Methemoglobinemia in children with acute lymphoblastic leukemia (ALL) receiving dapsone for...
-
Upload
suzan-williams -
Category
Documents
-
view
221 -
download
5
Transcript of Methemoglobinemia in children with acute lymphoblastic leukemia (ALL) receiving dapsone for...

Pediatr Blood Cancer 2005;44:55–62
Methemoglobinemia in Children With Acute LymphoblasticLeukemia (ALL) Receiving Dapsone for Pneumocystis Carinii
Pneumonia (PCP) Prophylaxis: A Correlation WithCytochrome b5 Reductase (Cb5R) Enzyme Levels
Suzan Williams, MD,1,2,3 Paula MacDonald, BSc Pharm,2 James D. Hoyer, MD,4
Ronald Duncan Barr, MBChB, MD,1,2 and Uma Harish Athale, MD1,2*
INTRODUCTION
Prophylaxis against pneumocystis carinii pneumonia(PCP) is a standard of supportive care for immuno-compromised patients including children with cancer,transplant recipients, and patients with acquired immuno-deficiency syndrome (AIDS). In 1997, the Centers forDisease Control and Prevention (CDC) recommendeddapsone (4-40-diaminodiphenylsulfone) for prevention ofPCP pneumonia in HIV infected patients [1]. With thepopulation of immunocompromised patients increasing,dapsone use for PCP prophylaxis is on the rise. Currentlydapsone is the most cost-effective prophylaxis againstPCP [1]. It is commonly used as an alternative agent forchildren unable to tolerate the first line drug, trimetho-prim-sulfamethaxazole (TMP-SMX) [1–3].
Methemoglobinemia is a known side effect of dapsone,reported most often after an accidental or intentionaloverdosage [4–8]. Recently methemoglobinemia has also
been reported in patients on prophylactic regimes of dap-sone, including children with cancer [1,9–11]. However,there are no studies reporting the frequency of and the pre-disposing factors for development ofmethemoglobinemia
Background. Dapsone is commonly used forpneumocystis carinii pneumonia (PCP) prophy-laxis in immunocompromised patients. Methe-moglobinemia is a known complication ofdapsone, but its true frequency and pathogen-esis in childhood cancer patients are unknown.Additionally, practice guidelines for evaluationand management of dapsone-induced methe-moglobinemia are not available. Procedure.We studied 15 children with acute lymphoblas-tic leukemia (ALL) receiving dapsone for PCPprophylaxis to determine the frequency ofmethemoglobinemia, and correlate its occur-rence with cytochrome b5 reductase (Cb5R)enzyme levels. Ten children with ALL receivingtrimethoprim-sulfamethaxazole (TMP-SMX) werestudied as controls. All patients underwentphysical examination, pulse oximetry, andmethemoglobin (metHb) estimation. Commer-cially available assay was used to measure Cb5Rlevels. Results. Three (20%) patients receivingdapsone developed symptomatic methemoglo-binemia. Average duration of dapsone pro-phylaxis prior to diagnosis was 6.6 weeks(range 3.5–10 weeks). Mean metHb level insymptomatic patients was 11.67%; 95% confi-
dence interval (CI) 0–25.79 (range 7–18%), and1.37%; 95% CI 0.6–2.14 (range 0.02–3%) inasymptomatic patients (P¼0.09), whereas themean metHb level in the control group was0.54%; 95% CI 0.35–0.73 (range 0.1–0.8%)(asymptomatic vs control P< 0.0001). MeanCb5R level in symptomatic patients was 8.6 IU/gHb; 95% CI 3.4–13.7 (range 6.9–10.9) compar-ed to 12.5 IU/g Hb; 95% CI 11.1–13.9 (range10.8–14.6) in asymptomatic patients (P¼0.06).Two symptomatic patients had Cb5R levels at orbelow 50% of normal, consistent with hetero-zygosity. Parental studies for Cb5R levels weresuggestive of a carrier state in one of eachpatient’s parents. Conclusions. Heterozygosityfor Cb5R deficiency may pre-dispose to methe-moglobinemia even on a thrice-weekly regimenof dapsone. Such individuals should avoidsubsequent exposure to oxidant agents, if pos-sible. Children with ALL tend to be symptomaticat low levels of metHb and may have delayeddetection of methemoglobinemia. Hence, fre-quent monitoring of patients receiving dapsoneis recommended. Monitoring guidelines for dap-sone prophylaxis are proposed. Pediatr BloodCancer 2005;44:55–62. � 2004 Wiley-Liss, Inc.
Key words: acute lymphoblastic leukemia; cytochrome b5 reductase; dapsone;methemoglobinemia; pneumocystis carinii
——————1Division of Hematology/Oncology, Department of Pediatrics,
McMaster University, Hamilton, Ontario, Canada
2Hematology/Oncology Service, McMaster Children’s Hospital,
Hamilton Health Sciences Corporation, Hamilton, Ontario, Canada
3Division of Hematology, The Hospital for Sick Children, Toronto,
Ontario, Canada
4Division of Hematopathology, Mayo Clinic, Rochester, Minnesota
Work performed at Division of Hematology/Oncology, Department of
Pediatrics, McMaster University and McMaster Children’s Hospital,
Hamilton Health Sciences Corporation, Hamilton, ON, Canada.
*Correspondence to: Uma Harish Athale, 3N27D, Health Sciences
Centre, McMaster University, 1200 Main Street West, Hamilton, ON,
Canada L8N 3Z5. E-mail: [email protected]
Received 13 February 2004; Accepted 12 July 2004
� 2004 Wiley-Liss, Inc.DOI 10.1002/pbc.20164

in childhood cancer patients receiving dapsone for PCPprophylaxis. In addition, guidelines for evaluation andmanagement of dapsone-inducedmethemoglobinemia arenot available.
The exact mechanism of methemoglobinemia encoun-tered in some patients receiving low and infrequent dosesof dapsone is not clearly understood. It has been suggestedthat heterozygosity for nicotinamide adenine dinucleotide(NADH)-dependent cytochrome b5 reductase (Cb5R)deficiency increases susceptibility tomethemoglobinemiainducing agents because this enzyme is a necessarycomponent of a major methemoglobin (metHb) reducingpathway. Cohen et al. first described this concept in 1968in a series of six American soldiers in Vietnam receivinganti-malarial prophylaxis with weekly chloroquin andprimaquin, and daily dapsone [12]. Since then therehave been only a few case reports describing methemo-globinemia following exposure to oxidants like localanesthetics and novel anti-cancer agents in individualsheterozygous for Cb5R [13,14]. In addition, the physio-logical lower levels of Cb5R are thought to be responsiblefor the methemoglobinemia following exposure to pri-locaine containing eutectic mixture of local anesthesia(EMLA) cream in young infants [15–17].
Despite these reports, and the reports describing the riskof acquiredmethemoglobinemia from exposure to variousoxidants in cancer patients, heterozygosity for NADH-dependent Cb5R deficiency as a pre-disposing factor forunexpected incidents of drug-induced methemoglobine-mia has not been studied systematically [18,19]. With theadvent of polypharmacy to treat complex medical condi-tions like cancer, we think it is time to revisit the issueof dapsone-induced methemoglobinemia. The followingstudy was undertaken to determine the frequency ofmethemoglobinemia, and to correlate the occurrence ofmethemoglobinemiawith Cb5R enzyme levels in childrenwith ALL on dapsone-prophylaxis. We hypothesized thata heterozygous carrier state for Cb5R deficiency or lowenzyme levels pre-dispose patients to develop methemo-globinemia on dapsone for PCP prophylaxis. Based on ourexperience, we suggest guidelines for monitoring patientsreceiving dapsone for PCP prophylaxis.
MATERIALS AND METHODS
All clinical and pharmacy records of children(�18 years) with ALL being treated in the Divisionof Hematology/Oncology, Department of Pediatrics,McMaster University, for the period April 2002 toFebruary 2003, were reviewed to identify patients receiv-ing dapsone for PCP prophylaxis. All patients receivedsimilar therapy for ALL. Patients with known respiratoryproblems (e.g., pneumonia) or relapsed disease wereexcluded from the study. At our center, dapsone for PCPprophylaxis is initiated for patients with TMP-SMX
allergy, cytopenia while on TMP-SMX PCP prophylaxisresulting in delayed chemotherapy or occasionally forpatient preference. The dosage used is 5–10 mg/kg/weekin three equally divided doses on Monday, Wednesday,and Friday; maximum single dose is 100 mg (Dapsone,Wyeth-Ayerst Pharmaceuticals, St. Laurent, Quebec,Canada).
All patients with ALL on dapsone prophylaxis under-went complete physical examination and measurementof oxygen saturation by pulse oximetry. MetHb levelswere measured using co-oximetry on venous blood in allpatients. Symptomatic methemoglobinemia was definedas an above normal level of metHb in association withhypoxemia (oxygen saturation <95%) with or withoutcyanosis or respiratory complaints. Cb5R levels weremeasured at the Mayo Medical Laboratories, Rochester,MN with a commercially available assay. This is a kineticspectrophotometric method, measuring the oxidation ofNADH at 340 nm at 308C as Cb5R catalyzes the NADH-linked reduction of ferricyanide [20]. Samples were col-lected and transported according to the laboratory guide-lines. For testing, 4 ml of blood was collected in ACD orEDTA. Samples were refrigerated after collection andtransported in refrigerated shipping containers at 48C.Glucose 6-phosphate dehydrogenase (G6PD) testing wasperformed in all three patients with symptomatic methe-moglobinemia using standard techniques [21]. Previousstudies have reported high metHb levels in patients withuntreated leukemia [22]. In order to exclude an effectof the disease or other potential oxidative exposuresduring ALL treatment, we measured the metHb levels ina group of ten ALL patients who were receiving TMP-SMX prophylaxis but identical anti-leukemic therapy, ascontrols.
Statistical analysis was performed using SAS Software[Release 8.2 (TS2M0) copyright 1999–2001, SAS Insti-tute Inc., Cary, NC]. All values are expressed asmeanwith95% confidence interval (CI) and range. Student t-test wasused to evaluate differences between the mean values ofmetHb and Cb5R amongst different groups of patients.Due to the differences in sample size, Student t-test wasapplied with assumption of unequal variance.
RESULTS
During the study period, a total of 16 patients withALLreceived dapsone for PCP prophylaxis. Fifteen patientswere enrolled in the study; one patient was excludedbecause of relapsed disease. No patients had pre-existingrespiratory problems. The majority of the patients wereCaucasians (n¼ 14).
Three of 15 (20%) patients receiving dapsone hadsymptomatic methemoglobinemia with a mean metHblevel of 11.67%; 95%CI 0–25.79 (range 7–18%) (normalrange 0–2%) and the remaining 12 patients were asympto-
56 Williams et al.

maticwith ameanmetHb level of 1.37%; 95%CI 0.6–2.14(range 0.02–3.0%) (P¼ 0.09). Only one asymptomaticpatient had above normal metHb level of 3% which onsubsequent testing normalized despite continuation ofdapsone. Patients with and without symptomatic methe-moglobinemia received similar chemotherapy as well asother supportive care medications. In addition, two pa-tients on dapsone PCP prophylaxis received enoxaparin(low molecular weight heparin) for deep venous throm-bosis; one patient (Case I) developed symptomatic methe-moglobinemia and the other did not. All the asymptomaticpatients had oxygen saturations above 95%.
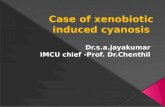
Table I describes the clinical characteristics, laboratoryevaluation, and management of the three patients withsymptomatic methemoglobinemia. All the patients hadnormal chest radiographs. In addition, Case 1 underwentspiral computerized tomography (CT) scan to rule outpulmonary embolism, the CT scan was normal. All threesymptomatic patients had normal liver function. Afterdetection of methemoglobinemia, dapsone was discon-tinued in all three patients and pentamidine was com-menced for PCP prophylaxis. All three patients weremonitored carefully with metHb levels. None of thepatients required any specific therapy for methemogloi-nemia. Within 3–5 days of discontinuation of dapsone,hypoxia resolved and metHb levels decreased to normal(Fig. 1).
Ten patients (including all three with symptomaticmethemoglobinemia) underwent estimation of Cb5Rlevels. Five patients (three due to perceived inconvenienceof blood collection and two due to difficult blood draw)were not tested. These five patients had normal physicalexamination, pulse oximetry and metHb levels. The meanCb5R level in asymptomatic patients was 12.49 IU/g Hb;95% CI 11.07–13.90; (range 10.8–14.6 IU/g Hb). In con-trast, the mean Cb5R level in symptomatic patients was8.56 IU/g Hb; 95% CI 3.39–13.74 (range 6.9–10.9 IU/gHb), (normal range for the laboratory 10.1–19.4 IU/gHb).With assumption of unequal variance, the associationbetweenmethemoglobinemia and low Cb5R level fell justbelow the usual limit of statistical significance (P¼ 0.06).This may be related to the small sample size. Two of thethree patients with symptomatic methemoglobinemia hadCb5R levels at approximately 50% of normal levelsconsistent with a heterozygous state for Cb5R deficiency(Table I). In addition to symptomatic methemoglobine-mia, both these patients had associated unexplainedanemia, detected prior to the diagnosis of methemoglo-binemia, requiring red cell transfusions. The exactetiology of this anemia is not clear. RBC morphologywas normal in both patients. Mild elevation of (total andunconjugated) bilirubin and lactate dehydrogenase (LDH)observed in Case 1 and marked elevation of LDH andreticulocyte count but normal bilirubin in Case 3 suggestan underlying hemolytic process. However, complete T
ABLEI.
ClinicalandLaboratory
FeaturesofChildrenWithALLonDapsoneforPCPProphylaxisWithSymptomaticMethem
oglobinem
ia
Case
Age
(year)/sex
Duration
ofdapsone
prophylaxis
(days)
Clinical
status
Pulseoxim
etry
O2-saturation
(%)
Hem
atological
evaluation
Other
investigations
Managem
entandoutcome
Hb(g/l)
MetHblevel
(%)(0–2%)a
bCb5Rlevel
(IU/g
Hb)
(10.1–19.4)a
G6PD
111/F
24
Unexplained
anem
ia,
cyanosis
88
67
18
6.9
Norm
alCXR,CTchest(toexcludepulm
onary
embolism
),SerolgoyforparvovirusB-19
Hospitalizationin
IntensiveCareUnit,
supportiveO2,PRBCtransfusion
23/M
26
‘‘Notfeelingwell’’,
cyanosis
88
91
10
10.9
Norm
alCXR(toexcludepeumonia),NPaspirate,
viral
serology
Hospitalization,supportiveO2
32/M
70
Unexplained
anem
ia,
low
energylevel
92
72
77.9
Norm
alCXR(toexcludepneumonia),NPaspirate,
BM
aspiration,serologyforparvovirusB-19
PRBCtransfusion
O2,oxygen;H
b,hem
oglobin;M
etHb,m
ethem
oglobin;C
b5R,cytochromeb5reductase;G6PD,glucose6phosphatedehydrogenase;CXR,chestX
-ray;C
T,computerizedtomography;F,fem
ale;NP,
nasopharyngeal;M,male;PRBC,pakcedredbloodcells.
aLevelsin
parenthesisindicatenorm
alrangeforthelaboratory.
bCb5Rlevelsestimated
followingseveralmonthsfrom
recoveryofmethem
oglobinem
ia.
Dapsone-Induced Methemoglobinemia in Childhood ALL 57

evaluation for hemolysis was not undertaken due to thepresumption of chemotherapy-related anemia.
In order to investigate a heterozygous state for Cb5Rdeficiency, Cb5R levels were tested in both parents ofCases 1 and 3. As shown in Table II, mothers of bothpatients had borderline low activity indicating possibleCb5R deficiency carrier state. Parents were tested almostafter 1 year following the testing of the children. This timedifference is responsible for the difference in the reportednormal range for the tests.
The mean metHb level in the control group, namelypatients with ALL receiving TMP-SMX PCP prophylaxis(n¼ 10) but otherwise similar ALL therapy, was 0.54%(range 0.1–0.8%). This level was significantly lowercompared to the mean metHb level in asymptomaticpatients receiving dapsone PCP prophylaxis (n¼ 12) of1.37% (range 0.02–3.0%) (P< 0.001). This excludes asignificant effect of ALL or its therapy on metHb levels.
DISCUSSION
Three of the fifteen (20%) children with ALL devel-oped symptomatic methemoglobinemia while receivingthrice-weekly doses of dapsone for PCP prophylaxis. As agroup, patients with symptomatic methemoglobinemiahad lower levels of Cb5R compared to asymptomatic pa-tients. Two of the three patients with symptomaticmethemoglobinemia had Cb5R levels consistent with aheterozygous state; whereas none of the seven patientswith normal levels of Cb5R developed methemoglobine-mia. Thus, low Cb5R levels or a heterozygous state forCb5Rdeficiency is likely to pre-dispose to development of
symptomatic methemoglobinemia in children with ALLreceiving dapsone for PCP prophylaxis.
In healthy individuals, metHb constitutes approxi-mately 1% of hemoglobin [23]. MetHb is an oxidizedform of hemoglobin in which the iron in the hememoiety is converted from the ferrous to the ferric form.Three enzymatic pathways are responsible for constantreduction of metHb to functional deoxyhemoglobin.They are, NADH-dependent Cb5R, nicotinamide ade-nine dinucleotide phosphate (NADPH)-dependent metHbreductase, and the NADPH-dependent glutathione re-duction pathway. NADH-dependent Cb5R pathway isresponsible for the conversion of approximately 95%of metHb to hemoglobin. Saturation of the capacities ofthe enzymatic pathways by exogenous oxidizing agentsleads to excessive oxidation of hemoglobin to metHb[24–27].
The gene for Cb5R is located on chromosome 22q13-qter [28,29]. Inherited as an autosomal recessive trait,homozygous deficiency of Cb5R leads to the rare congeni-tal methemoglobinemia. These individuals are cyanotic,with levels of metHb from 10% to 35% [30]. Individualsheterozygous for Cb5R deficiency have normal clinicalstatus and normal arterial oxygen saturations with metHblevels less than 2% [24]. They have approximately 50% ofnormal levels of Cb5R enzyme and are postulated to be atgreater risk of developing methemoglobinemia followingexposure to oxidizing agents [12–14,31]. Over 30 dif-ferentmutations have been reported in theCb5Rgene. Thediagnosis of suspected Cb5R deficiency is usually con-firmed by enzyme assay [29].
In the present series, two patients (Cases 1 and 3) hadlow Cb5R levels. Both patients presented with sympto-matic methemoglobinemia and persistent anemia requir-ing red cell transfusions. Although at birth, the Cb5Rlevels are 40–60% of adult values, the levels reach normaladult levels by 3 months of life [15,17]. Thus the lowerlevels seen in our patients, aged 2 and 10 years are not age-related phenomena. The Cb5R levels at 50% of the normalrange observed in our patients indicate a heterozygousstate for Cb5R deficiency. To confirm the heterozygosity,we tested both biological parents of the two affectedpatients. The parental studies of Cb5R levels in Cases 1and 3 are suggestive of a carrier state for Cb5R deficiency.At the lower limit of normal, the enzyme level in Case 2 isnot consistent with a heterozygous state and may not beresponsible for the development of methemoglobinemia.
Population studies have estimated a gene frequencyof 0.002–0.07 for Cb5R deficiency, with a heterozygotecarrier prevalence estimate of 0.004–0.13 [32–36]. How-ever, 2 of the 10 patients tested in the present study hadCb5R levels consistent with a heterozygous state. Thisfrequency seems to be higher in our mainly Caucasianpopulation than would have been expected based on esti-mated gene frequency. Since our sample size is small,
Fig. 1. Spontaneous decline of MetHb concentration in two hospita-
lized ALL patients presenting with symptomatic methemoglobinemia.
By 4–6 days after discontinuation of dapsone for PCP prophylaxis,
metHb levels had returned to normal. MetHb, methemoglobin.
TABLE II. Cb5R Levels in Parents of Children WithLow Cb5R Levels
Cb5R levels (IU/g Hb)
Normal rangea 10.1–19.4 8.2–19.2
Case Patient Mother Father
Case 1 6.9 8.2 11.2
Case 3 7.9 8.2 10.0
Cb5R, cytochrome b5 reductase.aRepresents two different time periods of testing, over 1 year apart.
58 Williams et al.

further prospective studies of a larger population withALL are needed to confirm this observation.
Hemolytic anemia is a known complication of dapsonetherapy. Increasing age and higher daily dose areassociated with increased hemolysis in association withdapsone; usually seen in patients receiving >200 mg/day[1,4]. The hemolysis is typically associated with Heinzbody formation. Although the exact mechanism of hemol-ysis is unknown, it is thought to be related to free oxygenradicals. Although over 80% of patients on dapsone (at adose of 100–150 mg/day) will have some drop in hemo-globin, the frequency and extent of anemia in childrenreceiving concurrent myelosuppressive therapy is notknown. We observed anemia in two patients with symp-tomatic methemoglobinemia. Interestingly, both thesepatients had low Cb5R levels. In the present series, twoother patients with dapsone-prophylaxis and normalmethemoglobin levels had anemia (Hb level of 62 and58 g/l) requiring red cell transfusions (data not presented).Both these children recovered from anemia despite con-tinuation of dapsone, indicating that dapsone may not beresponsible for the observed anemia. In all our patientswith multiple co-morbidities, the anemia was thought tobe related to ALL and its therapy. In future, however, suchpatients should be evaluated for dapsone-induced hemo-lytic anemia with reticulocyte counts, bilirubin levels,LDH, and peripheral smear evaluation.
Very few studies report methemoglobinemia as anadverse effect in patients receiving therapeutic or pro-phylactic dosage of dapsone [1,10,11,37]. When present,methemoglobinemia occurs with much less frequencycompared to our results. A retrospective analysis of3,330 patients with leprosy receiving WHO-multidrugtherapy reports only 2 patients with methemoglobinemia[37].
Stavola et al. evaluated safety and efficacy of dapsonefor the prevention of PCP pneumonia in 20 HIV-infectedchildren; only one patient (5.0%) had mild elevation ofmetHb [10]. Similarly Medina et al., while evaluatingdapsone and trimethoprim combination for PCP prophy-laxis in 30 patients with AIDS, reported 1 patient (3.3%)with methemoglobinemia [11]. In comparison, the 20%frequency of methemoglobinemia observed in the presentseries is much higher. Presence of leukemia or anti-leukemic therapy by itself does not seem to be responsiblefor development of methemoglobinemia since our controlgroup (patients with ALL receiving TMP-SMX prophy-laxis but otherwise similar anti-leukemic therapy) hadsignificantly lower metHb levels compared to asympto-matic patients on dapsone PCP prophylaxis. Interaction ofdapsone with anti-leukemic agents including steroids, ifany, is unknown. We believe that the higher frequency ofmethemoglobinemia may be a reflection of a higher fre-quency of heterozygosity for Cb5R deficiency, as indi-cated by enzyme levels, in our patient population.
Certainly further prospective studies of a larger populationof cancer patients is needed.
The exact mechanism of dapsone-induced methemo-globinemia is unknown. A correlation of methemoglobi-nemia with the dose and frequency of use of dapsonehas not been established. Many of the reported cases ofmethemoglobinemia occurred with overdosages or ondaily dosage of dapsone; whereas our patients receivedthree doses of dapsone per week [1,4–11]. Following oraladministration dapsone is well-absorbed reaching peakconcentrations within 2–6 hr [1,38,39]. It is metabolizedin the liver through the cytochrome P 450 enzyme systemto dapsone hydroxylamine, one of the several metabolitesof dapsone which is thought to be responsible formethemoglobinemia as well as hemolysis [4]. Studies inchildren (ages 0.3–12 years old) on dapsone for PCPprophylaxis report a median elimination half-life of 15–22.2 hr [40,41]. Such a long half-life of dapsone and itsmetabolites may explain the development of methemo-globinemia in our pediatric patients even with a threedoses per week regimen. Although liver dysfunction maypotentially affect dapsone metabolism and exacerbate thetoxicity, none of our patients with symptomatic methe-moglobinemia had significant hepatic dysfunction.
The clinical symptoms of methemoglobinemia usuallymanifest at metHb levels of 15–20% or higher [27,42].With increasing metHb levels, progressive metabolicacidosis and cardiovascular instability develop. Methe-moglobinemia in the range of 50–60% leads to seriouscomplications and levels exceeding 75% are usually fatal[43,44]. In contrast, methemoglobinemia in children withcancer, as described by others and us, is diagnosed atrelatively low levels ofmetHb [9]. Thismay be a reflectionof an age-related phenomenon or underlying disease.Gallant et al. reported life-threatening symptoms in anadult AIDS patient with a metHb level of 8.2%, andproposed that patients with chronic anemia or underlyingrespiratory problems are likely to become symptomatic atmuch lower levels of metHb [44].
The symptoms of methemoglobinemia usually resultfrom hypoxia, since metHb cannot carry oxygen [42]. Thecommon symptoms include cyanosis, headaches, dizzi-ness, fatigue, and weakness [30]. With the exception ofcyanosis, these symptoms are also common in childrenundergoing therapy for ALL. Besides, with disease-related anemia and sallow complexion, mild cyanosismay be difficult to detect in patients with ALL. Thus, thediagnosis of methemoglobinemia in this patient popula-tion may be delayed. In most adult patients dapsone-induced methemoglobinemia was detected within the firstweek or two of dapsone therapy [4–8,45–49]. In contrast,the average duration of dapsone prophylaxis prior to thediagnosis of symptomatic methemoglobinemia in the pre-sent series was 6.6weeks (range 3.5–10weeks). Althoughthe symptoms of anemia were present much before the
Dapsone-Induced Methemoglobinemia in Childhood ALL 59

diagnosis of methemoglobinemia in two patients, thesewere attributed to the underlying ALL and chemotherapy.Mandrell et al. reported methemoglobinemia in a childwith acute promyelocytic leukemia after 3 months ofdapsone for PCP prophylaxis [9]. This emphasizes theneed for careful monitoring and a high index of suspicionfor the diagnosis of methemoglobinemia in childhoodcancer patients.
Currently, however, there are no guidelines for moni-toring patients on dapsone.We propose such guidelines asoutlined in Figure 2.We suggest weekly pulse oximetry, asnone of our patients with normal oxygen saturations hadelevated metHb levels or symptoms. Animal and humanstudies support the use of oxygen saturation detected bypulse oximetry as a good screening for methemoglobine-mia [49,50]. A confirmatory metHb level should be donein the presence of abnormal saturation on room air. Since
patients on active ALL-therapy usually receive weeklychemotherapy in the hospital setting, weekly monitoringfor methemoglobinemia is feasible. In addition to discon-tinuation of dapsone, appropriate therapeutic interventionshould be instituted based on clinical status. As observedin our patients, drug-inducedmethemoglobinemia usuallyresolves after discontinuation of the offending agentwithout any specific therapy. The blood metHb levels inthe symptomatic patients should be monitored frequently.Patients with life-threatening symptoms or with persistentsymptoms, and/or high levels of metHb despite disconti-nuation of the toxic agent, will require specific therapy inthe form of 1%methylene blue (1–2mg/kg intravenously,maximum dose 7 mg/kg) [8,9,26,29,51,52]. Methyleneblue, a cofactor to the NADPH dependent metHb reduc-tase pathway, is reduced in tissues to leukomethylene bluewhich in turn reduces ferric iron to the ferrous state. Since
Fig. 2. Proposed guidelines for monitoring patients receiving dapsone for PCP prophylaxis for methemoglobinemia. Initially, weeklymonitoring
for symptoms and pulse oximetry are suggested, with subsequent decreased frequency ofmonitoring, if asymptomatic by 4–6weeks of prophylaxis.
Additionally evaluation for methemoglobinemia in association with intercurrent infection, respiratory problems, and anemia is suggested since
associated methemoglobinemia may exaggerate the symptom intensity.
60 Williams et al.

methylene blue administration to G6PD deficient patientsmay aggravate methemoglobinemia, G6PD deficiencyshould be excluded in patients receiving methylene blue.Ascorbic acid may be used as an alternative therapy.Occasionally an exchange transfusion may be necessary[26]. Concomitant administration of cimetidine, throughinhibition of dapsone-hydroxylamine formation, has beenshown to reduce metHb formation and improve patienttolerance [4,53].
LowCb5R levels in symptomatic patients in the presentseries indicated that development of methemoglobinemiaon prophylactic doses of dapsone was likely a reflectionof reduced capacity to respond to oxidant stress ratherthan oversaturation of normal enzyme capacity as seen inpatients with overdose of an oxidant agent. Hence, thesesusceptible individuals are likely to be at risk for re-currence of methemoglobinemia, if exposed to otheroxidant agents even at therapeutic doses. In immunocom-promised patients, including patients with cancer, there issubstantial risk of future exposure to oxidants (like anes-thetics, sulphones, and nitrites) causing methemoglobi-nemia. This point is highlighted particularly in the recentreport byMoreira et al. describing methemoglobinemia inan 8-year-old patient receiving clofazimine therapy forchronic graft-versus-host disease [54]. Hence, patientsdiagnosed with methemoglobinemia should be counseledfor avoidance of oxidizing agents. Ultimately this wouldavoid unnecessary investigations, hospitalization, and theincurred cost to the health care system.
CONCLUSIONS
Despite the small sample size, the present series in-dicates that methemoglobinemia is not an uncommonproblem in children with ALL receiving thrice-weeklydapsone for PCP prophylaxis. These patients are sympto-matic at low levels ofmetHb. IndividualswithCb5R levelsconsistent with a heterozygous state are more likely todevelop symptomatic methemoglobinemia when receiv-ing dapsone prophylaxis compared to those with normallevels of the enzyme. Due to this genetic pre-disposition,subsequent exposure to oxidant agents should be avoided,when possible. A high index of suspicion is required todetect methemoglobinemia, in this chronically ill patientpopulation. Due to symptomatic overlap between ALLand methemoglobinemia the diagnosis of methemoglobi-nemia may be delayed. Hence, we recommend frequentmonitoring of patients receiving dapsone and proposeguidelines for monitoring patients on dapsone for timelydetection and management of methemoglobinemia.
REFERENCES
1. Hughes WT. Use of Dapsone in the prevention and treatment of
Pneumocystis carinii pneumonia: A review. Clin Infect Dis 1998;
27:191–204.
2. Mirochnick M, Cooper E, Capparelli E, et al. Population pharma-
cokinetics of dapsone in children with human immunodeficiency
virus infection. Clin Pharmacol The 2001;70:24–32.
3. Castro M. Treatment and prophylaxis of Pneumocystis carinii
pneumonia. Semin Respir Infect 1998;13:296–303.
4. Zhu IY, Stiller MJ. Dapsone and sulfones in dermatology: Over-
view and update. J A Acad Dermatol 2001;45:420–434.
5. Chawla R, Gumani A, Bhattacharya A. Acute dapsone poisoning.
Anaesth Intensive Care 1993;21:349–351.
6. Szeremeta W, Dohar JE. Dapsone induced methemoglobinemia:
An anesthetic risk. Int J Pediatr Otorhinolaryngol 1995;33:75–80.
7. Dawson AH, Whyte IM. Management of dapsone poisoning com-
plicated by methemoglobinemia. Med Toxicol Adverse Drug Exp
1989;4:387–392.
8. Ward KE, McCarthy MW. Dapsone-induced methemoglobinemia.
Ann Pharmacother 1998;32:549–553.
9. Mandrell BN, McCormick JN. Dapsone-induced methemoglobi-
nemia in pediatric oncology patients: Case examples. J Pediatr
Oncol Nurs 2001;18:224–228.
10. Stavola JJ, Noel GJ. Efficacy and safety of dapsone prophylaxis
against Pneumocystis carinii pneumonia in human immunodefi-
ciency virus-infected children. Pediatr Infect Dis J 1994;12:644–
647.
11. Medina I, Mills J, Leoung G, et al. Oral therapy for Pneumocystis
carinii pneumonia in the acquired immunodeficiency syndrome: A
controlled trial of trimethoprime-sulfamethaoxazole versus tri-
methoprim-dapsone. N Eng J Med 1990;323:776–782.
12. Cohen RJ, Sachs JR, Wicker DJ, et al. Methemoglobinemia
provoked bymalarial chemoprophylaxis in Vietnam. N Engl JMed
1968;279:1127–1131.
13. Collins JF. Methemoglobinemia as a complication of 20% benzo-
caine spray for endoscopy. Gastroenterology 1990;98:211–213.
14. Molthrap DC, Wheeler RM, Hall KM, et al. Evaluation of the
methemoglobnemia associated with sulofenor. Invest New Drugs
1994;12:99–102.
15. Frey B, Kehrer B. Toxic methemoglobin concentrations in pre-
mature infants after application of prilocaine containing cream and
peridural prilocaine. Eur J Pediatr 1999;158:785–788.
16. Gunter JB. Benefits and risks of local anesthetics in infants and
children. Pediatr Drugs 2002;4:649–672.
17. Nilsson A, Engberg G, Hennsberg S, et al. Inverse relationship
between age dependent erythrocyte activity of methemoglobin
reductase and prilocaine-induced methemoglobinemia during
infancy. Br J Anesth 1990;64:72–76.
18. Conroy JM, Baker DJ, Martin J, et al. Acquired methemoglobi-
nemia from multiple oxidants. South Med J 1993;86:1156–
1159.
19. Dinneen SF, Mohr DN, Fairbank VF. Methemoglobinemia from
topically applied anesthetic spray. Mayo Clin Proc 1994;69:886–
888.
20. Beutler E. Red cellmetabolism:Amanual of biochemicalmethods.
New York, NY: Grune & Stration; 1971.
21. Lohr GW, Waller HD. Glucose-6-phosphate dehydrogenase. In:
Bergmeyer HU, editor. Methods of enzymatic analysis. New York:
Academic Press; 1974. 636p.
22. Pavri RS, Das Gupta A, Baxi AV, et al. Further evidence for oxida-
tive damage to hemoglobin and red cell membrane in leukemia.
Leuk Res 1983;7:729–733.
23. Curry S.Methemoglobinemia.AnnEmergMed 1982;11:214–221.
24. Price D. Methemoglobinemia. In: Goldfrank LR, Weisman RS,
Flomenbaum NE, Howland MA, Lewin NA, Hoffman RS, editors.
Goldfrank’s toxicologic emergencies. Norwalk, CT: Appleton and
Lange; 1994. pp 643–649.
25. Beutler E. Methemoglobinemia and sulfhemoglobinemia. In:
Beutler E, Lichtman DG, Caller BS, Kipps TJ, editors. Hematology.
Dapsone-Induced Methemoglobinemia in Childhood ALL 61

New York, NY: McGraw-Hill Book Company; 1995. pp 654–
663.
26. Mansourie A, Lurie AA. Concise review: Methemoglobinemia.
Am J Hematol 1993;42:7–12.
27. Konig MW, Dolinski SY. A 74-tear-old woman with desaturation
following surgery. Chest 2003;123:613–616.
28. Fisher RA, Povey S, Bobrow M, et al. Assignment of the DIA 1
locus to chromosome 22. Ann Hum Genet 1977;41:151–155.
29. PercyMJ,McFerran NV, Lappin TRJ. Disorders of oxidized hemo-
globin. BloodRev 2004 (Article in press; www.elsevierhealth.com/
journals/blre).
30. Bunn FH. Human hemoglobins: Normal and abnormal. In: Nathan
DG, Orkin SH, editors. Hematology of infancy and childhood. Vol
1. Philadelphia, PA: Saunders; 1998. pp 729–761.
31. Ganer A, Knobel B, Fryd CH, et al. Dapsone-induced methemo-
globinemia and hemolysis in the presence of familial hemo-
globinopathy hasharon and familial methemoglobin reductase
deficiency. Isr J Med Sci 1981;17:703–704.
32. Beretta M, Santachiara-Benerecetti AS. Study of human red cell
NADH diaphorase (Dia1) in the Italian population. Hum Hered
1985;35:7–10.
33. MooreMR, ConradME, Bradley EL, et al. Studies of nicotinamide
adenine dinucleotide methemoglobin reductase activity in a Jewish
population. Am J of Hem 1982;12:13–18.
34. Fisher RA, Edwards YH, Putt W, et al. An interpretation of human
diaphorase isozymes in terms of three gene loci DIA1, DIA2 and
DIA3. Ann Hum Genet 1977;41:139–149.
35. Scott EM, Hoskins DD. Hereditary methemoglobinemia in
Alaskan Eskimos and Indians. Blood 1958;13:795–802.
36. Scott EM. The relation of diaphorase of human erythrocyte to
inheritance of methemoglobinemia. J Clin Invest 1960;39:1176–
1179.
37. Kaluarachchi SI, Fernandopulle BM, Gunawardane BP. Hepatic
and hematological adverse reaction associated with the use of
multi-drug therapy in leprosy—A five year retrospective study. Ind
J Lepr 2001;73:121–129.
38. Erstad BL. Dapsone-induced methemoglobinemia and hemolytic
anemia. Clin Pharm 1992;11:800–805.
39. Uetrecht J,WalmsleySL.Drugs affecting nucleic acid synthesis. In:
Kalant H, Roschlau HE, editors. Principles of medical pharmacol-
ogy. 6th Edition, New York: Oxford University Press, New York;
1998. pp 707–711.
40. Mirochnick M, Cooper E, Capparelli E, et al. Pharmacokinetics
of dapsone administered daily and weekly in human immuno-
deficiency virus-infected children. Antimicrob Agents Chemother
1999;43:2586–2591.
41. Mirochnick M, Michaels M, Clarke D, et al. Pharmacokinetics of
dapsone in children. J Pediatr 1993;122:806–809.
42. Wright RO, Lewander WJ, Woolf AD. Methemoglobinemia: Etio-
logy, pharmacology and clinical management. Ann Emerg Med
1999;34:646–656.
43. Saito T, Takeichi S, Osawa M, et al. A case of fatal methemoglo-
binemia of unknown origin but presumably due to ingestion of
nitrate. Int J Legal Med 2000;113:164–167.
44. Jaeger A, Sauder P, Kopferschmitt J, et al. Clinical features and
management of poisoning due to antimalarial drugs. Med Toxicol
Adverse Drug Exp 1987;2:242–273.
45. Gallant JE, Hoehn-Saric E, Smith MD. Respiratory insufficiency
from dapsone induced methemoglobinemia. AIDS 1991;5:1392–
1393.
46. ReiterWM, Cinoch PJ. Dapsone-inducedmethemoglobinemia in a
patient with P. carinii pneumonia and AIDS (letter). N Engl J Med
1987;317:1740–1741.
47. Landers D, Bergin C, Leary A, et al. Dapsone induced methemo-
globinemia. Int J STD AIDS 1996;7:445–447.
48. Iserson KV. Methemoglobinemia from dapsone therapy for a
suspected brown spider bite. J Emerg Med 1985;3:285–288.
49. Barker SJ, Tremper KK,Hyatt J. Effects ofmethemoglobinemia on
pulse oximetry and mixed venous oximetry. Anesthesiology 1989;
70:112–117.
50. Anderson ST, Hajduczek J, Barker SJ. Benzocaine-induced
methemoglobinemia in an adult: Accuracy of pulse oximetry with
methemoglobinemia. Anesth Analg 1988;67:1099–1101.
51. Clifton J II, Leikin JB. Methylene blue. Am J Ther 2003;10:289–
291.
52. Groeper K, Katcher K, Tobias JD. Anesthetic management of a
patient with methemoglobinemia. South Med J 2003;96:504–
509.
53. Coleman MD. Dapsone toxicity: Some current perspectives. Gen
Pharmacol Vasc Sys 1995;26:1461–1467.
54. Moreira VdA, De Medeiros BC, Bonfim CMS, et al. Methemoglo-
binemia secondary to clofazimine treatment for chronic graft-
versus-host disease [letter]. Blood 1998;92:4872–4873.
62 Williams et al.