Microbial keratitis study from Fiji
-
Upload
laurence-sullivan -
Category
Health & Medicine
-
view
32 -
download
2
description
Transcript of Microbial keratitis study from Fiji

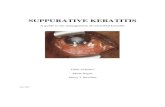
Pattern of Etiologic Agents and Sensitivities for Microbial Keratitis at CWM Hospital- Fiji.A 4 Year Retrospective Study (January 2007- December 2010).
Dr. Shereen Aiyub MBBS, DO1, Dr. John Szetu MBBS, DO, MSc (Ophth) 1, Dr. Laurence Sullivan MBBS, FRANZCO2
1Pacific Eye Institute, Suva, Fij 2Royal Victorian Eye and Ear Hospital , Melbourne, Australia.
IntroductionCorneal scarring is the second most common cause of avoidable blindness in the developing world following cataract.
A significant proportion of this opacity is due to microbial keratitis.
In order to prevent ocular morbidity , significant visual loss and secondary amblyopia in children ?????
Microbial keratitis is characterized by a corneal epithelial defect with underlying stromal infiltration by replicating microorganisms and the secondary inflammation caused.
Bacteria are responsible for 70-91% of keratitis in the Western world.
Acanthamoeba keratitis have been reported uncommon (Nepal 0% and South Asia 0.5%-2%) and usually associated with contact lens wearers.
Fungal keratitis have been commonly reported in Africa and India (35%-75%) , associated with a higher incidence of corneal perforation and subsequent poor visual prognosis even in the presence of best available antifungal therapy.
Fiji has a tropical climate, warm and humid weather mitigated by trade winds and frequent rainfall. The majority of the Fijian population reside in rural areas and survive on subsistence farming.
It is our observation that the most common predisposing factor to microbial keratitis is ocular injury from organic material and use of herbal medicine in eyes.
Results35 corneal scrapes were done in 4 years. 16 scrapes showed no growth while 24 pathogens were recovered from 19 corneal scrapings. Mean patient age: 39 years (age range 4-61 years). Male : Female - 3.75 : 1
Table 1- Etiologic Agents for Culture Positive Microbial Keratitis
Table 2 – Bacterial Sensitivity to Antibiotics.
E. Coli and Acintobacter Iowfii are resistant to Chloramphenicol.
MethodThis is a retrospective observational study of corneal scraping results over a 4 year period at the Colonial War Memorial Hospital Suva, Fiji (Year Jan 2007- Dec 2010)
The objectives of this study is to analyze
1. Percentage of Acanthamoeba, Bacterial and Fungal growth.
2. Percentage of microorganisms with in vitro sensitivity and resistance to tested antibiotics.
3. Percentage with positive smears on microscopy.
Culture results were recorded from CWM Hospital - Microbiology Laboratory Register.
Inclusion criterion for a positive culture was the growth of ≥ 5 colonies on one solid medium. Conjunctival and corneal pus swabs were excluded from this study.
Corneal scrapings were obtained from Bard Parker surgical blade and 21/23 gauge disposable needle under the magnification of a slit lamp and directly inoculated on chocolate agar, sheep blood agar and Mac Conkey agar. Culture was incubated at 37°C for 48 hours.Sabourauds dextrose agar plates for fungal culture was maintained at 37°C for 48 hours. Gram stain smears and wet mount microscopy of scraped corneal material were also done.
Etiologic Agents for Culture Positive Microbial Keratitis Percentage Number of Isolates N=24
Gram Positive Bacteria 29.2% N=(7/24)Coagulase Negative Staphylococcus Aureus 3Staphylococcus Aureus 2Methicillin Resistant Staphylococcus Aureus 2
Gram Negative Bacteria 58.3% N=(14/24)Pseudomonas Aeruginosa 2E. coli 1Acintobacter sp. 4Enterobacter sp. 4Citrobacter sp. 2Klebsiella 1
Fungi (Candida Albicans) 12.5% N=(3/24)
Acanthamoeba 0% N=(0/24)
Antibiotics Total Bacterial Sensitivity N=21 Resistance
Chloramphenicol 85.8% 21 14.2% (3/21)
Ciprofloxacin 100% 17 0%
Penicillin 16.7% 18 83.3% (15/18)
Gentamycin 94.5% 18 5.5% (1/18)
Cephalothin 68.4% 19 31.6% (6/19)
were
DiscussionGram Negative Bacteria have been identified here as the most common etiologic agent for Microbial Keratitis (14/24) 58.3%.
Keay L (2006) reported a large proportion of gram negative microbial keratitis in Taiwan (38%), Bangladesh (22%), Florida (19%) and but not (7%) in Melbourne (RVEEH).
Variations in pathogens are based on geographic and socioeconomic differences.
Gram positive isolates have been commonly isolated in the developed countries and it may be related to early presentation to medical care and premedication.
In the underdeveloped nations late presentation to health care and use of herbal medicine is not very uncommon resulting into fulminant corneal infection.
In this study Candida Albicans were the only fungal isolates identified.
The incidence of fungal keratitis varies throughout the world geographically: India (50%), Bangladesh (36%), Nepal (17%) and Melbourne (5% - 14/100)
Acanthamoeba requires Giemsa, PAS, or Calcoflour white stain besides as well as N non-nutrient agar with E Coli overlaying for growth and is very hard to grow.
ConclusionThe study supports use of ciprofloxacin as monotherapy for microbial keratitis in Fiji. This information helps in initial selection of therapy for microbial keratitis while waiting for culture results.
This study also recommends the need to establish a proper protocol for testing antibiotic sensitivity and resistance at CWM Hospital. An accurate database to record corneal scrape details, Incubation time for bacterial culture at 37 degrees for 2 weeks, fungal cultures at 27 degrees for 4 weeks and uniform testing of in vitro susceptibility.
Limitations of StudyRetrospective study with possible recording bias.
Improper documentation of demographic, duration of symptoms, predisposing factors and clinical findings.
Microbiologic focus of the study including insufficient microbiologic samples and incubation time, limited number of corneal scrapes taken, lack of accurate database to record details of corneal scrape and failure of uniform testing of pathogens to antibiotics.
ReferencesMichael R. Feilmeier, Kavitha R. Sivararam, Matt Oliva, Geofferey C. t Tabin, Reeta Gurung. Etiologic at a Tertiary Eye Centre In Kathmandu, Nepal. Cornea journal of clinical Science. 2010;0. Diagnosis of Corneal Ulcer Cornea. 2010 Dec;29(12):1380-5.Etiologic diagnosis of corneal ulceration at a tertiary eye center in Kathmandu, Nepal.Feilmeier MR, Sivaraman KR, Oliva M, Tabin GC, Gurung R.
2. Prashant Bhartiya, Mark Daniell, Marious Constantinou, FM Amiral Islam, Hugh R Taylor. Fungal Keratitis In Melbourne. Clinical and Experimental Ophthalmology. 2007;35(2):124-30. Fungal keratitis in Melbourne.Bhartiya P, Daniell M, Constantinou M, Islam FM, Taylor HR.Clin Experiment Ophthalmol. 2007 Mar;35(2):124-30.
8.M. Salton , K. Kim. Structure in Barons Medical Microbiology. University of Texas Medical Branch. 2010;1(1). ???what is this?
3. Lisa Keay, Katie Edwards, Thomas Naduvilath, Hugh R. Taylor, Grant R. Snibson, Kevin Forde, Fiona Stapleton. Microbial Keratitis: Predisposing Factors and Morbidity. American Journal of Ophthalmology. 2006; 113(1):109-16
4. Ifeoma R. Ezegwui ,Corneal Ulcers in a Tertiary Hospital in Africa. Journal of the National Medical Association. 2010;102(7).
5. N. Gangopadhyan, Mark Daniell, L. Weih, Hugh R Taylor. Fluoroquinolone and Fortified Antibiotics for Treating Bacterial Corneal Ulcer. British Journal of Ophthalmology. 2000;84(4):378-84
Acknowledgements1. Dr. Michael Loughnan, Senior Ophthalmologist,
Royal Victorian Eye and Ear Hospital, Melbourne, Australia.
2. Dr. Gary Phelps, RANZCO Consultant, Pacific Eye Institute, Suva, Fiji.
3. Pacific Eye Institute, Suva Fiji4. Colonial War Memorial Hospital, Suva Fiji5. Fred Hollows Foundation New Zealand