Mesenchymal Stem Cells for the Treatment of Spinal Arthrodesis:...
Transcript of Mesenchymal Stem Cells for the Treatment of Spinal Arthrodesis:...

Review ArticleMesenchymal Stem Cells for the Treatment of SpinalArthrodesis: From Preclinical Research to Clinical Scenario
F. Salamanna,1 M. Sartori,2 G. Barbanti Brodano,3 C. Griffoni,3 L. Martini,1
S. Boriani,3 and M. Fini1
1Laboratory of Preclinical and Surgical Studies, Rizzoli Orthopedic Institute, Bologna, Italy2Laboratory of Biocompatibility, Technological Innovations and Advanced Therapies,Rizzoli Research Innovation Technology Department, Rizzoli Orthopedic Institute, Bologna, Italy3Department of Oncological and Degenerative Spine Surgery, Rizzoli Orthopedic Institute, Bologna, Italy
Correspondence should be addressed to M. Sartori; [email protected]
Received 23 September 2016; Accepted 5 January 2017; Published 13 February 2017
Academic Editor: Marco Tatullo
Copyright © 2017 F. Salamanna et al. This is an open access article distributed under the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The use of spinal fusion procedures has rapidly augmented over the last decades and although autogenous bone graft is the “goldstandard” for these procedures, alternatives to its use have been investigated over many years. A number of emerging strategies aswell as tissue engineering with mesenchymal stem cells (MSCs) have been planned to enhance spinal fusion rate. This descriptivesystematic literature review summarizes the in vivo studies, dealing with the use ofMSCs in spinal arthrodesis surgery and the stateof the art in clinical applications. The review has yielded promising evidence supporting the use of MSCs as a cell-based therapyin spinal fusion procedures, thus representing a suitable biological approach able to reduce the high cost of osteoinductive factorsas well as the high dose needed to induce bone formation. Nevertheless, despite the fact that MSCs therapy is an interesting andimportant opportunity of research, in this review it was detected that there are still doubts about the optimal cell concentrationand delivery method as well as the ideal implantation techniques and the type of scaffolds for cell delivery. Thus, further inquiry isnecessary to carefully evaluate the clinical safety and efficacy of MSCs use in spine fusion.
1. Introduction
Spinal fusion is a commonmeans to treat vertebral instability.Its use has quickly increased over the last decades in orderto realize the stabilization of the spine in patients affected bydegenerative, oncologic, and traumatic spine diseases. Auto-genous bone harvested from the iliac crests is the standardprocedure for spinal fusion surgery and it is used in morethan 190.000 cases/year in Europe [1]. It owns all the key graftmaterial properties, that is to say osteoconduction, osteoin-duction, osteogenic potential, and also structural integrity ifcorticals are comprised. However, the use of autologous bonegraft has been described to be linked with 5% to 35% non-union rate, intraoperative blood loss, and residual morbidityat the donor sites in about 30% of the patients [2]. Thereare many factors inherent to the spine fusion failure such astensile forces, low bone surface, and interference by sur-rounding musculature [3]. In addition, the time required for
spinal fusion increases with advancing age and the fusion rateremains unpredictable in the ageing population [4]. More-over, smoking, osteoporosis, and systemic illnesses have anadverse impact on bone and in particular in spinal surgery[5, 6].The presence of these intrinsic complications has givenrise to research into newmaterials andmethods avoiding iliaccrest harvesting. Thus, there are differing lines of researchsuch as bone substitutes (allografts, demineralized bonematrix, and ceramics) and osteoinductive growth factors(bone morphogenic proteins). However, bone substitutes,which are merely osteoconductive and not osteoinductive,remain yet to be finished as substitutes for bone because thefusion achieved with them is not solid enough. In fact, for asuccessful spinal fusion to occur, several essential elementsin addition to a biocompatible scaffold are necessary. Theyinclude the presence of the bone-forming cells or theirprecursors and an appropriate biological signal that directbone synthesis. The most critical of these components are
HindawiStem Cells InternationalVolume 2017, Article ID 3537094, 27 pageshttps://doi.org/10.1155/2017/3537094

2 Stem Cells International
the osteoblasts or their precursors, the mesenchymal stemcell (MSC), both of which own the ability to form bone. Toovercome these limitations, researchers have focused on newtreatments that will allow for safe and successful bone repairand regeneration. In this field, adult stem cells derived frommesenchymal tissue represent a promising source for boneengineering for their ability to differentiate into osteoblasts.MSCs are undifferentiated cells characterized by a highproliferation rate that were found in several adult tissues[7–9]. The multipotent nature of individual MSCs was firstestablished in 1999 by Pittenger et al. [10], and since then theyhave been found to be pluripotent, giving rise to endoderm,ectoderm, and mesoderm cells [11]. Thus, MSCs are wellsuited to therapeutic applications also because they can beeasily cultured and have high ex vivo expansive potential[12–15]. In the treatment of several musculoskeletal injuries,such as bone, articular cartilage, and other joint tissues,MSCsfrom bone marrow (BMSCs) are the most widely used cells,followed byMSCs from adipose tissue (ADSCs) [16–18]. Bothtypes of cells have been demonstrated to have a significanteffect on spinal fusion in a multitude of settings including avariety of culturingmechanisms, scaffolds, and added growthfactors. However,MSCs represent a lesser (0.001–0.01%) frac-tion of the total population of the nucleated cells [19, 20]. Toincrease the concentration of MSCs, several techniques havebeen developed, especially cell ex vivo expansion, but manyproblems limited the clinical application, such as the sterilitytechnique, long culture time, high cost, and the mixtureof human cell culture mediumwith fetal bovine serum.Thus,the method of collecting MSCs, as well as the real number ofMSCs to be transplanted, remains yet to be established.
To date, a great body of research on MSCs for spinalfusion procedures was performed in vitro and in vivo but aclinical customary procedure for the use of cell-based strate-gies for spinal fusion surgery has not been established andcontrasting clinical but also preclinical results were reportedin literature. More importantly, the clinical transferabilityof some protocols is still to be settled, to optimize timeand sources when modified/stimulated cells, custom madescaffolds, and in vitro steps are required [21]. Thus, in thissystematic review, we aimed to evaluate the efficacy of MSCsin spinal arthrodesis procedures considering the preclinicaland clinical studies of the last 10 years to shed light on usingMSCs for spinal fusion treatment.
2. Motivations
2.1. Why a Systematic Review? We have seen the necessity forperforming a descriptive systematic literature review onMSCs use in spinal arthrodesis procedures in order to under-stand if the use of MSCs may represent a valid strategy ableto facilitate and accelerate bone regeneration during spinesurgery providing to researchers and clinicians a beginningpoint with solid foundations allowing this field tomake a leapforward. Our aim is to offer answers to questions such asthe following: “Since bone contains a complex environmentof many cell types, areMSCs able to perform all the necessaryphysiological functions to achieve, facilitate, and acceleratespinal fusion?,” “What happens to MSCs when they are
added to a scaffold?,” “Which source of MSCs is better touse and which techniques (ex vivo expansion and one-stepprocedure) are better to use?,” “How much does the existingpreclinical model reflect the data so far collected in clinicalstudies?,” and “What do we have to do to further clarifythe potential role of MSCs in spinal fusion procedures?”Specifically, we want to summarize the knowledge collectedin nearly 10 years of research, learning from previous preclin-ical and clinical research which used MSCs for spinal fusionprocedures, since there is an exigent need to have successfulspinal fusion.
3. Methods
3.1. Descriptive Systematic Literature Review. Our descriptiveliterature review involved a systematic search that was carriedout, according to the Preferred Reporting Items for Systema-tic Reviews andMeta-Analyses (PRISMA) statement, in threedatabases (https://www.ncbi.nlm.nih.gov/pubmed, https://www.webofknowledge.com, and https://www.scopus.com).In order to evaluate the ongoing clinical studies, the https://www.clinicaltrials.gov website was also checked. The key-words were mesenchymal stromal cells OR mesenchymalstem cells OR mesenchymal/progenitor stromal cells ORmesenchymal/progenitor stem cells AND spinal arthrode-sis OR spinal fusion OR interbody fusion OR vertebralarthrodesis OR vertebral fusion. We sought to identifystudies where MSCs were employed for spinal fusion pro-cedures. Publications from 2006 to 2016 (original articlesin English) were included. A public reference manager(“http://www.mendeley.com”) was used to delete duplicatearticles.
4. Results and Discussion
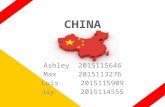
An initial literature search retrieved 444 references (Figure 1).Hundred and twenty-nine articles were identified usinghttps://www.ncbi.nlm.nih.gov/pubmed, 210 articles wereidentified using https://www.webofknowledge.com, and 105articles were found in https://www.scopus.com. Six addi-tional articles were obtained from the website https://www.clinicaltrials.gov. The resulting references were selected forsupplementary analysis based on the title and abstracts and149 were considered eligible. References were submitted to apublic referencemanager (Mendeley 1.14, “https://www.men-deley.com”) to eliminate duplicate articles. Sixty completearticles were then reviewed to establish whether the publica-tionmet the inclusion criteria and 50 articles were recognizedeligible for the review considering publications from 2006 to2016 (Figures 2(a) and 2(b)).Thirty-nine articles were in vivostudies on small, medium, and large animal models (Tables 1,2, and 3) while the remaining 11 articles were clinical studiesor clinical trials (Tables 4 and 5).
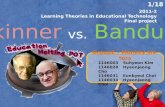
Figure 3 summarizes the main steps of spinal fusion stemcell-based therapy founded in this literature search.
We did not performmeta-analyses of the selected studiesbut reported the results in a descriptive fashion. By consid-ering the studies emerging from this review, we stratified the

Stem Cells International 3
Table1:Pu
blish
edin
vivo
studies
insm
allanimalmod
elso
nmesenchym
alste
mcells
forspinalarthrod
esisprocedures.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Ovarie
ctom
ized
rat
hPSC
sfrom
adiposetissue
ofpatie
ntsw
ithand
with
out
osteop
orosis
NEL
L-1
DBM
/𝛽-TCP
4weeks
L4-L5
Group1:DBM
/𝛽-TCP
with
hPSC
s(0.25×106cells/m
L)Gr
oup2:DBM
/𝛽-TCP
with
hPSC
s(0.75×106cells/m
L)Gr
oup3:DBM
/𝛽-TCP
with
NEL
L-1
(33.3𝜇
g/mL)
Group4:DBM
/𝛽-TCP
with
NEL
L-1
(66.6𝜇
g/mL)
Group5:DBM
/𝛽-TCP
with
hPSC
s/NEL
L-1atthe
dosage
ofgrou
ps1and
3Gr
oup6:DBM
/𝛽-TCP
with
ahP
SCs/NEL
L-1atthe
dosage
ofgrou
ps2and4
(i)Group
1achievedafusionrateof
20%
(1/5),grou
p2of
28.6%
(2/7),
grou
ps3and4of
20%
(1/5),and
grou
p5of
37.5%
(3/8),andgrou
p6
improved
thefusionratesu
pto
approxim
ately
83.3%
(5/6)
(ii)M
icrocompu
tedtomograph
yim
agingandqu
antifi
catio
nfurther
confi
rmed
solid
bony
fusio
nin
grou
p6
[22]
Rat
Intoto
ratb
one
marrowfro
mfemur
flush
(1.1×107cells/m
L)bF
GF
PEGDA-
co-
A6A
CAhydrogels
(poly(ethylene
glycol)-
diacrylate
hydrogel
(PEG
DA)a
ndN-acryloyl6-
aminocaproic
acid
(A6A
CA))
2,4,6,and8
weeks
L4-L5
Group1:scaffoldwith
bone
marrow
Group2:scaffo
ldwith
bFGF
Group3:scaffoldwith
salin
esolution
(i)Ra
diograph
ssho
wed
fusio
nmassesin4anim
also
utof
7in
each
grou
pat2weeks.A
t4weeks,all
anim
alssho
wed
clear
evidence
ofhard
tissueformation,
with
progressively
increase
at6and8
weeks
(ii)𝜇
-CTim
agingat8weeks
revealed
a51%
ofmineralized
hard
tissuefor
grou
p3,59%
forg
roup
2,and54%
forg
roup
1(iii)Manualp
alpatio
nprovided
evidence
offusio
nin
allgroup
s,with
nosig
nificantd
ifferencesinfusio
nindices
[23]
Rat
Freshbo
nemarrow(BM)cells
(range,0.60to
2.60×106BM
cells)
rhBM
P-2
(0.006
mg/mL)
Absorbable
collagen
spon
ge(A
CS)
8weeks
L4-L5
Group1:2A
CSwith
fresh
BMand
rhBM
P-2
Group2:2A
CSwith
rhBM
P-2
Group3:1A
CSwith
rhBM
P-2
Group4:AC
Swith
BMGr
oup5:AC
Salon
e
(i)In
grou
p1B
Mplus
rhBM
P-2/AC
Ssig
nificantly
increasedthefusionrate
to89%
(16/18)com
paredwith
abase
fusio
nrateof
33%
(4/12
)ingrou
p3
and50%
(6/12
)ingrou
p2(𝑝<0.05)
(ii)N
odifferenceinstr
engthor
stiffn
essw
asdetected
amon
ggrou
p1
andgrou
ps2and3.
(iii)Nofusio
nor
bone
form
ationwas
observed
inther
atso
fgroup
s4and5
[24]

4 Stem Cells International
Table1:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rat
Expand
edMSC
s(3×106)from
goatBM
iliac
crest
lentivira
llytransduced
toexpressluciferase
Non
eHA/𝛽-TCP
7weeks
L1-L2and
L4-L5
Group1:no
cells
Group2:MSC
sGr
oup3:MSC
sgam
ma-irr
adiated
(30G
y)Gr
oup4:MSC
sdippedin
liquidN2
(i)Th
eantilu
ciferase
immun
ohistochemistry
show
edno
newlyform
edbo
neor
luciferase-positive
cells.
(ii)H
istologicalstaining
with
Hem
atoxylin/Eosin
high
lighted
nosig
nsof
abon
eformationin
any
grou
ps
[25]
Rat
Expand
edbo
nemarrowfro
mrat
femur
(1×107
cell/mL)
Non
e
Silkfib
roin
(SF)
and
mineralized
silkfib
roin
(mSF)
12weeks
L4-L5
Group1:SF
scaffold
Group2:SF
with
MSC
sGr
oup3:mSF
Group4:mSF
with
MSC
sGr
oup5:autograft
Group6:sham
grou
p
Fusio
nrate,bon
evolum
e,biom
echanicalp
aram
eters,and
histo
logicalscore
show
edno
significantd
ifferencesb
etweengrou
p4andgrou
p5.Group
3was
significantly
greaterfor
most
parametersthangrou
p2
[26]
Rat
Allo
genicM
SCs
Non
e8weeks
L4-L5
Group1:trinity
evolution(D
BMwith
MSC
s)Gr
oup2:graft
on(D
BM)
Group3:DBM
Group4:decorticationon
ly
(i)Fu
sionrateby
radiograph
ywas
8/8forg
roup
1,3/8forg
roup
2,and
5/8forg
roup
3(ii)F
usionrateby𝜇-C
Tandmanual
palpationwas
4/8forg
roup
1,3/8for
grou
p2,and3/8forg
roup
3
[27]

Stem Cells International 5
Table1:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Mou
seBo
nemarrow
from
femur
and
tibia(1.0×108
cells/m
L)
PRPfro
mdo
nor(1.0×
109
platelets/mL)
orrhBM
P-2
(31𝜇
g/mL)
ACS
4weeks
L4-L5and
L5-L6
Group1:collagenspon
gewith
rhBM
P-2andsalin
esolution
Group2:collagenspon
gewith
rhBM
P-2andPR
PGr
oup3:collagenspon
gewith
rhBM
P-2andBM
Group4:decorticationon
ly
(i)Fu
sionappeared
radiograph
ically
andhisto
logically
similarinallthree
experim
entalgroup
s(ii)Th
earea,volume,anddensity
ofthefusionmassw
eres
ignificantly
greater(𝑝<0.05)for
grou
p3as
comparedwith
grou
p1
(iii)Group
2hadinterm
ediatefusio
narea
anddensity
(iv)N
ospinalfusio
nwas
detected
ingrou
p4
[28]
Rat
Expand
edrat
bone
marrow
from
femurs(1×
106cells/m
L)Fibrin
matrix
PCL-TC
P6weeks
L4-L5
Group1:10𝜇gof
rhBM
P-2with
1×106un
differentiatedBM
SCs
Group2:10𝜇gof
rhBM
P-2with
osteogenic-differentiatedBM
SCs
Group3:2.5𝜇
grhBM
P-2with
undifferentiatedBM
SCs
Group4:2.5𝜇
grhBM
P-2with
osteogenic-differentiatedBM
SCs
Group5:0.5𝜇
grhBM
P-2with
undifferentiatedBM
SCs
Group6:0.5𝜇
grhBM
P-2with
osteogenicdifferentiatedBM
SCs
(i)Predifferentia
tionof
BMSC
sbefore
transplantationfailedto
prom
otep
osterolateralspinalfusion
whencodelivered
with
low-doseo
frhBM
P-2in
grou
p5as
17%
fusio
nratewas
observed
(1/6)
(ii)Incontrast,
combineddeliveryof
undifferentiatedBM
SCsw
ithlow-doseB
MP-2(2.5𝜇g)
asin
grou
p5demon
strated
significantly
high
erfusio
nrate(4/6
or67%)a
swellas
significantly
increasedvolumeo
fnew
bone
form
ation
[29]
Rat
Hum
anbo
nemarrow(5×106
MSC
s)Non
eTitanium
microplates
with
HA
8weeks
L1–L
3Gr
oup1:titanium
microplates
with
HA
Group2:titanium
microplates
with
HA/M
SCs
Histolog
y,histo
morph
ometry,and
𝜇-C
Trevealed
nosig
nificantb
one
form
ationin
grou
p2in
comparis
onwith
grou
p1
[30]

6 Stem Cells International
Table1:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rat
ADSC
s(5×106
cells/scaffo
ld)
rhBM
P-2
oradenovira
lvector
containing
BMP-2gene
Type-Icollagen
spon
ge4weeks
L4-L5
Group1:ADSC
stransdu
cedwith
anadenovira
lvectorc
ontaining
rhBM
P-2gene
Group2:ADSC
swith
osteogenic
mediaand1m
g/mLof
recombinant
rhBM
P-2
Group3:rhBM
P-2(10m
g)Gr
oup4:rhBM
P-2(1mg)
Group5:ADSC
s
(i)Allanim
also
fgroup
1were
characteriz
edby
fusio
nmasses(8/8)
after
4weeks
(ii)G
roup
1revealedspinalfusio
nat
thec
ephaladlevel(L3
andL4
)(iii)New
bone
form
ationin
grou
ps1
was
significantly
larger
than
thosein
anyothertreatmentg
roup
(𝑝<0.005)
(iv)G
roup
s3and4show
edas
olid
fusio
nin
8/8and4/8anim
als,
respectiv
ely(v)G
roup
s2and5show
edno
fusio
n
[31]
Rat
hPSC
sfrom
adiposetissue
Non
eDBM
4weeks
L4-L5
Group1:DBM
Group2:DBM
with
0.15×106hP
SCs
Group3:DBM
with
0.50×106hP
SCs
Group4:DBM
with
1.50×106hP
SCs
(i)hP
SCtre
atment(grou
ps2,3,and
4)sig
nificantly
increasedspinal
fusio
nratesincomparis
onwith
grou
p1
(ii)G
roup
s2,3,and
4resultedin
fusio
nrateso
f100%,80%
,and
100%
,respectiv
ely,com
paredwith
20%
fusio
nin
grou
p1
(iii)Com
puteriz
edbiom
echanical
simulation(finiteelem
entanalysis
)furtherd
emon
strated
bone
fusio
nin
hPSC
treatmentg
roup
s(iv
)Histologicalanalyses
show
edendo
chon
dralossifi
catio
nin
hPSC
-treatedsamples
[32]
Rat
ADSC
sfrom
healthydo
nors
(1.0×106)
PurchasedBM
SCs
(1.0×106)
Adenovira
lvectors
adeno-BM
P-2
and
adeno-La
cZused
totransduce
ADSC
sand
BMSC
s
ACS
8weeks
L4-L5
Group1A
CSwith
ADSC
stransfected
with
adeno-BM
P-2
Group2AC
Swith
BMSC
stransfe
cted
with
adeno-BM
P-2
Group3AC
Swith
rhBM
P-2
Group4AC
Swith
ADSC
stransfected
with
adeno-LacZ
Group5AC
Swith
BMSC
stransfe
cted
with
adeno-LacZ
,and
Group6AC
S
(i)Spinalfusio
nwas
observed
ingrou
ps1,2,and3rats
(ii)7
5%(15/20)o
fthe
anim
also
fgrou
psIand
IIhadspon
taneou
sextensionof
thefusionto
asecon
dlevel
(iii)Noanim
alsingrou
ps4,5,and6
ratsdevelopedfusio
n(iv
)New
bone
volumew
assig
nificantly
greateringrou
ps1and
2than
ingrou
p4
[33]

Stem Cells International 7
Table1:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rat
Expand
edBM
cells
from
femurs
andtib
ias
(1×106/60𝜇
L)
FGF-4
(41𝜇
g)HA
8weeks
L4-L5
Group1:HA
Group2:HAwith
MSC
sGr
oup3:HAwith
MSC
sand
FGF-4
(i)Ra
diograph
ic,high-resolutio
n𝜇-C
T,andmanualp
alpatio
nrevealed
spinalfusio
nin
5/6(83%
)ingrou
p2
(ii)Ingrou
p1,3/6(60%
)rats
developedfusio
natL4
-L5by
radiograph
yand2/5(40%
)by
manualp
alpatio
nin
radiograph
icexam
ination
(iii)In
grou
p3,bo
nefusio
nwas
observed
inon
ly50%
ofratsby
manualp
alpatio
nandradiograph
icexam
ination
[34]

8 Stem Cells International
Table2:Pu
blish
edin
vivo
studies
inmedium
anim
almod
elso
nmesenchym
alste
mcells
forspinalarthrod
esisprocedures.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffoldmaterial
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rabbit
Expand
edBM
from
iliac
crest(1.5
×106cells/m
L)Oste
ogenic
medium
HA
6weeks
L5-L6
Group1:autograft
Group2:HAwith
type
Icollagengel
Group3:HAandtype
Icollagengel
with
MSC
sGr
oup4:HAandtype
Icollagengel
with
MSC
sind
uced
toward
osteogenicph
enotype
Thefusionratesw
ere
4/6in
grou
p1;
0/6in
grou
p2;
2/6in
grou
p3;and
4/5in
grou
p4
[35]
Rabbit
FreshBM
from
iliac
crests
Fibron
ectin
HA
6weeks
L4-L5
Group1:autograft
from
iliac
crest
Group2:autograft
from
transverse
processb
oneg
raft
Group3:HAsticksa
ndiliac
bone
graft
Group4:HAsticksw
ithBM
aspirate
Group5:HAsticks
Group6:HAsticksw
ithFN
andBM
aspirate.
Group7:decorticationon
ly
(i)Th
eelasticityandmechanical
strengthweres
ignificantly
high
erin
grou
p1thanin
grou
ps2,4,and5
(ii)Th
emechanicalstre
ngth
achieved
ingrou
ps3and6was
nearlyequalto
thatin
grou
p1
(iii)Th
emechanicalstre
ngth
was
significantly
high
erin
grou
p6than
ingrou
p4
(iv)H
istologyshow
edintraporou
sosteogenesisin
grou
ps3,4,and6
[36]
Rabbit
Expand
edBM
cells
from
iliac
crest(1×
106cells/m
L)
(i)rhBM
P-2
(ii)b
FGF
(iii)Au
tograft
HA
6weeks
L4–L
5
Group1:autograft
Group2:HAwith
MSC
sGr
oup3:HAwith
MSC
sand
BMP
Group4:HAwith
MSC
sand
bFGF
Group5:HAwith
MSC
sand
BMP/bF
GF
Thefusionratesw
ere
4/7in
autograft
grou
p;0/7in
MSC
s/HAgrou
p;2/7in
MSC
s/HA/BMPgrou
p;3/7in
MSC
s/HA/FGFgrou
p;and
6/7in
MSC
s/HA/BMP/bF
GFgrou
p
[37]

Stem Cells International 9
Table2:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffoldmaterial
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rabbit
Expand
edBM
cells
from
iliac
crest
Non
eNon
e8weeks
L4-L5
Group1:autograft
Group2:autograft
with
MSC
s(i)
Ingrou
p1,thefusionratewas
53%
(8/15
)(ii)Ingrou
p2,thefusionratewas
0%[38]
Rabbit
BMfro
mfemur,
tibia,trochanter,
andiliac
crest
Non
eTC
P7weeks
L5-L6
Group1:TC
Palon
eGr
oup2:TC
Pwith
MSC
sGr
oup3:TC
Pwith
MSC
sand
LIPU
S
(i)Sign
ificant
increase
inmanual
palpationin
grou
p3tre
ated
with
LIPU
S(86%
)incomparis
onwith
grou
ps1(0%
)and
2(14
%)w
ithou
tLIPU
S(ii)Th
ebon
evolum
eoffusionmass
was
significantly
larger
ingrou
p3
than
theo
ther
twogrou
psby
quantitativec
ompu
tedtomograph
icanalysis
(iii)Group
3fusio
nmassh
adab
etter
osteointegratio
nleng
thbetweenho
stbo
neandim
plantedcompo
sitea
ndpresentedmoren
ewbo
neform
edin
theT
CPim
plants
(iv)G
roup
3hadosteocho
ndral
bridging
,earlystageo
fbon
yfusio
n,fro
mhisto
logicalp
oint
ofview
[2]
Rabbit
Expand
edBM
from
iliac
crest
Non
ePo
ly(la
ctide-co-
glycolide)
(PLG
A)/HA/
type
Icollagen
6weeks
or12
weeks
after
graft
ing
L4-L5
Group1:autograft
Group2:PL
GA/H
A/TypeI
collagen
with
MSC
s
Radiograph
ic,com
putedtomograph
yexam
inations,torsio
nalloading
tests
,andhisto
logice
xaminations
show
edsolid
fusio
nin
3/5rabbits
inbo
thexperim
entalgroup
sat6
weeks
and
5/5solid
fusio
nin
both
grou
psat12
weeks
[39]

10 Stem Cells International
Table2:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffoldmaterial
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rabbit
ADSC
sfrom
the
inguinalgroo
veNon
eNano-
hydroxyapatite–
collagen–
polylactic
acid
(nHAC
–PLA
)10
weeks
L5-L6
Group1:autograft
Group2:nH
AC–P
LAGr
oup3:autograft
with
nHAC
–PLA
Group4:ADSC
swith
nHAC
–PLA
(i)Th
erateo
ffusionwas
significantly
high
erin
grou
p1and
grou
p4than
ingrou
p2andgrou
p3
(ii)M
icrostr
ucturalanalysis
ofthe
samples
show
edmoren
ewbo
ne-like
tissueformationin
grou
p1and
grou
p4than
intheo
ther
twogrou
ps(iii)Mechanicalpropertiessho
wed
thatthes
treng
thandstiffn
esso
fgrou
p1and
grou
p4werem
uch
high
erthan
thoseo
fgroup
2and
grou
p3
[40]
Rabbit
BMfro
mfemur
(1.0×108
allogeneicMSC
s)Non
e
Bioresorbable
purifi
edfib
rillar
collagenandcalcium
phosph
atec
eram
ics
containing
HAand𝛽-
TCP
18weeks
L5-L6
Group1:HA/𝛽
-TCP
with
MSC
sGr
oup2:HA/𝛽
-TCP
(i)In
grou
p1C
Tscanning
revealed
excellent
fusio
nin
2/12
rabbits
(17%
),good
fusio
nin
8/12
(66%
),andfair
fusio
nin
2/12
(17%
)(ii)Ingrou
p2ag
oodfusio
nresult
was
foun
din
3/12
rabbits
(25%
),fair
fusio
nin
6/12
(50%
),andpo
orfusio
nin
3/12
(25%
)
[41]
Rabbit
Expand
edhu
man
BMfro
miliac
crest(107)
Non
e
PLGA/BCP
/collagen
graft
and
MSC
/PLG
A/corallin
eHA/collagen
graft
10weeks
L4-L5
PLGA/BCP
/collagenwith
MSC
s(on
theleft
side)
PLGA/corallin
eHA/collagenwith
MSC
s(on
ther
ight
side)
(i)Ra
diograph
ic,C
T,andbo
nemineralcontentanalysessho
wed
continuo
usbo
nebridgesa
ndfusio
nmassincorpo
ratedwith
the
transverse
processes
(ii)B
onem
ineralcontentvaluesw
ere
high
erin
MSC
s/PL
GA/BCP
/collagen
grou
pthan
inMSC
s/PL
GA/corallin
eHA/collagengrou
p
[42]

Stem Cells International 11
Table2:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffoldmaterial
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rabbit
Expand
edBM
from
iliac
crest(2
×107)
Bac-BM
P-7
Collagen/TC
P/HA
12weeks
L4-L5
Group1:collagen/TC
P/HA
Group2:collagen/TC
P/HAwith
MSC
sGr
oup3:collagen/TC
P/HA/
Bac-BM
P-7with
MSC
s
(i)In
theC
Tresults,6/12
fused
segm
entswereo
bservedin
grou
p1
(50%
),8/12
ingrou
p2(67%
),and
12/12
ingrou
p3(100%)
(ii)Th
efusionrateby
manual
palpationwas
0%(0/6)ingrou
p1,
0%(0/6)ingrou
p2,and83%
(5/6)in
grou
p3
(iii)Histologyshow
edthatgrou
p3
hadmoren
ewbo
neandmatured
marrowform
ation
[43]
Rabbit
Expand
edand
osteogenic
indu
cedBM
from
iliac
crest
(OMSC
s)
Non
eAC
S8and12
weeks
L4-L5
Group1:AC
Swith
OMSC
sGr
oup2:AC
SGr
oup3:autograft
Group4:no
thing
(i)Bo
nyfusio
nwas
evidentase
arly
as8weeks
ingrou
ps1and
3(ii)A
t8and12
weeks,byCT
and
histo
logica
nalysis
,new
bone
form
ationwas
observed
ingrou
ps1
and3andfib
rous
tissuea
ndabsence
ofnewbo
newerep
resent
ingrou
ps2
and4
(iii)Manualp
alpatio
nshow
edbo
nyfusio
nin
40%
(4/10
)ofrabbitsin
grou
p1,70%
(7/10
)ofrabbitsin
grou
p3,and0%
(0/10
)ofrabbitsin
both
grou
ps2and4
[44]
Rabbit
Expand
edBM
from
iliac
crest
(105)
MSC
stransduced
with
Smad1C
gene
Absorbablegelatin
spon
ge4weeks
L6-L7
Group1:BM
SCstransdu
cedwith
Smad1cwith
Ad5vector
Group2:BM
SCstransdu
cedwith
Smad1cwith
Ad5vector
retargeted
to𝛼Vintegrins(RG
D)
Group3:BM
SCstransdu
cedwith
BMP-2with
Ad5vector
Group4:BM
SCstransdu
cedwith
BMP-2with
Ad5vector
retargeted
to𝛼Vintegrins(RG
D)
Group5:BM
SCstransdu
cedwith
anAd
5vector
expressin
gb-galactosidase
(i)Th
eareao
fnew
bone
form
edin
grou
ps1,2,3,and4was
significantly
greaterthanthea
reao
fnew
bone
form
edin
grou
p5(p<0.04
fore
ach
grou
pcomparedwith
grou
p5)
(ii)G
roup
4mediatedag
reater
amou
ntof
newbo
neform
ationthan
grou
p3
(iii)Similarly
,group
2mediateda
greatera
mou
ntof
newbo
neform
ationthan
grou
p1(𝑝<0.0007)
(iv)G
roup
2mediatedag
reater
amou
ntof
newbo
neform
ationthan
theo
ther
grou
ps(𝑝<0.02)
[45]

12 Stem Cells International
Table2:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffoldmaterial
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rabbit
Expand
edand
osteogenic
indu
cedBM
from
iliac
crest(2×106)
rhBM
P-2
Alginates
caffo
ld16
weeks
L4-L5
Group1:autograft
Group2:alginatescaffoldwith
MSC
sGr
oup3:alginatescaffoldwith
MSC
sandrhBM
P-2
Group4:alginatescaffoldwith
rhBM
P-2
(i)Ra
diograph
icun
ionof
grou
p1
was
11/12
,ofgroup
28/11,ofgroup
311/12
,and
ofgrou
p40/12
(ii)M
anualp
alpatio
nhigh
lighted
6/6
solid
fusio
nin
grou
p1,1/6
ingrou
p2,
5/6in
grou
p3,and0/6in
grou
p4
(iii)Th
emechanicalanalysis
(failu
retorque)d
idno
tdiffer
significantly
betweengrou
p1and
grou
p3that
wereb
othhigh
erthan
grou
p2
[46]
Rabbit
Expand
edand
osteogenic
indu
cedBM
from
iliac
crest(2×106)
Non
eAlginates
caffo
ld12
weeks
L4-L5
Group1:alginatescaffold
Group2:alginatescaffoldwith
MSC
sGr
oup3:alginatescaffold/
hyperbaric
oxygen
(HBO
)therapy
with
MSC
s
Radiograph
icexam
inationand
manualp
alpatio
nhigh
lighted
noun
ionforg
roup
1(0/12),10/22for
grou
p2,and6/12
forg
roup
3[47]
Rabbit
Expand
edBM
from
iliac
crest
TCP
Recombinant
baculovirus
encoding
BMP-2
(Bac-C
B)and
vascular
endo
thelial
grow
thfactor
(Bac-VEG
F)
12weeks
L4-L5
Group1:TC
PGr
oup2:TC
Pwith
MSC
Group3:TC
Pwith
MSC
s/Ba
c
(i)Ra
diograph
icallyfusio
nratewas
detected
asbeing0/12
ingrou
p1,4/12
ingrou
p2,and10/12
ingrou
p3
(ii)M
anualp
alpatio
nhigh
lighted
nofusio
nsin
grou
p1,twosolid
fusio
nsin
grou
p2,andfives
olid
fusio
nsin
grou
p3
[48]

Stem Cells International 13
Table2:Con
tinued.
Animalmod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffoldmaterial
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Rabbit
Expand
edand
osteogenic
indu
cedBM
from
iliac
crest
Bioresorbable
hydrogel
(pluronicF
27)
andcoralline
HA
Non
e6and12
weeks
L4-L5
Group1:Pluron
ic127/HAhybrid
graft
with
MSC
sGr
oup2:autograft
(i)Solid
fusio
nwas
achieved
in3/5
rabbits
from
both
grou
p1and
2at6
weeks,and
solid
fusio
nwas
present
in5/5fro
mbo
thgrou
pat12
weeks
(ii)N
odifferences
wered
etected
betweenthetwogrou
psfor
biom
echanicalanalysis
andfro
mhisto
logicalp
oint
ofview
[49]

14 Stem Cells International
Table3:Pu
blish
edin
vivo
studies
inlargea
nimalmod
elso
nmesenchym
alste
mcells
forspinalarthrod
esisprocedures.
Animal
mod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Pig
ADSC
sfrom
ingu
inal
subcutaneous
tissue
Non
eDBM
8and12
weeks
L2–L
6
Group1:on
ecagew
asleftandthree
filledwith
freezed
riedirr
adiated
cancellous
pigbo
negraft
Group2:fre
ezed
riedirr
adiated
cancellous
pigbo
negraft
Group3:cancellous
bone
autograft
Group4:bo
negraft
with
3DosteogenicdifferentiatedADSC
s
𝜇-C
Tscan,m
icroradiograph
y,andhisto
logy/histom
orph
ometry
demon
strated
asignificant
increase
inbo
necontentingrou
p4
[50]
Sheep
Expand
edand
osteogenic
indu
cedBM
SCs
from
iliac
crest
(5-6×107)
Fibrin
TCP/HA
12weeks
L1–L
6
Group1:HAwith
MSC
sGr
oup2:TC
P/HAwith
MSC
sGr
oup3:autograft
(i)Ra
diograph
y,manual
palpation,
histo
logicalanalysis
,andSE
Manalyses
revealed
demon
strated
bette
rbon
eform
ationin
grou
p2compared
togrou
p1
(ii)H
istom
orph
ometry
detected
55.8%of
newbo
nein
grou
p3,
follo
wed
bygrou
p2(42.7%
)and
grou
p1(10.7%)
[51]
Sheep
Allo
genics
heep
mesenchym
alprecursorc
ells
(MPC
s)fro
mBM
from
iliac
crest
Non
eHA/TCP
16–36weeks
L2–L
5
Group1:autograft
Group2:HA/TCP
Group3:HA/TCP
with
MPC
s(25×
106)
Group4:HA/TCP
with
MPC
s(75×
106)
Group5:HA/TCP
with
MPC
s(225
×106)
Com
putedtomograph
y,high
-resolutionradiograph
y,biom
echanicaltestin
g,organ
pathology,bo
nehisto
pathology,
andbo
nehisto
morph
ometry
show
edthatallogeneic
mesenchym
alprecursorc
ells
prod
uced
fusio
neffi
cacy
similar
tothatachieved
usingiliac
crest
autograft
[52]

Stem Cells International 15
Table3:Con
tinued.
Animal
mod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Sheep
Allo
genicM
PCs
from
BMfro
msheepiliac
crest
Non
eHA/TCP
16weeks
L4-L5
Group1:autograft
Group2:HA/TCP
with
MPC
s(2.5×
106)
Group3:HA/TCP
with
MPC
s(6.5×
106)
Group4:HA/TCP
with
MPC
s(12.5
×106)
(i)Manualp
alpatio
nof
the
fusio
nsiteind
icated
solid
fusio
nin
morethan75%of
MPC
-treatedgrou
pand65%of
grou
p1
(ii)C
ompu
tedtomograph
yand
histo
morph
ometry
analyses
show
edallanimalsintheM
PCs
grou
psandgrou
p1fusionmasses
werep
resent
at16
weeks
[53]
Sheep
Expand
edand
osteoind
uced
BMfro
miliac
crest
Non
eHA
6mon
ths
L4-L5
Group1:autograft
Group2:allograft
Group3:HA
Group4:HAwith
MSC
s.
(i)By
CTscan
andhisto
logy
lumbarfusionwe
rehigh
erfor
grou
ps1and
2(70%
)thanfor
grou
p3(22%
)and
grou
p4(35%
)(ii)N
ewbo
neform
ationwas
high
erforg
roup
s1and2
(iii)Group
4hadab
etterfusion
ratethan
grou
p3,bu
tthe
histo
logy
show
edno
significant
differences
betweenthem
interm
sofq
uantity
ofbo
neform
ation
[54]
Sheep
BMconcentrate
(1.5×106in
0.2
mL)
Non
e
Naturalbo
necollagenscaffold
(NBC
S)fro
mhu
man
organic
bone
particles
6and10
weeks
L3-L4and
L4-L5
Group1:autograft
Group2:NBC
SGr
oup3:BM
CsGr
oup4:NBC
Swith
BMCs
(i)Solid
spinalfusio
nwas
achieved
inallsixsegm
ents(6/6)
ingrou
p4at10
weeks,com
pared
with
4/8segm
entsin
grou
p1,2/8
segm
entsin
grou
p2,and3/6
segm
entsin
grou
p3
(ii)Th
ebiomechanicalstiff
ness
offusio
nmassesa
ndbo
nevolumea
tthe
fusio
nsitew
ere
high
erin
grou
p4(p<0.05)
(iii)At
10weeks,the
radiograph
icscorer
eached
was
significantly
high
erin
grou
p4
than
ingrou
ps1,2and3
(iv)H
istologicalfin
ding
srevealed
thatgrou
p4indu
ced
newbo
neform
ationintegrated
wellw
ithho
stbo
netissue
[55]

16 Stem Cells International
Table3:Con
tinued.
Animal
mod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Ewes
Allo
genicM
PCs
(5×106)
orallogenic
amnion
epith
elialstem
cells
(5×106AEC
s)
Non
e
Fidjiinterbo
dycage
madefrom
polyetherether-
ketone
andHA/TCP
3mon
ths
C3-C
4
Group1:cage
packed
with
autograft
Group2:cage
packed
with
HA/TCP
Group3:cage
packed
with
HA/TCP
andMPC
sGr
oup4:cage
packed
with
HA/TCP
andAEC
sGr
oup5:controls
(i)Sign
ificant
fusio
nmassw
asdetected
ingrou
p3comparedto
thatin
grou
ps1,2,or
4(ii)C
Tscan
at3mon
thsrevealed
that5/6anim
alsingrou
p3(83%
)hadcontinuo
usbo
nybridging
comparedwith
0/5of
grou
p4
and1/6
ofgrou
p1and
2/6of
grou
p2(p<0.01)
[56]
Ewes
Allo
geneic
MPC
s(5×106or
10×
106)
Non
e
Fidjiinterbo
dycage
madefrom
polyetherether-
ketone
andHA/TCP
3mon
ths
C3-C
4anterio
rcervical
discectomy
andfusio
nwith
ainterbod
ycage
Group1:cage
packed
with
autograft
Group2:cage
packed
with
HA/TCP
Group3:cage
packed
with
HA/TCP
and5×106MPC
sGr
oup4:cage
packed
with
HA/TCP
and10×106MPC
sGr
oup5:controls
(i)Nosig
nificantd
ifferences
werefou
ndbetweengrou
ps3
and4
(ii)C
Tscan
show
edthat9/12
(75%
)MPC
-treatedanim
alsh
adcontinuo
usbo
nybridging
comparedwith
1/6of
grou
p1and
2/6of
grou
p2(p<0.019andp<
0.04
4,resp.)
(iii)By
quantitativeC
T,density
ofnewbo
nein
MPC
-treated
anim
alsw
as121%
high
erthan
ingrou
p2(p<0.017)
and128%
high
erthan
ingrou
p1(p<
0.00
01)
[57]
Pig
BMSC
s(10×106)
rhBM
P-2
(0.6mg)
Bioresorbable
scaffolds
made
from
medical
gradep
oly
(Σ-
caprolactone)-
20%tricalcium
phosph
ate
(mPC
L/TC
P)
9mon
ths
L2-L3and
L4-L5
Group1:mPC
L/TC
Pwith
rhBM
P-2
Group2:mPC
L/TC
Pwith
BMSC
sGr
oup3:mPC
L/TC
PGr
oup4:autograft
(i)Th
emeanradiograph
icscores
were3
.0,1.7,
1.0,and
1.8for
grou
ps1to4,respectiv
ely(ii)Th
ebon
evolum
efractionof
grou
p1w
astwofoldhigh
erthan
grou
p2
(iii)Histolog
y,𝜇-C
T,and
biom
echanicalevaluation
show
edsolid
andcomparable
fusio
nbetweengrou
ps1and
4(iv
)Group
2show
edinferio
rqu
ality
offusio
nwhencompared
with
grou
ps1and
4whilegrou
p3show
edno
fusio
neven
at9
mon
ths
[58]

Stem Cells International 17
Table3:Con
tinued.
Animal
mod
elMSC
ssou
rce
Other
biological
adjuvant
Scaffold
material
Experim
ental
time(
weeks)
Spinalfusio
nlevel
Experim
entald
esign
Mainou
tcom
eRe
ference
Ovine
Autogeno
uswho
leBM
orBM
concentrate
Non
eTC
P6mon
ths
L4-L5
Group1:autograft
Group2:TC
Pwith
BMconcentrate
Group3:TC
Pwith
who
lebo
nemarrow/
Group4:TC
P.
(i)At
6mon
ths,33%of
grou
p2
and25%of
theg
roup
1sitesw
ere
fused,comparedwith
8%of
grou
p3and0%
ofgrou
p4
(ii)H
istolog
yof
fusedsamples
show
eddenser
bone
form
ation
ingrou
p2than
ingrou
p1sites
[59]

18 Stem Cells International
Table4:Pu
blish
edclinicalstudies
involvingtheu
seof
mesenchym
alste
mcells
forspinalarthrod
esisprocedures.
Arthrod
esislevel
MSC
ssou
rce
Cell
manipulation
Treatm
ent
Patie
nt’snu
mber
(meanage)
Follo
w-up
Com
plications
Reference
Sing
lelevel=
222or
morelevels
=13
Right
poste
rosuperio
riliac
crest
Freshbo
nemarrow
(i)Leftsid
e:autologous
bone
graft
(ii)R
ight
side:mixture
ofBC
Pand
fresh
autogeno
usbo
nemarrow
35(24males,11
females)
Meanage=
59.2
Minim
um30
mon
ths
1pseud
oarthrosis
[60]
Sing
lelevel=
142levels=23
3levels=4
Rightand
left
iliac
crest
Bone
marrow
concentrate
(enrichedusinga
cellseparator)
(i)Decom
pressio
ncases:locally
harvestedbo
necombinedwith
autologous
enric
hed
MSC
s/𝛽-TCP
(ii)N
ondecompressio
ncases:
autologous
enric
hedMSC
s/𝛽-TCP
41(30men,11
wom
en)
Meanage=
44.0
Median36.5
mon
ths
(i)4patie
ntsw
ithtransie
ntexud
ationor
mod
erates
wellingin
theirw
ound
s(ii)2
pseudo
arthrosis
(iii)1p
atient
with
bursas
ynovialis
(iv)1
patie
ntwith
progressive
insta
bilityof
thea
djoined
supra-vertebra
[20]
1and
2levels
Poste
rior
iliac
crest
Bone
marrow
concentrate
(i)Side
1:concentrated
bone
marrowassociated
with
macropo
rous
biph
asiccalcium
phosph
atec
eram
icsg
raftand
autologous
bone
(ii)S
ide2
:non
concentrated
bone
marrowwith
ceramicsg
raftand
autologous
bone
15Meanage=
46.3
24mon
ths
Non
e[61]
1,2,or
3levels
One
iliac
crest
Bone
marrow
concentrated
(i)Side
1:allograft
plus
autologous
bone
marrowconcentrate
(ii)S
ide2
:autologou
siliacc
rest
bone
25(15males
and10
females)
Meanage=
45.6
24mon
ths
Non
e[62]
Not
specified
Poste
rioriliac
crests
Bone
marrow
concentrate
(i)40
patie
nts:allograft
chipsa
lone
(ii)4
0patie
nts:spon
giou
sallo
graft
chipsm
ixed
with
bone
marrow
concentrate
80(22men,58
females)
24mon
ths
Twocomplications
occurred
ineach
ofthetwo
grou
ps:hem
atom
awith
subsequent
revisio
nsurgeryand
drainage
durin
gthefi
rstw
eek
posto
perativ
ely
[63]
Not
specified
Sing
leiliac
crest
Bone
marrow
concentrate
31patie
nts:concentrated
bone
marrowaspiratewith
allograft
and
demineralized
bone
matrix
31(9
men
and22
females)
Meanage:71.5
Atleast12
mon
ths
(i)One
seroma
(ii)O
nepseudarthrosis
(iii)Th
reer
eoperatio
nfor3
patie
nts
fora
djacentsegmentp
atho
logy
[64]
1or2
levels
Non
applicable
Allo
graft
cellu
lar
bone
matrix
containing
nativ
emesenchym
alste
mcells
and
osteop
rogenitor
cells
182patie
nts:allograft
cellu
larb
one
matrix
containing
nativ
emesenchym
alste
mcells
and
osteop
rogenitorc
ells
182
(49%
female,
51%male)
Meanage:51
24mon
ths
(i)1d
urotom
y(ii)2
wou
ndinfections
(iii)2incidences
ofnew
radiculopathy
(iv)1
incidenceo
fhypotensio
n(v)1
incidenceo
fhypertension
(vi)2incidences
ofpo
stoperativ
esoft-tissues
wellin
g
[65]

Stem Cells International 19
Table5:Listof
clinicaltria
lsinvolvingmesenchym
alste
mcells
forspinalarthrod
esisprocedures
(from
clinicaltrials.gov).
ClinicalTrials.gov
Identifi
erCon
ditio
nStud
ytype
Estim
ated
enrollm
ent/
enrolledpatie
nts
MSC
data
(sou
rce,manipulation,
orstr
ategy)
Num
bero
fcells
Stud
yarms
Follo
w-up
(mon
ths)
Activ
ity
NCT
01552707
Degenerative
spon
dylolisthesis
grades
I-II
Interventio
nal
phases1-2
62
Expand
edautologous
mesenchym
alste
mcells
obtained
underG
MPcond
ition
sfixedin
allogenicb
onetissue
Not
repo
rted
(i)Group
1:instr
umented
spinalfusio
nandthetissue
engineeringprod
uct
compo
sedby
“exvivo”
expand
edautologous
mesenchym
alste
mcells
fixed
inallogenicb
one
tissueinspinalfusio
n(ii)G
roup
2:sta
ndard
treatmento
finstrum
ented
spinalfusio
nandpatie
nt's
bone
iliac
crest
12mon
ths
Recruitin
g
NCT
00549913
Poste
rolateral
lumbarfusion
Interventio
nal
phases1-2
42
Immun
osele
cted,
cultu
re-expanded,nu
cleated,
allogeneicmesenchym
alprogenito
rcells
Not
repo
rted
(i)Ex
perim
entalgroup
1:lowestd
oseo
fNeoFu
se(ii)E
xperim
entalgroup
2:middled
oseo
fNeoFu
se(iii)Ex
perim
entalgroup
3:high
estd
oseo
fNeoFu
se(M
PCs)
(iv)C
ontro
lgroup
:autologous
bone
graft
24and36
mon
ths
Com
pleted
NCT
01513694
Intervertebraldisc
disease
Interventio
nal
phases1-2
15
Cellsuspensionof
MSC
sfrom
bone
marrowaspirateexpand
edin
vitro
inas
pecific
medium
enric
hedwith
plateletlysate
with
outadd
ition
ofanim
alprod
ucts
Not
repo
rted
(i)Au
tologous
mesenchym
alste
mcells
arrang
edin
apho
sphate
ceramic
Not
repo
rted
Unk
nown
NCT
01603836
Spon
dyloarthrosis
,spon
dylosis
Interventio
nal
80Spon
giou
sallo
graft
chipsm
ixed
with
bone
marrowconcentrate
74×104/L
ataverage(range,
1.06–
1.98×
104/L)
(i)Group
1:spon
giou
sallograft
chipsa
lone
(ii)G
roup
2:spon
giou
sallograft
chipsm
ixed
with
bone
marrowconcentrate
24mon
ths
Com
pleted

20 Stem Cells International
Articles located through learning-basedapproach
PubMed, n = 129 Web of Science, n = 210 Scopus, n = 105
Potentially relevant articles identified andtitle/abstract screened (n = 450)
Articles excluded (n = 301):(i) Noninherent and/or on other spinal pathology (i.e., spinal cord injury,
intervertebral disc regeneration, nucleus pulposus, spina bifida) (n = 213)(ii) Non-English article (n = 4)
(iii) In vitro studies (n = 10)(iv) Nonoriginal articles, reviews (n = 62)(v) Only abstract with data unabstractable (n = 10)
(vi) Withdrawn and noninherent clinical trials (n = 2)
Results sent to “Mendeley” to delete duplicatearticles (n = 60)
Potentially relevant articles for the review(n = 149)
Articles excluded on basis of full text (n = 10):(i) Case report (n = 1)
(ii) Noninherent in vivo studies (n = 7)(iii) Withdrawn clinical trials (n = 1)(iv) Noninherent clinical trial (n = 1)
Relevant articles identified on basis of full text(n = 50)
In vivo studies (n = 39) Clinical studies (n = 7)
Articles obtained from other sources:https://www.clinicaltrials.gov (n = 6)
Clinical trials (n = 4)
Figure 1: Systematic literature review flow diagram. Flow of information through the different phases of the systematic review.
papers according to in vivo studies (small, medium, and largeanimal models) and clinical trials.
4.1. In Vivo Studies
4.1.1. Small Animal Models. Thirteen studies (Table 1)employed MSCs in small animal models (𝑛 = 1 in mice and𝑛 = 12 in rats) in order to achieve or improve spinal fusionrate. In the majority of the studies the spinal fusion surgery
was carried out by decortications of L4 and L5 but also L1-L2 [25] and L4–L6 [28] transverse processes. Klıma et al.[30] used titaniummicroplates and titanium screws to fix thespinous processes of L1–L3 vertebrae. The experimental timeafter surgery ranges from 4 to 8 weeks. Most of the studiesused in vitro expanded MSCs [22, 25–27, 29–34] principallyderived from bone marrow [25–27, 29, 30, 33, 34] but alsofrom adipose tissue [22, 31–33]. Beyond the use of expandedMSCs, some authors, in order to take advantage not only

Stem Cells International 21
Publications
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
Years
0123456789
Num
ber o
f in
vivo
stud
ies
(a)
2006
2008
2010
2012
2014
2016
2015
2013
2011
2009
2007
YearsPublications
0123456789
Num
ber o
f clin
ical
stud
ies
(b)
Figure 2: Historical distribution of (a) in vivo models and (b) clinical studies on MSCs use in spinal arthrodesis procedures according to theyear of publication.
Stem cell isolation
Bone marrow in toto
MarrowSpongy bone
Adipocyte
Erythrocyte
Normoblast
MyeloplaxMyelocyte
Myelocyte
Myelocyte
Normoblast withdividing nucleus
Bone marrow
Eosinophil Spinal arthrodesissurgery
Adipose tissue
Adipose derived MSCs ✓Expanded✓Differentiated in osteogenic medium
Combination ortotoinmarrowboneofMSCs derived from bone marrow or
adipose tissue with a scaffold
✓Expanded (differentiated and undifferentiated)✓Transfected✓Codelivered with growth factor or osteogenic protein
Alizarin red staining
ALP staining+
Figure 3: Flow chart summarizing the main steps of spinal fusion procedure when stem cell therapy is used.
by the mesenchymal component but also by the presence oftrophic factors, cytokines, and extracellular matrix molecule,used bone marrow in toto [23, 24, 28]. Few studies usedautologous MSCs [23, 29, 34] while the majority employedallogenic MSCs [22, 24–26, 30–33]. All the examined studiesinvolved seeding cells into allograft [22, 27, 32] or into variousscaffolds, such as ceramic [25, 30, 34], collagen sponge [24, 28,31, 33], silk fibroin [26], and composites [23, 29]. Only oneauthor employed autologous bone graft as control material[26] while the others used allografts or scaffolds withoutMSCs as control. When expanded MSCs were used the cellnumber, loaded on allografts or scaffolds, is 1.0–1.50× 106 [26,29, 32–34] but also lower concentration as in the study of Leeet al. (0.25 × 106) [22] or higher concentration was used [23,26, 30, 31]. Differently from the studies where bonemarrow intoto [23, 24, 28] and undifferentiatedMSCswere cultured andloaded on a scaffold [25, 26, 30, 32–34] four studies [22, 29,
31, 34] employed cells cultured in osteogenic differentiationmedium. In particular, Rao et al. examined also the role of lowdoses bone morphogenic protein- (BMP-) 2 codelivered withboth undifferentiated and differentiated BMSCs showing thatundifferentiated BMSCs with low-dose BMP-2 loaded ona composite scaffold demonstrated superior fusion rate incomparison to all the other examined groups. Low dose ofBMP-2 was also evaluated in association with bone marrowin toto loaded on a collagen sponge, showing that freshbone marrow aspirate increases the osteogenic potency andbiologic efficiency of BMP-2 [24, 28] also in comparison toBMP-2 associated with other adjuvant factors such as plateletrich plasma [28]. BMP-2was used also byMiyazaki et al. in anathymic rat model to compare the efficacy of human ADSCsand BMSCs transduced with an adenovirus containing thecDNA for BMP-2 loaded on collagen sponge.Authors showedthat ADSCs transfected with adeno-BMP-2 induce abundant

22 Stem Cells International
bone formation in a manner similar to genetically modifiedBMSCs [33]. Similar results were also obtained by Hsu et al.[31] that demonstrate the potential of adipose derived stemcell as cellular vehicle for this osteoinductive factor. Contraryto the positive effect on spinal fusion derived by the associa-tion of MSCs or bone marrow with BMP-2, the associationof fibroblast growth factor-4 (FGF-4) with differentiatedBMSCs loaded on a HA scaffold did not stimulate fusionbut appears to induce fibrotic change rather than differen-tiation to bone [34]. Despite these negative results, recentlyShih et al. [23] suggested a good performance in promotingspinal fusion rate associating new biomineralized matriceswith bone marrow or basic FGF. Differently from the above-mentioned studies that used growth factors in associa-tion with BMSCs to enhance spinal fusion, other authorsdetermined the efficacy of a 𝛽-tricalcium phosphate (TCP)/demineralized bone matrix (DBM) [22] or DBM alone [32]loaded with different doses of human perivascular stem cells(hPSCs) also in presence and absence of osteogenic proteinNELL-1. Authors highlighted that both in healthy [32] and inosteoporotic condition [22] the presence of hPSCs [32] also inassociation with NELL-1 significantly improved spinal fusion[22]. Differently from all the other studies, Klıma et al. [30]adopted an instrumentedmodel of interspinous fusion show-ing a nonsignificant new bone formation in animals treatedwith hydroxyapatite (HA) and BMSCs in comparison to ani-mals treatedwith scaffold alone, even if in presence of BMSCsauthors describedminor inflammatory reaction compared tothe animals treated without BMSCs. Finally, since the fateand contribution of the MSCs are not sufficiently clarified,especially at clinically relevant locations, Geuze et al. [25]using the bioluminescence imaging of luciferase-markedMSCs and adopting different experimental setup tried toelucidate and clarify the contributionmade not only byMSCsitself on spinal fusion but also by the paracrine effect ofMSCswhen loaded on a ceramic scaffold. Results suggested that thesoluble factors or the presence of extracellular matrix was notsufficient to induce bone formation; thus unfortunately theydid not provide an answer to the critical question whetherthe principal mechanism of action of MSCs is based on theiractivity on the release of soluble mediators.
4.1.2. Medium Animal Model. MSCs treatment to achievespinal fusion was employed in 16 in vivo studies that usedmedium sized animal models (Table 2). All the studies useda single level posterolateral transverse process arthrodesisbetween L4-L5 or L5-L6 or L6-L7. With the exception of onestudy [44] spinal fusion surgery was carried out by creatinga defect between L4 and L5 (depth of 5mm and diameter of10mm); in all the others studies a transverse process decor-tication was performed. The experimental time after surgeryranges from 4 up to 18 weeks. Unless for the study by Kogaet al. [36] that use fresh bone marrow to enhance the spinalfusion rate all the other authors used expanded, autologous[2, 35, 37–40, 42–47, 49], or allogeneic [41, 48] MSCs isolatedfrom bonemarrow [2, 35, 37, 38, 41–49] or adipose tissue [40]at different dosages (from 1.0 × 106 cells to 1.0 × 108). Someauthors used MSCs with osteogenic differentiation [35, 37–40, 42, 44–47, 49] to increase the fusion rate while other
used undifferentiated MSCs [2, 36, 41, 43, 48]. In all thestudies MSCs were loaded on a scaffold (i.e., ceramic,polymeric, collagen sponge, and gelatin sponge) with theexception of Urrutia et al. [38] that used a pellet of culturedBMSCs cografted with an autologous bone graft and showedthat adding differentiated BMSCs in a pellet without ascaffold not only failed to increase fusion rate, but completelyinhibited bony growth. Differently, Nakajima et al. [35], usingdifferentiated BMSCs plusHA, obtained a high rate of lumbarfusion similar to that obtained using autograft alone. In mostof the studies the experimental treatment with MSCs wascompared with autologous bone but in some of them thiscomparison is missing [2, 41–43, 45, 47, 48]. Niu et al. [42]compared BMSCs cultured in a biphasic calcium phosphatewith BMSCs cultured with coralline HA. Coralline HA wasused also by Chen et al. [49] who used MSCs fluorescentlabeledwith PKH-67 dye in combinationwith a bioresorbablehydrogel and coralline HA in comparison to autograft show-ing similar results between groups. In addition, to the use of aceramic graft in associationwithBMSCs, several authors usedBMP to enhance the osteogenic potency of MSCs [37, 43, 46]showing that MSCs in combination with BMP-2 enhancedbone formation in posterolateral spine fusion exerting amore osteoinductive action than MSCs alone [46]. Favorableresults were also obtained comparing the association of acomposite [43] and a ceramic [48] material with baculovirusgenetically modified BMSCs overexpressing BMP-7 [43] orBMP-2 associated vascular endothelial growth factor (VEGF)[48] with nongenetically modified BMSCs. Additionally,Minamide et al. [37] tested also the hypothesis that bothBMP-2 and basic fibroblast growth factor (FGF) mutuallyacted on the proliferation and osteogenic differentiation ofrabbit BMSCs. They showed that the combined treatmentwith BMP-2 and basic FGF produced a favorable degree ofspinal fusion comparable to autograft. An increased spinalfusion rate was also obtained by Koga et al. [36] assessingthe osteogenic potential of HA sticks soaked with freshbone marrow and fibronectin (FN). Interesting were also theresults obtained byHui et al. [2] that underlined that the com-bination of synthetic biomaterials, autologous differentiatedBMSCs, and also low-intensity pulsed ultrasound promotespinal fusion. Differently from the use of low-intensity pulsedultrasound, the use of hyperbaric oxygen therapy adminis-trated to the animals did not enhance the spinal fusion ratewhen a combination of allogenic differentiate MSCs/alginatescaffold was evaluated [47]. The effectiveness of autologousdifferentiated BMSCs was evaluated also by Yang et al. [44]in association with a collagen sponge showing a high fusionrate similar to autologous bone. Another approach exploitedby Douglas et al. is the ex vivo transfer of a gene encodingan osteoinductive factor to BMSCs which are subsequentlyreimplanted into the host. In this study Smad1C gene wastransferred into rabbitMSCs isolated from bonemarrow.Therationale for the use of this approach is to control more effi-ciently bone formationmimicking the natural cascade signalsand avoiding the drawbacks associated with the direct useof BMPs. Authors showed that animals BMSCs transducedex vivo with the Smad1C-expressing tropism-modified Ad5vector mediated a greater amount of new bone formation

Stem Cells International 23
than BMSCs transduced with any other vector [45]. Differ-ently from all the other studies Urrutia et al. [38] evaluating acomposite of hot compression-molded PLGA, HA, and type Icollagen as anBMSCs carrier for a posterolateral spinal fusionused also a PKHfluorescence labeling system and highlightedthat the transplanted BMSCs were partly responsible for thenew bone formation. Positive results were also obtained usingallogeneic undifferentiated rabbit BMSCs added to a type Icollagen and calciumphosphate ceramics that promote spinalfusion and did not induce an adverse immune response [41].Only one study evaluated the effectiveness of autologousADSCs combined with a new mineralized collagen matrix(nHAC–PLA) for posterolateral spinal fusion. Results indi-cated that the rate of fusion was significantly higher in theautologous bone and ADSCs + nHAC-PLA groups thanthat in the nHAC-PLA and autologous bone + nHAC-PLAgroups, demonstrating the effective impact of the scaffold alsowhen combined with ADSCs [40].
4.1.3. Large Animal Models. Ten studies used ovine as largeanimal models (Table 3) [51–57, 59] while two used swine[50, 58].These studies carried out four-level, three-level, two-level, or single level spinal fusions surgery all instrumentedwith screws and bars with the exception of Gupta et al. thatused a single level noninstrumented lumbar fusion [59]. Inthese studies both autologous bone marrow or expandedMSCs [50, 51, 54, 55, 58] and allogeneic bone marrow ormesenchymal precursor cells [52, 53, 56, 57, 59] were used toenhance spinal fusion and all of them involved seeding cellsinto allografts [50], collagen scaffolds [55], ceramics [51–54,56, 57, 59], and composites [58] scaffolds. Except for Schubertet al. who use MSCs derived from adipose tissue [50] andGoldschlager et al. that used amnion epithelial cells [57] allthe other authors used differentiatedMSCs andmesenchymalprecursor cells derived from bone marrow but also bonemarrow in toto loaded on the scaffolds at different dosages.Wheeler et al. also compared different dosages of MSCs [52,53, 56]. All the researchers used autografts and grafts withoutcells as controls and the majority highlighted superior resultof the graft associated with MSCs and bone marrow incomparison to the graft alone, while similar [50] or best [51–53, 55, 56, 59] results were seen for autografts in comparisonto grafts associated with MSCs. In addition, Goldschlager etal. showed superior results of mesenchymal precursor cellsloaded onMastergraftmaterial also in comparison to amnionepithelial cells [57]. Differently from the above-mentionedstudies, Cuenca-Lopez et al. observed that bone autograftsperformed better than MSCs loaded on hybrid constructs[54]. Inferior results were also observed for MSCs loaded ona composite scaffold in comparison to autograft but also incomparison to scaffold associated with BMP-2 [58].
4.2. Clinical Studies. The search strategy identified 10 clinicalstudies (Table 4) about MSCs used for spinal fusion proce-dures. Among these 10 articles, three were excluded: for twoarticles we found only the abstract and not the full-text andthe other one was a case report of an 88-year-old multi-diseased osteoporotic patient treated with corticocancellous
bone allograft, augmented with autologous bone marrowconcentrate from iliac crest aspirate enriched with plateletrich fibrin from peripheral blood. Thus, due to the treatmentprotocol and the lack of a control group, the real contribu-tion of MSCs on spinal fusion procedure could not be extra-polated.Therefore, 7 articles were analyzed: by comparing thecharacteristics of each study, it is evident that, in all studies,with the exception of the study by Moro-Barrero et al. [60],the authors employed the concentrate autologous bone mar-row in comparison to fresh one inside the operating theater[20, 61–65]. Three studies associated bone marrow with aceramic graft [20, 60, 61] while the remaining 4 combinedbone marrow with allograft [62–65]. Three studies wereprospective, randomized trials [61–63], two of which withlimited number of patients [61, 62], while one was a prospec-tive, multicenter, nonrandomized study on 182 patients [65].All the studies withdrew the bonemarrow from iliac crest andperformed spinal fusion surgery on 1, 2, or 3 levels with simi-lar surgical procedures and approaches. As far as the numberof transplanted cells, cell concentration was not alwaysreported as cell number in one milliliter or was not reportedat all, thus making comparison among studies extremelydifficult. In addition, another variable among studies is themethod used for cell concentration (cell separator based onthe density gradient centrifugation, centrifugation over a gra-dient, orwithout any gradient).Obviously, the absence of pro-cedural and methodological guidelines affected the cell yieldand thus it was not possible to identify a range for the cellsnumber to be transplanted and to correlate it with the clinicaloutcome. In addition to the cells number, in two studies a con-trol groupwas not used [64, 65], while other two studies com-pared the experimental treatment with autologous bone [60,62] and one study with allograft chips alone [63]. Anotherstudy by Gan et al. compared autologous enriched MSCs/𝛽-TCP with locally harvested bone combined with autologousenriched MSCs/𝛽-TCP [20], while Odri et al. in a simpleblind randomized clinical, prospective, monocentric studycompared a biphasic calcium phosphate ceramics graft thatwas associated with autologous bone and concentrated bonemarrow with unconcentrated bone marrow with ceramicsgraft and autologous bone [61].The follow-up of the analyzedstudies ranged from 12 months to 36.5 months [20, 60–65],demonstrating, through radiographic and clinical analyses,the safety and in one case a greater efficacy [63] of MSCsuse in spinal fusion; however, these studies were conductedin too small patient cohorts and there is the need to con-firm these data also from preclinical animal models, wheretransplanted cell phenotype, fate, and contribution to healingcould be monitored and quantitatively measured to excludemalignant transformation.
As of August 2016, the ongoing clinical trials onMSCs forspinal fusion applications found through https://www.clin-icaltrials.gov web site are 6 (Table 5). One of them wasexcluded because the objective of the trial was the definitionof the osteogenic potential of MSCs and their progenitorsduring spinal fusion complication (pseudarthrosis). Anothertrial has not been analyzed because it has been withdrawnprior to the patients enrollment. The remaining 4 trials were

24 Stem Cells International
all interventional study of phase I-II with a minimum follow-up of 12 months. Of them 2 were completed. In detail thetrials assessed (1) the feasibility and safety of ex vivo expandedautologous MSCs fixed in allogenic bone tissue in compar-ison to autologous bone; (2) the effectiveness of autologousmesenchymal stem cells arranged in a calcium phosphateceramic; (3) the effectiveness of allograft alone versus allograftwith bone marrow concentrate; (4) the feasibility, safety, andtolerability of 3 different doses of immunoselected, culture-expanded, nucleated, allogenic mesenchymal precursor cellscombined with resorbable ceramic granules in comparisonto autograft alone. In all studies fusion surgery, surgicalprocedures, clinical approaches, and follow-up evaluationswere similar. However, each trial was different from the otherfor patients number, MSCs manipulation or strategy, studyarms, and presence and/or type of control group. In addition,the information available was not always complete. In somecases it was not clear which strategy would be employed forMSCmanipulation and almost all the studies did not indicatethe number of cells or the medium for cell infusion. Thus,although some studies could provide useful information, itwas evident that more controlled clinical trials are necessaryto understand whether MSCs can be successfully employedin spinal fusion procedures.
5. Conclusion and Future Prospective
In recent years, the basic and preclinical research literatureclearly indicates the use of MSCs also in combination withvarious scaffolds, to repair bone defects, and many stud-ies concern their use also for the treatment of vertebralinstability. Thus, with the rapidly growing number of spinefusion surgeries performed annually, we have seen the needfor performing this descriptive systematic literature reviewon MSCs use in spinal arthrodesis procedures in order toelucidate if the use of MSCs may really represent a validstrategy able to facilitate and accelerate spinal fusion.
In this review, several therapeutic strategies for theenhancement of spinal fusion rate based on stem cells havebeen developed in both preclinical and clinical studies. Theapplication of an allograft or a scaffold, prevalently ceramics,associated with stem cells was adopted in all preclinicalstudies while the application of autograft, but also ceramicscaffolds, still in association with stem cell was used inthe clinical setting (tissue engineering strategy). However,the use of growth factors (principally BMP-2) and otherosteoinductive factors, as well as ex vivo gene therapy, wastaken into consideration.
We found that numerous preliminary researches in thisreview were carried out in small, medium, and large animalmodels showing the potential for MSCs use in spinal fusionprocedures. Despite the fact that in some of these studiesadipose derivedmesenchymal stem cells, human perivascularstem cells, and also amnion epithelial cells were used, themajority of the studies employed bone marrow cells. Basedon these preclinical data it would seem that MSCs are ableto perform the necessary physiological functions to achieve,facilitate, and accelerate spinal fusion.However, none of theseexamined studies was able to give a detailed elucidation about
the fate ofMSCswhen theywere added to a scaffold, althoughthe success demonstrated that, in the animal models, somebarriers remain prior to this therapy translation into the clin-ical setting. In fact, this review underlines that there are fewand basic clinical trials, although some of them have shownthat bone marrow cells used in humans can give a successfulspine fusion. Some critical existing limitations include alsothe choice of the optimal cell concentration, the deliverymethod, the ideal manipulation procedure (ex vivo expan-sion and one-step procedure), and the best implantationtechniques. In addition, researches that examine the optimalMSCs concentration are needed in large animal model,which are more similar to humans. These critical pointsalso highlight the need for methods able to maximize thenumber ofMSCs collected, as well as the presence of easy andfeasible techniques in the clinical scenario. However, othermatters that need further consideration comprise also theelimination of fetal calf serum, the possible reversibility ofthe differentiated state, the survival of the cells in vivo, theintegration with the preexisting bone, and the capacity toform bone and marrow in vivo.
In conclusion, the use of MSCs as a cell-based therapymay represent a biological approach to reduce the high costof osteoinductive factors as well as the high dose needed toinduce bone formation. Thus, implementing this availablepotential treatment based onMSCs use and probablymitigat-ing some adverse effects would make this kind of approacha possible therapeutic tool. Finally, although MSCs ther-apy remains an interesting and important opportunity ofresearch, it is necessary that the spine surgery communitycarefully evaluates the safety and efficacy ofMSCs use in spinefusion through randomized controlled and blinded clinicaltrials.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgments
This work was supported by grants from Rizzoli OrthopedicInstitute (Ricerca Corrente), 5 × 1000 2013 Project “Sviluppoe Validazione di Modelli Alternativi e Complementari InVitro (Intelligent Testing Strategy) in Ortopedia e Trau-matologia,” Fondazione del Monte di Bologna e Ravenna2016 Project “Cellule Mesenchimali Staminali Autologhe daCorpo Vertebrale come Prospettiva Biologica Innovativa perla Chirurgia Vertebrale,” and the Operational ProgrammeERDF 2007–2013 in the region Emilia-Romagna: Activity 1.1“Creation of Technology Centers for Industrial Research andTechnological Transfer.”
References
[1] G. F.Muschler, H. Nitto, Y.Matsukura et al., “Spine fusion usingcell matrix composites enriched in bone marrow-derived cells,”Clinical Orthopaedics and Related Research, no. 407, pp. 102–118,2003.

Stem Cells International 25
[2] C. F. F.Hui, C.W.Chan,H. Y. Yeung et al., “Low-intensity pulsedultrasound enhances posterior spinal fusion implanted withmesenchymal stem cells-calcium phosphate composite withoutbone grafting,” Spine, vol. 36, no. 13, pp. 1010–1016, 2011.
[3] R. D. Rao, V. Bagaria, K. Gourab, S. T. Haworth, V. B. Shidham,andB.C. Cooley, “Autograft containment in posterolateral spinefusion,” Spine Journal, vol. 8, no. 4, pp. 563–569, 2008.
[4] S.A.Malik,M.Murphy, P.Connolly, and J.O’Byrne, “Evaluationof morbidity, mortality and outcome following cervical spineinjuries in elderly patients,” European Spine Journal, vol. 17, no.4, pp. 585–591, 2008.
[5] M. Fini, F. Salamanna, F. Veronesi et al., “Role of obesity, alcoholand smoking on bone health,” Frontiers in Bioscience (EliteEdition), vol. 4, pp. 2686–2706, 2012.
[6] M. V. Risbud, I. M. Shapiro, A. Guttapalli et al., “Osteogenicpotential of adult human stem cells of the lumbar vertebral bodyand the iliac crest,” Spine, vol. 31, no. 1, pp. 83–89, 2006.
[7] J. Picchi, L. Trombi, L. Spugnesi et al., “HOX and TALE signa-tures specify human stromal stem cell populations from differ-ent sources,” Journal of Cellular Physiology, vol. 228, no. 4, pp.879–889, 2013.
[8] G. B. Brodano, S. Terzi, L. Trombi et al., “Mesenchymal stemcells derived from vertebrae (vMSCs) show best biological pro-perties,” European Spine Journal, vol. 22, supplement 6, pp.S979–S984, 2013.
[9] M. Manfrini, G. Barbanti-Brodano, E. Mazzoni et al., “Micro-RNA regulatory networks are involved in osteogenic differen-tiation of human mesenchymal stem cells from bone marrow,”European Journal of Histochemistry, vol. 57, supplement 1, p. 7,2013.
[10] M. F. Pittenger, A. M. Mackay, S. C. Beck et al., “Multilineagepotential of adult human mesenchymal stem cells,” Science, vol.284, no. 5411, pp. 143–147, 1999.
[11] Y. Jiang, B. Vaessen, T. Lenvik, M. Blackstad, M. Reyes, andC. M. Verfaillie, “Multipotent progenitor cells can be isolatedfrom postnatal murine bone marrow, muscle, and brain,”Experimental Hematology, vol. 30, no. 8, pp. 896–904, 2002.
[12] C. Morelli, G. Barbanti-Brodano, A. Ciannilli, K. Campioni, S.Boriani, andM.Tognon, “Cellmorphology,markers, spreading,and proliferation on orthopaedic biomaterials. An innovativecellular model for the ‘in vitro’ study,” Journal of BiomedicalMaterials Research Part A, vol. 83, no. 1, pp. 178–183, 2007.
[13] M. Manfrini, M. Fiorini, G. Barbanti-Brodano, D. Pressato, andM. Tognon, “New generation of orthopaedic mimetic bioce-ramics assayed with humanmesenchymal stem cells,” EuropeanMusculoskeletal Review, vol. 6, no. 2, pp. 96–99, 2011.
[14] M. Manfrini, C. Di Bona, A. Canella et al., “Mesenchymal stemcells from patients to assay bone graft substitutes,” Journal ofCellular Physiology, vol. 228, no. 6, pp. 1229–1237, 2013.
[15] G. B. Brodano, E. Mazzoni, M. Tognon, C. Griffoni, and M.Manfrini, “Human mesenchymal stem cells and biomaterialsinteraction: a promising synergy to improve spine fusion,”European Spine Journal, vol. 21, supplement 1, pp. S3–S9, 2012.
[16] X. Liu, Q. Feng, A. Bachhuka, andK. Vasilev, “Surfacemodifica-tion by allylamine plasma polymerization promotes osteogenicdifferentiation of human adipose-derived stem cells,” ACSApplied Materials and Interfaces, vol. 6, no. 12, pp. 9733–9741,2014.
[17] A. F. Steinert, L. Rackwitz, F. Gilbert, U. Noth, and R. S. Tuan,“Concise review: the clinical application of mesenchymal stem
cells for musculoskeletal regeneration: current status and per-spectives,” Stem Cells Translational Medicine, vol. 1, no. 3, pp.237–247, 2012.
[18] F. Veronesi, F. Salamanna, M. Tschon, M. Maglio, N. N. Aldini,and M. Fini, “Mesenchymal stem cells for tendon healing: whatis on the horizon?” Journal of Tissue Engineering and Regenera-tive Medicine, 2016.
[19] D. Logeart-Avramoglou, F. Anagnostou, R. Bizios, andH. Petite,“Engineering bone: challenges andobstacles,” Journal of Cellularand Molecular Medicine, vol. 9, no. 1, pp. 72–84, 2005.
[20] Y. Gan, K. Dai, P. Zhang, T. Tang, Z. Zhu, and J. Lu, “The clini-cal use of enriched bone marrow stem cells combined withporous beta-tricalcium phosphate in posterior spinal fusion,”Biomaterials, vol. 29, no. 29, pp. 3973–3982, 2008.
[21] K. K. Hansraj, “Stem cells in spine surgery,” Surgical TechnologyInternational, 2016.
[22] S. Lee, X. Zhang, J. Shen et al., “Brief report: human perivascularstem cells and Nel-like protein-1 synergistically enhance spinalfusion in osteoporotic rats,” Stem Cells, vol. 33, no. 10, pp. 3158–3163, 2015.
[23] Y.-R. Shih, A. Phadke, T. Yamaguchi et al., “Synthetic bonemimeticmatrix-mediated in situ bone tissue formation throughhost cell recruitment,” Acta Biomaterialia, vol. 19, pp. 1–9, 2015.
[24] H. W. Bae, L. Zhao, L. E. A. Kanim, P. Wong, D. Marshall, andR. B. Delamarter, “Bone marrow enhances the performance ofrhBMP-2 in spinal fusion: a rodent model,”The Journal of Bone& Joint Surgery—American Volume, vol. 95, no. 4, pp. 338–347,2013.
[25] R. E. Geuze, H.-J. Prins, F. C. Oner et al., “Luciferase labeling formultipotent stromal cell tracking in spinal fusion versus ectopicbone tissue engineering in mice and rats,” Tissue Engineering A,vol. 16, no. 11, pp. 3343–3351, 2010.
[26] Y. Gu, L. Chen, H.-Y. Niu, X.-F. Shen, and H.-L. Yang, “Promot-ing spinal fusions by biomineralized silk fibroin films seededwith bone marrow stromal cells: an in vivo animal study,”Journal of Biomaterials Applications, vol. 30, no. 8, pp. 1251–1260,2016.
[27] T. Hayashi, E. L. Lord, A. Suzuki et al., “A comparison ofcommercially available demineralized bone matrices with andwithout human mesenchymal stem cells in a rodent spinalfusion model,” Journal of Neurosurgery: Spine, vol. 25, no. 1, pp.133–137, 2016.
[28] R. D. Rao, K. Gourab, V. B. Bagaria, V. B. Shidham, U. Metkar,and B. C. Cooley, “The effect of platelet-rich plasma and bonemarrow on murine posterolateral lumbar spine arthrodesiswith bone morphogenetic protein,”The Journal of Bone & JointSurgery—American Volume, vol. 91, no. 5, pp. 1199–1206, 2009.
[29] T. Hu, S. A. Abbah, S. Y. Toh et al., “Bone marrow-derivedmesenchymal stem cells assembled with low-dose BMP-2 ina three-dimensional hybrid construct enhances posterolateralspinal fusion in syngeneic rats,” Spine Journal, vol. 15, no. 12, pp.2552–2563, 2015.
[30] K. Klıma, V. Vanecek, A. Kohout et al., “Stem cells regenera-tive properties on new rat spinal fusion model,” PhysiologicalResearch, vol. 64, no. 1, pp. 119–128, 2015.
[31] W. K. Hsu, J. C. Wang, N. Q. Liu et al., “Stem cells from humanfat as cellular delivery vehicles in an athymic rat posterolateralspine fusion model,” The Journal of Bone & Joint Surgery—American Volume, vol. 90, no. 5, pp. 1043–1052, 2008.
[32] C. G. Chung, A. W. James, G. Asatrian et al., “Human perivas-cular stem cell-based bone graft substitute induces rat spinal

26 Stem Cells International
fusion,” Stem Cells Translational Medicine, vol. 3, no. 10, pp.1231–1241, 2014.
[33] M. Miyazaki, P. A. Zuk, J. Zou et al., “Comparison of humanmesenchymal stem cells derived from adipose tissue and bonemarrow for ex vivo gene therapy in rat spinal fusion model,”Spine, vol. 33, no. 8, pp. 863–869, 2008.
[34] H. S. Seo, J. K. Jung, M. H. Lim, D. K. Hyun, N. S. Oh, and S. H.Yoon, “Evaluation of spinal fusion using bone marrow derivedmesenchymal stem cells with or without fibroblast growthfactor-4,” Journal of Korean Neurosurgical Society, vol. 46, no.4, pp. 397–402, 2009.
[35] T. Nakajima, H. Iizuka, S. Tsutsumi, M. Kayakabe, and K.Takagishi, “Evaluation of posterolateral spinal fusion usingmesenchymal stem cells: differences with or without osteogenicdifferentiation,” Spine, vol. 32, no. 22, pp. 2432–2436, 2007.
[36] A. Koga, Y. Tokuhashi, A. Ohkawa, T. Nishimura, K. Takayama,and J. Ryu, “Effects of fibronectin on osteoinductive capability offresh iliac bone marrow aspirate in posterolateral spinal fusionin rabbits,” Spine, vol. 33, no. 12, pp. 1318–1323, 2008.
[37] A. Minamide, M. Yoshida, M. Kawakami et al., “The effects ofbone morphogenetic protein and basic fibroblast growth factoron culturedmesenchymal stem cells for spine fusion,” Spine, vol.32, no. 10, pp. 1067–1071, 2007.
[38] J. Urrutia, P. Mery, R. Martınez, F. Pizarro, D. Apablaza, andR. Mardones, “Cultured autologous bone marrow stem cellsinhibit bony fusion in a rabbit model of posterolateral lumbarfusion with autologous bone graft,” Journal of Clinical Neuro-science, vol. 17, no. 4, pp. 481–485, 2010.
[39] J.-W. Huang, S.-S. Lin, L.-H. Chen et al., “The use offluorescence-labeled mesenchymal stem cells in poly(lactide-co-glycolide)/hydroxyapatite/collagen hybrid graft as a bonesubstitute for posterolateral spinal fusion,” Journal of Trauma—Injury, Infection and Critical Care, vol. 70, no. 6, pp. 1495–1502,2011.
[40] Z.-B. Tang, J.-K. Cao, N.Wen et al., “Posterolateral spinal fusionwith nano-hydroxyapatite-collagen/PLA composite and auto-logous adipose-derived mesenchymal stem cells in a rabbitmodel,” Journal of Tissue Engineering and Regenerative Medi-cine, vol. 6, no. 4, pp. 325–336, 2012.
[41] T.-H. Lee, Y.-H. Huang, N.-K. Chang et al., “Characterizationand spinal fusion effect of rabbit mesenchymal stem cells,” BMCResearch Notes, vol. 6, article 528, 2013.
[42] C.-C. Niu, S.-S. Lin, W.-J. Chen et al., “Benefits of biphasic cal-cium phosphate hybrid scaffold-driven osteogenic differentia-tion of mesenchymal stem cells through upregulated lep-tin receptor expression,” Journal of Orthopaedic Surgery andResearch, vol. 10, article 111, 2015.
[43] J.-C. Liao, “Cell therapy using bone marrow-derived stem celloverexpressing BMP-7 for degenerative discs in a rat tail discmodel,” International Journal of Molecular Sciences, vol. 17, no.2, article 147, 2016.
[44] W. Yang, Y. Dong, Y. Hong, Q. Guang, and X. Chen, “Evaluationof anterior vertebral interbody fusion using osteogenic mes-enchymal stem cells transplanted in collagen sponge,” Journalof Spinal Disorders and Techniques, 2012.
[45] J. T. Douglas, A. A. Rivera, G. R. Lyons et al., “Ex vivo transferof the Hoxc-8-interacting domain of Smad1 by a tropism-modified adenoviral vector results in efficient bone formationin a rabbit model of spinal fusion,” Journal of Spinal Disorders &Techniques, vol. 23, no. 1, pp. 63–73, 2010.
[46] T.-S. Fu, W.-J. Chen, L.-H. Chen, S.-S. Lin, S.-J. Liu, and S. W.N. Ueng, “Enhancement of posterolateral lumbar spine fusion
using low-dose rhBMP-2 and cultured marrow stromal cells,”Journal of Orthopaedic Research, vol. 27, no. 3, pp. 380–384,2009.
[47] T.-S. Fu, S. W. Ueng, T.-T. Tsai, L.-H. Chen, S.-S. Lin, and W.-J.Chen, “Effect of hyperbaric oxygen on mesenchymal stem cellsfor lumbar fusion in vivo,” BMCMusculoskeletal Disorders, vol.11, article 52, 2010.
[48] T.-S. Fu, Y.-H. Chang, C.-B. Wong et al., “Mesenchymal stemcells expressing baculovirus-engineered BMP-2 and VEGFenhance posterolateral spine fusion in a rabbit model,” SpineJournal, vol. 15, no. 9, pp. 2036–2044, 2015.
[49] W.-J. Chen, J.-W. Huang, C.-C. Niu et al., “Use of fluorescencelabeled mesenchymal stem cells in pluronic F127 and poroushydroxyapatite as a bone substitute for posterolateral spinalfusion,” Journal of Orthopaedic Research, vol. 27, no. 12, pp. 1631–1636, 2009.
[50] T. Schubert, S. Lafont,G. Beaurin et al., “Critical size bone defectreconstruction by an autologous 3D osteogenic-like tissuederived from differentiated adipose MSCs,” Biomaterials, vol.34, no. 18, pp. 4428–4438, 2013.
[51] B. S. Shamsul, K. K. Tan, H. C. Chen, B. S. Aminuddin, and B.H. I. Ruszymah, “Posterolateral spinal fusion with ostegenesisinduced BMSC seeded TCP/HA in a sheep model,” Tissue andCell, vol. 46, no. 2, pp. 152–158, 2014.
[52] D. L.Wheeler, J. M. Lane, H. B. Seim III, C.M. Puttlitz, S. Itescu,and A. S. Turner, “Allogeneic mesenchymal progenitor cells forposterolateral lumbar spine fusion in sheep,”The Spine Journal,vol. 14, no. 3, pp. 435–444, 2014.
[53] D. L. Wheeler, D. C. Fredericks, R. F. Dryer, and H. W. Bae,“Allogeneic mesenchymal precursor cells (MPCs) combinedwith an osteoconductive scaffold to promote lumbar interbodyspine fusion in an ovine model,” Spine Journal, vol. 16, no. 3, pp.389–399, 2016.
[54] M. D. Cuenca-Lopez, J. A. Andrades, S. Gomez et al., “Eval-uation of posterolateral lumbar fusion in sheep using mineralscaffolds seededwith cultured bonemarrow cells,” InternationalJournal of Molecular Sciences, vol. 15, no. 12, pp. 23359–23376,2014.
[55] Y. Qian, Z. Lin, J. Chen et al., “Natural bone collagen scaffoldcombined with autologous enriched bone marrow cells forinduction of osteogenesis in an ovine spinal fusion model,”Tissue Engineering—Part A, vol. 15, no. 11, pp. 3547–3558, 2009.
[56] T. Goldschlager, P. Ghosh, A. Zannettino et al., “A comparisonof mesenchymal precursor cells and amnion epithelial cellsfor enhancing cervical interbody fusion in an ovine model,”Neurosurgery, vol. 68, no. 4, pp. 1025–1035, 2011.
[57] T. Goldschlager, J. V. Rosenfeld, P. Ghosh et al., “Cervical inter-body fusion is enhanced by allogeneic mesenchymal precursorcells in an ovine model,” Spine, vol. 36, no. 8, pp. 615–623, 2011.
[58] S. A. Abbah, C. X. F. Lam, A. K. Ramruttun, J. C. H. Goh, andH.-K. Wong, “Fusion performance of low-dose recombinanthuman bone morphogenetic protein 2 and bone marrow-derived multipotent stromal cells in biodegradable scaffolds: acomparative study in a large animal model of anterior lumbarinterbody fusion,” Spine, vol. 36, no. 21, pp. 1752–1759, 2011.
[59] M. C. Gupta, T. Theerajunyaporn, S. Maitra et al., “Efficacy ofmesenchymal stem cell enriched grafts in an ovine posterolat-eral lumbar spinemodel,” Spine, vol. 32, no. 7, pp. 720–726, 2007.
[60] L. Moro-Barrero, G. Acebal-Cortina, M. Suarez-Suarez, J.Perez-Redondo, A. Murcia-Mazon, and A. Lopez-Muniz,“Radiographic analysis of fusion mass using fresh autologous

Stem Cells International 27
bone marrow with ceramic composites as an alternative toautologous bone graft,” Journal of Spinal Disorders and Tech-niques, vol. 20, no. 6, pp. 409–415, 2007.
[61] G. A. Odri, A. Hami, V. Pomero et al., “Development of a per-operative procedure for concentrated bone marrow adjunctionin postero-lateral lumbar fusion: radiological, biological andclinical assessment,” European Spine Journal, vol. 21, no. 12, pp.2665–2672, 2012.
[62] R. G. Johnson, “Bone marrow concentrate with allograft equiv-alent to autograft in lumbar fusions,” Spine, vol. 39, no. 9, pp.695–700, 2014.
[63] R. Hart, M. Komzak, F. Okal, D. Nahlık, P. Jajtner, and M.Puskeiler, “Allograft alone versus allograft with bone marrowconcentrate for the healing of the instrumented posterolaterallumbar fusion,” Spine Journal, vol. 14, no. 7, pp. 1318–1324, 2014.
[64] R. M. Ajiboye, J. T. Hamamoto, M. A. Eckardt, and J. C. Wang,“Clinical and radiographic outcomes of concentrated bonemar-row aspirate with allograft and demineralized bone matrix forposterolateral and interbody lumbar fusion in elderly patients,”European Spine Journal, vol. 24, no. 11, pp. 2567–2572, 2015.
[65] R. K. Eastlack, S. R. Garfin, C. R. Brown, and S. C. Meyer,“Osteocel plus cellular allograft in anterior cervical discectomyand fusion: evaluation of clinical and radiographic outcomesfrom a prospective multicenter study,” Spine, vol. 39, no. 22, pp.E1331–E1337, 2014.

Submit your manuscripts athttps://www.hindawi.com
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Anatomy Research International
PeptidesInternational Journal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporation http://www.hindawi.com
International Journal of
Volume 2014
Zoology
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Molecular Biology International
GenomicsInternational Journal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
The Scientific World JournalHindawi Publishing Corporation http://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
BioinformaticsAdvances in
Marine BiologyJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Signal TransductionJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
BioMed Research International
Evolutionary BiologyInternational Journal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Biochemistry Research International
ArchaeaHindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Genetics Research International
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Advances in
Virolog y
Hindawi Publishing Corporationhttp://www.hindawi.com
Nucleic AcidsJournal of
Volume 2014
Stem CellsInternational
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Enzyme Research
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
International Journal of
Microbiology