Management of acute graft-versus-host disease
-
Upload
christina101 -
Category
Technology
-
view
3.888 -
download
0
description
Transcript of Management of acute graft-versus-host disease

Management of acute graft-versus-host disease
Andrea Bacigalupo
Divisione Ematologia e Trapianto di Midollo, Ospedale San Martino, Genova, Italy
Summary
Acute graft-versus-host disease (GvHD) is a frequent compli-
cation of allogeneic haemopoietic stem cell transplantation
(HSCT) and donor lymphocyte infusions (DLI). Its incidence
and severity depends on several factors, such as prophylaxis
method, donor/recipient matching, intensity of the condition-
ing regimen and composition of the graft. Significant progress
has been made in recent years in understanding the pathogen-
esis of the disease, and some of these advances have been
translated into clinical trials. First-line treatment of acute GvHD
is based on corticosteroids, and produce sustained responses in
50–80% of patients depending on the initial severity. Non-
responders are offered second-line therapy, with combinations
of immunosuppressive agents, but 1-year survival is 30% in
most large trials. New strategies explored include infusion of
expanded mesenchymal stem cells (MSC), down regulation of
antigen-presenting cells (APC) and suicide gene transduced
T cells. Acute GvHD is complicated by severe immunodefi-
ciency causing life-threatening infections. To date, GvHD has
not been differentiated from the graft-versus-leukaemia effect.
The present review will discuss some of these aspects.
Keywords: graft-versus-host disease, haemopoietic stem cell
transplantation, donor lymphocyte infusion, immunosuppres-
sive therapy, mesenchymal stem cells.
Do we understand the pathogenesis of GvHD?
Although the pathogenesis of graft-versus-host disease (GvHD)
is not the aim of the present review, a few words are warranted:
indeed some of the recent advances in understanding cellular
and cytokine mechanisms leading to GvHD have been useful in
the clinic. GvHD is thought to be caused by donor T cells
reacting against host allo-antigens: this may well be the case,
but the mechanism underlying such immune reaction are quite
complex (Teshima & Ferrara, 2002a). The early work of
Ferrara and coworkers showed that inflammatory cytokines
play a crucial role in the initial, amplification and cytotoxic
phases of the disease (reviewed in Ferrara, 2002). Unfortu-
nately, it seems that inactivation of cytokines, such as tumour
necrosis factor (TNF) is not sufficient per se, and some initial
success has come at the expense of increased infectious
complications (Marty et al, 2003). More recently, the presen-
tation of target antigens by host antigen presenting cells (APC)
has been shown to be crucial for the initiation and develop-
ment of acute GvHD (Shlomchik et al, 1999): in an early
experiment, Shlomchik showed that mice with APC that were
unable to present class I-restricted peptides (grafted from b2
knock-out), but that expressed class I on target tissues, were
unable to develop acute GvHD (Shlomchik et al, 1999).
Therefore host APC participate in activating donor T cells to
kill host cells and the age of host APC seems relevant (in
keeping with the notion that older patients have more GvHD)
(Ordemann et al, 2002). The presentation of host antigens by
host APC can be further enhanced by host gamma/delta T
cells, as recently shown in the mouse (Maeda et al, 2005). The
interplay of APC, T cells and cytokines is such that, in a mouse
transplant model – with mismatch only between donor T cells
and host APC, but not between donor and host gut-donor T
cells still efficiently killed host gut cells, suggesting that tissue
destruction can be achieved with a by-stander effect (Teshima
et al, 2002b). Finally, attention has also been given to cellular
interplay leading to tolerance: Two reports merit mentioning.
Mc Donald et al (2005) dealt with cytokine-expanded myeloid
precursors regulating APC and promoting tolerance through
interleukin (IL)-10-producing regulatory T cells. Lan et al
(2001) looked directly at regulatory T cells (TREGS): mice
given lymphoid radiation and antithymocyte globulin (ATG)
were depleted of most T cells, but not of NK 1.1 T cells, and
became resistant to GvHD. The Stanford group has brought
this in to the clinic: they have shown that the combination of
total lymphoid radiation (TLI) and ATG depletes host T cells
with the exception of CD4+CD25+ TREGS: when allografted
these patients showed little or no GvHD, suggesting a
regulatory role of host TREGS on donor incoming alloreactive
T cells (Lowsky et al, 2005).
Do we understand the pathogenesis of GvHD?
Not fully: however, we have become aware of the complexity of
the disease, and we have learned to take advantage of some
developments in the lab. Further studies in the animal model
Correspondence: Dr A Bacigalupo, Divisione di Ematologia II,
Ospedale San Martino, Piazzale Rosanna Benzi, 10, Genova, Italy.
E-mail: [email protected]
review
ª 2007 The AuthorJournal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98 doi:10.1111/j.1365-2141.2007.06533.x

will possibly bring further advances in the clinic. Tolerance
may be achieved in more than one way.
Can acute GvHD be accurately graded?
The original grading system for acute GvHD was proposed by
Glucksberg et al (1974) and identified five categories of
patients (grades 0, I, II, III, IV). It is known as the
Glucksberg-Seattle criteria (GSC) and it is based on the degree
of skin, liver and gut involvement (skin rash, total serum
bilirubin and diarrhoea volume), together with a subjective
assessment of clinical status. The GSC have been widely used
for 30 years and correlate well with transplant-related mortal-
ity (TRM): a recent analysis of 4174 human leucocyte antigen
(HLA)-identical sibling transplants for chronic myeloid leuk-
aemia (CML) in first chronic phase showed that early and
long-term outcome is influenced by severity of acute GvHD as
identified by the classic GSC (Gratwohl et al, 2002). Indeed at
3 years survival was 74%, 74%, 64%, 37% and 10% for
patients with acute GvHD grades 0, I, II, III and IV
respectively. In 1997, the International Bone Marrow Trans-
plant Registry (IBMTR) designed a staging system from a large
data set of adult patients receiving an HLA identical sibling
BMT (Rowlings et al, 1997): the IBMTR Severity Index
regroups patients into five categories (0, A, B, C, D) based
on differences in TRM with a significance level of 0Æ05. Despite
good correlation of the IBMTR index with outcome, the classic
GSC is still used in most centres. Recently, we have shown that
the GSC can be further implemented by adding platelet counts
on day+50: patients with grade II acute GvHD and a platelet
count of less than 50 · 109/l had significantly higher TRM
when compared to patients with grade II GvHD and platelets
‡50 · 109/l (Dominietto et al, 2001).
Can we score GvHD?
Not well enough: however the classic GSC is still here after
three decades, suggesting it is clinically useful. The use of
laboratory values, such as platelet counts and cholinesterase, or
other clinical parameters (Lee et al, 2005) may further improve
our ability to predict the outcome of patient undergoing an
allogeneic transplant, and perhaps to modify treatment
accordingly.
Can GvHD be prevented?
HLA matching
HLA matching between donor and recipient is one of the most
powerful predictors of GvHD, together with other factors such
as age, donor/recipient sex match. Other supportive measures,
such as a sterile environment have been shown to protect
against GvHD both in animals and humans. Therefore using
a young-HLA matched, male donor, in a protected sterile
environment, is a very effective way of having little GvHD.
However, HLA-matched related donors are less common, at
least in Europe and the USA, and there is greater use of
unrelated donors or related HLA-mismatched donors. Thus
the question really is: can GvHD be prevented in less
favourable situations?
T cell depletion ex-vivo
Removal of T cells from the stem cell suspension, referred to as
T cell depletion (TCD) ex-vivo, was very popular in the 1980s,
but its use has declined over the past decade: this is because
survival, disease-free survival and transplant mortality were
not reduced, in the setting of HLA-matched grafts, when
compared with conventional unmanipulated transplants (Mar-
mont et al, 1991). One situation in which ex vivo-TCD is
essential, is 3 loci mismatched transplants: in this setting T cell
depletion must be thorough and one should not infuse more
than 5 · 104 CD3+ cells/kg of recipients weight, as shown by
Aversa et al (1998). TCD should be performed in a centre with
a dedicated programme, where different forms of T cell
removal can be explored, including physical and immunolo-
gical TCD (Martin & Kernan, 1997; Aversa et al, 1998).
T cell depletion in vivo
Treatment of the patient with T cell antibodies before the
transplant, in vivo-TCD, has a double target: it reduces the host
immune response, favouring engraftment, and downregulates
donor T cells, because the antibody is still in circulation at the
time of transplant, and thus prevents GvHD (Hows et al, 1993;
Holler et al, 1998; Baurmann et al, 1999; Zander et al, 1999;
Byrne et al, 2000; Finke et al, 2000). In vivo-TCD is indicated
in programmes involving alternative donor transplants, and is
used in many, but not all centres performing unrelated donor
grafts (Hows et al, 1993; Hansen et al, 1998; Holler et al, 1998;
Baurmann et al, 1999; Zander et al, 1999; Byrne et al, 2000;
Finke et al, 2000). In a recent randomised trial, we showed that
rabbit anti thymocyte globulin (ATG) significantly reduced the
risk of grade III–IV acute GvHD in unrelated donor
transplants (Bacigalupo et al, 2001a). However, TRM and
survival were unchanged due to a higher risk of lethal
infections in the ATG 15 mg/kg arm (Bacigalupo et al,
2001a). An update of the same study showed that ATG
provided significant protection against acute and chronic
GvHD, shortened time to terminate immunosuppression and
improved quality of life (Bacigalupo et al, 2006). Whether
different schedules of administration of ATG or different
agents may further improve results remains to be determined.
Expanding regulatory T cells (TREGS)
CD4+CD25+ immunoregulatory T cells (TREGS) can be
administered to inhibit GVHD while preserving graft-
versus-leukaemia activity after allogeneic bone marrow
transplantation in mice. Preclinical studies suggest that it is
Review
ª 2007 The Author88 Journal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98

necessary to infuse as many TREGS as conventional donor
T cells to achieve a clinical effect on GVHD (Trenado et al,
2006). How do we translate this to the clinic? The Stanford
group has designed a transplant programme consisting of
fractionated TLI (800 rads delivered in 2 weeks, 80 rads/
d ·5 ·2) and ATG (5 d) followed by allogenic unmanipulated
peripheral blood transplants (Lowsky et al, 2005), resulting in
little or no acute GvHD. A recent update of that study at the
2006 meeting of the European Group for Blood and Marrow
Transplantation (EBMT) has confirmed these results of 64
patients, half of whom received grafts from unrelated donors
(R. Lowski, unpublished observations).
Post-transplant immunosuppressive therapy
This therapy is still the conventional form of GvHD prevention
both in HLA-identical as well as unrelated-donor transplants.
It is usually based on the combination of cyclosporin A (CsA)
and short course methotrexate (MTX) on days+1, +3, +6, +11
(Storb et al, 1986; Zikos et al, 1998). The CsA dose used in the
first 10 d post-transplant may have a significant impact on
leukaemia control: in two prospective randomised trials, both
in children and in adults, low-dose CsA (1 mg/kg) was shown
to protect patients from leukaemia relapse when compared
with higher doses of CsA (3 mg/kg or 5 mg/kg) (Bacigalupo
et al, 1991; Locatelli et al, 2000). This was recently confirmed
at a 10-year follow up (Bacigalupo et al, 2001b) and should be
kept in mind especially when grafting patients at high risk of
relapse. Recently tacrolimus (FK506), a calcineurin inhibitor,
has been introduced in the prophylaxis of GvHD: 180 patients
grafted from a matched unrelated donor were randomised to
receive CsA+MTX or FK506+MTX (Nash et al, 2000). Acute
GvHD II-IV was significantly lower (51%) in FK506-treated
patients when compared with the CsA patients (70%)
(P ¼ 0Æ0002), but this did not translate in a lower risk of
chronic GvHD. The adverse events, in particular nephrotox-
icity, infections or leukaemia relapses were not significantly
different (Nash et al, 2000). There was also no difference in
survival. Therefore, both CsA+MTX and FK506+MTX com-
binations offer some protection for GvHD and have signifi-
cantly reduced the risk of severe GvHD when compared to
single agent prophylaxis (MTX or CyA alone). Mycophenolate
mofetil (MMF) has been successfully introduced for GvHD
prevention, and may substitute MTX in the standard CsA
combination, mainly because of less mucositis and overall
good tolerance (Basara et al, 2000; Nash et al, 2005; Neumann
et al, 2005).
Mesenchymal stem cells
Mesenchymal stem cell (MSC) are pluripotent stem cells
capable of generating osteoblasts, myoblats, condroblasts,
tenoblasts, adipocytes and stromal cells (Pittenger et al,
1999). There have been several reports on the immunosup-
pressive effect of MSC, both in vitro (Klyushnenkova et al,
1998; Tse et al, 2000). and in vivo (Bartholomew et al, 2002).
The co-infusion of a large number of osteoblasts together with
hemopoietic stem cells, in a mismatched mouse model,
resulted in successful engraftment and immune reconstitution
(El-Badri et al, 1998), whereas control animals died of GvHD
or rejection. A recent trial has been completed in 40 patients
with haematological malignancies, using expanded MSC from
an HLA-identical sibling, and co-infusing these cells with
a conventional unmanipulated bone marrow (BM) or periph-
eral bood (PB) transplant: the infusion of MSC was safe, and
this was the primary end point of the study (El-Badri et al,
1998); in addition, hemopoietic reconstitution was prompt.
However, the study failed to show a significant reduction in
acute or chronic GvHD when these patients were compared
with a matched pair cohort of CIBMTR patients (El-Badri
et al, 1998). MSC are now being co-transplanted in different
settings, such as cord blood or unrelated marrow grafts. One
has to note that the number of MSC or osteoblasts given
to animals (El-Badri et al, 1998) exceeds the numbers given to
humans by at least 3 logs (Lazarus et al, 2005): if we want to
achieve what has been shown in the experimental models,
perhaps we will need to escalate the number of MSC we infuse.
Inactivation of antigen presenting cells
Depleting host APC before the conditioning regimen may
reduce GvHD: in keeping with this observation, patients
receiving extracorporeal photopheresis (ECP) before the
conditioning regimen have a low incidence of GvHD (Chan
et al, 2001), because ECP may downregulate host APC
(Gorgun et al, 2001). It is also understood that broad
specificity T cell antibodies (ATG and CAMPATH), commonly
used in allotransplants, significantly deplete host APC cells. An
other way of killing APC is by using natural killer (NK) cells.
Ruggeri et al (2001) showed that elimination of host APC in
the mouse, using donor incompatible NK cells, made the
recipients resistant to GvHD (they could be infused with large
numbers of mismatched T cells, without GvHD). Thus
expanding donor NK cells may be one way of reducing GvHD,
and some centres have started to investigate whether donor NK
cells can be expanded and co-infused to reduce GvHD, and
possibly also to kill tumour cells (Aversa et al, 1998). Indeed,
in the best possible donor-recipient combination, donor NK
cells would reduce GvHD (by killing host APC), reduce
rejection (by killing host T cells) and reduce relapse (by killing
leukaemia cells). Whether we will be able to use NK cells so
cleverly remains to be determined,
Reduced-intensity conditioning regimens
Reduced-intensity conditioning (RIC) regimens were intro-
duced in the late 1970s when busulfan 8 mg/kg was used
instead of the conventional 16 mg/kg, in children with inborn
errors (Hobbs et al, 1981). These regimens are usually
associated with less severe (or delayed) acute GvHD, because
Review
ª 2007 The AuthorJournal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98 89

of the persistence of host cells (mixed chimaeras), which
counteract GvHD (Mielcarek & Storb, 2005), although early
GvHD may still occur (Mielcarek et al, 2005). There may also
be a lower level of inflammatory cytokines. RIC regimens
based on low-dose TBI (2 Gy) (Storb et al, 1999), low-dose
busulfan (Slavin et al, 1998), low-dose thiotepa (Raiola et al,
2000) low-dose melphalan (Kottaridis et al, 2000) or cyclo-
phosphamide and fludarabine (Khouri et al, 1998) are being
used widely in elderly patients up to the age of 70 years, and
the overall risk of GvHD is probably less than what would be
seen in patients of the same age with conventional intensity
regimens. Acute GvHD still remains a major obstacle after RIC
HSCT, occurring in 15% of patients in its severe form (grade
III–IV), while extensive chronic GvHD is diagnosed in 50% of
all patients (Bacigalupo, 2002). Several questions need to be
answered in this context: timing and intensity of in vivo
immunosuppression, timing of CsA discontinuation, timing of
DLI, and use of T-cell antibodies. Some regimens include anti-
T cell antibodies, such as alentuzumab (CAMPATH) (Kottar-
idis et al, 2000) or ATG (Slavin et al, 1998). It is interesting
that Russell and coworkers have taken a different approach:
they used ablative doses of intravenous busulfan combined
with fludarabine and tried to maximise GvHD prevention with
rabbit ATG in the conditioning regimen and CsA MTX for
postgraft immunosuppression (Russell et al, 2002). The pro-
gramme, designated FLU-BUP, was given up to the age of
65 years, for patients with haematological malignancies, and
yields a TRM of 4% in HLA-identical siblings and 20% in
unrelated transplants.
Anti-IL2 anti-TNF antibodies
Other monoclonal antibodies (mAbs) that interact with IL2 or
TNF have been tested in the clinical setting. Anti- CD25 mAb
seemed to delay the occurrence of GvHD; in a randomised trial
the administration of a CD25 mAb (in addition to CsA+MTX)
appeared to decrease leukaemia-free survival, in comparison to
conventional GvHD prophylaxis (Blaise et al, 1995).
A humanised CD25 mAb, assessed in a double-blind,
placebo-controlled randomised study, involving a total of
210 patients, failed to prevent GvHD or improve the outcome
of unrelated HSCT recipients (Anasetti et al, 1995). A mAb
neutralising TNF-a has also been tested in 21 patients as
GvHD prophylaxis: in a prospective trial Holler et al (2002)
showed that GvHD could be delayed (by 10 d), although the
overall grading was similar to controls.
Can GvHD be prevented?
The answer is clearly yes, and there has been a progressive
decline in the severe form of acute GvHD (III–IV) in the last
decade (Bacigalupo et al, 2004). Whether reduction of GvHD
produces improved survival, is a more difficult question.
However, this should not discourage further studies on GvHD
prevention, because if survival is comparable, morbidity is
clearly lower if patients do not experience acute or chronic
GvHD.
Can acute GvHD be treated?
First-line treatment
Corticosteroids Corticosteroids are used as first-line therapy: in
a study of 443 patients who received prednisone 60 mg/m2 for
14 d as first-line therapy, followed by an 8-week taper, an
overall improvement was observed in 55% of the patients with
durable (‡28 days) complete responses in 35% (Blazar, 2002).
The probability of survival at 1 year after initiation of therapy
was 53%: favourable predictors of survival were younger
patient age, HLA-identical sibling donor and GvHD
prophylaxis other than ex-vivo T cell depletion (Blazar,
2002). The authors of this important study concluded that
steroids provide an active but inadequate therapy for acute
GvHD, especially in patients with severe GvHD, and that more
effective prophylaxis for mismatched and unrelated donor
transplants is needed. Unfortunately. There is no evidence that
more aggressive first-line therapy is beneficial: the Italian
Group for Marrow Transplantation (GITMO) could not show
an advantage of high-dose steroids (10 mg/kg of 6-MPred)
over conventional 2 mg/kg MPred, with a transplant mortality
at 1 year of 30% in both groups (Van Lint et al, 1998).
A randomised study comparing steroids + ATG versus steroids
alone came to the same conclusion (Cragg et al, 2000). Two
additional observations were made in the GITMO study: (i)
despite the very early day of randomization (median day +12
from transplant), high dose MPred did not prevent
progression towards grade III–IV GvHD and (ii) responders
to 5 d of 6MPred 2 mg/kg had a significantly lower TRM
(16%) when compared with non-responders (46%) (Van Lint
et al, 1998). We have confirmed this result in a more recent
study (Van Lint et al, 2006).
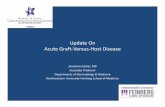
Thus, primary treatment of acute GvHD should be pred-
nisone or 6MPred 2 mg/kg/d for 5 d (Fig 1): responsive
patients should taper steroid therapy. An IBMTR survey
confirmed that a 5-d course is sufficient to identify steroid-
refractory acute GvHD (Hsu et al, 2001). There may be less
agreement on criteria to define response on day+5 or day+7: it
is unlikely that patients will be free of GvHD. The most
common situation will be reduction of clinical signs of acute
GvHD, which may allow reduction of the 6MPred dose
(Fig 1): indeed in two consecutive studies we found it very
useful to identify day+5 responders as those patients who were
considered eligible for MPred dose tapering (Cragg et al, 2000;
Van Lint et al, 2006). The probability of response will be
higher for patients who have limited acute GvHD on day 0 of
treatment (Van Lint et al, 2006). Patients not responding on
day+5 or day+7 could not reduce their dose of steroidsand
were eligible for second-line treatment (Fig 1). Transplant
mortality is higher (as expected) in non-responders as
compared to day+5 responders, and this indicates that
Review
ª 2007 The Author90 Journal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98

strategies for second-line therapy can be designed very early in
the course of the disease.
Second-line treatment
A large number of studies have been performed for patients
not responding to 2 mg/kg of MPred (Fig 1). Most of these
were phase II uncontrolled studies, showing some degree of
response with the use of a large variety of agents. Very few were
prospective randomised trials, and these have failed to show
any advantage of experimental treatment over standard steroid
therapy.
Anti-thymocyte globulin (ATG) Anti-thymocyte globulin is one
treatment option for steroid-refractory patients, and some
encouraging results have come from phase II trials (Roy et al,
1992; Aschan, 1994), especially when ATG was given early after
the diagnosis of GvHD (MacMillan et al, 2002). However, we
are lacking evidence that ATG improves survival. In a recent
prospective randomised trial the Italian group GITMO has
been unable to confirm that ATG is beneficial as a second-line
therapy of steroid-refractory acute GvHD (Van Lint et al,
2006): 61 patients not responding to 5 d of MPred 2 mg/kg,
were randomised to receive MPred 5 mg/kg/d for 10 d, alone
(n ¼ 34) or in combination with rabbit ATG (n ¼ 27). The
two groups were balanced for clinical and GvHD characteristic.
One-month after randomisation 26% had a complete
response, 25% a partial response, 33% stable GvHD, 10%
worsened and 8% had died: there was no significant difference
in response, TRM and survival between the non-ATG and
ATG group (Van Lint et al, 2006). Five-year actuarial survival
was 36% and 34% for controls and ATG patients.
Therefore, although ATG can induce a significant response
in GvHD patients, survival is unchanged when compared with
patients not receiving ATG: clinical response of GvHD does
not mean improved survival, and responders may still die of
infections and other complications, as suggested in a recent
review (Antin et al, 2004).
Interleukin 2 receptor antibodies
There are several monoclonal antibodies to IL2 (reviewed in
Antin et al (2004): denileukin difitox (Ontac), inolinomab
(Leukotac), Basiliximab (Simulect), Daclizumab (zenapax).
They have all shown efficacy in steroid-resistant acute GvHD
(Antin et al, 2004). Nevertheless, infections remain a serious
problem: is this due to the fact that patients come to
monoclonal antibody therapy after failing several lines of
treatment? Perhaps early administration of IL2R antibodies
would prove more effective. A large prospective randomised
trial is ongoing within the National Marrow Donor Program,
testing, among other agents, an IL2 receptor antibody.
Anti -CD147 monoclonal antibody
Deeg et al (2001) have reported a pilot study on the use of
anti-CD147 (a neurothelin member of the immunoglobulin
superfamily which is upregulated on activated T and B cells):
27 patients with GvHD entered this study and 51% were
considered as responders, including 25% complete responses.
Survival at 6 months was 44% (Deeg et al, 2001).
TNF antibodies
Tumour necrosis factor is of one the inflammatory cytokines
mediating cellular cytotoxicity. TNF can be downregulated by
steroids, pentoxifilline, transforming-growth factor beta
(TGFB) and IL4. Antibodies to TNF (infliximab) or to the
TNFreceptor (etanercept) have been developed and used both
in first- and second-line treatment of acute GvHD (Marty et al,
2003; Couriel et al, 2004; Uberti et al, 2005). Responses are
seen, some patients clear their symptoms rapidly, but infections
remain an issue (Marty et al, 2003).
Other agents
Other agents, such as MMF are being tested with some success:
MMF has a good efficacy profile, is well tolerated in general
and may prove useful in sparing steroids and steroid-associ-
ated complications (Antin et al, 2004).
Pre-emptive treatment
We have previously shown that patients at high risk of GvHD
and TRM can be identified on day +7 following an allogeneic
Methylprednisolone2 mg/kg/dx5 or 7 d
Response
1st line treatmentDay 0
Day 7
2nd line treatment
Taper MPred
No response
Diagnosis ofAcute GvHD
MPred 2–5 mg/kgATG, anti-IL2, anti-CD147TNF antibodiesMMF, ECPMesenchymal Stem CellsOther
Fig 1. Flow chart of events after the diagnosis of acute GvHD is made
(day 0). First-line treatment consists of methylprednisolone (Mpred)
2 mg/kg/d i.v. for 5 or 7 d. On day 7, responders are assigned to
a steroid-taper programme. Non-responders receive second-line
therapy: there are a number of options. Continue MPred alone; add
antithymocyte globulin (ATG), monoclonal antibodies to interleukin
2 (IL2), tumour necrosis factor (TNF), CD147, add extracorporeal
photopheresis (ECP). The most promising option today seems the
addition of mesenchymal stem cells (MSC).
Review
ª 2007 The AuthorJournal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98 91

bone marrow transplant (BMT), based on serum bilirubin and
blood urea nitrogen levels (Bacigalupo et al, 1999): we have
recently revised the scoring system with the inclusion of day+7
cholinesterase, gammaglutamyltransferase, total protein to-
gether with cell dose and donor type (Sormani et al, 2003).
One possible approach to reduce the risk of GvHD and TRM,
is pre-emptive treatment before the disease develops. In a pilot
study, we tested the feasibility of this approach in patients
undergoing an alternative donor HSCT: the risk of severe
GvHD and the actuarial 1 year TRM was reduced in the ATG
treated patients (Bacigalupo et al, 2001c). This is in keeping
with a previous randomised trial, published some years ago,
showing that early administration of ATG after an HLA-
identical sibling transplant, could significantly reduce the risk
of acute GvHD (Ramsay et al, 1982). Whether this will
translate in survival advantage is being now tested in
a prospective multicenter trial by GITMO.
Cellular therapy of GvHD
This section includes the use of MSC, ECP directed against
APC, and suicide gene transduced T cells
Suicide gene transduction of T cells This approach is based on
transducing T cells with a gene, such as herpes simplex virus
thymidine kinase (HSV-TK) which renders them susceptible to
killing by ganciclovir, provided the cell is also dividing. The
T cells are infused into the host and when GvHD develops,
ganciclovir is given, killing only transduced T cells. This system
requires efficient gene transduction and the ability to select
transduced cells. It has been implemented in humans and
animals models with some positive results, although anectotal
(Bonini et al, 1997). The model is based on the hypothesis,
that established GvHD can be turned off by killing alloreactive
T cells, although there is scanty evidence that this can be
achieved: the activation system is very complex, and by the
time it is established there are many cell types (both of donor
and recipient origin) and many cytokines involved, often with
opposite actions. During induction phase the administration
of IL12 inhibits GvHD (Sykes et al, 1995). If, in the same
mouse model, IL12 was given later after transplant, there was
enhancement of GvHD by induction of host-derived
interferon-c (IFNc) (Sykes et al, 1999). T cells from IFNcknock-out mice, surprisingly, caused a more virulent GvHD,
suggesting a protective effect of IFNc (Murphy et al, 1998). In
a different mouse P¤ F1 model, the lack of IFNc T cells
delayed GvHD (Minasi et al, 1993). These results outline the
complex pathogenesis of GvHD and the multiple effectors
involved, which may vary according to the animal model
chosen. If this is the case, can GvHD be turned off by killing
T cells, and if so, which T cells need to be killed? Although
suicide gene transduction was reported almost 10 years ago,
and despite some pilot phase I/II studies, it has not been used
in the clinic as a standard approach for acute GvHD
prevention and treatment: it faces numerous problems,
including logistic, technical and conceptual. For the time
being, it remains an interesting investigational tool.
Mesenchymal stem cells There has been great interest in the use
of MSC for treatment of acute GvHD in the past few years
(Ringden et al, 2006): at the EBMT meeting 2006 we presented
a cooperative report on patients treated in Huddinge, Genova
and Pavia, and we further updated this report at the 2006 ASH
meeting (Le Blanc et al, 2006): 40 patients with grades III–IV
acute GvHD receiving MSC were evaluated. The median MSC
dose was 1Æ0 (range 0Æ4–9) 106 cells/kg body weight of the
recipient. No side-effects were seen after MSC infusions.
Nineteen patients received one dose, 19 patients received two
doses, two patients received three and five doses, respectively.
MSC donors were HLA-identical siblings in five cases,
haploidentical in 19 cases and third-party HLA-mismatched
in 41 cases. Among the 40 patients treated for severe acute
GvHD, 19 had complete responses, nine showed improvement,
seven patients did not respond, four had stable disease and one
patient was not evaluated due to short follow-up. Twenty-one
patients were alive between 6,weeks up to 3Æ5 years after
transplantation, Nine of whom had extensive chronic GvHD.
These results suggest that immunomodulatory and tissue
repairing effects of MSC should be further explored as
treatment of severe acute GvHD in prospective randomised
trials, especially as there have been negative reports in the
experimental model (Sudres et al, 2006).
Extracorporeal photopheresis
Extracorporeal photopheresis has been mostly used in patients
with chronic GvHD, and significant responses have been seen
in a proportion of patients (Couriel et al, 2006). A randomised
study has been completed in chronic GvHD patients, and
should be available for definitive analysis this year (Greinix
et al, 2006a). Recent reports have been published, of ECP used
for acute GvHD: the procedure is invasive, requires a dedicated
team at the Blood Bank and responses are not seen before
12 weeks, therefore requiring long-term supportive care (Gar-
ban et al, 2005; Greinix et al, 2006b). However, given the
current poor results with second-line therapy, waiting
12 weeks for a response would not be the greatest of problems.
Greinix et al (2006b)) reported an 82% complete response rate
for patients with severe skin acute GvHD treated with ECP and
steroids, 61% for gut involvement and 61% for liver involve-
ment. A randomised trial comparing prednisone + ECP versus
prednisone alone has been activated this year.
Can GvHD be treated ?
The answer is a cautious ‘Yes’. Most events occur very early in
the course of the transplant. First-line therapy with conven-
tional dose steroids (1–2 mg/kg/d) can be successfully given to
over half of affected patients. Response depends on the severity
of GvHD and organ involvement. If patients respond, their
Review
ª 2007 The Author92 Journal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98

transplant mortality is relatively low; if they don’t respond to
first-line treatment, their transplant mortality is high (possibly
exceeding 60%). Mortality after second-line therapy has not
been reduced in the last three decades: patients do respond to
second-line therapy and GvHD severity is diminished, but the
patients may still succumb to infectious complications. New
agents, antibodies or intensified immunosuppression have not
changed GvHD-related mortality, cellular therapy holds
promise. The important take-home message is: whatever you
decide to do, please enter your patients in to a clinical trial
(Bolanos-Meade & Vogelsang, 2005): this is the only way we
can expect to make progress in the near future.
Can we improve immune-reconstitution ?
Immune reconstitution remains a significant problem follow-
ing allogeneic stem cell transplantation and several studies
have analysed this. The number of NK cells, as monitored by
CD56 or CD16 expression on peripheral blood lymphocytes,
rose rapidly after transplant, and returned quickly to the
normal range while CD8+ cells frequently remained high
(Dokhelar et al, 1981). There is a strong imbalance of helper/
suppressor cells, first described many years ago (Bacigalupo
et al, 1981), which still needs to be fully understood. It may be
associated with immune reconstitution or with alloreactivity
(Noel et al, 1978; Paulin et al, 1987; Barrett et al, 2003): the
former seems more probable, since the CD4/CD8 ratio is not
a good indicator of acute GvHD. Other factors associated with
poor immune recovery also predict GvHD: older age (Seddik
et al, 1984), unrelated donors (Small et al, 1999) and of course
steroid therapy given to treat GvHD (Douek et al, 2000). The
thymus plays an important role in reconstitution of T-cell
immunity and increasing patient age has an adverse effect on
the regeneration of naive CD4+ T cells, probably due to age-
related thymic involution: these observations were confirmed
by TCR rearrangement excision circlet (TREC) assay to
measure thymic output (Douek et al, 1998, 2000; ). Attempts
to boost immune reconstitution by IL7 or IL7-engeneered cells
have been reported (Li et al, 2006), but we have not yet seen
these studies translated in the clinic. Recently, keratinocyte
growth factor (KGF) has been shown to promote immune
reconstitution after HSCT in the animal model (Min et al,
2002): trials using KGF are underway in clinical allograft
programs.
Immune reconstitution is inversely correlated with the
severity of GvHD: the more severe the disease the worse the
immune recovery (Sale et al, 1992). The situation is worsened
by treatment of GvHD with steroids, antibodies and other
suppressive manoeuvres. Attempts to manipulate immune
recovery with cytokines have failed so far, although IL7 holds
promise. Infections are a frequent and often lethal complica-
tion: they include viral, fungal and bacterial infections in
patients with GvHD. Discussing these complications is outside
the scope of the present review, however, monitoring and early
treatment of infections should be a major part of standard
protocols or prospective trials. This is also relevant because of
the many old and new agents available to treat cytomegalovirus
(CMV), Epstein–Barr virus (EBV), aspergillus and vancomy-
cin-resistant enterococci.
We can not leave this section without mentioning the
elegant studies, pursued by several groups, in expanding
antigen-specific T cells (Peggs et al, 2001; Rauser et al, 2004;
Perruccio et al, 2005; Bollard et al, 2006; Riddell et al, 2006):
immunity to CMV, EBV and aspergillus has been successfully
transferred with expanded antigen-specific T cells, with no
GvHD, and with clearance of the infection. A very powerful
proof-of-principle indeed. Thus the technology is now estab-
lished, but is the cost and the laboratory resources affordable
for most transplant centres? Possibly not, but developing this
technology should advance our ability to manipulate the
immune system, and this is important for the management of
transplants, and possibly also for the treatment of tumours.
Is acute GVHD influenced by stem cell source?
What about the three stem cell sources: PB, BM, cord blood
(CB). They are listed here in the order of current ‘preference’,
because numbers do represent what happens every day in our
centres. The last EBMT survey told us that allogeneic PB is the
preferred source, followed by BM and CB. The influence on
acute and chronic GvHD is probably also falls in the same
order; PB, BM, CB.
There are four large international randomised studies that
used BM or PB as the source of stem cells (Blaise et al, 2000;
Bensinger et al, 2001; Couban et al, 2002; Schmitz et al, 2002).
Acute GvHD grade III–IV was similar in three studies, and
significantly increased in PB recipients in one study (Schmitz
et al, 2002). It is therefore reasonable to say that acute GvHD
was rather comparable in patients receiving allogeneic BM or
PB cells, although chronic GvHD was significantly increased in
almost all studies. Three recent publications have set the stage
for HLA-identical sibling CB transplants (Rocha et al, 2000)
and for unrelated CB transplants in children (Rocha et al,
2001) and in adults (Laughlin et al, 2001). Common to these
three publications is the low risk of acute and chronic GvHD
for patients receiving CB transplants: in the HLA-identical
study, the risk of acute GvHD was 0Æ41 for CB when compared
with BM (P ¼ 0Æ001) and for chronic GvHD the risk was 0Æ35
(P ¼ 0Æ02).
But, perhaps comparing unmanipulated PB, BM and CB is
not the right question at present: efforts should be made to
optimise programs involving each of these stem cell sources:
we will then find patients who might benefit from the different
impact these stem cell sources have on GvHD and outcome.
Conclusions
Treatment of established GvHD is complex and has not made
major advances in the last decade. Possibly we treat our
patients too late, when tissue damage has already taken place
Review
ª 2007 The AuthorJournal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98 93

and cytokine production by activated donor T cells and
autologous macrophages can proceed undisturbed. It would
seem that acute GvHD is, to a certain extent, self-programmed,
since very early treatment with high dose corticosteroids and/
or ATG does not modify the natural course of the disease. Over
the last three decades we have considerably reduced the risk of
acute GvHD and understood how to prevent it by modifying
the transplant program and the stem cell source: we now need
to improve our ability to predict GvHD and develop new
strategies of early treatment.
References
Anasetti, C., Lin, A., Nademanee, A., Gluckman, E., Messner, H.,
Beatty, P., Chauncey, T., Jacobsen, N., Chao, N., Powles, R., Territo,
M., Walker, I., Davis, J. & Light, S. (1995) A phase II/III randomized
double blind, placebo-controlled multicentre trial of humanised
anti-Tac for prevention of acute graft-versus-host disease in recip-
ients of marrow transplantats from unrelated donors. Blood,
86(Suppl. 1), 621a.
Antin, J.H., Chen, A.R., Couriel, D.R., Ho, V.T., Nash, R.A. & Weis-
dorf, D. (2004) Novel approaches to the therapy of steroid resistant
acute graft versus host disease. Biology of Blood and Marrow
Transplantation, 10, 655–668.
Aschan, J. (1994) Treatment of moderate to severe acute GvHD:
a retrospective analysis. Bone Marrow Transplantation, 14, 601–
607.
Aversa, F., Tabilio, A., Velardi, A., Cunningham, I., Terenzi, A., Falz-
etti, F., Ruggeri, L., Barbabietola, G., Aristei, C., Latini, P., Reisner,
Y. & Martelli, M.F. (1998) Treatment of high-risk acute leukemia
with T-cell-depleted stem cells from related donors with one fully
mismatched HLA haplotype. New England Journal of Medicine, 339,
1186–1193.
Bacigalupo, A. (2002) Second EBMT Workshop on reduced intensity
allogeneic hemopoietic stem cell transplants (RI-HSCT). Bone
Marrow Transplantation, 29, 191–195.
Bacigalupo, A., Mingari, M.C., Moretta, L., Podesta, M., Van Lint,
M.T., Piaggio, G., Raffo, M.R. & Marmont, A. (1981) Imbalance of
T-cell subpopulations and defective pokeweed mitogen-induced B-
cell differentiation after bone marrow transplantation in man.
Clinical Immunology and Immunopathology, 20, 137–145.
Bacigalupo, A., van Lint, M.T., Occhini, D., Gualandi, F., Lamperelli,
T., Sogno, G., Tedone, E., Frassoni, F., Tong, J. & Marmont, A.M.
(1991) Increased risk of leukemia relapse with high-dose cyclos-
porine A after allogeneic marrow transplantation for acute leukemia.
Blood, 77, 1423–1428.
Bacigalupo, A., Oneto, R., Bruno, B., Soracco, M., Lamparelli, T.,
Gualandi, F., Occhini, D., Raiola, A.M., Mordini, N., Berisso, G.,
Bregante, S., Dini, G., Lombardi, A., Van Lint, M.T. & Brand, R.
(1999) Early predictors of transplant-related mortality (TRM) after
allogeneic bone marrow transplants (BMT): blood urea nitrogen
(BUN) and bilirubin. Bone Marrow Transplantation, 24, 653–659
Bacigalupo, A., Lamparelli, T., Bruzzi, P., Guidi, S., Alessandrino, P.E.,
di Bartolomeo, P., Oneto, R., Bruno, B., Barbanti, M., Sacchi, N.,
van Lint, M.T. & Bosi, A. (2001a) Antithymocyte globulin for graft-
versus-host disease prophylaxis in transplants from unrelated do-
nors: 2 randomized studies from Gruppo Italiano Trapianti Midollo
Osseo (GITMO). Blood, 98, 2942–2947.
Bacigalupo, A., Lamparelli, T., Gualandi, F., Bregante, S., Raiola, A.M.,
Di Grazia, C., Dominietto, A., Romagnani, C., Occhini, D., Frassoni,
F. & van Lint, M.T. (2001b) Increased risk of leukemia relapse with
high-dose cyclosporine A after allogeneic marrow transplantation
for acute leukemia: a 10 year follow up of a randomized study.
Blood, 98, 3174–3175.
Bacigalupo, A., Oneto, R., Lamparelli, T., Gualandi, F., Bregante, S.,
Raiola, A.M., Di Grazia, C., Dominietto, A., Romagnani, C., Bruno,
B., Van Lint, M.T. & Frassoni, F. (2001c) Pre-emptive therapy of
acute graft versus host disease: a pilot study with anti-thymocyte
globulin (ATG). Bone Marrow Transplantation, 28, 1093–1096.
Bacigalupo, A., Soriani, M.P., Lamparelli, T., Gualandi, F., Occhini, D.,
Bregante, S., Raiola, A.M., di Grazia, C., Dominietto, A., Tedone, E.,
Piaggio, G., Podesta, M., Bruno, B., Oneto, R., Lombardi, A.,
Frassoni, F., Rolla, D., Rollandi, G., Viscoli, C., Ferro, C., Garbar-
ono, L. & Van Lint, M.T. (2004) Reducing transplant-related mor-
tality after allogeneic hematopoietic stem cell transplantation.
Haematologica, 89, 1238–1247.
Bacigalupo, A., Lamparelli, T., Barisione, G., Bruzzi, P., Guidi, S.,
Alessandrino, P.E., di Bartolomeo, P., Oneto, R., Bruno, B., Sacchi,
N., van Lint, M.T., Bosi, A. Gruppo Italiano Trapianti Midollo
Osseo (GITMO). (2006) Thymoglobulin prevents chronic graft-
versus-host disease, chronic lung dysfunction, and late transplant-
related mortality: long-term follow-up of a randomized trial in
patients undergoing unrelated donor transplantation. Biology of
Blood and Marrow Transplantation, 12, 560–565.
Barrett, A.J., Rezvani, K., Solomon, S., Dickinson, A.M., Wang, X.N.,
Stark, G., Cullup, H., Jarvis, M., Middleton, P.G. & Chao, N. (2003)
New developments in allotransplants immunology. Hematology
American Society of Hematology. Education Program, 102, 350–
371.Review.
Bartholomew, A., Sturgeon, C., Siatskas, M., Ferrer, K., McIntoch, K.,
Patil, S., Hardy, W., Devine, S., Ucker, D., Deans, R., Mosely, A.M.,
Hoffman, R. & Nchleunng, M. (2002) Mesenchymal stem cells
suppress lymphocyte proliferation in vitro and prolong skin graft
survival in vivo. Experimental Hematology, 30, 42–48.
Basara, N., Blau, W.I., Kiehl, M.G., Schmetzer, B., Bischoff, M.,
Kirsten, D., Gunzelmann, S. & Fauser, A.A. (2000) Mycophenolate
mofetil for the prophylaxis of acute GVHD in HLA-mismatched
bone marrow transplant patients. Clinical Transplantation, 14, 121–
126.
Baurmann, H., Bonnefoy-Berard, N., Thiede, C. Oelschlagel, U., Eh-
ninger, G., Revillard, J.P. & Schwerdtfeger, R. (1999) Clinical and
biological effects of ATG used as part of the conditioning in matched
unrelated donor (MUD) transplantation. Blood, 94, 134a.
Bensinger, W.I., Martin, P.J., Storer, B., Clift, R., Forman, S.J., Negrin,
R., Kashyap, A., Flowers, M.E., Lilleby, K., Chancey, T.R., Storb, R.
& Appelbaum, F.R. (2001) Transplantation of bone marrow as
compared with peripheral-blood cells from HLA-identical relatives
in patients with hematologic cancers. New England Journal of
Medicine, 344, 175–181.
Blaise, D., Olive, D., Michallet, M., Marit, G., Leblond, V. & Mar-
aninchi, D. (1995) Impairment of leukaemia-free survival by addi-
tion of interleukin-2- receptor antibody to standard graft-versus-
host prophylaxis. Lancet, 345, 1144–1146
Blaise, D., Kuentz, M. & Container, C. (2000) Randomized trial of
bone marrow versus lenograstim primed blood cell allogeneic
transplantation. Journal of Clinical Oncology, 18, 537–546.
Review
ª 2007 The Author94 Journal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98

Blazar, B.R. (2002) Response of 443 patients to steroids as primary
therapy for acute GvHD: comparison of grading systems. Biology of
Blood and Marrow Transplantation, 8, 387–394.
Bolanos-Meade, J. & Vogelsang, G.B. (2005) Novel strategies for
steroid-refractory acute graft-versus-host disease. Current Opinion in
Hematology, 12, 40–44.Review.
Bollard, C.M., Gottschalk, S., Huls, M.H., Molldrem, J., Przepiorka, D.,
Rooney, C.M. & Heslop, H.E. (2006) In vivo expansion of LMP
1- and 2-specific T-cells in a patient who received donor-derived
EBV-specific T-cells after allogeneic stem cell transplantation.
Leukemia & Lymphoma, 47, 837–842.
Bonini, C., Ferrari, G., Verzeletti, S., Servida, P., Zappone, E., Ruggieri,
L., Ponzoni, M., Rossini, S., Mavilio, F., Traversari, C. & Bordignon,
C. (1997) HSV-TK gene transfer into donor lymphocytes for control
of allogeneic graft-versus-leukemia. Science, 276, 1719–1724.
Byrne, J.L., Stainer, C., Cull, G., Haynes, A.P., Bessell, E.M., Hale, G. &
Waldmann, H. (2000) The effect of the serotherapy regimen used and
the marrow cell dose received on rejection, graft-versus-host disease
and outcome following unrelated donor bone marrow transplanta-
tion for leukaemia. Bone Marrow Transplantation, 25, 411–417.
Chan, G., Foss, F.M., Roberts, T., Sprague, K., Schenkein, D. & Miller,
K.B. (2001) Decreased acute and chronic graft versus host disease
with early full donor engraftment following a pentostatin-based
preparative regimen for allogeneic bone marrow transplant in high-
risk patients. Blood, 98, 383a, (abstr. 1612).
Couban, S., Simpson, R., Barnett, M.J. & Bredeson, C. (2002) A ran-
domized multicenter comparison of bone marrow and peripheral
blood in recipients of matched sibling allogeneic transplants for
myeloid malignancies. Blood, 100, 1525–1528.
Couriel, D., Saliba, R., Hicks, K., Ippoliti, C., de Lima, M., Hosing, C.,
Khouri, I., Andersson, B., Gajewski, J., Donato, M., Anderlini, P.,
Kontoyiannis, D.P., Cohen, A., Martin, T., Giralt, S. & Champlin, R.
(2004) Tumor necrosis factor alpha blockade for the treatment of
acute GVHD. Blood, 104, 649–654.
Couriel, D.R., Hosing, C., Saliba, R., Shpall, E.J., Anderlini, P., Rhodes,
B., Smith, V., Khouri, I., Giralt, S., de Lima, M., Hsu, Y., Ghosh, S.,
Neumann, J., Andersson, B., Qazilbash, M., Hymes, S., Kim, S.,
Champlin, R. & Donato, M. (2006) Extracorporeal photo-
chemotherapy for the treatment of steroid-resistant chronic GVHD.
Blood, 107, 3074–3080.
Cragg, L., Blazar, B.R., Defor, T., Kolatker, N., Miller, W., Kersey, J.,
Ramsay, M., McGlave, P., Filipovich, A. & Weisdorf, D. (2000) A
randomized trial comparing prednisone with antithymocyte globu-
lin/prednisone as an initial systemic therapy for moderately severe
acute graft-versus-host disease. Biology of Blood and Marrow
Transplantation, 6, 441–447
Deeg, H.J., Blazar, B.R., Bolwell, B.J., Long, G.D., Schuening, F.,
Cunningham, J., Rifkin, R.M., Abhyankar, S., Briggs, A.D., Burt, R.,
Lipani, J., Roskos, L.K., White, J.M., Havrilla, N., Schwab, G. &
Heslop, H.E. (2001) Treatment of steroid-refractory acute graft-
versus-host disease with anti-CD147 monoclonal antibody ABX-
CBL. Blood, 98, 2052–2058.
Dokhelar, M.C., Wiels, J., Lipinski, M., Tetaud, C., Devergie, A.,
Gluckman, E. & Tursz, T. (1981) Natural killer cell activity in hu-
man bone marrow recipients. Early reappearance of peripheral
blood natural killer activity in graft versus host disease. Transplan-
tation, 31, 61–65.
Dominietto, A., Raiola, A.M., van Lint, M.T., Lamparelli, T., Gualandi,
F., Berisso, G., Bregante, S., Frassoni, F., Casarino, L., Verdini, S. &
Bacigalupo, A. (2001) Factors influencing haematological recovery
after allogeneic haemopoietic stem cell transplants: graft-versus-host
disease, donor type, cytomegalovirus infections and cell dose. British
Journal of Haematology, 112, 219–227.
Douek, D.C., McFarland, R.D., Keiser, P.H., Gage, E.A., Massey, J.M.,
Haynes, B.F., Polis, M.A., Haase, A.T., Feinberg, M.B., Sullivan, J.L.,
Jamieson, B.D., Zack, J.A., Picker, L.J. & Koup, R.A. (1998) Change
in thymic function with age and during the treatment of HIV in-
fection. Nature, 396, 690–695.
Douek, D.C., Vescio, R.A., Betts, M.R., Brenchley, J.M., Hill, B.J.,
Zhang, L., Berenson, J.R., Collins, R.H. & Koup, R.A. (2000) As-
sessment of thymic output in adults after haematopoietic stem-cell
transplantation and prediction of T-cell reconstitution. Lancet, 355,
1875–1881.
El-Badri, N.S., Wang, B.Y. & Good, R.A. (1998) Osteoblast promote
engraftment of allogeneic hematopoietic stem cells. Experimental
Hematology, 26, 110–114.
Ferrara, J.L. (2002) Cellular and cytokine effectors of acute graft versus
host disease. International Journal of Hematology, 76(Suppl. 1),
195–198.
Finke, J., Bertz, H., Schmoor, C., Veelken, H., Behringer, D., Wasch, R.,
Kunzmann, R., Heidecker, L., Lang, H., Meyer-Konig, U. & Mer-
telsmann, R. (2000) Allogeneic bone marrow transplantation from
unrelated donors using in vivo anti-T-cell globulin. British Journal of
Haematology, 111, 303–313.
Garban, F., Drillat, P., Makowski, C., Jacob, M.C., Richard, M.J.,
Favrot, M., Sotto, J.J., Bensa, J.C. & Cahn, J.Y. (2005) Extracorporeal
chemophototherapy for the treatment of graft-versus-host disease:
hematologic consequences of short-term, intensive courses. Hae-
matologica, 90, 1096–1101.
Glucksberg, H., Storb, R., Fefer, A., Buckner, C.D., Neiman, P.E., Clift,
R.A., Lerner, K.G. & Thomas, E.D. (1974) Clinical manifestations of
graft-versus-host disease in human recipients of marrow from
HL-A-matched sibling donors. Transplantation, 18, 295–304.
Gorgun, G., Alcindor, T., Rao, R. & Foss, F. (2001) Immunologic
mechanism of extracorporeal photochemotherapy (ECP) in chronic
GVHD. Blood, 98, 650a, (abstr. 2729).
Gratwohl, A., Brand, R., Apperley, J., van Biezen, A., Bandini, G.,
Devergie, A., Schattenberg, A., Frassoni, F., Guglielmi, C., Iacobelli, S.,
Michallet, M., Kolb, H.J., Ruutu, T. & Niederwieser, D. (2002) Graft-
versus-host disease and outcome in HLA-identical sibling trans-
plantations for chronic myeloid leukemia. Blood, 100, 3877–3886.
Greinix, H.T., Socie, G., Bacigalupo, A., Holler, E., Edinger, M.G.,
Apperley, J.F., Schwarz, T., Ullrich, S.E., Albert, M.L., Knobler, R.M.,
Peritt, D. & Ferrara, J.L. (2006a) Assessing the potential role of
photopheresis in hematopoietic stem cell transplant. Bone Marrow
Transplantation, 38, 265–273.
Greinix, H.T., Knobler, R.M., Worel, N., Schneider, B., Schneeberger,
A., Hoecker, P., Mitterbauer, M., Rabitsch, W., Schulenburg, A. &
Kalhs, P. (2006b) The effect of intensified extracorporeal photo-
chemotherapy on long-term survival in patients with severe acute
graft-versus-host disease. Haematologica, 91, 405–408.
Hansen, J.A., Gooley, T.A., Martin, P.J., Appelbaum, F., Chauncey,
T.R., Clift, R.A., Petersdorf, E.W., Radich, J., Sanders, J.E., Storb,
R.F., Sullivan, K.M. & Anasetti, C. (1998) Bone marrow transplants
from unrelated donors for patients with chronic myeloid leukemia.
New England Journal of Medicine, 338, 962–968.
Hobbs, J.R., Barrett, A.J., Chambers, D., James, D.C.O., Hugh-Jones,
K., Byrom, N., Henry, K. & Lucas, C.F. (1981) Reversal of clinical
Review
ª 2007 The AuthorJournal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98 95

features of hurler’s disease and biochemical improvement after
treatment by bone marrow transplantation. Lancet, 3, 709–712.
Holler, E., Ledderose, G., Knabe, H., Muth, A., Gunther, C., Wilmanns,
W. & Kolb, H.J. (1998) ATG serotherapy during pre-transplant
conditioning in unrelated donor BMT: dose-dependent modulation
of GVHD. Bone Marrow Transplantation, 21, 105a.
Holler, E., Kolb, H.J., Mittermuller, J., Kaul, M., Ledderose, G., Duell,
Th., Seeber, B., Schleuning, M., Hintermeier-Knabe, R., Ertl, B.,
Kempeni, J. & Wilmanns, W. (2002) Modulation of acute graft-
versus-host disease after allogeneic bone marrow transplantation by
tumor necrosis factor a (TNF a) release in the course of pretrans-
plant conditioning: role of conditioning regimens and prophylactic
application of a monoclonal antibody neutralizing human TNF a(MAK 195F). Biology of Blood and Marrow Transplantation, 8, 1–8.
Hows, J., Bradley, B., Gore, S. Downie, T., Howard, M. & Gluckman, E.
(1993) Prospective evaluation of unrelated donor bone marrow
transplantation. Bone Marrow Transplantation, 12, 371–380.
Hsu, B., May, R., Carrum, G., Krance, R. & Przepiorka, D. (2001) The
criteria for steroid-refractory acute graft-versus host disease: an
international practice survey. Blood, 98, 663a, (abstr. 2779).
Jacobsohn, D.A. & Vogelsang, G.B. Anti-cytokine therapy for the
treatment of graft-versus-host disease. Current Pharmaceutical
Design, 10, 1195–1205.
Khouri, I.F., Keating, M., Korbling, M., Przepiorka, D., Anderlini, P.,
Obrien, S., Giralt, S., Ippoliti, C., von Wolff, B., Gajewski, J., Do-
nato, M., Claxton, D., Ueno, N., Andersson, B., Gee, A. & Champlin,
R. (1998) Transplant lite: induction of graft versus malignancy using
fludarabine based non ablative chemotherapy and allogeneic blood
progenitor cell transplantation as treatment for lymphoid malig-
nances. Journal of Clinical Oncology, 16, 2817–2824.
Klyushnenkova, E.N., Mosca, J. & McIntosh, K.R. (1998) Human
mesenchymal stem cells suppress allogeneic T cell responses in vitro:
implications for allogeneic transplantation. Blood, 92, 642a.
Kottaridis, P.D., Chakraverty, R., Milligan, D.W., Chakrabarti, S.,
Robinson, S., Chopra, R., Pettengell, R., Marsh, J., Mahendra, P.,
Schey, S., Morgan, G., Williams, C., Hale, G., Waldmann, H., Linch,
D.C., Devereux, S., Glodstone, A.H. & Mackinnon, S. (2000) A non-
myeloablative regimen for allogeneic stem cell transplantation with
a low incidence of GVHD. Bone Marrow Transplantation, 25, S26.
Lan, F., Zeng, D., Higuchi, M., Huie, P., Higgins, J.P. & Strober, S.
(2001) Predominance of NK1.1+TCR alpha beta+ or DX5+TCR
alpha beta+ T cells in mice conditioned with fractionated lymphoid
irradiation protects against graft-versus-host disease: ‘‘natural sup-
pressor’’ cells. Journal of Immunology, 167, 2087–2096.
Laughlin, M.J., Barker, J., Bambach, B., Koc, O.N., Rizzieri, D.A.,
Wagner, J.E., Gerson, S.L., Lazarus, H.M., Cairo, M., Stevens, C.E.,
Rubinstein, P. & Kurtzberg, J. (2001) Hematopoietic engraftment
and survival in adult recipients of umbilical-cord blood from un-
related donors. New England Journal of Medicine, 344, 1860–1861.
Lazarus, H.M., Koc, O.N., Devine, S.M., Curtin, P., Maziarz, R.T.,
Holland, H.K., Shpall, E.J., McCarthy, P., Atkinson, K., Cooper,
B.W., Gerson, S.L., Laughlin, M.J., Loberiza, Jr, F.R., Moseley, A.B.
& Bacigalupo, A. (2005) Cotransplantation of HLA-identical sibling
culture-expanded mesenchymal stem cells and hematopoietic stem
cells in hematologic malignancy patients. Biology of Blood and
Marrow Transplantation, 11, 389–398.
Le Blanc, K., Frassoni, F., Ball, L., Lanino, E., Sundberg, B., Lonnies, L.,
Roelofs, H., Dini, G., Bacigalupo, A., Locatelli, F., Fibbe, W.F. &
Ringden, O. (2006) Mesenchymal stem cells for treatment of severe
acute graft-versus-host disease. Blood (ASH Annual Meeting Ab-
stract), 108, 5304a.
Lee, K.H., Choi, S.J., Lee, J.H., Lee, J.S., Kim, W.K., Lee, K.B., Sohn,
S.K., Kim, J.G., Kim, D.H., Seol, M., Lee, Y.S., Lee, J.H. (2005)
Prognostic factors identifiable at the time of onset of acute graft-
versus-host disease after allogeneic hematopoietic cell transplanta-
tion. Haematologica, 90, 939–948.
Li, A., Zhang, Q., Jiang, J., Yuan, G., Feng, Y., Hao, J., Li, C., Gao, X.,
Wang, G. & Xie, S. (2006) Co-transplantation of bone marrow
stromal cells transduced with IL-7 gene enhances immune recon-
stitution after allogeneic bone marrow transplantation in mice. Gene
Therapy, 13, 1178–1187.
Locatelli, F., Zecca, M., Rondelli, R., Bonetti, F., Dini, G., Prete, A.,
Messina, C., Uderzo, C., Ripaldi, M., Porta, F., Giorgiani, G., Gir-
aldi, E. & Pession, A. (2000) Graft versus host disease prophylaxis
with low dose cyclosporine reduces the risk of relapse in children
with acute leukemia given HLA identical sibling bone marrow
transplantation: results of a randomized trial. Blood, 95, 1572–1579.
Lowsky, R., Takahashi, T., Liu, Y.P., Dejbakhsh-Jones, S., Grumet,
F.C., Shizuru, J.A., Laport, G.G., Stockerl-Goldstein, K.E., Johnston,
L.J., Hoppe, R.T., Bloch, D.A., Blume, K.G., Negrin, R.S. & Strober,
S. (2005) Protective conditioning for acute graft-versus-host disease.
New England Journal of Medicine, 353, 1321–1331.
MacMillan, M.L., Weisdorf, D.J., Davies, S.M., De For, T.E., Burns,
L.J., Ramsay, N.K.C., Wagner, J.E. & Blazar, B.L. (2002) Early an-
tithymocyte globulin therapy improves survival in patients with
steroid-resistant acute graft-versus-host disease. Biology of Blood
Marrow Transplantation, 8, 40–46.
Maeda, Y., Reddy, P., Lowler, K.P., Liu, C., Bishop, D.K. & Ferrara, J.L.
(2005) Critical role of host gammadelta T cells in experimental acute
graft-versus-host disease. Blood, 106, 749–755.
Marmont, A.M., Horowitz, M.M., Gale, R.P., Sobocinski, K., Ash, R.C.,
van Bekkum, D.W., Champlin, R.E., Dicke, K.A., Goldman, J.M. &
Good, R.A. (1991) T-cell depletion of HLA-identical transplants in
leukemia. Blood, 78, 2120–2130.
Martin, P.J. & Kernan, N.A. (1997) T-cell depletion for GHD pre-
vention in humans. In: Graft-versus-host disease (ed. by J.L.M. Fer-
rara & H.J. Deeg), pp. 615–637. Marcel Dekker: New york.
Marty, F.M., Lee, S.J., Fahey, M.M., Alyea, E.P., Soiffer, R.J., Antin,
J.H. & Baden, L.R. (2003) Infliximab use in patients with severe
graft-versus-host disease and other emerging risk factors of non-
Candida invasive fungal infections in allogeneic hematopoietic stem
cell transplant recipients. A cohort study. Blood, 102, 2768–2776.
Mc Donald, K.P., Rowe, V., Clouston, A.D., Welply, J.K., Kuns, R.D.,
Ferrara, J.L., Thomas, R. & Hill, G.R. (2005) Cytokine expanded
myeloid precursors function as regulatory antigen-presenting cells
and promote tolerance through IL-10-producing regulatory T cells.
Journal of Immunology, 174, 1841–1850.
Mielcarek, M. & Storb, R. (2005) Graft-vs-host disease after non-
myeloablative hematopoietic cell transplantation. Leukemia &
Lymphoma, 46, 1251–1260.
Mielcarek, M., Burroughs, L., Leisenring, W., Diaconescu, R., Martin,
P.J., Sandmaier, B.M., Maloney, D.G., Maris, M.B., Chauncey, T.R.,
Shizuru, J.A., Blume, K.G., Hegenbart, U., Niederwieser, D., For-
man, S., Bruno, B., Woolfrey, A. & Storb, R. (2005) Prognostic
relevance of ‘early-onset’ graft-versus-host disease following non-
myeloablative haematopoietic cell transplantation. British Journal of
Haematology, 129, 381–391.
Review
ª 2007 The Author96 Journal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98

Min, D., Taylor, P.A., Panoskaltsis-Mortari, A., Chung, B., Danilenko,
D.M., Farrell, C., Lacey, D.L., Blazar, B.R. & Weinberg, K.I. (2002)
Protection from thymic epithelial cell injury by keratinocyte growth
factor: a new approach to improve thymic and peripheral T-cell re-
constitution after bone marrow transplantation. Blood, 99, 4592–4600.
Minasi, L.E., Kamogawa, Y., Carding, S., Bottomly, K. & Flavell, R.A.
(1993) The selective ablation of interleukin 2 producing cells iso-
lated from transgenic mice. Journal of Experimental Medicine, 177,
1451–1459.
Murphy, W.J., Welniak, L.A., Taub, D.D., Wiltrout, R.H., Taylor, P.A.,
Vallera, D.A., Kopf, M., Young, H., Longo, D.L. & Blazar, B.R.
(1998) Differential effects of the absence of interferon-c and IL-4 in
acute graft-versus-host disease after allogeneic bone marrow trans-
plantation in mice. Journal of Clinical Investigation, 102, 1742–1748.
Nash, R.A., Antin, J.H., Karanes, C., Fay, J.W., Avalos, B.R., Yeager,
A.M. Przepiorka, D., Davies, S., Petersen, F.B., Bartels, P., Buell, D.,
Fitzsimmons, W., Anasetti, C., Storb, R. & Ratanatharathorn, V.
(2000) Phase 3 study comparing methotrexate and tacrolimus with
methotrexate and cyclosporine for prophylaxis of acute graft-versus-
host disease after marrow transplantation from unrelated donors.
Blood, 96, 2062–2068.
Nash, R.A., Johnston, L., Parker, P., McCune, J.S., Storer, B., Slattery,
J.T., Furlong, T., Anasetti, C., Appelbaum, F.R., Lloid, M.E., Deeg,
H.J., Kiem, H.P., Martin, P.J., Schubert, M.M., Witherspoon, R.P.,
Forman, S.J., Blume, K.G. & Storb, R. (2005) A phase I/II study of
mycophenolate mofetil in combination with cyclosporine for pro-
phylaxis of acute graft-versus-host disease after myeloablative con-
ditioning and allogeneic hematopoietic cell transplantation. Biology
of Blood and Marrow Transplantation, 11, 495–505.
Neumann, F., Graef, T., Tapprich, C., Vaupel, M., Steidl, U., Germing,
U., Fenk, R., Hinke, A., Haas, R. & Kobbe, G. (2005) Cyclosporine A
and mycophenolate mofetil vs cyclosporine A and methotrexate for
graft-versus-host disease prophylaxis after stem cell transplantation
from HLA-identical siblings. Bone Marrow Transplantation, 35,
1089–1093.
Noel, D.R., Witherspoon, R.B., Storb, R., Atkinson, K., Doney, K.,
Mickelson, E.M., Ochs, H.D., Warren, R.P., Weiden, P.L. & Thomas,
E.D. (1978) Does graft versus host disease influence the tempo of
immunologic recovery after allogeneic human marrow transplan-
tation? An observation on long-term survivors. Blood, 51, 1087–
1105.
Ordemann, R., Hutchinson, R., Friedman, J., Burakoff, S.J., Reddy, P.,
Duffner, U., Braun, T.M., Liu, C., Teshima, T. & Ferrara, J.L. (2002)
Enhanced allostimulatory activity of host antigen-presenting cells in
old mice intensifies acute graft-versus-host disease. Journal of Clin-
ical Investigation, 109, 1249–1256.
Paulin, T., Ringden, O. & Nilsson, B. (1987) Immunological recovery
after bone marrow transplantation: role of age, graft versus host
disease, prednisolone treatment and infections. Bone Marrow
Transplantation, 1, 317–328.
Peggs, K., Verfuerth, S. & Mackinnon, S. (2001) Induction of cyto-
megalovirus (CMV)-specific T-cell responses using dendritic cells
pulsed with CMV antigen: a novel culture system free of live CMV
virions. Blood, 97, 994–1000.
Perruccio, K., Tosti, A., Burchielli, E., Topini, F., Ruggeri, L., Carotti,
A., Capanni, M., Urbani, E., Mancusi, A., Aversa, F., Martelli, M.F.,
Romani, L. & Velardi, A. (2005) Transferring functional immune
responses to pathogens after haploidentical hematopoietic trans-
plantation. Blood, 106, 4397–4406.
Pittenger, M.F., MacKay, A.M. & Beck, C. (1999) Multilineage potential
of adult human mesenchymal stem cells. Science, 284, 143–145.
Raiola, A.M., van Lint, M.T., Lamparelli, T., Gualandi, F., Mordini, N.,
Berisso, G., Bregante, S., Frassoni, F., Sessarego, M., Fugazza, G., Di
Stefano, F., Pitto, A. & Bacigalupo, A. (2000) Reduced intensity
thiothepa-cyclophosphamide conditioning for allogeneic hemo-
poietic stem cell transplants (HSCT) in patients up to 60 years of
age. British Journal of Haematology, 109, 716–721.
Ramsay, N.K.C., Kersey, J.H., Robinson, L.L., McGlave, P.B., Woods,
W.G., Krivit, W., Kim, T.H., Goldman, A.I. & Nesbit, Jr, M.E.
(1982) A randomized study of the prevention of acute graft versus
host disease. New England Journal of Medicine, 306, 392–397.
Rauser, G., Einsele, H., Sinzger, C., Wernet, D., Kuntz, G., Assenma-
cher, M., Campbell, J.D. & Topp, M.S. (2004) Rapid generation of
combined CMV-specific CD4+ and CD8+ T-cell lines for adoptive
transfer into recipients of allogeneic stem cell transplants. Blood,
103, 3565–3572.
Riddell, S.R., Bleakley, M., Nishida, T., Berger, C. & Warren, E.H.
(2006) Adoptive transfer of allogeneic antigen-specific T cells.
Biology of Blood and Marrow Transplantation, 12, 9–12.
Ringden, O., Uzunel, M., Rasmusson, I., Remberger, M., Sundberg, B.,
Lonnies, H., Marschall, H.U., Dlugosz, A., Szakos, A., Hassan, Z.,
Omazic, B., Aschan, J., Barkholt, L. & Le Blanc, K. (2006) Me-
senchymal stem cells for treatment of therapy-resistant graft-versus-
host disease. Transplantation, 81, 1390–1397.
Rocha, V., Wagner, Jr, J.E., Sobocinski, K.A., Klein, J.P., Zhang, M.J.,
Horowitz, M.M. & Gluckman, E. (2000) Graft-versus-host disease in
children who have received a cord-blood or bone marrow transplant
from an HLA-identical sibling. Eurocord and International Bone
Marrow Transplant Registry Working Committee on Alternative
Donor and Stem Cell Sources. New England Journal of Medicine,
342, 1846–1854.
Rocha, V., Cornish, J., Sievers, E.L., Filipovich, A., Locatelli, F., Peters,
C., Remberger, M., Michel, G., Arcese, W., Dallorso, S., Tiedemann,
K., Busca, A., Chan, K.W., Kato, S., Ortega, J., Vowels, M., Zander,
A., Souillet, G., Oakill, A., Woolfrey, A., Pay, A.L., Green, A., Gar-
nier, F., Ionescu, I., Wernet, P., Sirchia, G., Rubinstein, P., Chevret,
S. & Gluckman, E. (2001) Comparison of outcomes of unrelated
bone marrow and umbelical cord blood transplants in children with
acute leukemia. Blood, 97, 2962–2971.
Rowlings, P.A., Przepiorka, D., Klein, J.P., Gale, R.P., Passweg, J.R.,
Henslee-Downey, P.J., Cahn, J.Y., Calderwood, S., Gratwohl, A.,
Socie, G., Abecasis, M.M., Sobocinski, K.A., Zhang, M.J. & Hor-
owitz, M.M. (1997) IBMTR Severity Index for grading acute graft-
versus-host disease: retrospective comparison with Glucksberg
grade. British Journal of Haematology, 97, 855–864.
Roy, J., McGlave, P.B., Filipovich, A.H., Miller, W.J., Blazar, B.R.,
Ramsay, N.K., Kersey, J.H. & Weisdorf, D.J. (1992) Acute graft
versus-host disease following unrelated donor marrow transplanta-
tion: failure of conventional therapy. Bone Marrow Transplantation,
10, 77–82.
Ruggeri, L., Shlomchik, W.D., Capanni, M., Perruccio, K. & Velardi, A.
(2001) Donor-vs-recipient alloreactive NK cells prevent gVHD by
killing host APC in MHC disparate hematopoietic transplants.
Blood, 98, 813a (abstr. 3378).
Russell, J.A., Tran, H.T., Quinlan, D., Chaudhry, A., Duggan, P.,
Brown, C., Stewart, D., Ruether, J.D., Morris, D., Glick, S., Gyonyor,
E. & Andersson, B.S. (2002) Once-daily intravenous busulfan given
with fludarabine as conditioning for allogeneic stem cell trans-
Review
ª 2007 The AuthorJournal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98 97

plantation: study of pharmacokinetics and early clinical outcomes.
Biology of Blood and Marrow Transplantation, 8, 468–476.
Sale, G.E., Alavaikko, M., Schaefers, K.M. & Mahan, C.T. (1992) Ab-
normal CD4:CD8 ratios and delayed germinal center reconstitution
in lymphnodes of human graft recipients with graft-versus-host
disease (GVHD): an immunohistological study. Experimental He-
matology, 20, 1017–1021.
Schmitz, N., Beksac, M., Hasenclever, D., Bacigalupo, A., Ruutu, T.,
Nagler, A., Gluckman, E., Russell, N., Apperley, J.F., Gorin, N.C.,
Szer, J., Bradstock, K., Buzyn, A., Clark, P., Borkett, K., Gratwohl, A.,
for the European Group for Blood and Marrow Transplantation.
(2002) Transplantation of mobilized peripheral blood cells to HLA
identical siblings with standard risk leukaemia. Blood, 100, 761–767.
Seddik, M., Seemayer, T.A. & Lapp, W.S. (1984) The graft versus host
reaction and immune function. T helper cell immunodeficiency
associated with graft versus host induced thymic epithelial cell da-
mage. Transplantation, 37, 281–286.
Shlomchik, W.D., Couzens, M.S., Tang, C.B., McNiff, J., Robert, M.E.,
Liu, J., Shlomchik, M.J. & Emerson, S.G. (1999) Prevention of graft
versus host disease by inactivation of host antigen-presenting cells.
Science, 285, 412–415.
Slavin, S., Nagler, A., Naparstek, E., Kapelushnik, Y., Aker, M., Civi-
dalli, G., Varadi, G., Kirschbaum, M., Ackerstein, A., Samuel, S.,
Amar, A., Brautbar, C., Ben-Tal, O., Eldor, A. & Or, R. (1998)
Nonmyeloablative stem cell transplantation and cell therapy as an
alternative to conventional bone marrow transplantation with lethal
cytoreduction for the treatment of malignant and nonmalignant
hematologic diseases. Blood, 91, 756–763.
Small, T.N., Papadopoulos, E.B., Boulad, F., Black, P., Castro-Mala-
spina, H., Childs, B.H., Collins, N., Gillio, A., George, D., Jaku-
bowski, A., Heller, G., Fazzari, M., Kernan, N., MacKinnon, S.,
Szabolcs, P., Young, J.W. & O’Reilly, R.J. (1999) Comparison of
immune reconstitution after unrelated and related T-cell depleted
bone marrow transplantation: effect of patient age and donor leu-
kocyte infusions. Blood, 93, 467–480.
Sormani, M.P., Oneto, R., Bruno, B., Fiorone, M., Lamparelli, T.,
Gualandi, F., Raiola, A.M., Dominietto, A., van Lint, M.T., Frassoni,
F., Bruzzi, P. & Bacigalupo, A. (2003) A revised day +7 predictive
score for transplant-related mortalita: serum cholinesterase, total
protein, blood urea nitrogen, c glutamil transeferase, donor type and
cell dose. Bone Marrow Transplantation, 32, 205–211.
Storb, R., Deeg, H.J., Whitehead, J., Appelbaum, F., Beatty, P., Ben-
singer, W., Buckner, C.D., Clift, R., Doney, K., Farewell, V., Hansen,
J., Hill, R., Lum, L., Martin, P., McGuffin, R., Sanders, J., Stewart, P.,
Sullivan, K., Witherspoon, R., Yee, G. & Thomas, E.D. (1986)
Marrow transplantation for leukemia: methotrexate and cyclospor-
ine compared with cyclosporine alone for prophylaxis of GVHD
after marrow transplantation for leukemia. New England Journal of
Medicine, 314, 729–735.
Storb, R., Yu, C., Sanmeier, B.M., Mc Sweeney, P.A., Georges, G.,
Nash, R.A. & Woolfrey, A. (1999) Mixed hemopoietic chimerism
after marrow allografts. Transplantation in the ambulatory care
setting. Annals of the New York Academy of Sciences, 872,
372–375.
Sudres, M., Norol, F., Trenado, A., Gregoire, S., Charlotte, F., Leva-
cher, B., Lataillade, J.J., Bourin, P., Holy, X., Vernant, J.P., Klatz-
mann, D. & Cohen, J.L. (2006) Bone marrow mesenchymal stem
cells suppress lymphocyte proliferation in vitro but fail to prevent
graft-versus-host disease in mice. Journal of Immunology, 176,
7761–7767.
Sykes, M., Szot, G.L., Nguyen, P.L. & Pearson, D.A. (1995) Interleukin-
12 inhibits murine graft-versus-host disease. Blood, 86, 2429–2438.
Sykes, M., Pearson, D.A., Taylor, P.A., Szot, G.L., Goldman, S.J. &
Blazar, B.R. (1999) Dose and timing of interleukin (IL)-12 and
timing and type of total-body irradiation: effects on graft-vs-host
disease inhibition and toxicity of exogenous IL-12 in murine bone
marrow transplant recipients. Biology of Blood and Marrow Trans-
plantation, 5, 277–284.
Teshima, T. & Ferrara, J.L. (2002a) Understanding the alloresponse:
new approaches to graft-versus-host disease prevention. Seminars in
Hematology, 39, 15–22.
Teshima, T., Ordemann, R., Reddy, P., Gagin, S., Liu, C., Cooke, K.R. &
Ferrara, J.L. (2002b) Acute graft-versus-host disease does not require
alloantigen expression on host epithelium. Nature, 8, 575–581.
Trenado, A., Sudres, M., Tang, Q., Maury, S., Charlotte, F., Gregoire, S.,
Bonyhadi, M., Klatzmann, D., Salomon, B.L. & Cohen, J.L. (2006) Ex
vivo-expanded CD4+CD25+ immunoregulatory T cells prevent
graft-versus-host-disease by inhibiting activation/differentiation of
pathogenic T cells. Journal of Immunology, 176, 1266–1273.
Tse, W.T., Beyer, W., Pendleton, J.D., D’Andrea, A. & Guinan, E.C.
(2000) Bone marrow derived mesenchymal stem cells suppress T cell
activation without inducing allogeneic anergy. Blood, 96, 1034a.
Uberti, J.P., Ayash, L., Ratanatharathorn, V., Silver, S., Reynolds, C.,
Becker, M., Reddy, P., Cooke, K.R., Yanik, G., Whitfield, J., Jones,
D., Hutchinson, R., Braun, T., Ferrara, J.L. & Levine, J.E. (2005)
Pilot trial on the use of etanercept and methylprednisolone as pri-
mary treatment for acute graft-versus-host disease. Biology of Blood
and Marrow Transplantation, 11, 680–687.
Van Lint, M.T., Uderzo, C., Locasciulli, A., Majolino, I., Scime, R.,
Locatelli, F., Georgiani, G., Arcese, W., Iori, A.P., Falda, M., Bosi, A.,
Miniero, R., Alessandrino, P., Dini, G., Rotoli, B. & Bacigalupo, A.
(1998) Early treatment of acute graft-versus-host disease with high-
or low-dose 6-methylprednisolone: a multicenter randomized trial
from the Italian Group for Bone Marrow Transplantation. Blood, 92,
2288–2293.
Van Lint, M.T., Milone, G., Leotta, S., Uderzo, C., Scime, R., Dallorso,
S., Locasciulli, A., Guidi, S., Mordini, N., Sica, S., Cudillo, L., Fagioli,
F., Selleri, C., Bruno, B., Arcese, W. & Bacigalupo, A. (2006)
Treatment of acute graft-versus-host disease with prednisolone:
significant survival advantage for day +5 responders and no
advantage for nonresponders receiving anti-thymocyte globulin.
Blood, 107, 4177–4181.
Zander, A.R., Zabelina, T., Kroger, N., Renges, H., Kruger, W., Loliger,
C., Durken, M., Stockschlader, M., de Wit, M., Wacker-Backhaus, G.,
Bielack, S., Jaburg, N., Russmann, B., Erttmann, R. & Kabisch, H.
(1999) Use of a five-agent GvHD prevention regimen in recipients of
unrelated donor marrow. Bone Marrow Transplantation, 23, 889–893.
Zikos, P., van Lint, M.T., Frassoni, F., Lamparelli, T., Gualandi, F.,
Occhini, D., Mordini, N., Berisso, G., Bregante, S., De Stefano, F.,
Soracco, M., Vitale, V. & Bacigalupo, A. (1998) Low transplant
mortality in allogeneic bone marrow transplantation for acute
myeloid leukemia: a randomized study of low-dose cyclosporin
versus low-dose cyclosporin and low-dose methotrexate. Blood, 91,
3503–3508.
Review
ª 2007 The Author98 Journal Compilation ª 2007 Blackwell Publishing Ltd, British Journal of Haematology, 137, 87–98