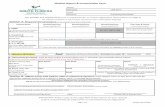
MEDICAL HISTORY
description
Transcript of MEDICAL HISTORY


U.S. 28 year old male, catholic, married, born on May 6, 1981, works as a tricycle driver since 2001, residing in Caloocan City with wife.
Chief Complaint:

7 Yrs PTA
•White scales of the scalp resembled dandruff when scratched (no consult)• Few mos. later: pustules and papules that later coalesced to erythematous plaques topped with scales spread all over his body affecting his back, trunk, upper and lower extremities and his face consult at UST Dermatology OPD; punch biopsy: Psoriasis – medications: PUVA therapy (once in 2002), Methotrexate 1 tab BID for 1 wk, Dermovate with Petroleum Jelly and LCD, Hydroxizine (Iterax) for pruritus 3x/day prn resolution of Symptoms
2 Yrs PTA
• Reappearance of lesions • Painful swelling of distal and proximal joints of the fingers of right and left hands and feet (self-medication: Naproxen temporary relief)• Gradual limitation of in the movement of digits• Consult to Rheumatologist, prescribed with Celebrex and requested for further lab work-ups; but patient lost to follow-up
1 Yr PTA• Pain and swelling in both knees, noted to be limping, and pain when walking down the stairs• Relieved by rest or sitting down

1 month PTA
• Swelling of both knees with increasing severity of pain (no consult)
1 week PTA
• Pain in the hips extending down to his ankles• More difficulty in ambulating
5 days PTA
• Consulted an Orthopedic Surgeon in Marikina; was told to have excess fluid in knee joints & advised arthrocentesis (pt. opted not to)
4 days PTA
•Fever [undocumented] (self-medication: Paracetamol temporary lysis of fever)• Persistence of pain and fever consult at FEU Hospital (X-Ray of leg: soft tissue swelling); advised admission but refused due to financial constraints; referred to USTH for further evaluation & management
ADMISSION

• (-) DM• (-) HPN• (-) Joint surgery• (-) history of trauma• (-) Allergy• Diagnosed with dengue fever (2nd year
high school)• Excision of cyst at the back (2007)

(+) Myocardial Infarction – father (+) DM – father (-) HPN (-) stroke (-) Psoriasis (-) Cancer (-) Arthrides

Smoker: 16-22 y/o (1-2 sticks per day) Occasional Alcoholic Beverage Drinker Denies Illicit Drug Use 3 past sexual partners, all protected

No wt. loss, no loss of appetite No hearing loss, no nasal congestion, no
cough No dyspnea, orthopnea, cyanosis No chest pain, palpitations No abdominal pain, diarrhea, constipation No dysuria, frequency, change in
character of urine

General Survey• Conscious, coherent, oriented as to time, place
and person, not in cardio-respiratory distressVital Signs• BP 120/70 mmHg, PR 83 bpm, RR 20 cpm, T
36.6 °CSkin• Warm moist skin, (+) erythematous plaques
topped with scales all over the body, (+) hyperpigmented patches over the extremitie, (+) oil spots, (+) nail pitting, (+) onychodystrophy

HEENT• Pink palpebral conjunctivae, anicteric
sclerae, no naso-aural discharge, no tragal tenderness, moist buccal mucosa, nonhyperemic PPW, tonsils not enlarged
Neck• Supple neck, trachea midline, no palpable
cervical lymph nodes, thyroid gland not enlarged
Cardiovascular• Adynamic precordium, AB at 5th LICS, MCL;
no murmurs• All pulses full and equalRespiratory• Symmetric chest expansion, no retractions,
clear breath sounds on all lung fields, no crackles, no wheezes

Abdomen• Flat abdomen, NABS, soft, nontender, no
massesMusculoskeletal• (+) sausage-shaped 4th digit of the right
hand• (+) swelling and tenderness, both knees,
DIP 4th R digit of the hand, R ankle• (+) flexed 5th left digit and the 4th R digit
of the hand• Cannot flex the PIP and DIP of the right
2nd digit of the hand

Neurological• Conscious, oriented to person, place and
time, can follow commands• GCS 15 E4V5M6; pupils 2-3 mm, isocoric
ERTL, V1,V2,V3 intact; intact hearing, can swallow, (+) gag reflex, can shrug shoulders, tongue midline on protrusion
• Motor: MMT 5/5 on both UE; 4/5 on both LE, no atrophy
• Cerebellum: no deficits, can do FTNT, APST, HTST
• Sensory: no sensory deficits• DTRs: 2+ on the UE, LE not assessed• (-) Babinski; no nuchal rigidity

• History of Psoriasis• Painful swelling of distal and proximal joints
of the fingers of right and left hands and feet• Gradual limitation of in the movement of
digits• Pain and swelling in both knees (increasing
severity of pain), limping, and pain when walking down the stairs (difficulty in ambulating); Relieved by rest or sitting down
• Pain in the hips extending down to ankle• excess fluid in knee joints• Persistence of pain and fever• X-ray of leg: soft tissue swelling

• (+) erythematous plaques topped with scales all over the body, (+) hyperpigmented patches over the extremitie, (+) oil spots, (+) nail pitting, (+) onychodystrophy
• (+) sausage-shaped 4th digit of the right hand
• (+) swelling and tenderness, both knees, DIP 4th R digit of the hand, R ankle
• (+) flexed 5th left digit and the 4th R digit of the hand
• Cannot flex the PIP and DIP of the right 2nd digit of the hand


Differential diagnosis Gout Osteoarthritis Reactive Arthritis Rheumatoid Arthritis Septic Arthritis

Gout• a common disorder of uric acid
metabolism– can lead to deposition of monosodium urate
(MSU) crystals in soft tissue and recurrent episodes of debilitating joint inflammation
• if untreated - joint destruction and renal damage
• definitively diagnosed based on the demonstration of urate crystals in aspirated synovial fluid

GoutPhysical examination findings:• During an acute gout attack, examine all joints to
determine if the patient's arthritis is monoarticular or polyarticular
• Involved joints have all the signs of inflammation: swelling, warmth, erythema, and tenderness
• The erythema over the joint may resemble cellulitis; the skin may desquamate as the attack subsides
• The joint capsule becomes quickly swollen, resulting in a loss of range of motion of the involved joint
• During an acute gout attack, patients may be febrile, particularly if it is an attack of polyarticular gout
• Look for sites of infection that may have seeded the joint and caused an infectious arthritis that can resemble or coexist with acute gouty arthritis
• The presence of tophi suggests long-standing hyperuricemia

Osteoarthritis • Predominantly involves the weight-
bearing joints, including the knees, hips, cervical and lumbosacral spine, and feet
• Other commonly affected joints - the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints of the hands
• Cartilage is grossly affected– Focal ulcerations eventually lead to cartilage
loss and eburnation– Subchondral bone formation also occurs, with
development of bony osteophytes

OsteoarthritisPhysical examination findings:• Mostly limited to the affected joints• Malalignment with a bony enlargement
(depending on the disease severity) may occur
• Most cases of osteoarthritis do not involveerythema or warmth over the affected joint(s)– however, an effusion may be present
• Limitation of joint motion or muscle atrophy around a more severely affected joint may occur

Reactive Arthritis• Also known as Reiter syndrome, is an autoimmune condition that
develops in response to an infection• Usually develops 2-4 weeks after a genitourinary or gastrointestinal
infection – recent evidence indicates that a preceding respiratory infection
with Chlamydia pneumoniae may also trigger the disease– about 10% of patients do not have a preceding symptomatic
infection. • Both postvenereal and postenteric forms of reactive arthritis may
manifest initially as nongonococcal urethritis• Mild dysuria, mucopurulent discharge, prostatitis and epididymitis in
men, and vaginal discharge and/or cervicitis in women are other possible manifestations
• Onset - usually acute and characterized by malaise, fatigue, and fever
• An asymmetrical, predominately lower-extremity, oligoarthritis - the major presenting symptom
• Low-back pain occurs in 50% of patients• Heel pain is common because of enthesopathies at the Achilles or
plantar aponeurosis insertion on the calcaneus• The complete Reiter triad of urethritis, conjunctivitis, and arthritis
may occur

Reactive ArthritisPhysical examination findings:• Joints, axial skeleton, entheses
– Peripheral joint involvement associated - typically asymmetric and usually affects the weight-bearing joints (ie. knees, ankles, hips), but the shoulders, wrists, and elbows may also be affected
– More chronic and severe cases - the small joints of the hands and feet may also be involved; as in other spondyloarthropathies, dactylitis (ie, sausage digits) may develop.
– While 50% of patients with reactive arthritis may develop low-back pain, most physical examination findings in patients with acute disease - minimal except for decreased lumbar flexion; patients with more chronic and severe axial disease may develop physical findings similar to ankylosing spondylitis
– As with other spondyloarthropathies, the enthesopathy of reactive arthritis may be associated with findings of inflammation (ie. pain, tenderness, swelling) at the Achilles insertion; other sites include the plantar fascial insertion on the calcaneus, ischial tuberosities, iliac crests, tibial tuberosities, and ribs
• Skin and nails – Keratoderma blennorrhagica on the palms and soles is indistinguishable
from pustular psoriasis - highly suggestive of chronic reactive arthritis– Erythema nodosum may develop but uncommon– Nails can become thickened and crumble, resembling mycotic infection or
psoriatic onychodystrophy, but nail pitting is not observed – Circinate balanitis may also develop
• Other mucosal signs and symptoms: Painless shiny patches in the palate, tongue, and mucosa of the cheeks and lips have been described

Reactive ArthritisPhysical examination findings:• Ocular findings
– Conjunctivitis - part of the classic triad of Reiter syndrome and can occur before or at the onset of arthritis
– Other ocular lesions include acute uveitis (20% of patients), episcleritis, keratitis, and corneal ulcerations; the lesions tend to recur
• Enteric infections – May trigger reactive arthritis; pathogens include Salmonella,
Shigella, Yersinia, and Campylobacter species; the frequency of reactive arthritis after these enteric infections - about 1-4%
– Some patients continue with intermittent bouts of diarrhea and abdominal pain; lesions resembling ulcerative colitis or Crohn disease have been described when ileocolonoscopy is performed in patients with established reactive arthritis
• Other manifestations – Mild renal pathology with proteinuria and microhematuria– In severe chronic cases, amyloid deposits and
immunoglobulin A (IgA) nephropathy have been reported– Cardiac conduction abnormalities may develop, and aortitis
with aortic regurgitation occurs in 1-2%

Rheumatoid Arthritis• A chronic systemic inflammatory disease of unknown
cause that primarily affects the peripheral joints in a symmetric pattern
• Constitutional symptoms, including fatigue, malaise, and morning stiffness are common
• Extra-articular involvement of organs such as the skin, heart, lungs, and eyes can be significant
• Causes joint destruction and thus often leads to considerable morbidity and mortality
• Has a significant genetic component, and the shared epitope of the HLA-DR4/DR1 cluster is present in up to 90% of patients with RA, although it is also present in more than 40% of controls
• Synovial cell hyperplasia and endothelial cell activation are early events in the pathologic process that progresses to uncontrolled inflammation and consequent cartilage and bone destruction
• Genetic factors and immune system abnormalities contribute to disease propagation

Rheumatoid ArthritisPhysical examination findings:• Joint involvement - the characteristic feature• In general, the small joints of the hands and feet are affected in a relatively
symmetric distribution• The most commonly affected joints, in decreasing frequency, include the
MCP, wrist, PIP, knee, MTP, shoulder, ankle, cervical spine, hip, elbow, and temporomandibular joints
• Joints show inflammation with swelling, tenderness, warmth, and decreased range of motion
• Atrophy of the interosseous muscles of the hands is a typical early finding• Joint and tendon destruction may lead to deformities such as ulnar deviation,
boutonnière and swan-neck deformities, hammer toes, and, occasionally, joint ankylosis
• Other commonly observed musculoskeletal manifestations – tenosynovitis and associated tendon rupture due to tendon and ligament involvement,
most commonly involving the fourth and fifth digital extensor tendons at the wrist– periarticular osteoporosis due to localized inflammation; generalized osteoporosis due
to systemic chronic inflammation, immobilization-related changes, or corticosteroid therapy; and carpal tunnel syndrome
– most patients have muscle atrophy from disuse, which is often secondary to joint inflammation

Septic Arthritis• Also known as infectious arthritis• May represent a direct invasion of joint space
by various microorganisms, including bacteria, viruses, mycobacteria, and fungi
• Reactive arthritis, a sterile inflammatory process, may be the consequence of an infectious process located elsewhere in the body
• Bacterial pathogens - the most significant because of their rapidly destructive nature
• Failure to recognize and to appropriately treat septic arthritis results in significant rates of morbidity and may even lead to death

Septic ArthritisPhysical examination findings:• The most commonly involved joint is the knee
(50% of cases), followed by the hip (20%), shoulder (8%), ankle (7%), and wrists (7%)
• The elbow, interphalangeal, sternoclavicular, and sacroiliac joints each make up 1-4% of cases
• A thorough inspection of all joints for signs of erythema, swelling (90% of cases), warmth, and tenderness is essential for diagnosing infection
• Infected joints usually exhibit an obvious effusion, which is associated with marked limitation of both active and passive ranges of motion
• Frequently, these findings are apparent but may be diminished or poorly localized in cases of infection of the spine, hip, and shoulder joints

• An acute inflammatory condition of the skin characterized by localized pain, erythema, swelling and heat.
• Caused by indigenous flora colonizing the skin and appendages and exogenous bacteria (e.g. Staphylococcus aureus, Streptococcus pyogenes)
• May gain access through cracks in the skin, wounds, abrasions, burns
• Lesions are nodular and surrounded by vesicles that rupture and discharge pus and necrotic material


Check for rheumatoid factor for coincident occurence of RA; PsA alone = (-) RF
Check also for gout ANA, autoantibodies For seronegative arthritis without skin
changes, check for HLA-B13, -BW57, -B27.
Sudden onset is assoc. with HIV so check for HIV disease

NO diagnostic laboratory tests ESR and CRP often elevated Extensive psoriasis = uric acid may be
elevated HLA-B27 is found in 50-70% of patients
with axial disease, but <15-20% if only peripheral joint involvement

Examine the fluid in joints a. Gross examination – clarity, colorb. Cell count – WBC perc. Microscopic examination – crystals, Gram staining d. Culture and sensitivity

** Aspirating needle should never be passed through an overlying cellulitis or psoriatic plaque because of the risk of introducing infection

Reference 8/27/09
Hgb 120-170 d/L 105
Hct 0.37-0.54 0.32
RBC 4-6x 10^12/L 4.03
WBC 4.5-10x 10^9/L 8.60
Neutrophil 0.50-0.70 0.70
Segs 0.50-0.70 0.70
Bands
Lympho 0.20-0.40 0.30
Mono 0-0.07
Eos 0-0.05
Plt 150-450x 10^9/L 552
MCV 87 +/-5 U^3 79.60
MCH 29+/-2 pg 26.0
MCHC 34+/-2 g/dL 32.70
RDW 25.90 13.40

Reference 8/27/09
BUN 9-23 6.9
Crea 0.5-0.2 0.76
AST-SGOT 0-32 27.3
ALT-SGPT 0-31 41.2


DIP involvement – “pencil-in-cup” deformity

marginal erosions of bone and irregular destruction of joint and bone, which, in the phalanx, may give the appearance of a sharpened pencil

“whiskering” – marginal erosions with adjacent bony proliferation
Small joint ankylosis Osteolysis of phalangeal and metacarpal
bone with telescoping of digits Periostitis and proliferative new bone at
site of enthesitis

Asymmetric sacroiliiitis

Less zygoapophyseal joint arthritis, fewer and less symmetric and delicate syndesmophytes
Fluffy hyperperiostosis on anterior vertebral bodies
Paravertebral ossification

Severe cervical spine involvement but relative sparing of thoracolumbar spine

Ultrasound and MRI demonstrate enthesitis and tendon sheath effusions

Thick S. corneum and projections of the epidermis
Parakeratosis(cell nuclei within thickened s. corneum)
Elongation of rete ridges

PMN leukocyte and lymphocyte infiltration of dermis and epidermis forming microabscesses of Munro in the s.corneum
exocytosis of neutrophils into epidermis producing spongiform pustules (Kogoj)

PsoriasisPsoriatic Arthritis
Cellulitis



Areas of Predilection Scalp Nails Extensor Surface,
Limbs Umbilical region Sacrum


Erythematous rash Scaling Plaques
Silvery white lamellar
Auspitz’s Sign Koebner’s
Phenomenon




An inflammatory arthritis that occurs in a patient with psoriasis.
Harrison’s Internal Medicine 17th edition
A form of arthritis that occurs in patients with psoriasis with the hallmarks of an "inflammatory" arthritis, including joint pain, erythema, and swelling, often with
prominent stiffness. Mease, P., Menter, A. (2005) , Psoriatic Arthritis: Understanding Its Pathophysiology and
Improving Its Diagnosis and Management. Retrieved from: http://cme.medscape.com/viewarticle/509053

Unique to Psoriatic Arthritis: DIP joint involvement Nail changes Dactylitis Enthesitis Spondylitis Lytic and periarticular new bone
formation x-ray features Iritis or Uveatis
Mease, P., Menter, A. (2005) , Psoriatic Arthritis: Understanding Its Pathophysiology and Improving Its Diagnosis and Management. Retrieved from: http://cme.medscape.com/viewarticle/509053

• Patterns of Arthropathy1. Arthritis of DIP joints2. Asymmetric oligoarthritis3. Symmetric polyarthritis4. Axial involvement5. Arthritis Mutilans

Distal Interphalangeal joint arthritis
Occurs in 15 % of cases
Nail changes also seen
Harrison’s Internal Medicine 17th edition

Asymmetric Oligoarthritis
Involves the knee or any large joint with a few small joints in the fingers and toes Metarsophalangeal Proximal interphalengeal Distal interphalengeal
Dactylis Sausage shaped digits due to
inflammation of the flexor tendons and synovium and pitting edema of the distal extremities may be observed
Harrison’s Internal Medicine 17th edition

Symmetric polyarthritis
Affects the Hands, wrists, knees, and feet symmetrically Proximal interphalangeal
joints Metacarpophalangeal joints
Peripheral joints are less tender compared to RA
Harrison’s Internal Medicine 17th edition

Axial Arthropathy Spine and sacroiliac
joints
Harrison’s Internal Medicine 17th edition

Arthritis mutilans• Widespread shortening
or telescoping of digits due to osteolysis of the phalanges and metacarpals
• coexisting with ankylosis and contractures in other digits
• opera-glass deformity or pencil-in-cup radiographic findings
• Fever
Harrison’s Internal Medicine 17th edition

Pitting Horizontal ridging Onycholysis Discoloration of
nail margins Dystrophic
hyperkeratosis
Onycholysis
Nail pitting
OnychodystrophyHarrison’s Internal Medicine 17th edition

Involvement of the distal and proximal interphalangeal joints, together with
tendon sheath involvement, may give the digit a sausage shape
Harrison’s Internal Medicine 17th edition

Inflammation at the sites of ligamentous and tendinous insertions
Emedicine Retrieved from: http://emedicine.medscape.com/article/1108557-overview

Risk Factors:•Immunocompromised due to meds•Auspitz sign – break in skin integrity

Cellulitis
Indigenous flora colonizing the skin
Staphylococcus aureus
Streptococcus pyogenes
Exogenous bacteria
Harrison’s Principles of Internal Medicine 17th ed.

At the involved site Localized pain Erythema Swelling Warmth Borders are not sharply
demarcated Fever and chills Malaise
Harrison’s Principles of Internal Medicine 17th ed.



Improve patient’s quality of life Achieve and maintain control of psoriatic
lesions Relieve pain Halt progression of disease

AlefaceptEfalizumabCyclosporineMethotrexateAcitretinPUVA

• Usually for treatment of plaque psoriasis• Immunosuppressive dimeric fusion protein• Consists of extracellular CD2 binding
portion of human leukocyte function • MOA: Interferes with lymphocyte activation
resulting in the reduction in subsets of CD2 lymphocyte and circulating CD4 and CD8 lymphocyte counts
• Administration: IM• Warnings: Lymphopenia, increased
malignancies and serious infections
Basic and Clinical Pharmacology, 10th EdHarrison’s Principles of Internal Medicine, 17th Ed

• Usually for SEVERE psoriasis• Immunosuppresive recombinant humanized
anti CD11a monoclonal antibody• MOA: Binding to CD11a inhiits the
interaction of LFA-1 on all lymphocutes with intercellular adhesion molecule inhibiting activation, adhesion and migration of T-Lymphocytes into skin
• Administration: SC injection• Warnings: Serious infections, potential
increased malignancy, thrombocytopenia, hemolytic anema and worsening of psoriasis
* Should not be given with other immunosuppresive medication
Basic and Clinical Pharmacology, 10th EdHarrison’s Principles of Internal Medicine, 17th Ed

• Immunosuppresive agent– Calcineurin inhibitor
• MOA:Form a complex with cyclophilin that inhibits the cysoplasmic phosphatase, calcineurin, which is necessary for activation of T-cell specific transcription factor
• Adverse effects: Renal dysfunction, hypertension, hyperkalemia, hyperuricemia, hypomagnesemia, hyperlipidemia, increased risk of malignancies
*reported to benefit Psoriatic arthritis Basic and Clinical Pharmacology, 10th EdHarrison’s Principles of Internal Medicine, 17th Ed

• Antimetabolite• MOA: Inhibition of dihydrofolate reductase, an
enzme important in the production of thymidine and purines– May interere with actions of interleukin-1– May also simulate increased release of adenosine, and
endogenous anti-inflammatory autocoid– May stimulate apoptosis and death of activated T
Lymphocytes• Administration: Oral• Adverse effects: Hepatotoxicity, pulmonary
toxicity, panctopenia, potential for increased malignancies , ulcerative stomatitis, nausea, diarrhea, teratogenecity
Basic and Clinical Pharmacology, 10th EdHarrison’s Principles of Internal Medicine, 17th Ed

• Effective in psoriasis (especially pustular forms)• Metabolite of etretinate , an aromatic retinoid • Retinoids include natural compounds and
synthetic derivatives of retinol that exhibit vitamin A activity• Because vitamin A affects normal epithelial differentiation,
it was investigated as a treatment for cutaneous disorders • Administration: Oral• Adverse Effects: teratogenecity, osteophyte
formation, hyperlipidemia, flare of inflammatory bowel disease, hepatotoxicity and depression
*Ethanol should be strictly avoided during treatment and for 2
months after discontinuing therapyBasic and Clinical Pharmacology, 10th EdHarrison’s Principles of Internal Medicine, 17th Ed

Topically applied or systemically administered psoralens are combined with UV-A
Psoralens Tricyclic furocouramins intercalated into DNA exposed to UV-A
form adducts with pyrimidine basesform DNA crosslinksdecrease DNA synthesisimprovement of psoriasis
Adverse Effects: skin dryness, actinic keratoses, increased risk of skin cancer

EtanerceptInfliximabAdalimumabTramadol

Decreases the activity of TNF Often used with methotrexate Mechanism of Action: binds two
molecules of TNF (α and β) and prevents them from binding to cellular receptors
Adverse Effects: risk of serious infections, neurologic and hematologic events, increased malignant potential

Chimeric IgGК monoclonal antibody composed of human and murine regions
Often used with methotrexate Mechanism of Action: Neutralizes
cytokines by binding specifically to TNF-α Adverse Effects: serious infections,
hepatotoxicity, hematologic events, hypersensitivity reactions, neurologic events, potential for increased malignancies

Recombinant monoclonal antibody Mechanism of Action: binds to TNF-α
receptor sites, thus inhibiting endogenous TNF-α activity
Adverse Effects: serious infections, neurologic events, potential for increased malignancies, hypersensitivity reactions, hematologic events

Used to manage moderate to moderately severe pain
Mechanism of Action: centrally acting analgesic that binds to μ-opioid receptor and additionally inhibits re-uptake of Norephinephrine and Serotonin
Adverse Effects: anaphylactoid reactions, seizures
Drug Interactions: Carbamazepine – inc. metabolism Quinidine – inc. Levels of tramadol Avoid in patients taking SSRI’s and MAO inhibitors