866, mouse IgG2a-PE; R&D Systems 1C003P).
Flow cytometry was performed on a FACSCalibur (BD Biosciences, San Jose, CA) and results
were analyzed using flow cytometry analysis software (FlowJo, Treestar Inc.).

26 | M a t e r i a l s a n d M e t h o d s
ANTIGEN-DEPENDENT STIMULATION
Tetanus Toxoid Assays
Post-phlebotomy, PBMCs from suitable donors were purified by Ficoll-Paque separation as
described previously. A portion of the purified PBMCs were kept aside to be used as APCs.
These cells were resuspended in RPMI + 10% FBS, at room temperature, at 400,000 cells/mL.
50uL (20,000 cells) and were added to wells of a 96-well plate. They were then gamma-
irradiated at 1500 RAD (Nordion Gamma Cell Irradiator, A234). Non-irradiated PBMCs were
added to wells post-gamma-irradiation as a control. The rest of the PBMCs that were not to be
used as APCs, underwent CD4+ T cell enrichment via magnetic separation (as described above).
Enriched CD4+ T cells were then adjusted to 1,000,000 cells/mL in RPMI + 10% FBS. 100uL of
this solution (corresponding to 100,000 CD4+ T cells) were added to the gamma-irradiated and
non-gamma irradiated PBMCs. 25uL of a tetanus toxoid and diphtheria toxoid cocktail (DTT; at
final dilution corresponding to 1/100 in 200uL total volume, Sanofi-Pasteur, DIN 00514462) or
PHA-P at 5ug/mL final concentration were added to wells. FXa (Enzyme Research Laboratories,
HFXa 3460) at concentrations corresponding to 15nM, 25nm, 75nM and 150nM was added to
certain wells. In all cases, total volume was adjusted to 200uL. Cells were seeded in replicates of
4 and grown for 3 days at 37°C, 5% CO2. Cells were then pulsed with 1.0uCi of 3H-Thymidine
(Perkin Elmer, NET027X001MC) for 6 hours at 37°C, and were subsequently harvested on filter
plates ( Unifilter-96, GF/C, Perkin Elmer, 6005174) using and allowed to dry overnight. 25uL of
liquid scintillation cocktail (Microscint, Packard Bioscience Company, 6013611) were added to

27 | M a t e r i a l s a n d M e t h o d s
each well before assessing counts per minute (CPM) using a liquid scintillation counter
(Canberra Packard Top Count NXT, 420221).
Influenza A Matrix Peptide Assay
HLA-A2+ donors were tested further for a response to the Influenza A Matrix Peptide MP58-66
(residues 58-66 of the matrix protein, synthesized by JPT Peptide Technologies GmBH,
Germany). PBMCs from donors were cultured in AIM-V medium (GIBCO, 12055) supplemented
with sodium pyruvate, minimal essential amino acids, L-glutamine , HEPES buffer, 2-beta-
mercaptoethanol, penicillin/streptomycin, and amphotericin B, for two weeks in the presence
of the MP58-66 peptide, or alternately, in the presence of the EBV peptide, BMLF1 (a kind gift
of Dr. Spaner, U of T), as a control, in 6-well plates, at a concentration of 1x106 cells/mL. IL-2 at
various concentrations, between 10IU/ml and 50IU/mL, was added every 3-4 days to certain
samples. After two weeks, cells were counted via a trypan-blue exclusion assay using a
hemacytometer, washed with PBS, and resuspended in ice-cold FACS buffer at a concentration
of 1x106 cells/mL before undergoing cell-surface analysis via flow cytometry. Once positive
responders were identified, the assay was repeated to determine the effect of FXa. Briefly, FXa
was added at various concentrations, between 25nm and 300nM, to certain wells at the start of
the assay, and once again after a week.
ANTIGEN-INDEPENDENT STIMULATION
Post-phlebotomy, PBMCs were purified from donors using ficoll density centrifugation (as
previously described). Half of the purified PBMCs underwent CD8+ T cell enrichment, and half
underwent CD4+ T cell enrichment, using magnetic separation (previously described). Cells were

28 | M a t e r i a l s a n d M e t h o d s
then adjusted to 400,000 cells/mL in AIMV medium. Wells of a 96-well plate were coated with
an anti-human CD3 mAb (OKT3 hybridoma, a kind gift of Dr. Tania Watts, University of Toronto)
and an anti-human CD28 mAb (9.3 hybridoma, a kind gift of Dr. Tania Watts, U of T) for 2 hours
prior to cell plating, and were washed once with PBS. FXa, at various concentrations, between
25nM and 300nM, was added to certain wells. 50uL of the CD4+ or CD8+ cell solution were then
added to wells in replicates of 4. Total volumes were adjusted to 100uL. Cells were then grown
for 2 days at 37°C, 5% CO2, following which cells were pulsed with 1.0uCi of 3H-Thymidine for 6
hours at 37°C. Cells were then harvested on filter plates, as described above, and were allowed
to dry overnight. 25uL of liquid scintillation cocktail were added to wells before assessing CPMs
using a liquid scintillation counter.
REVERSE TRANSCRIPTASE-POLYMERASE CHAIN REACTION (RT-PCR)
Total RNA was extracted from Jurkat E6.1 and primary T cells at 0h or 2h, 6h, 12h, 24h, and 48h
post-stimulation with anti-human CD3 mAb (1ug/mL), and anti-CD3 mAb (1ug/ml) and anti-
human CD28 mAb (5ug/mL) using a total RNA isolation reagent (TRIZOL Reagent, Life
Technologies, Invitrogen, 15596-026) according to manufacturer’s instructions. 2ug of RNA
were pre-treated with RNase-free DNase (Fermentas Life Sciences) prior to cDNA synthesis via
RT-PCR. First-strand synthesis was primed using random hexanucleotides (Fermentas Life
Sciences) with a 10 min annealing incubation at 70°C. 1ug total RNA was then reverse
transcribed in 20uL volumes. 1uL of cDNA from each sample was amplified by PCR using primer
pairs specific for human PAR1 (PAR1 forward, 5’-CGCAGAGCCCGGGACAA-3’; PAR1 reverse 5’-
GATGAACACAACGATGG-3’), and human PAR2 (PAR2 forward 5’-TGCAGTGGCACCATCCAAGG-3’;

29 | M a t e r i a l s a n d M e t h o d s
PAR2 reverse 5’-GCAAACCCACCACAAACA CA-3’).The amount of cDNA synthesized from each
sample was calibrated according to the relative expression of ABL or 18s rRNA, as determined
by agarose gel electrophoresis of RT-PCR products generated using the oligonucleotide primers
ABL forward (5’- CCCAACCTTTTCGTTGCACTGT-3’), ABL reverse (5’-
CGGCTCTCGGAGGAGACGTAGA-3’), 18s rRNA forward (5’-GTAACCCGTTGAACCCCATT-3’) and
18s rRNA reverse (5’-CCATCCAATCGGTAGTAGCG-3’, all oligonucleotide primers were
synthesized by IDT Inc). Amplification by PCR was performed using 2.5 U Taq DNA polymerase
(Choice Taq, Denville Scientific) in a buffer containing MgCl2 (Denville Scientific CB 3702-7) and
the deoxynucleotide phosphates dATP, dTTP, dGTP and dCTP ( Fermentas Life Sciences), using a
thermal cycler (Brinkmann Eppendorf, Model 5345). An initial denaturation step of 4 min at
94°C, followed by 40 cycles of 30 sec at 94°C, 30 sec at 58 °C, and 45 sec at 72°C, with a final
extension step of 10min at 72°C was used. PCR products were separated by electrophoresis on
a 1.8 % agarose (Denville Scientific, CA3510-8) gel in TAE buffer and visualized using 0.5ug/mL
ethidium bromide on a gel imager (Bio-Rad UVP Gel Doc Sys 7500).
ERK PHOSPHORYLATION ASSAYS
Prior to assays, Jurkat E6.1 cells were serum-starved for 18 hours by growing them in medium
without the presence of FBS. For both JE6.1 and primary T cells, ~3x106 cells were used per
sample. Cells were pelleted from culture and resuspended in complete RPMI 1640 at room
temperature. In certain cases, cells were blocked with anti-human PAR1 Abs (mouse mAb clone
ATAP2; Santa Cruz SC13503; and mouse mAb clone WEDE15) and anti-human PAR2 Abs (mouse
mAb clone SAM11; Santa Cruz SC13504) prior to stimulation. For blocking, cells that were

30 | M a t e r i a l s a n d M e t h o d s
pelleted from culture were resuspended at 12x107 cells/mL in PBS in 25uL volumes. Blocking
antibodies were added at various concentrations, followed by incubation on ice for 30min. For
antigen-independent sub-maximal stimulation of T cells, wells of a 12-well plate were pre-
coated overnight with anti-human CD3 Abs (OKT3 mAb) at various concentrations, between
0.05ug/mL and 10ug/mL, and washed once with PBS prior to assay. For antigen-dependent sub-
maximal stimulation of T cells, PHA-P was added to certain wells prior to addition of cells at
various concentrations between 0.1ug/mL and 10ug/mL. FXa was added at various
concentrations, between 25nM and 150nM, to certain wells. Cells were added to wells in total
volumes of 1mL complete RPMI 1640 per well. Following a 10 min incubation at room
temperature, cells were pelleted and lysates were prepared for SDS-PAGE and western blotting
(see below).
SDS-PAGE
Lysates were prepared from cell pellets by agitation on ice for 30 minutes in NP40 lysis buffer
[50mM Tris-HCl (Bioshop Canada, TRS001.1), 150mM NaCl (Bioshop Canada, SOD002.205), 1%
Nonidet P40 detergent (Bioshop Canada, NON505.100)] supplemented with protease inhibitor
cocktail (1ug/mL each of AEBSF.HCL, aprotonin, leupeptin/pepstatin, all purchased from
Bioshop Canada), and phosphatase inhibitors sodium orthovanadate (25mM, Sigma, S6508) and
sodium pyrophosphate (500mM, Sigma Chemical Company, S-9515). Following centrifugation
at 10,000xg for 15 minutes, the supernatants were collected and quantified for protein content
using a Lowry based protein quantification assay (DC Protein Assay Kit, Bio-Rad Laboratories,
500—112). Equal amounts of total protein (10ug) were normalized to the same volume

31 | M a t e r i a l s a n d M e t h o d s
(adjusted with lysis buffer) and mixed 3:1 with sample buffer [1% SDS (Bioshop Canada,
SDS001.500), 10% glycerol (Sigma), 10mM Tris-Cl, 2mM EDTA, 2-ME, Bromphenol Blue, pH
8.0]and boiled for 5 minutes. These were then size-separated electrophoretically on 10% SDS-
PAGE gels run at 90V in SDS running buffer [25mM Tris, 192mM Glycine (Bioshop Canada,
GLN001.5), 0.1% SDS] for 2 – 3 hr. The gel was then equilibrated in transfer buffer [25mM Tris,
192 nM Glycine, 20% Methanol (Caledon Laboratories Ltd, 6701-7), pH7.8] by washing for 5
minutes. Typically gels were electrotransferred overnight to PVDF membranes (Immobilon-P,
Millipore Corporation, IPVH00010) by a wet transfer at 24V. Upon completion of transfer, PVDF
membranes were washed with TBST [Tris buffered saline (50mM Tris-Cl, 150mM NaCl) with 1%
v/v Tween-20 detergent (Bioshop Canada, TWN510.500), 2x5min].
WESTERN BLOTTING
PVDF membranes were blocked non-specifically for 1hr at RT with blocking buffer [TBST + 5%
BSA (Protease-free grade, Bioshop Canada, ALB003.100), pH5.0]. Following washes with TBST
(2x5min), the membrane was incubated overnight, with gentle agitation, in 10mL of a rabbit-
anti-Phospho-ERK antibody (Cell Signaling Technologies, 9101S) solution (1:10,000 v/v dilution
in TBST + 1%BSA). Following washes with TBST (2x5min), the membrane was incubated for 1hr,
with gentle agitation, in 10mL of a goat-anti-rabbit IgG-HRP (horseradish peroxidase; Bio-Rad
Labs, 170-6515) antibody solution (1:20,000 v/v dilution in TBST + 1%BSA). Following further
washes, phospho-ERK1/2 signals were visualized using an enhanced chemiluminescence
detection system (ECL Plus Western Blotting Detection System, GE Healthcare/Amersham,
RPN2132). Prestained standard markers (PageRuler Prestained Protein Ladder, Fermentas Life

32 | M a t e r i a l s a n d M e t h o d s
Sciences, SM0671) were used to verify the approximate molecular weights. All membranes
were stripped for 30 minutes at RT with stripping solution (25mM Glycine-HCl, 1% SDS, pH 2.0)
and washed 2x10min with TBST. Following blocking of non-specific binding with a 1 hr
incubation in blocking buffer, membranes were re-probed with polyclonal anti-total-ERK1/2 Ab
(Cell Signaling Technologies, 4696; 1:1000 v/v dilution) as a loading control.
DATA ANALYSIS
Data are presented as mean +/- SE. Statistical analysis of experimental data was performed
using the two-tailed Student’s t test and the level of significance was set at a probability of
<0.05.

33 | R e s u l t s
RESULTS
FXA ENHANCES THE ANTIGEN-INDEPENDENT PROLIFERATION OF BOTH HUMAN PRIMARY CD4+ AND
CD8+ T CELLS
Previous studies in our laboratory have demonstrated that FXa enhances the proliferation of
enriched human T cells that are activated submaximally in an antigen-independent fashion, i.e.
with anti-human CD3 antibodies that bind to and crosslink the CD3 epitopes that are associated
with the T cell receptor, or in conjunction with anti-human CD28 antibodies that stimulate the
costimulatory molecule, CD28, on the surface of T cells. Importantly, these early results were
not due to thrombin, the direct downstream product of FXa in the coagulation cascade, as no
prothrombin was detected in culture supernatants, no prothrombin transcripts were detected
in T cells, and the effects were not inhibited by lepirudin, a hirudin analog that inhibits
thrombin. It was unclear, however, what the individual contributions of subsets of T cells, CD4+
and CD8+ T cells, were to the overall effect. We wanted to determine if there was cellular
specificity in the response to FXa. Hence, primary human T cells were purified into CD4+ and
CD8+ T cell subpopulations and cultured for 48 hrs in the presence of plate-coated anti-human
CD3 and/or anti-human CD28 antibodies and various concentrations of FXa. Following this, the
cells were pulsed with 3H-Thymidine, a nucleotide analog that is radioactively labelled and
incorporates into sister DNA strands during DNA replication events, and were assessed for
incorporated radioactivity using a liquid scintillation counter. In both CD4+ and CD8+ T cells,
mean counts per minute (CPM) from three donors, based on 4 replicates each, demonstrate
that FXa enhances the proliferation induced by submaximal activation, and that this effect is

34 | R e s u l t s
dose-dependent (Figures 5 and 6). Importantly, the FXa effect occurs in the absence of added
anti-human CD28 antibodies. This, together with the observation that FXa does not induce
proliferation of T cells without prior submaximal activation (Figure 5a) suggests that FXa likely
delivers a costimulatory signal to T cells.
Having showed that the proliferation of both primary human CD4+ and CD8+ T cells is enhanced
in the presence of FXa, we next wanted to determine if the same occurred in response to a
specific antigen. This would represent a more physiologically relevant scenario of T cell
activation as it requires antigen presentation to T cells via APCs, which is how native activation
of T cells typically ensues in vivo.
FXA ENHANCES THE ANTIGEN-DEPENDENT PROLIFERATION OF HUMAN PRIMARY CD8+ T CELLS
The Influenza A Matrix Peptide, residues 58-66 of the core matrix protein of the virus (MP58-
66), was chosen as an antigen for primary human CD8+ T cells due to several convenient
properties. First, the antigen is presented to T cells exclusively via MHC Class I molecules on
APCs, ensuring that only CD8+ T cells are engaged, thereby circumventing the need to purify
CD8+ T cells. There exists allelic restriction, however, as the antigen binds only to derivatives of
the HLA-A*0201 allele [118] (for a review of MHC class of genes, see Introduction). For this
reason, HLA-A2+ donors were first identified by flow cytometry. The typical frequency of HLA-
A2+ donors is around 45% in a Caucasian population, and within an HLA-A2+ population, the
frequency of HLA-A*0201+ individuals is almost 95%. To determine if the donors carried the
HLA-A*0201 allele, they were tested to see if they could mount a response to MP58-66 in vitro.
PBMCs from HLA-A2+ donors were cultured for two weeks in the presence of MP58-66 as well

Donor 3
0
500
1000
1500
2000
2500
150nM Fxa
0.5ug/mL OKT3
Unstim. 0.5ug/mL 9.3
Me
an
CP
M
Donor 3
0
100
200
300
400
500
600
300nM Fxa
Unstim. 2.5ug/mL OKT3
Me
an
CP
M
A
B

35 | R e s u l t s
Figure 5: FXa enhances the proliferation of CD4+ primary human T cells, in vitro.
Primary human CD4+ T cells were stimulated with either 2.5 – 5ug/mL immobilized anti-CD3
(OKT3) mAbs, or with 0.1 – 0.5 ug/mL immobilized anti-CD3 mAbs and 0.1 -0.5 ug/mL
immobilized anti-CD28 (9.3) mAbs, in the presence or absence of 75, 150, or 300 nM FXa.
Proliferation after 48 hours was determined by 3H-thymidine incorporation. A. The addition of
FXa in the absence of anti-CD3 did not induce T cell proliferation. Mean counts (+SE) from three
donors are shown (SE is based on 4 replicates).

Donor 3
0
4000
8000
12000
16000
20000
75nM Fxa
0.5ug/mL OKT3
Unstim. 0.5ug/mL 9.3
Me
an
CP
M

36 | R e s u l t s
Figure 6: FXa enhances the proliferation of CD8+ primary human T cells, in vitro.
Primary human CD8+ T cells were stimulated with either 3.5 – 5ug/mL immobilized anti-CD3
(OKT3) mAbs, or with 0.25 – 0.5 ug/mL immobilized anti-CD3 mAbs and 0.25 -0.5 ug/mL
immobilized anti-CD28 (9.3) mAbs, in the presence or absence of 75, 150, or 300 nM FXa.
Proliferation after 48 hours was determined by 3H-thymidine incorporation. Mean counts (+SE)
from three donors are shown (SE is based on 4 replicates).

37 | R e s u l t s
as various concentrations of IL-2, which was used to amplify any response. To determine
whether there was a response, I took advantage of another convenient property of the MP58-
66 peptide. Studies have shown that the population of CD8+ T cells that proliferate in response
to MP58-66 is skewed heavily (85%) towards those that bear the Vβ17 rearrangement of the
variable region of the TCR [119]. As such, dual staining of PBMCs with an anti-human CD8
antibody and an anti-human Vβ17 antibody, at the start and at the end of the assay, as assessed
by flow cytometry, revealed whether there was skewing within the CD8+ T cell population
towards CD8+/ Vβ17+ T cells, which would indicate that a response to MP58-66 had occurred.
Donors that responded to MP58-66 were then tested further to see whether FXa enhanced the
MP58-66 response. The initial percentage of CD8+/ Vβ17+ within the total CD8+ population,
determined by flow cytometry, typically ranged from between 2-5%. Flow cytometric analysis
shows that FXa significantly enhanced the proliferative response of CD8+ T cells activated by
MP58-66 (Figure 7). In certain donors, FXa enhanced the MP58-66 response between 8-10 fold
more (Figure 7b). Interestingly, it appears that IL-2 signalling might be synergistic with FXa
signalling to some degree, as the response to Xa appears to be masked by the addition of IL-2 in
certain cases (Figure 7b, c). Similar to the results from antigen-independent assays, FXa appears
to be able to stimulate T cells only when they have already been activated submaximally by
antigen, as it has no effect on T cells that have not been exposed to antigen (Figure 7b), an
observation consistent with the notion that FXa provides a co-stimulatory signal to T cells.

A
B Donor 6
C

38 | R e s u l t s
Figure 7: FXa enhances a primary human CD8+ T cell response to Flu MP58-66 antigen, in vitro.
PBMCs were grown for two weeks in the presence or absence of 10ug/mL Flu peptide, 10ug/mL
EBV BMLF1 peptide, 10 IU/mL IL-2, and 75 or 300nM FXa. A. Following this, two-colour flow
cytometry was performed on cell cultures by staining them with anti-human Vβ17 mAbs and
anti-human CD8 mAbs to determine Vβ17 positivity within CD8+ T cell population. Percentage of
double positive (Vβ17+/CD8+), top right quadrant, shows a robust increase. B. Effects of 75nM
FXa and 300nM FXa are shown on cells from Donor 6. Black bars indicate Flu peptide, grey bars
indicate Epstein-Barr virus (EBV) peptide BMLF1, and clear bars indicate no antigen. No
response is seen to FXa in the absence of antigenic stimulation. A robust response is seen even
in the absence of added IL-2 stimulation. C. Results from another donor, Donor 13, show a
robust increase in the response of CD8+/ Vβ17+ T cells to Flu MP58-66 peptide in the absence of
added IL-2 stimulation. The response reaches saturation with added IL-2 stimulation indicating
potential synergism between FXa and IL-2 signalling. Grey bars indicate 25nM FXa, black bars
indicate 300nM FXa, and white bars indicate no FXa. Mean counts (+SE) are shown (SE is based
on 3 replicates).

39 | R e s u l t s
FXA ENHANCES THE ANTIGEN-DEPENDENT PROLIFERATION OF HUMAN PRIMARY CD4+ T CELLS
Next, I wanted to identify whether CD4+ T cells respond to FXa similarly. A cocktail of tetanus
toxoid and diphtheria toxoid (DTT) was chosen as antigen as their presentation to T cells is
restricted via MHC Class II molecules on the surface of APCs [120], which ensures that only CD4+
T cells are engaged. Since 3H-Thymidine incorporation assays were used to measure
proliferation, autologous primary PBMCs that were used as APCs were gamma-irradiated first
to ensure that they did not undergo mitosis, and that any measured proliferation could be
attributed solely to responsive CD4+ T cells (Figure 8b). Suitable human donors were chosen
according to whether they mounted a response to the DTT cocktail, a reflection of their
immunization record. Primary CD4+ T cells were mixed with autologous gamma-irradiated
PBMCs at a ratio of 100,000:20,000 cells and were incubated for three days in the presence of
the various concentrations of the DTT toxoid cocktail. After pulsing the cells with 3H-Thymidine,
cells were assessed for incorporated radioactivity. Once responding donors were identified, the
effect of FXa on submaximally activated CD4+ T cells was evaluated. Data from several donors
demonstrate that FXa enhances the proliferation of primary CD4+ T cells that are activated by
the DTT cocktail (Figure 8). This effect is seen with concentrations of FXa as low as 25nM for all
donors. Similar to previous results, the necessity for submaximal activation of T cells was a
requirement for the effect, as cells that were exposed to FXa without simultaneous antigen-
dependent stimulation showed no proliferative response, again implicating FXa in a
costimulatory role.

A
B Donor 1
APC PHA-P response
0
2000
4000
6000
8000
10000
12000
Gamma-irradiated Non-irradiated
Me
an
CP
M

40 | R e s u l t s
Figure 8: FXa enhances the proliferation of primary human CD4+ T cells in response to DTT.
A. Enriched primary human CD4+ T cells were grown with autologous gamma-irradiated (1500
RAD) PBMCs in the presence or absence of the DTT cocktail and 15, 25, 75, or 150 nM FXa.
Proliferation after 72 hours was determined by 3H-thymidine incorporation. No proliferation is
seen in response to FXa in the absence of antigen. Responses to FXa are seen as low as 25nM in
all donors tested. B. As a control, autologous gamma-irradiated PBMCs were shown to be
unable to undergo mitosis in response to PHA (phytohemagglutinin) compared to non-
irradiated autologous PBMCs, demonstrating that any measured proliferation is attributable
solely to CD4+ T cell populations. Mean counts (+SE) from three donors are shown (SE is based
on 4 replicates).

41 | R e s u l t s
The results so far demonstrated that FXa enhanced the proliferation of T cells that were
activated submaximally in both antigen-independent and antigen-dependent scenarios.
However, as the readouts for the assays above were taken between two days to two weeks
post-stimulation, autocrine and paracrine activation feedback loops within T cell populations
and between T cells and APCs are likely responsible, at least in part, for the amplification of
phenotypic changes, and therefore leave ambiguous the direct consequences of FXa mediated
signalling. A clearer understanding of how FXa interacts with T cells and the nature of the signal
transduction was required. Since the identity of a previously determined putative FXa receptor
on lymphocytes known as EPR-1 was brought under suspicion recently, the obvious next step
was to determine a novel mechanism by which FXa could interact with T cells, thereby possibly
shedding light as to how FXa interacts with T cells and the nature of the signal transduction. As
mentioned before, the PARs have been shown to mediate signals by a variety of serine-
proteases, including FXa, in several non-lymphoid cells. PAR1 and PAR2 have been notably
implicated in FXa mediated signalling. As such, I sought to determine the role of these receptors
as a potential point of interaction between FXa and T cells.
PAR1 AND PAR2 ARE EXPRESSED BY T CELLS
As a preliminary step in evaluating the role that the PARs might play in mediating the FXa signal
in T cells, we wanted to identify whether primary T cells and Jurkat E6.1 cells express PAR1 and
PAR2 on the cell surface. In the ensuing sections of the results, experiments using the Jurkat
E6.1 T lymphoblastic cell-line (JE6.1) were performed in parallel with experiments using primary
human T cells, as results that were obtained using JE6.1 cells were more consistent compared

42 | R e s u l t s
to those using primary human T cells. Enriched primary human T cells and JE6.1 cells were
stained with fluorochrome conjugated antibodies directed against the extracellular N-termini
epitopes of either PAR1 or PAR2 and were evaluated for fluorescence via flow cytometry. The
results indicated that both PAR1 and PAR2 were expressed on both primary human T cells and
JE6.1 cells (Figure 9). Interestingly, the expression of both PAR1 and PAR2 appeared to be
elevated on JE6.1 cells (Figure 9c, f). As these cells lack PTEN (phosphatase and tensin
homologue) leading to constitutive activation of the phosphatidylinositol 3-kinase (PI3K)-
signalling pathway [as reviewed in 121], an important mitogenic pathway, I wanted to
determine whether activated T cells had a distinct PAR1/PAR2 expression profile. As a
preliminary observation, JE6.1 cells, when serum-starved, did not show any increase in the level
of surface PAR2 expression depending on the magnitude and duration of activation (Figure 10).
Thus, the slightly higher expression of PAR2 by JE6.1 cells is likely independent of activation.
PAR1 AND PAR2 MRNA EXPRESSION IS ACTIVATION-INDEPENDENT
To determine further whether PAR expression varied in T cells depending on the state of
activation of the cells, mRNA expression of PAR1 and PAR2 were evaluated in primary human T
cells and Jurkat E6.1 cells at various time-points post-stimulation with anti-human CD3 and anti-
human CD28 antibodies. The time-points were chosen to coincide with possible cellular events
such as any immediate signal transduction that occurs in response to activation stimuli,
downstream responses such as the initiation of protein synthesis, and further downstream
responses such as any phenotypic changes in the cells. Total RNA was harvested from cells,
depleted of genomic DNA, and converted to complementary DNA via reverse transcription


43 | R e s u l t s
Figure 9: PAR1 and PAR2 are expressed on the surface of human primary T cells and JE6.1 cells.
PAR1 and PAR2 surface expression (indicated by green lines) was analyzed by flow cytometry
using the anti-human PAR1 mAbs, ATAP2 (B. and C.) or WEDE15 (A.), and an anti-human PAR2
mAb, 344222 (D., E., and F.), respectively. Unstained controls are indicated by red lines, and
appropriate isotype controls are indicated by blue lines.


44 | R e s u l t s
Figure 10: Activation of JE6.1 cells does not modify PAR2 surface expression.
Jurkat E6.1 cells that were activated by other 1ug/mL immobilized anti-CD3 (OKT3) for 10
minutes (B.) or 6 hours (C.) show no increase in cell surface PAR2 expression (indicated by
green lines), as measured by the anti-human PAR2 mAb 344222, compared to unstimulated
cells (A.). Appropriate isotype controls are indicated by blue lines, and unstained controls are
indicated by red lines.

45 | R e s u l t s
using random hexamer priming. The presence of PAR1 and PAR2 mRNA was confirmed via PCR
amplification of segments of the PAR1 and PAR2 genes. Primers that gave rise to products
spanning both exons were used in order to ensure that there was no genomic DNA
contamination, the presence of which would give rise to a larger amplified product due to the
inclusion of the intron. Subsequent electrophoretic separation and visualization revealed that
PAR1 and PAR2 mRNA expression was visible and roughly constant at all time-points (Figures 11
and 12) indicating that the expression of these proteins, at least at the mRNA level, did not
change with the type and duration of antigen-independent activation. mRNA expression was
normalized by RT-PCR analysis of 18s rRNA and ABL transcripts (Figure 13).
FXA ENHANCES ERK1/2 PHOSPHORYLATION IN T CELLS
One of the downstream signalling events during PAR1/PAR2 receptor cleavage and activation is
the phosphorylation of the MAP kinases, ERK1 and ERK2, which are also downstream signal
transduction components of T cell activation. By demonstrating that ERK1/2 are
phosphorylated in T cells upon exposure to FXa, we could demonstrate a direct and immediate
consequence of FXa mediated signalling, and could further speculate that PAR1/PAR2 may be
involved somehow in the mediation of the FXa signal. A western blotting technique was used to
determine whether, and to what degree, ERK1/2 were phosphorylated upon exposure of
primary human T cells and JE6.1 cells to FXa. Typically, JE6.1 cells were serum-starved prior to
assays to downregulate constitutive activation of the MAPK pathway, thereby allowing any
subtle changes in FXa-induced ERK1/2 phosphorylation to be revealed. Enriched primary human
T cells were first cultured in medium for 4 days to allow background activation of the MAPK

.

46 | R e s u l t s
Figure 11: PAR1 mRNA expression in primary human T cells and JE6.1 cells is not activation-dependent, in vitro.
Primary human T cells and JE6.1 cells were grown in the presence of 1ug/mL anti-CD3 mAbs
with or without 5ug/mL anti-CD28. Total RNA from samples at O hr (10 minutes stimulation),
+2hr, +6hr, +12hr, +24hr and +48hr was harvested and analyzed by RT-PCR using human PAR1-
specific oligonucleotide primers. PAR1 expression by JE6.1 cells and two representative donors
is shown. –RT lanes indicate no genomic DNA contamination.


47 | R e s u l t s
Figure 12: PAR2 mRNA expression in primary human T cells and JE6.1 cells is not activation-dependent, in vitro.
Primary human T cells and JE6.1 cells were grown in the presence of 1ug/mL anti-CD3 mAbs
with or without 5ug/mL anti-CD28. Total RNA from samples at O hr (10 minutes stimulation),
+6hr, +24hr and +48hr was harvested and analyzed by RT-PCR using human PAR2-specific
oligonucleotide primers. PAR2 expression by JE6.1 cells and two representative donors is
shown. –RT lanes indicate no genomic DNA contamination.

A.
B
C.

48 | R e s u l t s
Figure 13: 18s rRNA and ABL mRNA expression in primary human T cells and JE6.1, in vitro.
The expression of the housekeeping genes, 18s rRNA and ABL, was assessed in samples used in
Figure 11., and Figure 12, as a control. RT-PCR analysis was performed using 18s rRNA-specific
and ABL-specific oligonucleotide primers. A. 18s rRNA expression in Donors 1 and 3, B. 18s
rRNA expression corresponding to PAR1 expression in JE6.1 cells, and C. ABL expression
corresponding to PAR2 expression in JE6.1 cells, all indicate similar levels across activation
scenarios. –RT lanes indicate no genomic DNA contamination.

49 | R e s u l t s
pathway (a consequence of the purification method) to subside. Cells were activated
submaximally by either plate-bound anti-human CD3 antibodies or by soluble PHA antigen, and
were simultaneously exposed to FXa at various concentrations. Protein lysates from samples
were evaluated for the presence and degree of ERK1/2 phosphorylation using anti-Phospho-
ERK1/2 antibodies. An anti-Total-ERK1/2 antibody was used as a loading control to normalize
results prior to densitometry analysis. In both human primary T cells and JE6.1 cells that were
submaximally activated, there was a robust increase in the level of ERK1/2 phosphorylation
upon exposure to FXa (Figure 14). Similar to previous findings, there was a requirement for
submaximal activation of T cells in order to see any FXa induced ERK1/2 phosphorylation
(Figure 14a, b). As well, this effect was observed regardless of whether cells were activated
submaximally by plate-bound anti-human CD3 antibody (Figure 14) or by soluble PHA antigen
(Figure 15a), demonstrating that FXa enhances both antigen-independent and antigen-
dependent activation induced ERK1/2 phosphorylation.
PAR2 LIKELY MEDIATES FXA SIGNALLING IN T CELLS
The results thus far were consistent with a model where PAR1 and/or PAR2 mediated the FXa
signal in T cells, but fell short as far as establishing PAR1 or PAR2 as FXa receptors on T cells,
and determining what their individual contributions were. I therefore performed receptor
blocking studies to determine whether the FXa-induced enhancement of ERK1/2
phosphorylation was abrogated when either PAR1 or PAR2 were blocked. ERK1/2
phosphorylation assays were performed as described above using human primary T cells and
JE6.1 cells. However, prior to stimulation, cells were blocked with the PAR1 blocking

Donor 5
Donor 4
Donor 1
Jurkat E6.1 cells

50 | R e s u l t s
Figure 14: FXa induces ERK1/2 phosphorylation in human primary T cells and JE6.1 cells, in vitro.
Primary human T cells or JE6.1 cells were stimulated for 10 minutes in the presence or absence
of 0.1 – 1ug/mL immobilized anti-CD3 (OKT3) mAb, with or without 5ug/mL immobilized anti-
CD28 mAb, with or without 25nM, 75nM, 150nM or 300nM FXa. Lysates were analyzed for
ERK1/2 phosphorylation via western blotting using an anti-phospho-ERK1/2 mAb. Results were
normalized using an anti-total-ERK1/2 mAb and analyzed via densitometry in certain cases.
Results from three donors and JE6.1 cells are shown.

A. Donor 1
B. Jurkat E6.1 cells

51 | R e s u l t s
Figure 15: PAR2 mediates FXa signal in T cells and JE6.1 cells.
Primary human T cells or JE6.1 cells were blocked with an anti-human PAR2 mAb (SAM11) prior
to being stimulated for 10 minutes in the presence or absence of 0.25ug/mL immobilized anti-
CD3 (OKT3) mAb or 0.05ug/mL PHA, with or without 75nM or 150nM FXa. Lysates were
analyzed for ERK1/2 phosphorylation via western blotting using an anti-phospho-ERK1/2 mAb.
Results were normalized using an anti-total-ERK1/2 mAb and analyzed via densitometry.
Blocking of PAR2 results in abrogation of FXa induced ERK1/2 phosphorylation. Results from
one of two representative donors and JE6.1 cells are shown.

52 | R e s u l t s
monoclonal antibodies (mAbs), ATAP2 and WEDE15, or the PAR2 blocking mAb, SAM11. The
ATAP2 and WEDE15 mouse mAbs target the PAR1 tethered ligand domain and the hirudin-like
sequence that promotes thrombin binding and receptor cleavage, respectively. The mouse anti-
human PAR2 mAb SAM11 is raised against amino acid residues 37-50 of PAR2 corresponding to
the extracellular tethered ligand epitope, and has been shown to inhibit Trypsin-induced IL-6
release in human conjunctival epithelial cells (HCECs) by blocking protease activation of PAR2
[122]. Densitometry analysis on western blots revealed that when both primary human T cells
and JE6.1 cells were blocked with anti-human PAR2 (SAM11) antibodies, the FXa-induced
enhancement of ERK1/2 phosphorylation above submaximal activation-induced levels was
abrogated almost completely (Figure 15). These results seemed to suggest that PAR2 plays a
key role in mediating the FXa signal. Studies using PAR1 blocking antibodies were inconclusive,
however, and therefore any role that PAR1 may play in mediating the FXa interaction with T
cells remains unclear (see Discussion).
In summary, it is my hope that the results obtained will help establish a clearer understanding
of the nature of the interaction between FXa and T cells. I have shown that both CD4+ and CD8+
T cells receive a signal from FXa, likely a co-stimulatory signal, which induces an enhanced
proliferative response when the cells are activated submaximally in an antigen-independent
fashion (Figures 5 and 6). Furthermore, I have shown that this effect is observed when T cells
are natively activated through interaction with APCs that present antigen, which represents a
more physiologically relevant scenario. Specifically, FXa enhances the proliferative response of
both CD8+ T cells and CD4+ T cells to Flu MP58-66 antigen (Figure 7) and to diphtheria/tetanus
toxoids (Figure 8), respectively. I have also demonstrated that ERK1/2 phosphorylation in T cells

53 | R e s u l t s
is a direct consequence of their interaction with FXa (Figure 14), thus establishing a more
concrete causal role for FXa in T cell activation. Finally, I have shown that the addition of anti-
human PAR2 blocking antibodies abrogates FXa-induced ERK1/2 phosphorylation (Figure 15),
thereby implicating PAR2 as a key player in the mediation of the FXa signal in T cells.
In the following section, I will discuss the implications of these results and any unresolved
issues. As well, I will discuss possible models of how and where T cells may interact with FXa
that are consistent with the results, and will outline any future studies that will help further
determine the specific nature of the interaction.

54 | D i s c u s s i o n
DISCUSSION
Although a crucial role for FXa in hemostasis is well-established, increasing evidence suggests
that FXa elicits various and complex signalling events on a wide range of cell types by activating
protease-activated receptor (PAR)-1 and PAR-2, which act as receptors for multiple coagulation
factors (see Introduction). Of relevance to this thesis, many of the effects induced by FXa are
proinflammatory in nature [78, 79, 90, 123], and have established FXa as an important link
between coagulation and immune responses. However, further investigation is required in
order to gain a definitive understanding of the role that FXa plays in inflammatory and immune
responses. The work presented in this thesis demonstrates a clear immunomodulatory role for
FXa in T cell function, further highlighting the proinflammatory nature of FXa, and overall,
contributing to the growing body of work that describes the intimate linkage between
coagulation and inflammation.
FXA ENHANCES THE PROLIFERATION OF BOTH CD4+ AND CD8+
T CELLS
From the antigen-independent stimulation studies that I have done, it is clear that FXa can
directly enhance the proliferation of submaximally activated primary human T cells without the
need for antigen presentation through interactions with antigen presenting cells such as
dendritic cells, B cells and macrophages. Importantly, both subsets of T cells, CD4+ and CD8+,
contribute to this effect. Interestingly, this FXa-induced proliferative response is seen in the
absence of added anti-CD28 mAbs, suggesting a costimulatory role for FXa. This notion will be
discussed further in subsequent sections. Physiologically, however, the activation of naive T
cells occurs in response to specific antigenic stimuli mediated via interactions with accessory

55 | D i s c u s s i o n
antigen presenting cells. To address this issue, I have assessed the effect that FXa has on the
proliferation of T cells when the cells undergo antigen-dependent activation. Specifically, I have
shown that FXa enhances the proliferation of both CD4+ and CD8+ T cells in response to the
specific antigens, diphtheria/tetanus toxoid and the influenza A Matrix peptide MP58-66,
respectively. Furthermore, one can speculate from the antigen-independent studies, that FXa is
likely directly affecting the T cells responding to the antigens. However, due to the involvement
of APCs in these assays, we must also consider any effect or interaction that FXa may have with
these cells.
Antigen-dependent activation of naive T cells proceeds both directly, via contact between the T
cell receptor (TCR) and the MHC molecule/ antigen complex on the APC, and the various
costimulatory receptors and their respective ligands, as well as more indirectly, through
paracrine and autocrine cytokine feedback loops between the T cells and the APCs. Previous
studies have demonstrated that FXa has a multitude of proinflammatory effects on a variety of
cell types (see Introduction). Of relevance to the T cell-APC interaction, is the fact that FXa
induces IL-1 release from macrophages, which among other roles, function as antigen
presenting cells. IL-1 is one of three cytokines (IL-1, IL-6, and TNF-α) that are crucial during the
acute phase response of inflammation. During the adaptive phase of an immune response,
however, IL-1 is also crucial to macrophage activation and T helper cell costimulation.
Therefore, FXa that is present during the T cell-APC interaction may enhance the activation of
not only the T cell, but also the macrophage, which in turn could ensue in a positive feedback
loop in activation leading to a stronger response. Indeed, there may be other such FXa induced
proinflammatory effects that are as yet unknown and may serve to enhance, modulate or

56 | D i s c u s s i o n
regulate the interaction between T cells and accessory cells. In the flu-peptide study I have
presented in this thesis, the magnitude of the response may therefore be attributable not only
to the effect that FXa has on responsive CD8+ T cells, but also to the effect that FXa might have
on accessory cells such as B cells, dendritic cells and macrophages, potentially enhancing their
respective responses. Similarly, in the diphtheria/tetanus toxoid assay I have performed,
though APCs cannot undergo proliferation due to gamma irradiation, their ability to release
cytokines, which is preserved at the gamma irradiation level used, may be enhanced in the
presence of FXa thereby, potentially further contributing to the FXa-induced proliferative effect
on CD4+ T cells. As newer studies evaluate the effects of FXa on accessory cells such as dendritic
cells, B cells, and macrophages, a clearer understanding of the role that FXa plays in the T cell
activation milieu will be achieved.
FXA PROVIDES A COSTIMULATORY SIGNAL TO T CELLS
The data presented in this thesis are consistent with a costimulatory role for FXa in T cell
signalling. The strongest argument for this proposal comes from the observation that T cells
must be activated submaximally, either in an antigen-independent fashion via CD3 crosslinking,
or in an antigen-dependent fashion using specific antigenic stimuli, in order for any FXa
enhancement of proliferation to occur. In antigen-independent studies, primary T cells must at
least be activated via CD3 crosslinking to see any FXa induced proliferation. This is an
interesting result, as unlike the antigen-dependent studies where T cells are activated by
accessory cells, here, due to the high purity of the CD4+ and CD8+ T cell populations, the lack of
accessory cells, and the absence of added anti-human CD28 mAbs, one can speculate that it is

57 | D i s c u s s i o n
unlikely that the T cells receive adequate CD28 stimulation. This suggests that FXa signalling
can, to a certain degree, compensate for the lack of CD28 stimulation, in vitro, at least with
regard to proliferation. However, the magnitude of the proliferative response is much greater
when cells undergo both CD3 crosslinking and CD28 stimulation, via added anti-human CD28
antibodies, simultaneously with FXa stimulation, suggesting that while FXa may provide a
costimulatory signal, CD28 signalling represents a more crucial activation signal. Also,
physiologically, it is unlikely that T cell activation proceeds without CD28 stimulation from
accessory cells, as this would render the T cell ‘anergic’ or deactivated. This is consistent with
literature, as to date, no surrogate costimulatory signalling pathway has been demonstrated to
completely replace CD28 signalling.
Further evidence for a costimulatory role for FXa comes from the antigen-dependent
proliferation studies presented in this thesis. FXa robustly enhances the proliferation of
CD8+/Vβ17+ in response to the Flu MP58-66 peptide antigen, but no proliferation is observed in
the absence of antigenic stimulation. These results were similar to the finding that added IL-2,
the major T cell growth factor, could only enhance the proliferation of CD8+/Vβ17+ T cells in the
presence of antigenic stimulation, consistent with a pre-established costimulatory role for IL-2,
and hence, suggestive of the same for FXa. Furthermore, what is interesting is that in the
absence of added IL-2, a dose-dependent response to FXa was much more evident in
comparison to when IL-2 was added, in which case, although a robust response was seen with
the lowest concentration of FXa, a higher dose of FXa did not significantly increase the
response. This is suggestive of potential synergism between the signalling pathways of IL-2 and
FXa as the induced proliferative responses appear to be additive until a threshold is reached,

58 | D i s c u s s i o n
and therefore, further suggestive of a costimulatory role for FXa. This same restriction on FXa-
induced enhancement of proliferation is observed with CD4+ T cells that are activated by the
diphtheria/tetanus toxoids. No CD4+ T cell proliferation was observed in response to FXa
without antigenic stimulation. Taken together, these results are suggestive of a general
costimulatory role for FXa that is not T cell subset-specific.
Lastly, evaluation of ERK1/2 phosphorylation, which is a more immediate and direct indicator of
signal transduction, provides another line of evidence suggesting a costimulatory role for FXa.
Although FXa has been shown to induce ERK1/2 phosphorylation and Ca2+ oscillation on its own
in a variety of non-lymphoid cells through PAR1 and PAR2, the lack of submaximal activation
precludes any FXa-induced effect in T cells. No ERK1/2 phosphorylation is observed in T cells
when they are stimulated with FXa in the absence of antigen-independent or antigen-
dependent submaximal activation. Taking all of the above observations together, it is likely that
FXa mediates a general immunostimulatory effect in T cells. The exact function of FXa,
however, remains undefined.
Several T cell costimulatory roles for FXa can be envisioned. The historical two signal hypothesis
of T cell activation states that naive T cells require at least two signals for proper activation and
immunological function – one through the TCR and associated CD4 or CD8 molecule (depending
on the subset of T cell), and another costimulatory signal through the CD28 molecule. It is now
believed that the two signal model is too simplistic, as proper T cell activation, differentiation
and function is dependent on a multitude of signalling events that occur over a long period in
various physiological environments, and depending on the specific nature of the immune

59 | D i s c u s s i o n
response [124]. A variety of molecules and ligand-receptor pairs, including lymphocyte
function-associated antigen 1 (LFA-1)/ intercellular adhesion molecule (ICAM)-1 [125-127],
CD45 [128], CD2/CD48/CD59 [129], ICOS/B7RP-1 [130], CD40/CD40 ligand [131], 4-1BB/4-1BB
ligand [132,133], and OX40/OX40L [134-137], have thus far been implicated in T cell
costimulation. Furthermore, within hours of activation, additional costimulatory molecules are
upregulated and may serve to sustain or diversify the T cell response [138-141]. However, none
of the alternative costimulatory pathways can completely replace CD28 signalling in resting T
cell activation, but compared to CD28, such alternative costimulatory molecules can act at
different stages of T cell activation and differentiation, on different subsets of T cells, or can
promote the development of different effector functions. FXa may be one such alternative
costimulatory molecule, as I have shown that it can compensate for inadequate CD28
stimulation to activate T cells. It is likely, then, that FXa contributes some accessory interaction
that is separate, but synergistic in some way, to the effect of CD28. What remains to be
determined is when and where FXa signalling in T cells likely occurs, how FXa is presented to T
cells, how the FXa-T cell signal is transduced, and lastly, the significance of such signalling.
PAR2 IS INVOLVED IN FXA SIGNALLING IN T CELLS
In this thesis, I have demonstrated that FXa provides a direct costimulatory signal to T cells
which is reminiscent of earlier reports that suggested a direct effect of FXa on lymphocytes. In
these earlier studies, FXa reportedly contributed to an alternative costimulatory pathway of T
cell proliferation through binding to a novel cellular receptor deemed effector cell protease
(EPR)-1. This putative FXa receptor was identified immunochemically via cross-reacting FV/Va

60 | D i s c u s s i o n
monoclonal antibodies (mAbs) [88], and shown to be expressed on monocytes and monocytoid
cells, neutrophils, natural killer cells, and on a small subset of circulating CD3+ lymphocytes [88,
142]. Cloned as a 337aa protein, EPR-1 was characterized phenotypically as a T cell activation-
dependent antigen and was reported to bind FXa specifically [88, 89]. The inter-EGF sequence
of FXa was identified as the novel recognition site for EPR-1, and the EPR-1 mediated FXa
effects in T lymphocytes and in other cell types were reportedly not dependent on protease
activity and could be mimicked by mAbs and peptides that functioned as surrogate EPR-1
ligands [78, 80, 83, 85, 90, 91, 143-147]. Recent studies, however, have brought the very
identity of EPR-1 into question. The EPR-1 gene could not be detected in the mouse or human
genomes [94]. Furthermore, the cDNA encoding Survivin, an inhibitor of apoptosis, was shown
to be nearly identical to the reverse orientation of the reported EPR-1 cDNA sequence [147].
Moreover, the various EPR-1 detecting mAbs were shown to have non-EPR-1 specificities [88,
89, 145, 146] bringing into question the reported expression patterns of FXa receptors on
lymphocytes and other cells. As well, as the majority of the reported effects were produced
using surrogate EPR-1 ligands (now of unclear specificity) rather than FXa itself, the relationship
of these observations to FXa became unclear. Furthermore, several studies since have
demonstrated that the serine protease activity of FXa is necessary for signalling in endothelial,
vascular and smooth muscle cells [79, 92, 93]. Consistent with these observations, previous
work done in our laboratory demonstrated that the serine protease activity of FXa was
necessary for signalling in human primary T cells. Taking these observations together, it is likely
that EPR-1 does not exist and that FXa signalling is mediated by another mechanism.

61 | D i s c u s s i o n
The PARs are attractive FXa receptor candidates as they have been shown to mediate signalling
by various other coagulation factors, the most well described being thrombin. Furthermore, the
PARs are expressed on a variety of immune cells and several immunological roles for the PARs
have been described, thus establishing them as an important link between blood coagulation
and immune responses.
The role of PAR1, the main receptor for thrombin, has been studied extensively in
pathophysiology over recent decades. FXa and thrombin share PAR1 as a cellular receptor, and
this led to the assumption that FXa signalling would be highly reminiscent of thrombin
signalling. Therefore, the significance of FXa-induced cellular responses remained largely
underexplored, and their contribution to pathophysiological processes was not recognized.
Interest in FXa signalling was ignited after the realization that PAR2, rather than PAR1, acts as a
key player in the progression of a wide pattern of pathologies at the fibro-proliferative interface
(among others). The fibro-proliferative process, the formation of fibrous tissue in a repair or
reactive process, as opposed to formation of fibrous tissue as a normal part of the tissue or
organ, is intimately linked to tissue remodelling, fibrosis and cancer. Because coagulation
cascade activation in general appears to be closely linked to these processes, investigators
started to challenge the concept that the functional consequences of FXa-induced signal
transduction are simply redundant of thrombin, dramatically boosting research linking
coagulation cascade activation to the progression of various diseases. The results of these
efforts have uncovered FXa signalling as a cardinal player in fibro-proliferative pathology and
now have led to the realization that FXa is situated on the crossroads between coagulation and
inflammation and that this is of significance in pathophysiology [as reviewed in 148].

62 | D i s c u s s i o n
An overwhelming amount of data suggests that FXa mediates intracellular signalling via
activation of PAR1 and/or PAR2 (dependent on cell type and concentration used). Several
studies have determined the preferential receptor that mediates FXa-dependent signalling. A
picture emerges that FXa activates PAR2 when engaged in the ternary TF–FVIIa–FXa complex,
whereas soluble FXa activates both PAR1 and PAR2. However, the cell type and the receptor
repertoire on individual cell types is also of major importance for receptor selection by FXa.
Specifically, PAR activation is also tightly regulated by heterologous receptor crosstalk. For
instance, during angiogenesis, TF exerts a negative regulatory control on PAR2 signalling that is
released by the phosphorylation of the cytoplasmic domain of TF. Moreover, alternative
receptors, for instance those of the sphingosine 1-phosphate (S1P) receptor family, might also
modify FXa-dependent PAR activation [as reviewed in 148].
The results presented in this thesis have established a role for PAR2 in mediating FXa signalling
in T cells. An anti-human PAR2 blocking antibody, SAM11, that binds to the tethered ligand
motif in the extracellular portion of PAR2, corresponding to amino acids 37-50, was used to
determine the contribution of PAR2 to FXa signalling in T cells. This antibody has been shown to
inhibit Trypsin-induced IL-6 release in human conjunctival epithelial cells (HCECs) by blocking
protease activation of PAR2 [122]. The results I have presented indicate that when PAR2 is
blocked in primary human T cells and JE6.1 cells, the ERK1/2 phosphorylation that is induced by
FXa signalling is almost entirely inhibited. This is indicative of the preferential use of PAR2 for
FXa signalling in T cells, and is consistent with certain literature. Since studies that I performed

63 | D i s c u s s i o n
using blocking antibodies to PAR1 were inconclusive, largely due to an unexpected mitogenic
effect attributed to the blocking antibodies used, a role for PAR1 in FXa signalling in T cells can
neither be established nor ruled out. Notwithstanding, recent studies have shown that both
PAR1 and PAR2 are involved in soluble FXa signalling. Furthermore, as certain studies have
shown in other cell types, this likely proceeds via intermolecular PAR signalling whereby the
activation of PAR1 transactivates uncleaved PAR2 via the tethered ligand domain of PAR1
(Figure 16). Peptides corresponding to the tethered ligand of PAR1 (SFLLRN) can also activate
PAR2, but not vice versa. It is possible then, that soluble FXa signalling in T cells may proceed
via a similar mechanism where PAR1 is first cleaved and then transactivates PAR2 through the
action of the newly exposed tethered ligand. Thus, depending on whether T cells encounter
soluble FXa or FXa in the context of ternary complexes, there may be differential usage of the
PAR1 and PAR2 receptors. I will speculate as to how FXa in both these contexts may be
presented to T cells, physiologically, in the following section. It remains to be determined what
the consequences of signalling through one or both receptors are.
ROLE OF FXA IN INNATE/ ADAPTIVE IMMUNITY
In order to understand the potential role of FXa-T cell signalling in innate and adaptive immune
responses, it is necessary first to understand the progression of the adaptive immune response
- the events leading to the recruitment of armed effector T cells to the site of local pathogenic
infection. T cells that are recruited to such sites have already been activated into effector cells
by antigen presenting cells that are predominantly comprised of dendritic cells, and to a lesser
degree, macrophages and memory B cells. These antigen presenting cells capture antigen at the


64 | D i s c u s s i o n
Figure 16: PAR1 transactivation of PAR2.
Upon proteolytic cleavage of the extended N-terminus of PAR1 by thrombin, the neo-N-
terminus that serves as a tethered ligand for the receptor transactivates intact PAR2 without
the need for proteolytic cleavage and activation of PAR2.

65 | D i s c u s s i o n
site of infection and then migrate to the downstream lymph node. The delivery of antigen from
a site of infection to downstream lymphoid tissue, and its subsequent presentation to naive T
cells, is actively aided by the innate immune response to infection. This response is rapidly
triggered at the site of infection by non-clonotypic receptors that recognize molecular patterns
that are associated with pathogens but not with host cells. One of the induced responses of
innate immunity is an inflammatory reaction that increases the entry of plasma into the
infected tissues and the subsequent drainage of tissue fluids into the lymph, an interstitial
plasma-like fluid that acts as the circulatory medium for the lymphatic system. Another induced
response is the maturation of tissue dendritic cells that have been taking up particulate and
soluble antigens at the site of infection. These cells are activated through receptors that signal
the presence of pathogen components bound by dendritic cell receptors, or by cytokines
produced during the inflammatory response. The dendritic cells respond by migrating to the
local downstream lymph node and expressing the co-stimulatory molecules that are required,
in addition to antigen, for the activation of naive T cells. Macrophages, which are phagocytic
cells found in the tissues and scattered throughout lymphoid tissue, and B cells, which bind
pathogen components, may be induced similarly through non-specific receptors to express co-
stimulatory molecules and act as antigen-presenting cells. Thus the innate response to infection
hastens the transport of antigens to the local lymphoid tissue, and enables those cells that have
taken up antigen to present it effectively to the naive T cells that migrate through this tissue.
Following this APC/T cell interaction in lymphoid tissue, naive T cells that have been activated
into armed effector T cells, and activated accessory immune cells, then exit the local lymph
node and enter the bloodstream, where they circulate in the blood until they are recruited to

66 | D i s c u s s i o n
the site of infection/injury by binding to inflammation-induced endothelial leukocytic adhesion
molecules. Upon binding to such ‘activated’ vascular endothelial surfaces, effector T cells, as
well as accessory immune cells, penetrate the vascular endothelium and enter the
extravascular site of infection by a process known as diapedesis or extravasation, where they
then engage in an effector immune process specific to the nature of the immunogen.
Interestingly, previous studies have shown that not only do components of the coagulation
system exist in lymph, but also within the germinal centers (GCs) of lymph nodes. In a study
that assessed the composition of rabbit limb lymph, coagulation components such as FX, FVII,
prothrombin, fibrinogen, as well as inhibitory components such as antithrombin and TFPI were
found, some at levels comparable to those found in plasma [149]. Interestingly, though FVIIa-TF
activity, as well as the presence of FXa and fibrinogen were detected, negligible amounts of
fibrin were detected. This, taken together with the high concentrations of TFPI-FXa and
antithrombin, and extremely low concentrations of the cofactors FVIII and FV that were
detected, as well as the insufficient availability of anionic phospholipid residues in the
interstitium that is required for membrane associated procoagulant activity, and the presence
of anticoagulant glycosaminoglycans on lymph endothelium, suggested that under physiological
conditions, extravascular VIIa-TF activation of factor X is prevented from progressing to the
generation of fibrin in the interstitial fluid and lymph of peripheral tissues [149]. This is
consistent with the notion that FXa signalling is not redundant to thrombin signalling, as levels
of generated thrombin would presumably be low due to the relative lack of cofactor V and the
high levels of antithrombin.

67 | D i s c u s s i o n
Furthermore, components of the coagulation system have been detected within the GCs of
lymph nodes, where naive T cells encounter antigen and are activated into effector cells via
interaction with accessory cells [150]. Specifically, FXa has been shown to be localized on the
surface of follicular dendritic cells, macrophages, and lymphocytes, and as well, in proximity to
adjacent T cells within GCs. Importantly, FX was not detectable within the cytoplasm of these
cells, suggesting that detected FXa was not being synthesized by these cells, but rather was
likely being adsorbed from the lymphatic circulation. Consistent with this notion is the
observation that monocytes, precursors to macrophages, can generate and sequester FXa on
their cell surfaces (discussed further below). Since dendritic cells, and to a lesser degree,
macrophages, are key antigen presenting cells and T cell activators, and considering the
localization of FXa in this milieu, it is possible that FXa signalling in T cells occurs at the very
onset of T cell activation, thereby potentially representing an important initial costimulatory
signal. Considering the proliferative effect of FXa on T cells that I have demonstrated, perhaps
FXa in germinal centers provides a costimulatory signal to T cells that contributes towards their
rapid clonal expansion as effector T cells.
FXa signalling in T cells may also be relevant to T cell effector function at the site of injury,
where both blood clotting, as well as the induction of immune/ inflammatory responses are
required. At sites of injury, abundant amounts of FXa would be generated at the site of injury
through the action of the blood pro-coagulant pathways. In order to avoid occlusion of the
blood vessel, coagulation would be localized to the specific site of vascular injury, likely
extending into the immediate adjacent extravascular area. In addition to local pro-coagulant
and tissue repair activities, should the innate immune response fail to neutralize the particular

68 | D i s c u s s i o n
immunogen whose entry accompanied the vascular damage, an adaptive immune response
would ensue whereby effector T cells, and accessory immune cells, would be recruited to the
site of vascular injury ensuing in a localized immune response. Due to the proximity of
simultaneous procoagulant activity, such recruited T cells would likely encounter FXa at these
sites. One might suggest, therefore, that FXa signalling at these sites might function to
enhance/ ensure sustained effector T cell activity by maintaining a proliferative and cytokine-
releasing response. Taken together, therefore, one can envision FXa playing a role in both the
initial T cell selection/activation within lymphoid tissue, as well as in T cell effector function
within the site of injury. How a T cell might interact with FXa in the above scenarios is discussed
below.
T cells could presumably encounter FXa in soluble form, or as part of a membrane-associated
ternary complex such as the TF-VIIa-FXa, FIXa-FVIIIa-FXa and FVa-FXa complexes, whose
formation is crucial to procoagulant processes. Since soluble FXa was used in all of the
experiments that I have presented in this thesis, it is likely that, at least in vitro, FXa can
mediate its cellular effects without the need for association with ternary complexes. However,
it is unclear whether direct binding of FXa to T cells is required for its T cell activity, or whether
an alternative interaction is sufficient. During the initiating events of blood coagulation, FX is
converted to its active form FXa by either the TF-VIIa ternary complex on endothelial surfaces,
the FIXa-FVIIIa ternary complex on the surface of platelets, or by the Mac-1 complex on the
surface of monocytes. Importantly, the association of FX with these complexes is crucial to its
biological activity during coagulation. In the former two scenarios, in order for FX to associate
with these complexes, it must first bind to the respective cellular surfaces (reviewed in

69 | D i s c u s s i o n
Introduction). This association is achieved initially through the binding of calcium to the γ-
carboxyglutamic acid (Gla) domain of FX, which then facilitates the binding of FX to
phospholipids on the respective cellular surface. Bound FX is then able to associate with the TF-
VIIa and FIXa-FVIIIa ternary complexes, whereby it is activated. It is possible that soluble FXa
present in lymph nodes, or at the interface of coagulation and inflammatory processes, which
are induced by an injury, might bind to T cells in the same way via its Gla domain. Through
subsequent, or activation-related cell surface rearrangement in T cells, FXa could then associate
with either PAR1 or PAR2. This notion is consistent with literature demonstrating the
involvement of both PAR1 and PAR2 in soluble FXa signalling.
FXa may also be presented to T cells while associated with the ternary complexes mentioned
above. Monocytes, which are precursors to macrophages, may present FXa to T cells via the TF-
VIIa complex. It has been shown that FXa can induce the expression of TF on monocytes,
representing an important link between coagulation and inflammation. Monocytes that
produce TF on their surfaces can then contribute to procoagulant activities through the
formation of the TF-VIIa complex that leads to the formation of FXa. A unique feature of the TF
initiation reaction is the transient stability of the TF-VIIa-FXa product complex that exists prior
to the release of produced FXa. The TF-VIIa-FXa complex can be trapped with a highly specific
nematode-derived inhibitor, NAPc2, which stabilizes the ternary complex by inhibiting FVIIa,
while maintaining FXa in a catalytically active confirmation [151]. The NAPc2-stabilized ternary
complex has been shown to signal predominantly through PAR2 on cytokine-stimulated
endothelial cells. Quantitative analysis of the dose-response of cell signalling induced by free
FXa vs. FXa that is associated transiently with TF-VIIa in the initiation complex, demonstrated at

70 | D i s c u s s i o n
least 5-fold enhanced cell signalling with the ternary TF-VIIa-FXa complex. Cell signalling is
coupled directly to the mechanism of the TF-dependent initiation of coagulation. If we envision
an injury scenario similar to the one described in the preceding section, monocytes that are
bound transiently to FXa in this way may come into contact with effector T cells in extravascular
sites. They may also migrate to the local draining lymph node and come into contact with, and
activate naive T cells into effector T cells via antigen presentation.
Alternatively, as mentioned earlier, monocytes have the ability to generate FXa on their cell
surface by the catalytic activation of FX upon its binding to the Mac-1 complex on the
monocytic cell surface (see Introduction). Importantly, any FXa that is generated this way
remains bound to the complex whereby it promotes procoagulant activity and thrombin
formation. Similar to the previous scenario, monocytes that retain FXa at their surfaces may
migrate to local draining lymph nodes and activate naive T cells via antigen presentation. Also,
in a scenario in which both coagulation and inflammation processes are triggered, such as in
the case of an injury, monocytes that have generated FXa in such a way and are involved in the
inflammatory response, may come into contact with responder T cells. Although, the work
presented in this thesis is highly suggestive of PAR2 involvement in FXa signalling in T cells
(discussed previously), the exact nature of this interaction is unknown. Specifically, although
FXa likely interacts directly with PAR2 by cleaving the N-terminus portion and revealing a
tethered ligand, it is unclear whether FXa binds to PAR2 or to an accessory receptor on the T
cell first, or whether it is presented to the T cell by an accessory cell. For example, if FXa
remains bound to monocytes via the Mac-1 complex, the direct contact that monocytes and T
cells share during immune function may obviate the need for FXa binding to PAR2. In such a

71 | D i s c u s s i o n
scenario, FXa bound to monocytes may activate PAR2 on T cells while the cells are undergoing
reciprocal activation. This interaction would likely occur in extravascular areas that are not host
to the full complement of coagulation proteases. Both the preceding models are consistent
with the observed requirement for pre-activation of T cells as a prerequisite for FXa signalling.
The scenarios above are consistent with a ‘temporal engagement’ model of T cell activation and
effector function that predicts that signalling from two or more molecules are required
sequentially over an extended time frame to ensure a long lasting differentiated T cell mediated
immune response. I have shown that FXa enhances the proliferative response of both CD4+ and
CD8+ T cells in response to antigen, indicating a general costimulatory action on T cells.
Therefore, FXa signalling may serve to provide an initial costimulatory signal to naive T cells, or
to enhance the immune function of recruited effector T cells, by inducing a greater proliferation
rate and enhancing cytokine release (previously shown in our lab), and thereby potentially
expediting the removal of the infectious agent.
CONCLUSIONS
In summary, the work presented in this thesis further establishes FXa as an important signalling
molecule in inflammatory and immune responses. I have expanded on established literature
and shown that FXa delivers a general costimulatory signal to both CD4+ and CD8+ primary
human T cells, and can induce proliferation in these cells even in the absence of added CD28
stimulation. Furthermore, I have shown that this effect is direct and immediate as indicated by
rapid upregulation of ERK1/2 phosphorylation in human primary T cells in response to FXa
signalling. Lastly, I have established that FXa signalling in T cells is likely mediated by PAR2,

72 | D i s c u s s i o n
further implicating the PAR family of receptors as coagulation factor sensors, and modulators of
immune and inflammatory responses. FXa signalling in T cells likely becomes important during
‘dirty wound’ scenarios when procoagulant and immune process must be mounted
simultaneously. A modulated immune response may be necessary in this scenario. Thus, taken
together, FXa likely functions not only as an indicator of nearby coagulation processes, but
directly as an immunomodulatory agent, and as such, a better understanding of the role of FXa
in immune responses may lead to new therapeutic insights into modulation of immune
responses.
FUTURE WORK
In this thesis, I have expanded further on previous studies and have elucidated an
immunomodulatory role for FXa in T cell function. These results are preliminary, however, and
require further investigation, validation, and expansion into in vivo models to determine the
physiological significance of such interactions. Notwithstanding, I have presented plausible
mechanistic explanations for how and where T cells in the body might encounter FXa, and as
well have speculated as to the nature, outcome and biological reason for such an interaction. It
would thus be prudent to evaluate these models in order to gain a clearer understanding of the
involvement of FXa in immune responses.
To begin with, although the results I have presented are indicative of PAR2 involvement in FXa
signalling in T cells, further studies are required to determine whether PAR2 is solely
responsible for the propagation of the FXa signal, or whether it works in conjunction with PAR1
via transactivation, both scenarios of which are consistent with literature. Genetic approaches

73 | D i s c u s s i o n
such as the use of siRNA downregulation of PAR1 and PAR2, PAR1-/- and/or PAR2 -/- gene
knockout, or inducible repression through the Tet-Off system in T cells might help determine
the individual contributions of these receptors to FXa signalling, as would evaluation of FXa
signalling in T cells from PAR1 and/or PAR2 knockout mice, which have previously been
characterized [152-157].
Another question that would be worth exploring is whether FXa binds to the PARs or accessory
receptors, or whether it binds directly to the cell surface, as it does during procoagulant
activities, and then associates with the PARs. Co-immunoprecipitation of lysates from T cells
that are crosslinked to FXa may answer the question of whether FXa binds to PAR1 or PAR2, a
requirement for thrombin signalling via PAR1. PAR proteins from lysates could be
immunoprecipitated first, and then probed with an anti-FXa antibody to determine whether
FXa remains associated. Alternatively, as I have speculated before, FXa may bind to the
phospholipid bilayer of T cells through its Gla domain, an event that is crucial to its
procoagulant activity, and then associate with the PARs. A Gla-domain-less version of FXa,
designated des-Gla-FXa, which has been shown to be unable to bind to the cell surface of
platelets, can be used to determine if FXa signalling is abrogated when binding to phospholipid
is disrupted [158]. Alternatively, Annexin V, which has a strong affinity for negatively charged
phospholipids and has been shown to potently inhibit FX binding to platelet surfaces, can be
used to disrupt any potential FXa association with phospholipids [158].
Finally, although I have shown that FXa signalling is likely physiologically relevant as it enhances
the proliferative response of T cells to specific antigen, it would be worth exploring whether FXa

74 | D i s c u s s i o n
induces modified CD4+ and CD8+ T cell effector function, which is a downstream consequence
of T cell activation. To begin with, evaluation of any transcriptional events and ensuing protein
synthesis downstream of FXa signalling through the use of gene expression microarrays and
proteome arrays may provide insight into any modulation of T cell function due to FXa
signalling. These assays may also shed light onto any potential crosstalk between downstream
components of PAR signalling and TCR signalling. 51Chromium release cytotoxicity assays can
also be performed with specific antigens, like the Influenza A virus, to determine whether the
effector function of cytotoxic T cells is modulated in the presence of FXa. Furthermore, as
mentioned before, in order to fully understand the role FXa plays in immune responses, one
should also consider the effect that FXa might have on accessory cells such as dendritic cells, B
cells and macrophages. Studies that evaluate the effect of FXa on the proliferation, cytokine
release, surface expression profiles, and antibody production (in the case of B cells) of these
cells may be invaluable in gaining a more complete understanding of the role FXa plays in the T
cell activation milieu.
The results presented in this thesis, however, have defined a clearer immunomodulatory role
for FXa and furthermore have provided insights into how FXa interacts mechanistically with T
cells. Future studies that further explore these processes will not only lead to a better
understanding of the immune system and how it is intimately linked with coagulation
processes, but also provide insight into potential therapeutic developments.

75 | R e f e r e n c e s
REFERENCES
1. Dugina, T.N., et al., Receptors of the PAR family as a link between blood coagulation and inflammation. Biochemistry (Mosc), 2002. 67(1): p. 65-74
2. Cicala, C. And Cirino, G., Linkage between inflammation and coagulation: an update on the molecular basis of crosstalk. Life Sci, 1998. 62(20): p. 1817-24
3. McGilvray, I.D. and O.D. Rotstein, Role of the coagulation in the local and systemic inflammatory response. World J Surg, 1998. 22(2): p 179-86
4. Esmon, C. T., Inflammation and thrombosis. J Thromb Haemost, 2003. 1(7): p. 1343-8
5. Davie, E.W., Fujikawa, K., and Kisiel, W., The coagulation cascade: initiation, maintenance, and regulation. Biochemistry, 1991. 30(43): p. 10363-70
6. Furie, B, and Furie, B.C., The molecular basis of blood coagulation. Cell, 1988. 53(4): p. 505-18
7. Davie, E.W., Biochemical and molecular aspects of the coagulation cascade. Thromb Haemost, 1995. 74(1): p. 1-6
8. King, M.W.a.M., S. 1996
9. Giesen, P.L., et al., Blood-borne tissue factor: another view of thrombosis. PNAS, 1999. 96(5): p. 2311-5
10. Esmon, C.T., Thombomodulin as a model of molecular mechanisms that modulate protease specificity and function at the vessel surface. Faseb J, 1995. 9(10): p. 946-55
11. Huang, Z.F., et al., Tissue factor pathway inhibitor gene disruption produces intrauterine lethality in mice. Blood, 1997. 90(3): p. 944-51
12. Broze, G.J. Jr., Girard, T.J., and Novotny, W.F., Regulation of coagulation by a multivalent Kunitz-type inhibitor. Biochemistry 1990. 29(33): p. 7539-46
13. Sanset, P.M., et al., Immunodepletion of extrinsic pathway inhibitor sensitizes rabbits to endotoxin induced intravascular coagulation and the generalized Shwartzman reaction. Blood, 1991. 78(6): p. 1496-502
14. Broze, G.J., Jr., The role of tissue factor pathway inhibitor in a revised coagulation cascade. Semin Hematol, 1992. 29(3): p. 159-69
15. Lawson, J.H., et al., Complex-dependent inhibition of factor VIIa by antithrombin III and heparin. J Biol Chem, 1993. 268(2): p. 767-70
16. Rapaport, S.I. and Rao, L.V., Initiation and regulation of tissue factor-dependent blood coagulation. Arterioscler Thromb, 1992. 12(10): p. 1111-21
17. Hematology, Pathophysiologic Basis for Clinical Practice. Third ed, ed. S.H.a.R. Robinson, P.R. 1993, Boston: Little, Brown and Company Inc.
18. Owen, W.G. and Esmon, C.T., Function properties of an endothelial cell cofactor for thrombin-

76 | R e f e r e n c e s
catalyzed activation of protein C. J Biol Chem, 1981. 256(11): p. 5532-5.
19. Jesty, J., et al., Initiation of the tissue factor pathway of coagulation in the presence of heparin: control by antithrombin III and tissue factor pathway inhibitor. Blood, 1996. 87(6): p. 2301-7
20. Esmon, C.T., Hemostasis and thrombosis: basic principles and clinical practice, ed. R.W. Colman, Hirsh, J., Marder, V.J., CLowes, A.W., and George, J.N. 2001, Philadelphia: Lippincott Williams and Wilkins. 335-353
21. Lijnen, H.R. and Collen, D. Mechanisms of physiological fibrinolysis. Baillieres Clin Haematol, 1995. 8(2): p. 277-90
22. Lijnen, H.R. and Collen, D., Interaction of plasminogen activators and inhibitors with plasminogen and fibrin. Semin Thromb Hemost, 1982. 8(1): p. 2-10
23. Taylor, F.b., Jr., et al., Endothelial cell protein C receptor plays an important role in protein C activation in vivo. Blood, 2001. 97(6): p.1685-8
24. Dano, K., et al., Plasminogen activators, tissue degradation, and cancer. Adv Cancer Res, 1985. 44: p.139-266.
25. Preissner, K.T., Physiological role of vessel wall related antithrombotic mechanisms: contribution of endogenous and exogenous heparin-like components to the anticoagulant potential of the endothelium. Haemostasis, 1990. 20 Suppl 1: p. 30-49
26. Nagashima, M., et al., Thrombin-activatable fibrinolysis inhibitor (TAFI) deficient mice. Front Biosci, 2002. 7: p.d556-68
27. Mann, K.G., et al., Surface-dependent reactions of the vitamin K-dependent enzyme complexes. Blood, 1990. 76(1): p. 1-16
28. Van der Poll, T., et al., Activation of coagulation after administration of tumor necrosis factor to normal subjects. N Engl. J. Med., 1990 322(23): p. 1622-7
29. Altieri, D.C., Inflammatory cell participation in coagulation. Semin. Cell Biol., 1995. 6(5): p. 269-74
30. Fink, M.A., Anaphylaxis in the mouse: possible relation of the Schultz-Dale reaction to serotonin release. Proc. Soc. Biol. Med., 1956. 92(4): p. 673-5
31. Collier, H.O., Prostaglandins and aspirin. Nature, 1971. 232 (5305): p. 17-9
32. Crunkhorn, P. And Willis, A.L., Cutaneous reactions to intradermal prostaglandins. Br. J. Pharmacol, 1971. 41(1): p. 49-56
33. Vane, J.R., Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat. New Biol., 1971. 231(25): p. 232-5
34. Williams, T.J., Prostaglandin E2, prostaglandin I2 and the vascular changes of inflammation.Br. J. Pharmacol., 1979. 65(3): p. 517-24
35. Lewis, T., Blood vessels of the human skin and their responses. 1927, London: Shaw and Sons Ltd.

77 | R e f e r e n c e s
36. Vugman, T., Histamine and antihistaminics., in Handbook of Experimental Pharmacology., M. Rocha e Silva, Editor. 1966, Springer Verlag: New York. P. 367-385
37. Opal, S.M., and Esmon, C.T., Bench-to-bedside review: functional relationships between coagulation and the innate immune response and their respective roles in the pathogenesis of sepsis. Crit. Care, 2003. 7(1): p. 23-38
38. Morrissey, J.H., et al., Molecular cloning of the cDNA for tissue factor, the cellular receptor for the initiation of the coagulation protease cascade. Cell, 1987. 50(1): p. 129-35
39. Sadler, J.E., Thrombomodulin structure and function. Thromb Haemost, 1997. 78(1): p. 392-5.
40. Oganesyan, V., et al., The crystal structure of the endothelial protein C receptor and a bound phoshoplipid. J Biol Chem., 202. 277(28): p. 24851-4
41. Plescia, J., and Altieri, D.C., Activation of Mac-1 (CD11b/CD18)-bound factor X by released Cathepsin G defines an alternative pathway of leukocyte initiation of coagulation. J. Biochem., 1996. 319 (Part 3): p. 873-9
42. Altieri, D.C., and Edgington, T.S., The saturable high affinity association of Factor X to ADP-stimulation monocytes defines a novel function of the Mac-1 receptor. J Biol. Chem., 1988. 263 (15): p. 7007-15
43. Altieri, D.C., Morrissey, J.H., and Edgington, T.S., Adhesive receptor Mac-1 coordinates the activation of Factor X on stimulated cells of monocytic and myeloid differentiation: an alternative initiation of the coagulation protease cascade. PNAS USA, 1988. 85(20): p. 7462-6
44. Drake, T.A., Morrissey, J.H., and Edgington, T.S., Selective cellular expression of tissue factor in human tissues. Implications for disorders of hemostasis and thrombosis. Am. J. Pathol., 1989. 134(5): p. 1087-97
45. Furie, B., et al., Molecular and cellular biology of blood coagulation. N Engl J Med., 1992. 326(12): p. 800-6
46. Camerer, E., Kolsto, A.B., and Prydz, h., Cell biology of tissue factor, the principal initiator of blood coagulation. Thromb. Res., 1996 81(1): p. 1-41
47. Nachman, R.L., Platelets. A Multidisciplinary Approach., ed. G.a.G. de Gaetano, S. 1978, New York: Raven Press. 161-197
48. Willis, A.L., Inflammation, Experimental Handbook of Pharmacology., ed. J.R.a.F, Vane, S.H. 1978, New York: Springer Verlag. 138-189
49. Loppnow, H., et al., Platelet-derived interleukin-1 induces cytokine production, but not proliferation of human vascular smooth muscle cells. Blood, 1998. 91(1): p. 134-41
50. Henn, V., et al., CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells. Nature, 1998. 391(6667): p. 591-4
51. Aukrust, P., et al., Inflammatory role of platelets in acute coronary syndromes. Heart, 2001. 86(6): p. 605-6.
52. Osterud, B., Tissue factor expression by monocytes: regulation and pathophysiological roles. Blood

78 | R e f e r e n c e s
Coagul. Fibrinolysis, 1998. 9 Suppl 1: p. S9-14
53. Altieri, D.C., Coagultion assembly on leukocytes in transmembrane signalling and cell adhesion. Blood, 1993. 81(3): p.569-79.
54. Sims, P.J., et al., Complement proteins C5b-9 cause release of membrane vesicles from the platelet surface that are enriched in the membrane receptor for coagulation factor Va and express prothrombinase activity. J. Biol. Chem, 1988. 263(34): p. 18205-12
55. Fukudome, K., et al., Identification, cloning, and regulation of a novel endothelial cell protein C/activated protein C receptor. J Biol Chem, 1994. 269(42): p. 26486-91
56. Conway, E.M. and Rosenberg, R.D., Tumor necrosis factor suppresses transcription of the thrombomodulin gene in endothelial cells. Mol. Cell Biol., 1988 8(12): p. 5588-92
57. Burstein, S.A., Cytokines. Platelets, 1997. 8: p. 93-104
58. Esmon, C.T., Crosstalk between inflammation and thrombosis. Maturitas, 2004. 47(4): p. 305-14
59. Ruf, W., Protease-activated receptor signalling in the regulation of inflammation. Crit. Care Med., 2004. 32(5th Suppl.): p. S287-92
60. Grey, S., et al., Selective effects of protein C on activation of human monocytes by lipopolysaccharide, interferon-gamma, or PMA: modulation of effects on CD11b and CD14 but not CD25 or CD54 induction. Transplant Proc., 1993. 25(5): p. 2913-4
61. Yuksel, M., et al., Activated protein C inhibits lipopolysaccharide-induced tumor necrosis factor-alpha production by inhibiting activation of both nuclear factor-kappa B and activator protein-1 in human monocytes. Thromb Haemost., 2002. 88(2): p. 267-73
62. Taoka, Y., et al., Activated protein C reduces the severity of compression-induced spinal cord injury in rats by inhibiting activation of leukocytes. J. Neurosci., 1998. (18(4): p. 1393-8
63. White, B., et al., Activated protein C inhibits lipopolysaccharide-induced nuclear translocation of nuclear factor kappaB (NF-kappaB) and tumor necrosis factor alpha (TMF-alpha) production in the THP-1 monocytic cell line. Br J Haemotol, 2000. 110(1): p. 130-4.
64. Joyce, D.E., et al., Gene expression profile of antithrombotic protein C defines new mechanisms modulating inflammation and apoptosis. J Biol Chem, 2001. 276(14): p. 11199-203
65. Bar-Shavit, R., et al., Localization of a chemotactic domain in human thrombin. Biochemistry, 1984. 23(3): p. 397-400
66. Kudahl, K., Fisker, S., and Sonne, O., A thrombin receptor in resident rat peritoneal macrophages. Exp. Cell Res., 1991. 193(1): p. 45-53
67. Bar-Shavit, R., et al., Monocyte chemotaxis: stimulation by specific exosite region in thrombin. Science, 1983. 220(4598): p. 728-31
68. Strukova, S.M., et al., Thrombin-mediated events implicated in mast cell activation. Sem. Thromb. Hemost., 1996 22(2): p. 145-50

79 | R e f e r e n c e s
69. Lorant, D.E., et al., Coexpression of GMP-140 and PAF by endothelium stimulated by histamine or thrombin: a juxtacrine system for adhesion and activation of neutrophils. J. Cell Biol., 1991. 115(1): p. 223-34
70. Pendurthi, U.R., Alok, D., and Rao, L.V., Binding of factor VIIa to tissue factor induces alterations in gene expression in human fibroblast cells: up-regulation of poly(A) polymerase. PNAS USA, 1997. 94(23): p. 12598-603
71. Andre, P., et al., CD40L stabilized arterial thrombi by a beta3 intergrin-dependent mechanism. Nat Med, 2002. 8(3): p. 247-52.
72. Miller, D.L., Yaron, R., and Yellon, M.J.,l CD40L-CD40 interactions regulate endothelial cell surface tissue factor and thrombomodulin expression. J. Leukoc. Biol., 1998. 63(3): p.373-9
73. Burstein, S.A., Cytokines, platelet production and hemostasis. Platelets, 1997. 8:p.93-104
74. Drake, W.T., et al., Thrombin enhancement of interleukin-1 and tumor necrosis factor-alpha induced polymorphonuclear leukocyte migration. Lab Invest, 1992. 67(5): p. 617-27
75. McNamara, C.A., et al., Thrombin stimulates proliferation of cultured rat aortic smooth muscle cells by proteolytically activated receptor. J Clin Invest, 1993 91(1): p. 94-8
76. Weiss, R.H., and Nuccitelli, R., Inhibition of tyrosine phosphorylation prevents thrombin-induced mitogenesis, but not intracellular free calcium release , in vascular smooth muscle cells. J. Biol. Chem., 1992. 267(8): p. 5608-13
77. Derian, C.K., et al., Thrombin regulation of cell function through protease-activated receptors: implication for therapeutic intervention. Biochemistry (Mosc), 2002. 67(1): p. 56-64
78. Cirino, G., et al., Factor Xa as an interface between coagulation and inflammation. Molecular mimicry of factor Xa association with effector cell protease recetpro-1 induces acute inflammation in vivo. J Clin Invest, 1997. 99(10): p. 2446-51.
79. Senden, N.H., et al., Factor Xa induces cytokine production and expression of adhesion molecules by human umbilical vein endothelial cells. J Immunol, 1998. 161(8): p. 4318-24.
80. Blanc-Brude, O.P., et al., Factor Xa is a fibroblast mitogen via binding to effector-cell protease receptor-1 and autocrine release of PDGF. AM J Physiol Cell Physiol, 2001. 281(2): p. C681-9
81. Jones, A. and Geczy, C.L., Thrombin and factor Xa enhance the production of interleukin-1. Immunology, 1990. 71: p. 236–241
82. Tanaka, M., Arai, H., Liu, N.., Nogaki, F., Nomura, K., Kasuno, K., Oida, E., Kita, T., and Ono, T., Role of coagulation factor Xa and protease-activated receptor 2 in human mesangial cell proliferation. Kidney International, 2005. 67: p. 2123-2133
83. Altieri, D.C., and Stamnes, S.J., Protease-dependent T cell activation: ligation of effector cell protease receptor-1 (EPR-1) stimulates lymphocyte proliferation. Cell Immunol., 1994. 155(2): p. 372-83
84. Riewald, M., and Ruf, W., Mechanistic coupling of protease signalling and initiation of coagulation by tissue factor. PNAS USA, 2001. 98(14): p.7742-7

80 | R e f e r e n c e s
85. Bono, F., et al., Factor Xa activates endothelial cells by a receptor cascade between EPR-1 and PAR-2. Arteroscler Thromb Vasc Biol, 2000. 20(11): p. E107-12
86. Camerer, E., et al., Coagulation factors VIIa and Xa induce cell signalling leading to up-regulation of the egr-1 gene. J Biol Chem, 1999. 274(45): p. 32225-33.
87. Ambrosini, G., et al., Activation-dependent exposure of the inter-EGF sequence Leu83-Leu88 in factor mediates ligand binding to effector cell protease receptor-1. J Biol Chem, 1997. 272(13): p. 8340-5
88. Altieri, D.C., and Edgington, T.S., Identification of effector cell protease receptor-1. A leukocyte-distributed receptor for the serine protease factor Xa. J Immunol, 1990. 145(1): p. 246-53
89. Altieri, D.C., Molecular cloning of effector cell protease receptor-1, a novel cell surface receptor for the protease factor Xa. J Biol Chem, 1994. 269(5): p. 3139-42.
90. Papapetropoulos, A., et al., Hypotension and inflammatory cytokine gene expression triggered by factor Xa-nitric oxide signalling. PNAS USA, 1998. 95(8): p. 4738-42
91. Nicholson, A.C., et al., Effector cell protease receptor-1 is a vascular receptor for coagulation factor Xa. J Biol. Chem., 1996. 271(45): p. 28407-13
92. McLean, K., et al., FXa-induced responses in vascular wall cells are PAR-mediated and inhibited by ZK-807834. Thromb Res, 2001. 103(4): p. 281-97
93. Camerer, E., et al., Coagulation factors VII and X induce Ca2+ oscillations in Madin-Darby canine kidney cells only when proteolytically active. J Biol Chem, 1996. 271(46): p. 29034-42.
94. Zaman, G.J., and Conway, E., The elusive factor Xa receptor: failure to detect transcripts that correspond to the published sequence of EPR-1. Blood, 2000. 96(1): p. 145-8
95. Coughlin, S.R., Thrombin signalling and protease-activated receptors. Nature, 2000. 407 (6801); p. 258-64
96. Grand, R.J., Turnell, A.S., and Grabham, P.W., Cellular consequences of thrombin-receptor activation. Biochem J, 1996. 313(Pt 2): p. 353-68
97. Cirino, G., et al., Inflammation-coagulation network: are serine protease receptors the knot? Trends Pharmacol Sci, 2000. 21(5): p. 170-2
98. Naldini, A., et al., Thrombin enhancement of interleukin-1 expression in mononuclear cells: involvement of proteinase-activated receptor-1. Cytokine, 2002. 20(5): p. 191-9
99. Camerer, E., et al., Genetic evidence that protease-activated receptors mediate FXa signalling in endothelial cells. J Biol Chem, 2002. 277(18): p. 16081-7.
100. Riewald, M., et al., Gene induction by coagulation factor Xa is mediated by activation of protease-activated receptor 1. Blood, 2001. 97(10): p. 3109-16
101. Kawabata, A., et al., Factor Xa-evoked relaxation in rat aorta; involvement of PAR-2. Biochem Biophys Res Commun, 2001. 282(2): p. 432-5.
102. Bretschneider, E. and Schror, K., Cellular effects of factor Xa on vascular smooth muscle cells –

81 | R e f e r e n c e s
inhibition by heparins? Semin. Thromb.Hemost., 2001. 27: p. 489–93
103. Kaiser, B., DX-9065a, a direct inhibitor of factor Xa. Cardiovasc. Drug Rev., 2003. 21: p. 91–104
104. Daubie, V. et al., Osteosarcoma cell-calcium signalling through tissue factor–factor VIIa complex and factor Xa. FEBS Lett., 2007. 581: p. 2611–15
105. Vu, T.K., et al., Molecular cloning of a functional thrombin receptor reveals a novel proteolytic mechanism of receptor activation. Cell, 1991. 64(6): p. 1057-68.
106. O’Brien, P.J., et al., Protease activated receptors: theme and variations. Oncogene, 2001. 20(13): p. 1570-81.
107. Schmidlin, F., and Bunnett, N.W., Protease-activated receptors: how proteases signal to cells. Curr Opin Pharmacol, 2001. 1(6): p. 575-82.
108. Trejo, J., Protease-activate receptors: new concepts in regulation of G protein-coupled receptor signalling and trafficking. J Pharmacol Exp Ther, 2003. 307(2): p. 437-42.
109. Oganesyan, V., et al., The crystal structure of the endothelial protein C receptor and a bound phospholipid. J Biol Chem, 2002. 277(28): p. 24851-4.
110. Nystedt, S., et al., Molecular cloning of a potential proteinase activated receptor. PNAS USA, 1994. 91(20): p. 9208-12
111. Molino, M., et al., Interactions of mast cell tryptase with thrombin receptors and PAR-2. J Biol Chem, 1997. 272(7): p. 4043-9
112. Xu, W.F., et al., Cloning and characterization of human protease-activated receptor 4. PNAS USA, 1998. 95(12): p. 6642-6
113. Hollenberg, M.D., Protease-activated receptors: PAR4 and counting: how long is the course? Trends Pharmacol Sci, 1999. 20(7): p. 271-3.
114. Macfarlane, S.R., et al., Proteinase-activated receptors. Pharmacol Rev, 2001. 53(2): p. 245-82
115. Lanzavecchia, A., and Sallusto, F., Dynamics of T lymphocyte responses: intermediates, effectors and memory cells. Science, 2000. 290(5489): p. 92-7
116. Lenschow, D.J., Walunas, T.L., and Bluestone, J.A., CD28/B7 system of T cell costimulation. Annual Rev. Immunol, 1996. 14: p. 233-58
117. Sharpe, A.H., and Freeman, G.J., The B7-CD28 superfamily. Nat Rev Immunology, 2002. 19: p. 116-26
118. Gotch F., et al., Identification of viral molecules recognized by influenza-specific human cytotoxic T lymphocytes. J Exp Med, 1987. 165: p. 408.
119. MacIsaac, C., et al., Rapid analysis of the Vbeta repertoire of CD4 and CD8 T lymphocytes in whole blood. J. Immunol Methods, 2003. 283: p. 9-15
120. Geha, R.S., et al., Effect of anti-HLA antisera on macrophage - T-cell interaction. PNAS USA, 1979. 76(8): p. 4038-4041

82 | R e f e r e n c e s
121. Abraham, R.T., and Weiss, A., Jurkat T cells and development of the T-cell receptor signalling paradigm. Nature Rev Immun, 2004. 4: p. 301
122. Nickel, T.J., et al., Constitutive expression of functionally active protease-activated receptors 1 and 2 in human conjunctival epithelial cells. Mediators of Inflammation, 2006. 2006: p. 1-8
123. Schaeffer, P., et al., Coagulation factor Xa induces endothelium-dependent relaxations in rat aorta. Circ Res, 1997. 81(5): p. 824-8
124. Evans, D.E., et al., Boosting T cell costimulation in cancer: the possibilities seem endless. Int Rev Immunol, 2003. 22(2): p. 173-94
125. Sedwick, C.E., et al., TCR, LFA-1, and CD28 play unique and complementary roles in signalling T cell cytoskeletal reorganization. J Immunol, 1999. 162(3): p. 1367-75
126. Wulfing, C., et al., A receptor/cytoskeletal movement triggered by costimulation during T cell activation. Science, 1998. 282(5397): p. 2266-9
127. Lub, M., et al., Ins and outs of LFA-1. Immunol Today, 1995. 16(10): p. 479-83
128. Huntington, N.D., et al., CD45: direct and indirect government of immune regulation. Immunol Lett, 2004. 94(3): p. 167-74
129. Anton van der Merwe, P., et al., Cytoskeletal polarization and redistribution of cell-srface molecules during T cell antigen recognition. Semin Immunol, 2000. 12(1): p. 5-21
130. Hutloff, A., et al., ICOS is an inducible T-cell co-stimulator structurally and functionally related to CD28. Nature, 1999. 397(6716): p. 263-6
131. McAdam, A.J., et al., ICOS is critical for CD40-mediated antibody class switching. Nature, 2001. 409(6816): p. 102-5
132. Takahashi, C., et al., Cutting edge: 4-1BB is a bona fide CD8 T cell survival signal. J Immunol, 1999. 162(9): p. 5037-40
133. Hurtado, J.C., et al., Potential role of 4-1BB in T cell activation. Comparison with the costimulatory molecule CD28. J Immunol, 1995. 155(7): p. 3360-7.
134. Maxwell, J.R., et al., Danger and OX40 receptor signalling synergize to enhance memory T cell survival by inhibiting peripheral deletion. J Immunol, 2000. 164(1): p. 107-12.
135. Godfrey, W.R., et al., Identification of a human OX-40 ligand, a costimulator of CD4+ T cells with homology to tumor necrosis factor. J Exp Med, 1994. 180(2): p. 757-62
136. Gramaglia, I., et al., The OX40 costimulatory receptor determines the development of CD4 memory by reglating primary clnal expansion. J Immunol, 2000. 165(6): p. 3043-50.
137. Gramaglia, I., et al., OX-40 ligand: a potent costimulatory molecule for sustaining primary CD4 T cell responses. J Immunol, 1998. 161(12): p. 6510-7.
138. Harrop, J.A., et al., Herpesvirus entry mediator ligand (HVEM-L), a novel ligand for HVEM/TR2, stimulates proliferation of T cells and inhibits HT29 cell growth. J Biol Chem, 1998. 273(42): p. 27548-

83 | R e f e r e n c e s
56.
139. Zhai, Y., et al., LIGHT, a novel ligand for lymphotoxin beta receptor and TR2/HVEM induces apoptosis and suppresses in vivo tumor formation via gene transfer. J Clin Invest, 1998. 102(6): p. 1142-51.
140. Tamada, K., et al., LIGHT, a TNF-like molecule, costimulates T cell proliferation and is required for dendritic cell-mediated allogeneic T cell response. J Immunol, 2000. 164(8): p. 4105-10.
141. Tamada, K., et al., Modulation of T-cell-mediated immunity in tumor and graft-versus-host disease models through the LIGHT co-stimulatory pathway. Nat Med, 2000. 6(3): p. 283-9.
142. Altieri, D.C., Xa receptor EPR-1. Faseb J, 1995. 9(10): p. 860-5
143. Bono, F., et al., Human umbilical vein endothelial cells express high affinity receptors for factor Xa. J Cell Physiol, 1997. 172(1): p. 36-43.
144. Herbert, J., et al., Effector protease receptor mediates the mitogenic activity of factor Xa for vascular smooth muscle cells in vitro and in vivo. J Clin Invest, 1998. 101(5): p. 993-1000.
145. Rothermel, A.L., et al., High affinity cross-reacting mAb generated by minimal mimicry: implications for the pathogenesis of anti-nuclear autoantibodies and immunosuppression. PNAS USA, 1998. 95(7): p. 3816-20
146. Altieri, D.C., et al., Sequential receptor cascade for coagulation proteins on monocytes. Constitutive biosynthesis and functional prothrombinase activity of a membrane form of factor V/Va. J Biol Chem, 1989, 264(5): p. 2969-72.
147. Conway, E.M., et al., Three differentially expressed survivin cDNA variants encode proteins with distinct antiapoptotic functions. Blood, 2000. 95(4): p. 1435-42
148. Borenstajn, K., et al., Factor Xa: at the crossroads between coagulation and signalling in physiology and disease. Trends Mol Med, 2008. 10: p. 439-40
149. Le, D.T., et al., Hemostatic factors in rabbit limb lymph: relationship to mechanisms regulating extravascular coagulation. Am. J. Physiol. Heart Circ. Physiol., 1998. 274: p. H769-76
150. Yamakawa, M., et al., Localization of blood coagulation factors and fibrinolysis factors within lymphoid germinal centers in human lymph nodes. Histochemistry, 1991. 96: p. 123-7
151. Ruf, W., et al., Specificity of coagulation factor signalling. J Thromb and Haemost, 2003. 1(7): p. 1495-1503
152. Connolly, A.J., et al., Mice lacking the thrombin receptor, PAR1, have normal skin wound healing. Am J Pathol, 1997. 151(5): p. 1199-204
153. Connolly, A.J., et al., Role of the thrombin receptor in development and evidence for a second receptor. Nature, 1996. 381(6582): p. 516-9
154. Weiss, E.J., et al., Protection against thrombosis in mice lacking PAR3. Blood, 2002. 100(9): p. 3240-4
155. Garcia-Cao, I., et al., Genetic inactivation of PAR4 results in hyperactivation of NF-kappaB and impairment of JNK and p38. EMBO Rep, 2003. 4(3): p. 307-12
156. Sambrano, G.R., et al., Role of thrombin signalling in platelets in haemostasis and thrombosis. Nature,

84 | R e f e r e n c e s
2001. 413(6851): p. 74-8
157. Kataoka, H., et al., Protease-activated receptors 1 and 4 mediate thrombin signalling in endothelial cells. Blood, 2003. 102(9): p. 3224-31
158. Scandura, J.M., et al., A binding site expressed on the surface of activated human platelets is shared by Factor X and Prothrombin. Biochemistry, 1996. 35(27): p. 8890–8902