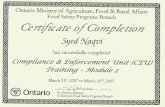
McLeod Trauma Informed Basics CEU
39
David A. McLeod, PhD, MSW UNDERSTANDING TRAUMA INFORMED PRACTICE
-
Upload
david-mcleod -
Category
Education
-
view
205 -
download
2
Transcript of McLeod Trauma Informed Basics CEU
- 1. David A. McLeod, PhD, MSW UNDERSTANDING TRAUMA INFORMED PRACTICE
- 2. So why am I so interested? LE background Detective Interrogations Justifications and outs Clinical Social Work Exp. NGRI Offender Tx Psychosexual risk evaluation Research area Intersection of Criminal Bx Development Traumatology Gender 2
- 3. Develop a more rich understanding of the ties between traumatic experiences and complex problems we seek to intervene in as social workers Relate to the process of how our brains associate stimuli with memories And think through how a better understanding and awareness of that individualized process can improve clinical practice Enjoy ourselves and talk a lot for 3 hours Sit for 3 hours and look at a lot of slides while David talks Become neuroscientific experts Spend extensive time on the anatomy of the brain Push the limits of the use of multisyllabic medical terminology in open CEU conversation TODAYS EXPECTATIONS What are not even gonna try to do today What we are going to try and do 3
- 4. SECTION 1: INTRO - TRIGGERS 4
- 5. WARM-UP (KEEP YOUR PAGE TURNED OVER UNTIL I SAY GO) Instructions: Part 1: As soon as you turn the page over quickly write by each picture the first feeling that comes over you as related to that picture. One word!!! Go Part 2: Now take a minute to think through and connect why you related that feeling to that picture Now at your table discuss with the other participants what you felt about each picture Look for similarities and themes Discuss as a group (All of us) 5
- 6. IMAGE 1 - MJ 6
- 7. IMAGE 2 FRESHLY CUT GRASS 7
- 8. IMAGE 3 SOUTHERN COMFORT 8
- 9. IMAGE 4 CHRISTMAS TREES (TREE FARM) 9
- 10. IMAGE 5 CAMPFIRE (CAMPFIRE SMELL) 10
- 11. IMAGE 6 - WORLD TRADE CENTER 11
- 12. Why is this important? We all have unconscious/subconscious connections/reactions/triggers where our brain neurologically connects small sensory experiences with significant memories and feelings. 12 1st major takeaway of the day
- 13. LETS TAKE A BREAK See you back in 5 13
- 14. SECTION 2: MECHANICS 14
- 15. WHY IS NEUROSCIENCE (THE BASE OF TRAUMA INFORMED PRACTICE) IMPORTANT FOR SOCIAL WORK PRACTICE? 15 Bio-Psycho-Social-Spiritual (BPSS) framework central to social work theorizing and practice Where is the BIO? Age, gender, medical conditions, but what else? Trauma Informed Practice engages the BIO dimension of our practice Provides the Missing Link that can enhance clinical practice Neuroscientific insights corroborate our psychosocial perspective (esp. related to brain plasticity) & help authenticate our therapeutic interventions
- 16. WHAT IS BRAIN PLASTICITY? 16 Brain (neuro) Plasticity (Introduced in 1949 but really understood in recent yrs): Basically means the brain changes throughout life slower rate as we age brain alters (it physically and chemically changes) in response to what it experiences by learning new information, we can reshape our brain via changes at nerve cell level thinking, learning, acting change the brains functioning and its structure We used to think the brain matured in adolescence and that was the end of growth (not so); changes are lifelong
- 17. MORE ON BRAIN PLASTICITY 17
- 18. The BIG Take away on Neuroplasticity What fires together wires together 18 2nd major takeaway of the day
- 19. TRAUMA 19 Trauma (defined)- an emotional or physical wound that is painful, distressful or shocking (e.g. child abuse, chronic neglect, natural disaster, domestic violence exposure, repeated foster care placements, bullying, chronic community violence) Acute Trauma a single traumatic event that is limited in time, such as an auto accident, a gang shooting, a parent's suicide, or a natural disaster. Chronic Trauma repeated assaults on the mind and body, such as chronic sexual or physical abuse or exposure to ongoing domestic violence. Complex Trauma is a term used by some trauma experts to describe both exposure to prolonged trauma, often inflicted by trusted people Multi-layered
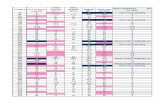
- 20. TRAUMA ISNT THAT PREVALENT.. RIGHT? 20 AdverseChildhoodExperiencesStudy(CDC)
- 21. Results of trauma Affective and Emotional dysregulation Cognitive impairment Attachment impairment Behavioral regulation Social development Negative Self concept 21 Alcoholism and alcohol abuse Chronic obstructive pulmonary disease (COPD) Depression Fetal death Health-related quality of life Illicit drug use Ischemic heart disease (IHD) Liver disease Risk for intimate partner violence Multiple sexual partners Sexually transmitted diseases (STDs) Smoking Suicide attempts Unintended pregnancies Early initiation of smoking Early initiation of sexual activity Adolescent pregnancy
- 22. SO WHAT ABOUT THE BRAIN? 22 Neuroscience research of past 30 yrs.---a major origin of psychopathology is trauma to the early developing nervous system, resulting in affective or emotional dysregulation ADHD? Other diagnoses? Brain scans (from Dr. Bruce Perry) CT scans on leftfrom healthy 3 yr.olds with average head size Images on rightfrom a series of 3 yr. olds following severe abuse and neglect in early childhood
- 23. Normal Extreme Neglect 3 Year Old Children
- 24. 24 Extreme NeglectNormal 3 Year Old Children
- 25. Normal Extreme Neglect 3 Year Old Children
- 26. TRAUMA AND THE BRAIN 26 Brain areas disrupted in presence of trauma are areas involved in responses to stress and fear: Base brain Brain stem & Locus coeruleus (regulate homeostasis); Hippocampus (memory); amygdala (emotions), brains alarm system; frontal cortex (learning / processing); orbito-frontal cortex, dorsolateral pre-frontal cortex (executive functions) Trauma response patterns hyperarousal - freeze, flight or fight reaction dissociative response - detached, becoming compliant, and numb to abuse Both responses become imprinted (fire together / wire together)
- 27. 27 Trauma regresses brain functionality
- 28. Trauma makes our brains act primal Regresses to brainstem level functions BASICALLY 28 3rd major takeaway of the day
- 29. WHY IS TRAUMA INFORMED PRACTICE IMPORTANT IN SOCIAL WORK? 29ReMoved
- 30. LETS TAKE A BREAK See you back in 5 30
- 31. SECTION 3: WRAP UP 31
- 32. WHERE DO WE GO FROM HERE? GOALS OF TRAUMA SPECIFIC TREATMENT Safe expression of feelings; Relief from symptoms and post-traumatic behaviors; Recovery of a sense of mastery and control in life; Corrections of misunderstanding and self-blame; Restoration of a sense of trust in oneself and the future; Development of a sense of perspective and distance regarding the trauma; Minimizing the scars of the trauma; An enhanced sense of safety and security; and Providing support and skills to help non-offending caregivers cope effectively with their own emotional distress and optimally respond to the traumatized child. 32
- 33. TRAUMA-SPECIFIC TREATMENTS EVIDENCE BASED APPROACHES ALL WITH GREAT ACRONYMS! Attachment, Self-Regulation, and Competency (ARC) Eye Movement Desensitization and Reprocessing Therapy (EMDR) involves Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) Child and Family Traumatic Stress Intervention (CFTSI) Child Parent Psychotherapy (CPP) Parent Child Interaction Therapy (PCIT) Others too 33
- 34. NO Others will disagree with me, and thats ok. You just have to ask yourself the right questions Who am I working with? What is their story? How could the trauma of their past be creating a barrier for helping them change their life? Each client is the expert here We have to ask the right questions BUT DO YOU NEED SPECIALIZED TRAINING TO BE TRAUMA INFORMED? 34
- 35. On the sheet I am passing out think about how to apply Trauma Informed Practice to your own area where you work. Answer the questions to yourself Then talk with your table Look for similarities and differences In how trauma impacts your clients How trauma can create barriers for intervention Ideas for moving your practice forward YOU ARE YOUR OWN EXPERT LAST ACTIVITY, I PROMISE 35
- 36. WHEN DO PEOPLE COME TO US FOR HELP? We work with vulnerable people who come to us for help in the most fragile states of their lives. Trauma is a part of their story and impacts the way they interact with you and the rest of their world. This impact is physical (neurological) 36 4th major takeaway of the day
- 37. CLOSING - FOUR MAIN POINTS OF TODAY 4 major takeaways for the day We all have instinctual reactions to stimuli These connect deeply (neurologically speaking) We often dont think about where they are coming from What Fires together wires together For good or bad our experienced physically change the brain Brain plasticity Trauma physically makes our brains function primally Base level brain function limited upper level reasoning Up and down We work with people in the most vulnerable states of their lives Trauma is a part of their story It improves our intervention when we can identify and work through it 37
- 38. 38
- 39. David Axlyn McLeod, PhD, MSW University of Oklahoma College of Arts and Sciences Assistant Professor | Anne and Henry Zarrow School of Social Work Affiliate Faculty | Women's & Gender Studies & Center for Social Justice Faculty Associate | Knee Center for Strong Families ZH 305 | 405.325.4647 [email protected] | www.damcv.com | @mcleodda THANKS FOR COMING! 39