Menopause and Migraine: What is the Evidence? Cases and ... · also likely to have resolution of...
Transcript of Menopause and Migraine: What is the Evidence? Cases and ... · also likely to have resolution of...
Menopause and Migraine:
What is the Evidence?
Cases and Implications
Jelena Pavlović, MD, PhD
Assistant Professor or Neurology
Montefiore Headache Center
Albert Einstein College of Medicine
Disclosures
Consultant: Allergan
Primary investigator for clinical trial - Alder Biopharmaceuticals (funds to
Montefiore Medical Center)
Objectives
• Describe the stages of menopausal transition (MT), common
complaints associated with MT and accompanying changes in
hormones that impact migraine
• Appreciate changes in migraine across the stages of menopausal
transition
• Appreciate the effects of medically induced vs. natural menopause
on migraine
• Discuss the adequate approach to treatment of migraine during
menopausal transition with focus on hormone therapy (HT)
Case 1
• MK is a 65 yo woman whose migraine with aura began around the time of her first period at age 15. Attacks often clustered around menses (without aura at those times). Her headaches improved in pregnancy and during lactation, but worsened in her mid 40s without an clear reason at first, becoming less predictable, more frequent and more difficult to treat. Preventive treatment with propranolol significantly improved her symptoms. Her final menstrual period was at age 51. Two years later she decided to stop her preventive medication and has since been headache free.
Terminology of Menopause
• Menopause - final menstrual period resulting from the physiologic permanent decline in gonadal hormone levels confirmed by 12 months of amenorrhea in women with a uterus
• Premenopause/Premenopausal – refers to phase of life that precedes menopause
• Menopausal Transition (MT) - begins with the onset of intermenstrual cycle irregularities (± 7 days) and/or other menopause-related symptoms ends with FMP
• Perimenopause - “around menopause” same at MT + extends beyond the FMP to include the 12 months after menopause
Case 2
• MK contacts you wondering if you’d see her 45-year old daughter, PK, whose occasional (previously readily responsive to NSAIDs) menstrual migraine has significantly worsened resulting in significant loss of productivity. Her headaches are now occurring 18 days per month and are less responsive to treatment with NSAIDs. Her period has become irregular and she is no longer able to predict when her headache may occur which is leading to considerable anxiety.
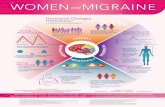
Menopausal transition (MT) is characterized by dynamic hormone changes
FMP – Final Menstrual PeriodPavlovic et al. Neurology 2016 Jul 5;87(1):49-56,.; Jaffe H. NAMS Oct 2016.
O'Connor KA, Ferrell R, Brindle E, Trumble B, Shofer J, Holman DJ, Weinstein M. Progesterone and ovulation across stages of
the transition to menopause. Menopause. 2009;16(6):1178
Hormonal changes vary in pattern across MT and within individuals
Case 2
• PK was on OCPs until age 40 when she went through 3 rounds of IVF in an attempt to conceive. She did experience headaches during hormonal treatment for IVF which quickly improved once she became pregnant. She delivered her son at 42 years of age and nursed him until a year ago. Since stopping nursing, she has had 8 periods, which have varied in length and symptoms. In addition to having increased headaches, her sleep has suffered and she has just started experiencing night-sweats and what she thinks are hot flashes, though she is not sure.
MT Symptoms are highly variable
• Vasomotor instability
• Sleep disturbances
• Mood disturbances
• Somatic symptoms: – Fatigue, palpitations, breast pain and enlargement
- Headache/Migraine?
Symptom frequency can vary depending on race/ethnicity/culture and women follow specific
trajectories with respect to symptom change
(Sievert et al. 2007)
• Obermeyer et al . Menopause. 2007 Jul-Aug;14(4):788-97.
• R
Migraine and Menopausal Transitionchallenges in available knowledge
• Lack of studies with systematic collection of hormonal data,
characterization of stage of MT and reliable migraine data
• Smaller studies with appropriate migraine information tend to
have inadequate MT/hormonal data while larger studies of MT
and menopause often lack criteria for migraine diagnosis
• Majority of studies cross-sectional, retrospective questionnaire
based
• No longitudinal studies available to date
Migraine and Menopausal Transition
Study approach using retrospective questionnaires:
- 8 to 13% develop new onset migraine during MT
- Prevalence of migraine ranges from 10% to 29% during MT
- Prevalence the highest in late perimenopausal group (31% vs 16.7 in pre-menopausal)
- Over 60% of women in menopause clinics report headache
- Population studies generally support the notion that migraine prevalence peaks in late perimenopause and declines following FMP, in clinic studies migraine often persists post FMP
Hodson J, Climacteric. 2000;3(2):119-124; Granella F,. Headache. 1993;33(7):385-389; Ripa et al. Int J Womens Health. 2015 Aug 20;7:773-82
Migraine and Menopausal Transition
- Migraine improves in 8% to 36%, worsens in 9% to 42%, and remains unchanged in 27% to 64% at the time of menopause
- Trend toward fewer migraine attacks and milder symptoms in menopause
- Migraine without aura appears to be influenced by MT more than migraine with aura
- In women with migraine without aura time since menopause predictor of improvement
- Women with menstrual migraine and PMS tend to have best prognosis post-menopause
- Unclear whether migraine associated with other menopausal symptoms
Hodson J, Climacteric. 2000;3(2):119-124; Granella F,. Headache. 1993;33(7):385-389; Ripa et al. Int J Womens Health. 2015 Aug 20;7:773-82; Makita K. et al. Cephalalgia. 2016 Jun 2.
American Migraine Prevalence and Prevention Study (AMPP)
Perimenopause and Menopause Associated With High Frequency Headache in Migraineurs
Headache: The Journal of Head and Face PainVolume 56, Issue 2, pages 292-305, 21 JAN 2016 http://onlinelibrary.wiley.com/doi/10.1111/head.12763/full#head12763-fig-0002
Daily changes up to 5 days post peaks in ovulatory cycles in women with and without history of migraine (absolute level, daily rate of decline and percent change)
Women with migraine have distinct hormone patterns:the rate of estrogen decline is faster than controls and is phase (luteal only) and day (first two days from peak) specific and independent of headache occurrence
SWAN: Daily Hormone Study
Pavlović JM, Allshouse AA, Santoro NF, Crawford SL, Thurston RC, Neal-Perry GS, Lipton RB, Derby CA. Sex hormones in women with and without migraine: Evidence of migraine-specific hormone profiles. Neurology, 2016 Jul 5;87(1):49-56.
*
*
*
Faster rate of estrogen decline in migraineurs over the first two days from peak
No difference between controls and migraineurs
Case 2 continued
• PK asks that since her symptom are due to hormonal fluctuations and her mother has been symptoms free since menopause, should she consider undergoing early menopause by having an oophorectomy now?
Surgical menopause
- Leads to the abrupt withdrawal of estrogen
- Sudden menopause whether medical or surgical or due to ovarian failure is associated with worse symptom profiles
- 67% had worsening of existing migraine
- Migraine improvement occurred only in spontaneous menopause group
Case 2 continued
• PK wonders if re-starting OCPs would be helpful as her migraines were previously well controlled with OCPs
Managing Migraine in Perimenopause
Symptom
Relief
Migraine
relief
Birth
Control
Endometrial
Cancer
Prevention
Hormonal
contraceptives
(oral or ring)
+++ ++ +++ +++
Cyclic progestin
therapy
+/- ? - ++
Progesterone
IUD
- +/- +++ +++
EPT ++ ++ - +++
Treatment Options
• Lifestyle adjustments
• Behavioral approaches
• Diet/alcohol
• Regular sleep pattern
• Symptomatic treatment
• Acute treatment
• Standard preventive
• Menstrual mini-prevention
• Hormone therapy
Non-medication Medication
Case 1 continued
• MK, PK’s mother and your 65 yo patient with migraine with aura (MA) who has been headache free since menopause returns to your office wondering if given her history of MA, she should start hormone therapy (HT) that has been recommended by her internist for osteoporosis following a recent hip fracture.
Hormone Therapy
• Risks are dependent on– Age (total mortality reduced by 30% if started at age <60)– Time since menopause– Age at menopause– Duration of therapy– Type of HT– Route of administration– Dose of HT
• Benefits are dependent on– Number of menopause related symptoms
Areas of Concern
Migraine, MT and HTcurrent knowledge
• Like OCPs, HT can improve, worsen or not change migraine
depending on
– Preparation used and route of delivery
– Dose used
– Continous vs. intermittent dosing
– Concomitant use of progestin
– Worsening is more likely with tablets than transdermal
preparations
Migraine, MT and HTcurrent knowledge
- Traditionally not thought to have adverse effects on migraine without aura
- Some evidence for adverse effects in migraine with aura, but no contraindication for use in migraine with aura – risk unclear
- Migraine is more common among HT users than non-users
- Worsening of headache on HT is associated with worsening of headache during menopause
- Recent study suggests that new worsening of headache while on HT for symptoms of menopause, predicts increased risk of stroke
Conclusions
• Prevalence of migraine is high in perimenopause
• Women who report migraine associated with menstruation
are more likely to experience perimenstrual worsening but
also likely to have resolution of headache after menopause
• Sudden menopause – related to worse headache outcomes
• Need to tailor treatment to individual patient needs and for
each stage of perimenopause – use of HT appropriate with
awareness of caveats
• Menopause often provides relief from migraine