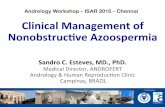
Management of Nonobstructive Azoospermia Before Surgical Sperm Retrieval
-
Upload
sandro-esteves -
Category
Health & Medicine
-
view
738 -
download
1
Transcript of Management of Nonobstructive Azoospermia Before Surgical Sperm Retrieval
Management of NOA before Sperm Retrieval
Sandro C. Esteves, MD., PhD. Medical & Scien,fic Director, ANDROFERT Andrology & Human Reproduc,on Clinic
Campinas, BRAZIL
4th International Congress - Academy of Clinical Embryologists 18-20 September 2015, Kochi INDIA
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 2 2015
ANDROFERT
Azoospermia: the complete lack of sperm in ejaculate aEer centrifugaFon
10-15% infertile males
1-3% male population
Cooper et al. Hum Reprod Update 2009; Esteves & Agarwal, Clinics 2013
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 3 2015
ANDROFERT
Esteves et al Int Braz J Urol 2014; 40: 443-53
Goals of semen analysis are to reduce analytical error and enhance precision
Examination of pelleted semen Differentiation between ‘true’ azoospermia and cryptozoospermia
Minimum 2 analyses Transient azoospermia due to medical conditions and biological variability
Supernatant is discharged
Pellet is meticulously
examined
Centrifugation at 3,000g for 15
minutes
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 4 2015
ANDROFERT
Prognosis and management differenFally affected by type of azoospermia
ObstrucFve
Non-‐obstrucFve
Hypo-‐hypo
Spermatogenic failure
Clinical picture
FSH/LH: ñ or nl TT: low or nL
Testes: small or nl
Normal testes & endocrine profile;
Mechanical blockage
FSH/LH <1.2 mUI/mL,
Low TT, small tesFs, poor virilizaFon
Disrupted
Normal
Spermatogenesis
Esteves et al, Clinics 2011
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 5 2015
ANDROFERT
Cryptorchidism, testicular trauma, torsion, infection, radio-/chemotherapy, congenital abnormalities, systemic diseases Small testes (<15 cc; long axis <4.6 cm) Flat epididymis, palpable vas Elevated FSH levels (>7.6 mIU/ml in 90% men) Low testosterone levels (<300 ng/dl in up to 50%)
Diagnostic parameters provide >90% prediction of whether azoospermia is due
to spermatogenic failure Medical history
Physical examination
Endocrine profile
Esteves et al Clinics 2011
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 6 2015
ANDROFERT
Verza Jr & Esteves, Atlas of Human Reproduction SBRH 2013
Isolated diagnostic biopsy rarely indicated provide no definitive proof of whether sperm will be
found; may jeopardize future retrieval attempts
Differential diagnosis with obstructive azoospermia Work-up in NOA associated to maturation arrest is unrevealing
Wet examination and cryopreservation if sperm found
Hypospermatogenesis
Maturation arrest
Sertoli cell-only
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 7 2015
ANDROFERT
Frequency of azoospermia among 2,383 patients attending an Infertility Clinic
Esteves et al. Clinics 2011; 66: 691-700.
Azoospermia 35%
61%
36%
3% Hypo-hypo
OA
SF
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 8 2015
ANDROFERT
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 9 2015
ANDROFERT
Esteves et al Fertil Steril 2010; Raman & Schlegel J Urol 2003; Hopps et al. Hum Reprod 2003; Damani et al JCO 2002
Etiology category Success in finding sperm
Cryptorchidism 52-74% Post-infection 67% Torsion >50% Post-chemotherapy/RT 25-75% Genetic (KS, AZFc) 25-70% Idiopathic 50-60%
Etiology cannot determine whether or not sperm will be found within the testis
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 10 2015
ANDROFERT
FSH levels Testosterone levels
Testicular volume
elecFng candidates for SR Can biomarkers predict SR success?
Diagnostic markers reflect global testicular function but not the presence of a site of
active spermatogenesis
Verza Jr & Esteves. Fertil Steril 2011; 96 (Suppl.): S53
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 11 2015
ANDROFERT
Biopsy helpful for counseling but does not provide definitive proof of whether sperm will be found; may jeopardize future retrieval attempts
100%
40.3% 19.5%
Hypospermatogenesis Maturation Arrest Sertoli-cell only
Presence of sperm within the testicle (N=357)
Esteves & Agarwal. Asian J Androl 2014; 16: 642
Testicular histopathology
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 12 2015
ANDROFERT
Complete AZFa, AZFb or AZFa+b microdeleFons unfavorable prognosis
YCMD SR success
AZFa nil AZFb nil AZFc 50-‐70%
Krausz et al. 2014; Esteves et al. 2013; Esteves 2015
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 13 2015
ANDROFERT
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 14 2015
ANDROFERT
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 15 2015
ANDROFERT
IntervenFons to inferFle males men with SF prior to a sperm retrieval acempt
Rationale for varicocele repair Catch-up testicular growth among
adolescents following varicocele repair
Improvement in sperm parameters after varicocele repair
Abnormally-low T restored to normal levels in some men after varicocele repair
Wang et al Fertil Steril 1991; 55: 152-5; Su et al J Urol 1995; 154: 1752-5; Çayan et al J Urol 2002; 168: 929731-4; Hamada et al Nat Rev Urol 2013; 10: 26-37
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 16 2015
ANDROFERT
Among 233 men with SF and clinical varicocele, about 1/3 had motile sperm in
postoperative ejaculate
Weedin et al J Urol 2010; 183: 2309-15
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 17 2015
ANDROFERT
MaturaFon arrest and hypospermatogenesis favorable prognosis
Weedin et al J Urol 2010;183:2309-‐15
Among 233 men with SF and treated varicocele, 1/3 had moFle sperm in postop.
ejaculate
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 18 2015
ANDROFERT
Inci et al J Urol 2009;182:1500-‐5; Haydardedeoglu et al Urology 2010;75:83-‐6
§ Inci 2009 OR: 2.63
(95% CI: 1.05-‐6.60; p=0.03)
Although 2/3 remain azoospermic aEer varicocele repair, SRR is increased
§ Haydardedeoglu 2010
53 30
Treated (N=66) Untreated (N=30)
SR success (%)
61 38
Treated (N=31) Untreated (N=65)
p<0.01
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 19 2015
ANDROFERT
MedicaFon Hypogonadism (TT<300 ng/dl) in up to 50% men with SF High ITT levels essen,al for regula,ng spermatogenesis in combina,on with Sertoli cell s,mula,on by FSH
Paradoxically weak sFmulaFon of Leydig and Sertoli cells by endogenous gonadotropins Due to high baseline FSH and LH levels the rela,ve amplitudes are low
Shiraishi et al Hum Reprod 2012;27:331-‐9; Sussman et al Urol Clin N Am 2008;35:147-‐55
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 20 2015
ANDROFERT
ITT levels increase aEer hCG; sFmulatory effect on residual spermatogenic areas
Shinjo E et al Andrology 2013;1:929-‐35; Shiraishi et al Hum Reprod 2012;27:331-‐9
273
1348
Before After
ITT (ng/dl)
ITT levels increased aEer hCG-‐based therapy
Spermatogonial DNA synthesis increased
PCNA expression
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 21 2015
ANDROFERT
Testosterone and estradiol levels
<300 ng/dL
(10.4 nmol/L)
Hypogonadism category
Pure
MedicaFon algorithm at Androfert Tx aimed at boosFng T
Aromatase inhibitor (anastrozole 1mg orally
qid)
Rec-‐hCG (250 mcg SC qw); rec-‐FSH added (75 IU SC biw) if FSH levels <1.5 mIU/ml
T/E raFo <10
Aromatase hyperacFvity
T/E raFo >10 (nl)
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 22 2015
ANDROFERTEsteves Asian J Androl 2015;17:1-‐12
Shiraishi et al Hum Reprod 2012;27:331-‐9; Esteves Int Braz J Urol 2013;39:440
Medical therapy may increase SR success in men with SF
MicrodissecFon TESE Rescue ~15% of paFents with previous failed SR acempts
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 23 2015
ANDROFERT
Esteves Asian J Androl 2015;17:1-‐12
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 24 2015
ANDROFERT
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 25 2015
ANDROFERT
OpFons for sperm retrieval in spermatogenic failure
Technique Acronym Success TesFcular sperm aspiraFon TESA 15-‐50%
TesFcular sperm extracFon TESE 20-‐60%
MicrodissecFon tesFcular sperm extracFon
Micro-‐TESE 40-‐67%
Esteves et al Int Braz J Urol 2013;37:570-‐83; Deruyver et al Andrology 2014;2:20-‐4
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 26 2015
ANDROFERT
• Minimal tissue excision • Mechanical mincing • Enzymatic tissue digestion • Avoid iatrogenic damage • Lab air quality control
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 27 2015
ANDROFERT
3,412 cycles involving severe male factor inferFlity
Individualized COS strategies to retrieve 10-‐15 oocytes per treatment cycle
0% 10% 20% 30% 40% 50% 60%
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 20 25 Number of oocytes retrieved
Clinical pregnancy Live birth
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 28 2015
ANDROFERT
Conclusions Best management of NOA prior to SR includes: 1. Proper diagnosis (clinical & endocrine)
Ø DeselecFng AZF (a/b) carriers
2. IdenFficaFon of candidates to intervenFons
Ø varicocele Rx & medical Tx
3. Carry out SR ≥3 months aEer intervenFons 4. Tailored COS to retrieve 10-‐15 oocytes
ANDROLOGY AND HUMAN REPRODUCTION CLINIC - REFERRAL CENTER FOR MALE REPRODUCTION S ESTEVES, 29 2015
ANDROFERT







































![Sperm DNA Fragmentation is Significantly Increased in ... · Sperm DNA fragmentation assessment The sperm DNA damage was evaluated by Sperm Chromatin Dispersion (SCD) test [23] using](https://static.fdocuments.in/doc/165x107/5f3a6b0098469b5f937b3512/sperm-dna-fragmentation-is-significantly-increased-in-sperm-dna-fragmentation.jpg)